Abstract
Background and Objectives:
Open surgery has been the mainstay treatment for liver hydatidosis in the past. Today, for treatment of simple and uncomplicated cysts, we have a variety of choices: antihelmintic therapy, the PAIR (puncture, aspiration, injection, and respiration) technique, and the laparoscopic approach. We reviewed our series of 267 cases of hepatic hydatidosis submitted to surgery over a period of 20 years, from 1995 through 2014, comparing the results of these minimally invasive treatments.
Methods:
In 92 patients (25.7% of cases) who presented with complicated liver hydatid cysts, we performed open surgery. In 16.4% of cases (59 patients), we used a laparoscopic approach, and in 208 patients (57.9% of cases), we used the PAIR technique. All patients were monitored after surgery for a mean of 61.7 months (range, 16–127). Postoperative follow-up consisted of clinical examination, laboratory investigation, abdominal ultrasound, and magnetic resonance imaging.
Results:
Almost all patients (198, 95.2%) treated with the PAIR technique and 55 patients (93.2%) treated with the laparoscopic approach were cured. Six patients (2.8%) from the echo-guided puncture group had to undergo a repeat of the procedure because the cavity did not disappear after 2 years. In 4 patients (2%), we performed open surgery for 2 biliary fistulas and 2 hepatic abscesses. Four patients from the laparoscopic group needed additional procedures. Open surgery was necessary in 2 patients for a recurrence after 2 years; 1 patient had developed a liver abscess and the other had a biliary fistula.
Conclusions:
In conclusion, open surgery remains the viable option for complicated cysts, with biliary communication, with multiple daughter vesicles, or with calcified walls. For simple, uncomplicated hydatid cysts, both methods (the PAIR technique and laparoscopic procedure) are safe and efficient, with very good results and low morbidity rates.
Keywords: Laparoscopic approach, Liver hydatidosis, Percutaneous echo-guided puncture
INTRODUCTION
Liver hydatidosis, the parasitic disease produced by Taenia echinococcus granulosus, leads to suffering caused by the complications it generates in both the organ and the whole organism. Pathological consequences in the absence of accurate and timely treatment can be fatal.1,2
General morbidity from hydatid cysts remains high, despite preventative measures taken in many countries. This high morbidity, generating sometimes-important hepatobiliary sequelae, fully justifies the continued interest and attention of clinicians and surgeons worldwide.
Traditionally, surgery has been the only acceptable treatment. Today, modern medical therapy with anthelmintics has been shown to have some advantages, in particular for the prophylaxis of relapses in patients in whom surgery is prohibited.3–5
In 1985, the treatment for hepatic hydatid cyst by echo- or tomographic-guided puncture was evaluated as a modern optimized alternative to surgical therapy. This minimally invasive treatment was initially received with restraint,6 because of fears about secondary peritoneal seeding and the possibility of alcohol-induced cholangitis from instillation of cysts that have cystobiliary communication.
However, after the first reports of percutaneous puncture of a hepatic hydatid cyst followed by alcohol instillation,7 there have been numerous articles showing that the method is safe and efficient and provides good results.8–13 This method was introduced in our clinic starting in March 1996.
The laparoscopic approach to the hydatid cyst emerged in 1993 as an alternative to the classic surgical treatment. We performed our first laparoscopic partial pericystectomy in 1998.
MATERIALS AND METHODS
For this retrospective study, we reviewed the data of all patients admitted with liver hydatidosis between 1995 and 2014. A total of 359 medical records were reviewed. There were 148 men (41%) and 211 women (59%), with a mean age of 36.8 years (range, 6–67 years).
The most frequent clinical symptom was diffuse abdominal pain (179 cases, 49.8%). Hepatomegaly was encountered in 98 patients (27.2%) and abdominal discomfort in 74 (20.6%). Other signs or symptoms were allergic reactions, jaundice, and acute pancreatitis (Table 1). It is important to mention that more than 30% of patients were asymptomatic; the diagnoses were established incidentally during a routine ultrasound examination.
Table 1.
Symptoms of Patients With Liver Hydatidosis
| Symptom | Number of Patients (%)* |
|---|---|
| Abdominal pain | 179 (49.8) |
| Asymptomatic | 112 (31.9) |
| Hepatomegaly | 98 (27.2) |
| Dyspepsia | 74 (20.6) |
| Allergic reactions | 56 (15.5) |
| Jaundice | 32 (8.9) |
| Pancreatic reactions | 5 (1.4) |
| Previous surgery for hydatidosis | 14 (3.8) |
Percentage based on a total of 359 patients.
In our group, there were 14 patients (3.8%) who had undergone surgical procedures for liver hydatidosis, and they presented with a recurrence of the disease after 2–10 years.
All 359 patients underwent a preoperative ultrasound, and the cysts were initially classified according to Gharbi's system.14 After the introduction of the World Health Organization's Informal Working Group on Echinococcosis (WHO-IWGE) classification in 2003,15 we used that ultrasound classification method (Table 2). The number of cysts encountered was 557: 86 patients had 2 cysts and 56 had 3 (Table 3).
Table 2.
Classifications of Cysts
| Gharbi's Classification14 | WHO-IWGE Classification | Number of Patients (%)* |
|---|---|---|
| — | Type CL | 156 (28) |
| Type I | Type CE1 | 107 (19) |
| Type II | Type CE2 | 99 (17) |
| Type III | Type CE3 | 83 (15) |
| Type IV | Type CE4 | 69 (12) |
| Type V | Type CE5 | 43 (9) |
| Total number of cysts | 557 (100) |
Percentage based on a total of 359 patients.
Table 3.
WHO-IWGE Classification of Liver Hydatid Cysts
| Description |
|---|
| Type CL: cystic lesions, anechoic, without visible wall |
| Type CE1: cystic lesions, active, fertile, unilocular, anechoic, with visible wall |
| Type CE2: cystic lesions, active, fertile, with multiple daughter vesicles, multilocular |
| Type CE3: transitional cyst, with germinate membrane detached |
| Type CE4: inactive cyst, scratchy aspect |
| Type CE5: inactive cyst, calcified wall |
Four hundred nine cysts were located in the right liver lobe, and the mean diameter of the cysts was 6.7 cm (range, 3–19 cm). There were also multiple locations of the cysts: lung (7 cases), spleen (3 cases), pancreas (2 cases), peritoneum (2 cases), and diaphragm (1 case) (Table 4).
Table 4.
Cyst Characteristics
| Type/Characteristics | Data |
|---|---|
| Hepatic, n (%) (n = 557) | |
| Right lobe | 409 (73) |
| Left lobe | 148 (27) |
| Extrahepatic, n | |
| Lung | 7 |
| Splenic | 3 |
| Pancreas | 2 |
| Peritoneal | 2 |
| Diaphragmatic | 1 |
| Cysts/patient, n patients | |
| Single | 217 |
| Two | 86 |
| Three | 56 |
| Cyst size | Mean, 6.7 cm (range, 3–19 cm) |
Preoperative workups included computed tomography or magnetic nuclear resonance and biochemical and immunochemistry profiles. All patients were treated with 10–15 mg/kg albendazole, starting 1 to 3 days before the procedure and for 1 to 3 months afterward.
The year 1996 saw the start of our minimally invasive treatment of liver hydatidosis. We performed echo-guided puncture in the operating room in patients under general intravenous anesthesia. We started with the measurement of the cyst volume and then inserted an 18–22-gauge echo-guided needle. It is very important to insert the needle through the liver parenchyma, to avoid spillage of the hydatid liquid. We aspirated as much liquid as was consistent with the hydatid cyst's measured volume. We inspected to determine whether the suctioned liquid was clear, and alcohol, at a temperature of 98 degrees, was injected equal to one-third of the amount removed. The liquid was maintained for 10 minutes, after which it was aspirated. Initially, we selected the patients strictly from types CL and CE1, but later we performed the procedure, even in patients with CE2 cysts.
For the laparoscopic approach, we used the same manner as in the open approach in cases of partial pericystectomy. We put gauze dressing with hypertonic saline solution around the cyst and inserted the aspiration needle into the cavity, where we instilled hypertonic saline solution. After 10 min, we aspirated the cysts and drilled a small hole in them for better aspiration of the hydatid liquid. We extracted the germinative membrane or daughter vesicles and put them into an Endobag (Covidien, Dublin, Ireland). We controlled the cavity of the cysts and, if biliary leakage appeared, we performed a suture of the biliary fistula. After the procedure, these patients were sent for an endoscopic sphincterectomy. Finally, we placed a drainage tube into the cavity for several days.
RESULTS
In a group of 359 patients, minimally invasive treatment was performed in 267 (74.3%) and open surgery in 92 (25.7%) (Table 4).
We employed the PAIR (puncture, aspiration, injection, and respiration) technique in 208 patients (57.9%), and opted for a laparoscopic approach in 59 (16.4%) (Table 5). Only patients with CL, CE1, and CE2 liver hydatid cysts were selected for minimally invasive treatment (puncture or laparoscopy) after WHO-IWGE sonographic classification of the liver hydatidosis.
Table 5.
Procedures Performed
| Type | Number of Patients (%) |
|---|---|
| Echo-guided aspiration | 208 (57.9) |
| Laparoscopic partial/total pericystectomy | 59 (16.4) |
| Open partial/total pericystectomy | 92 (25.7) |
| Total | 3 |
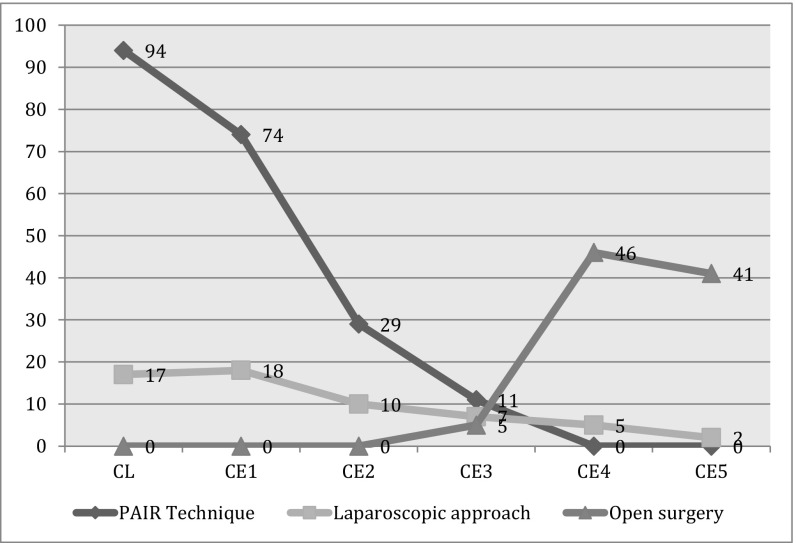
For the laparoscopic approach, the cysts were located mostly in the left liver lobe or in the lateral segments, as they were easy to manage. After gaining sufficient expertise in the laparoscopic field, we performed the laparoscopic approach, even for types CE3, CE4, and CE5. In terms of location, we can now resolve any segment of the liver laparoscopically, except for those cysts located in the central segments (Figure 1).
Figure 1.
Procedures performed.
All patients were followed up for a mean of 61.7 months (range, 16–127). Postoperative follow-up consisted of clinical examination, laboratory investigation, abdominal ultrasound, and computed tomography.
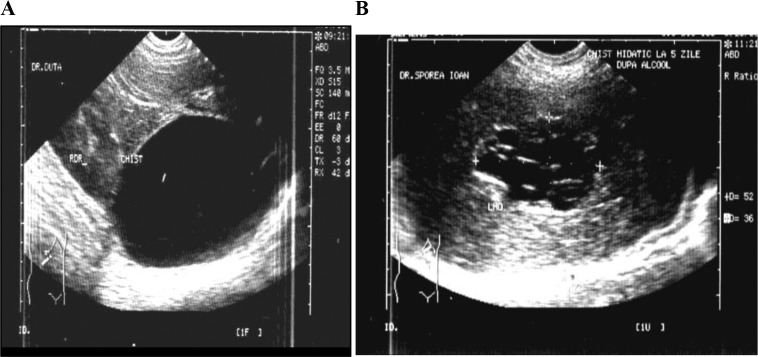
The patients treated by echo-guided puncture were cured in 95.2% of cases (198 patients). A decrease in the hepatic cavity was noted for up to 2 years after the puncture. We encountered a mean decrease in cavity of 73% after 1 month (range, 54–100%) and 89% after 1 year (range, 72–100%) (Figure 2).
Figure 2.
Ultrasound aspects before (A) and after (B) the PAIR technique.
Six patients (2.8%) from the echo-guided puncture group underwent a repeat of the procedure, because the cavity did not disappear after 2 years. Four patients (2%) needed a classic reoperation, in 2 cases because of the development of liver abscesses and in 2 others because of biliary fistulas.
We had 8 patients (3.8%) with allergic reactions after puncture that were easily controlled with corticoids and antihistamines.
The patients treated by the laparoscopic approach were cured in 93.2% of cases (55 patients). In 4 cases, we had to perform an open procedure: in 2 patients for of a recurrence after 2 years, in 1 patient for a liver abscess, and in 1 for a biliary fistula (Figure 3).
Figure 3.
Laparoscopic approach for a cyst located in segment VIII type CE4.
The mean hospital stay was 2.9 days (range, 1–5) after an echo-guided puncture and 3.6 days (range, 2–8) after a laparoscopic procedure. The mortality rate was nil.
DISCUSSION
There is still a great deal of controversy regarding the management of liver hydatidosis. Initially, open surgery was the only accepted treatment for this disease. In recent decades, however, dramatic changes have taken place. The first was the introduction of percutaneous echo-guided puncture, which was met with strong opposition. In fact, the procedure contravenes many of the principles of hydatid surgery, such as inserting a needle into the cyst cavity without the fear of disseminating the hydatid liquid. For this reason, there are several recommendations associated with it, such as that the needle should always be inserted through the liver's parenchyma to avoid spreading the liquid contents.18–20
There are no randomized studies to compare the results of percutaneous treatment with other surgical procedures. Gupta et al21 published a retrospective study that compared 52 patients treated with the PAIR technique, with or without drainage, with 61 patients treated with radical/excisional surgery and 33 with conservative surgery. In 10 patients, the PAIR procedure was abandoned because of an initial aspiration of an unclear liquid, which indicates a cysto-biliary communication. It was concluded that for a safe PAIR procedure, it is very important to select only patients with type I or II cysts, according to Gharbi's classification.14
In our study, 57.9% of the patients were selected for the PAIR procedure. The percentage can be explained by the changes in the early diagnosis of liver hydatidosis which translates into higher percentages of type CL, CE1, and CE2 cysts, in which percutaneous treatment is the procedure of choice, with very good results.
We noted that age is an important factor in the time needed for disappearance of liver cavities. Thus, children need healing time that averages up to 1 year, but in patients over 50 years of age, a decrease in the maximum diameter of the cavity took up to 2 years. If the cavity had not disappeared after 2 years, we performed another puncture, as happened in 6 patients.
There are no randomized studies to compare open versus laparoscopic treatment of liver hydatidosis. In a retrospective study, Zaharie et al22 compared 59 patients treated with the laparoscopic approach with 172 patients treated with open surgery. They concluded that the laparoscopic approach is safe for the treatment of liver hydatidosis in almost all segments of the liver.
In our study, after the first period, we selected only cysts located in the left lobe, but now we consider that cysts in almost all segments are suitable for the laparoscopic approach, and almost all types of cysts can be resolved using this approach. In our experience, even type CE4 or CE5 cysts can be managed laparoscopically.
Regarding safety, there are many methods described for avoiding leakage of the hydatid liquid at the moment of the first insertion of a needle into the cyst.23–26 In our opinion, isolating the area around the cyst, using precautions when inserting the needle, and administering albendazole for at least 1 month after the procedure is sufficient, and we did not have any peritoneal recurrences after using the laparoscopic or percutaneous approach.
CONCLUSION
In dealing with the hepatic hydatid cyst, treatment must be adapted to each patient, depending on the stage of development, location, size, and complications of the cyst.
Classic radical or conservative surgery should remain an option for solving complicated cysts. For simple cysts, the uncomplicated minimally invasive treatment option should be considered the best course of action.
Both the laparoscopic approach and the ultrasound guided puncture are safe and effective procedures, but, with a difficult cyst location, a puncture should be considered.
Contributor Information
Ciprian Duta, Surgical Clinic 2, University of Medicine and Pharmacy, “V. Babes,” Timisoara, Romania..
Stelian Pantea, Surgical Clinic 2, University of Medicine and Pharmacy, “V. Babes,” Timisoara, Romania..
Caius Lazar, Surgical Clinic 2, University of Medicine and Pharmacy, “V. Babes,” Timisoara, Romania..
Abdullah Salim, Surgical Clinic 2, University of Medicine and Pharmacy, “V. Babes,” Timisoara, Romania..
Daniela Barjica, Surgical Clinic 2, University of Medicine and Pharmacy, “V. Babes,” Timisoara, Romania..
References:
- 1. Milicevic M. Hydatid disease. In: Baumgart LH, ed. Surgery of the Liver and Biliary Tract. London: Churchill Livingston; 1994:1121–1150. [Google Scholar]
- 2. Kune GA, Morris DL. Hydatid disease. In: Maingot's Abdominal Operations. 9th ed, vol 2 Schwartz SI, Ellis H, eds. Stamford, CT: Appleton & Lange; 1990, pp 1225–1239. [Google Scholar]
- 3. Ammann RW, Fleiner-Hoffmann A, Grimm F, Eckert J. Long-term mebendazole therapy may be parasitocidal (sic) in alveolar echinococcosis. J Hepatol. 1998;29:994–998. [DOI] [PubMed] [Google Scholar]
- 4. Franchi C, Di Vico B, Teggi A. Long-term evaluation of patients with hydatidosis treated with benzimidazole carbamates. Clin Infect Dis. 1999;29:304–309. [DOI] [PubMed] [Google Scholar]
- 5. Gomez i Gavara C, López-Andújar R, Belda Ibáñez T, et al. Review of the treatment of liver hydatid cysts. World J Gastroenterol. 2015;21:124–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Livraghi T, Damascelli B, Lombardi C, Spagnoli I. Risk in fine-needle abdominal biopsy. J Clin Ultrasound. 1983;11:77–81. [DOI] [PubMed] [Google Scholar]
- 7. Mueller PR, Dawson SL, Ferrucci JT, Nardi GL. Hepatic echinococcal cyst: successful percutaneous drainage. Radiology 1985;155:627–628. [DOI] [PubMed] [Google Scholar]
- 8. Akhan O, Ozmen MN. Percutaneous treatment of liver hydatid cysts. Eur J Radiol. 1999;32:76–85. [DOI] [PubMed] [Google Scholar]
- 9. Bastid C, Azar C, Doyle M, Sahel J. Percutaneous treatment of hydatid cysts under sonographic guidance. Digest Dis Sci. 1994;39:1576–1580. [DOI] [PubMed] [Google Scholar]
- 10. Giorgio A, Tarantino L, de Stefano G, et al. Long term follow-up of echoguided percutaneous aspiration and ethanol injection in the treatment of unilocular and multilocular hydatid liver cysts. Newsletter Int Assoc Hydatidol. 1998:16:10. [Google Scholar]
- 11. Khuroo MS, Zargar SA, Mahajan R. Echinococcus granulosus cysts in the liver: management with percutaneous drainage. Radiology. 1991;180:141–145. [DOI] [PubMed] [Google Scholar]
- 12. Ormeci N, Soykan I, Bektas A, et al. A new percutaneous approach for the treatment of hydatid cysts of the liver. Am J Gastroenterol. 2001;96:2225–2230. [DOI] [PubMed] [Google Scholar]
- 13. Nasseri-Moghaddam S, Abrishami A, Taefi A, Malekzadeh R. Percutaneous needle aspiration, injection, and re-aspiration with or without benzimidazole coverage for uncomplicated hepatic hydatid cysts. Cochrane Database Syst Rev. 2011:CD003623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gharbi HA, Hassin W, Braener MW, Dupich K. Ultrasound examination of the hydatid liver. Radiology. 1981;139:459–463. [DOI] [PubMed] [Google Scholar]
- 15. WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253–261. [DOI] [PubMed] [Google Scholar]
- 16. Smego RA, Bhatti S, Khaliq AA, Beg MA. Percutaneous aspiration-injection-respiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis. 2003;37:1073–1083. [DOI] [PubMed] [Google Scholar]
- 17. Brunetti E, Troia G, Garlaschelli AL, Gulizia R, Filice C. Twenty years of percutaneous treatments for cystic echinococcosis: a preliminary assessment of their use and safety. Parasitologia. 2004;46:367–370. [PubMed] [Google Scholar]
- 18. Brunetti E, Filice C. Percutaneous treatment of a complex hydatid cyst of the liver under sonographic control: a cautionary note. Gastroenterol Clin Biol. 2006;30:1107. [DOI] [PubMed] [Google Scholar]
- 19. Akhan O, Ozmen MN, Dincer A, Sayek I, Gocmen A. Liver hydatid disease: long-term results of percutaneous treatment. Radiology. 1996;198:259–264. [DOI] [PubMed] [Google Scholar]
- 20. Bosanac ZB, Lisanin L. Percutaneous drainage of hydatid cyst in the liver as a primary treatment: review of 52 consecutive cases with long-term follow-up. Clin Radiol. 2000;55:839–848. [DOI] [PubMed] [Google Scholar]
- 21. Gupta N, Javed A, Puri S, Jain S, Singh S, Agarwal AK. Hepatic hydatid: PAIR, drain or resect? J Gastrointest Surg. 2011;15:1829–1836. [DOI] [PubMed] [Google Scholar]
- 22. Zaharie F, Bartos D, Mocan L, Zaharie R, Iancu C, Tomus C. Open or laparoscopic treatment for hydatid disease of the liver? A 10-year single-institution experience. Surg Endosc. 2013;27:2110–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sinha R, Sharma N. Abdominal hydatids: a minimally invasive approach. JSLS 2001;5:237–240. [PMC free article] [PubMed] [Google Scholar]
- 24. Bicket A, Norman L, Benjamin S. Laparoscopic treatment of hydatid cyst of the liver initial experience with a small series of patients. J Laparoendosc Surg. 1994;4:127–133. [DOI] [PubMed] [Google Scholar]
- 25. Aarons BJ, Kune GA. A suction cone to prevent spillage during hydatid surgery. Aust N Z J Surg. 1983;53:471–472. [DOI] [PubMed] [Google Scholar]
- 26. Mompean JAL, Paricio PP, Camprs RR, Ayllowo GG. Laparoscopic treatment of a liver hydatid cyst. Br J Surg. 1993;80:907–908. [DOI] [PubMed] [Google Scholar]