Abstract
Correct definition of the level of risk of invasive fungal infections is the first step in improving the targeting of preventive strategies. We investigated the potential relationship between pre-hospitalization exposure to sources of fungi and the development of invasive fungal infections in adult patients with newly diagnosed acute myeloid leukemia after their first course of chemotherapy. From January 2010 to April 2012, all consecutive acute myeloid leukemia patients in 33 Italian centers were prospectively registered. Upon first admission, information about possible pre-chemotherapy risk factors and environmental exposure was collected. We recorded data regarding comorbid conditions, employment, hygienic habits, working and living environment, personal habits, hobbies, and pets. All invasive fungal infections occurring within 30 days after the first course of chemotherapy were recorded. Of the 1,192 patients enrolled in this study, 881 received intensive chemotherapy and were included in the present analysis. Of these, 214 developed an invasive fungal infection, including 77 proven/probable cases (8.7%). Of these 77 cases, 54 were proven/probable invasive mold infections (6.1%) and 23 were proven yeast infections (2.6%). Upon univariate analysis, a significant association was found between invasive mold infections and age, performance status, diabetes, chronic obstructive pulmonary disease, smoking, cocaine use, job, hobbies, and a recent house renovation. Higher body weight resulted in a reduced risk of invasive mold infections. Multivariate analysis confirmed the role of performance status, job, body weight, chronic obstructive pulmonary disease, and house renovation. In conclusion, several hospital-independent variables could potentially influence the onset of invasive mold infections in patients with acute myeloid leukemia. Investigation of these factors upon first admission may help to define a patient’s risk category and improve targeted prophylactic strategies.
Introduction
Invasive fungal infections in patients with hematologic malignancies have increased during the last few years, particularly in patients with acute myeloid leukemia (AML).1,2 These complications are associated with a high risk of infection-related death; furthermore, experiencing an invasive fungal infection may affect the outcome of the hematologic malignancy.3 For these reasons, during the last few years, much effort has been devoted to optimizing the prevention of invasive fungal infections for those patients in high-risk categories.4–6 Antifungal prophylaxis with newer azoles (e.g., posaconazole) has shown good efficacy, although newer azoles cost more and confer a higher risk of resistance.7
Stratifying risk for invasive fungal infection is the logical first step in identifying patients who would most likely benefit from antifungal prophylaxis, more intensive monitoring or early treatment. A patient’s risk level is the result of multiple factors, such as the presence of an underlying malignancy (including therapies and immune status), factors intrinsic to the patient (genetic pattern, comorbidities, performance status) and the environment (in or out of the hospital).8 The role of air concentrations of fungi during hospitalization has been investigated in several studies, and it has been shown to correlate with the onset of aspergillosis in susceptible patients.9,10 In contrast, the role of hospital-independent exposure to sources of fungi (e.g., in the home or in the work place) is not known.
The aim of the present study was to evaluate the potential relationship between pre-chemotherapy risk factors and the onset of invasive fungal infection after the first induction treatment.
Methods
The present prospective study was conducted in 33 hematology wards of tertiary care centers or university hospitals located throughout Italy from January 1st, 2010 to April 30th, 2012. All adult patients with newly diagnosed AML were consecutively included in the registry and monitored. A minimum follow-up of 90 days after completion of the first cycle of chemotherapy was required. The last patient entered the trial on April 30th, 2012, and the last follow-up was completed on July 31st, 2012. The ethics committee of each participating site approved the use of the SEIFEM registry.
This was a non-interventional study. Accordingly, the enrollment of a patient had no impact on the standard clinical practice of the participating hematology units. The data were entered prospectively into case report forms that were divided into two parts.
The first part was compiled at the time of first admission to the hematology ward and included questions about AML subtype and treatment, demographic data and personal history before hospitalization. In particular, the following information was collected: age, gender, race, body weight, comorbid conditions [diabetes, chronic obstructive pulmonary disease (COPD), renal or hepatic failure], performance status, job, hobbies, workplace, home (area of residence, type of house, pets/poultry ownership, exposure to plants or fireplace) and personal habits (alcohol, use of illicit drugs). The type of hospital (teaching versus non-teaching) and the season of diagnosis were also included in the analysis.
The second part of the case report form was compiled on the 30th day after the end of the first cycle of chemotherapy, and it collected data regarding post-chemotherapy factors, particularly the level and duration of neutropenia, mucosal damage, vomiting, diarrhea, the presence of medical devices (e.g., urinary catheter, central venous catheter) and antifungal prophylaxis. Antifungal prophylaxis was given according to local clinical practice, and none of the analyzed pre-hospital risk factor was used a priori as a trigger for prescription.
The diagnostic work-up in the cases of fever was similar at all participating centers and included the following tests: nasal, pharyngeal, and rectal swabs at the time of admission; blood cultures and chest radiography at onset of fever; galactomannan assays twice weekly and a chest computed tomography (CT) scan on the fourth to seventh day of fever. Additional examinations (e.g., abdominal ultrasound scan, sinus or brain CT, skin biopsy, bronchoalveolar lavage, or fundus examination) were performed when clinically indicated.
The presence of invasive fungal infection was assessed within the first 30 days after chemotherapy had ended, according to current EORTC criteria.11
Definitions
Various terms were defined before data analysis. Neutropenia was defined as an absolute neutrophil count of <500 cells/mm3. Neutropenia was considered prolonged if the duration was 10 days and severe if the absolute neutrophil count was <100 cells/mm3. Mucositis was graded according to the World Health Organization (WHO).12 High risk jobs included those employments more likely to expose the patient to fungal spores, such as construction work, farming, gardening, being a florist shop employee, and forestry work.13 High risk hobbies included those activities that were more likely to expose the participants to fungal spores, such as hunting, gardening, fishing, and hiking.13 Being overweight was defined as having a body mass index ≥30 kg/m2.14 Performance status was graded according to the Eastern Cooperative Oncology Group scale.15 Invasive fungal infections were classified according to the 2008 European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) criteria.11
Patients with proven/probable mold infections were termed “mold cases”. Patients with possible mold infections were considered to have insufficient evidence of infection and were excluded from the analysis. Patients with proven yeast infections were termed “yeast cases”. Patients without any evidence of invasive fungal infection were termed “controls” and were compared to both the yeast and mold cases (Figure 1).
Figure 1.
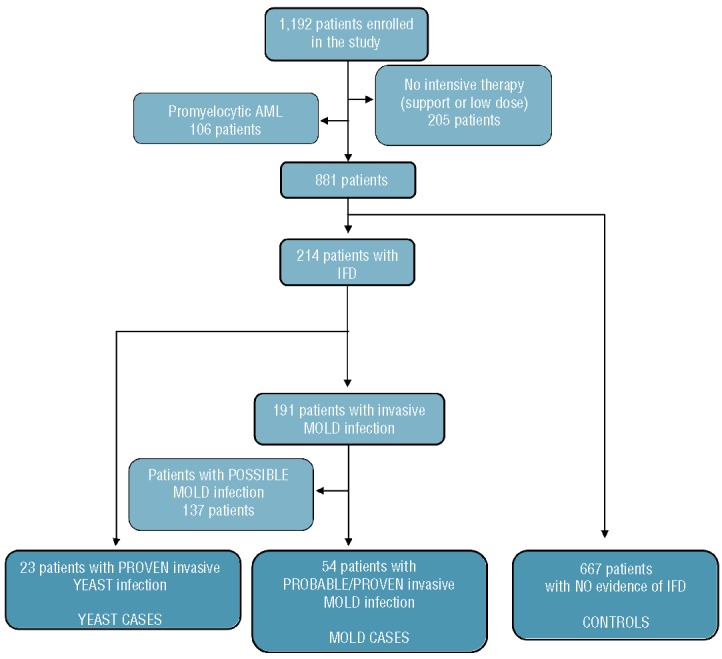
Study flow chart. IFD:invasive fungal disease.
Statistical analysis
Values are expressed as the mean ± standard deviation or median (range) (continuous variables) or as a percentage of the group from which they were derived (categorical variables). Continuous variables were compared using the Student t-test for normally distributed variables or the Mann-Whitney U test for non-normally distributed variables. Categorical variables were evaluated using the χ2 test or the two-tailed Fisher exact test. Variables associated with the onset of an invasive fungal infection in univariate analysis (P≤0.10) were included in a logistic regression analysis, and a backward stepwise approach was used to identify those factors independently associated with the onset the infection. The area under the receiver-operator characteristics (ROC) curve was calculated for the predictive model. A P-value less than 0.05 was considered statistically significant. All statistical analyses were performed with the Intercooled Stata software program, version 11 for Windows (StataCorp, College Station, TX, USA).
Results
Over a 28-month period, 1,192 adult patients with newly diagnosed AML from 33 participating centers were enrolled in this study [male 48.8%, median age 58 years (interquartile range, 47–66 years)]. Of these, 205 patients received only low-dose antineoplastic therapies or palliative treatments and were excluded from the present analysis (Figure 1). Another 106 patients were diagnosed with promyelocytic leukemia and were also excluded. The present analysis focuses on the 881 AML patients who received conventional intensive chemotherapy.
Among the 712 evaluable patients who were treated with systemic prophylaxis, the majority received posaconazole prophylaxis (n=439, 61.7%); the remaining patients received either fluconazole (n=81, 11.4%), or itraconazole (n=149, 20.9%) or other drugs (n=19, 2.7%).
Over a 28-month period, 214 cases of invasive fungal infection were recorded (incidence 24.3%); 23 were invasive yeast infections (incidence 2.6%), while the other 191 cases were attributed to molds (incidence 21.5%). The majority of these cases were possible mold infections (n=137, 71.7%; incidence 15.5%), while the remaining 54 cases were classified as probable/proven invasive mold infections (28.3%, incidence 6.1%). In particular, seven cases were classified as proven invasive mold infections.
Mold cases
Fifty-four patients with proven/probable invasive mold infections (mold cases) were compared to 667 controls (Figure 1). Mold cases were more often older than 50 years (83% versus 67%, P=0.015) and had a poorer performance status at the time of admission (Table 1A). Higher body weight was found to reduce the risk of invasive mold infection. No differences were found with regards to patients’ race. Similarly, neither the type of hospital (teaching versus non-teaching) nor the season was significant.
Table 1A.
Univariate analysis of the main PRE-chemotherapy risk factors for proven/probable invasive fungal infection.
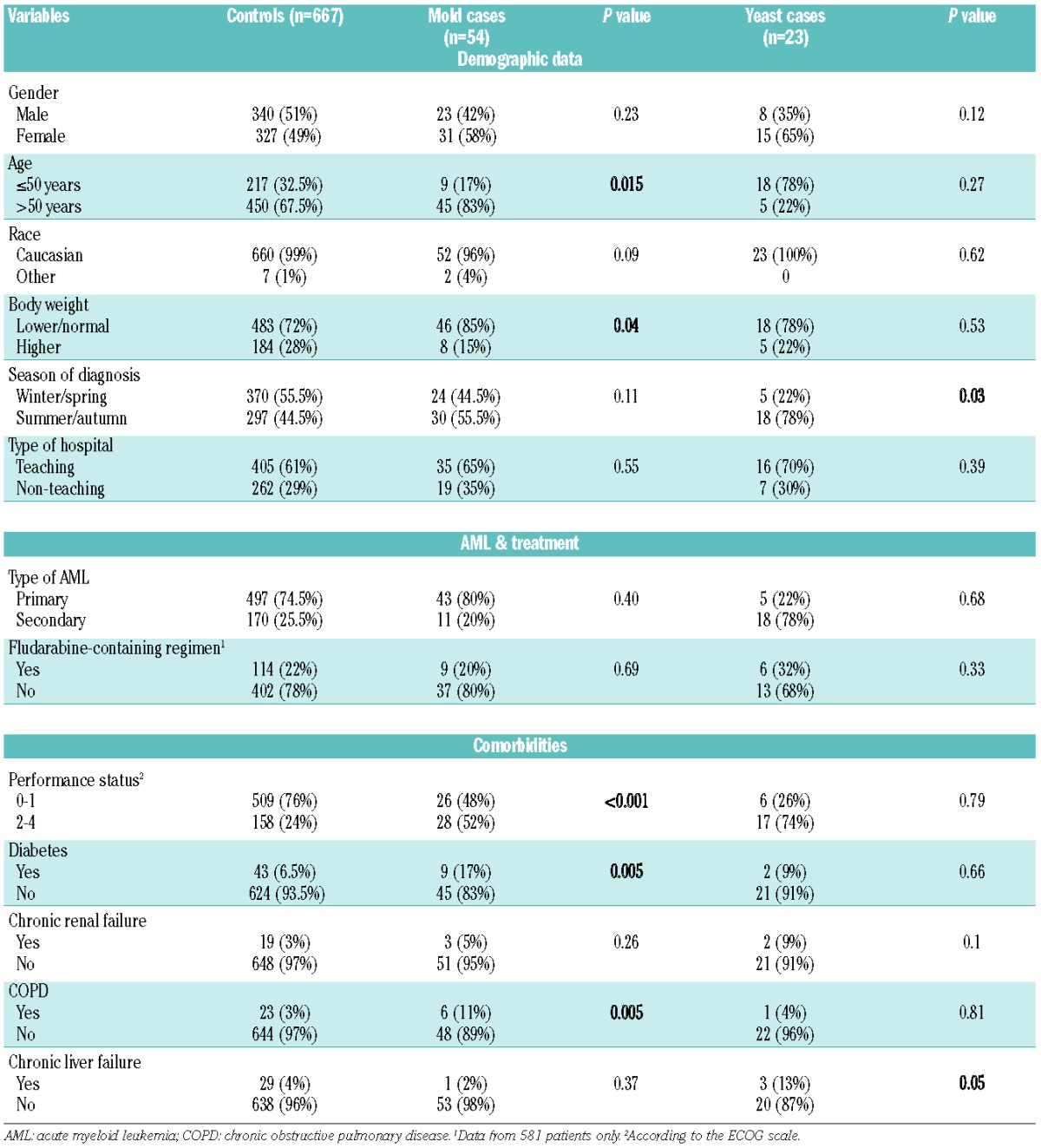
The frequency of therapy-related AML was similar between cases and controls (20.4% versus 25.5%, P=0.4). A fludarabine-containing chemotherapeutic regimen did not appear to represent an additional risk factor (Table 1A). Both diabetes and COPD were more frequent in mold cases than in the controls, while the frequency of chronic renal failure and liver disease was similar between the two groups.
Data regarding personal habits and working and living environment are reported in Table 1B. Cigarette smoking and cocaine abuse were associated with invasive mold infections (P=0.02 and P=0.006, respectively), while no significant association was observed for marijuana use or regular alcohol assumption. Notably, alcohol abuse was reported by only three patients. Hobbies involving high exposure to fungal agents were associated with invasive mold infections (18.5% in cases versus 8.7% in controls, P=0.017). A possible correlation between invasive mold infections and jobs with high exposure to fungal agents was also found (P=0.0001). Among the working and living place factors, only a recent house renovation (within the 6 months preceding the diagnosis of AML) was found to be more frequent in the mold cases (24% versus 9.6%, P<0.001).
Table 1B.
Univariate analysis of the main PRE-chemotherapy risk factors for proven/probable invasive fungal infection.
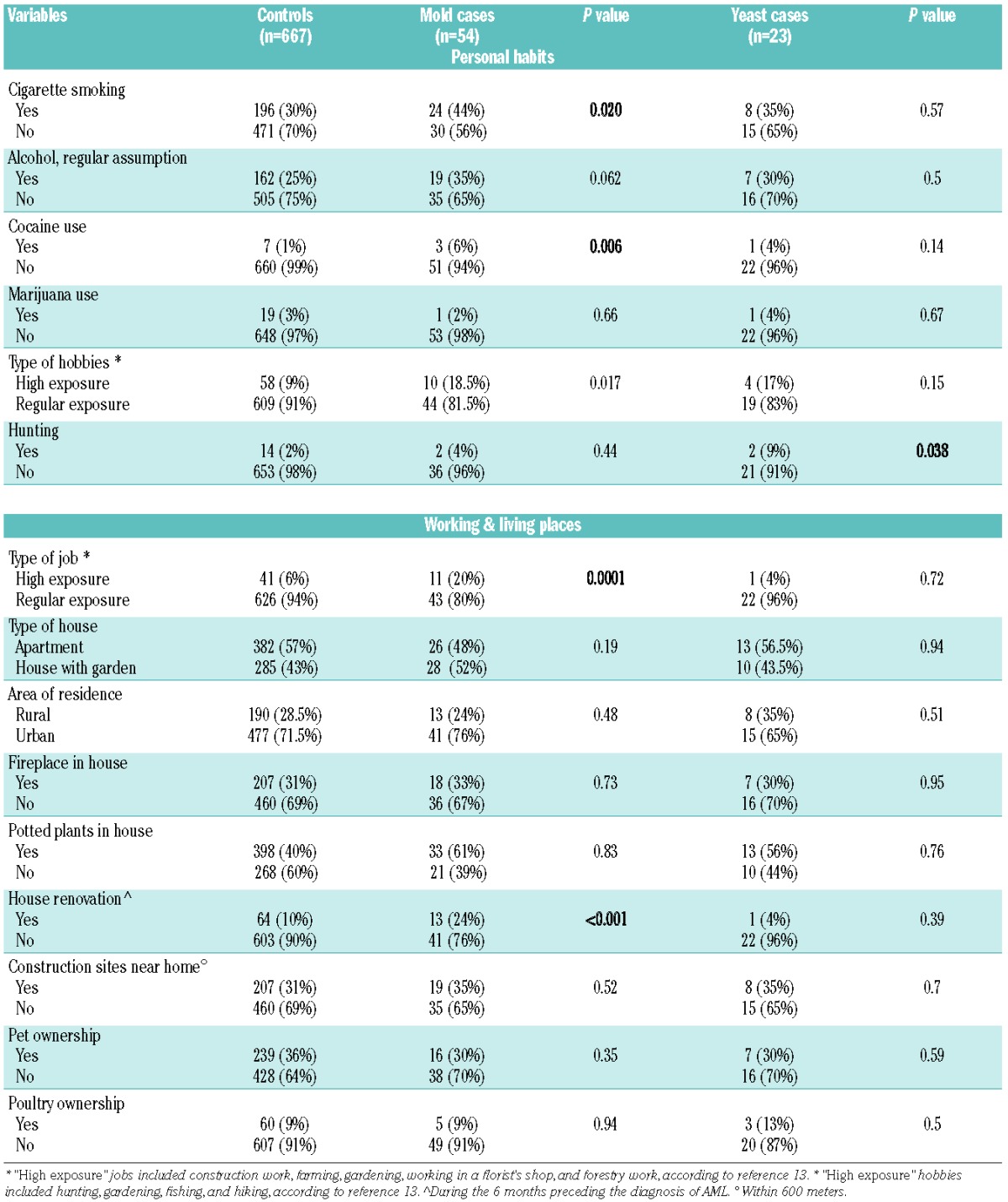
When considering post-treatment variables, we found an increased risk of invasive mold infection in patients with grade 3–4 esophagitis (Table 2). Systemic prophylaxis (with any drug) resulted in protection from invasive mold infection onset. Posaconazole was the most frequently used drug and it emerged as a protective factor (P=0.002).
Table 2.
Univariate analysis of the main POST-chemotherapy risk factors for proven/probable invasive fungal infections.
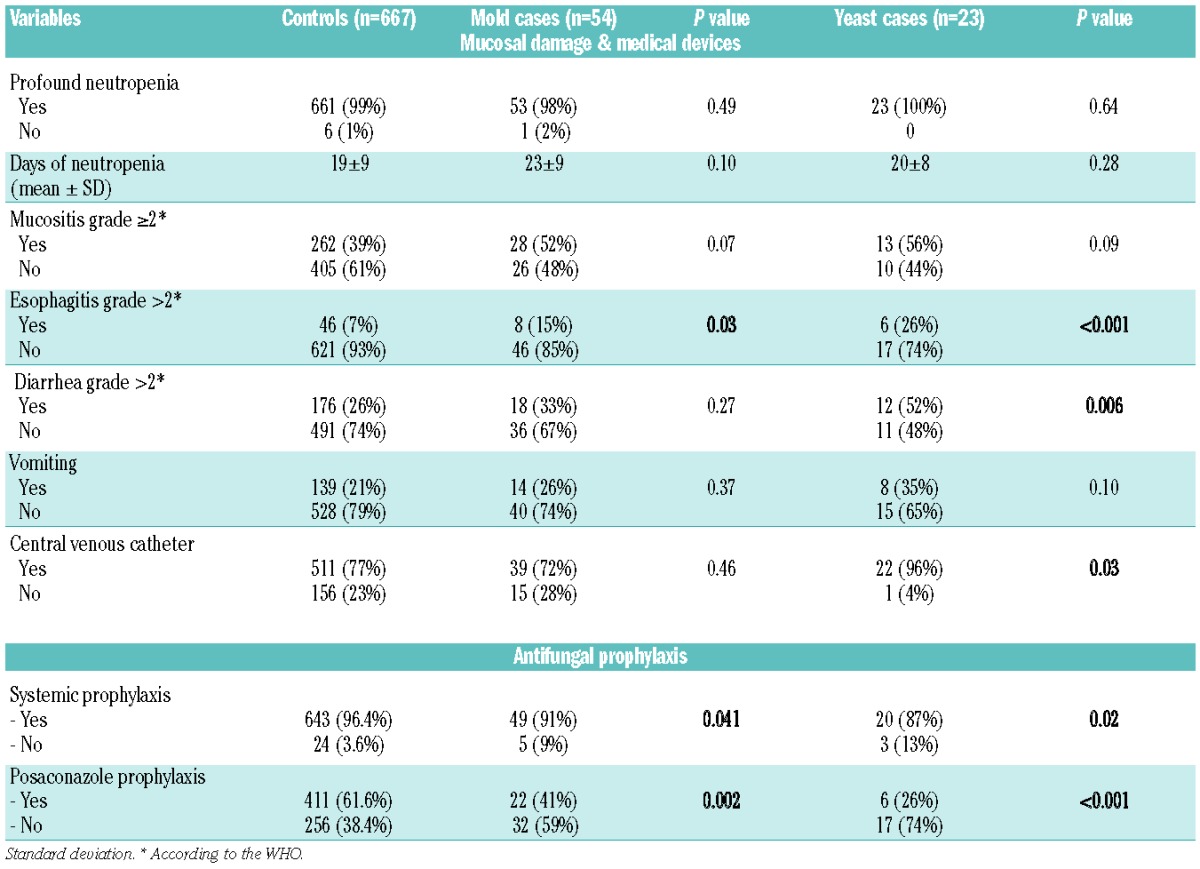
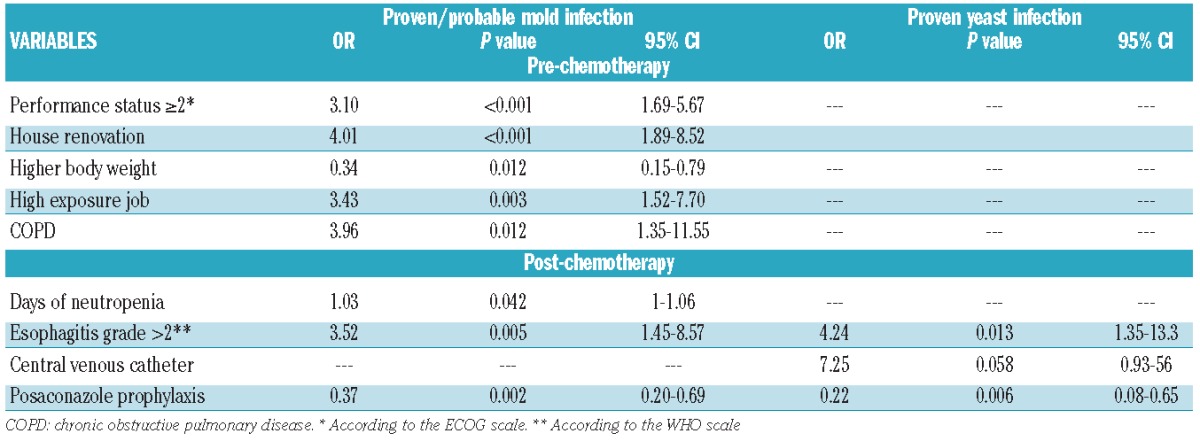
Pre- and post-chemotherapy variables were thus included in a common multivariate model for evaluating the risk of proven/probable invasive mold infections. As for pre-chemotherapy variables, the analysis confirmed that a performance status of 2 or greater (P<0.001), a recent house renovation (during the 6 months preceding the diagnosis of AML) (P<0.001), higher body weight (P=0.012), job with high exposure (P=0.003) and COPD (P=0.012) significantly influenced the onset of mold infections. Of the post-treatment variables, three remained statistically significant: posaconazole prophylaxis (protective factor, P=0.002) and days of neutropenia and esophagitis (both risk factors, P=0.042 and P=0.005, respectively) (Table 3).
Table 3.
Multivariate analysis of the PRE- and POST-chemotherapy risk factors for proven/probable invasive mold infections and proven yeast infections.
The logistic regression model exhibited good discrimination, with an area under the ROC curve of 0.77 (Figure 2).
Figure 2.
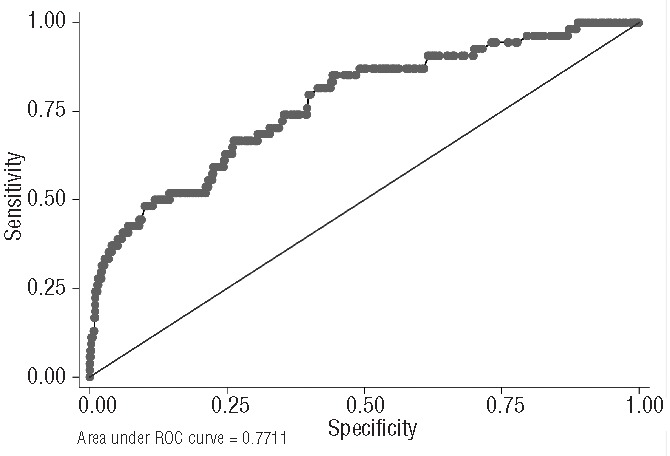
Receiver-operator characteristic (ROC) curve for the multivariate model for invasive mold infections.
Yeast cases
Twenty-three patients with proven invasive yeast infections (yeast cases) were compared to 667 controls (Figure 1). Upon univariate analysis of pre-chemotherapy variables, chronic liver disease and hunting were found to be more frequent in the yeast cases than in the controls (Table 1A,B).
Post-chemotherapy risk factors that emerged as significantly influencing the onset of invasive yeast infections were the presence of a central venous catheter (P=0.03), grade 3–4 esophagitis (P<0.001), and grade 3–4 diarrhea (P=0.006) (Table 2). Posaconazole prophylaxis significantly reduced the incidence of yeast infections.
The impact of esophagitis, posaconazole prophylaxis and a central venous catheter in influencing the risk of yeast infections was confirmed by multivariate analysis; however, none of the pre-chemotherapy variables was shown to independently influence the risk of invasive yeast infections, according to the final multivariate model (Table 3).
Discussion
Underlying hematologic malignancies and neutropenia have been recognized as crucial risk factors for invasive fungal infections.16,17 However, it is well known that only a few patients among those considered at the highest risk (i.e., patients with AML) will develop an invasive fungal infection. With this in mind, it has been proven that many other factors, both intrinsic and extrinsic, modifiable and not, should be considered when defining a patient’s risk level.8
To our knowledge, this is the first prospective study analyzing the impact of potential risk factors for invasive fungal infections at the time of the patients’ first admission. The multicenter study allowed an analysis of a large cohort of hematologic patients. Enrollment was limited to those patients with newly diagnosed AML; furthermore, to increase the homogeneity of our study population, we excluded those patients who had not received either intensive (hypomethylating agents, support) or highly myelosuppressive regimens (promyelocytic leukemia).
In several previous studies, the first induction of remission was proven to be the phase at which patients with AML were at highest risk of invasive fungal infections.18 It has, therefore, been speculated that pre-hospital exposure to fungi may play a role in invasive fungal infections. However, while the crucial role of the patient’s environment during hospitalization has been clearly demonstrated, the role of the environment outside the hospital is more difficult to evaluate.19,20 We assumed that some variables (location of residence, type of house, presence of potted plants, etc.) may be a surrogate indicator of the patient’s exposure to spores in the air.21 Not surprisingly, we found a strong correlation (confirmed by multivariate analysis) between a recent house renovation and the onset of an invasive mold infection. This is congruent with reports of outbreaks of invasive aspergillosis during construction work in hospitals.20
Pet ownership has been traditionally associated with fungal zoonoses.22,23 For this reason, we analyzed the risk of pet owners and hunters in particular, but neither of these variables emerged as a significant risk factor for invasive fungal infections in our cohort.24
Patients are generally advised against gardening and other activities exposing them to dust that may contain spores, even though the role of such activities has never been proven. In our analysis “high exposure” hobbies and jobs were more frequent in patients with invasive mold infections. It can be speculated that such activities may have led to mold colonization in the patients prior to their hospitalization.
In a study by Panackal et al., it was found that the incidence of invasive aspergillosis was higher during the summer and autumn.25 This seasonal difference in incidence did not emerge in our series, in which invasive mold infections were equally distributed throughout the year. In contrast, a higher proportion of yeast cases occurred during the summer and autumn.
Specific personal habits relating to exposure were also investigated. In a previous similar study, a sub-analysis of a small subgroup of AML patients revealed them to be at higher risk if they were cigarette smokers.21 Both tobacco and cannabis contain fungal spores that may contaminate the lower respiratory tract.26,27 In addition, nicotine has marked effects on the immune response system and has been reported to inhibit the release of some cytokines (e.g., interleukin-6, tumor necrosis factor-a) and to depress the functions of murine alveolar macrophages.28,29 In our experience, there was an association between smoking and invasive mold infections only in the univariate analysis. Similarly, alcohol is known to have multiple effects on host immune responses, including depletion of circulating lymphocytes and reduction of the Th1 cytokine response, which is protective against microbial infections,30,31 but we did not find any correlation between alcohol and invasive fungal infections in our study.
Smoking marijuana has been reported to be associated with pulmonary aspergillosis because of the possible contamination of the leaves by Aspergillus spp.32,33 This correlation was not confirmed in our series, most likely due to the very low number of patients reporting marijuana use. In contrast, cocaine emerged as a possible risk factor for invasive mold infections in the univariate analysis. The effects of this drug on immunity have been extensively investigated, mainly in murine models and in vitro studies. Nearly all of these studies have shown a correlation with reduced immune function, including both cellular and humoral immunity.31
Performance status and comorbid conditions can easily be evaluated at the time of first admission. Diabetes is a well-known risk factor for mucormycosis, but it has never been investigated in patients with invasive aspergillosis, nor in a prospective study of a large cohort of patients.34,35 In our analysis, diabetes was more frequent in mold cases, suggesting a potential role as an additional risk factor for all invasive mold infections. Patients with severe COPD who receive broad-spectrum antibiotics and corticosteroids are becoming one of the main risk groups for invasive pulmonary aspergillosis.36 However, the role of COPD as a potential additional risk factors in hematologic patients has never been investigated before. In our study, both univariate and multivariate analyses confirmed COPD as an additional risk factor in AML patients.
In the last few years, an association between liver failure and invasive aspergillosis has been suspected.37,38 Because patients with AML have abnormal cellular and humoral immunity, they may be unable to eliminate inhaled conidia, and this may predispose them to invasive aspergillosis.39 Our study did not confirm such an association, but this may be related to the very low number of patients reporting a history of hepatic disease. Renal dysfunction has been reported to be a risk factor for invasive aspergillosis in lung transplant recipients.40 This relationship did not emerge from our analysis.
Surprisingly, we found that patients with a higher body mass index were protected from invasive mold infections and that this relationship was highly significant upon multivariate analysis. Some smaller studies have shown that obese subjects may have an altered response to sepsis. Some investigations have focused on hormonal mediators, including leptin and adiponectin, showing that their levels are altered.41,42 Both these alterations were correlated with human survival of sepsis, although the relationships were complex and the studies involved few patients.
Hospital- and treatment-dependent risk factors were also analyzed because they are potentially confounding variables in our analysis. It was impossible to prove the role of severe neutropenia in either mold or yeast infections because all patients received intensive chemotherapy and were, thus, all profoundly neutropenic. However, an association between the duration of neutropenia and the risk of invasive mold infections was confirmed.
In a recent single center analysis conducted at the M.D. Anderson Cancer Center involving 165 patients with AML, those receiving investigational clofarabine-containing protocols and those with therapy-related disease were at higher risk of invasive fungal infections, with the effect of clofarabine-containing protocols being confirmed in the multivariate analysis.43 Both these variables were included in our analysis, but neither resulted predictive of the onset of invasive fungal infections.
The protective role of posaconazole prophylaxis in high-risk patients has been demonstrated in several clinical trials and confirmed in clinical experience.4–6,44 According to these previous results, posaconazole prophylaxis resulted in a significantly reduced incidence of mold infections.6 The higher number of patients in the present analysis allowed us to prove the protective role of posaconazole against yeast infections as well.
Post-treatment variables were the only variables that were significantly related to yeast cases in the multivariate analysis. This is likely because of the differing pathogenesis of yeast infections, which are related to mucosal damage rather than to entrance via the respiratory system.
In conclusion, our study indicates several chemotherapy-independent risk factors for mold infections in patients with AML; these risk factors include hospital-independent exposure to infectious agents, comorbidities and personal habits. The recognition of these factors at the time of admission may be useful to define a patient’s risk category better and to improve targeted prophylactic, diagnostic and therapeutic measures. Assessing the coexistence of these risk factors to anticipate the risk of invasive mold infections may be feasible and useful for all centers, particularly those with limited resources.
Acknowledgments
Other contributors (SEIFEM Group): Annarosa Cuccaro, Giulia Dragonetti, Università Cattolica del Sacro Cuore, Roma; Marta Stanzani, Riccardo Ragionieri, Istituto di Ematologia ed Oncologia Clinica “Lorenzo e Ariosto Serágnoli,” Ospedale S.Orsola-Malpighi, Università di Bologna; Francesca Antoniazzi, Div. di Ematologia-Spedali Civili Brescia; Sergio Storti, Università Cattolica del Sacro Cuore, Campobasso; Mario Luppi, Dipartimento di Oncologia ed Ematologia, Università di Modena e Reggio Emilia, Azienda Ospedaliera Policlinico, Modena; Simona Pagliuca, Azienda Ospedaliera Universitaria Federico II Napoli, Dipartimento di Medicina Clinica e Chirurgia; Elena Rossetti, Sezione di Ematologia, Università di Parma; Matteo Da Vià, Dipartimento Onco-Ematologico, Fondazione ICRRS Policlinico San Matteo, Pavia; Luigi Di Caprio, Unità di Ematologia, Università Tor Vergata, Roma; Ignazio Majolino, Divisione di Ematologia, Ospedale S. Camillo, Roma; Nicola Cascavilla, Divisione di Ematologia, IRCCS Ospedale S. Giovanni Rotondo; Gloria Turri, UOC Ematologia, Azienda Ospedaliera Universitaria Integrata di Verona; Renato Fanin, Clinica di Ematologia, Università di Udine.
Footnotes
The online version of this article has a Supplementary Appendix.
Authorship and Disclosures
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Pagano L, Caira M, Picardi M, et al. Invasive aspergillosis in patients with acute leukemia: update on morbidity and mortality--SEIFEM-C Report. Clin Infect Dis. 2007; 44(11):1524–1525. [DOI] [PubMed] [Google Scholar]
- 2.Perkhofer S, Lass-Flörl C, Hell M, et al. The Nationwide Austrian Aspergillus Registry: a prospective data collection on epidemiology, therapy and outcome of invasive mould infections in immunocompromised and/or immunosuppressed patients. Int J Antimicrob Agents. 2010;36(6):531–536. [DOI] [PubMed] [Google Scholar]
- 3.Even C, Bastuji-Garin S, Hicheri Y, et al. Impact of invasive fungal disease on the chemotherapy schedule and event-free survival in acute leukemia patients who survived fungal disease: a case-control study. Haematologica. 2011;96(2):337–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cornely OA, Maertens J, Winston DJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356(4):348–359. [DOI] [PubMed] [Google Scholar]
- 5.Ullmann AJ, Lipton JH, Vesole DH, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356(4):335–347. [DOI] [PubMed] [Google Scholar]
- 6.Pagano L, Caira M, Candoni A, et al. Evaluation of the practice of antifungal prophylaxis use in patients with newly diagnosed acute myeloid leukemia: results from the SEIFEM 2010-B registry. Clin Infect Dis. 2012;55(11):1515–1521. [DOI] [PubMed] [Google Scholar]
- 7.Georgiadou SP, Kontoyiannis DP. The impact of azole resistance on aspergillosis guidelines. Ann NY Acad Sci. 2012; 1272:15–22. [DOI] [PubMed] [Google Scholar]
- 8.Pagano L, Akova M, Dimopoulos G, Herbrecht R, Drgona L, Blijlevens N. Risk assessment and prognostic factors for mould-related diseases in immunocompromised patients. J Antimicrob Chemother 2011;66(S1):i5–14. [DOI] [PubMed] [Google Scholar]
- 9.Oren I, Haddad N, Finkelstein R, Rowe JM. Invasive pulmonary aspergillosis in neutropenic patients during hospital construction: before and after chemoprophylaxis and institution of HEPA filters. Am J Hematol. 2001;66(4):257–262. [DOI] [PubMed] [Google Scholar]
- 10.Flynn PM, Williams BG, Hetherington SV, Williams BF, Giannini MA, Pearson TA. Aspergillus terreus during hospital renovation. Infect Control Hosp Epidemiol. 1993; 14(7):363–365. [DOI] [PubMed] [Google Scholar]
- 11.de Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parulekar W, Mackenzie R, Bjarnason G, Jordan RC. Scoring oral mucositis. Oral Oncol. 1998;34(1):63–71. [DOI] [PubMed] [Google Scholar]
- 13.Sipsas NV, Kontoyiannis DP. Occupation, lifestyle, diet, and invasive fungal infections. Infection. 2008;36(6):515–525. [DOI] [PubMed] [Google Scholar]
- 14.Kuperman EF, Showalter JW, Lehman EB, Leib AE, Kraschnewski JL. The impact of obesity on sepsis mortality: a retrospective review. BMC Infect Dis. 2013;13(1):377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655. [PubMed] [Google Scholar]
- 16.Bodey GP. The changing face of febrile neutropenia-from monotherapy to moulds to mucositis. Fever and neutropenia: the early years. J Antimicrob Chemother. 2009; 63(S1):i3–13. [DOI] [PubMed] [Google Scholar]
- 17.Pagano L, Caira M, Candoni A, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006; 91(8):1068–1075. [PubMed] [Google Scholar]
- 18.Pagano L, Caira M, Candoni A, et al. Invasive aspergillosis in patients with acute myeloid leukemia: SEIFEM-2008 registry study. Haematologica. 2010;95(4):644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cristina ML, Sartini M, Spagnolo AM. Health care-acquired aspergillosis and air conditioning systems. J Prev Med Hyg. 2009; 50(1):3–8. [PubMed] [Google Scholar]
- 20.Weber DJ, Peppercorn A, Miller MB, Sickbert-Benett E, Rutala WA. Preventing healthcare-associated Aspergillus infections: review of recent CDC/HICPAC recommendations. Med Mycol. 2009;47(S1):199–209. [DOI] [PubMed] [Google Scholar]
- 21.Blum G, Eschertzhuber S, Auberger J, et al. Airborne fungus exposure prior to hospitalisation as risk factor for mould infections in immunocompromised patients. Mycoses. 2012;55(3):237–243. [DOI] [PubMed] [Google Scholar]
- 22.Litwin CM. Pet-transmitted infections: diagnosis by microbiologic and immunologic methods. Pediatr Infect Dis J. 2003;22(9): 768–777. [DOI] [PubMed] [Google Scholar]
- 23.Schubach A, Schubach TM, Barros MB, Wanke B. Cat-transmitted sporotrichosis, Rio de Janeiro, Brazil. Emerg Infect Dis. 2005;11(12):1952–1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Armstrong CW, Jenkins SR, Kaufman L, Kerkering TM, Rouse BS, Miller GB., Jr Common-source outbreak of blastomycosis in hunters and their dogs. J Infect Dis. 1987; 155(3):568–570. [DOI] [PubMed] [Google Scholar]
- 25.Panackal AA, Li H, Kontoyiannis DP, et al. Geoclimatic influences on invasive aspergillosis after hematopoietic stem cell transplantation. Clin Infect Dis. 2010; 50(12):1588–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verweij PE, Kerremans JJ, Voss A, Meis JF. Fungal contamination of tobacco and marijuana. JAMA. 2000;284(22):2875. [DOI] [PubMed] [Google Scholar]
- 27.Szyper-Kravitz M, Lang R, Manor Y, Lahav M. Early invasive pulmonary aspergillosis in a leukemia patient linked to aspergillus contaminated marijuana smoking. Leuk Lymphoma. 2001;42(6):1433–1437. [DOI] [PubMed] [Google Scholar]
- 28.Sopori M. Effects of cigarette smoke on the immune system. Nat Rev Immunol. 2002; 2(5):372–377. [DOI] [PubMed] [Google Scholar]
- 29.Ouyang Y, Virasch N, Hao P, et al. Suppression of human IL-1beta, IL-2, IFN-gamma, and TNF-alpha production by cigarette smoke extracts. J Allergy Clin Immunol. 2000; 106(2):280–7. [DOI] [PubMed] [Google Scholar]
- 30.Szabo G, Mandrekar P. A recent perspective on alcohol, immunity, and host defense. Alcohol Clin Exp Res. 2009;33(2):220–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedman H, Pross S, Klein TW. Addictive drugs and their relationship with infectious diseases. FEMS Immunol Med Microbiol. 2006;47(3):330–342. [DOI] [PubMed] [Google Scholar]
- 32.Levitz SM, Diamond RD. Aspergillosis and marijuana. Ann Intern Med. 1991;115(7): 578–579. [DOI] [PubMed] [Google Scholar]
- 33.Gargani Y, Bishop P, Denning DW. Too many mouldy joints - marijuana and chronic pulmonary aspergillosis. Mediterr J Hematol Infect Dis. 2011;3(1):e2011005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caira M, Trecarichi EM, Mancinelli M, Leone G, Pagano L. Uncommon mold infections in hematological patients: epidemiology, diagnosis and treatment. Expert Rev Anti Infect Ther. 2011;9(7):881–892. [DOI] [PubMed] [Google Scholar]
- 35.Rammaert B, Lanternier F, Poirée S, Kania R, Lortholary O. Diabetes and mucormycosis: a complex interplay. Diabetes Metab. 2012; 38(3):193–204. [DOI] [PubMed] [Google Scholar]
- 36.Guinea J, Torres-Narbona M, Gijón P, et al. Pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: incidence, risk factors, and outcome. Clin Microbiol Infect. 2010;16(7):870–877. [DOI] [PubMed] [Google Scholar]
- 37.Wang W, Zhao CY, Zhou JY, et al. Invasive pulmonary aspergillosis in patients with HBV-related liver failure. Eur J Clin Microbiol Infect Dis. 2011;30(5):661–667. [DOI] [PubMed] [Google Scholar]
- 38.Li D, Chen L, Ding X, Tao R, Zhang YX, Wang JF. Hospital-acquired invasive pulmonary aspergillosis in patients with hepatic failure. BMC Gastroenterol. 2008;8:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheruvattath R, Balan V. Infections in patients with end-stage liver disease. J Clin Gastroenterol. 2007;41(4):403–411. [DOI] [PubMed] [Google Scholar]
- 40.Gordon SM, Avery RK. Aspergillosis in lung transplantation: incidence, risk factors, and prophylactic strategies. Transpl Infect Dis. 2001;3(3):161–167. [DOI] [PubMed] [Google Scholar]
- 41.Bornstein SR, Licinio J, Tauchnitz R, et al. Plasma leptin levels are increased in survivors of acute sepsis: associated loss of diurnal rhythm, in cortisol and leptin secretion. J Clin Endocrinol Metab. 1998;83(1): 280–283. [DOI] [PubMed] [Google Scholar]
- 42.Walkey AJ, Rice TW, Konter J, et al. Plasma adiponectin and mortality in critically ill subjects with acute respiratory failure. Crit Care Med. 2010;38(12):2329–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gomes M, Mulanovich V, Ying J, Lewis R, Kontoyiannis D. Risk factors for invasive fungal infections in acute myeloid leukaemia patients during primary antifungal prophylaxis at M.D. Anderson Cancer Center, 2009–2011. Poster P1002. 23rd ECCMID Berlin 27–30 April 2013. [Google Scholar]
- 44.Pagano L, Caira M, Cuenca-Estrella M. The management of febrile neutropenia in the posaconazole era: a new challenge? Haematologica. 2012;97(7):963–965. [DOI] [PMC free article] [PubMed] [Google Scholar]


