ABSTRACT
Highly pathogenic avian influenza viruses of the H5N1 subtype continue to circulate in poultry in Asia, Africa, and the Middle East. Recently, outbreaks of novel reassortant H5 viruses have also occurred in North America. Although the number of human infections with highly pathogenic H5N1 influenza viruses continues to rise, these viruses remain unable to efficiently transmit between humans. However, we and others have identified H5 viruses capable of respiratory droplet transmission in ferrets. Two experimentally introduced mutations in the viral hemagglutinin (HA) receptor-binding domain conferred binding to human-type receptors but reduced HA stability. Compensatory mutations in HA (acquired during virus replication in ferrets) were essential to restore HA stability. These stabilizing mutations in HA also affected the pH at which HA undergoes an irreversible switch to its fusogenic form in host endosomes, a crucial step for virus infectivity. To identify additional stabilizing mutations in an H5 HA, we subjected a virus library possessing random mutations in the ectodomain of an H5 HA (altered to bind human-type receptors) to three rounds of treatment at 50°C. We isolated several mutants that maintained their human-type receptor-binding preference but acquired an appreciable increase in heat stability and underwent membrane fusion at a lower pH; collectively, these properties may aid H5 virus respiratory droplet transmission in mammals.
IMPORTANCE We have identified mutations in HA that increase its heat stability and affect the pH that triggers an irreversible conformational change (a prerequisite for virus infectivity). These mutations were identified in the genetic background of an H5 HA protein that was mutated to bind to human cells. The ability to bind to human-type receptors, together with physical stability and an altered pH threshold for HA conformational change, may facilitate avian influenza virus transmission via respiratory droplets in mammals.
INTRODUCTION
Highly pathogenic H5N1 avian influenza viruses are now enzootic in poultry populations throughout Southeast Asia and Egypt (1). However, these viruses lack the ability to efficiently transmit between humans despite continuing reports of diagnosed cases by the World Health Organization (http://www.who.int/influenza/human_animal_interface/H5N1_cumulative_table_archives/en/). The hemagglutinin (HA) protein of influenza A viruses is a type 1 transmembrane glycoprotein that confers virus binding to host cell receptors (2). The receptor-binding pocket, located in the globular head region of the HA1 subunit (2), mediates influenza virus binding to oligosaccharides containing terminal sialic acid residues (3). Influenza viruses circulating in humans typically bind to sialic acid residues attached to galactose in an α2,6 linkage (Siaα2,6Gal), whereas influenza viruses circulating in avian species preferentially bind to sialic acid residues attached to galactose in an α2,3 linkage (Siaα2,3Gal) (3). In addition to their preferential binding to Siaα2,3Gal, some H5N1 viruses also bind to a limited extent to human-type receptors (4, 5); however, such viruses still lack the ability to transmit among ferrets via respiratory droplets (6). Furthermore, the experimental introduction of amino acids that promote human-type receptor-binding specificity to avian H5 HA proteins does not produce a virus that transmits among ferrets via respiratory droplets (7, 8).
Recently, we (8) and others (9–11) identified H5 viruses that can transmit via respiratory droplets in ferrets or guinea pigs. We introduced human-type receptor-binding mutations (N224K and Q226L, H3 numbering) into the HA protein of the A/Vietnam/1203/2004 (H5N1) strain and generated a reassortant virus with the remaining seven viral RNA segments from the human A/California/04/2009 (H1N1) virus (8). After two passages in ferrets, the virus acquired the ability to transmit via respiratory droplets in these animals (8). The ferret-transmissible H5 virus possessed additional mutations in HA that eliminated a potential glycosylation site in HA (N158D) and increased the protein's stability (T318I) (8). Further testing demonstrated that the mutations that conferred human-type receptor-binding specificity also reduced HA stability, requiring compensatory mutations (8). Fouchier and colleagues introduced human-type receptor-binding mutations into an avian H5N1 virus and performed sequential virus passages in ferrets, followed by respiratory droplet transmission studies in these animals (9). Sequence analysis of a variant that transmitted among ferrets via respiratory droplets revealed additional mutations in HA (9), one of which also conferred stability to the protein (12, 13). Together, these two studies demonstrated that mutations that alter the receptor-binding preference of HA may reduce the protein's stability, leading to the need for additional compensatory stabilizing mutations for the virus to be respiratory droplet transmissible.
The HA protein comprises two disulfide bridge-linked subunits (HA1 and HA2) that exist in infecting viruses in a spring-loaded metastable confirmation (14). During receptor-mediated endocytosis, HA undergoes an irreversible conformational change when exposed to the increasingly acidic environment of late endosomes. This conformational change exposes the hydrophobic N terminus of the HA2 subunit (also called the “fusion peptide”), which triggers fusion of the endosomal and viral membranes and the release of viral ribonucleoprotein complexes into the cytosol of infected cells. The pH threshold at which HA undergoes the conformational change and triggers membrane fusion differs among influenza viruses of different subtypes and among influenza viruses isolated from different hosts (reviewed in reference 15). Highly pathogenic avian H5N1 HAs trigger membrane fusion at pH ∼5.5 to 6.0 (16–18), whereas contemporary human H1N1 and H3N2 HAs undergo the conformational change and membrane fusion at a more acidic pH of ∼5.0 to 5.5 (18). Interestingly, the N224K/Q226L mutations in HA that confer binding to human cells increased the pH threshold for membrane fusion, whereas the T318I (8) and H110Y (12) mutations that emerged during virus replication in ferrets reduced the pH threshold for membrane fusion. Here, we sought to identify additional mutations in H5 HA that increase physical stability and reduce the pH optimum of fusion. Such mutations may affect respiratory droplet transmission in mammals of an H5 virus that binds to human-type receptors and replicates efficiently in mammalian cells.
MATERIALS AND METHODS
Cells.
Madin-Darby canine kidney (MDCK) cells overexpressing Siaα2,6Gal (AX4 cells) (19, 20) were maintained in Eagle minimal essential medium (MEM) containing 5% newborn calf serum (NCS) and antibiotics. Human embryonic kidney 293T cells were maintained in Dulbecco modified Eagle medium containing 10% fetal bovine serum (FBS) and antibiotics. Human epithelial HeLa cells were maintained in MEM containing 10% FBS and antibiotics. All cells were maintained at 37°C in 5% CO2.
Plasmids.
Plasmids for viral RNA production contained the individual viral gene segments bordered by the human RNA polymerase I promoter and the mouse RNA polymerase I terminator sequences as described previously (21). For reassortant viruses possessing the A/Vietnam/1203/2004 (H5N1; VN1203) HA and neuraminidase (NA) genes in the genetic background of A/Puerto Rico/8/34 (H1N1; PR8) virus, the multibasic amino acid sequence at the VN1203 HA cleavage site (RERRRKKR↓G; the arrow indicates the cleavage site) was changed to RETR↓G by site-directed mutagenesis.
Viruses.
All viruses were generated using plasmid-driven reverse genetics as described previously (21). Recombinant viruses were amplified in AX4 cells and stored at −80°C until use. The HA segment of all viruses was sequenced to ensure the absence of unwanted mutations. All experiments with viruses possessing the VN1203 HA gene with the multibasic cleavage sequence in HA in the genetic background of the human A/California/04/2009 (H1N1; CA04) virus were performed in enhanced biosafety level 3 (BSL3) containment laboratories approved for such use by the Centers for Disease Control and Prevention (CDC) and the U.S. Department of Agriculture (USDA). All experiments with VN1203/PR8 reassortant viruses (possessing a single basic amino acid at the VN1203 HA cleavage site) were performed in BSL2 laboratories after these viruses were exempted from Select Agent status and approved for work in BSL2 containment. Viruses used for tissue-binding studies and glycan arrays were inactivated by incubating them with 0.1% β-propiolactone (final concentration).
Library construction.
Random mutations were introduced into the ectodomain (amino acids 17 to 531; H3 numbering) of the VN1203 HA protein by using the GenoMorph II random mutagenesis kit (Agilent). A mutation rate of 2 to 3 amino acids was achieved by optimization of PCR cycles and was confirmed by using Sanger sequencing. Mutant PCR products were introduced into an RNA transcription plasmid encoding the remaining portions of HA. The resultant plasmid library was used to generate the mutant virus library as described previously (8).
Thermostability assay.
Aliquots of viruses and virus libraries were transferred to 0.5-ml tubes and incubated in a heat block at 50°C for 10 min, 20 min, 30 min, 1 h, or 2 h. After the designated length of heat treatment, samples were immediately placed on ice. Infectivity and hemagglutination activity were determined using plaque and HA assays, respectively.
HA assay.
Viruses (50 μl) were serially diluted with 50 μl of phosphate-buffered saline (PBS) in a U-well microtiter plate. Portions (50 μl) of 0.5% (vol/vol) turkey red blood cells (TRBCs) were added to each well. The plates were incubated at room temperature, and hemagglutination was evaluated after 45 min.
Plaque assay.
Viruses were diluted in a 10-fold dilution series, in duplicate, with MEM containing 0.3% bovine serum albumin (BSA). Monolayers of AX4 cells in a 12-well plate were washed with PBS, inoculated with 50 μl of virus dilutions, and incubated for 30 min at 37°C. Cells were washed with MEM containing 0.3% BSA and overlaid with a mixture of MEM containing 0.3% BSA, agarose (1:1), and TPCK (tolylsulfonyl phenylalanyl chloromethyl ketone)-trypsin (0.5 μg/ml). Plates were incubated at 37°C for 48 h before virus titers were calculated using the method of Reed and Munch (22).
Polykaryon formation assay.
HeLa cells cultured in a 12-well plate were transfected with the protein expression plasmid pCAGGS encoding wild-type or mutant HA. At 24 h posttransfection, the HA-expressing HeLa cells were treated with TPCK-trypsin (1 μg/ml) in MEM containing 0.3% BSA for 30 min. H5 HA does not require trypsin treatment for HA cleavage; nonetheless, incubation with trypsin was carried out for better comparison with experiments that are not part of this study. Polykaryon formation was induced by incubating cells with low-pH buffer (145 mM NaCl, 20 mM sodium citrate [pH 5.0 to 5.8]) for 2 min at 37°C. The low-pH buffer was removed, MEM containing 10% FBS was added, and plates were incubated for 3 h at 37°C. The cells were fixed with methanol and stained with Giemsa solution (Sigma-Aldrich). Photographs were taken using an integrated digital camera in an inverted microscope (AMG, EVOS XL Core). The efficiency of polykaryon formation was calculated as the number of nuclei in polykaryons divided by the total nuclei in the field of view. Averages were calculated from five randomly chosen fields.
Solid-phase binding assay.
Viruses were amplified in AX4 cells. Supernatant collected from infected cells was centrifuged at 1,462 × g for 30 min to remove cell debris. Virus supernatant was laid over a cushion of 30% sucrose in PBS, ultracentrifuged at 76,755 × g for 2 h at 4°C, and then resuspended in PBS containing glycerol for storage at −80°C. Virus concentrations were determined by using hemagglutination assays with 0.5% (vol/vol) TRBCs. Microtiter plates (Nunc) were incubated with the sodium salts of sialylglycopolymers [poly-l-glutamic acid backbones containing N-acetylneuraminic acid linked to galactose through either an α2,3 (Neu5Acα2,3Galβ1,4GlcNAcβ1-pAP) or an α2,6 (Neu5Acα2,6Galβ1,4GlcNAcβ1-pAP) bond] (23) in PBS at 4°C overnight. The glycopolymer solution was removed, and the plates were blocked with 150 μl of PBS containing 4% BSA at room temperature for 1 h. After four washes with cold PBS, a solution containing influenza virus (8 to 16 HA units in PBS) was added to the plates for incubation at 4°C overnight. After washing as described above, the plates were incubated for 2 h at 4°C with rabbit polyclonal antiserum to either VN1203 or A/Kawasaki/173/2001(H1N1; K173) virus. The plates were washed again as before and incubated with horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG antiserum for 2 h at 4°C. After washing, the plates were incubated with o-phenylenediamine (Sigma) in PBS containing 0.03% H2O2 for 10 min at room temperature. The reaction was stopped with 50 μl of 1 M HCl. Absorbance was measured at 490 nm using an optical plate reader (Infinite M1000; Tecan).
Tissue binding.
Viruses were amplified in AX4 cells. Supernatants collected from infected cells were centrifuged at 1,462 × g for 30 min to remove cell debris. Viruses were inactivated by mixing the supernatants with 0.1% β-propiolactone (final concentration). Virus supernatant was laid over a cushion of 30% sucrose in PBS, ultracentrifuged at 76,755 × g for 2 h at 4°C, and then resuspended in PBS for storage at −80°C. Virus concentrations were determined by using hemagglutination assays with 0.5% (vol/vol) TRBCs. Paraffin-embedded normal human trachea and lung (US Biomax) tissue samples were deparaffinized and rehydrated. Sections were blocked by using Carbo-Free blocking solution (Vector) and TNB blocking buffer (Perkin-Elmer). The equivalent of 8 HA units of fluorescein-5-isothiocyanate (FITC)-labeled viruses was added to the tissue sections, followed by incubation at 4°C overnight. The slides were washed five times with cold PBS and then incubated with an HRP-conjugated rabbit anti-FITC antibody (Dako) for 30 min at room temperature. The slides were washed again five times with cold PBS and then incubated with AEC (3-amino-9-ethyl-carbozole) substrate chromogen (Dako) for 15 min at room temperature. The slides were then rinsed with water and counterstained with Mayer's hematoxylin (Sigma-Aldrich) for 3 min at room temperature. A final rinse with water was performed before coverslips were mounted by using Shandon Immu-Mount (Thermo Scientific). Tissue sections were examined by using a high-resolution camera (AxioCam HRc) mounted on a microscope (Axio Imager.A2; Zeiss).
Glycan array.
Glycan array analysis was performed on a glass slide microarray containing six replicates of 58 diverse sialic acid-containing glycans, including terminal sequences and intact N-linked and O-linked glycans found on mammalian and avian glycoproteins and glycolipids (24, 25). Viruses were amplified in AX4 cells. Supernatants collected from infected cells were centrifuged at 1,462 × g for 30 min to remove cell debris. Viruses were inactivated by mixing the supernatants with 0.1% β-propiolactone (final concentration). Virus supernatant was laid over a cushion of 30% sucrose in PBS, ultracentrifuged at 76,755 × g for 2 h at 4°C, and then resuspended in PBS for storage at −80°C. Virus samples were directly labeled with biotin (26) and then applied to the slide array. Slide scanning to detect virus bound to glycans was conducted as described previously (27). A complete list of glycans on the array is presented in Table S1 in the supplemental material.
Biosafety statement.
All experiments were approved by the University of Wisconsin—Madison's Institutional Biosafety Committee. All experiments involving H5 viruses with a multibasic HA cleavage site were performed in enhanced BSL3 (BSL3+) laboratories approved for such use by the CDC and USDA. All experiments involving live H5N1 viruses were concluded prior to the pause on gain-of-function research announced by the U.S. Government on 17 October 2014.
RESULTS
Isolation of HA mutants with increased heat stability.
Our goal was to identify stabilizing mutations in the context of an H5 HA that binds to human-type receptors. We, therefore, used the A/Vietnam/1203/2004 (H5N1; VN1203) HA protein possessing the N224K and Q226L mutations which confer a switch from avian- to human-type receptor-binding preference in the VN1203 HA (8). Starting with this mutated H5 HA cDNA, we introduced random mutations into the ectodomain of HA (amino acids 17 to 531; H3 numbering, Fig. 1). A mutation rate of 2 to 3 amino acids per HA segment was achieved by optimizing the error-prone PCR cycles and was confirmed by using Sanger sequencing. The mutant cDNAs were inserted into plasmids encoding the remaining portions of HA (i.e., the signal peptide, transmembrane region, and cytoplasmic tail), and possessing RNA polymerase I promoter and terminator sequences essential for plasmid-driven reverse genetics (21) (Fig. 1). This constituted the mutant HA plasmid library, which was subsequently transfected into human embryonic kidney (293T) cells together with plasmids encoding the remaining seven viral RNA segments of A/California/04/2009 (H1N1; CA04), resulting in viruses (termed H5HA-N224K+Q226L/CA04) of the same genetic composition as the virus used in our previous H5 virus transmission study in ferrets (8). Supernatant from the transfected 293T cells was amplified in Madin-Darby canine kidney (MDCK) cells overexpressing Siaα2,6Gal (AX4 cells) (19, 20).
FIG 1.
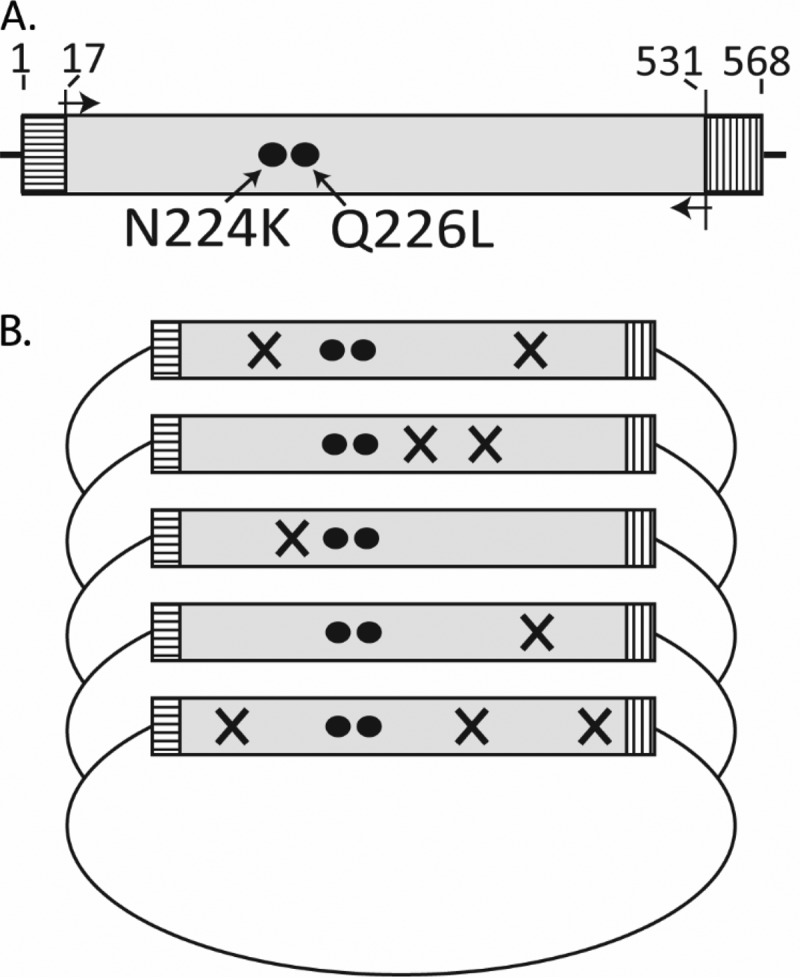
Generation of the mutant virus library. (A) The target area for mutagenesis (amino acids 17 to 531) is shown in gray; the sequences encoding the signal peptide (amino acids 1 to 16) and the transmembrane region and cytosolic tail (amino acids 532 to 568) are depicted by horizontal and vertical lines, respectively. The amino acid changes that confer binding to human-type receptors (N224K and Q226L) are depicted as black circles. (B) Schematic diagram showing the construction of the mutant plasmid library. The cDNA template encoding HA amino acids 17 to 531 was amplified by using error-prone PCR, resulting in random amino acid changes. The mutated PCR products were then used to replace the wild-type sequence in the plasmid vector; the resulting plasmid library was subsequently used to generate the mutant virus library.
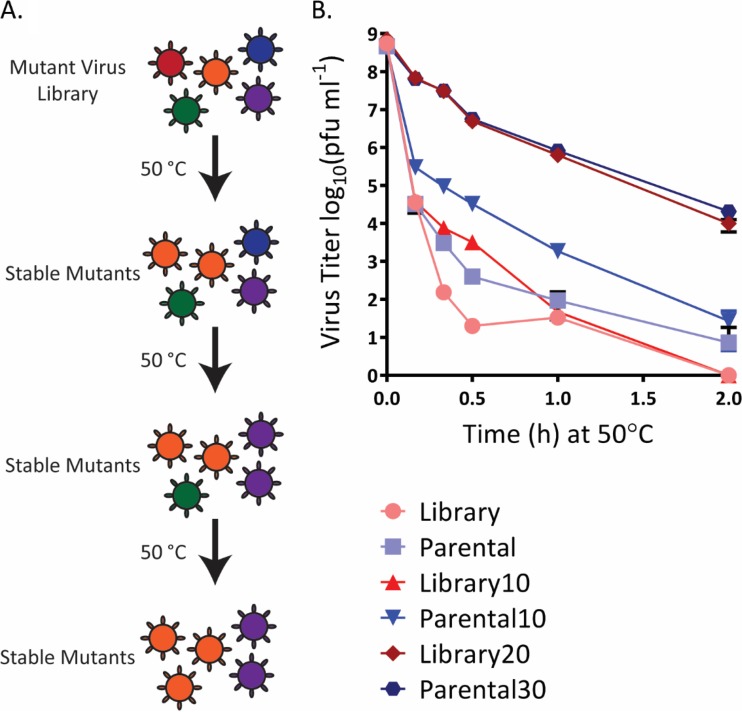
Heat treatment at 50°C inactivates viruses with low physical stability. Moreover, heat treatment at neutral pH induces a conformational change in HA that mimics the low-pH-induced conformational change in late endosomes (14, 28). To isolate variants with increased heat stability, we first assessed the kinetics of virus inactivation for an aliquot of the mutant virus library and found that incubation for 10 min at 50°C reduced virus titers by ∼4 log10 units (Fig. 2, “Library”). We also tested an aliquot of the parental H5HA-N224K+Q226L/CA04 virus; comparable to the mutant virus library, virus titers were reduced by ∼4 log10 units after 10 min at 50°C (Fig. 2, “Parental”). Fresh aliquots of both samples (i.e., the mutant virus library and the parental H5HA-N224K+Q226L/CA04 virus) were incubated for 10 min at 50°C, followed by amplification of the remaining infectious viruses in AX4 cells. These new stocks (called “Library10” and “Parental10” because they represent the viruses that remained viable after 10 min of treatment at 50°C) underwent heat treatment again as described above. In this second heat treatment, the kinetics of virus inactivation shifted toward slower virus inactivation compared with the first heat treatment (Fig. 2); in addition, the Parental10 sample displayed slower inactivation kinetics compared to the Library10 sample. Therefore, fresh aliquots of the Library10 and Parental10 stocks were incubated for 20 or 30 min, respectively, followed by amplification of the remaining infectious viruses in AX4 cells. After this third heat treatment, the heat stability of both samples increased considerably (Fig. 2, “Library20” and “Parental30”), suggesting the enrichment of variants with increased heat stability. We therefore incubated the Library20 and Parental30 samples for 2 h at 50°C, performed plaque assays in AX4 cells, randomly isolated 20 plaques each, and amplified them in AX4 cells. All 40 viruses were then tested for their infectious virus titers and hemagglutination (HA) activity after heat treatment for various times at 50°C (Fig. 3 and 4). We detected considerable variability in heat stability among the isolated viruses; most, but not all, displayed increased stability at 50°C compared with the parental virus.
FIG 2.
Isolation of HA mutants with increased heat stability. (A) Schematic diagram of the selection strategy used. The mutant virus library was subjected to three consecutive rounds of heat treatment, resulting in the selection of variants with increased heat stability. Likewise, the parental virus was subjected to three rounds of heat treatment (not shown here). (B) The mutant virus library and parental stock of H5HA-N224K+Q226L/CA04 underwent three consecutive heat treatments at 50°C for the indicated times. Shown are the means and standard deviations at each time point (plaque assay in AX4 cells in triplicate).
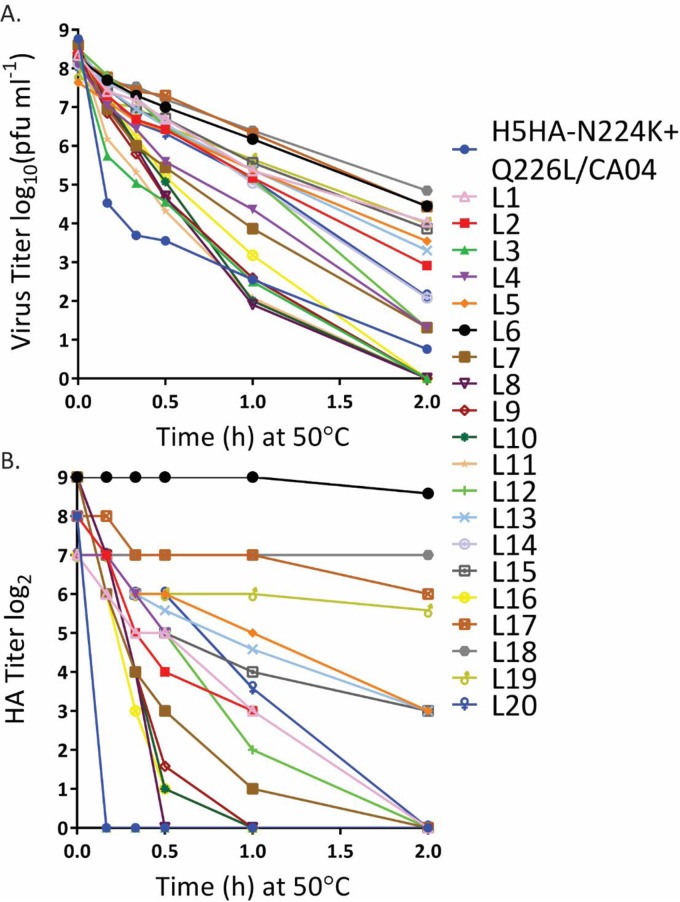
FIG 3.
Heat stability of mutant viruses selected from the mutant virus library. After the third heat treatment, we performed plaque assays in AX4 cells, randomly selected 20 plaques (L1 to L20), amplified them in AX4 cells, and determined their virus titers (A) and HA titers (B) after treatment at 50°C for the indicated time periods. The mutations detected in the HA proteins of these viruses are presented in Tables 1 and 2.
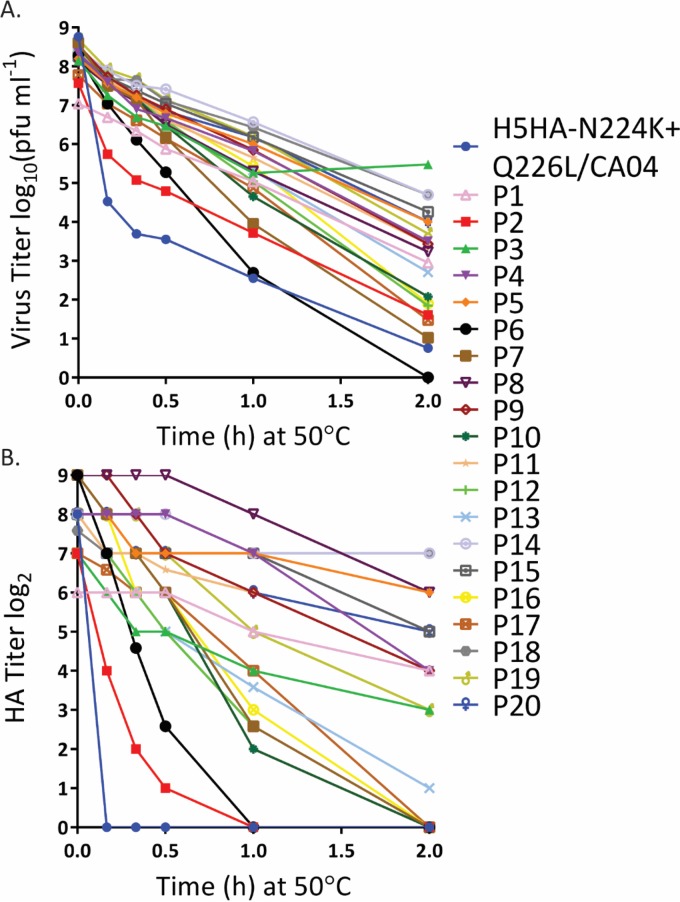
FIG 4.
Heat stability of mutant viruses derived from the H5HA-N224K+Q226L/CA04 virus. After the third heat treatment, we performed plaque assays in AX4 cells, randomly selected 20 plaques (P1 to P20), amplified them in AX4 cells, and determined their virus titers (A) and HA titers (B) after treatment at 50°C for the indicated time periods. The mutations detected in the HA proteins of these viruses are presented in Tables 1 and 2.
For further studies, we selected the eight most heat-stable viruses from the mutant virus library screen and the 12 most heat-stable viruses derived from the parental virus. Sanger sequencing of the HA genes of these viruses revealed several mutations in HA that may be responsible for the increased heat stability (Tables 1 and 2). The most frequently detected mutations were S221P and R397M, which are located in the receptor-binding domain and stalk, respectively (Fig. 5). Four mutations (I29M, R397M, L418I, and L427I) were detected both in viruses isolated from the mutant virus library and derived from the parental virus. The finding that these mutations were selected in two independent screens suggests that they may have biological significance for HA heat stability. Six virus samples (all derived from the parental H5HA-N224K+Q226L/CA04 virus) showed a partial or complete L226Q reversion, suggesting they may no longer preferentially recognize human-type receptors.
TABLE 1.
HA-stabilizing mutations listed by amino acid position
| Mutation | Structural region | Virus plaque(s)a |
|---|---|---|
| I29 M | Stalk | L133, P193 |
| D95*G | Globular head receptor-binding domain | P33 |
| D101N | Globular head receptor-binding domain | L153 |
| A218V | Globular head receptor-binding domain | L1 |
| S221P | Globular head receptor-binding domain | P11, P32,3, P41, P52,3 P81, P92, P193, P203 |
| M230V | Globular head receptor-binding domain | L153 |
| R397 M | Stalk | L6, L18, P14, P18 |
| L418I | Stalk | L53, L17, P15 |
| L427I | Stalk | L19, P11 |
| M431L | Stalk | P193 |
| R456K | Stalk | P41 |
L1 to L20, plaques derived from virus library; P1 to P20, plaques derived from parental sample. Superscript numbers: 1, sequencing revealed reversion from L226 to Q226; 2, sequencing revealed both L226 and Q226; 3, sequencing revealed both the wild-type amino acid and the amino acid identified after heat treatment (for example, sequence analysis of plaque P19 revealed both isoleucine and methionine at position 29).
FIG 5.
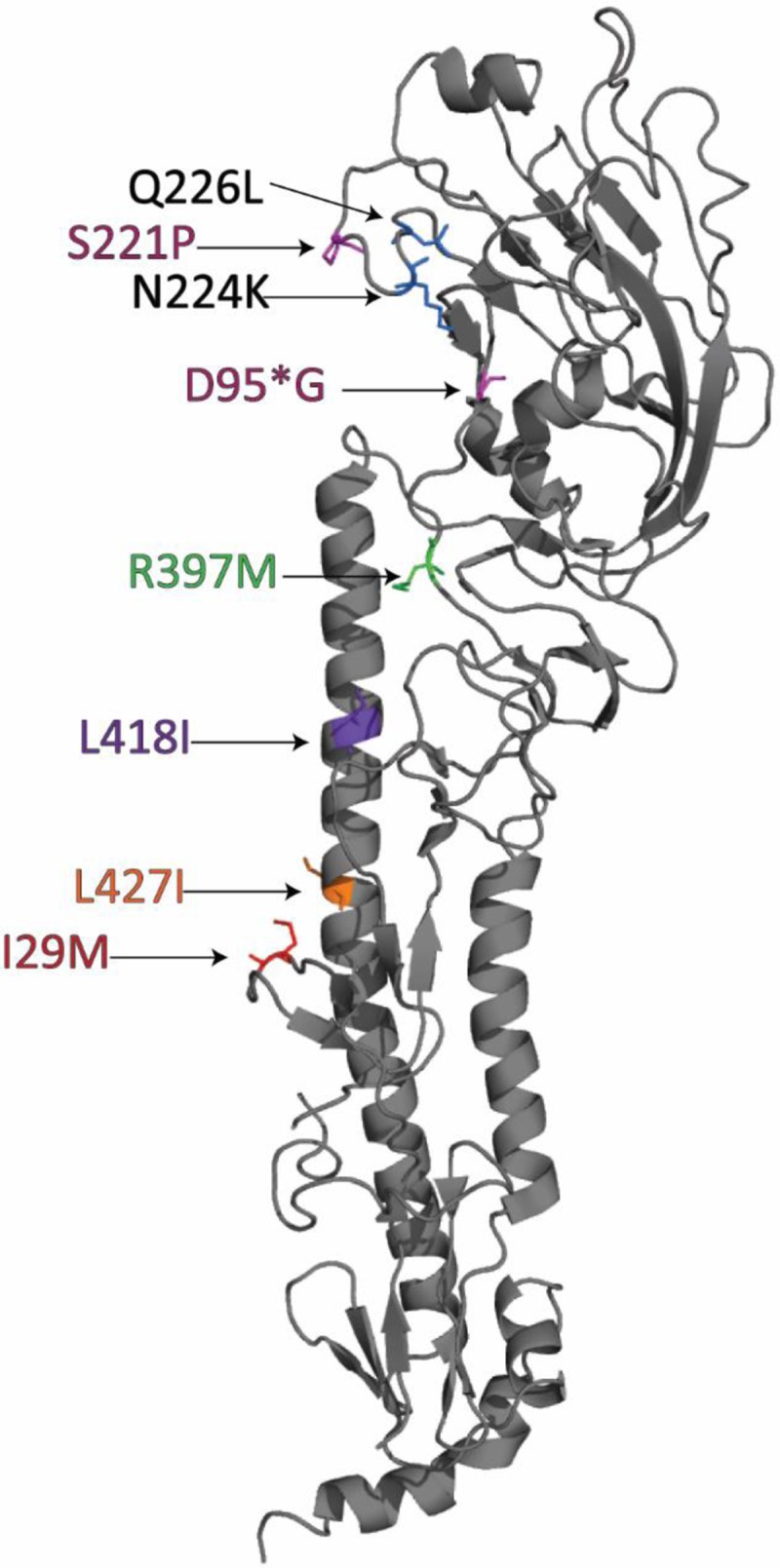
Localization of HA stabilizing mutations. Shown is the VN1203 HA monomer structure (Protein Data Bank accession number 2FK0 [36]) with the N224K/Q226L mutations (black labels) that confer human-type receptor-binding and the HA-stabilizing mutations (colored labels) identified here.
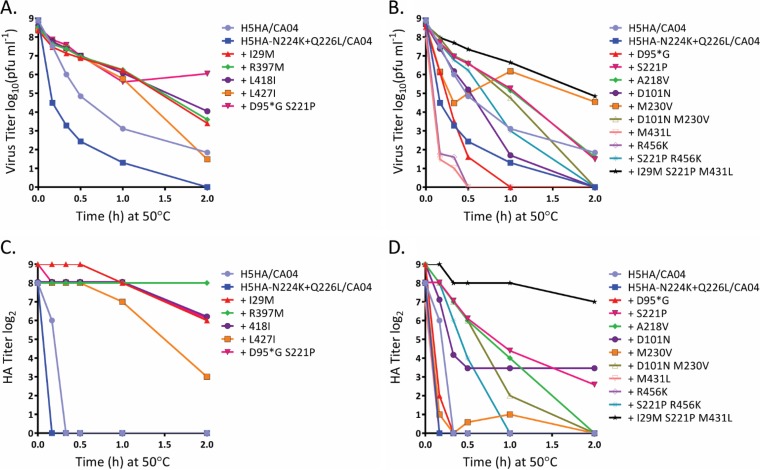
Generation and characterization of mutant viruses possessing stabilizing mutations in HA.
To confirm that the increased viral heat stability resulted from mutations in HA, we created 15 mutant viruses by introducing the HA mutations shown in Tables 1 and 2 into the parental H5HA-N224K+Q226L/CA04 virus. If more than one mutation was found in an HA (see Tables 1 and 2), we also generated viruses possessing the individual mutations. The resulting 15 mutant viruses were subjected to heat treatment at 50°C and assessed for their infectivity and HA titers (Fig. 6). A virus possessing the VN1203 HA gene in the background of CA04 (H5HA/CA04) rapidly lost infectivity and HA activity. The H5HA-N224K+Q226L/CA04 virus (which possesses mutations that confer binding to human-type receptors) displayed even lower heat stability, as described previously (8). In contrast, several of the mutations isolated here increased the heat stability above that detected for H5HA/CA04 and H5HA-N224K+Q226L/CA04. In particular, introduction of the I29M, R397M, L418I, L427I, or D95*G/S221P (an asterisk [*] denotes the position after 95 in H5 HA, which does not have an equivalent in H3 HA numbering) mutations into H5HA-N224K+Q226L/CA04 generated viruses with high heat stability (Fig. 6). These mutants were therefore selected for further analysis. A virus possessing three mutations in HA (I29M+S221P+M431L) also displayed high heat stability; however, we did not include this virus in our further studies because multiple mutations may not cooccur frequently in nature.
TABLE 2.
HA-stabilizing mutations listed by plaque number
| Virus plaquea | Mutation(s) |
|---|---|
| L1 | A218V |
| L53 | L418I |
| L6 | R397M |
| L133 | I29M |
| L153 | D101N, M230V |
| L17 | L418I |
| L18 | R397M |
| L19 | L427I |
| P11 | S221P |
| P32,3 | D95*G, S221P |
| P41 | S221P, R456K |
| P52,3 | S221P |
| P81 | S221P |
| P92 | S221P |
| P11 | L427I |
| P14 | R397M |
| P15 | L418I |
| P18 | R397M |
| P193 | I29M, S221P, M431L |
| P203 | S221P |
L1 to L20, plaques derived from virus library; P1 to P20, plaques derived from parental sample. Superscript numbers: 1, sequencing revealed reversion from L226 to Q226; 2, sequencing revealed both L226 and Q226; 3, sequencing revealed both the wild-type amino acid and the amino acid identified after heat treatment (for example, sequence analysis of plaque P19 revealed both isoleucine and methionine at position 29).
FIG 6.
Stability at 50°C of selected HA mutants. Shown are the virus titers (A and B) and HA titers (C and D) of the HA mutants selected from the mutant virus library screen and the parental H5HA-N224K+Q226L/CA04 virus after three rounds of treatment at 50°C. HA mutants further characterized for fusion and receptor-binding activity are shown in panels A and C. The mutants that were not characterized further are shown in panels B and D. A “+” indicates that the HA protein encodes the respective amino acid change(s) in the background of H5HA-N224K+Q226L.
Effect of heat-stabilizing mutations on HA-induced membrane fusion.
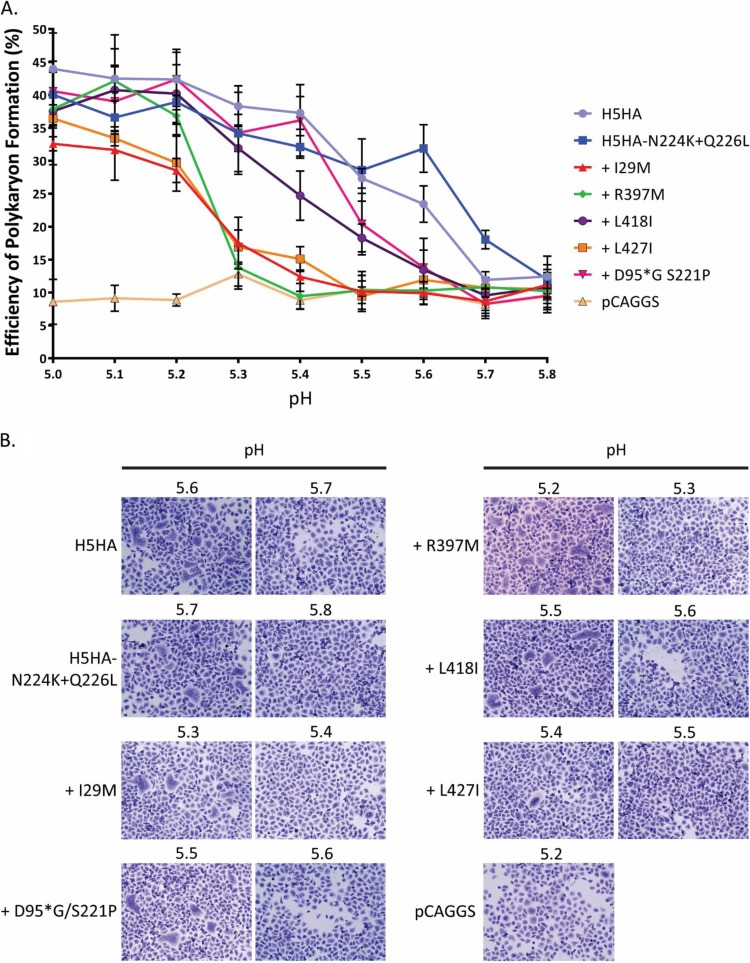
Heat treatment induces a conformational change in HA comparable to that triggered by the low pH in late endosomes, which subsequently leads to the fusion of the viral and endosomal membranes. We previously reported that the N224K and Q226L mutations in the background of VN1203 HA decrease heat stability and increase the pH at which membrane fusion is triggered, whereas the T318I mutation in HA reverses this effect (8). We therefore tested the effect of the heat-stabilizing mutations on HA-induced membrane fusion. Briefly, HeLa cells were transfected with plasmids expressing wild-type or mutant HA proteins. Twenty-four hours later, polykaryon formation was induced by incubating the cells with buffer of different pH values for 2 min at 37°C. Three hours later, cells were fixed and stained with Giemsa solution (Sigma-Aldrich) (Fig. 7). The efficiency of polykaryon formation was calculated as the number of nuclei in polykaryons divided by the total nuclei in the field of view; presented are the averages of five randomly chosen fields (Fig. 7A).
FIG 7.
Efficiency of polykaryon formation (as a measure of fusion activity) of mutant HA proteins. HeLa cells were transfected with plasmids expressing the indicated wild-type or mutant HA proteins and were then exposed to acidic buffers over a pH range (5.0 to 5.8) to induce cell-cell fusion. (A) The efficiency of polykaryon formation was calculated from the number of nuclei in the polykaryons divided by the total number of nuclei in the same field. Shown are the means and standard deviations determined from five randomly selected fields. pCAGGS, vector control. (B) Representative photographs of polykaryon formation at the indicated pH values. Images were taken at ×20 magnification. A “+” indicates that the HA protein encodes the respective amino acid change(s) in the background of H5HA-N224K+Q226L.
H5HA protein triggered considerable levels of polykaryon formation at pH 5.6 (Fig. 7A). Introduction of the N224K+Q226L mutations slightly increased the pH threshold for membrane fusion, an observation consistent with our previous findings (8). Introduction of the L418I or D95*G/S221P mutations into the H5HA-N224K+Q226L protein reversed this effect, and these mutant HA proteins triggered membrane fusion at pH values lower than those observed for H5HA and H5HA-N224K+Q226. This effect was even stronger upon the introduction of the I29M, R397M, or L427I mutations into the H5HA-N224K+Q226L/CA04 HA protein; these mutant HAs did not trigger appreciable polykaryon formation until the pH was lowered to 5.2. Thus, all five HA-stabilizing mutants tested here triggered membrane fusion at a more acidic pH compared to the parental H5HA-N224K+Q226L HA.
Receptor-binding specificity of viruses possessing HA-stabilizing mutations.
Our study aimed to identify HA-stabilizing mutations in the background of an H5 HA that binds to human-type receptors. After establishing the effects of the isolated mutations in HA on heat stability and the pH threshold for membrane fusion, we assessed their potential effect on receptor-binding specificity. For these studies, the multibasic sequence at the HA cleavage site was replaced with a single arginine residue; this HA gene was combined with VN1203 NA and the six remaining viral genes of A/Puerto Rico/8/34 (H1N1) virus. The resulting virus (H5NAHAΔ/PR8) and HA-stabilizing variants were approved for use in BSL2 containment by the University of Wisconsin—Madison's Institutional Biosafety Committee.
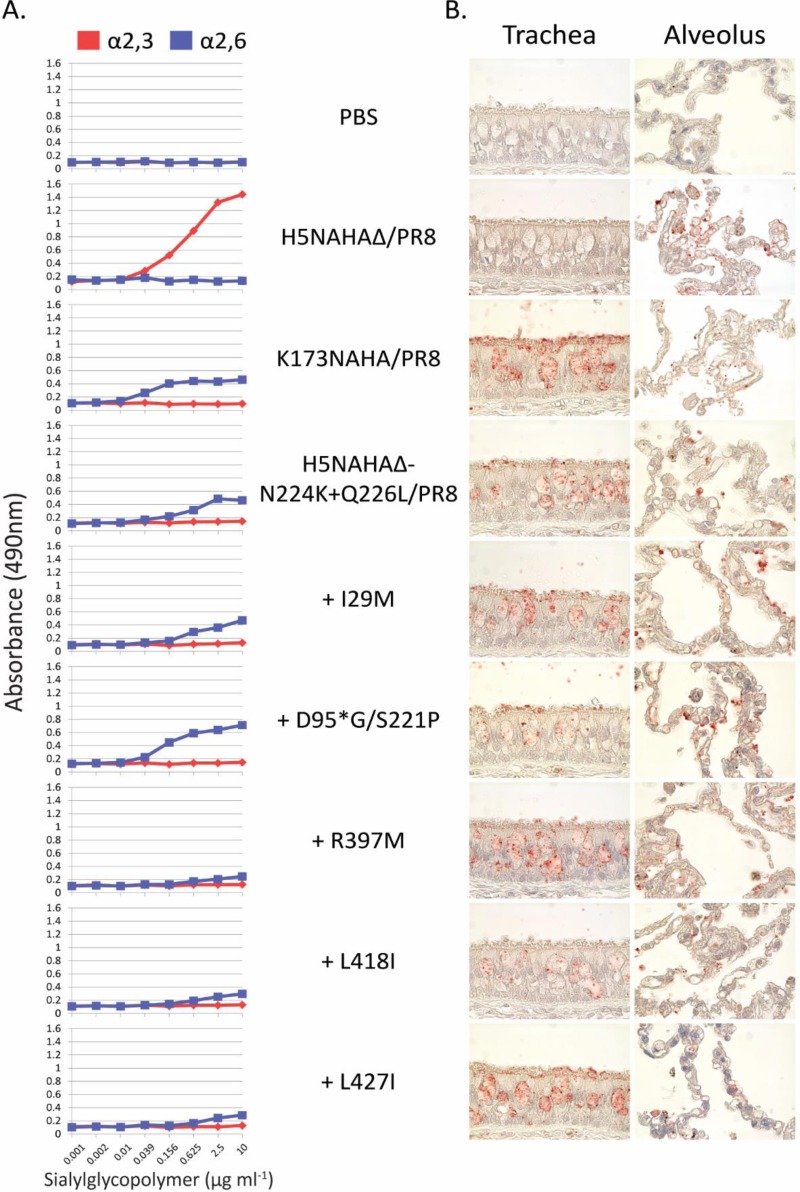
First, we performed a solid-phase binding assay in which α2,3- or α2,6-linked sialylglycopolymers were coated onto a microtiter plate and incubated with virus (Fig. 8A). The human control virus K173NAHA/PR8 (consisting of the A/Kawasaki/173/2001 [H1N1] NA and HA genes in the background of PR8) bound to α2,6-linked sialylglycopolymers (Fig. 8A), as expected. Consistent with our previous study (8), H5NAHAΔ/PR8 displayed specificity for α2,3-linked sialylglycopolymers, which was shifted to human-type receptor-binding specificity upon introduction of the N224K/Q226L mutations (Fig. 8A, see H5NAHAΔ-N224K+Q226L/PR8) (8). The introduction of additional HA-stabilizing mutations into H5NAHAΔ-N224K+Q226L/PR8 did not affect the receptor-binding specificity in this assay; hence, the mutant viruses' ability to bind to human cells was retained.
FIG 8.
Receptor-binding preference of mutant HA proteins. (A) Binding of HA proteins to sialylglycopolymers that correspond to influenza virus receptors on avian (α2,3; red) or human (α2,6; blue) cells. H5NAHAΔ/PR8 (a virus that binds to avian-type receptors), K173NAHA/PR8 (a virus that binds to human-type receptors), and the indicated mutant viruses were evaluated for their ability to bind to the avian- or human-type receptor analogs. (B) Binding to human tissue sections (trachea, alveolus). The indicated viruses were labeled with FITC and incubated with the tissue samples. Tracheal cells contain primarily α2,6 (human-type) receptors, whereas alveolar cells contain α2,6 (human-) and α2,3 (avian-type) receptors. PBS, control. A “+” indicates that the HA protein encodes the respective amino acid change(s) in the background of H5HA-N224K+Q226L.
Binding to human respiratory tract tissue samples is a biologically relevant assay. The upper human respiratory tract primarily contains cells that express Siaα2,6Gal receptors (29). In the lower respiratory tract (the bronchiole and alveolus), some cells such as type II pneumocytes express Siaα2,3Gal receptors (29). To examine the binding properties of the HA stability-enhancing mutants identified here, we inactivated viruses with β-propiolactone, labeled them with FITC, and added them overnight to deparaffinized and rehydrated normal human trachea and lung tissue samples (Fig. 8B). The sialic acid receptors on tracheal sections are representative of the respiratory tissue in the upper human airway (29). Virus binding was detected by using HRP-conjugated rabbit anti-FITC antibody and AEC substrate chromogen. H5NAHAΔ/PR8 did not bind to tracheal sections, in contrast to the human control virus (K173NAHA/PR8) and H5NAHAΔ-N224K+Q226L/PR8, which possesses the N224K+Q226L mutations that confer binding to human-type receptors. The introduction of HA-stabilizing mutations did not appreciably affect the receptor-binding properties of the mutant viruses. In contrast to tracheal samples, all viruses tested here bound to alveolar lung sections, reflecting the expression of both human- and avian-type receptors on the cells of the alveoli. Thus, in agreement with the data from the solid-phase binding assays, the HA-stabilizing mutations identified here do not affect binding to human-type receptors.
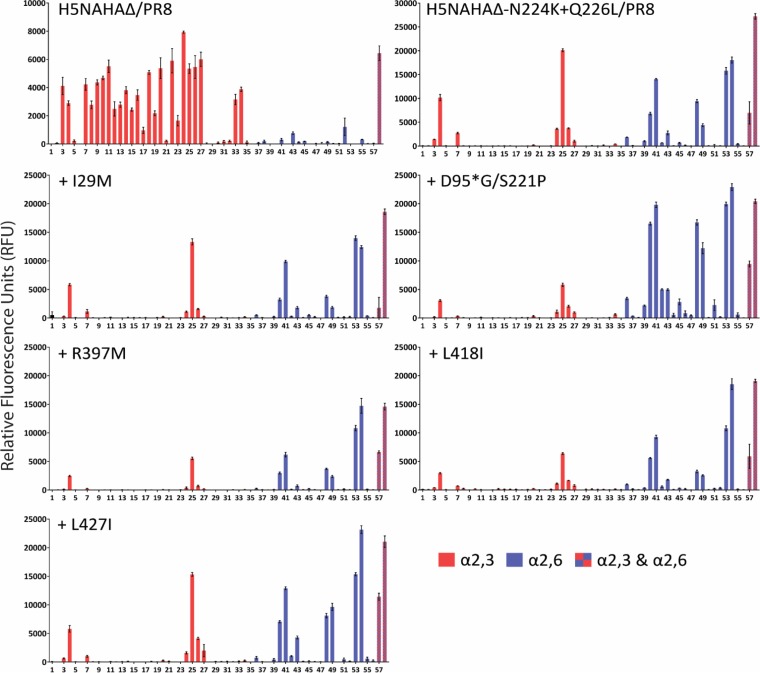
To further characterize the receptor-binding specificity of the HA mutants with increased stability, we performed a glycan array analysis as described previously (13). Inactivated virus stocks were added to glass slide microarrays containing replicates of 58 diverse sialic acid-containing glycans found on avian (α2,3-linked) and mammalian (α2,6-linked) glycoproteins and glycolipids. H5NAHAΔ/PR8 displayed specificity for α2,3-linked sialosides (Fig. 9). Introduction of the N224K/Q226L mutations resulted in a shift to human-type receptor-binding specificity (Fig. 9, see H5NAHAΔ-N224K+Q226L/PR8), although the mutant virus retained the ability to bind to some of the α2,3-linked glycans. The Introduction of additional HA-stabilizing mutations into H5NAHAΔ-N224K+Q226L/PR8 did not appreciably affect the receptor-binding specificity of the mutant viruses.
FIG 9.
Glycan microarray analysis of mutant HA proteins. Glycan microarrays containing nonsialylated controls (glycans 1 and 2), α2,3-linked sialosides (red bars, glycans 3 to 35), α2,6-linked sialosides (blue bars, glycans 36 to 56), and glycans possessing both α2,3- and α2,6-linked sialic acids (checkered bars, glycans 57 and 58); a complete list of glycans is provided in Table S1 in the supplemental material. Viruses were evaluated for their ability to bind to the respective sialosides (relative fluorescence units). A “+” indicates that the HA protein encodes the respective amino acid change(s) in the background of H5HA-N224K+Q226L.
DISCUSSION
Previous findings by us (8, 13) and others (9, 12) demonstrated that HA heat stability and pH-dependent fusion activity contribute to the respiratory droplet transmissibility of avian H5 influenza viruses in mammals. In particular, mutations in H5 HA that conferred binding to human-type receptors reduced stability and increased the pH threshold for membrane fusion. Compensatory mutations in HA, such as T318I and H110Y, which reversed these effects, were critical for H5 virus transmissibility in ferrets. Here, we identified several additional mutations in an H5 HA that compensate for the reduced stability and higher pH threshold for membrane fusion conferred by mutations that facilitate binding to human-type receptors. Such mutations could contribute to the emergence of influenza viruses capable of transmitting among mammals.
The pH threshold for membrane fusion may be an important determinant of influenza virulence (reviewed in reference 15). In avian species, relatively high pH thresholds for membrane fusion (i.e., pH 5.5 to 6.0) are associated with high virulence (17, 30). Several studies have found that mutations in H5N1 viruses that increase or decrease the pH threshold for membrane fusion cause an increase or decrease, respectively, in virulence in avian species (17, 30). In mammalian hosts, the correlation between the pH threshold for membrane fusion and influenza virulence is less clear. In mice, a relatively high pH threshold for HA conformational change and membrane fusion was correlated with high virulence of human influenza viruses (31–33); in contrast, high mouse virulence of an H5N1 virus correlated with a mutation in HA that reduced the pH threshold of membrane fusion (34). High virulence in ferrets appears to be associated with a more acidic pH optimum for membrane fusion of pH ∼5.0 to 5.7 (8, 9, 12). Here, we also found that the N224K/Q226L mutations increased the pH of fusion compared to H5HA, whereas the heat-stabilizing mutations identified decreased the pH threshold for membrane fusion to ∼5.2 to 5.5. Likewise, human influenza viruses of the H1N1 and H3N2 subtypes typically undergo HA conformational changes at a pH of between 5.0 and 5.5. This relatively acidic pH optimum may be necessary for human influenza viruses to prevent premature HA conformational change in the mucosa of the human respiratory tract, which has a pH of approximately 5.5 to 6.5 (35). Thus, viruses possessing the VN1203 HA or the VN1203 HA with the N224K and Q226L mutations may undergo premature HA conformational change in the human mucosa to some extent, which would likely reduce their infectivity. The HA mutations identified here shift the pH threshold for membrane fusion to a pH range that has been reported effective for human influenza viruses (18) and for influenza viruses that are highly virulent in ferrets (8, 9, 12).
A considerable number of mutations have now been described that affect the stability and/or fusion activity of HA (reviewed in reference 15). The S221P mutation described here was previously identified as a stabilizing mutation (30), but it has not been reported in conjunction with the D95*G mutation. We also found that S221P affects the heat stability of HA (Fig. 6) and that this effect is enhanced when combined with the D95*G mutation. The other stabilizing mutations characterized here have not been described previously. Many of the known HA-stabilizing mutations are located in regions that undergo major structural changes during the HA fusion process (reviewed in reference 15). In fact, the R397M mutation identified in this study is located in the B-loop of the HA2 subunit (Fig. 5), which rearranges into a coiled domain during the acid-induced HA conformational change. The I29M, L418I, and L427I mutations are part of the trimer interface in the stalk region of the protein; a number of other mutations that affect the pH threshold for membrane fusion also map to this region (reviewed in reference 15). The D95*G and S221P mutations are located near the receptor-binding pocket.
During the preparation of the manuscript, we analyzed the influenza sequence database (http://www.fludb.org) to determine the prevalence of the mutations we identified here among H5N1 influenza viruses. The I29M, R397M, L418I, and L427I mutations have not been detected in H5N1 viruses isolated from humans and have each been detected in 0 to 4 avian H5N1 viruses. The D95*G and S221P mutations have been detected in 19 and 25 human H5N1 viruses, respectively, but not in combination. In contrast, the D95*G mutation has been detected in >250 avian H5N1 viruses, and the S221P mutation was present in >150 avian H5N1 viruses; an appreciable number of these H5N1 avian isolates encoded both mutations. Based on currently available surveillance data, the HA-stabilizing mutations identified here do not appear to be selected in humans.
We currently do not know the effect of the HA-stabilizing mutations identified in this study on the respiratory droplet transmissibility of H5 viruses in ferrets. On 17 October 2014, the U.S. Government announced a research pause on certain gain-of-function studies with influenza viruses, so the potential role of these novel HA-stabilizing mutations in respiratory droplet transmission in ferrets cannot be assessed at this time.
Supplementary Material
ACKNOWLEDGMENTS
We thank Susan Watson for editing the manuscript.
This study was supported by NIAID grant R01 AI 069274 (Transmissibility of Avian Influenza Viruses in Mammals) to Y.K.; by an NIAID-supported Virology Training Grant (T32 AI078985) to A.H.; by the Japan Initiative for Global Research Network on Infectious Diseases from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; by the Japan Agency for Medical Research and Development, AMED; and by The Yin Foundation and NIH grant GM62116 to J.C.P. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JVI.02790-15.
REFERENCES
- 1.Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, de Jong MD, Naghdaliyev A, Peiris JS, Shindo N, Soeroso S, Uyeki TM. 2008. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med 358:261–273. doi: 10.1056/NEJMra0707279. [DOI] [PubMed] [Google Scholar]
- 2.Skehel JJ, Wiley DC. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem 69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 3.Rogers GN, Paulson JC. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127:361–373. doi: 10.1016/0042-6822(83)90150-2. [DOI] [PubMed] [Google Scholar]
- 4.Auewarakul P, Suptawiwat O, Kongchanagul A, Sangma C, Suzuki Y, Ungchusak K, Louisirirotchanakul S, Lerdsamran H, Pooruk P, Thitithanyanont A, Pittayawonganon C, Guo CT, Hiramatsu H, Jampangern W, Chunsutthiwat S, Puthavathana P. 2007. An avian influenza H5N1 virus that binds to a human-type receptor. J Virol 81:9950–9955. doi: 10.1128/JVI.00468-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watanabe Y, Ibrahim MS, Ellakany HF, Kawashita N, Mizuike R, Hiramatsu H, Sriwilaijaroen N, Takagi T, Suzuki Y, Ikuta K. 2011. Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS Pathog 7:e1002068. doi: 10.1371/journal.ppat.1002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yen HL, Lipatov AS, Ilyushina NA, Govorkova EA, Franks J, Yilmaz N, Douglas A, Hay A, Krauss S, Rehg JE, Hoffmann E, Webster RG. 2007. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J Virol 81:6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maines TR, Chen LM, Van Hoeven N, Tumpey TM, Blixt O, Belser JA, Gustin KM, Pearce MB, Pappas C, Stevens J, Cox NJ, Paulson JC, Raman R, Sasisekharan R, Katz JM, Donis RO. 2011. Effect of receptor binding domain mutations on receptor binding and transmissibility of avian influenza H5N1 viruses. Virology 413:139–147. doi: 10.1016/j.virol.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. 2012. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology 422:105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Zhang Q, Kong H, Jiang Y, Gao Y, Deng G, Shi J, Tian G, Liu L, Liu J, Guan Y, Bu Z, Chen H. 2013. H5N1 hybrid viruses bearing 2009/H1N1 virus genes transmit in guinea pigs by respiratory droplet. Science 340:1459–1463. doi: 10.1126/science.1229455. [DOI] [PubMed] [Google Scholar]
- 12.Linster M, van Boheemen S, de Graaf M, Schrauwen EJ, Lexmond P, Manz B, Bestebroer TM, Baumann J, van Riel D, Rimmelzwaan GF, Osterhaus AD, Matrosovich M, Fouchier RA, Herfst S. 2014. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell 157:329–339. doi: 10.1016/j.cell.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Vries RP, Zhu X, McBride R, Rigter A, Hanson A, Zhong G, Hatta M, Xu R, Yu W, Kawaoka Y, de Haan CA, Wilson IA, Paulson JC. 2014. Hemagglutinin receptor specificity and structural analyses of respiratory droplet-transmissible H5N1 viruses. J Virol 88:768–773. doi: 10.1128/JVI.02690-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carr CM, Chaudhry C, Kim PS. 1997. Influenza hemagglutinin is spring-loaded by a metastable native conformation. Proc Natl Acad Sci U S A 94:14306–14313. doi: 10.1073/pnas.94.26.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russell CJ. 2014. Acid-induced membrane fusion by the hemagglutinin protein and its role in influenza virus biology. Curr Top Microbiol Immunol 385:93–116. doi: 10.1007/82_2014_393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scholtissek C. 1985. Stability of infectious influenza A viruses at low pH and at elevated temperature. Vaccine 3:215–218. doi: 10.1016/0264-410X(85)90109-4. [DOI] [PubMed] [Google Scholar]
- 17.Reed ML, Bridges OA, Seiler P, Kim JK, Yen HL, Salomon R, Govorkova EA, Webster RG, Russell CJ. 2010. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity and transmissibility in ducks. J Virol 84:1527–1535. doi: 10.1128/JVI.02069-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galloway SE, Reed ML, Russell CJ, Steinhauer DA. 2013. Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: implications for host range and adaptation. PLoS Pathog 9:e1003151. doi: 10.1371/journal.ppat.1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hatakeyama S, Sakai-Tagawa Y, Kiso M, Goto H, Kawakami C, Mitamura K, Sugaya N, Suzuki Y, Kawaoka Y. 2005. Enhanced expression of an alpha2,6-linked sialic acid on MDCK cells improves isolation of human influenza viruses and evaluation of their sensitivity to a neuraminidase inhibitor. J Clin Microbiol 43:4139–4146. doi: 10.1128/JCM.43.8.4139-4146.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matrosovich M, Matrosovich T, Carr J, Roberts NA, Klenk HD. 2003. Overexpression of the α-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J Virol 77:8418–8425. doi: 10.1128/JVI.77.15.8418-8425.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumann G, Watanabe T, Ito H, Watanabe S, Goto H, Gao P, Hughes M, Perez DR, Donis R, Hoffmann E, Hobom G, Kawaoka Y. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci U S A 96:9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am J Epidemiol 27:493–497. [Google Scholar]
- 23.Totani K, Kubota T, Kuroda T, Murata T, Hidari KI, Suzuki T, Suzuki Y, Kobayashi K, Ashida H, Yamamoto K, Usui T. 2003. Chemoenzymatic synthesis and application of glycopolymers containing multivalent sialyloligosaccharides with a poly(l-glutamic acid) backbone for inhibition of infection by influenza viruses. Glycobiology 13:315–326. doi: 10.1093/glycob/cwg032. [DOI] [PubMed] [Google Scholar]
- 24.Xu R, Krause JC, McBride R, Paulson JC, Crowe JE Jr, Wilson IA. 2013. A recurring motif for antibody recognition of the receptor-binding site of influenza hemagglutinin. Nat Struct Mol Biol 20:363–370. doi: 10.1038/nsmb.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nycholat CM, McBride R, Ekiert DC, Xu R, Rangarajan J, Peng W, Razi N, Gilbert M, Wakarchuk W, Wilson IA, Paulson JC. 2012. Recognition of sialylated poly-N-acetyllactosamine chains on N- and O-linked glycans by human and avian influenza A virus hemagglutinins. Angew Chem Int Ed Engl 51:4860–4863. doi: 10.1002/anie.201200596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramya TN, Weerapana E, Cravatt BF, Paulson JC. 2013. Glycoproteomics enabled by tagging sialic acid- or galactose-terminated glycans. Glycobiology 23:211–221. doi: 10.1093/glycob/cws144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watanabe T, Zhong G, Russell CA, Nakajima N, Hatta M, Hanson A, McBride R, Burke DF, Takahashi K, Fukuyama S, Tomita Y, Maher EA, Watanabe S, Imai M, Neumann G, Hasegawa H, Paulson JC, Smith DJ, Kawaoka Y. 2014. Circulating avian influenza viruses closely related to the 1918 virus have pandemic potential. Cell Host Microbe 15:692–705. doi: 10.1016/j.chom.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruigrok RW, Martin SR, Wharton SA, Skehel JJ, Bayley PM, Wiley DC. 1986. Conformational changes in the hemagglutinin of influenza virus which accompany heat-induced fusion of virus with liposomes. Virology 155:484–497. doi: 10.1016/0042-6822(86)90210-2. [DOI] [PubMed] [Google Scholar]
- 29.Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. 2006. Avian flu: Influenza virus receptors in the human airway. Nature 440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 30.DuBois RM, Zaraket H, Reddivari M, Heath RJ, White SW, Russell CJ. 2011. Acid stability of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity. PLoS Pathog 7:e1002398. doi: 10.1371/journal.ppat.1002398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narasaraju T, Sim MK, Ng HH, Phoon MC, Shanker N, Lal SK, Chow VT. 2009. Adaptation of human influenza H3N2 virus in a mouse pneumonitis model: insights into viral virulence, tissue tropism, and host pathogenesis. Microbes Infect 11:2–11. doi: 10.1016/j.micinf.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 32.Keleta L, Ibricevic A, Bovin NV, Brody SL, Brown EG. 2008. Experimental evolution of human influenza virus H3 hemagglutinin in the mouse lung identifies adaptive regions in HA1 and HA2. J Virol 82:11599–11608. doi: 10.1128/JVI.01393-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koerner I, Matrosovich MN, Haller O, Staeheli P, Kochs G. 2012. Altered receptor specificity and fusion activity of the haemagglutinin contribute to high virulence of a mouse-adapted influenza A virus. J Gen Virol 93:970–979. doi: 10.1099/vir.0.035782-0. [DOI] [PubMed] [Google Scholar]
- 34.Zaraket H, Bridges OA, Russell CJ. 2013. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus replication and pathogenesis in mice. J Virol 87:4826–4834. doi: 10.1128/JVI.03110-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.England RJ, Homer JJ, Knight LC, Ell SR. 1999. Nasal pH measurement: a reliable and repeatable parameter. Clin Otolaryngol Allied Sci 24:67–68. doi: 10.1046/j.1365-2273.1999.00223.x. [DOI] [PubMed] [Google Scholar]
- 36.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.