Abstract
Background:
Do not resuscitate (DNR) order is an important aspect of medical practice. Since the implementation of critical care response team (CCRT), frequently we have encountered with patients in the wards that should have been made DNR. Initiating DNR became an important part of CCRT activity. We were obliged to extended the role of CCRT - beyond managing seriously ill patients - in addressing the code status for patients after discussion with the managing teams.
Purpose:
We compare the trend of initiation of DNR orders in the regular ward before and after implementing CCRT.
Methods:
Our hospital is 1200 bed tertiary care center. CCRT has been launched in January 1, 2008. The CCRT is 24/7 service led by in-house North American certified intensivists. Cohort analysis of prospectively collected data of 5406 CCRT activation from January 1, 2008, to September 30, 2013. Data before implementation of CCRT was available for 299 patients from the period of June 1, 2007, to December 31, 2007. A comparison made between the two groups (before and after implementation of CCRT) for demographic data and percentage of patients in whom DNR order initiated.
Results:
Before CCRT implementation, 299 patients were attended by Intensive Care Unit physician for regular consultation, 41.1% were females and 52.4% were males with mean of age 58.44 ± 18.47 standard deviation (SD). DNR was initiated in 2.7% of patients. After CCRT implementation, 5904 CCRT activations, 47.6% females and 52.4% males with mean of age 59.17 ± 20.07 SD DNR initiated in 468 (7.9%) of cases. There was 5.2% increase in DNR orders initiation and completion after CCRT introduced to our institute.
Keywords: Critical care, do not resuscitate, end-of-life care, ethics, intensive care, rapid response team
Introduction
Although do not resuscitate (DNR) order is an important part in the field of medical practice since the introduction of the concept of cardiopulmonary resuscitation 1960 by The American Heart Association, still DNR concept is not very well-perceived in the Middle Eastern Arab countries.
The critical care response team (CCRT) was introduced to bring intensive care expertise to any acutely ill patient irrespective of location within the hospital, envisioned, as “critical care without walls” is one of these initiatives.[1]
Deployment of such teams was one of the main interventions recommended by the Institute for Healthcare improvement in its “100,000 Lives Campaign” that was launched in 2005.[2]
A preset physiologic and clinical representing warning system for activation of CCRT was suggested.[3]
The effects and benefits of CCRT on patients care are not limited to the identification and resuscitation of critically ill patients, we have found in our institution that actions, work, and planning goes much further, and one of the major treatment impacts that can occur is the planning for escalation or setting limits of care as the situation demands it.
A new role for CCRT has been explored during the process of implementation of such teams, which is addressing the DNR status for patients in the ward,[4] thus preventing unnecessary Intensive Care Unit (ICU) admissions. No studies from the Middle Eastern Arab countries have addressed the implementation of rapid response team (RRT) (equivalent to CCRT) in initiating DNR as part of their activities. In one previous study from our center, the ICU physicians proved to have a major role in initiating DNR.[5]
Since the implementation of CCRT, frequently we were in a situation evaluating patients in the wards that should have been made DNR status based on their terminal illness, poor functional and mental health status, terminal malignancy futile treatment, and multiple irreversible organ failure. Initiating DNR became an important part of CCRT activity.
We have found ourselves obliged to extended role of CCRT - beyond managing seriously ill patients - in addressing the DNR status for patients after discussion with the managing teams and through explanation and communication with the families.
Objective
Is to evaluate the role of CCRT in evaluation and initiation of DNR status for patients in whom CCRT was activated after discussion with the attending physicians and families.
Many studies have evaluated the effectiveness of RRTs by overall decrease in cardiac arrest rates among hospitalized patients. We studied an alternative outcome of RRT, namely, its on goals of care and designation of DNR orders in a single institution.
We compared the frequency of DNR order for patients who deserve to be made DNR before and after implementing CCRT.
Methods
This study was carried out in King Abdulaziz Medical City, Riyadh, Saudi Arabia, which is 1200 bed tertiary care center. CCRT has been launched in January 1st, 2008, after ethical approval of the CCRT committee. The CCRT is 24/7 service led by in-house North American certified intensivists with a team of physician in training, respiratory therapist, and ICU nurse.
The design of the study is a retrospective chart review of a collected data of 5904 CCRT activation from January 1st, 2008, to September 30, 2013, and did not include actual intervention with human subjects.
Data of DNR status before implementation of CCRT was available for 299 patients; whom the intensivist was involved as a consultation service; from the period of June 1, 2007, to December 31, 2007.
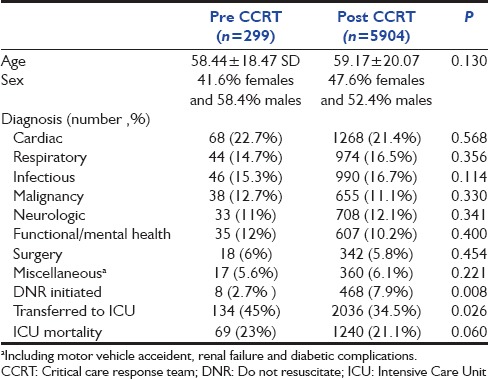
A comparison was made for the two groups (before and after implementation of CCRT) for demographic data and percentage of patients in whom DNR order was initiated by CCRT [Table 1]. The data were analyzed using SPSS V 16.0 (SPSS Inc., Chicago, IL, USA). Traditional statistical analysis, such as t-test, frequencies, and descriptive statistics were used. The results were expressed as percentage and mean ± standard deviation (SD). A two-sided P < 0.05 was considered statistically significant.
Table 1.
Demographic date
Results
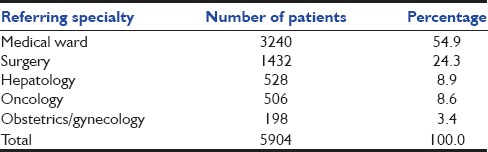
Before CCRT implementation, 299 patients referred to ICU service as consultation, 41.1% females and 52.4% males with mean of age 58.44 ± 18.47 SD. The outcome of 299 patients, 57.5.8% transferred to ICU, 39.8% managed in the floor, and DNR was initiated in 2.7% of patients by the consulting ICU service. The attending physician or his designee was present at bedside in 71.6% of CCRT activations. After CCRT implementation, 5904 CCRT activations, 47.6% females and 52.4% males with mean of age 59.17 ± 20.07 SD The CCRT activation outcome of patients was 2036 (34.5%) transferred to a critical care area, 3400 patients (57.6%) managed in the floor, and DNR initiated in 468 (7.9%) of cases by CCRT. The attending physician or his designee was present at bedside in 87.6% of CCRT activations. The referring specialties were summarized in [Table 2].[2]
Table 2.
Referring specialties
Total of 468/5904 patients made DNR, 192 DNR orders completed immediately, 201 completed within the same CCRT activation event, and 75 patients made DNR during their hospital course.
The difference in percentage of patients who were made DNR after implementation of CCRT compared to the percentage of patients who were made DNR before implementation of CCRT was statistically significant with P = 0.0008. This result is significant at P < 0.05 using Chi-square statistic with the limitation of a small number of the control group.
Discussion
A few limitations are applied to our study being single center, retrospective design, and a small number of the control group. In addition, the results might not be applicable internationally as the RRTs structure is varied widely. However, if mortality is the only outcome; RRT should be questioned.[6]
In a cohort of Australian hospitals, it was found that emergency teams in those hospitals that implemented an RRT than in control hospitals[7] issued more DNR orders.
In spite that the initial MERIT study[8] did not prove the effect of RRT systems in decreasing the incidence of cardiac arrest, unplanned ICU admissions, or unexpected death; responders who were part of an RRT were more likely than other caregivers to add DNR orders (8% vs. 3%). The activation of RRT resulted in some instances in an increase of DNR orders up to 10%.[9]
The research continued exploring new roles for enhanced end-of-life (EOL) care associated with deploying an RRT.[10] Deployment of the RRT was associated with generally improved EOL pain management and psychosocial care.
There are several reasons why intensivists are in a unique position to participate in the EOL decisions. Intensive care physicians have a detailed understanding of key aspects of critical illness and limits of vital organ support.[11]
The management of dying and the provision of in-hospital EOL care have become vital daily practice of intensivists. Because the intensivists role has also recently expanded to that of RRT systems leader, EOL decision became part of the RRT system practice.[12]
There are many potentials for RRT consultation to play an important milestone for many patients approaching EOL as they are frequently participate in EOL.
Discussions and decision-making but they may miss opportunities to facilitate EOL care.[13] Some authors have demonstrated the increase of DNR orders after implementation of RRT.[4,14] The proposed reason for the increase in DNR order after implementation of CCRT in our institute is the early call of CCRT with the earliest physiologic or clinical derangement of patients giving more time to discuss with the primary team and families about the DNR status of the patient. Thus, preventing unnecessary ICU admission and prolongation of patient and family suffering, together with the cost reduction and preservation of limited ICU resources. DNR is an important aspect of patient care, yet it is still underutilized by many physicians in spite of clear hospital policy due to variation in cultural and religious believes among physicians specially the Middle East area.
Our CCRT has relatively unique structure compared to other RRT systems with four-member intensivist-led multidisciplinary RRT responded to provide the necessary management and disposition. The RRT function extended to provide follow-up until clinical stabilization. In addition, the RRT provided a mandatory post-ICU follow-up for a minimum of 48 h.[15]
In general, non-ICU physicians may be less favorably positioned to address the DNR status of their patients. As the ability of non-ICU physicians to prognosticate in cases of advanced disease has been reported to be poor and typically overly optimistic and lack of follow-up their patients once in the ICU.[16,17,18]
We are proposing another reason for the increase in DNR order after implementation of CCRT in our institute is the observed increase in the awareness and confidence of the attending physicians to address the DNR status of the patient in the presence of CCRT.
Our hospital policy requires signature by three physicians to complete the DNR status of the patient.
A new criterion to activate CCRT after considering DNR status of the patient by the attending physicians has been established, and the reason is to involve ICU physicians in countersigning the DNR order, as the attending usually prefer ICU physicians to be involved in EOL care of the patients who have been made DNR.
We can see many potentials in expanding the role of CCRT to be involved in the EOL care particularly when addressing DNR status of the patients and careful follow-up of patients and proper cooperation with palliative care teams. DNR orders as well as many aspects of EOL issues are still to be more explored specially in the Arab Middle Eastern countries and hopefully, this study might be one of many studies to pave the way to answer other important questions such as what is the rate of patients receiving a DNRorder in relation to the rate of patients requiring such an order and not addressed.
Conclusion
CCRT plays an important role in addressing and initiating DNR for those patients seen in the medical floor preventing unnecessary ICU admission.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Miss. Lian Fong for her help in following up data collection for the CCRT.
References
- 1.Hillman K. Critical care without walls. Curr Opin Crit Care. 2002;8:594–9. doi: 10.1097/00075198-200212000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Cambridge, MA: Institute for Healthcare Improvement; [Last updated on 2010 Aug 16; Last cited on 2013 May 04]. Million Lives Campaign. Getting Started Kit: Rapid Response Teams. Available from: http://www.ihi.org . [Google Scholar]
- 3.Gao H, McDonnell A, Harrison DA, Moore T, Adam S, Daly K, et al. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med. 2007;33:667–79. doi: 10.1007/s00134-007-0532-3. [DOI] [PubMed] [Google Scholar]
- 4.Jones DA, McIntyre T, Baldwin I, Mercer I, Kattula A, Bellomo R. The medical emergency team and end-of-life care: A pilot study. Crit Care Resusc. 2007;9:151–6. [PubMed] [Google Scholar]
- 5.Gouda A, Al-Jabbary A, Fong L. Compliance with DNR policy in a tertiary care center in Saudi Arabia. Intensive Care Med. 2010;36:2149–53. doi: 10.1007/s00134-010-1985-3. [DOI] [PubMed] [Google Scholar]
- 6.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: A systematic review and meta-analysis. Arch Intern Med. 2010;170:18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 7.Chen J, Flabouris A, Bellomo R, Hillman K, Finfer S MERIT Study Investigators for the Simpson Centre and the ANZICS Clinical Trials Group. The medical emergency team system and not-for-resuscitation orders: Results from the MERIT study. Resuscitation. 2008;79:391–7. doi: 10.1016/j.resuscitation.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: A cluster-randomised controlled trial. Lancet. 2005;365:2091–7. doi: 10.1016/S0140-6736(05)66733-5. [DOI] [PubMed] [Google Scholar]
- 9.Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: Preliminary study. BMJ. 2002;324:387–90. doi: 10.1136/bmj.324.7334.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vazquez R, Gheorghe C, Grigoriyan A, Palvinskaya T, Amoateng-Adjepong Y, Manthous CA. Enhanced end-of-life care associated with deploying a rapid response team: A pilot study. J Hosp Med. 2009;4:449–52. doi: 10.1002/jhm.451. [DOI] [PubMed] [Google Scholar]
- 11.Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006;34:2463–78. doi: 10.1097/01.CCM.0000235743.38172.6E. [DOI] [PubMed] [Google Scholar]
- 12.Jones DA, DeVita M, Bellomo R. Current concepts: Rapid-response teams. N Engl J Med. 2011;365:139–46. doi: 10.1056/NEJMra0910926. [DOI] [PubMed] [Google Scholar]
- 13.Downar J, Rodin D, Barua R, Lejnieks B, Gudimella R, McCredie V, et al. Rapid response teams, do not resuscitate orders, and potential opportunities to improve end-of-life care: A multicentre retrospective study. J Crit Care. 2013;28:498–503. doi: 10.1016/j.jcrc.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Smith RL, Hayashi VN, Lee YI, Navarro-Mariazeta L, Felner K. The medical emergency team call: A sentinel event that triggers goals of care discussion. Crit Care Med. 2014;42:322–7. doi: 10.1097/CCM.0b013e3182a27413. [DOI] [PubMed] [Google Scholar]
- 15.Al-Qahtani S, Al-Dorzi HM, Tamim HM, Hussain S, Fong L, Taher S, et al. Impact of an intensivist-led multidisciplinary extended rapid response team on hospital-wide cardiopulmonary arrests and mortality. Crit Care Med. 2013;41:506–17. doi: 10.1097/CCM.0b013e318271440b. [DOI] [PubMed] [Google Scholar]
- 16.Gibbins J, McCoubrie R, Alexander N, Kinzel C, Forbes K. Diagnosing dying in the acute hospital setting – Are we too late? Clin Med (Lond) 2009;9:116–9. doi: 10.7861/clinmedicine.9-2-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glare P, Virik K, Jones M, Hudson M, Eychmuller S, Simes J, et al. A systematic review of physicians’ survival predictions in terminally ill cancer patients. BMJ. 2003;327:195–8. doi: 10.1136/bmj.327.7408.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finucane TE. How gravely ill becomes dying: A key to end-of-life care. JAMA. 1999;282:1670–2. doi: 10.1001/jama.282.17.1670. [DOI] [PubMed] [Google Scholar]


