Abstract
Objective:
To examine trajectories of adolescent borderline personality (BP) features in a normative-risk cohort (n = 566) of Canadian children assessed at ages 13, 14, 15, and 16 and childhood predictors of trajectory group membership assessed at ages 8, 10, 11, and 12.
Method:
Data were drawn from the McMaster Teen Study, an on-going study examining relations among bullying, mental health, and academic achievement. Participants and their parents completed a battery of mental health and peer relations questionnaires at each wave of the study. Academic competence was assessed at age 8 (Grade 3). Latent class growth analysis, analysis of variance, and logistic regression were used to analyze the data.
Results:
Three distinct BP features trajectory groups were identified: elevated or rising, intermediate or stable, and low or stable. Parent- and child-reported mental health symptoms, peer relations risk factors, and intra-individual risk factors were significant predictors of elevated or rising and intermediate or stable trajectory groups. Child-reported attention-deficit hyperactivity disorder (ADHD) and somatization symptoms uniquely predicted elevated or rising trajectory group membership, whereas parent-reported anxiety and child-reported ADHD symptoms uniquely predicted intermediate or stable trajectory group membership. Child-reported somatization symptoms was the only predictor to differentiate the intermediate or stable and elevated or rising trajectory groups (OR 1.15, 95% CI 1.04 to 1.28). Associations between child-reported reactive temperament and elevated BP features trajectory group membership were 10.23 times higher among children who were bullied, supporting a diathesis–stress pathway in the development of BP features for these youth.
Conclusions:
Findings demonstrate the heterogeneous course of BP features in early adolescence and shed light on the potential prodromal course of later borderline personality disorder.
Keywords: attention-deficit hyperactivity disorder, borderline personality features, diathesis–stress, trajectory analysis
Abstract
Objectif:
Examiner les trajectoires des traits de la personnalité limite (PL) à l’adolescence dans une cohorte de risque normatif (N = 566) d’enfants canadiens évalués à 13, 14, 15 et 16 ans, et les prédicteurs dans l’enfance de l’appartenance à un groupe de trajectoires évaluée à 8, 10, 11 et 12 ans.
Méthode:
Le données ont été tirées de la McMaster Teen Study, une étude en cours qui examine les relations entre l’intimidation, la santé mentale, et la réussite scolaire. Les participants et leurs parents ont répondu à une batterie de questionnaires sur la santé mentale et les relations avec les pairs à chaque cycle de l’étude. Le rendement scolaire a été évalué à 8 ans (3e année). Une analyse de croissance de la structure latente, une analyse de variance, et une régression logistique ont servi à analyser les données.
Résultats:
Trois groupes distincts de trajectoires des traits de la PL ont été identifiés : élevé/montant, intermédiaire/stable, et faible/stable. La symptomatologie de santé mentale, les facteurs de risque des relations avec les pairs, et les facteurs de risque intra-individuels déclarés par les parents et les enfants étaient des prédicteurs significatifs des groupes de trajectoires élevé/montant et intermédiaire/stable. La symptomatologie du TDAH et de la somatisation déclarée par les enfants prédisait à elle seule le groupe de trajectoires élevé/montant, alors que l’anxiété déclarée par les parents et la symptomatologie du TDAH déclarée par les enfants prédisaient uniquement l’appartenance au groupe de trajectoires intermédiaire/stable. La symptomatologie de la somatisation déclarée par les enfants était le seul prédicteur qui différenciait les groupes de trajectoires intermédiaire/stable et élevé/montant (RC = 1,15; IC à 95% [1,04 à 1,28]). Les associations entre le tempérament réactif déclaré par les enfants et l’appartenance au groupe de trajectoires des traits élevés de la PL étaient 10,23 fois plus élevées chez les enfants qui se faisaient intimider, ce qui soutient un modèle diathèse-stress dans le développement des traits de la PL pour ces adolescents.
Conclusions:
Les résultats démontrent le cours hétérogène des traits de la PL au début de l’adolescence et jettent la lumière sur le cours prodromal potentiel du trouble de la personnalité limite (TPL) ultérieur.
Understanding the unfolding of personality disturbance in childhood and adolescence is crucial to illuminating our understanding of adult personality psychopathology and to informing prevention and intervention science. As personality disturbance does not simply manifest de novo in adulthood, research exploring the developmental precipitants and comorbid mental health psychopathology in young people with elevated personality disturbance affords an important opportunity to better understand specific vulnerabilities and prodromal features which may foreshadow the later emergence of clinical disorder.1–3
Borderline personality disorder (BPD) is characterized by an enduring “pattern of instability in personal relationships, self-image, and affect, and marked impulsivity.”4 BPD is estimated to affect 1.6% to 5.9% of the general population and about 10% of people seen in outpatient settings and 20% of people seen in inpatient settings.4 High rates of comorbidity exist between BPD and anxiety and depressive disorders,5 and there is substantial overlap between BPD and attention-deficit hyperactivity disorder (ADHD) and other problems on the externalizing spectrum, such as impulsivity and poor self-regulation, regarding their behavioural and neuropsychological impairments.6 Increasing evidence indicates that borderline personality (BP)-related characteristics or BP-related features are present in children and adolescents and that they confer risk for the development of BPD in adulthood.2,7–11
Empirical research progress has highlighted numerous environmental and biological factors and their interactive influence in the development of BPD in adulthood.12,13 Broadly, it is thought that both adverse early attachment or interpersonal experiences (for example, abuse or neglect) and the core personality traits of affective dysfunction (for example, emotional reactivity and lability) and disinhibition (for example, impulsivity) are integral for the development of BPD in adulthood.14 Indeed, most contemporary theoretical accounts of the pathogenesis of BPD in adulthood15–18 suggest a diathesis–stress process involving these signature risk factors. Despite this generative research, much remains to be understood about the etiological course of BPD. Perhaps most crucial, is whether early subthreshold markers of the disorder have unique developmental patterns of growth across childhood and adolescence and whether they may be differentially associated with biological and environmental risk factors. This question is particularly important given the clinical characterization of the stable instability of patients with BPD19 and longitudinal research which indicates considerable instability of BPD diagnoses, with at least 50% to 70% of adolescents shifting to a subclinical level of symptoms at subsequent assessments.8,20,21 As such, it is reasonable to suspect that the potential prodromal course of this personality disturbance in childhood and adolescence may be characterized by multinomial heterogeneity with important individual differences in both the magnitude and direction of change.22
Guided in part by extant theoretical models of the pathogenesis of BPD in adulthood, as well as the high degree of covariation between BPD and both internalizing and externalizing psychopathology, we examined associations of childhood intra-individual and interpersonal risk factors from ages 8, and 10 to 12 with person-centred trajectories of BP features for ages 13 to 16 in a community-based sample. To the best of our knowledge, it is the first study to identify and examine the developmental course of BP features in adolescence. Research of this kind is important as little work has examined childhood risk factors for the later development of BPD symptoms or clinical BPD.6,23 This is especially the case regarding the influence of peer social functioning on the development of BP features.2 In addition, given limited empirical tests of the biosocial diathesis–stress model of borderline etiology,15,16 we also examined whether children who carry a putative biological diathesis of reactive temperament were more likely to be in an elevated BP features trajectory group if they also experience being bullied in childhood.
Methods
Participants and Procedure
Data were drawn from the McMaster Teen Study, an on-going study examining the relations between bullying, mental health, and academic achievement.24 The study began in the spring of 2008 (Grade 5, age 10; time 1 [T1]). Participants were initially recruited from a random sample of 51 schools within a large Southern Ontario Public School Board. From the recruitment process, 875 participants agreed to be part of the longitudinal arm of the study. Parental consent and child assent were obtained at each time point. The study has maintained consistent yearly approval status from the pertinent university research ethics boards (McMaster University and the University of Ottawa). Data collected annually from T1 (Grade 5; age 10) to T7 (Grade 11; age 16) were included in the present study, as were data from participants’ official school records from Grade 3 (age 8).
Data for our study were selected on the basis of 566 (252 [44.5%] boys, 314 [55.5%] girls) participants who had valid reports of BP features for at least 1-time point across T4 (Grade 8; age 13) to T7 (Grade 11; age 16), thus permitting inclusion in trajectory analyses. Among the analytic sample, 89.8% (n = 508) had complete BP features data at T4, 85.5% (n = 484) had complete data at T5, 79.2% (n = 448) had complete data at T6, and 73.7% (n = 417) had complete data at T7. Data at all 4 time points were available for 62.4% (n = 353) of the sample.
Measures
Indicators of Borderline Personality Features Trajectories
The Borderline Personality Features Scale for Children (BPFS-C) was used to examine child-reported features of BP from T4 (age 13) to T7 (age 16).2 The BPFS-C consists of 24 items rated on a 5-point Likert-type scale, with the response set including 0 = not at all true, 1 = hardly ever true, 2 = sometimes true, 3 = often true, and 4 = always true. The BPFS-C is a psychometrically sound measure of BP features.2,25 Criterion validity with reference to clinical diagnoses of BPD in youth has also been established.26 A BP features composite was calculated as an average of all items. Internal consistencies for the BPFS-C in the present sample were 0.90 at T4 (age 13), 0.91 at T5 (age 14), 0.91 at T6 (age 15), and 0.91 at T7 (age 16).
Predictors of Borderline Personality Features Trajectories
An adaptation of the Olweus Bully/Victim Questionnaire27,28 was used to measure peer victimization. Internal consistency for the peer victimization items was good at each time point (T1 Cronbach α = 0.82; T2 Cronbach α = 0.80; T3 Cronbach α = 0.82). Scores were averaged across T1 to T3 (ages 10 to 12) to form a composite measure of peer victimization (composite Cronbach α = 0.74).
A shortened version of the Aggressive Behaviour Scale29 was used to assess T1 to T3 (ages 10 to 12) child-reported physical and relational aggression. Children responded on a 4-point scale (0 = not at all true to 3 = completely true). Internal consistencies for both forms of aggression over time were good (T1 Cronbach α = 0.87, T2 Cronbach α = 0.85, T3 Cronbach α = 0.84 for physical aggression and T1 Cronbach α = 0.81, T2 Cronbach α = 0.80, T3 Cronbach α = 0.80 for relational aggression). Physical and relational aggression scores were averaged across T1 to T3 (ages 10 to 12) to provide composite measures of childhood physical and relational aggression (composite Cronbach αs = 0.84 and 0.76 for physical and relational aggression, respectively).
Parent-reported child anxiety, depression, ADHD, and somatization symptoms were assessed from T1 to T3 using the Brief Child and Family Phone Interview Version 3 (BCFPI-3)30 and the parent report somatization subscale of the Behavior Assessment System for Children, Second Edition (BASC-2).31 The BCFPI-3 is a 30-minute structured phone interview used to screen for emotional and behavioural issues in children ages 3 to 18 years. The BASC-2 is a multi-method, multidimensional measure of behaviour and self-perceptions of people aged between 2 and 25. Items were rated on a 3-point Likert scale (0 = never to 2 = often). Responses were summed within each scale (items reversed where necessary) to yield total scores. Internal consistency (Cronbach α) of the BCFPI-3 subscales across T1 to T3 (age 10 to 12) ranged from 0.81 to 0.82 (anxiety), 0.81 to 0.82 (depression), and 0.84 to 0.81 (symptoms of ADHD). Scales were averaged across T1 to T3 to provide composite measures of parent-reported symptoms of anxiety, depression, and ADHD symptoms. Parent-report data on the BASC-2 somatization subscale were collected at T3. Internal consistency of this subscale at T3 was 0.75.
Child-reported symptoms of anxiety, depression, and hyperactivity symptoms were assessed from T1 to T3 (ages 10 to 12), and child-reported attention problems and somatization symptoms at T3, using the Self-Report of Personality (SRP) form of the BASC-2.31 Attention problem and somatization symptoms were assessed at T3 as these scales are only included in the adolescent version of the BASC-2. Internal consistency of the BASC-2 subscales at relevant time points ranged from 0.85 to 0.88 (anxiety), 0.87 to 0.90 (depression), 0.78 to 0.80 (hyperactivity), 0.83 (attention problems), and 0.68 (somatization problems). Child-reported symptoms of psychopathology were averaged across T1 to T3 to provide composite measures of anxiety, depression, and hyperactivity symptoms. Additionally, the hyperactivity composite (T1 to T3) and the attention problems score at T3 (r = 0.62) were averaged to yield a child report ADHD symptom composite.
Child-reported reactive temperament was measured at T1 and T2 (ages 10 and 11) using the Frustration or Negative Affect subscale of The Early Adolescent Temperament Questionnaire–Revised (EATQ-R).32 Items were measured on a 5-point response scale (0 = very false to 4 = very true). This scale consisted of 7 items that tap negative affect related to interruption of ongoing tasks or goal blocking. Items were averaged to yield a total scale score. Internal consistency of the negative affectivity scale at both T1 (Cronbach α = 0.82) and T2 (Cronbach α = 0.79) was good. Scale scores at T1 and T2 were averaged to form a negative affectivity composite.
The Education Quality and Accountability Office (EQAO)33 is an Ontario province-wide standardized assessment of reading, writing, and mathematics administered to all students attending a publicly funded school at the end of grades 3 and 6. The Grade 3 (age 8) EQAO assessment was used in our study. The EQAO provides an objective evaluation of students’ cumulative reading, writing, and mathematics ability throughout the elementary division. For each category, students answer numerous multiple choice, short, and long answer questions, that are then converted into a single measure of achievement. Correlations among the Grade 3 reading, writing, and mathematics assessment scores were strong (mean r = 0.67) and were averaged to form an index of general academic skills.
Semi-parametric group-based methods were used to identify the number and shape of distinct trajectories of BP features using 4 cycles of data (T4 [Grade 8; age 13] –T7 [Grade 11; age 16]). Models were estimated in Mplus 7.1134 through latent class growth analysis. Given the lack of any prior theoretical or empirical work suggesting distinct trajectories of BP features in adolescence, up to a 5-class solution was examined. Evaluation of the best fitting models was based on consideration of the following criteria: 1) the Bayesian information criterion (BIC); 2) the Lo-Mendell-Rubin adjusted likelihood ratio test (LMR-LRT); 3) entropy; 4) a conceptually clear model; and 5) a model with a sufficient number of members in each group to allow for examination of group differences.
Results
Empirically Derived Borderline Personality Features Trajectory Groups
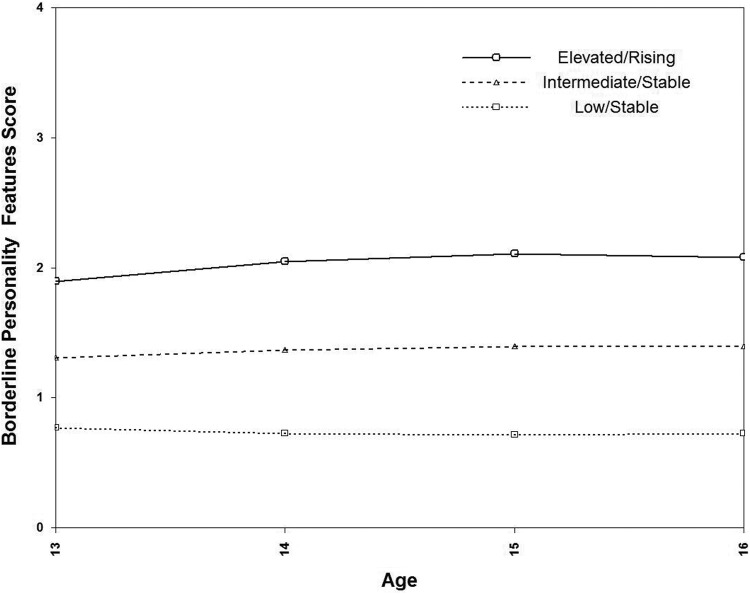
Evaluation of model fit statistics (Figure 1) suggested that a 3-class solution was both empirically and conceptually justified. The 3-group solution is presented in Figure 1. In the 3-group trajectory model, most adolescents demonstrated an intermediate or stable level of BP features (42% of the sample; n = 235; 107 boys, 128 girls) with the second largest group following a low or stable pattern of BP features (34%; n = 195; 109 boys, 86 girls). Finally, there were a group of youth who followed an elevated or rising pattern of BP features (24%; n = 136; 36 boys, 100 girls). Examination of posterior probabilities indicated that children were well matched to their group (0.85 for the intermediate or stable, 0.92 for the low or stable, and 0.90 for the elevated or rising increasing groups, respectively).
Figure 1.
Three trajectory model of borderline personality features. Fit indices for 1 trajectory model (Bayesian Information Criteria [BIC] = 3541.67; Lo-Mendell-Rubin likelihood ratio test [LMR-LRT], not applicable; entropy, not applicable), 2 trajectory (BIC = 2837.52; LMR-LRT, P < 0.001; entropy = 0.78), 3 trajectory (BIC = 2633.15; LMR-LRT, P < .001; entropy = 0.75), 4 trajectory (BIC = 2602.85; LMR-LRT, P = 0.49; entropy = 0.78); 5 trajectory (BIC = 2589.00; LMR-LRT, P = 0.15; entropy = 0.72).
There were differences in the proportion of boys and girls in the BP features trajectory groups (χ2 = 28.26, df = 2, P < 0.001). Examination of adjusted standardized residuals in the differences in sex proportions across the 3 trajectory groups indicated that there were significantly more girls in the elevated or rising group (31.8% girls, compared with 14.3% boys) and significantly more boys in the low or stable group (43.3% boys, compared with 27.4% girls).
Covariates Associated with Trajectory Group Membership
Analyses of variance procedures were used to explore whether mental health, peer relations, and intra-individual risk factors differentiated among the BP features trajectory groups. The Benjamini-Hochberg (BH)35 correction for multiple testing was used to protect against type 1 error. For these analyses, estimates of effect size (Cohen d) are provided.36 In follow-up multinomial and logistic regression analyses, the predictive significance of each covariate for membership in the empirically-derived BP features trajectory groups was also examined in conjunction with child sex given evidence that BPD prevalence rates may be higher among women than men.4,37,38 Because relatively few such sex interactions emerged, we note in Table 2 when effects were significantly larger for boys or girls and describe below relevant interaction effects. Finally, we also tested if some of the covariates were better predictors of BP features trajectory group than others by simultaneously entering all predictors, using the low or stable group as the reference group in a multinomial logistic regression analyses and the intermediate or stable group as the reference group in a binary logistic regression analyses comparing the intermediate or stable and elevated or rising groups.
Table 2.
Planned comparisons on risk factors with borderline personality features trajectory groups.
| Outcome | Trajectory group contrasts | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Intermediate or stable (n = 235; 41.5%, compared with low or stable (n = 195; 34.5%) | Elevated or rising (n = 136; 24.0%), compared with low or stable (n = 195; 34.5%) | Elevated or rising (n = 136; 24.0%), compared with intermediate or stable (n = 235; 41.5%) | |||||||
| B (SE) | P | d | B (SE) | P | d | B (SE) | P | d | |
| Mental health parent report | |||||||||
| Anxiety | 0.72 (0.23) | 0.002a | 0.31 | 0.80 (0.27) | 0.003a | 0.34 | 0.08 (0.26) | 0.75 | 0.04 |
| Depression | 0.48 (0.14) | 0.001a | 0.36 | 0.73 (0.16) | <0.001a | 0.53 | 0.25 (0.15) | 0.10 | 0.17 |
| ADHD | 1.09 (0.26) | <0.001a | 0.41 | 1.27 (0.30) | <0.001a | 0.50 | 0.19 (0.29) | 0.52 | 0.07 |
| Somatization | 0.76 (0.33) | 0.02a | 0.24 | 1.32 (0.38) | 0.001a | 0.44 | 0.56 (0.36) | 0.13 | 0.17 |
| Mental health child report | |||||||||
| Anxiety | 2.87 (0.47)b | <0.001a | 0.60 | 5.75 (0.55) | <0.001a | 1.21 | 2.88 (0.53) | <0.001a | 0.57 |
| Depression | 1.84 (0.40) | <0.001a | 0.48 | 4.28 (0.46) | <0.001a | 1.10 | 2.44 (0.45) | <0.001a | 0.53 |
| ADHD | 2.25 (0.33) | <0.001a | 0.72 | 3.79 (0.38) | <0.001a | 1.15 | 1.54 (0.36) | <0.001a | 0.42 |
| Somatization | 0.85 (0.28) | 0.003a | 0.33 | 2.44 (0.33) | <0.001a | 0.88 | 1.59 (0.32) | <0.001a | 0.53 |
| Peer relations (child report) | |||||||||
| Peer victimization | 0.26 (0.05) | <0.001a | 0.48 | 0.44 (0.06) | <0.001a | 0.87 | 0.18 (0.06) | 0.003a | 0.30 |
| Physical aggression | 0.13 (0.04) | <0.001a | 0.38 | 0.24 (0.04)c | <0.001a | 0.67 | 0.11 (0.04) | 0.006a | 0.27 |
| Relational aggression | 0.12 (0.03) | <0.001a | 0.47 | 0.23 (0.03) | <0.001a | 0.85 | 0.11 (0.03) | <0.001a | 0.37 |
| Intra-individual risk | |||||||||
| Child temperament | 0.23 (0.07)b | 0.001a | 0.32 | 0.53 (0.08) | <0.001a | 0.84 | 0.30 (0.07) | <0.001a | 0.45 |
| General academic skills (EQAO composite); Grade 3 | 0.04 (0.06) | 0.51 | 0.07 | –0.00 (0.07) | 0.98 | 0.00 | –0.04 (0.07) | 0.54 | 0.08 |
aSignificant at the Benjamini–Hochberg adjusted P value; bEffect significantly larger for boys; cEffect significantly larger for girls
ADHD = attention-deficit hyperactivity disorder; EQAO = The Education Quality and Accountability Office
Analysis of variance F statistics were significant for each measure except General Academic Skills (EQAO Composite).
Means and standard deviations of risk factors by BP features trajectory group are presented in Table 1. As shown in Table 2, all of the indicators with the exception of the general academic competence indicator distinguished the intermediate or stable and the elevated or rising trajectory groups from the low stable trajectory group (BH corrected). Follow-up multinominal regressions revealed that 1 of 26 effects were larger for girls than boys, while 2 of 26 effects were larger for boys than girls. Regarding contrasts between the elevated or rising group and the intermediate or stable group, only child-report measures of mental health symptoms, peer relations, and temperament were significant discriminators of membership in the elevated or rising group compared with the intermediate or stable group (BH corrected). There were no interactions with child sex in follow-up logistic regressions.
Table 1.
Means and standard deviations (SD) of antecedent symptoms of psychopathology, peer relations, and intra-individual risk variables by empirically derived borderline personality features trajectory groups.
| Outcome | Borderline personality features trajectory group | |||||
|---|---|---|---|---|---|---|
| Low or stable | Intermediate or stable | Elevated or rising | ||||
| Mean | SD | Mean | SD | Mean | SD | |
| Mental health parent report | ||||||
| Anxiety | 3.62 | 2.35 | 4.34 | 2.34 | 4.43 | 2.46 |
| Depression | 0.68 | 1.20 | 1.15 | 1.44 | 1.40 | 1.58 |
| ADHD | 3.22 | 2.43 | 4.30 | 2.82 | 4.49 | 2.76 |
| Somatization | 3.73 | 2.86 | 4.48 | 3.46 | 5.04 | 3.25 |
| Mental health child report | ||||||
| Anxiety | 6.68 | 4.45 | 9.55 | 5.04 | 12.43 | 5.18 |
| Depression | 2.80 | 3.08 | 4.64 | 4.42 | 7.08 | 4.86 |
| ADHD | 3.87 | 2.71 | 6.12 | 3.44 | 7.66 | 4.04 |
| Somatization | 1.50 | 2.32 | 2.35 | 2.76 | 3.94 | 3.37 |
| Peer Relations child report | ||||||
| Peer victimization | 0.48 | 0.43 | 0.74 | 0.62 | 0.92 | 0.61 |
| Physical aggression | 0.25 | 0.29 | 0.38 | 0.39 | 0.49 | 0.45 |
| Relational aggression | 0.28 | 0.23 | 0.40 | 0.29 | 0.51 | 0.34 |
| Intra-individual risk | ||||||
| Child temperament | 1.98 | 0.68 | 2.20 | 0.74 | 2.51 | 0.57 |
| General academic skills (EQAO Composite); grade 3 | 3.21 | 0.59 | 3.25 | 0.57 | 3.21 | 0.50 |
ADHD = attention-deficit hyperactivity disorder; EQAO = The Education Quality and Accountability Office.
Estimates of our multinomial model in which all predictors were entered simultaneously are presented in Table 3. Only parent-reported anxiety and child-reported ADHD symptoms were associated with the intermediate or stable trajectory group relative to the low or stable group. Membership in the elevated or rising trajectory group (compared with the low or stable group) was associated with child-reported ADHD and somatization symptoms and relational aggression. Lastly, we conducted a binomial logistic regression model comparing the elevated or rising group to the intermediate or stable group, again entering all predictors simultaneously. The only indicator to significantly distinguish these groups was child-reported somatization symptoms (OR 1.15, 95% CI 1.04 to 1.28).
Table 3.
Multinomial logistic regression of empirically derived borderline personality features trajectory groups with symptoms of psychopathology, peer relations, and intra-individual risk factors: combined model.
| Outcome | Trajectory group contrasts | |||||||
|---|---|---|---|---|---|---|---|---|
| Intermediate, compared with low or stable | Elevated or rising, compared with low or stable | |||||||
| B (SE) | eb | P | 95% CI | B (SE) | eb | P | 95% CI | |
| Mental health parent report | ||||||||
| Anxiety | 0.15 (0.06) | 1.17 | 0.01 | (1.04 to 1.31) | 12 (0.08) | 1.13 | 0.11 | (0.97 to 1.31) |
| Depression | 0.06 (0.13) | 1.07 | 0.63 | (0.82 to 1.38) | 0.09 (0.15) | 1.10 | 0.55 | (0.81 to 1.48) |
| ADHD | –0.03 (0.06) | 0.98 | 0.69 | (0.86 to 1.11) | –0.04 (0.08) | 0.96 | 0.59 | (0.82 to 1.12) |
| Somatization | –0.02 (0.05) | 0.98 | 0.66 | (0.89 to 1.08) | –0.03 (0.06) | 0.97 | 0.56 | (0.86 to 1.08) |
| Mental health child report | ||||||||
| Anxiety | 0.07 (0.04) | 1.07 | 0.08 | (0.99 to 1.15) | 0.07 (0.05) | 1.07 | 0.13 | (0.98 to 1.18) |
| Depression | –0.01 (0.06) | 0.99 | 0.81 | (0.88 to 1.10) | 0.05 (0.06) | 1.05 | 0.47 | (0.93 to 1.18) |
| ADHD | 0.23 (0.06) | 1.26 | <0.001 | (1.12 to 1.42) | 0.28 (0.07) | 1.33 | <0.001 | (1.16 to 1.52) |
| Somatization | 0.09 (0.06) | 1.09 | 0.15 | (0.97 to 1.24) | 0.24 (0.07) | 1.27 | 0.001 | (1.11 to 1.46) |
| Peer relations (child report) | ||||||||
| Peer victimization | 0.41 (0.32) | 1.50 | 0.20 | (0.81 to 2.78) | 0.23 (0.37) | 1.25 | 0.54 | (0.61 to 2.57) |
| Physical aggression | –0.36 (0.53) | 0.72 | 0.53 | (0.25 to 2.02) | –0.07 (0.58) | 0.93 | 0.90 | (0.30 to 2.92) |
| Relational aggression | 0.78 (0.64) | 2.17 | 0.23 | (0.62 to 7.63) | 1.74 (0.73) | 5.67 | 0.02 | (1.36 to 23.58) |
| Intra-individual risk | ||||||||
| Child temperament | –0.02 (0.22) | 0.98 | 0.93 | (0.64 to 1.50) | 0.20 (0.29) | 1.22 | 0.50 | (0.69 to 2.15) |
| General academic skills (EQAO composite); Grade 3 | 0.32 (0.25) | 1.37 | 0.21 | (0.84 to 2.24) | 0.23 (0.30) | 1.26 | 0.44 | (0.70 to 2.29) |
ADHD = attention-deficit hyperactivity disorder; EQAO = The Education Quality and Accountability Office.
Test of Diathesis–Stress for Borderline Personality Features Trajectory Group Membership
In a final analysis we tested whether early adolescent child-reported reactive temperament interacted with peer victimization to predict BP features trajectory group. In this model child-reported reactive temperament was considered a proxy reflecting biological susceptibility to the development of BP when triggered by childhood bullying (that is, harsh interpersonal experiences; a diathesis–stress model). As in prior work,7 we defined interaction as the epidemiological construct of biological synergy39 in which the effect of 2 risk factors present together is greater than the sum of their independent effects. We also used the 2 × 4 table method40 to present relative risks among children with different combinations of reactive temperament and being bullied. Because the 2 × 4 method is designed for binomial outcome variables and requires dichotomization of continuous treatment measures we collapsed the intermediate or stable and elevated or rising trajectory groups into an elevated BP features group and dichotomized at the 80th percentile both the focal predictor (child-reported reactive temperament, scale score = 2.79) and the moderator (peer victimization, scale score = 1.13). Biological interaction was evaluated by calculating 3 measures including the relative excess risk due to interaction (RERI) relative to the risk without exposure, the attributable portion (AP) due to interaction, which is interpreted as the AP of membership in the elevated BP features trajectory group due to interaction among children possessing both risk factors, and the synergy (S) index, which can be interpreted as the excess risk from both risk factors when there is an interaction relative to the excess risk from both risk factors without interaction. If there is no biological interaction, RERI and AP will equal 0 and S will equal 1.41
The point estimates of all 3 interaction metrics suggested evidence for biological interaction between child-reported reactive temperament and peer victimization in the prediction of elevated BP features trajectory group membership (Table 4). Children possessing both risk factors of child-reported reactive temperament (top 20%) and being bullied (top 20%) were 10.23 (95% CI 2.40 to 43.58) times more likely to be in the elevated borderline features trajectory group than were children with neither risk factor. Evidence for biological interaction was also obtained (although attenuated in magnitude) when using the original continuous metric of the predictor variables in follow-up analyses using a method developed by Knol et al42 (results available on request).
Table 4.
Two × 4 table of diathesis–stress interaction between child-reported childhood reactive temperament and peer victimization in predicting membership in elevated borderline personality features trajectory groups.
| Exposure | n | Effect size | ||
|---|---|---|---|---|
| Reactive temperament | Peer victimization | Low or stable | Elevated | RR (95% CI) |
| + | – | 19 | 52 | [RR01] 2.00 (1.14 to 3.52) |
| – | + | 12 | 65 | [RR10] 3.96 (2.07 to 7.58) |
| + | + | 2 | 28 | [RR11] 10.23 (2.40 to 43.58) |
| – | – | 162 | 226 | REF [1.0] |
| Total | 195 | 371 | ||
| Biological interaction measure | Point estimate (95% CI) | |||
| RERI | 5.27 (–9.67 to 20.21) | |||
| AP | 0.52 (–0.23 to 1.26) | |||
| S | 2.33 (0.41 to 13.13) | |||
AP = attributable portion due to interaction; RERI = relative excess risk due to interaction; RR = relative risk; S = synergy index.
RERI is calculated as RR11 – RR10 – RR01 + 1; AP = RERI/RR11; S = [RR11 - 1]/[(RR10 -1) + (RR01 - 1)].
The reference group (REF) are individuals who possess neither exposure factor (that is, not in the top 20% of either reactive temperament or peer victimization).
Discussion
Our study is the first to our knowledge to model person-centred developmental trajectories of BP features over the course of adolescence and examine their associations with non-age-overlapping antecedent risk factors in a community-based sample. Trajectory modelling supported the identification of 3 distinct BP features trajectory groups—low or stable, intermediate or stable, and elevated or rising—and provides further evidence that a distinct group of people with elevated BP features are present and identifiable in childhood and adolescence.2,7,9 The preponderance of girls in the elevated or rising BP features trajectory group provides preliminary support for a downward extension of sex differences that have been noted in BPD diagnoses in adults4,37,38 and is consistent with prior work using the BPFS-C which found that girls had elevated total scores relative to boys.2 Nevertheless, empirical research regarding sex differences in BPD has been inconsistent13,43,44 and remains a question of much interest for clinicians and researchers.45
Results of planned comparisons are consistent with existing empirical evidence indicating high rates of comorbidity and symptom overlap between BPD and anxiety and depressive disorders, as well as the common behavioural and neuropsychological impairments between BPD and ADHD and other symptoms on the externalizing spectrum.5,46 These results also converge with more recent work7,47,48 which has found associations between childhood ADHD, internalizing, and externalizing symptoms, lower IQ, and poor behavioural control, and subsequent adolescent BPD symptoms.
Burke and Stepp47 and Stepp et al48 have called particular attention to the possibility that childhood ADHD may represent part of an early developmental path to BPD as both disorders share a common impulsivity component. In addition, in a recent prospective follow-up of girls,49 it was found that ADHD was associated with self-harm behaviour in young adults. Thus some of the biological states that underlie the development of BPD and other mood disorders may present in the context of ADHD symptoms or more broadly as trait impulsivity in childhood.50
To our knowledge, no studies have examined the predictive significance of childhood somatization symptoms for the development of BP features in adolescence. One possibility explaining the robust predictive significance of somatization symptoms is that they may reflect prodromal elements of the histrionic or emotional hypochondriasis element of BPD as they reflect the tendency of the child or adolescent to be overly sensitive and complain about relatively minor physical problems or ailments, and to overreport the occurrence of various physical complaints—all of which by definition are help seeking and involve attaining the attention of caretaking figures.51 Findings for relational aggression are consistent with previous work23,52 calling attention to this form of aggression as particularly relevant in the development of BP symptoms. Lastly, the few predictor interaction effects with child sex suggested that they may operate differently for girls and boys. Additional research examining the moderating role of child sex in predicting adolescent BP features is needed.
The results of our diathesis–stress interaction test suggested that youth were more likely to be in an elevated BP features trajectory group if they experienced higher levels of peer victimization in the context of their own self-reported reactive temperament. These findings provide suggestive evidence that the invalidating environment component of the diathesis–stress model of BPD15 etiology may continue to be more fully developed to include those occurring in the context of peer relations.16 They also underscore the importance of identifying children at risk for or currently experiencing high levels of peer victimization for potential prevention services or mental health intervention.
Limitations
Several limitations of our study should be considered when interpreting our results. We were unable to control for early family or interpersonal variables (for example, physical maltreatment) as these types of data were not available in the McMaster Teen Study. Biological and genetic markers were also not available in this study. Evidence that adult BPD is highly heritable,53 suggests that genetic factors play an important role in the etiology of BP features. Finally, shared method variance may in part account for unique child report (but not parent report) predictive effects on elevated or rising BP features trajectory group membership. Despite these limitations, a key strength of the study was the temporal precedence of predictor variable sets from BP features data.
Conclusions
Our findings provide important evidence to mental health practitioners to identify ports of entry for prevention and intervention strategies aimed at reducing the development of BP features in adolescence and young adulthood.23,54 It is important to point out, however, that this study, as with other studies of BP symptoms or features in childhood and adolescence,2,5,7,23,46,47,55 did not examine a clinical diagnosis of BPD and that absolute levels of BP features for people in the elevated or rising trajectory group were modest in degree. An important task for future work will be to examine whether elevated BP features in childhood and adolescence are predictive of later clinical BPD diagnoses.
Acknowledgments
We thank Heather Brittain, Amanda Krygsman, and Patricia McDougall for the help with the study.
Footnotes
Author Note: All authors were involved in all aspects of the study; authors contributed to the design and implementation and interpretation of the results. All authors contributed to the review, writing, and editing of the manuscript. The authors maintained control over the final contents of the manuscript and the decision to publish in The Canadian Journal of Psychiatry. Analyses were conducted by Dr Haltigan.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and (or) publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and (or) publication of this article: This study was supported by the Social Sciences and Humanities Research Council of Canada (833-2004-1019) and the Canadian Institutes for Health Research (201009MOP-232632-CHI-CECA-136591).
References
- 1. Cicchetti D, Crick NR. Precursors and diverse pathways to personality disorder in children and adolescents. Dev Psychopathol. 2009;21:683–685. [DOI] [PubMed] [Google Scholar]
- 2. Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: a short-term longitudinal study. Dev Psychopathol. 2005;17:1051–1070. [PubMed] [Google Scholar]
- 3. Lenzenweger MF, Cicchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Dev Psychopathol. 2005;17:893–898. [DOI] [PubMed] [Google Scholar]
- 4. American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 5th ed Washington (DC): APA; 2013. p. 645. [Google Scholar]
- 5. Zanarini MC, Frankenburg FR, Dubo ED, et al. Axis 1 comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155:1733–1739. [DOI] [PubMed] [Google Scholar]
- 6. Beauchaine TP, Klein DN, Crowell SE, et al. Multifinality in the development of personality disorders: a biology × sex × environment interaction model of antisocial and borderline traits. Dev Psychopathol. 2009;21:735–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Belsky DW, Caspi A, Arseneault L, et al. Etiological features of borderline personality related characteristics in a birth cohort of 12-year old children. Dev Psychopathol. 2012;24:251–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bernstein DP, Cohen P, Velez CN, et al. Prevalence and stability of the DSM-III-R personality-disorders in a community-based sample of adolescents. Am J Psychiatry. 1993;150:1237–1243. [DOI] [PubMed] [Google Scholar]
- 9. Trull TJ. Borderline personality features in nonclinical young adults: 1. Identification and validation. Psychol Assess. 1995;7:33–41. [Google Scholar]
- 10. Chabrol H, Montovany A, Chouicha K, et al. Frequency of borderline personality disorder in a sample of French high school students. Can J Psychiatry. 2001;46:847–849. [DOI] [PubMed] [Google Scholar]
- 11. Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: prognosis for functioning over 20 years. J Child Psychol Psychiatry. 2008;49:933–941. [DOI] [PubMed] [Google Scholar]
- 12. Lieb K, Zanarini MC, Schmahl C, et al. Borderline personality disorder. Lancet. 2004;364:453–461. [DOI] [PubMed] [Google Scholar]
- 13. Leichsenring F, Leibing E, Kruse J, et al. Borderline personality disorder. Lancet. 2011;377:74–84. [DOI] [PubMed] [Google Scholar]
- 14. Gratz KL, Tull MT, Reynolds EK, et al. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: the roles of affective dysfunction, disinhibition, and self-and emotion-regulation deficits. Dev Psychopathol. 2009;21:1263–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Linehan M. Cognitive-behavioral treatment of borderline personality disorders. New York (NY): Guilford Press; 1993. [Google Scholar]
- 16. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: elaborating and extending Linehan’s theory. Psychol Bull. 2009;135:495–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paris J. Childhood trauma as an etiological factor in personality disorders. J Pers Disord. 1997;11:34–49. [DOI] [PubMed] [Google Scholar]
- 18. Gunderson JG, Lyons-Ruth K. BPD’s interpersonal hypersensitivity phenotype: a gene-environment-developmental model. J Pers Disord. 2008;22:22–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lenzenweger MF, Castro DD. Predicting change in borderline personality: using neurobehavioral systems indicators within an individual growth curve framework. Dev Psychopathol. 2005;17:1207–1237. [DOI] [PubMed] [Google Scholar]
- 20. Chanen AM, Jackson HJ, McGorry PD, et al. Two-year stability of personality disorder in adolescent outpatients. J Pers Disord. 2004;18:526–541. [DOI] [PubMed] [Google Scholar]
- 21. Grilo CM, Becker DF, Edell WS, et al. Stability and change of DSM-III-R personality disorder dimensions in adolescents followed up 2 years after psychiatric hospitalization. Compr Psychiatry. 2001;42:364–368. [DOI] [PubMed] [Google Scholar]
- 22. Nagin DS. Group-based modeling of development. Cambridge (MA): Harvard University Press; 2005. [Google Scholar]
- 23. Underwood MK, Beron KJ, Rosen LH. Joint trajectories for social and physical aggression as predictors of adolescent maladjustment: internalizing symptoms, rule-breaking behaviors, and borderline and narcissistic personality features. Comprehensive Psychiatry. 2011;23:659–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vaillancourt T, Brittain HL, McDougall P, et al. Longitudinal links between childhood peer victimization, internalizing and externalizing problems, and academic functioning: developmental cascades. J Abnorm Child Psychol. 2013;41:1203–1215. [DOI] [PubMed] [Google Scholar]
- 25. Sharp C, Mosko O, Chang B, et al. The cross-informant concordance and concurrent validity of the Borderline Personality Features Scale for Children in a community sample of boys. Clin Child Psychol Psychiatry. 2011;16:335–349 [DOI] [PubMed] [Google Scholar]
- 26. Chang B, Sharp C, Ha C. The criterion validity of the Borderline Personality Features Scale for Children in an adolescent inpatient setting. J Pers Disord. 2011;25:492–503. [DOI] [PubMed] [Google Scholar]
- 27. Olweus D. The revised Olweus Bully/Victim Questionnaire. Bergen (NO): Research Center for Health Promotion (HEMIL Center), University of Bergen; 1996. [Google Scholar]
- 28. Vaillancourt T, Trinh V, McDougall P, et al. Optimizing population screening of bullying in school-aged children. J Sch Violence. 2010;9:233–250. [Google Scholar]
- 29. Little T, Henrich C, Jones S, et al. Disentangling the “whys” from the “whats” of aggressive behaviour. Int J Behav Dev. 2003;27(2):122–133. [Google Scholar]
- 30. Cunningham CE, Pettingill P, Boyle M. The Brief Child and Family Phone Interview (BCFPI). Hamilton (ON): Canadian Centre for the study of Children at Risk, Hamilton Health Sciences Corporation, McMaster University; 2000. [Google Scholar]
- 31. Reynolds CR, Kamphaus RW. Behavior assessment system for children–2nd edition manual. Minneapolis (MN): Pearson; 2004. [Google Scholar]
- 32. Ellis LK, Rothbart MK. Revision of the Early Adolescent Temperament Questionnaire. Poster presented at the 2001 Biennial Meeting of the Society for Research in Child Development; 2001; Minneapolis (MN). [Google Scholar]
- 33. Education Quality Accountability Office (EQAO). EQAO’s Executive Summary of the Technical Report for the 2008–2009 Assessments of Reading, Writing and Mathematics, Primary Division, (Grades 1–3) and Junior Division (Grades 4–6), Grade 9 Assessment of Mathematics, and Ontario Secondary School Literacy Test; 2010 Toronto (ON): EQAO; 2011. [Google Scholar]
- 34. Muthén K, Muthén BO. Mplus user’s guide. 7th ed Los Angeles (CA): Múthen & Múthen; 1998. –2012. [Google Scholar]
- 35. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. 1995;57:289–300. [Google Scholar]
- 36. Cohen J. A power primer. Psychol Bull. 1992;112:155–159. [DOI] [PubMed] [Google Scholar]
- 37. Sansone RA, Sansone LA. Gender patterns in borderline personality disorder. Innov Clin Neurosci. 2011;8:16–20. [PMC free article] [PubMed] [Google Scholar]
- 38. Swartz M, Blazer D, George L, et al. Estimating the prevalence of borderline personality disorder in the community. J Pers Disord. 1990;4:257–272. [Google Scholar]
- 39. Rothman KJ, Greenland S, Walker AM. Concepts of interaction. Am J Epidemiol. 1980;112:467–470. [DOI] [PubMed] [Google Scholar]
- 40. Botto L, Khoury M. Commentary: Facing the challenge of gene-environment interaction: the two-by-four table and beyond. Am J Epidemiol. 2001;153:1016–1020. [DOI] [PubMed] [Google Scholar]
- 41. Andersson T, Alfredsson L, Källberg H, et al. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20:575–579. [DOI] [PubMed] [Google Scholar]
- 42. Knol MJ, van der Tweel I, Grobbee DE, et al. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int J Epidemiol. 2007;36:1111–1118. [DOI] [PubMed] [Google Scholar]
- 43. De Moor MH, Distel MA, Trull TJ, et al. Assessment of borderline personality features in population samples: is the Personality Assessment Inventory-Borderline Personality Features Scare measurement invariant across sex and age? Psychol Assess. 2009;21:125–130. [DOI] [PubMed] [Google Scholar]
- 44. Zanarini MC, Horwood J, Wolke D, et al. Prevalence of DSM-IV borderline personality disorder in two community samples: 6,330 English 11-year-olds and 34,653 American adults. J Pers Disord. 2011;25:607–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sharp C, Michonski J, Steinberg L, et al. An investigation of differential item functioning across gender of BPD criteria. J Abnorm Psychol. 2014;123:231–236. [DOI] [PubMed] [Google Scholar]
- 46. Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiological Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:533–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. J Abnorm Child Psychol. 2012;40:35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stepp SD, Burke JD, Hipwell AE, et al. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality symptoms in adolescent girls. J Abnorm Child Psychol. 2012;40:7–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hinshaw SP, Owens EB, Zalecki C, et al. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self-injury. J Consult Clin Psychol. 2012;80:1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Peluso MAM, Hatch JP, Glahn DC, et al. Trait impulsivity in patients with mood disorders. J Affect Disord. 2007;100(1–3):227–231. [DOI] [PubMed] [Google Scholar]
- 51. Zanarini MC, Franekburg FR. Pathways to the development of borderline personality disorder. J Pers Disord. 1997;11:3–104. [DOI] [PubMed] [Google Scholar]
- 52. Ostrov JM, Houston RJ. The utility of forms and functions of aggression in emerging adulthood: association with personality disorder symptomatology. J Youth Adolesc. 2008;37:1147–1158. [Google Scholar]
- 53. Bornovalova MA, Hicks BM, Iacono WG, et al. Stability, change, and heritability of borderline personality traits from adolescence to adulthood: a longitudinal twin study. Dev Psychopathol. 2009;21:1335–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Dev Psychopathol. 2009;21:1311–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Vaillancourt T, Brittain HL, McDougall P, et al. Predicting borderline personality disorder symptoms in adolescents from childhood physical and relational aggression, depression, and ADHD. Dev Psychopathol. 2014;26:817–830. [DOI] [PubMed] [Google Scholar]