Abstract
Objectives. We evaluated use of the Index of Concentration at the Extremes (ICE) for public health monitoring.
Methods. We used New York City data centered around 2010 to assess cross-sectional associations at the census tract and community district levels, for (1) diverse ICE measures plus the US poverty rate, with (2) infant mortality, premature mortality (before age 65 years), and diabetes mortality.
Results. Point estimates for rate ratios were consistently greatest for the novel ICE that jointly measured extreme concentrations of income and race/ethnicity. For example, the census tract–level rate ratio for infant mortality comparing the bottom versus top quintile for an ICE contrasting low-income Black versus high-income White equaled 2.93 (95% confidence interval [CI] = 2.11, 4.09), but was 2.19 (95% CI = 1.59, 3.02) for low versus high income, 2.77 (95% CI = 2.02, 3.81) for Black versus White, and 1.56 (95% CI = 1.19, 2.04) for census tracts with greater than or equal to 30% versus less than 10% below poverty.
Conclusions. The ICE may be a useful metric for public health monitoring, as it simultaneously captures extremes of privilege and deprivation and can jointly measure economic and racial/ethnic segregation.
Public health monitoring data need to be informative about not only health outcomes, but also their societal distribution and determinants, so that the data can be useful for policies, programs, and advocacy focused on improving population health and advancing health equity.1–3 Both the global and US literature increasingly recognize the importance of assessing progress and setbacks in reducing health inequities (i.e., unfair, unnecessary, and preventable health differences between the groups at issue).1–11 Adding to the urgency of using measures that illuminate inequitable health gaps is growing concern about 21st-century rising concentrations of income and wealth12–19 and their implications for public health and health inequities.12,20,21
Most public health monitoring systems, however, do not employ metrics that convey societal distributions of concentrations of privilege and deprivation.1,2 Instead, the typical practice is to present health data in relation to characteristics measured at the individual or household level, such as income, educational level, and also, chiefly in the United States, race/ethnicity. Health outcomes are then compared across groups defined in relation to the chosen characteristics, which may be modeled either continuously or categorically.1–3,22–24
Some analyses additionally employ variants of these measures aggregated to the neighborhood level (e.g., percentage of persons or households below poverty, percentage of persons with less than a high-school education, percentage of persons who are Black).22–24 In either case, although gaps in health outcomes can be quantified by comparing groups with less versus more resources, distributional information on the extent to which the population is divided into the groups at issue is not part of the metric. The excess risk of societal groups that get the proverbial short end of the stick becomes the focus, and these groups effectively become characterized as the “problem”; by contrast, the societal groups holding the stick’s other, longer end simply stand as a referent group, and the problematic economic, political, and social relationships that produce health inequities are hidden from view.11,12,25,26
A troubling feature of our era, however, is not a property of individuals or households but instead pertains to increasing spatial social polarization, part and parcel of growing concentrations of extreme income and wealth.12–21,26,27 Memorably capturing this phenomenon is the title of Charles Dickens’ classic novel A Tale of Two Cities.28,29 This novel, set amid the French Revolution of 1789 and its aftermath, vividly depicted the social and spatial relationships between vicious aristocrats and vengeful plebian citizens. The stark economic differences between neighborhoods, and between who literally held which stick, to beat or to protect whom, are a key theme of the book.
We accordingly designed our study to assess the utility, for public health monitoring, of using a measure of spatial social polarization: the Index of Concentration at the Extremes (ICE).30 Introduced into the social science literature in 2001 by Douglas Massey, a leading researcher on residential segregation,13,14,31 the ICE has been used primarily in the social sciences,32–34 as well as in a handful of etiological public health investigations.35–45 To our knowledge, however, the ICE has not been used by any health department or agency with the responsibility of monitoring population health.
The ICE is designed to reveal the extent to which an area’s residents are concentrated into groups at the extremes of deprivation and privilege: a value of −1 means that 100% of the population is concentrated in the most deprived group and a value of 1 means that 100% of the population is concentrated into the most privileged group; the formula is provided in the Methods section.30 We chose to employ the ICE over 2 of the most commonly used population measures of economic and social inequality—the Gini coefficient (for income inequality)46,47 and the Index of Dissimilarity (for residential racial segregation)46,48–50—because these latter measures, unlike the ICE, fail to be informative at the neighborhood level, precisely because of spatial social polarization.3,30 For example, neighborhoods whose residents are either 100% low-income or 100% high-income have the same Gini coefficient (given perfect equality of income level within the neighborhood), and neighborhoods whose subunits (e.g., block groups) are either 100% White or 100% Black have the same Index of Dissimilarity for White–Black segregation (because everyone belongs to only 1 of the 2 groups at issue); by contrast, the ICE would appropriately assign these very different types of areas the values, respectively, of −1 and 1. Thus, a valuable feature of the ICE is that it can provide, at a glance, the directional tendency toward an extreme.
To date, the ICE within the social science literature has been computed solely in relation to economic measures (e.g., income, education),30,32–34 as is also true for 9 of the 11 published public health studies that have used the ICE.35–43 Recognizing the importance of the entangled realities of socioeconomic and racial/ethnic inequities in the United States,3,11,22,23,26,29–31 2 small public health studies, however, used a novel ICE measure pertaining to concentrations of low-income Black persons versus high-income White persons,44,45 which are the 2 groups who, in Massey’s words, “continue to occupy opposite ends of the socioeconomic spectrum” in the United States.51(p324)
To determine whether ICE measures might be useful for monitoring population health, we examined health outcomes in relation to 2 sets of comparisons. The first comparison examined use of the ICE measures computed for (1) city neighborhoods (i.e., relatively large political units relevant to health department planning and resource allocation) and (2) census tracts (relatively smaller US Census administrative units52). The second set of comparisons, carried out at each level of geography, pertained to use of different ICE measures (i.e., ICE measures employing solely income data, solely racial/ethnic data, and also jointly integrating the socioeconomic and racial/ethnic data, in relation to each other), and also used the area-based poverty level.3,24 To conduct our study, we analyzed data for New York City, which is the largest city in the United States and one whose population of 8.5 million53 exceeds that of half the countries in the European Union.54 We focused our analyses on 3 important public health outcomes for which notable health inequities exist: infant mortality, diabetes mortality (all ages), and premature mortality (all cause).22–24,55–57
METHODS
In our cross-sectional population-based study of the population of New York City, we used data centered around 2010 and employed 2 levels of geography. The larger political unit, termed the community district (CD), is a unit of geography defined by New York City community boards, and has an average population size of 144 000 residents. The smaller administrative unit, the census tract (CT), is a unit of census geography that optimally contains 4000 persons.52 In 2010, New York City encompassed 59 CDs and 2126 CTs.
Health Outcomes
We obtained all health and population data from the New York City Department of Health and Mental Hygiene (DOHMH). The infant mortality rate equaled the number of infant deaths (< 1 year) divided by the number of live births within the given geographic unit within a specified calendar year, and was expressed as deaths per 1000 live births. We computed rates (per 100 000) for premature mortality (all-cause, for persons younger than 65 years) and diabetes mortality (all ages; International Classification of Diseases, 10th Revision, codes E10–E1458) by using 3-year and 5-year age-group bands, respectively, and age-standardized them to the year-2000 standard million.59 Analyses at the CT level employed 2010 vital statistics data, to correspond to 2010 CT boundaries. Analyses at the CD level, whose boundaries remained unchanged before and after the 2010 Census, employed 5-year average annual health data for 2008 through 2012. Virtually all of the vital statistics records could be geocoded to the CT and CD levels (range of percentage missing: 0% for CD birth outcomes to 0.32% for CT mortality outcomes), with geocoding conducted with Geosupport Desktop Editor version 15B (New York City Department of City Planning, New York, NY).
Index of Concentration at the Extremes Measures and Poverty Level
We employed the US Census American Community Survey (ACS) to compute the CT- and CD-level ICE measures and poverty rates, using each variable’s 2008 to 2012 average annual value.60 We used the ACS 5-year annual average values because there are no public-use single-year CT-level ACS estimates available, and such estimates can both be imprecise and vary widely across years (because of both changing sampling frames and sample sizes).61
We computed the ICE by using the following formula30:
where, say, in the case of the ICE for income, Ai is equal to the number of affluent persons in neighborhood i (e.g., in the 80th income percentile), Pi is equal to the number of poor persons in neighborhood i (e.g., in the 20th income percentile), and Ti is equal to the total population with known income level in neighborhood i. Mathematically, the ICE is thus a single metric that simultaneously quantifies concentrated extremes of both privilege and deprivation, whereby a value of 1 connotes that all residents are in the privileged group and a value of −1 denotes that all residents are in the most deprived group.
One valuable property of the ICE is that it avoids well-known problems of multicollinearity that occur when analyses try to employ, simultaneously, separate measures of neighborhood poverty and wealth, which typically are highly (and inversely) correlated,30,34 as would also be the case for models that jointly included measures of percentage White and percentage Black. In addition, in contrast to the Gini Index and Index of Dissimilarity, which, as noted previously, cannot be meaningfully used at lower levels of geography on account of spatial social segregation,3,30,34 the ICE can meaningfully be computed for both smaller and larger geographic units (e.g., block group, CT, CD, city, county).30,42,44,45
For each geographic unit (CD and CT), we generated 3 different ICE measures, for (1) income, (2) race/ethnicity, and (3) race/ethnicity plus income, as defined in the next paragraph.44,45 For these analyses, we conceptualized race/ethnicity as a social construct arising from inequitable race relations that historically have been linked to, but are not identical to, inequitable social class relations.11,26,62,63
The ICE for income set as the extremes the ACS household income categories that most closely approximated cutpoints for the US 20th and 80th household income percentiles (as typically used in analyses of income inequality24,46,47), which for this time period were less than $25 000 and greater than or equal to $100 000.64 The ICE for race/ethnicity set as the extreme groups persons who self-identified as non-Hispanic White versus non-Hispanic Black.44,45 For the ICE for income and race/ethnicity combined, the extreme groups were non-Hispanic White persons whose household income was greater than or equal to the 80th income percentile (most privileged) versus non-Hispanic Black persons in households below the 20th income percentile (least privileged).44,45
We additionally obtained ACS data on the percentage of the population categorized as being poor, by using the US Census definition of poverty.65–67 The US poverty threshold was first devised in the mid-1960s in relation to the cost of what was termed an “economy food plan,” which took into account the number and age of persons supported by the household income; it subsequently has been adjusted annually for inflation.65–67 We used area-based poverty categories validated for New York City by the New York City DOHMH.68
Statistical Analyses
To provide context for the study results, we first computed the 2010 5-year average annual rate (2008–2012) for the health outcomes among the total New York City population. We next tabulated and mapped the distribution of the ICE measures and poverty level at the CT and CD levels, and also quantified their correlations. Using Poisson regression, we then computed and compared the age-standardized rates for the health outcomes for strata defined by quintiles of the ICE measures and by poverty category.
For a global test of significance (P < .05), we computed the difference of the log likelihood of the base model (only age) versus a model that additionally included the ICE measure or poverty measure. For a test of linear trend, we used the P value for the regression coefficient for the ICE or poverty measure. We conducted data analyses with SAS version 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
In 2010, the New York City average annual rates (2008–2012) for infant mortality equaled 4.73 infants per 1000 live births (95% confidence interval [CI] = 4.55, 4.91), and the age-standardized rate per 100 000 persons for premature mortality (aged < 65 years) equaled 181.77 (95% CI = 180.42, 183.12) and for diabetes mortality (all ages), it equaled 19.59 (95% CI = 19.17, 20.02).
With regard to the distribution of the ICE and poverty measures (Table A, available as a supplement to the online version of this article at http://www.ajph.org), at the CT level, for each ICE measure, the values ranged from −1 to 1 and the poverty rate ranged from 0% to 100%. At the CD level, the range of values was narrower: the ICE values spanned, for income, from -0.527 to 0.490, for race/ethnicity (Black vs White) from −0.868 to 0.830, and for race/ethnicity and income (low-income Black vs high-income White) from −0.378 to 0.444, and the poverty rate ranged from 5.4% to 45.1% (Table A). At both the CT and CD levels, the median value for the ICE for income was slightly below 0 (–0.026 and –0.067, respectively), indicating the preponderance of areas leaning toward deprivation. By contrast, the CT and CD values for the ICE including race/ethnicity exceeded 0 (for race/ethnicity alone: 0.113 and 0.106, respectively; for race/ethnicity plus income: 0.033 and 0.042, respectively), reflecting the greater preponderance of neighborhoods with higher concentrations of White persons (Table A), as shown also by the maps (Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
Pearson correlation coefficients were high (absolute value > 0.75; P < .001) at both the CT and CD levels for pairwise relationships for 3 variables: the ICE for income, the ICE for income and race/ethnicity, and the poverty level (Table A). By contrast, for the ICE for race/ethnicity, the Pearson correlation coefficients were lower with both the ICE for income and the poverty level (absolute value = 0.3–0.6; P < .001; Table A). Additional analyses empirically demonstrated that for CTs with an ICE value equal to 0 (< 1% of all CTs in New York State) or close to 0, these values were attributable to no or relatively few persons in the extreme categories, as opposed to resulting from the entire population being divided evenly between persons in the 2 extreme categories (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
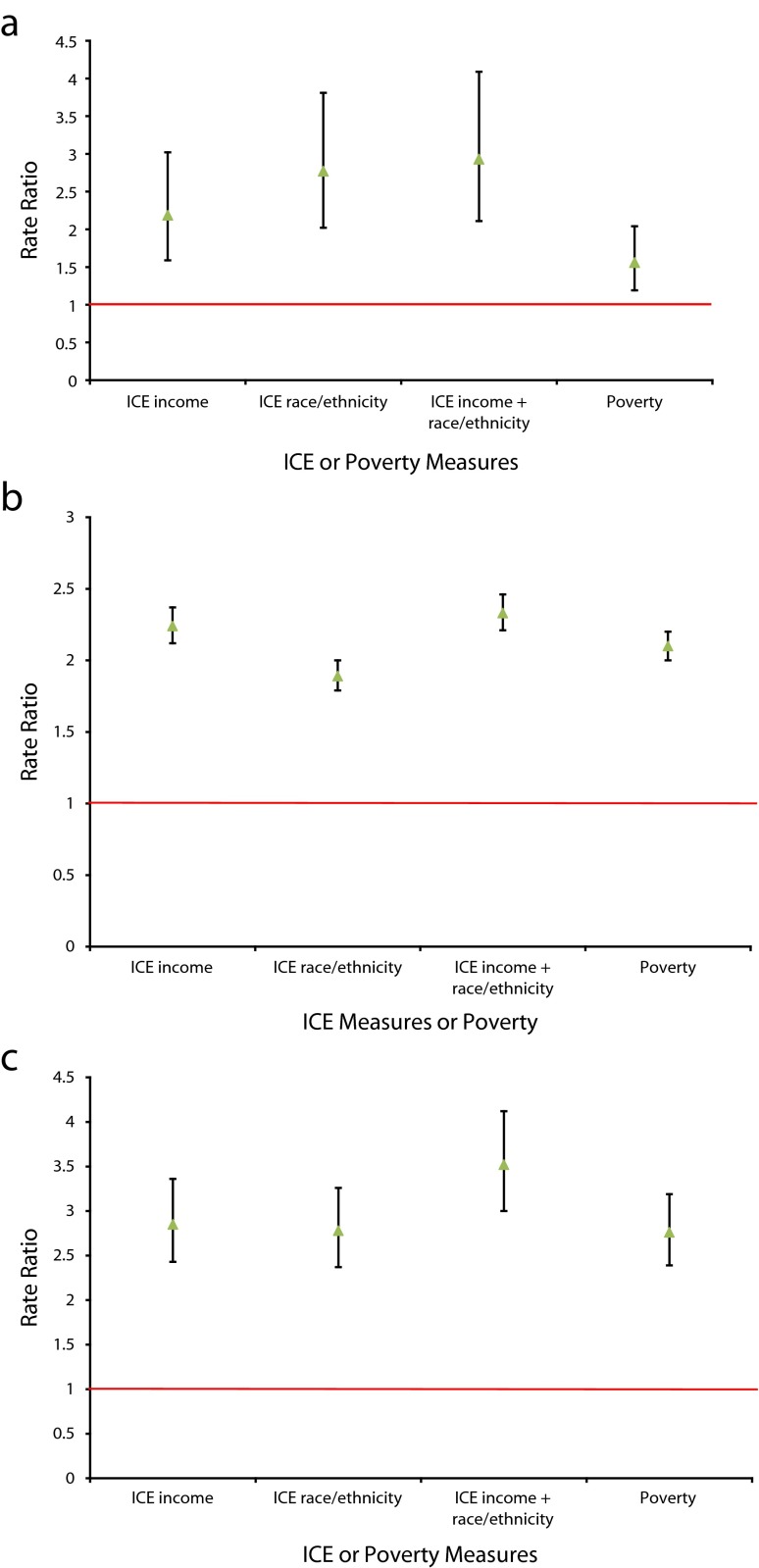
Infant mortality was significantly associated, at both the CT and CD level, with all 3 ICE measures and also the poverty level; in all models, the global test and test for trend had P values less than .005 (Table 1, and Tables C and D, available as supplements to the online version of this article at http://www.ajph.org, respectively). At the CT level (Table 1; Figure 1), the rate ratios (RRs) comparing the bottom versus top quintile for the ICE measures were highest for the ICE that jointly combined data on race/ethnicity and income (RR = 2.93; 95% CI = 2.11, 4.09) and for race/ethnicity only (RR = 2.77; 95% CI = 2.02, 3.81), followed by the ICE for income only (RR = 2.19; 95% CI = 1.59, 3.02); for the poverty measure, the RR for CTs with greater than or equal to 30% versus less than 10% of persons below poverty equaled 1.56 (95% CI = 1.19, 2.04). At the CD level (Table D), the corresponding RRs for the ICE for race/ethnicity and for race/ethnicity plus income were similarly high (respectively, 2.66; 95% CI = 2.33, 3.05; and 2.57; 95% CI = 2.21, 2.99) and higher than the RR observed for the ICE for income only (2.19; 95% CI = 1.89, 2.53) and for poverty (1.99; 95% CI = 1.70, 2.32).
TABLE 1—
Infant Mortality: New York City 2010 Rates and Rate Ratios at the Census Tract Level in Relation to the Index of Concentration at the Extremes and the Poverty Level
| ICE Incomeb |
ICE Race/Ethnicityc |
ICE Income + Race/Ethnicityd |
Poverty (4 Levels) |
||||||
| ICE Quintilea | Ratee | RR (95% CI) | Ratee | RR (95% CI) | Ratee | RR (95% CI) | Poverty Level, % |
Ratee | RR (95% CI) |
| Q1 (low) | 5.5 | 2.19 (1.59, 3.02) | 6.6 | 2.77 (2.02, 3.81) | 6.7 | 2.93 (2.11, 4.09) | ≥ 30 | 5.0 | 1.56 (1.19, 2.04) |
| Q2 | 4.3 | 1.71 (1.22, 2.41) | 6.0 | 2.51 (1.85, 3.41) | 5.4 | 2.36 (1.67, 3.31) | 20–29 | 5.4 | 1.69 (1.28, 2.22) |
| Q3 | 4.6 | 1.82 (1.27, 2.59) | 4.3 | 1.81 (1.31, 2.51) | 4.5 | 1.97 (1.39, 2.79) | 10–19 | 4.3 | 1.34 (1.01, 1.78) |
| Q4 | 4.5 | 1.79 (1.23, 2.60) | 2.6 | 1.10 (0.74, 1.62) | 2.5 | 1.11 (0.74, 1.68) | 0–9 | 3.2 | 1 (Ref) |
| Q5 (high) | 2.5 | 1 (Ref) | 2.4 | 1 (Ref) | 2.3 | 1 (Ref) | . . . | . . . | . . . |
Note. CI = confidence interval; ICE = Index of Concentration at the Extremes; RR = rate ratio. The ICE and poverty values are from Census Bureau American Community Survey 2008–2012 5-year file.60 The sample size was n = 2126 census tracts.
ICE quintile cutpoints (–1 = extreme concentration of deprivation; 1 = extreme concentration of privilege). ICE for income (low vs high): Q1: −1.00 to < −0.27; Q2: −0.27 to < −0.10; Q3: −0.10 to < 0.05; Q4: 0.05 to < 0.23; Q5: 0.23 to 1.00. ICE for race/ethnicity (non-Hispanic Black vs non-Hispanic White): Q1: −1.00 to < −0.47; Q2: −0.47 to < −0.04; Q3: −0.04 to < 0.34; Q4: 0.34 to < 0.65; Q5: 0.65 to 1.00. ICE for income + race/ethnicity (low-income non-Hispanic Black vs high-income non-Hispanic White): Q1: −1.00 to < −0.15; Q2: −0.15 to < −0.02; Q3: −0.02 to < 0.09; Q4: 0.09 to < 0.24; Q5: 0.24 to 1.00.
Low vs high.
Non-Hispanic Black vs non-Hispanic White.
Low-income non-Hispanic Black vs high-income non-Hispanic White.
The infant mortality rate equaled the number of infant deaths (< 1 year) divided by the number of live births within the given geographic unit within a specified calendar year, and was expressed as deaths per 1000 live births.
FIGURE 1—
Rate Ratio for Census Tract Level Deprivation (Q1) vs Privilege (Q5) for (a) Infant Mortality, (b) Premature Mortality, and (c) Diabetes Mortality: Index of Concentration at the Extremes and Poverty Level, New York City, 2010
Note. ICE = Index of Concentration at the Extremes. The ICE and poverty values are from Census Bureau American Community Survey 2008–2012 5-year file.60
For premature mortality, however, at both the CT and CD levels, the largest (and equally high) RR observed were for the 2 ICE measures that included income and also the poverty measure (RRs on the order of 2.4, with 95% CIs excluding 1), whereas the RR for the ICE for race/ethnicity was lower (1.9 for CTs, 1.8 for CDs, in both cases with the 95% CIs excluding 1; Table 2, Figure 1, and Tables C and D). For diabetes mortality, the RRs at both the CT and CD levels were highest for the ICE measure for income plus race/ethnicity (RR = 3.52; 95% CI 3.00, 4.12; and RR = 3.79; 95% CI = 3.50, 4.11, respectively); the corresponding RRs for the poverty level (≥ 30% vs < 10% below poverty) were 2.76 (95% CI = 2.39, 3.19) at the CT level and 3.49 (95% CI = 3.20, 3.80) at the CD level (Table 3, Figure 1, and Tables C and D).
TABLE 2—
Premature Mortality: New York City 2010 Rates and Rate Ratios at the Census Tract Level in Relation to the Index of Concentration at the Extremes and the Poverty Level
| ICE Incomeb |
ICE Race/Ethnicityc |
ICE Income+Race/Ethnicityd |
Poverty (4 Levels) |
||||||
| ICE Quintilea | Rate | RR (95% CI) | Rate | RR (95% CI) | Rate | RR (95% CI) | Poverty Level, % | Rate | RR (95% CI) |
| Q1 (low) | 267.8 | 2.24 (2.12, 2.37) | 239.2 | 1.89 (1.79, 2.00) | 281.9 | 2.33 (2.21, 2.46) | ≥ 30 | 272.3 | 2.10 (2.00, 2.20) |
| Q2 | 188.1 | 1.58 (1.49, 1.67) | 250.4 | 1.98 (1.87, 2.09) | 203.6 | 1.68 (1.59, 1.78) | 20–29 | 195.6 | 1.51 (1.43, 1.58) |
| Q3 | 163.0 | 1.36 (1.28, 1.45) | 154.5 | 1.22 (1.15, 1.29) | 148.8 | 1.23 (1.16, 1.31) | 10–19 | 160.3 | 1.23 (1.17, 1.30) |
| Q4 | 150.4 | 1.26 (1.18, 1.34) | 137.2 | 1.08 (1.02, 1.15) | 148.0 | 1.22 (1.15, 1.30) | 0–9 | 130.0 | 1 (Ref) |
| Q5 (high) | 119.4 | 1 (Ref) | 126.7 | 1 (Ref) | 120.9 | 1 (Ref) | . . . | . . . | . . . |
Note. CI = confidence interval; ICE = Index of Concentration at the Extremes; RR = rate ratio. Premature mortality rate (deaths when aged < 65 years): per 100 000, age-standardized to the year-2000 standard million. The ICE and poverty values are from Census Bureau American Community Survey 2008–2012 5-year file.60 The sample size was n = 2126 census tracts.
ICE quintile cutpoints (–1 = extreme concentration of deprivation; 1 = extreme concentration of privilege). ICE for income (low vs high): Q1: −1.00 to < −0.27; Q2: −0.27 to < −0.10; Q3: −0.10 to < 0.05; Q4: 0.05 to < 0.23; Q5: 0.23 to 1.00. ICE for race/ethnicity (non-Hispanic Black vs non-Hispanic White): Q1: −1.00 to < −0.47; Q2: −0.47 to < −0.04; Q3: −0.04 to < 0.34; Q4: 0.34 to < 0.65; Q5: 0.65 to 1.00. ICE for income + race/ethnicity (low-income non-Hispanic Black vs high-income non-Hispanic White): Q1: −1.00 to < −0.15; Q2: −0.15 to < −0.02; Q3: −0.02 to < 0.09; Q4: 0.09 to < 0.24; Q5: 0.24 to 1.00.
Low vs high.
Non-Hispanic Black vs non-Hispanic White.
Low-income non-Hispanic Black vs high-income non-Hispanic White.
TABLE 3—
Diabetes Mortality: New York City 2010 Rates and Rate Ratios at the Census Tract Level in Relation to the Index of Concentration at the Extremes and the Poverty Level
| ICE Incomeb |
ICE Race/Ethnicityc |
ICE Income+Race/Ethnicityd |
Poverty (4 Levels) |
||||||
| ICE Quintilea | Rate | RR (95% CI) | Rate | RR (95% CI) | Rate | RR (95% CI) | Poverty Level, % | Rate | RR (95% CI) |
| Q1 (low) | 31.1 | 2.85 (2.43, 3.36) | 31.6 | 2.78 (2.37, 3.26) | 37.1 | 3.52 (3.00, 4.12) | ≥ 30 | 31.9 | 2.76 (2.39, 3.19) |
| Q2 | 22.8 | 2.09 (1.77, 2.48) | 30.6 | 2.69 (2.30, 3.16) | 24.0 | 2.28 (1.92, 2.70) | 20–29 | 23.3 | 2.01 (1.73, 2.34) |
| Q3 | 18.3 | 1.68 (1.40, 2.01) | 15.5 | 1.37 (1.15, 1.63) | 16.3 | 1.55 (1.29, 1.86) | 10–19 | 19.0 | 1.64 (1.42, 1.89) |
| Q4 | 15.1 | 1.39 (1.15, 1.68) | 14.8 | 1.31 (1.09, 1.56) | 14.5 | 1.37 (1.14, 1.65) | 0–9 | 11.6 | 1 (Ref) |
| Q5 (high) | 10.9 | 1 (Ref) | 11.4 | 1 (Ref) | 10.6 | 1 (Ref) | . . . | . . . | . . . |
Note. CI = confidence interval; ICE = Index of Concentration at the Extremes; RR = rate ratio. Diabetes mortality rate: per 100 000, age-standardized to the year-2000 standard million. The ICE and poverty values are from Census Bureau American Community Survey 2008–2012 5-year file.60 The sample size was n = 2126 census tracts.
ICE quintile cutpoints (–1 = extreme concentration of deprivation; 1 = extreme concentration of privilege). ICE for income (low vs high): Q1: −1.00 to < −0.27; Q2: −0.27 to < −0.10; Q3: −0.10 to < 0.05; Q4: 0.05 to < 0.23; Q5: 0.23 to 1.00. ICE for race/ethnicity (non-Hispanic Black vs non-Hispanic White): Q1: −1.00 to < −0.47; Q2: −0.47 to < −0.04; Q3: −0.04 to < 0.34; Q4: 0.34 to < 0.65; Q5: 0.65 to 1.00. ICE for income + race/ethnicity (low-income non-Hispanic Black vs high-income non-Hispanic White): Q1: −1.00 to < −0.15; Q2: −0.15 to < −0.02; Q3: −0.02 to < 0.09; Q4: 0.09 to <0.24; Q5: 0.24 to 1.00.
Low vs high.
Non-Hispanic Black vs non-Hispanic White.
Low-income non-Hispanic Black vs high-income non-Hispanic White.
DISCUSSION
A central finding of our study is that the ICE can usefully and feasibly be employed for public health monitoring, using a metric that reveals, in a single measure, the extremes of selected social and economic relationships implicated in producing health inequities.1–27,29–31,62,63,67 For all 3 outcomes—infant mortality, premature mortality (death before age 65 years; all-cause), and diabetes mortality (all ages)—the greatest RR consistently occurred for point estimates of the ICE that combined data on income and race/ethnicity (RR on the order of 2–4, comparing bottom to top quintile). These point estimates, moreover, typically exceeded those observed for the poverty contrast (≥ 30% vs < 10% poverty). For example, in the case of infant mortality at the CT level, the ICE for race/ethnicity and income was significantly higher than for the poverty contrast (respectively 2.93; 95% CI = 2.11, 4.09 vs 1.56; 95% CI = 1.19, 2.04).
It is unlikely that our results reflect biased estimates of the variables included in our models. The New York City DOHMH is the repository of death certificates and, by law, must receive reports of all deaths that occur in New York City. Moreover, any bias affecting classification of mortality as being attributable to diabetes would equally affect the analyses using the ICE measures and poverty level, and thus could not account for differences in their estimated magnitude of effects. Similarly, any biases affecting the data used to compute the ICE and poverty level (e.g., US Census population undercounts or overcounts69,70) would equally affect all analyses, and not explain observed differences in effect estimates, because all models employed the same US Census data to compute the different ICE measures and poverty level. Moreover, we addressed instability of ACS annual CT data by employing the 5-year annual average ACS data, and further improved stability of CT-level estimates by analyzing the CT (as well as CD) data by ICE quintiles.
One implication of our findings is that the ICE can provide a useful complement to the poverty level as a metric for monitoring population health.3,68,71,72 In contrast to the poverty measure, the ICE usefully brings into focus the full range of concentrations of privilege and deprivation; it also can capture spatial social polarization jointly involving both income and race/ethnicity. By contrast, a poverty rate of, say, 0%, or 10%, or 30%, is not informative about how high the income level is of the nonimpoverished population, and this measure must be cross-stratified by race/ethnicity to yield data on racial/ethnic distributions of poverty. The poverty measure nevertheless remains critically important because of its policy and programmatic relevance and also the health harms associated with impoverishment.3,22–24,65–68,71,72
Results of our analyses can usefully advance work to improve population health and reduce health inequities in 2 ways. First, the ICE can assist with framing the problem of health inequities as inequitable relationships between societal groups,25 as opposed to focusing solely on the “disadvantaged.”22–24 In addition, by calling attention to problems arising from the “hollowing out” of the middle,12–21,34 the ICE further points to the need for interventions that address how growing concentrations of wealth can simultaneously lead to growing concentrations of poverty12–21,34 and larger health inequities.20,21,29,35–45 The joint ICE for income and race/ethnicity is likewise key for capturing the joint impact of economic and racial/ethnic inequality and segregation,44,45 as opposed to the conventional approach of focusing on only one or the other.16,17,47–50,73,74
Second, the observed associations between the ICE and health outcomes invite further research on the causal pathways linking extreme concentrations of privilege and deprivation to both on-average health and the magnitude of health inequities. Extant research on the societal determination of health would suggest that likely pathways would include the impact of spatial social polarization on local education, economies, and environments, as well as spatial and economic access to health services.1–27,29–31,62,63,67 Because the ICE can be meaningfully employed for within-city areas (including CTs and CDs), in contrast to conventional measures of income inequality (e.g., the Gini46,47) and residential segregation (e.g., the Index of Dissimilarity46,48–50), it extends the scale for analyzing how spatial social polarization affects both population health and the magnitude of health inequities, and addresses the gap in the literature regarding the health impacts of within-city social spatial polarization.
We accordingly suggest that US health researchers and health agencies consider studying and employing the ICE, and especially the ICE that jointly assesses income and race/ethnicity. Standard health department reports on population health data, for example, could supplement analyses focused on poverty with analyses that use the ICE. Moreover, in jurisdictions where the combined ICE for income and race/ethnicity provides evidence of steeper gradients than observed with solely the poverty measure, this ICE should become a standard indicator to assess progress in advancing health equity. Only by accurately telling the “tale of two cities” can public health data spur analysis and action to create a better and less divided world in which no group experiences unfair, unnecessary, and preventable health inequities.
ACKNOWLEDGMENTS
We gratefully acknowledge, with written permission, Mary Huynh, PhD, and James Hadler, MD, MPH, both at the New York City Department of Health and Mental Hygiene, for their thoughtful advice regarding our project and article, and Jarvis T. Chen, ScD, at the Harvard T. H. Chan School of Public Health, for his methodological advice.
HUMAN PARTICIPANT PROTECTION
The project was exempt for the Harvard T. H. Chan School of Public Health investigators because they had no access to human participants data (IRB15-2304; approved June 25, 2015). The New York City Department of Health and Mental Hygiene institutional review board deemed this analysis to be exempt human participants research because of the use of de-identified data sets.
REFERENCES
- 1.World Health Organization. Monitoring health inequality: an essential step for achieving health equity—illustrations of fundamental concepts. 2014. Available at: http://apps.who.int/iris/bitstream/10665/164530/1/WHO_HIS_HSI_2015.1_eng.pdf?ua=1&ua=1. Accessed October 6, 2015.
- 2.Friedman DJ, Hunter EL, Parrish RG., II . Health Statistics: Shaping Policy and Practice to Improve the Population’s Health. New York, NY: Oxford University Press; 2005. [Google Scholar]
- 3.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95(2):312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitehead M. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1990. The concepts and principles of equity and health. Document EUR/ICP/RDP/414. Available at: http://salud.ciee.flacso.org.ar/flacso/optativas/equity_and_health.pdf. Accessed October 6, 2015. [Google Scholar]
- 5.World Health Organization. WHO glossary: “Health inequality and inequity.”. Available at: http://www.who.int/hia/about/glos/en/index1.html. Accessed October 6, 2015.
- 6.World Health Organization Commission on the Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. 2008. Available at: http://www.who.int/social_determinants/thecommission/finalreport/en/index.html. Accessed October 6, 2015.
- 7.US Centers for Disease Control and Prevention. CDC’s Healthy Communities Program: Attaining health equity. Available at: http://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/overview/healthequity.htm. Accessed October 6, 2015.
- 8.Braveman P, Gruskin S. Poverty, equity, human rights and health. Bull World Health Organ. 2003;81(7):539–545. [PMC free article] [PubMed] [Google Scholar]
- 9.Casas-Zamora JA, Ibrahim SA. Confronting health inequity: the global dimension. Am J Public Health. 2004;94(12):2055–2058. doi: 10.2105/ajph.94.12.2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawachi I, Subramanian SV, Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health. 2002;56(9):647–652. doi: 10.1136/jech.56.9.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krieger N. Defining and investigating social disparities in cancer: critical issues. Cancer Causes Control. 2005;16(1):5–14. doi: 10.1007/s10552-004-1251-5. [DOI] [PubMed] [Google Scholar]
- 12.Dorling D. Injustice: Why Social Inequality Still Persists. Rev ed. Bristol, UK: Policy Press; 2015. [Google Scholar]
- 13.Massey DS. The age of extremes: concentrated affluence and poverty in the twenty-first century. Demography. 1996;33(4):395–412. [PubMed] [Google Scholar]
- 14.Massey DS. Reflections on the dimensions of segregation. Soc Forces. 2012;91(1):39–43. doi: 10.1093/sf/sos118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harvey D. Spaces of Global Capitalism: Towards a Theory of Uneven Geographical Development. New York, NY: Verso; 2006. [Google Scholar]
- 16.Dwyer RE. Poverty, prosperity, and place: the shape of class segregation in the age of extremes. Soc Probl. 2010;57:114–137. [Google Scholar]
- 17.Walks A. From financialization to sociospatial polarization of the city? Evidence from Canada. Econ Geogr. 2013;90:33–66. [Google Scholar]
- 18.Stiglitz JE. The Great Divide: Unequal Societies and What We Can Do About Them. New York, NY: W. W. Norton; 2015. [Google Scholar]
- 19.Piketty T. Capital in the Twenty-First Century. Goldhammer A, trans. Cambridge, MA: Harvard University Press; 2014. [Google Scholar]
- 20.Leigh A, Jencks C, Smeeding TM. Health and economic inequality. In: Salverda W, Nolan B, Smeeding T, editors. The Oxford Handbook of Economic Inequality (Oxford Handbooks Online) New York, NY: Oxford University Press; 2011. [Google Scholar]
- 21.Truesdale BC, Jencks C. The health effects of income inequality: averages and disparities. Annu Rev Public Health. 2016 doi: 10.1146/annurev-publhealth-032315-021606. In press. [DOI] [PubMed] [Google Scholar]
- 22.Department of Health and Human Services. Healthy People 2020. Disparities. Available at: http://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities. Accessed October 6, 2015.
- 23.Centers for Disease Control and Prevention. CDC Health Disparities & Inequalities Report, 2013. MMWR Surveill Summ. 2013;62(suppl 3):1–187. [PubMed] [Google Scholar]
- 24.Catlin B, Jovaag A, Van Dijik Willems J. 2015 county health rankings key findings report. Robert Wood Johnson Foundation. 2015 Available at: http://www.countyhealthrankings.org/sites/default/files/resources/CHR%26R%202015%20Key%20Findings.pdf. Accessed October 6, 2015. [Google Scholar]
- 25.Krieger N, Alegría M, Almeida-Filho N et al. Who, and what, causes health inequities? Reflections on emerging debates from an exploratory Latin American/North American workshop. J Epidemiol Community Health. 2010;64(9):747–749. doi: 10.1136/jech.2009.106906. [DOI] [PubMed] [Google Scholar]
- 26.Grusky DB, editor. Social Stratification: Class, Race, and Gender in Sociological Perspective. 4th ed. Boulder, CO: Westview Press; 2014. [Google Scholar]
- 27.Bishaw A. Washington, DC: US Census Bureau; 2014. Changes in areas with concentrated poverty: 2000 to 2010. American Community Survey Reports (ACS-27). Available at: https://www.census.gov/content/dam/Census/library/publications/2014/acs/acs-27.pdf. Accessed October 6, 2015. [Google Scholar]
- 28.Dickens C. A Tale of Two Cities. London, England: Chapman & Hall; 1859. [Google Scholar]
- 29.Susser I. A tale of two cities. Anthropol Now. 2014;6(3):8–16. [Google Scholar]
- 30.Massey DS. The prodigal paradigm returns: ecology comes back to sociology. In: Booth A, Crouter A, editors. Does It Take a Village? Community Effects on Children, Adolescents, and Families. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. pp. 41–48. [Google Scholar]
- 31.Massey D, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 32.Casciano R, Massey DS. Neighborhoods, employment, and welfare use: assessing the influence of neighborhood socioeconomic composition. Soc Sci Res. 2008;37(2):544–558. doi: 10.1016/j.ssresearch.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kubrin CE, Stewart EA. Predicting who reoffends: the neglected role of neighborhood context in recidivism studies. Criminology. 2006;44:165–198. [Google Scholar]
- 34.Sampson RJ, Mare RD, Perkins KL. Achieving the middle ground in an age of concentrated extremes: mixed middle-income neighborhoods and emerging adulthood. Ann Am Acad Political Soc Sci. 2015;660(1):156–174. doi: 10.1177/0002716215576117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Do DP, Dubowitz T, Bird CE, Lurie N, Escarce JJ, Finch BK. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using the NHANES III survey (1988–1994) Econ Hum Biol. 2007;5(2):179–203. doi: 10.1016/j.ehb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carpiano RM, Lloyd JEV, Hertzman C. Concentrated affluence, concentrated disadvantage, and children’s readiness for school: a population-based, multi-level investigation. Soc Sci Med. 2009;69(3):420–432. doi: 10.1016/j.socscimed.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 37.Finch BK, Do DP, Heron M, Bird C, Seeman T, Lurie N. Neighborhood effects on health: concentrated advantage and disadvantage. Health Place. 2010;16(5):1058–1060. doi: 10.1016/j.healthplace.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ludwig J, Duncan GJ, Gennetian LA et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Casciano R, Massey DS. Neighborhood disorder and anxiety symptoms: new evidence from a quasi-experimental study. Health Place. 2012;18(2):180–190. doi: 10.1016/j.healthplace.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rudolph AE, Crawford ND, Latkin C, Fowler JH, Fuller CM. Individual and neighborhood correlates of membership in drug using networks with a higher prevalence of HIV in New York City (2006–2009) Ann Epidemiol. 2013;23(5):267–274. doi: 10.1016/j.annepidem.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eastwood JG, Jalaludin BB, Kemp LA, Phung HN, Barnett BEW. Immigrant maternal depression and social networks. A multilevel Bayesian spatial logistic regression in South Western Sydney, Australia. Spat Spatiotemporal Epidemiol. 2013;6:49–58. doi: 10.1016/j.sste.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 42.Kramer M. Some thoughts on measuring place and health. Oral presentation at Health Places Research Group, Georgia Institute of Technology; March 26, 2013. Available at: http://www.cqgrd.gatech.edu/sites/files/cqgrd/measuringneighborhoods_march2013.pdf. Accessed October 6, 2015.
- 43.Baglivio MT, Wolff KT, Epps N, Nelson R. Predicting adverse childhood experiences: the importance of neighborhood context in youth trauma among delinquent youth. Crime Delinq. 2015 Epub ahead of print. [Google Scholar]
- 44.Krieger N, Waterman PD, Gryparis A, Coull BA. Black carbon exposure, socioeconomic and racial/ethnic spatial polarization, and the Index of Concentration at the Extremes (ICE) Health Place. 2015;34:215–228. doi: 10.1016/j.healthplace.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feldman J, Waterman PD, Coull BA, Krieger N. Spatial social polarization: Using the Index of Concentration at the Extremes jointly for income and race/ethnicity to analyze risk of hypertension. J Epidemiol Community Health. 2015 doi: 10.1136/jech-2015-205728. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shaw M, Galobardes B, Lawlor DA, Lynch J, Wheeler B, Davey Smith G. The Handbook of Inequality and Socioeconomic Position: Concepts and Measures. Bristol, UK: The Policy Press; 2007. [Google Scholar]
- 47.Watson T. Inequality and the measurement of residential segregation by income in American neighborhoods. Rev Income Wealth. 2009;55(3):820–844. [Google Scholar]
- 48.Iceland J, Weinberg DH, Steinmetz E. Washington, DC: US Census Bureau; 2002. Racial and ethnic residential segregation in the United States: 1980–2000. Census 2000 special report. Available at: http://www.census.gov/prod/2002pubs/censr-3.pdf. Accessed October 6, 2015. [Google Scholar]
- 49.Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Massey DS, Brodmann S. Spheres of Influence: The Social Ecology of Racial and Class Inequality. New York, NY: Russell Sage Foundation; 2014. [Google Scholar]
- 52.US Census Bureau. Geographic terms and concepts—census tract. Available at: https://www.census.gov/geo/reference/gtc/gtc_ct.html. Accessed October 6, 2015.
- 53.New York City Department of Planning. Population: current population estimates. Available at: http://www.nyc.gov/html/dcp/html/census/popcur.shtml. Accessed October 6, 2015.
- 54.European Union. Living in the EU. Available at: http://europa.eu/about-eu/facts-figures/living/index_en.htm. Accessed October 6, 2015.
- 55.Rossen LM, Schoendorf KC. Trends in racial and ethnic disparities in infant mortality rates in the United States, 1989–2006. Am J Public Health. 2014;104(8):1549–1556. doi: 10.2105/AJPH.2013.301272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Betancourt JR, Duong JV, Bondaryk MR. Strategies to reduce diabetes disparities: an update. Curr Diab Rep. 2012;12(6):762–768. doi: 10.1007/s11892-012-0324-1. [DOI] [PubMed] [Google Scholar]
- 57.Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of US inequities in premature mortality: 1960–2002. PLoS Med. 2008;5(2):e46. doi: 10.1371/journal.pmed.0050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.US Centers for Disease Control and Prevention. International Classification of Diseases, Tenth Revision. Available at: http://www.cdc.gov/nchs/icd/icd10.htm. Accessed October 6, 2015.
- 59.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the Year 2000 standard. Natl Vital Stat Rep. 1998;47(3):1–16. 20. [PubMed] [Google Scholar]
- 60.US Census Bureau. American Community Survey, 2006–2010. 2014. Available at: http://www.census.gov/acs/www. Accessed October 6, 2015.
- 61.Spielman SE, Filch D, Nagle N. Patterns of causes of uncertainty in the American Community Survey. Appl Geogr. 2014;46:147–157. doi: 10.1016/j.apgeog.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Winant H. Race and race theory. Annu Rev Sociol. 2000;26:169–185. [Google Scholar]
- 63.Krieger N. Discrimination and health inequities. In: Berkman LF, Kawachi I, Glymour M, editors. Social Epidemiology. 2nd ed. New York, NY: Oxford University Press; 2014. pp. 63–125. [Google Scholar]
- 64.US Census Bureau. Historical income data: households. Table H-1. Income limits for each fifth and top 5 percent. All races. Available at: https://www.census.gov/hhes/www/income/data/historical/household. Accessed October 6, 2015.
- 65.US Census Bureau. How the US Census measures poverty. Available at: http://www.census.gov/hhes/www/poverty/about/overview/measure.html. Accessed October 6, 2015.
- 66.Fisher GM. The development and history of the poverty threshholds. Soc Secur Bull. 1992;55(4):3–14. [PubMed] [Google Scholar]
- 67.O’Connor A. Poverty Knowledge: Social Science, Social Policy, and the Poor in Twentieth-Century US History. Princeton, NJ: Princeton University Press; 2001. [Google Scholar]
- 68.Toprani A, Hadler JL. Selecting and applying a standard area-based socioeconomic status measure for public health data: analysis for New York City. New York City Department of Health and Mental Hygiene. Epi Research Report. 2013:1–11. Available at: http://www.nyc.gov/html/doh/downloads/pdf/epi/epiresearch-SES-measure.pdf. Accessed October 6, 2015. [Google Scholar]
- 69.US Census Bureau. DSSD 2010 Census coverage measurement memorandum series #2010-G-01. May 22, 2012. Available at: http://www.census.gov/coverage_measurement/pdfs/g01.pdf. Accessed October 6, 2015.
- 70.Hogan H, Cantwell PJ, Devine J, Mule VT, Jr, Velkoff V. Quality and the 2010 Census. Popul Res Policy Rev. 2013;32:637–662. [Google Scholar]
- 71.Krieger N, Waterman PD, Chen JT, Rehkopf DH, Subramanian SV. Boston, MA: Harvard School of Public Health; Geocoding and monitoring US socioeconomic inequalities in health: an introduction to using area-based socioeconomic measures—The Public Health Disparities Geocoding Project monograph. Available at: http://www.hsph.harvard.edu/thegeocodingproject. Accessed October 6, 2015. [Google Scholar]
- 72.Council of State and Territorial Epidemiologists. CSTE Pilot Project: Analyze public health data for health disparities by SES using census tract poverty level. Available at: http://www.cste.org/?CSTEPilotProject. Accessed October 6, 2015.
- 73.Smith CL. Economic deprivation and racial segregation: comparing Superfund sites in Portland, Oregon and Detroit, Michigan. Soc Sci Res. 2009;38(3):681–692. doi: 10.1016/j.ssresearch.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 74.White K, Haas J, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;47(3 pt 2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]