Abstract
In t(8;21)(q22;q22) acute myeloid leukemia, the prognostic value of early minimal residual disease assessed with real-time quantitative polymerase chain reaction is the most important prognostic factor, but how long-term minimal residual disease monitoring may contribute to drive individual patient decisions remains poorly investigated. In the multicenter CBF-2006 study, a prospective monitoring of peripheral blood and bone marrow samples was performed every 3 months and every year, respectively, for 2 years following intensive chemotherapy in 94 patients in first complete remission. A complete molecular remission was defined as a (RUNX1-RUNX1T1/ABL1)×100 ≤ 0.001%. After the completion of consolidation therapy, a bone marrow complete molecular remission was observed in 30% of the patients, but was not predictive of subsequent relapse. Indeed, 8 patients (9%) presented a positive bone marrow minimal residual disease for up to 2 years of follow-up while still remaining in complete remission. Conversely, a peripheral blood complete molecular remission was statistically associated with a lower risk of relapse whatever the time-point considered after the completion of consolidation therapy. During the 2-year follow-up, the persistence of peripheral blood complete molecular remission was associated with a lower risk of relapse (4-year cumulative incidence, 8.2%), while molecular relapse confirmed on a subsequent peripheral blood sample predicted hematological relapse (4-year cumulative incidence, 86.9%) within a median time interval of 3.9 months. In t(8;21)(q22;q22) acute myeloid leukemia, minimal residual disease monitoring on peripheral blood every 3 months allows for the prediction of hematological relapse, and to identify patients who could potentially benefit from intervention therapy.
Introduction
In young adult patients with core binding factor acute myeloid leukemia (CBF-AML, i.e. with t(8;21)(q22;q22) [CBFA-AML] or inv(16)(p13q22)/t(16;16)(p13;q22) [CBFB-AML]), complete remission (CR) is reached in more than 90% of cases. However, around 20–30% of patients will experience hematological relapse.1,2 In CBFA-AML, many disease-related factors have been correlated to the risk of relapse, including extramedullary disease,3 hyperleucocytosis,4 CD56 expression,5 additional cytogenetic aberrations6 and gene mutations such as KIT and FLT3-ITD.7,8 Quantification of the leukemia associated fusion gene RUNX1-RUNX1T1 (formerly AML1-ETO) by RQ-PCR provides a perfect target for minimal residual disease (MRD) assessment. In the French CBF-2006 study, we previously showed that early reduction in MRD level (>3 logs) during consolidation treatment in AML with t(8;21) was the most powerful marker to predict relapse in multivariable analysis.2
During longer term post-consolidation follow-up, retrospective studies reported that MRD detection was associated with an increased risk of relapse in these patients.9,10 However, several studies also observed that a bone marrow positive MRD could be detectable in patients with long-term persistent CR.1,10,11 Recently, the Medical Research Council (MRC) reported that MRD positivity at a rate of >500 RUNX1-RUNX1T1 copies in bone marrow (BM) and >100 copies in peripheral blood (PB) during follow-up was predictive of hematological relapse.1
We herein report the results of a prospective assessment of BM and PB MRD levels during the follow-up of 94 CBFA-AML patients enrolled in the French CBF-2006 study.
Methods
Patients and Treatment Protocol
The diagnosis of CBFA-AML was defined by the presence of either the t(8;21) translocation by karyotype and/or fluorescence in situ hybridization analysis and/or evidence of RUNX1-RUNX1T1 fusion transcript. Ninety-seven patients aged 18–60 years and with newly diagnosed CBA-AML were enrolled at 35 French centers between July 2007 and November 2010 in the CBF-2006 trial.
The CBF-2006 trial (EudraCT #2006-005163-26; ClinicalTrials.gov ID #NCT00428558) compared two intensive induction regimens in CBF leukemias.2 After induction, complete remission (CR) was obtained in 96 CBF-AML patients (1 early death). Patients received 3 monthly consolidation cycles with cytarabine at 3,000 mg/m2/12 h by 2-hour IV infusion on days 1, 3, and 5, followed by lenograstim granulocyte colony-stimulating factor starting at day 8 until neutrophil recovery.
The study was approved by the ethics committee of Nimes University Hospital and by the Institutional Review Board of the French Regulatory Agency and was conducted in accordance with the Declaration of Helsinki. All samples were collected as part of the treatment protocol. Clinicians were prospectively informed of the MRD results. According to the protocol, patients with molecular recurrence defined by an MRD ratio increase of more than 1-log on two successive samples were eligible to participate in the phase II clinical trial DasaCBF.12 Thus, 5 patients were preemptively treated with dasatinib 140mg once daily. All 5 patients rapidly presented a hematological relapse within a median of 1.8 months. Another patient was preemptively treated with high-dose chemotherapy (MIDAM; intermediate-dose cytarabine, mitoxantrone and gemtuzumab ozogamycin) after a molecular relapse confirmed on a subsequent sample without hematological relapse. This patient was censored at the time of an allogeneic transplant.
Samples and MRD evaluation
Bone marrow and PB samples were requested at diagnosis and then during therapy, after induction chemotherapy and before the second and third consolidation chemotherapy. Results of early MRD evaluation have already been published.2 At the end of treatment, MRD was again assessed on PB and BM. During post-consolidation follow-up, PB samples were monitored every 3 months for 2 years and BM samples annually for 2 years. Among the 96 CR patients, 2 patients had no MRD monitoring during follow-up. Long-term MRD level monitoring was thus analyzed in 94 patients (Figure 1).
Figure 1.
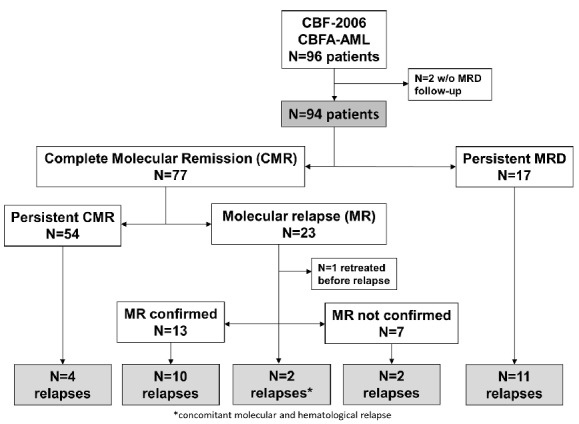
Patient flow chart.
MRD levels were monitored for RUNX1-RUNX1T1 transcript by RQ-PCR in 2 central laboratories (Angers, Lille), as previously described.13 Calibration curves were performed using Ipsogen plasmids (Ipsogen SA, Marseille, France) and ABL1 was amplified concomitantly as an internal reference. Results were expressed as a [RUNX1-RUNX1T1/ABL1] × 100 transcript ratio. The sensitivity of this quantification was 0.001%. A complete molecular response (CMR) was thus defined as a transcript ratio ≤0.001%, providing that at least 20 000 copies of the ABL1 control gene had been amplified. Molecular relapse was arbitrarily defined as a positive MRD occurring after having reached CMR.
Statistical analysis
The Spearman rank correlation coefficient and the Pearson correlation tests were used to calculate correlation between transcript ratio in BM and PB. The rate of PB-MRD increase was calculated in patients with an available PB-MRD at relapse as log10(PB-MRDR/PB-MRDbefR)/ΔT, where PB-MRDR is the MRD at relapse, PB-MRDbefR is the MRD on the prior PB sample before relapse, and ΔT is the time between both assessments. The outcomes were updated as of August 2013, with a median follow-up of 44.7 months.
Overall survival (OS) was estimated by the Kaplan-Meier method and compared by the log-rank test. Cumulative incidence of relapse (CIR) was estimated taking into account death in first CR for competing risk and compared by cause-specific hazards Cox models. Patients were censored at allogeneic stem cell transplant in first complete remission. Specific hazards of relapse (SHRs) and HRs are given with 95% confidence interval (CI). To evaluate the impact of time to CMR or time to molecular relapse, outcome data were estimated by the Mantel-Byar method, considering CMR or molecular relapse as a time-dependent covariate. This method, described by Simon and Makuch, was applied for an appropriate graphical representation of CMR and molecular relapse impact on OS and CIR.14,15 All statistical tests were performed with the Stata/IC 12.1 software (StataCorp, College Station, TX, USA).
Results
A total of 479 BM samples and 800 PB samples were collected, corresponding respectively to 71.3% and 64.1% of the samples planned by the protocol. Seventy-four BM samples and 74 PB samples were assessed at the end of treatment time-point (after the third consolidation cycle), and 78 BM samples and 399 PB samples during longer follow-up. During the 2 years of follow-up, a median number of 5 PB samples per patient (range 0–9) were collected. Seventy-nine BM and 79 PB samples not planned by the protocol, corresponding to control of previous MRD results or relapse time-points, were also included in the analysis.
Correlation between MRD results obtained on BM and PB
To evaluate the correlation between PB- and BM-MRD levels, 525 paired PB and BM samples were compared at diagnosis, after induction, before each consolidation course, at the end of treatment and during the follow-up. Analyses were restricted to paired samples with comparable ABL Ct values. With a threshold of 0.001%, a positive MRD was detected on BM but not on PB in 134 paired samples (25.5%). Conversely, only 8 (1.5%) of the paired samples presented a detectable MRD on PB but not on BM (Figure 2).
Figure 2.
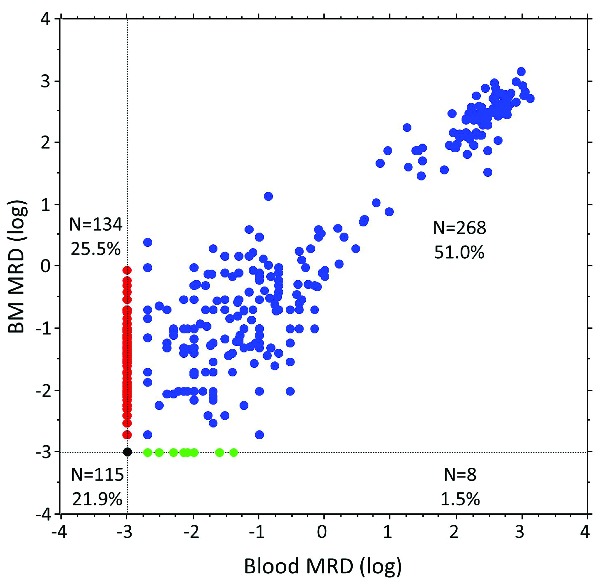
Peripheral blood (PB) and (BM) bone marrow MRD in 525 paired samples.
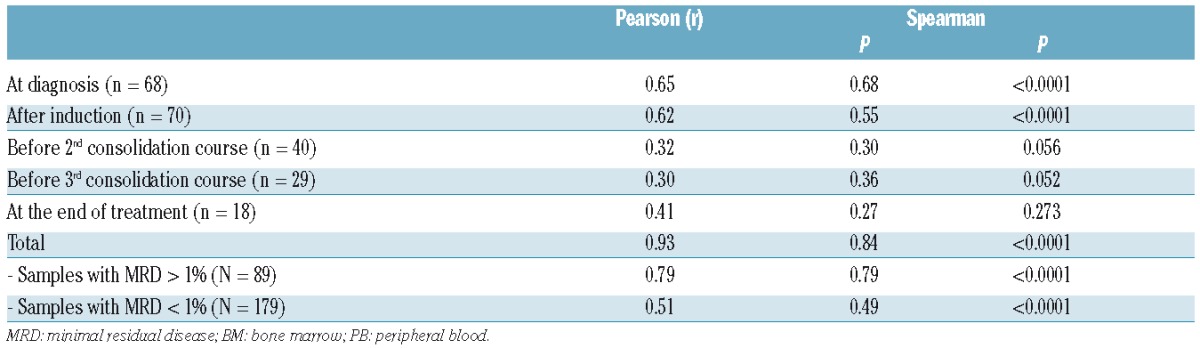
A comparison of the 268 (51.0%) paired samples with both PB- and BM-MRD levels >0.001% was performed. This analysis was split into two groups of MRD levels lower or higher than 1%, corresponding to samples collected in CR or at diagnosis/relapse, respectively. A significant correlation was observed between BM and PB MRD levels, irrespective of the MRD subgroup (Table 1). However, low PB- and BM-MRD values (<1%) were less closely correlated than more elevated values collected at diagnosis or at hematological relapse. The median value of BM-MRD in patients with persistent CHR was 0.03% (range: 0.001–125) and 70.8% (range: 0.8–383) in the case of hematological relapse. The corresponding PB-MRD levels were 0.001% (range: 0.001–27) and 64.6% (range: 0.1–368), respectively.
Table 1.
Correlation between paired BM and PB MRD transcript ratio at specific time-points. Only MRD>0.001% on both PB and BM were considered.
Peripheral blood versus bone marrow MRD prognostic value
The clinical characteristics of the 94 patients included in this MRD study are shown in Table 2. All patients were in first CR after induction chemotherapy. Median follow-up was 44.7 months. For this entire cohort, the 4-year estimated CIR was 33.3% (95%CI: 24.4–44.4) and the 4-year estimated OS was 83.4% (95%CI: 74.0–89.7). Of note, 4 hematological relapses were observed after the 2 years of MRD follow-up planned by protocol.
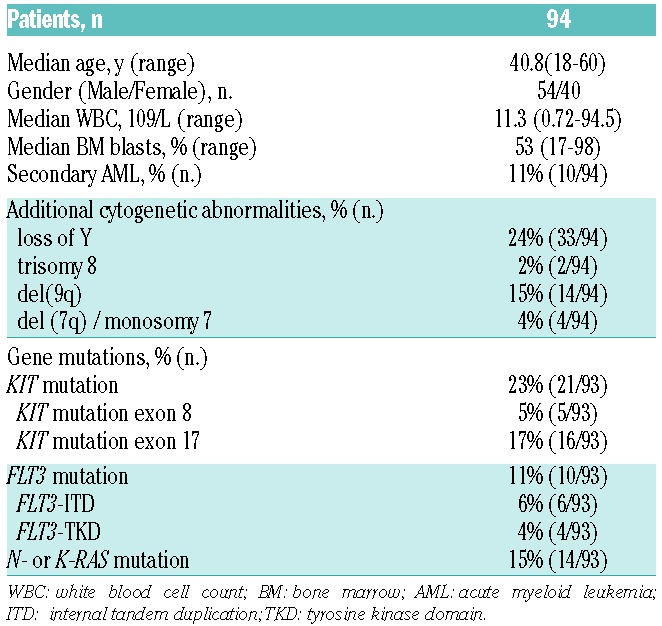
Table 2.
Characteristics of the 94 patients with CBFA-AML included in the CBF-2006 trial.
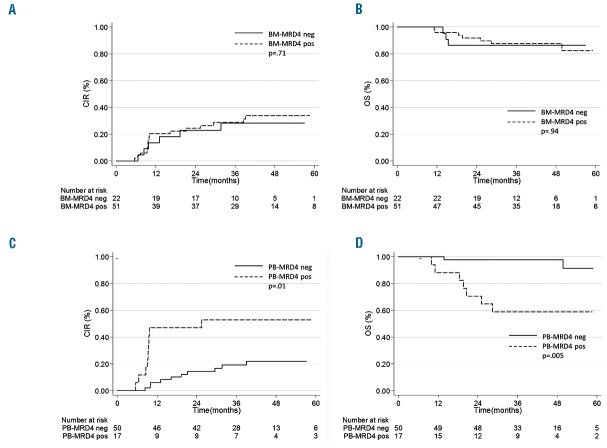
At the end of consolidation therapy, MRD (called MRD4) was assessed on PB and BM within a median time of 39 days after the third consolidation (range: 15–100). Of the 74 patients evaluated at the end of treatment, 52 (70%) obtained a PB complete molecular response (CMR) compared to 22 (30%) on BM. The persistence of a detectable BM-MRD was not associated with an increased risk of relapse (4-year CIR, 33.8% versus 28.2%; SHR 1.20, P= 0.71; Figure 3A) or death (4-year OS, 87.7% versus 86.4%; HR 0.95, P=0.94; Figure 3B). Conversely, detectable PB-MRD at the end of consolidation was significantly associated with both a higher risk of relapse (4-year CIR, 50.9% versus 23.6%; SHR= 2.97, P=.01; Figure 3C) and a shorter survival rate (4-year OS, 63.6% versus 96.0%; HR= 6.8, P=0.005; Figure 3D). Among the 94 patients studied, 8 patients (9%) had a detectable BM-MRD for up to 2 years of follow-up (BM-MRD<0.1%; range: 0.002–0.076%), while still remaining in first CR and in PB-CMR (Figure 4). Notably, the 4 patients that were found to have both positive PB- and BM-MRD at 2 years relapsed. After consolidation completion, whatever the time-point, BM-MRD failed to predict subsequent outcome (data not shown). For these reasons, further analyses were performed using PB-MRD.
Figure 3.
Outcome according to PB- or BM-MRD at the end of consolidation therapy (MRD4). Cumulative incidence of relapse and overall survival are shown according to BM-MRD4 (A and B, respectively) or to PB-MRD4 (C and D, respectively). A MRD >0.001% was considered as positive.
Figure 4.
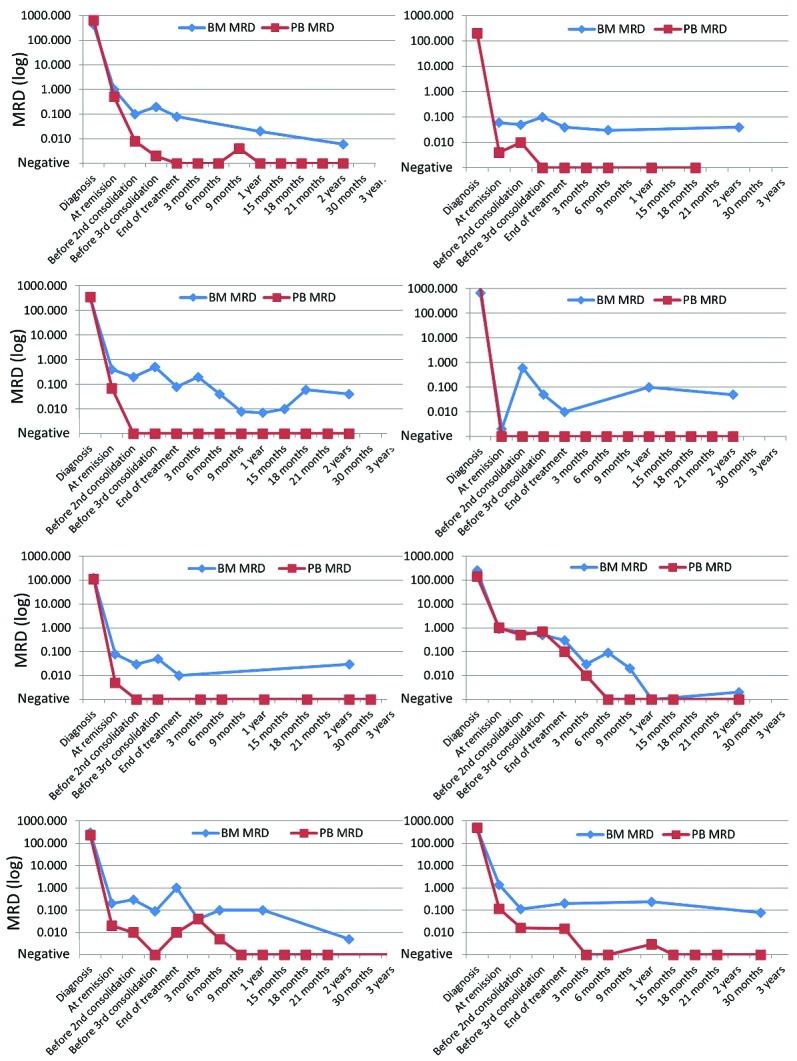
PB- and BM-MRD in 8 patients with persistent BM-MRD up to two years after end of treatment.
Prognostic impact of complete molecular response and time to complete molecular response
During the follow-up, 77 patients (81.9%) reached a PB-CMR. The median time from CR to PB-CMR was 2.5 months. Notably, PB-CMR was achieved up to 16 months after CR (Online Supplementary Figure S1A). Among these 77 patients, 18 experienced a hematological relapse. Among the 17 patients that never reached PB-CMR, 11 were in relapse within 13 months after CR.
In time-dependent Mantel-Byar analysis, patients who achieved PB-CMR had a significantly reduced incidence of relapse (4-year CIR, 26.6% versus 51.2%; SHR .25, P=.001; Figure 5A) and a significantly better overall survival rate (4-year OS, 89.8% versus 56.1%; HR 0.23, P=0.008; Figure 5B). In this favorable subgroup of patients, the presence of FLT3-ITD was associated with a trend towards a longer time to achieve PB-CMR (7.8 months versus 2.4 months in FLT3-ITDpos and FLT3-ITDneg, respectively; P=0.11, Online Supplementary Figure S1D) while RAS gene mutation was associated with a significantly shorter time to PB-CMR (1.8 months versus 2.59 months in RAS mutated and RAS wild-type, respectively; P=0.05, Online Supplementary Figure S1C). None of the other patient- or disease-related characteristics (i.e. age, WBC, bone marrow blast %, del(9q), loss of sexual chromosome, KIT and FLT3-TKD mutations) significantly impacted time to CMR (see Online Supplementary Figure S1B for KIT mutations).
Figure 5.
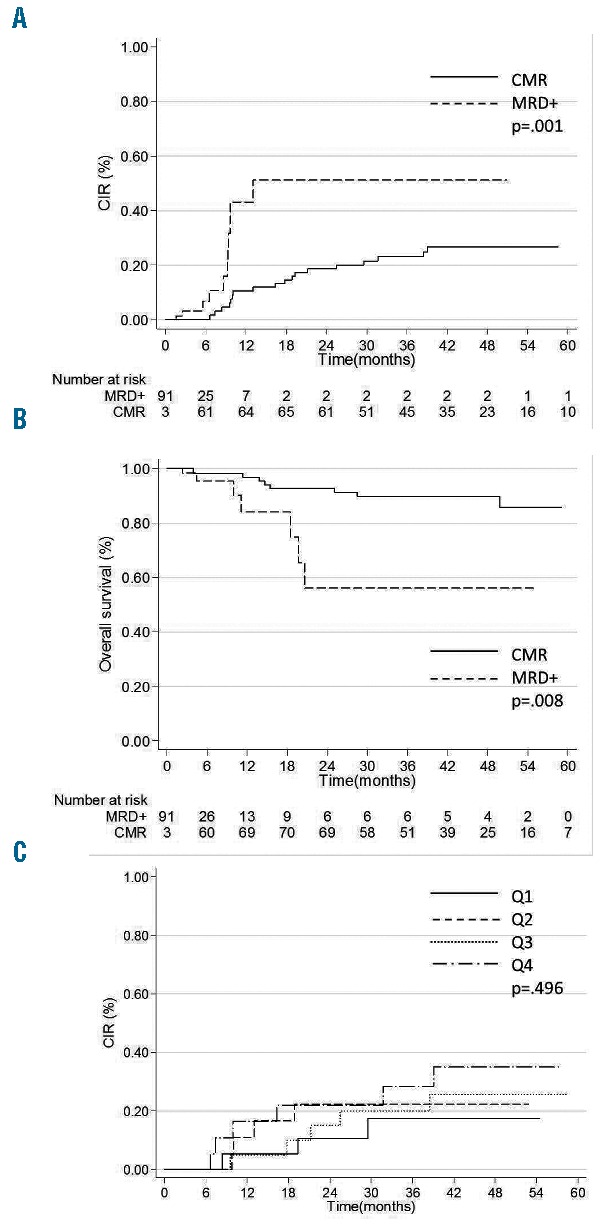
Impact of CMR achievement on patient outcome. Peripheral Blood CMR was evaluated as a time-dependent variable and Simon-Makuch representations are shown for cumulative incidence of relapse (A) and overall survival (B). Time to PB CMR was split into 4 quartiles (Q1–4) to evaluate its impact on cumulative incidence of relapse (C).
The prognostic impact of time to achieve CMR was investigated considering CMR as a time-dependent variable. Time to CMR was not predictive of outcome, neither when considered as a continuous (data not shown) nor as a categorical variable (Figure 5C).
Prognostic impact of loss of complete molecular response
Among the 77 patients who achieved PB-CMR, 23 patients presented a molecular relapse (MR), arbitrarily defined as MRD>0.001% on one PB sample. Among these 23 patients, 1 patient immediately received salvage therapy, 2 patients (9%) were simultaneously in hematological relapse, 13 patients (57%) presented a confirmed positive MRD on the subsequent sample and 7 patients (30%) had a negative MRD on the subsequent sample. Median time between PB-CMR and MR was 6.9 months (95%CI: 3.3–25.7). The median MRD level in patients with a MR not confirmed on a subsequent sample was 0.007% (range 0.003%–0.06%) compared to 0.04% (range: 0.02%–1.55%) in patients with a confirmed MR (P=0.07).
In time-dependent Mantel-Byar analysis, a molecular relapse was associated with a higher cumulative incidence of hematological relapse when compared to persistent PB-CMR (4-year CIR, 74.5% versus 8.2%; SHR= 16.5, P< 0.001; Figure 6A). This excess of relapse translated into a shorter OS (4-year OS, 78.6% versus 94.2%; HR=5.9, P=0.019; Figure 6B). The outcome of patients that presented a confirmed positive MRD was compared to those with a negative MRD on the subsequent sample. Patients with a confirmed molecular relapse had a higher cumulative incidence of molecular relapse (4-year CIR, 86.9% versus 23.4%; SHR= 5.7, P=0.026; Figure 6C) but a similar survival rate (4-year OS, 77.8% versus 77.8%; HR=0.6, P=0.604; Figure 6D). The median time from confirmed detectable PCR positivity to hematological relapse was 3.9 months (IQ, 3.3–6.9). Of note, in the case of loss of CMR with a PB-MRD ≥0.5%, hematological relapse was systematically observed within a median time of 28 days (range: 10–99 days).
Figure 6.
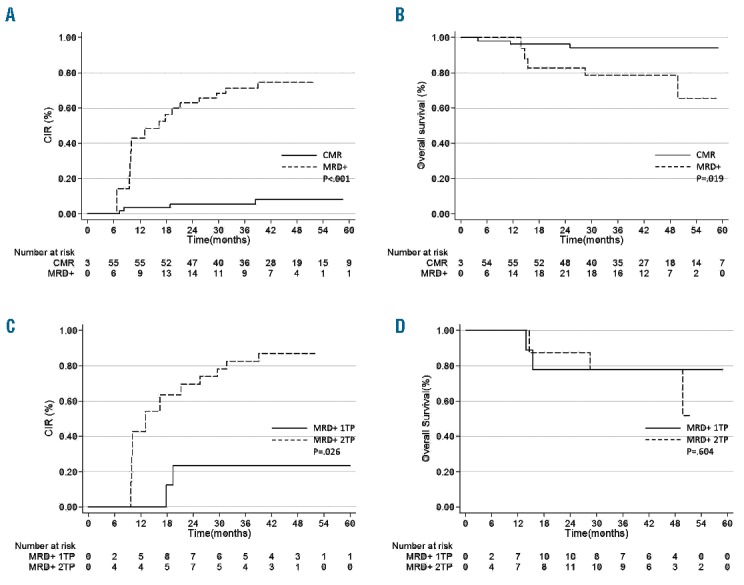
Impact of molecular relapse in patients with complete molecular remission. Simon-Makuch representations are shown for cumulative incidence of relapse (A) and overall survival (B) in patients who remain in CMR (CMR) or who experienced a molecular relapse (MRD+). Simon-Makuch representations are shown for cumulative incidence of relapse (C) and overall survival (D) in patients who experienced a molecular relapse confirmed (2 consecutive time-points, 2TP) or not confirmed (1 time-point, 1TP) on a subsequent sample.
Peripheral blood kinetic of molecular relapse
In 22 out of the 29 patients who experienced a relapse, a PB-MRD was assessed at the time of relapse. Among these 22 patients, 15 of them had a previous positive PB-MRD assessment within the preceding 3 months. In these 15 patients, the median rate in PB-MRD increase was 1.25 log10/month (range: −0.14,3.58), which is in line with the 3.9 months of median time from confirmed detectable PCR positivity to hematological relapse observed above. Individual PB-MRD evolutions for the 22 patients are shown in the Online Supplementary Figure S2.
Discussion
In CBF-AML, recent reports have indicated that RUNX1-RUNX1T1 MRD reduction in the BM after 1 or 2 consolidation courses was the most powerful prognostic factor of relapse.1,2,16 However, early MRD response to treatment does not allow for the prediction of all subsequent events, and patients with satisfying early response will still experience relapse in around 20% of cases.2 In this supplementary analysis, we showed that PB monitoring on a 3 monthly basis for up to 24 months after the end of treatment allowed for the detection of molecular relapse and the anticipation of hematological relapse in RUNX1-RUNX1T1 positive AML patients.
This study is the first report of systematic prospective MRD monitoring in CBFA-AML patients homogeneously treated in a phase III study. In CBFA-AML patients, persistent detection of RUNX1-RUNX1T1 transcripts have been reported in BM and/or PB in patients with prolonged CR.1,10,11,17 Thus, no real consensus has emerged concerning the source of the sample to monitor MRD after the end of chemotherapy. We herein confirm the good correlation between BM and PB MRD levels in a large number of samples.18 Despite the use of a quantitative RT-PCR assay with a sensitivity of 0.001%, we observed a significant amount of positive BM-MRD with negative PB-MRD samples (25.5%). A difference in MRD kinetics upon therapy partially accounts for this disparity between PB and BM samples. However, as previously reported, the persistence of a positive BM MRD at 2 years was detected in 9% of patients who remained in long-term CR. The persistence of RUNX1-RUNX1T1 positive non-leukemic cells (hematopoietic stem cells, B-cells, monocytes and mast cells) in the BM has been suggested to explain this persistence of a positive BM signal.19,20 This probably contributes to the lack of prognostic impact of post-consolidation BM MRD, and strongly supports the use of PB MRD to monitor RUNX1-RUNX1T1 positive AML patients.
Out of the 29 hematological relapses observed in our cohort, 11 (38%) occurred early, before 13 months of follow-up, in the context of persistent PB-MRD positivity, 2 (7%) were diagnosed at the same time as molecular relapse, 2 (7%) after molecular relapse with a negative MRD on a subsequent sample and 10 (34%) after molecular relapse confirmed on a subsequent sample. Among the 4 patients (14%) who relapsed without previous molecular relapse, one patient had a late relapse occurring after the last negative PB-MRD assessed at 2 years, and the other 3 patients were not monitored as scheduled. In 21 patients, the relapse was thus predicted either by the persistence of PB-MRD positivity or by a confirmed molecular relapse. Complete molecular response on PB occurred in 81.9% of patients and was associated with a reduced risk of relapse and a longer survival rate. However, our data do not suggest a preferable time-point to consider persistent PB MRD positivity for intervention, a positive PB-MRD at 3, 6 or 9 months after the end of treatment being associated with a 4-year CIR of around 60% (data not shown). Consistent with previous reports, a molecular relapse was highly correlated to a subsequent risk of hematological relapse. Indeed, Ommen et al., reporting on 42 patients, found that a MRD > 10−4 on PB or BM was highly predictive of hematological relapse within 3 months.10 In a more recent study, Yin JA et al. reported that MRD positivity at a rate of >500 RUNX1-RUNX1T1 copies on BM and >100 RUNX1-RUNX1T1 copies on PB were highly correlated to the risk of hematological relapse and to survival.1 In this study, median times between detectable PCR positivity (10−5 sensitivity, normalized to ABL1) to hematological relapse were 4.9 months and 4.5 months in BM and PB, respectively. All patients with loss of CMR and PB MRD ≥ 0.5% relapsed, but we were not able to define an optimal threshold to predict hematological relapse. With a median time to hematological relapse of 3.9 months, it seems reasonable to recommend confirming a molecular relapse on a second sample before considering any therapeutic intervention.
Nowadays, there are no recommendations concerning patients with CBF-AML in molecular relapse. Gemtuzumab ozogamicin has been suggested as a drug of interest in CBF- AML therapy, in frontline and as part of salvage therapy, but it has been shown to be associated with increased liver toxicity.21,22 Allogeneic stem cell transplant in second CR is a standard recommendation in young adults with AML, but it remains a subject of discussion in CBF-AML.22,23
In conclusion, we suggest that MRD level monitoring by quantitative RT-PCR during follow-up after high-dose cytarabine-based therapy in CBFA-AML should be evaluated in PB every 3 months for up to two years after consolidation completion. In the case of persistent positive PB MRD after treatment, patients should be closely monitored. These data also suggest that the reappearance of a detectable MRD in PB should be confirmed in a second PB sample to more accurately predict hematological relapse. Further studies will be mandatory to define the best strategy in terms of therapeutic attitude according to molecular relapse.
Acknowledgments
The authors thank all hematologists who participated in the CBF 2006 trial for providing follow up samples and their helpful to extend clinical follow up and Annaëlle Beucher for technical support with MRD analysis.
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/101/3/328
Trial registration
This study has been part of the CBF 2006 trial referred in EudraCT #2006-005163-26 and ClinicalTrials.gov ID #NCT00428558.
References
- 1.Yin JA, O’Brien MA, Hills RK, Daly SB, Wheatley K, Burnett AK. Minimal residual disease monitoring by quantitative RT-PCR in core binding factor AML allows risk stratification and predicts relapse: results of the United Kingdom MRC AML-15 trial. Blood. 2012;120(14):2826–2835. [DOI] [PubMed] [Google Scholar]
- 2.Jourdan E, Boissel N, Chevret S, et al. Prospective evaluation of gene mutations and minimal residual disease in patients with core binding factor acute myeloid leukemia. Blood. 2013;121(12):2213–2223. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JC, Weiss RB, Arthur DC, et al. Extramedullary leukemia adversely affects hematologic complete remission rate and overall survival in patients with t(8;21)(q22;q22): results from Cancer and Leukemia Group B 8461. J Clin Oncol. 1997;15(2):466–475. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen S, Leblanc T, Fenaux P, et al. A white blood cell index as the main prognostic factor in t(8;21) acute myeloid leukemia (AML): a survey of 161 cases from the French AML Intergroup. Blood. 2002;99(10):3517–3523. [DOI] [PubMed] [Google Scholar]
- 5.Baer MR, Stewart CC, Lawrence D, et al. Expression of the neural cell adhesion molecule CD56 is associated with short remission duration and survival in acute myeloid leukemia with t(8;21)(q22;q22). Blood. 1997;90(4):1643–1648. [PubMed] [Google Scholar]
- 6.Schoch C, Haase D, Haferlach T, et al. Fifty-one patients with acute myeloid leukemia and translocation t(8;21)(q22;q22): an additional deletion in 9q is an adverse prognostic factor. Leukemia. 1996;10(8):1288–1295. [PubMed] [Google Scholar]
- 7.Paschka P, Marcucci G, Ruppert AS, et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol. 2006;24(24):3904–3911. [DOI] [PubMed] [Google Scholar]
- 8.Boissel N, Leroy H, Brethon B, et al. Incidence and prognostic impact of c-Kit, FLT3, and Ras gene mutations in core binding factor acute myeloid leukemia (CBF-AML). Leukemia. 2006;20(6):965–970. [DOI] [PubMed] [Google Scholar]
- 9.Schnittger S, Weisser M, Schoch C, Hiddemann W, Haferlach T, Kern W. New score predicting for prognosis in PML-RARA+, AML1-ETO+, or CBFBMYH11+acute myeloid leukemia based on quantification of fusion transcripts. Blood. 2003;102(8):2746–2755. [DOI] [PubMed] [Google Scholar]
- 10.Ommen HB, Schnittger S, Jovanovic JV, et al. Strikingly different molecular relapse kinetics in NPM1c, PML-RARA, RUNX1-RUNX1T1, and CBFB-MYH11 acute myeloid leukemias. Blood. 2010;115(2): 198–205. [DOI] [PubMed] [Google Scholar]
- 11.Krauter J, Gorlich K, Ottmann O, et al. Prognostic value of minimal residual disease quantification by real-time reverse transcriptase polymerase chain reaction in patients with core binding factor leukemias. J Clin Oncol. 2003;21(23):4413–22. [DOI] [PubMed] [Google Scholar]
- 12.Boissel N, Renneville A, Leguay T, et al. Dasatinib in high-risk core binding factor acute myeloid leukemia in first complete remission: a French Acute Myeloid Leukemia Intergroup trial. Haematologica. 2015;100(6):780–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabert J, Beillard E, van der Velden VH, et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia - a Europe Against Cancer program. Leukemia. 2003;17(12):2318–2357. [DOI] [PubMed] [Google Scholar]
- 14.Simon R, Makuch RW. A non-parametric graphical representation of the relationship between survival and the occurrence of an event: application to responder versus non-responder bias. Stat Med. 1984;3(1):35–44. [DOI] [PubMed] [Google Scholar]
- 15.Mantel N. Evaluation of Response-Time Data Involving Transient States: An Illustration Using Heart-Transplant Data. J Am Stat Assoc. 1974;69:81–86. [Google Scholar]
- 16.Zhu HH, Zhang XH, Qin YZ, et al. MRD-directed risk stratification treatment may improve outcomes of t(8;21) AML in the first complete remission: results from the AML05 multicenter trial. Blood. 2013;121(20):4056–4062. [DOI] [PubMed] [Google Scholar]
- 17.Tobal K, Yin JA. Monitoring of minimal residual disease by quantitative reverse transcriptase-polymerase chain reaction for AML1-MTG8 transcripts in AML-M2 with t(8; 21). Blood. 1996;88(10):3704–3709. [PubMed] [Google Scholar]
- 18.Leroy H, de Botton S, Grardel-Duflos N, et al. Prognostic value of real-time quantitative PCR (RQ-PCR) in AML with t(8;21). Leukemia. 2005;19(3):367–372. [DOI] [PubMed] [Google Scholar]
- 19.Miyamoto T, Weissman IL, Akashi K. AML1/ETO-expressing nonleukemic stem cells in acute myelogenous leukemia with 8;21 chromosomal translocation. Proc Natl Acad Sci USA. 2000;97(13):7521–7526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cornet E, Dumezy F, Roumier C, et al. Involvement of a common progenitor cell in core binding factor acute myeloid leukaemia associated with mastocytosis. Leuk Res. 2012;36(11):1330–1333. [DOI] [PubMed] [Google Scholar]
- 21.Hills RK, Castaigne S, Appelbaum FR, et al. Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: a meta-analysis of individual patient data from randomised controlled trials. Lancet Oncol. 2014;15(9):986–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hospital MA, Prebet T, Bertoli S, et al. Core-binding factor acute myeloid leukemia in first relapse: a retrospective study from the French AML Intergroup. Blood. 2014;124(8):1312–1319. [DOI] [PubMed] [Google Scholar]
- 23.Burnett AK, Goldstone A, Hills RK, et al. Curability of patients with acute myeloid leukemia who did not undergo transplantation in first remission. J Clin Oncol. 2013;31(10):1293–1301. [DOI] [PubMed] [Google Scholar]