Abstract
Background
Prophylactic ethanol lock therapy (ELT) reduces central line–associated bloodstream infections (CLA-BSIs) in children with intestinal failure (IF). However, the risk of associated complications is unclear. We aim to describe our experience with prophylactic ethanol locks in a cohort of patients with IF.
Materials and Methods
Thirty patients on ELT from 2010–2013 were identified by review of our intestinal rehabilitation registry. Patient demographics, CLA-BSI events, and line complications were extracted. Comparisons in infection and complication rates when on and off ELT were made using a Poisson mixed-effect regression model.
Results
CLA-BSIs when on and off ELT were 3.1 and 5.5 per 1000 catheter days, respectively (P < .015). Overall complication rates were similar in both groups. In those patients who experienced a complication, the complication rates on ELT compared with time off ELT were significantly lower (P < .003). Line perforation or breakage rates declined significantly when on ELT, from 1.8 to 1.53 per 1000 catheter days (P < .006). Line occlusion rates also decreased on ELT, from 0.6 to 0.3 per 1000 catheter days (P = .056). Infecting organisms were not different on and off ELT, and patients experienced a similar number of polymicrobial infections on or off therapy. Klebsiella pneumoniae was the most common infecting organism in both groups.
Conclusions
Ethanol lock therapy use reduces both CLA-BSI and central line complication rates in children with IF. These results underscore the safety and efficacy of ELT use in this population.
Keywords: ethanol lock, intestinal failure, central venous catheter, central line–associated bloodstream infection
Introduction
Pediatric intestinal failure (IF) occurs when adequate nutrition cannot be delivered through a child’s gastrointestinal (GI) tract to support normal growth and development. The most common cause of pediatric IF is short bowel syndrome (SBS), which is characterized by the loss of enteral autonomy following intestinal resection. In all cases of IF, parenteral nutrition (PN) is required for an extended period of time, necessitating the placement and maintenance of a central venous catheter.
Central line–associated bloodstream infection (CLA-BSI) is a primary bloodstream infection (BSI) in a patient who had a central line at least 48 hours before development of the BSI and is not related to an infection at another site.1 CLA-BSI rates for surveyed, pediatric inpatient units reported in the 2012 National Healthcare Safety Network data summary ranged from 0.5–1.9 per 1000 catheter days.2 The IF population has a higher risk for CLA-BSIs due to the use of PN, relative immune-deficient state, poor intestinal motility, frequency of line access, and reduced mucosal barrier function. Indeed, recent surveys of this population revealed rates between 8.0 and 10.2 infections per 1000 catheter days.3–5 These infections may briskly become life threatening, add to healthcare costs, and increase the risk of liver injury.6,7
Concerns for the development of antimicrobial resistance and the high antibiotic concentrations required to penetrate biofilms have led to the use of alternative lock agents (such as ethanol and taurolidine) with a more favorable profile.8 Pediatric ethanol lock therapy (ELT) was first described as an adjunctive treatment of CLA-BSIs in the pediatric oncology population, then as a prophylactic agent in the pediatric population receiving home PN.9,10 Ethanol is a widely used antiseptic that exhibits broad-spectrum antimicrobial and antifungal activity through the disruption of cell membranes, denaturation of proteins, and cell lysis.11 It is also capable of penetrating biofilms.8
Few studies have examined a prophylactic ELT strategy for reducing CLA-BSIs in the pediatric IF population. Five observational studies that included up to 23 patients per study have demonstrated efficacy.3–5,12,13 A meta-analysis of 4 of these studies revealed a reduction of 7.67 BSIs per 1000 catheter days with the use of ELT, although ELT protocols differed among studies.14 Still, little is known of ELT-associated complications. The goal of our study was to evaluate the potential benefits and associated complications of ELT in a large cohort of patients with IF managed by a single center.
Materials and Methods
The design was a retrospective cohort study with unplanned crossover performed with the approval of the Cincinnati Children’s Hospital Investigational Review Board. All patients included in this study required daily PN for IF of diverse etiologies. All patients were followed by the intestinal rehabilitation program at Cincinnati Children’s Hospital Medical Center and were enrolled in the Intestinal Rehabilitation Registry. Home care, including PN and ethanol prescriptions, was coordinated through the intestinal rehabilitation program.
ELT Protocol
Criteria for use of ELT included >3 line infections in a 1-year time period, >2 gram-negative line infections in a 1-year time period, 1 episode of a fungal line infection, continuation of a referral hospital ELT, or removal of 2 lines due to infections. Exclusion criteria included perceived allergy to ethanol, hypercoagulability, a loss of 2 or more catheters to line occlusion, psychosocial situations preventing safe use, guardian objection to the use of ethanol, or lines identified as possibly unsafe to use with ethanol (eg, polyurethane catheter). ELT is not used with peripherally inserted central catheters due to their composition (polyurethane) and the paucity of data informing its use in these devices.
Following the decision to begin ELT, the central venous catheter (CVC) priming volume was determined. Homecare orders were placed and primary care giver education accomplished. ELT dwells were performed daily during a planned window from CVC access. The CVC windows were largely determined by PN cycling tolerance and ranged between 2 and 12 hours daily. They were not influenced by the presence of multiple CVCs.
The CVC was flushed with normal saline. A priming volume of 70% ethanol solution was instilled into the CVC lumen and allowed to dwell for a minimum of 2 hours and up to 12 hours. During this time, neither medications nor PN were administered through the line. At the conclusion of dwell time, ethanol and a small flash of blood were drawn from the CVC and discarded. The line was then flushed with at least 5 mL of normal saline and use resumed. At no time was heparin used in solutions administered to patients on ELT. Although study participants use ethanol from a variety of manufacturers based on timely availability and cost, our own home care currently reconstitutes to 70% ethanol concentration from 98% dehydrated alcohol (Akorn Pharmaceuticals, Lake Forest, IL).
Study Population
Patients on ELT during the study period of January 1, 2011, to December 31, 2013, were identified by review of our intestinal rehabilitation registry. All patients also experienced some amount of time off ELT during the study period, and thus each patient acted as his or her own control. Events prompting return to time off ELT included admission to hospitals not trained in ELT use, replacement of a central line, or failure to continue during inpatient admission. Some patients entered the study period on ELT, which was started for infections occurring before the study start. Data fields were extracted and separated by status of ELT use. Fields extracted include those pertaining to demographic information, etiology of IF, CLA-BSI events, line complications, and infecting organism. Catheter days while on and off ELT were calculated and events reported per 1000 catheter days. An event occurring in a patient with multiple lines was only counted against 1 line, since most line infections were monomicrobial, thus likely originating from a single source.
Data Analysis
Descriptive analyses were performed to characterize the population using median and range values. A Poisson mixed-effect regression model was employed to assess significance of difference between the number of bloodstream infections when the patient was on and off ELT. Sex, age, and group were considered fixed effects, whereas a random patient effect was used to adjust for correlation. A zero-inflated Poisson (ZIP) model was used to analyze the number of complications between groups and the number of infections by infecting organism group, on and off ELT, to account for the large number of days when patients did not experience a complication (zero count). Thus, in our analysis using ZIP modeling, the denominator is the number of catheter days, and the resulting value is predictive. We also calculated the incidence rate of CLA-BSIs per 1000 catheter days in general and by organism classification. Central line days exceed days in the study period due to the existence of multiple simultaneous lines.
Results
Thirty patients (50% female) were identified during the 3-year study period (Table 1). The median age at study conclusion was 6 years (range, 1–20 years). The diagnostic categories included primary IF, SBS, and parenteral support following multivisceral transplant. Primary IF was caused by pseudo-obstruction (6 patients), metabolic or mitochondrial myopathy (3 patients), and tufting enteropathy (1 patient). SBS resulted from necrotizing enterocolitis (3 patients), gastroschisis (3 patients), jejunal or ileal atresia (4 patients), and trauma (1 patient).
Table 1.
Demographics of Study Participants.
| Demographic Category | Valuea |
|---|---|
| No. of patients | 30 |
| Patient age, median (range), y | 6.5 (1–20) |
| Sex | |
| Male | 15 |
| Female | 15 |
| Etiology | |
| Short bowel syndrome | 11 |
| Pseudo-obstruction | 6 |
| Congenital enteropathy | 1 |
| Metabolic | 3 |
| Post-multivisceral transplant | 9 |
| Total line days | 23,202 |
| Line type | |
| Tunneled central venous catheter | 87 |
| Peripherally inserted central catheter | 61 |
| Port | 8 |
Values are presented as numbers unless otherwise indicated.
Total line days were 23,202, of which 14,337 days were on ELT and 8865 days were off ELT. The median (range) of line days on ELT was 296 (50–1107) days. The median (range) of line days off ELT was 210 (0–1127) days. CVC type included 87 tunneled lines, 61 peripherally inserted central catheters, and 8 Mediports. Patients occasionally required short-term peripherally inserted central catheter (PICC) lines between tunneled line placements due to infection or other indications for line removal. These PICC lines were not exposed to ELT.
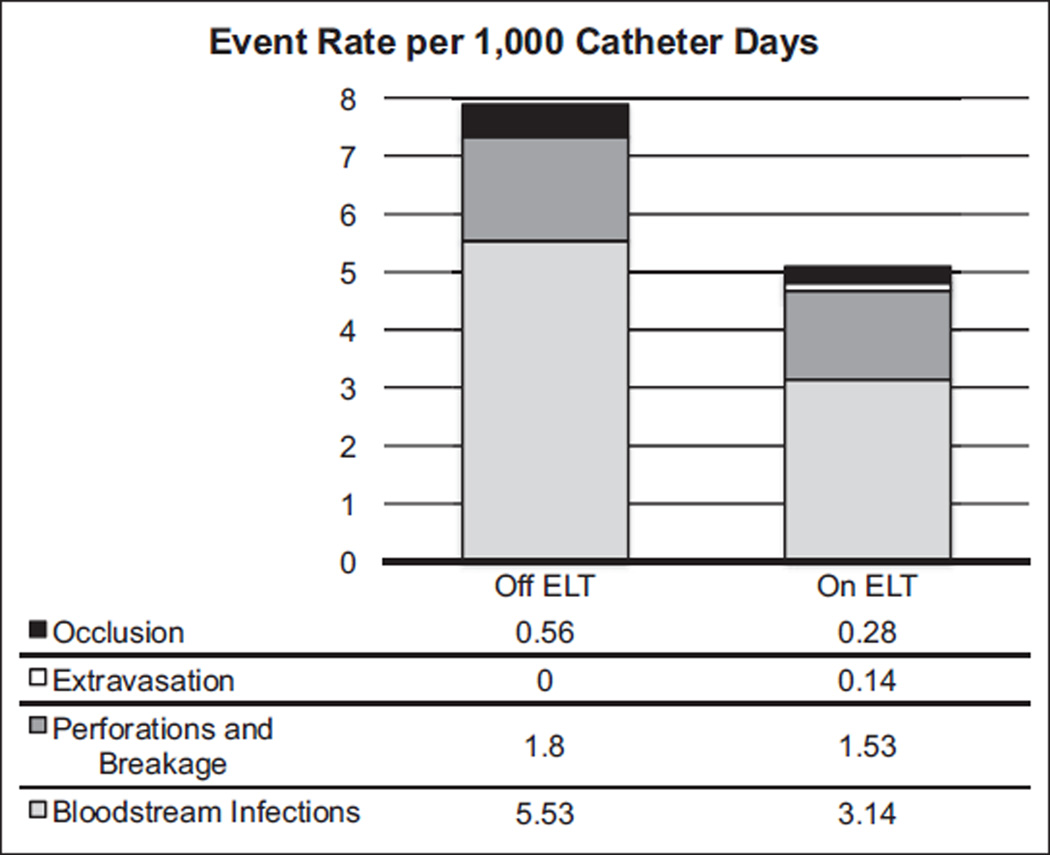
Bloodstream infections occurred in 22 of the 30 patients studied and occurred at a rate of 5.53 infections per 1000 catheter days when off ELT (Figure 1). BSI events off ELT ranged from 0–8 infections per patient during the study period. On ELT, BSI events occurred at a rate of 3.14 per 1000 catheter days with a range of 0–7 events per patient. ELT significantly lowered the BSI incidence compared with time off ELT (P < .015). Using Poison regression methods and adjusting for age and sex, the difference between the predicted BSI incidence on and off ELT remained significant (P < .013).
Figure 1.
Line complication and bloodstream infection rates on and off ethanol lock therapy (ELT). After adjustment for age and sex, ELT was found to significantly decrease rates of BSI (P < .015), overall complication counts in patients who experienced a complication (P < .003), and perforation and breakage rates (P < .006).
Overall, the observed complication rate on ELT was 1.95 events per 1000 catheter days and 2.37 events per 1000 catheter days off ELT (Figure 1) (P = .432). When the 16 patients without complications during the study period were excluded, complications on and off ELT occurred at rates of 2.98 and 8.46, respectively. The ZIP model revealed that, after adjusting for age and sex, the mean number of complications per 1000 catheter days was lowered by 71% in patients who had suffered at least 1 complication (P = .003). The perforation or breakage rate on ELT was 1.53 events per 1000 catheter days compared with 1.8 events per 1000 catheter days off ELT. After adjusting for age and sex, this difference was also found to be significant (P = .006). Line occlusion rates were observed to decrease on ELT to 0.28 events from 0.56 events per 1000 catheter days off ELT (P = .056 adjusted for age and sex with ZIP modeling). Two extravasation events while on ELT produced a rate of 0.14 events per 1000 catheter days. There were no extravasations off ELT.
Klebsiella pneumoniae was the organism cultured most frequently in both groups during febrile episodes. Enterococcus faecalis was the gram-positive organism cultured most frequently when off ELT compared with Staphylococcus aureus when on ELT. Candida albicans was cultured while on ELT, but multiple Candida species were recovered from polymicrobial infections in both groups. Gram-positive, gram-negative, fungal, and polymicrobial infections were not individually and significantly different between time on and off ELT (P = .19 for gram-positive, gram-negative, and polymicrobial infections; fungal counts too low for statistical analysis by zero-inflated Poisson regression) (Table 2).
Table 2.
Rates of Bloodstream Infection by Organism Classification and Ethanol Lock Therapy (ELT) Status.
| ELT Status | Organism Classification |
Rate (per 1000 Catheter Days) |
|---|---|---|
| Off ELT | Gram positive | 2.48 |
| Gram negative | 1.35 | |
| Fungal | 0.00 | |
| Polymicrobial | 1.13 | |
| On ELT | Gram positive | 1.39 |
| Gram negative | 0.84 | |
| Fungal | 0.07 | |
| Polymicrobial | 0.84 |
Discussion
ELT has previously been shown to reduce CLA-BSIs in the pediatric IF population.14 A criticism has been that ELT is associated with more line complications, specifically breakage and occlusion, although authors previously evaluating this were unable to demonstrate significance between groups on and off ELT.15 To address, this we evaluated our 3-year experience with ELT in a larger cohort of patients. Our study group is an appropriately heterogeneous representation of the IF population. Our design compares time on ELT with time spent off ELT, allowing patients to serve as their own controls.
Our data confirm that with the use of ELT, there is a significant reduction in CLA-BSIs in this population. Overall, we began with a low BSI rate; thus, the magnitude of difference is smaller than previously reported.14 The organisms causing infection in both groups are diverse but are not different between groups. This supports the general consensus that ethanol does not affect selectivity of infecting organisms or lead to drug resistance.
In vitro studies have demonstrated polymer elution with ethanol exposure from polyurethane and Carbothane catheters but not silicone catheters.16–18 In addition, polyurethane catheters exhibit less elasticity following ethanol exposure.19 However, neither polyurethane nor silicone catheters exhibited a significant change in breakage force after exposure.19 Indeed, clinical studies assessing differences in line breakage or perforation in the pediatric population have largely been inconclusive.14,15 We demonstrate a small but significant reduction of breakage or perforation rates in lines exposed to daily ethanol locks. We propose that this reflects greater attention to line care in patients requiring ethanol locks rather than a direct improvement of line integrity with ethanol.
Previous retrospective studies and 1 prospective study have demonstrated increased catheter occlusion rates when ELT is in use.5,20,21 Occlusion has been attributed to ethanol interaction with plasma protein or heparin. Indeed, in vitro studies have confirmed that the commonly used ethanol concentration of 70% induces heparin precipitation.22 In addition, plasma protein has been shown to aggregate in the presence of 70% ethanol.23 Our data did not indicate any increase in occlusions when on ELT. Although our protocol requires withdrawal of the lock solution prior to use, we discourage the use of heparin through lines requiring ELT. Thus, we suspect heparin precipitation as the predominant cause of line occlusions reported in previous studies.
Shortcomings of our study are generally similar to those of previous studies of the pediatric IF population. The group being studied is very heterogeneous, with a broad range of ages, catheter sizes, and etiologies of IF. PICCs composed of polyurethane and inserted at other institutions were not exposed to ELT. Patients occasionally required PICC lines between tunneled line placements due to infection or other indications for line removal. These PICC lines were invariably composed of silastic material rather than polyurethane when inserted within our own institution; however, they too were not exposed to ELT. Due to the nature of our registry, we were unable to determine whether internally or externally placed PICC lines produced different infection or complication rates than tunneled central venous catheters.
The shortcomings of our study and those involved when studying this population in general highlight the need for multicenter collaboration. A prospective, randomized, placebo-controlled study across several centers is needed to adequately and conclusively demonstrate ethanol lock efficacy and safety in children. Using methods for comparative effectiveness to evaluate the effectiveness of different durations (hours/day) on ELT, number of days per week on the ELT and the different concentrations of ethanol used are also needed.
Using a robust cohort study with unplanned crossover, we studied ethanol locks in a large pediatric IF population. We observed no difference in overall central line complications in patients when on and off ethanol lock therapy. Reduced perforation and breakage rates were observed with ELT, which is likely due to improved line care awareness. As expected, we also observed a decrease in the central line–associated bloodstream infection rate with ELT. Our data support previous studies indicating that ELT is an effective method for the prevention of central line–associated bloodstream infections and add that this strategy is safe for use in children with critical central lines without increasing complications.
Clinical Relevancy Statement.
Both adults and children with intestinal failure require daily central venous access, putting them at great risk for bloodstream infections. Ethanol lock therapy has emerged as a method of prophylaxis that does not increase the risk of antimicrobial resistance, but the association with complications such as catheter obstruction or perforation remains speculative. We report infection and complication rates in a cohort of patients while on and off ethanol lock prophylaxis. Our data confirm a reduction in bloodstream infections without increasing complication rates. We conclude that prophylaxis with ethanol lock therapy is not only effective but also safe in the pediatric intestinal failure population.
Acknowledgments
Financial disclosure: This work was supported in part by National Institutes of Health grants P30 DK078392, T32 DK007727 (EAM), and R21 DK88027 (CRC).
References
- 1.O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52:e162–e193. doi: 10.1093/cid/cir257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dudeck MA, Weiner LM, Allen-Bridson K, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Control. 2013;41:1148–1166. doi: 10.1016/j.ajic.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wales PW, Kosar C, Carricato M, et al. Ethanol lock therapy to reduce the incidence of catheter-related bloodstream infections in home parenteral nutrition patients with intestinal failure: preliminary experience. J Pediatr Surg. 2011;46:951–956. doi: 10.1016/j.jpedsurg.2011.02.036. [DOI] [PubMed] [Google Scholar]
- 4.Jones BA, Hull MA, Richardson DS, et al. Efficacy of ethanol locks in reducing central venous catheter infections in pediatric patients with intestinal failure. J Pediatr Surg. 2010;45:1287–1293. doi: 10.1016/j.jpedsurg.2010.02.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cober MP, Kovacevich DS, Teitelbaum DH. Ethanol-lock therapy for the prevention of central venous access device infections in pediatric patients with intestinal failure. JPEN J Parenter Enteral Nutr. 2011;35:67–73. doi: 10.1177/0148607110362758. [DOI] [PubMed] [Google Scholar]
- 6.Btaiche IF, Khalidi N. Parenteral nutrition–associated liver complications in children. Pharmacotherapy. 2002;22:188–211. doi: 10.1592/phco.22.3.188.33553. [DOI] [PubMed] [Google Scholar]
- 7.Blot SI, Depuydt P, Annemans L, et al. Clinical and economic outcomes in critically ill patients with nosocomial catheter-related bloodstream infections. Clin Infect Dis. 2005;41:1591–1598. doi: 10.1086/497833. [DOI] [PubMed] [Google Scholar]
- 8.Donlan RM. Biofilm elimination on intravascular catheters: important considerations for the infectious disease practitioner. Clin Infect Dis. 2011;52:1038–1045. doi: 10.1093/cid/cir077. [DOI] [PubMed] [Google Scholar]
- 9.Dannenberg C, Bierbach U, Rothe A, et al. Ethanol-lock technique in the treatment of bloodstream infections in pediatric oncology patients with broviac catheter. J Pediatr Hematol Oncol. 2003;25:616–621. doi: 10.1097/00043426-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Opilla MT, Kirby DF, Edmond MB. Use of ethanol lock therapy to reduce the incidence of catheter-related bloodstream infections in home parenteral nutrition patients. JPEN J Parenter Enteral Nutr. 2007;31:302–305. doi: 10.1177/0148607107031004302. [DOI] [PubMed] [Google Scholar]
- 11.McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev. 1999;12:147–179. doi: 10.1128/cmr.12.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mouw E, Chessman K, Lesher A, et al. Use of an ethanol lock to prevent catheter-related infections in children with short bowel syndrome. J Pediatr Surg. 2008;43:1025–1029. doi: 10.1016/j.jpedsurg.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 13.Pieroni KP, Nespor C, Ng M, et al. Evaluation of ethanol lock therapy in pediatric patients on long-term parenteral nutrition. Nutr Clin Pract. 2013;28:226–231. doi: 10.1177/0884533612468009. [DOI] [PubMed] [Google Scholar]
- 14.Oliveira C, Nasr A, Brindle M, et al. Ethanol locks to prevent catheter-related bloodstream infections in parenteral nutrition: a meta-analysis. Pediatrics. 2012;129:318–329. doi: 10.1542/peds.2011-1602. [DOI] [PubMed] [Google Scholar]
- 15.Abu-El-Haija M, Schultz J, Rahhal RM. Effects of 70% ethanol locks on rates of central line infection, thrombosis, breakage, and replacement in pediatric intestinal failure. J Pediatr Gastroenterol Nutr. 2014;58:703–708. doi: 10.1097/MPG.0000000000000354. [DOI] [PubMed] [Google Scholar]
- 16.Yokoyama H, Aoyamaj T, Nakajima K, et al. Investigation of the cause of polyurethane catheter cracking during constant infusion of etoposide (VP-16) injection (2)—analysis of ethanol eluting materials from catheter [in Japanese] Yakugaku Zasshi. 2003;123:799–803. doi: 10.1248/yakushi.123.799. [DOI] [PubMed] [Google Scholar]
- 17.Msakni N, Galmier MJ, Couret MJ, et al. Complementary mass spectrometric approaches and scanning electron microscopy to study the structural stability of polyurethane tunneled dialysis catheters after exposure to ethanol solutions. Rapid Commun Mass Spectrom. 2013;27:2343–2354. doi: 10.1002/rcm.6691. [DOI] [PubMed] [Google Scholar]
- 18.Guenu S, Heng AE, Charbonne F, et al. Mass spectrometry and scanning electron microscopy study of silicone tunneled dialysis catheter integrity after an exposure of 15 days to 60% ethanol solution. Rapid Commun Mass Spectrom. 2007;21:229–236. doi: 10.1002/rcm.2837. [DOI] [PubMed] [Google Scholar]
- 19.Crnich CJ, Halfmann JA, Crone WC, et al. The effects of prolonged ethanol exposure on the mechanical properties of polyurethane and silicone catheters used for intravascular access. Infect Control Hosp Epidemiol. 2005;26:708–714. doi: 10.1086/502607. [DOI] [PubMed] [Google Scholar]
- 20.Heng AE, Abdelkader MH, Diaconita M, et al. Impact of short term use of interdialytic 60% ethanol lock solution on tunneled silicone catheter dysfunction. Clinic Nephrol. 2011;75:534–541. doi: 10.5414/cn106559. [DOI] [PubMed] [Google Scholar]
- 21.Laird J, Soutar R, Butcher I. Complications of the ethanol-lock technique in the treatment of central venous catheter sepsis. J Infect. 2005;51:338. doi: 10.1016/j.jinf.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 22.Restrepo D, Laconi NS, Alcantar NA, et al. Inhibition of heparin precipitation, bacterial growth, and fungal growth with combined isopropanolethanol locking solution for vascular access devices. J Pediatr Surg. doi: 10.1016/j.jpedsurg.2014.07.003. In press. [DOI] [PubMed] [Google Scholar]
- 23.Schilcher G, Schlagenhauf A, Schneditz D, et al. Ethanol causes protein precipitation—new safety issues for catheter locking techniques. PLoS One. 2013;8:e84869. doi: 10.1371/journal.pone.0084869. [DOI] [PMC free article] [PubMed] [Google Scholar]