Abstract
Background. The purpose of this study was to analyse whether the parallel life situation between stroke patients and their informal caregivers (dyads) shown in cross-sectional studies prevails also in a longitudinal perspective.
Methods. A total of 377 Swedish stroke patients, aged ≥65 years, and their 268 informal caregivers were followed from hospital admission and one year on. Analyses were based on patient interviews, functional ability (MMSE) score, Nottingham Health Profile (NHP) score, Hospital Anxiety and Depression (HAD) score, self-rated health score, and the Gothenburg Quality of Life (GQL) activity score. Similar information was obtained by postal questionnaires from informal caregivers, also including information on the nature and amount of assistance provided and on Caregiver Burden (CB) score.
Results. Before index admission informal caregivers provided care on average 5 h per week and after discharge 11 h per week (P < 0.0001). Support volume was associated with patient sex (more for men), low patient’s functional ability, low received municipal social service support, closeness of patient–caregiver relation, and short distance to patient’s home. Significant positive associations within the dyads were found for HAD anxiety score (P < 0.0001), total NHP score (P < 0.0001), and GQL activity score (P < 0.0001) after adjustment for patient’s age, sex, functional ability, and patient–caregiver relationship. CB score increased with amount of informal caregiver support, patient’s age, and with low functional ability and low amount of municipal social service support. All these associations were constant across time.
Conclusions. There was an association within the dyads regarding anxiety score, NHP score, and activity score. CB score was generally high.
Keywords: Caregiver burden, dyad, elderly, informal caregiver, stroke
Introduction
Advances in stroke rehabilitation have reduced severe disability and institutionalization, and the number of disabled patients living at home and being supported by informal caregivers has increased (1), in Sweden dramatically since the late 1990s (2). The outcomes for stroke survivors have improved during the last decade, but still patients feel they receive insufficient support from the health care sector and the municipality (3).
Caregivers may play an essential role in preserving rehabilitation gains and in the long-term well-being of stroke patients (4–6). Care-giving is a dynamic process, and the impact of care-giving changes over time (7). Stroke-related problems, such as physical, psychological, emotional, and cognitive difficulties may affect the life satisfaction of patients as well as their caregivers (8,9), who may perceive the responsibilities and the amount of care given as a sometimes heavy burden (6,10–13).
There is a need to illuminate how stroke impacts everyday life for patients and informal caregivers (dyads), as well as the reciprocal symbiosis within the dyad. To date, the majority of studies on this subject have been cross-sectional, thereby limiting our understanding of changes taking place over the course of time for patient–informal caregiver dyads. The need for research regarding the caregiver dyad across time has been stressed (14,15).
This study is part of a comprehensive project following elderly stroke survivors over time. Previous publications from the study include a report on how well hospital staff may predict outcome after discharge regarding functional ability, health course, and ability to stay in one’s own home (16), a report on survival and stroke recurrence during follow-up (17), and a report on health problems during follow-up (18).
The aim of the present study was to compare the life situation after stroke in patient–informal caregiver dyads during the first post-stroke year. According to the hypothesis there is a parallel between the life situations of patients and their informal caregivers also in a longitudinal perspective. A further aim was to analyse the amount of care given and its effect on the perceived caregiver burden score.
Material and methods
Setting
The study was performed in a defined geographical region, the cities of Falun (population 55,000) and Borlänge (population 47,000), Dalecarlia county, central Sweden, including urban as well as rural areas. The region is served by Falun General Hospital only. Swedish counties run hospitals and primary health care centres, either directly in council-operated facilities, or indirectly in facilities operated by private contractors. At the time of the study all units in the study area were county council-operated, while nursing homes were generally municipality-operated.
Admission to hospital in Sweden is free of charge for the patient. Central and local governments all subsidize patient fees heavily at hospital outpatient clinics, general practices, and for municipal support, which means that private financial resources are seldom obstacles to health care utilization. Therefore, the vast majority of patients with clinical signs and symptoms indicating stroke are admitted to hospital, with the exception of already hospitalized patients or patients in nursing homes (19).
Swedish municipalities are required by law to provide support to residents who have social or medical needs. Such support may be provided in the form of medical home care in the resident’s own home, assisted accommodation, or nursing homes. All such care given must be documented either in regular health care records (medical home care) or in municipal elderly health care records (assisted accommodation or nursing homes).
Design
The study was designed as a longitudinal cohort study of subjects admitted to hospital because of stroke, with a planned follow-up at 1 week after discharge and 3 and 12 months from the day of admission, with patient interviews, and postal questionnaires to the informal caregivers.
Study population
The study population, design, case ascertainment, and definition of stroke types have been described in detail elsewhere (16). Briefly, the inclusion criteria were 65 years of age or older, living in their own home and with no dementia diagnosis prior to the index hospital admission, discharged alive from the Department of Internal Medicine (stroke unit or general ward) during the period 1 September 1999 to 31 May 2001 after an acute stroke (index admission), defined as intra-cerebral haemorrhage, brain infarction, or stroke of undetermined pathological type (ICD10 codes I61, I63, and I64) (20). Out of 432 potential participants, 42 died while at the Department of Internal Medicine, and 13 died at the Department of Geriatrics. The 377 survivors constitute the study population of this report. Among both men and women, 88% had a cerebral thrombosis, and 97% had a computerized tomography scan.
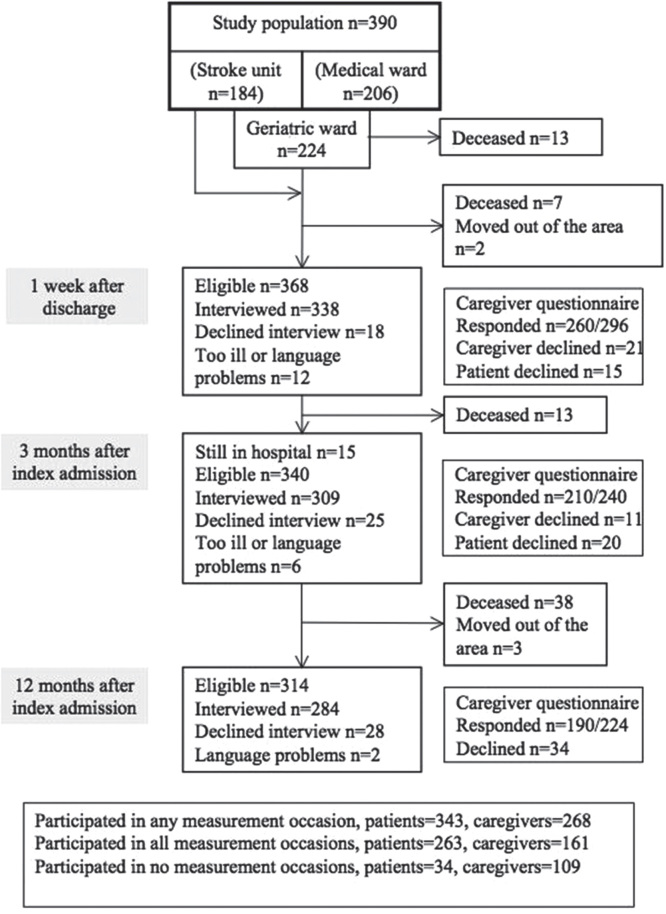
One week after discharge, 339 (92.1%) of 368 eligible patients had a structured and standardized face-to-face interview in their homes or in nursing homes, repeated at 3 (n = 309/340, 90.9%) and 12 (n = 284/314, 90.4%) months after admission by one of two registered nurses. The reasons for data loss are shown in (Figure 1).
Figure 1.
Flow chart of patients and caregivers in the study population.
At the first interview the patients were asked to name their most important informal caregiver: 296 did so, 60 had no informal caregiver, and 21 did not want to ‘bother’ the caregiver with questionnaires. The indicated informal caregivers received a postal questionnaire at the time of each interview. Caregivers were not replaced in case of non-response. In connection with the first interview, 260 of the eligible 296 (87.8%) caregivers responded, at the second interview 210 of 240 (87.5%), and at the third 190 of 224 (84.8%) (Figure 1).
Data collection—patients
The interviews were based on a set of questions drawn up in advance with fixed response alternatives and open alternatives when needed, and the responses were documented on a form with the questions. In case of cognitive or other communication problems, informal caregivers were generally present during the interview and helped to interpret patients’ answers.
In the interviews information on education, marital status, cohabitation, type of housing, functional ability (Katz Activity of Daily Life assessment, ADL) (21), Mini Mental State Examination (MMSE) (22), Nottingham Health Profile (NHP) (23), Hospital Anxiety and Depression Scale (HAD) (24), self-rated health, and the Gothenburg Quality of Life Instrument (GQL) activity scale (25) was sought.
Functional ability is graded A to G. In this study a three-degree grading scale was used with A (independent), B–E (partially dependent), and F–G (completely dependent). For MMSE the original grading scale of 0–30 was used, with normal range 24–30. The NHP questionnaire, tested in the general population and in various patient populations, including stroke patients, measures discomfort. Part I, used in this study, consists of 38 yes/no questions forming six dimensions: energy (3 statements), physical mobility (8 statements), sleep (5 statements), emotional reactions (9 statements), social isolation (5 statements), and pain (8 statements). Statements were weighted within each area, resulting in scores ranging from 0 to 100, with 0 indicating no problems. The HAD scale has 14 items, 7 on anxiety and 7 on depression, each with a four-point verbal rating scale scored 0–3, giving total scores ranging from 0 to 21. Scores of 8–10 on a subscale have been claimed to indicate possible pathology, and scores ≥11 as ‘definite’. Moreover, the patients were asked to grade their self-rated health on a five-degree ordinal scale, ranging from poor (=1) to excellent (=5).
The Activity Score subscale in GQL consists of questions on 32 specified leisure time activities and two open alternatives. At the first interview the subjects were asked which of these activities they had performed during the year preceding the stroke event, and at the last interview which activities they had performed during the first post-stroke year. Possible responses on each question were never (=0), occasionally (=1), or often/regularly (=2). The scores were then totalled to an overall activity score (range 0–64). Information on municipal social service support was obtained from municipal social service records.
Data collection—informal caregivers
Information on caregiver’s age and sex, relationship to the patient, distance from the caregiver’s to the patient’s home, the nature and amount of assistance provided, and the Caregiver Burden (CB) scale (11) was obtained by a questionnaire. The specific types of assistance provided during the previous period and the weekly time spent providing that assistance were requested. In connection with the first interview, caregivers were also asked about care provided in the year before the index admission. Only care specific to the patients was included. Activities regularly undertaken for the whole household (e.g. meal preparation or washing) were included as specific activities only if the patient was incapable of performing these tasks. A support score was calculated based on the frequency of help given from informal caregivers, ranging from no help (=0) to help several times a day (=4) for 15 different tasks, the total score range being 0–60.
The CB scale, originally developed to measure perceived burden in family caregivers of patients with stroke and dementia and shown to be a valid and reliable instrument to assess caregiver burden, consists of 22 items, with scores ranging from ‘not at all’ (=0) to ‘often’ (=4) (11). In addition NHP, HAD, and the Activity Scale questionnaires (the same as in patient interviews), were used.
Ethics considerations
All subjects gave verbal informed consent to participate, standard procedure at the time. The study was approved repeatedly, first by the Research Ethics Committee at Uppsala University and later by the National Research Ethics Board.
Statistical considerations
Data were analysed with the SAS software, version 9.3 (26). Both patient interview data and caregiver data were 95% complete. Forty patient interviews were performed in duplicate independently by two observers. A weighed kappa measure, based on cross-tabulation of reported patient responses, was obtained by the two observers regarding self-rated health, MMSE, functional ability according to Katz, NHP, HAD, and activity GQL score, all with kappa values in the range 0.96–1.0, indicating excellent agreement between the observers.
The analysis of the determinants of the caregiver support score was done with multiple linear regression using support score as the dependent variable, and using functional ability, distance to the patient, the patient–caregiver relationship, whether municipal social service support was given, patient’s age and sex, MMSE score, caregiver’s age and sex, and measurement occasion (time variable) as independent variables, with backward elimination of non-significant independent variables to avoid analysis model overload. The analyses of the determinants of CB score and the association between patients’ and caregivers’ responses to the same type of questionnaires were carried out accordingly. Only two-tailed tests were used. P < 0.05 was regarded as significant.
Results
Characteristics of the patients
At the time of hospital discharge the mean patient age was 78 years, 215 (57%) were women, 278 (73.7%) were receiving care for their first ever stroke, 179 (50.6%) were independent in their functional ability, 93 (26.3%) were partly dependent, 82 (23.2%) were dependent, 292 (77.5%) were back in their regular housing, and 114 (59.7%) of the women and 55 (37.7%) of the men were living alone. Before the index admission, 153 (39.2%) had municipality support. One week after discharge 228 (60.5%) had such support. At the first interview 215 (63.8%) had MMSE score >24, and 126 (41.7%) had a self-rated health score >3.
Characteristics of the informal caregivers
Two-thirds of the caregivers were women, and the mean age was 63 years (range 23–89), 45% were spouses, 40% were children of the patients, 48% were living in the same household or the same building as the patient, another 40% in the same municipality, and 12% in another municipality (Table I). Before index admission, 88% had provided some form of care to the patient, on average 5 hours per week (median 2), and had 8–10 support score (median 5–6). The corresponding numbers after discharge were 100%, 11 h per week (median 3–5), and 13–15 support score (median 7–11), all with P < 0.0001 for change across time. Female caregivers provided more care than male caregivers (P < 0.005). However, the amount of care given after the index stroke admission, whether measured as time or as support score, was non-significantly different across time, whether measured for female and male caregivers separately, or combined.
Table I.
Informal caregiver characteristics.
| Female caregivers | Male caregivers | |||
| n | Mean (SD) or % | n | Mean (SD) or % | |
| na | 174 | 92 | ||
| Age, years | 62.4 (13.26) | 62.9 (14.78) | ||
| Caregiver’s relationship to patient, % | ||||
| Spouse | 81 | 46.6 | 39 | 42.4 |
| Child | 65 | 37.4 | 42 | 45.7 |
| Sibling | 9 | 5.2 | 4 | 4.4 |
| Neighbour or friend | 3 | 1.7 | 1 | 1.1 |
| Grandchild | 3 | 1.7 | – | – |
| Son-in-law or daughter-in-law | 4 | 2.3 | 2 | 2.2 |
| Other relative | 9 | 5.2 | 4 | 4.4 |
| Distance to patient | ||||
| Same household | 79 | 45.4 | 41 | 44.6 |
| Same building | 6 | 3.5 | 3 | 3.3 |
| Same municipality | 71 | 40.8 | 34 | 37.0 |
| Other municipality | 18 | 10.3 | 14 | 15.2 |
| Support given to patient | ||||
| Before index admission: | ||||
| Caregivers providing support | 151 | 83 | ||
| Hours/week | 4.8 (14.60) | 5.3 (13.43) | ||
| Support score | 9.8 (9.64) | 7.9 (7.61) | ||
| One week after discharge: | ||||
| Caregivers providing support | 169 | 90 | ||
| Hours/week | 10.8 (20.00) | 10.2 (15.07) | ||
| Support score | 14.7 (11.71) | 13.0 (10.26) | ||
| Three months after index admission: | ||||
| Caregivers providing support | 140 | 68 | ||
| Hours/week | 12.7 (21.78) | 7.9 (12.63) | ||
| Support score | 14.6 (12.41) | 10.8 (8.88) | ||
| Twelve months after index admission: | ||||
| Caregivers providing support | 121 | 67 | ||
| Hours/week | 8.8 (17.17) | 9.6 (14.22) | ||
| Support score | 14.3 (12.86) | 10.7 (9.29) | ||
aData on sex missing for 2 caregivers.
Determinants of caregivers’ support
The significant determinants of the amount of care provided were, in ranked order of importance, low patient’s functional ability, low received municipal social service support, close relationship to the patient, low MMSE, short distance to patient’s home, and patient sex. Male patients received more informal care than female patients, support score 15.5 versus 11.5 (P < 0.005).
The support score increased from a mean of 8 among independent patients to 16 among those partly or totally dependent (data not shown). Members of the patient’s household provided most support. The most frequent caregivers were, in ranked order, spouses, children, neighbours, grandchildren, and others. In contrast, patient’s age, and caregiver’s age had no significant effects during the post-stroke year (Table II). Support score decreased with an insignificant 5% per measurement occasion.
Table II.
Effects of potential determinants on amount of care provided by informal caregivers, estimated in multiple linear regression analysis. The t value is a measure of independent factor impact on amount of care provided.
| Factor | Estimate | SD | t value | P |
| Functional ability, Katz score | 10.16 | 0.8 | 12.97 | <0.0001 |
| Municipal social service support, h/week | –0.09 | 0.0 | –9.11 | <0.0001 |
| Relationship to patienta | –0.90 | 0.3 | –3.08 | 0.0021 |
| Mini Mental State Examination (MMSE), score | –0.17 | 0.1 | –2.92 | 0.0036 |
| Distance to patient, score | –1.29 | 0.5 | –2.86 | 0.0044 |
| Patient’s sex | 1.63 | 0.8 | 2.01 | 0.0445 |
| Measurement occasion (time) during follow-up | –0.05 | 0.1 | –0.59 | 0.5524 |
| Patient’s age, years | 0.03 | 0.1 | 0.49 | 0.6275 |
| Caregiver’s age, years | –0.01 | 0.0 | –0.37 | 0.7118 |
a1 = spouse, 2 = children, 3 = neighbours, 4 = grandchildren, 5 = others.
Caregiver burden
Mean CB score was 14.9 (SD 12.90, median 11, range 0–55). The potential determinants, estimated in multiple regression analysis were, in ranked order of importance, amount of informal caregiver support, small amount of municipal social service support, close relationship to the patient, MMSE, and patient age, all significant; while patient’s sex, distance to patient’s home, patient functional ability, and caregiver’s age had no significant effects (Table III). CB score decreased with an insignificant 3% per measurement occasion across the follow-up year.
Table III.
Effects of potential determinants of Caregiver Burden Scale estimated by multiple linear regression analysis. The t value is a measure of independent factor impact on amount of care provided.
| Estimate | SD | t value | P | |
| Informal caregiver support, h/week | 0.44 | 0.0 | 10.06 | <0.0001 |
| Municipal social service support, h/week | 6.02 | 1.1 | 5.41 | <0.0001 |
| Relationship to patienta | –1.29 | 0.3 | –3.86 | 0.0001 |
| Mini Mental State Examination (MMSE), score | –0.18 | 0.1 | –2.71 | 0.0070 |
| Patient’s age, years | –0.20 | 0.1 | –2.41 | 0.0163 |
| Patient’s sex | 1.64 | 0.9 | 1.79 | 0.0746 |
| Distance to patient, score | 0.63 | 0.5 | 1.25 | 0.2114 |
| Functional ability, Katz score | 0.90 | 0.8 | 1.16 | 0.2452 |
| Caregiver’s age, years | –0.03 | 0.0 | –0.70 | 0.4854 |
| Measurement occasion (time) during follow-up | –0.03 | 0.1 | –0.31 | 0.7588 |
a1 = spouse, 2 = children, 3 = neighbours, 4 = grandchildren, 5 = others.
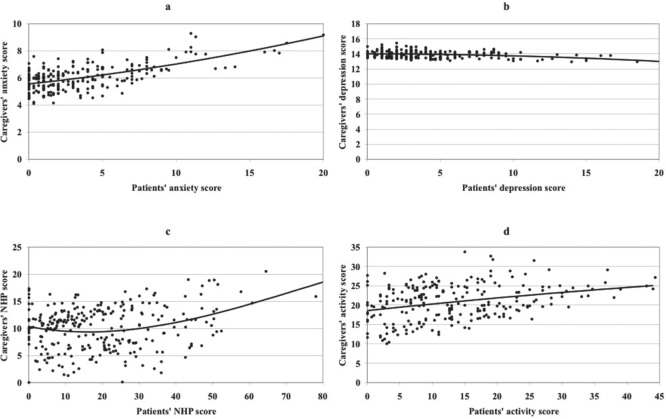
Parallel between caregivers’ and patients’ situation
On average, the caregivers had higher HAD anxiety scores than the patients (6.0 versus 3.5), higher depression scores (13.9 versus 4.1), and higher GQL activity scores (20.8 versus 13.7), while the patients had higher levels in all NHP dimensions (17.4 versus 7.4). Associations between patients’ and caregivers’ scores are shown in Figure 2, where dots represent crude data and solid lines represent splined (smoothed) data. There was a statistically significant positive relationship between patients’ and informal caregivers’ HAD anxiety scores (Figure 2a, P < 0.0001), NHP scores (Figure 2c, P < 0.0001), and activity score (Figure 2d, P < 0.0001). Regarding the HAD depression subscale (Figure 2b) there was a non-significant negative trend towards a relationship (P = 0.37). All these associations or absence of associations were stable over time.
Figure 2.
Associations between caregivers’ and patients’ reported anxiety (a) and depression (b) scores, both based on the Hospital Anxiety and Depression scale, the total Nottingham Health Profile score (c), and the Gothenburg Quality of Life activity score (d). All associations were adjusted for caregivers’ age and distance from caregivers’ home to patients’ home. Dots represent crude data, and solid lines represent splined (smoothed) data.
Non-participant analysis
To estimate selection effects, the distributions of age, sex, MMSE, functional ability, self-rated health, living alone, living in assisted accommodation or nursing home, and municipal social service support among patients with responding informal caregivers (referents) were compared with the corresponding data among patients with non-responding informal caregivers (non-participant group 1) and those who had no informal caregiver or who did not want to ‘bother’ their caregivers (non-participant group 2).
The only significant differences found were that group 2 had a higher proportion of women, were living alone to a larger extent, and had more municipal service support than patients and group 1, and those in group 1 were living in their own home to a lesser extent than patients and group 2. All these differences were significant but only marginally so.
Discussion
Informal caregivers provided a substantial amount of care, on average 11 hours per week. Variables affecting the amount of care given were the patient’s functional ability, municipal social services support, relationship to the patient, MMSE, distance to patient’s home, and patient’s sex. Determinants for caregiver burden score were amount of informal caregiver support given, amount of municipal social service support given, relationship to the patient, MMSE, and patient age. Significant associations between informal caregiver and patient responses (dyad responses) were found for HAD anxiety, total NHP, and GQL activity scale. The strengths of this observational study of stroke patients were that the study population included all patients in the area who fulfilled the inclusion criteria and who survived the acute stroke phase, representing more than 80% of the total stroke population during the recruitment period (17). The data were collected with validity-tested instruments. The longitudinal study design and the repeated measurements allowed for a comprehensive assessment of the effects across time. In addition, both patients and caregivers responded to largely the same questions within the same time frame.
The limitations of this study include a possible difficulty for the informal caregivers to distinguish between activities regularly undertaken for the whole household and specific activities which the patient was incapable of performing. Another possible limitation may have been that many items were based on recall and that the cognitive function of the patients may have been too impaired to provide adequate responses. However, 64% of the patients had an MMSE score of 24 or higher. Moreover, in interviews with subjects with low cognitive function an informal caregiver was usually present and provided additional information. For this reason the bias owing to impaired cognitive function was probably small. A further possible limitation may have been that information on medical history, continence, mental illness, and other factors affecting self-sufficiency were not at hand. However, the Katz index, intended to be a measure of independence, is a more direct measure of all factors affecting self-sufficiency and was used in this study.
Informal caregivers increased their support to the patients to a large extent after as compared with before the stroke, both in terms of time and the amount of care-giving tasks. In the present study the amount of informal care-giving increased with low patient’s functional ability, small received municipality social service support, close relationship to the patient, low MMSE, short distance to patient’s home, and patient’s sex. The support amount and the determinants stayed constant across time. McCullagh et al. (6) reported decreasing anxiety levels and caregiver burdens over time, in spite of the fact that there were no considerable changes in patients’ dependence or support levels, indicating that these changes might represent a response shift toward normalization over time.
Some researchers have reported defined aspects of patient characteristics that affect caregivers (11,27–29), while others did not find any specific relationship (10). We found that the amount of support given by the caregiver, amount of municipal social service support, relationship to the patient, MMSE, and patient age all significantly increased the caregiver burden, and the relationships to caregiver burden were constant across time.
In the present study informal caregivers had significantly higher anxiety as well as depression HAD scores than the patients. Kotila et al. (30) found that the frequency and severity of depression was similar between patients and caregivers. Others found that caregivers’ emotional outcome was associated with the stroke patients’ emotional status (27–29). Still others have shown that the patient may in some respects adapt more easily to the new situation than the caregiver (31,32), and the interaction between patients’ impairments and caregivers’ emotional health may be different at different phases post-stroke (33). In the present study, the mean ages for the stroke patients and their informal caregivers were 78 years and 63 years, respectively. This may affect the results because some of them were living together in own apartment, and others were living separately because the stroke survivor moved into a nursing home. In addition, the patients’ multi-morbidity may have an impact on the informal caregivers’ depression. Kalra et al. (1) found that a caregiver training programme reduced perceived caregiver burden, and both patients and caregivers reported less anxiety and depression, and had higher quality of life, one year after baseline.
In the present study significant associations between caregiver and patient responses were found for the HAD subscale anxiety, all NHP subscales, and all the activity subscales in GQL, constant across time. It is a common assumption that patients influence their caregiver’s health and well-being (10,11,27,28), although the reverse may also be possible, i.e. family problems may have an effect on the stroke patient’s recovery (28,29). It has been found that informal caregiver depression may worsen the depression in a patient and predict poor response to rehabilitation (34). A dyadic perspective may add to our understanding of the reciprocal influences between the stroke survivor and the caregiver (35). Long-term follow-up for stroke survivors should include identification and assessment of vulnerable caregivers (15).
In many respects, Swedish stroke care has improved. This applies in particular to access to care in stroke units, and medical treatment in the acute phase (3). However, there are still shortcomings in care after discharge from hospital. A large proportion of the patients feel they receive insufficient support from the health care sector and the municipality (3), indicating that the problem area dealt with in this report prevails.
In conclusion, time spent and amount of care given by informal caregivers increased significantly after hospital discharge as compared with before admission, and remained high during the first post-stroke year. The informal caregivers were under considerable strain as indicated by the caregiver burden and anxiety and depression scores. There was an association within the dyads regarding anxiety (HAD), health profile (NHP), and leisure time activity (GQL). A caregiver training programme might be part of a possible solution to these problems.
Acknowledgments
Funding: This study was supported by grants from the Vårdal Foundation (V98-401), Centre for Clinical Research Dalarna, the Dalarna County Council, and Uppsala University.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. None of the funders had any influence of the content of this paper.
References
- 1.Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, et al. . Training carers of stroke patients: randomised controlled trial. BMJ. 2004;328:1099–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jegermalm M, Jeppsson Grassman E. Patterns of informal help and caregiving in Sweden: A thirteen-year perspective. Social Policy Admin. 2009;43:681–701. [Google Scholar]
- 3.The Board of Directors of the National Stroke Register Stroke och TIA. Rapport från Riks-stroke 2013 [Stroke and TIA. Report of the national stroke register for the year 2013]. Available from http://www.riksstroke.org/wp-content/uploads/2014/07/Strokerapport_AKUTTIA3man_LR.pdf [Last accessed 2014. [Google Scholar]
- 4.Blake H, Lincoln NB, Clarke DD. Caregiver strain in spouses of stroke patients. Clin Rehabil. 2003;17:312–17. [DOI] [PubMed] [Google Scholar]
- 5.Low JT, Payne S, Roderick P. The impact of stroke on informal carers: a literature review. Soc Sci Med. 1999;49:711–25. [DOI] [PubMed] [Google Scholar]
- 6.McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36:2181–6. [DOI] [PubMed] [Google Scholar]
- 7.White CL, Mayo N, Hanley JA, Wood-Dauphinee S. Evolution of the caregiving experience in the initial 2 years following stroke. Res Nurs Health. 2003;26:177–89. [DOI] [PubMed] [Google Scholar]
- 8.Carlsson GE, Forsberg-Warleby G, Moller A, Blomstrand C. Comparison of life satisfaction within couples one year after a partner’s stroke. J Rehabil Med. 2007;39:219–24. [DOI] [PubMed] [Google Scholar]
- 9.Simon C, Kumar S, Kendrick T. Formal support of stroke survivors and their informal carers in the community: a cohort study. Health Soc Care Community. 2008;16:582–92. [DOI] [PubMed] [Google Scholar]
- 10.Anderson CS, Linto J, Stewart-Wynne EG. A population-based assessment of the impact and burden of caregiving for long-term stroke survivors. Stroke. 1995;26:843–9. [DOI] [PubMed] [Google Scholar]
- 11.Elmstahl S, Malmberg B, Annerstedt L. Caregiver’s burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch Phys Med Rehabil. 1996;77:177–82. [DOI] [PubMed] [Google Scholar]
- 12.Tooth L, McKenna K, Barnett A, Prescott C, Murphy S. Caregiver burden, time spent caring and health status in the first 12 months following stroke. Brain Inj. 2005;19:963–74. [DOI] [PubMed] [Google Scholar]
- 13.Vincent C, Desrosiers J, Landreville P, Demers L. Burden of caregivers of people with stroke: evolution and predictors. Cerebrovasc Dis. 2009;27:456–64. [DOI] [PubMed] [Google Scholar]
- 14.Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: perspectives from caregiver and receiver. J Gerontol B Psychol Sci Soc Sci. 2002;57:195–204. [DOI] [PubMed] [Google Scholar]
- 15.Rigby H, Gubitz G, Phillips S. A systematic review of caregiver burden following stroke. Int J Stroke. 2009;4:285–92. [DOI] [PubMed] [Google Scholar]
- 16.Olai L, Omne-Ponten M, Borgquist L, Svardsudd K. Prognosis assessment in stroke patients at discharge from hospital. Age Ageing. 2007;36:184–9. [DOI] [PubMed] [Google Scholar]
- 17.Olai L, Omne-Ponten M, Borgquist L, Svardsudd K. Survival, hazard function for a new event, and healthcare utilization among stroke patients >or=65 years. Stroke. 2009;40:3585–90. [DOI] [PubMed] [Google Scholar]
- 18.Olai L, Borgquist L, Svardsudd K. Health problems in elderly patients during the first post-stroke year. Ups J Med Sci. 2012;117:318–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asplund K, Bonita R, Kuulasmaa K, Rajakangas AM, Schaedlich H, Suzuki K, et al. . Multinational comparisons of stroke epidemiology. Evaluation of case ascertainment in the WHO MONICA Stroke Study. World health organization monitoring trends and determinants in cardiovascular disease. Stroke. 1995;26:355–60. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization International Classification of Diseases (ICD). Tenth Revision ICD10. WHO, Geneva, 1992. [Google Scholar]
- 21.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–19. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 23.Hunt SM, McEwen J, McKenna SP. Measuring health status: a new tool for clinicians and epidemiologists. J R Coll Gen Pract. 1985;35:185–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- 25.Tibblin G, Tibblin B, Peciva S, Kullman S, Svärdsudd K. ‘The Göteborg quality of life instrument’--an assessment of well-being and symptoms among men born 1913 and 1923. Methods and validity. Scand J Prim Health Care Suppl. 1990;1:33–8. [PubMed] [Google Scholar]
- 26.Statistical Analysis System: SAS Institute Inc SAS Campus Drive, Cary, NC 1995 [database on the internet]. Available from http://www.sas.com/technologies/analytics/statistics/stat/factsheet.pdf [Last accessed 29 March 2015. [Google Scholar]
- 27.Wade DT, Legh-Smith J, Hewer RL. Effects of living with and looking after survivors of a stroke. Br Med J. 1986;293:418–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dennis M, O’Rourke S, Lewis S, Sharpe M, Warlow C. A quantitative study of the emotional outcome of people caring for stroke survivors. Stroke. 1998;29:1867–72. [DOI] [PubMed] [Google Scholar]
- 29.Carnwath TC, Johnson DA. Psychiatric morbidity among spouses of patients with stroke. Br Med J. 1987;294:409–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kotila M, Numminen H, Waltimo O, Kaste M. Depression after stroke: results of the FINNSTROKE Study. Stroke. 1998;29:368–72. [DOI] [PubMed] [Google Scholar]
- 31.Jönsson AC, Lindgren I, Hallström B, Norrving B, Lindgren A. Determinants of quality of life in stroke survivors and their informal caregivers. Stroke. 2005;36:803–8. [DOI] [PubMed] [Google Scholar]
- 32.Gosman-Hedström G, Claesson L, Blomstrand C. Consequences of severity at stroke onset for health-related quality of life (HRQL) and informal care: a 1-year follow-up in elderly stroke survivors. Arch Gerontol Geriatr. 2008;47:79–91. [DOI] [PubMed] [Google Scholar]
- 33.Forsberg-Wärleby G, Moller A, Blomstrand C. Psychological well-being of spouses of stroke patients during the first year after stroke. Clin Rehabil. 2004;18:430–7. [DOI] [PubMed] [Google Scholar]
- 34.van Heugten C, Visser-Meily A, Post M, Lindeman E. Care for carers of stroke patients: evidence-based clinical practice guidelines. J Rehabil Med. 2006;38:153–8. [DOI] [PubMed] [Google Scholar]
- 35.Bergstrom AL, Eriksson G, von Koch L, Tham K. Combined life satisfaction of persons with stroke and their caregivers: associations with caregiver burden and the impact of stroke. Health Qual Life Outcomes. 2011;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]