Abstract
Purpose
Copy number alterations have been shown to be involved in melanoma pathogenesis. The randomized, phase III clinical trial E2603: carboplatin, paclitaxel, +/− sorafenib (CP vs. CPS) offers a large collection of tumor samples to evaluate association of somatic mutations, genomic alterations, and clinical outcomes, prior to current FDA approved therapies.
Materials and Methods
Copy number and mutational analysis on 119 pretreatment samples was performed.
Results
CPS therapy was associated with improved PFS compared to CP in patients with tumors with RAF1 (cRAF) gene copy gains (HR=0.372, P=0.025) or CCND1 gene copy gains (HR=0.45, P=0.035). CPS therapy was associated with improved OS compared to CP in patients with tumors with KRAS gene copy gains (HR=0.25, P=0.035). BRAF gene copy gain and MET amplification were more common in samples with V600K vs V600E mutations (P<0.001), which was validated in the TCGA data set.
Conclusion
We observed improved treatment response with CPS in melanoma patients whose tumors have RAF1 (cRAF), KRAS or CCND1 amplification, all of which can be attributed to sorafenib targeting CRAF. These genomic alterations should be incorporated in future studies for evaluation as biomarkers.
Keywords: Carboplatin, Copy Number Changes, Metastatic Melanoma, Paclitaxel, Sorafenib
INTRODUCTION
Despite recent improvements in the treatment of metastatic melanoma, it remains the deadliest form of skin cancer. In addition to tumor specific somatic mutations (e.g. in BRAF, NRAS, KIT), copy number alterations, both gains and losses, are thought to play integral roles in melanoma pathogenesis. Global genomic gain of chromosomes 1, 6p, 7, 17q, and 20 and loss of chromosomes 4, 6q, 9, 10, 11, 13, 16, and 18 have been observed 1-10. Gains of chromosome 7 and loss of chromosome 10 have been associated with melanomas with BRAF mutations, whereas loss of chromosome 11 has been associated with melanomas with NRAS mutations 3,6,8,9. Furthermore, a number of treatment options have been FDA approved in recent years, including both immunotherapies and targeted therapies. However, there is still a need to identify effective mechanisms to stratify patients to optimize treatment decision and improve clinical outcomes with many studies evaluating the use of biomarkers in the selection of patients for appropriate therapies. Despite the expansion of correlative studies, currently most cannot discriminate between the identification of predictive or prognostic biomarkers. In part, this issue is due to significant advances both in technologies since natural history studies were done, and revolutionary changes in therapies 11,12.
Prior to the development of the targeted mutant BRAF inhibitors, vemurafenib (Zelboraf, Genentch) and dabrafenib (Tafinlar, GlaxoSmithKline) 13,14, sorafenib was used in clinical trials in order to attempt to inhibit the MAPK signaling pathway and target angiogenesis. Sorafenib (Nexavar, Bayer Pharmaceuticals) is an oral multikinase inhibitor, including RAF kinases, BRAF and CRAF 15-17, approved by the U.S. Food and Drug Administration (FDA) for the treatment of renal cell carcinoma, hepatocellular carcinoma, and thyroid cancer 18-21. E2603 was a randomized phase III clinical trial investigating carboplatin, paclitaxel, +/− sorafenib in advanced stage melanoma patients, and demonstrated no difference in clinical outcome with the addition of sorafenib to chemotherapy in unselected melanoma populations 22-24. However, our recent observations suggest that melanoma patients whose tumors carry NRAS mutations may benefit from targeting CRAF. Patients with NRAS mutant melanoma with chemotherapy alone had poorer responses as compared to patients with BRAF mutant and WT melanoma, and the addition of sorafenib to chemotherapy improved treatment responses to a level similar to those observed in patients with BRAF mutant and WT melanoma in E2603 25.
In the current study, we used pretreatment tumor samples from patients enrolled on E2603 to explore whether copy number alterations were associated with somatic mutations and clinical outcome in patients with melanoma. E2603 provides a large, clinically annotated dataset, treated prior to the current FDA approved therapies, which can be used to evaluate associations with clinical outcome and discriminate between predictive and prognostic biomarkers for melanoma.
MATERIALS AND METHODS
Patients
Patients were enrolled on the double-blind phase III ECOG 2603 clinical trial and randomized to receive carboplatin/paclitaxel (CP, control arm) or carboplatin/paclitaxel plus sorafenib (CPS, experimental arm) as detailed in Flaherty et al 22. Dosing was carboplatin at area under the curve (AUC) of 6 and paclitaxel at 225 mg/m2 every three weeks, and sorafenib at 400mg orally twice daily for days 2-19 of every 21-day cycle. Trial enrollment required confirmed diagnosis of unresectable or metastatic melanoma, excluding uveal melanoma and patients with brain metastases. Eligibility criteria also included age greater than 18, ECOG performance status (PS) of 0 or 1, measurable disease, and normal baseline laboratory studies. Patient demographics, disease characteristics, and treatment history were all documented including disease stage, primary tumor site, numbers of involved sites, age at diagnosis, ECOG PS, Breslow thickness, ulceration, and lactate dehydrogenase (LDH).
Melanoma tumor samples and Tumor genotyping
Tumor samples from patients enrolled on E2603 were genotyped as described in Wilson et al 25. From the 179 tumor samples which were genotyped, 20 samples had inadequate DNA to undergo labeling and 40 samples failed multiple attempts at labeling, most likely due to decreased DNA integrity or inhibition of the reaction by melanin. In total, 119 tumor samples were labeled and underwent copy number analysis.
Copy number and genomic instability analysis
Tumor DNA was labeled using BioPrime® Array CGH Genomic Labeling System (Life Technologies, Grand Island, NY) according to manufacturer's instructions. Array-based comparative genomic hybridization (aCGH) and data analysis was performed as in 26 using the Agilent SurePrint G3 Human CGH 2×400K M microarrays following manufacturer's instructions. Extracted data were analyzed using BioDiscovery's Nexus 7 copy-number software (Nexus Genomics Inc.). Copy number variation was assessed using Nexus 7 and gene mapping was done to hg19, Feb 2009 build. Copy number gain was defined as log2 scale value > 0.3 and loss as log2 scale value < − 0.3, with at least three contiguous probes needed to call a gain or loss. High copy gains were defined as log2 scale value > 1.14, and homozygous loss as log2 scale value < −1.1. We measured genomic instability as the number of non-diploid copy number changes in each tumor sample. BRAF and MET mutation and copy number data were downloaded from the public TCGA data repository website of the Broad Institute (http://gdac.broadinstitute.org). We used Level 4 GISTIC copy number data in the analysis.
Statistical analysis
Along with analysis of global copy number gains and losses, copy number changes of 26 genes (Supplemental Table 1) known to be involved in melanoma pathogenesis were analyzed, and correlation between gene copy number gains and losses and outcomes were performed. Statistical analysis was performed as in Wilson et al 25. The Fisher's exact test was used to compare gene CNV by patients’ demographic and disease characteristics.. Kaplan-Meier methods were used to estimate the distribution of OS and PFS. Cox proportional hazards models were used to test prognostic and predictive value of CNV for each gene. The same set of covariates were adjusted in all multivariable Cox models, including age, gender, race, AJCC stage, ECOG PS, prior therapy, number of involved sites, and LDH. Pearson's Chi-squared tests were used to analyze TCGA BRAF and MET copy number data. Due to the exploratory nature of the study, no adjustment was made for multiple comparisons. All tests were two-sided and p<0.05 was considered statistically significant. All analysis was conducted using STATA 11.2 27.
RESULTS
Overall copy number analysis
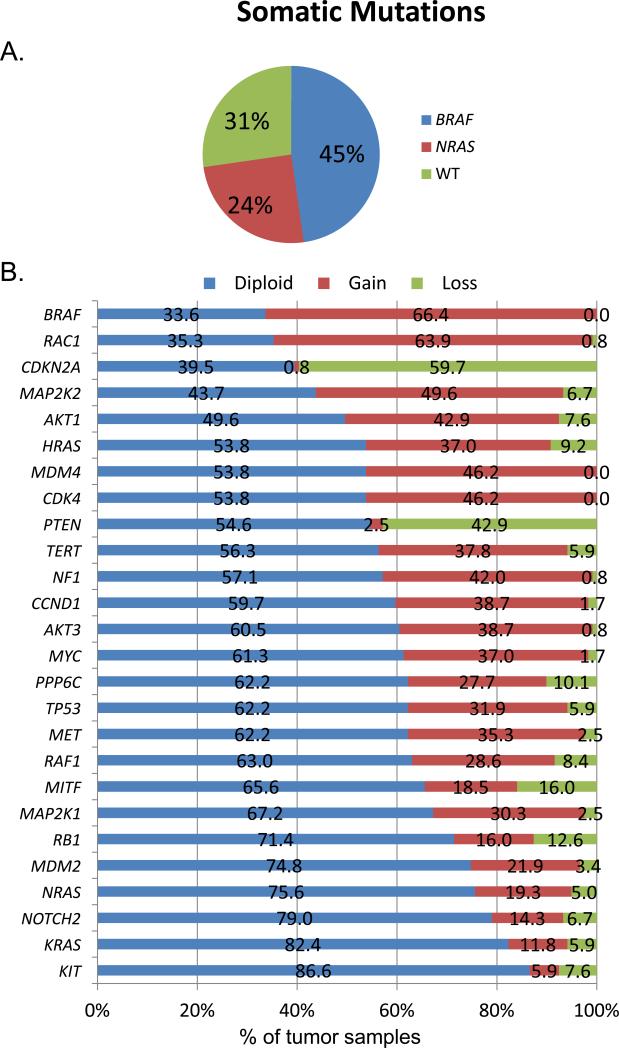
One hundred and nineteen pretreatment tumor samples from patients on E2603 had sufficient tumor tissue for CNV analysis for 26 genes via aCGH. The demographics and disease characteristics of the 119 patients were similar to those patients who did not have DNA samples available for or who failed aCGH analysis (Supplemental Table 2). Moreover, no differences were observed in clinical outcomes in patients with samples for analysis and those without (Supplemental Table 3). As no difference was seen in the overall outcome of the study, treatment arms were collapsed for analysis about prognostic markers. In these 119 tumor samples, 45% (54/119) had BRAF mutations, 24% (28/119) had NRAS mutations, and 31% (37/119) had neither, designated as WT (Figure 1A), consistent with the entire sample set from E2603 (Wilson, Zhao et al. 2014), as well as many other genetic studies of melanoma 28-30.
Figure 1. Somatic Mutations and Copy Number Changes in Melanoma Tumor Samples.
A. Genotype of melanoma tumor samples evaluated using array Comparative Genomic Hybridization (aCGH). WT – wildtype.
B. Aggregate copy numbers of specified genes in melanoma tumor samples. The genes evaluated are listed on the left and the legend, shown on the top, depicts copy number status, demonstrating diploid, gain, or loss, in tumor samples. Numbers represent percentage of tumors with indicated copy numbers.
Genomic alterations were evaluated in all tumor samples and frequency of copy gains and losses across the entire genome were identified (Supplemental Figure 1). We observed global genomic gain of chromosomes 1, 6p, 7, 17q, and 20 and loss of chromosomes 4, 6q, 9, 10, 11, 13, 16, and 18. Genomic instability was also assessed in all tumor samples, but no correlation was identified between genomic instability (non-diploid genome) and patient characteristics, treatment arms, or clinical outcomes (data not shown). As has been previously reported 1-10, we identified regions throughout the genome which demonstrated similar copy gains and copy losses in all melanoma tumor samples (e.g. chromosomes 1 and 6). We also observed genomic regions which exhibited differences in copy gains and losses in tumor samples stratified by somatic mutation cohorts, such as chromosome 7.
We next evaluated copy gains and losses in an initial set of 26 genes known to be involved in melanoma pathogenesis (Figure 1B). BRAF, CDK4, and MDM4 were found exclusively either as being diploid or copy gains. Conversely, the tumor suppressors, CDKN2A and PTEN, were identified mainly either as diploid or having copy loss, with rare copy gains identified. CDK4 copy number gain was more frequent in tumor samples with BRAF mutation (31/54, 57.4%) compared to tumors with NRAS mutation (9/28, 32.1%) or WT (15/37, 40.5%) (P=0.066). Moreover, PTEN copy number loss was more frequent in tumor samples with BRAF (28/54, 51.9%) and NRAS (13/28, 46.4%) mutations compared to WT (10/37, 27.0%) (P=0.051). These comparisons did not reach statistical significance due to small sample size.
Association of BRAF amplification with BRAF somatic mutations and clinical outcome
We observed gains of chromosome 7, most notably in the region around BRAF (7q34); BRAF gene amplification was present in 66% of the tumor samples (Figure 1B). In tumor samples with BRAF mutations, 82% had BRAF copy gains, compared to 64% of samples with NRAS mutations or 46% of samples that were WT (P=0.002) (Supplemental Table 4). Using Kaplan-Meier analysis in all samples, the presence of BRAF amplification was significantly associated with decreased PFS (median PFS 6.3 vs. 3.9 months for BRAF diploid and copy gain, logrank P=0.023) and OS (median OS 11.0 vs. 8.5 months respectively, logrank P=0.046) (Figure 2A and 2B), regardless of BRAF mutation status. The associations were no longer statistically significant after adjusting for patient characteristics in Cox models (HR=1.52, 95% CI: 0.97, 2.37, P=0.067 for PFS, HR=1.16, 95% CI: 0.73, 1.86, P=0.53 for OS).
Figure 2. BRAF gene amplification is associated with somatic mutations and worse clinical outcomes.
Kaplan-Meier curves of progression free survival (PFS) (A) and overall survival (OS) (B) based on BRAF gene copy number status, diploid versus copy gain. Median PFS for BRAF diploid and copy gain, 6.3 (95% CI: 3.0, 8.8) months and 3.9 (95% CI: 2.6, 5.3) months (P=0.023), respectively (A). Median OS for BRAF diploid and copy gain, 11.0 (95% CI: 8.8, 18.4) months and 8.5 (95% CI: 7.3, 10.4) months (P=0.046), respectively (B).
Copy number aberrations associated with response to sorafenib
Twenty-six pre-selected genes known to play a role in melanomagenesis were evaluated individually for their predictive values to explore whether sorafenib could provide survival benefit in any subgroups. In patients with KRAS copy gain, CPS was associated with better OS compared to CP (adjusted HR=0.25, 95% CI:0.07, 0.91, P=0.035) (Figure 3 A and B). In patients with CCND1 or RAF1 copy gain, CPS was associated with better PFS compared to CP (CCND1: adjusted HR=0.45, 95% CI:0.22, 0.95, P=0.035 (Figure 3 C and D), RAF1: adjusted HR=0.37, 95% CI: 0.16, 0.88, P=0.025 (Figure 3 E and F) . Figure 3 demonstrates the altered outcomes associated with copy number changes of KRAS, CCND1 and RAF1 in each treatment arm. For all three genes, patients whose tumors carried copy gains had worsened outcomes on CP treatment, but improved outcomes with CPS treatment. Results from copy number changes in remaining genes did not identify significant alterations in PFS or in outcomes in response to treatment arms (data not shown).
Figure 3. Association of gene copy number changes in treatment arms.
Adjusted survival curves from Cox models for gene copy number changes in each treatment arm. Gene copy changes are KRAS (A, B), CCND1 (C,D), and RAF1 (cRAF) (E,F). Adjusted covariates include age, gender, race,AJCC status, ECOG performance status, prior treatment, number of involved sites and LDH. CP – carboplatin and paclitaxel; CPS – carboplatin, paclitaxel, and sorafenib.
RAF1 was found to be amplified in 29% of tumor samples (Figure 1B) and RAF1 amplification was associated with worse performance status (PS) compared to diploid or copy loss (p=0.002) (Supplemental Table 5). We recently demonstrated a trend towards improved response with the addition of sorafenib to carboplatin and paclitaxel in patients with NRAS mutant melanoma 25. Therefore, we performed a conjoined analysis of NRAS somatic mutation status and RAF1 (cRAF) copy gain. We evaluated the effect of NRAS somatic mutations, RAF1 copy gains, both, or neither on PFS and OS. Our results demonstrate that there is no significant association of these variables, either alone or in combination, on PFS or OS, independent of treatment arm (Supplemental Figure 2). In patients without a NRAS mutation, RAF1 copy gain remained predictive of improved response to treatment with CPS compared to CP (N=90, HR=0.27, p=0.018). In patients with a NRAS mutation, RAF1 copy gain was no longer statistically significantly predicting response to CPS treatment, however, the sample size was small (N=25, HR=0.43, 95% CI:0.03, 6.04, p=0.532). We did not observe a correlation between RAF1 amplification and NRAS mutations in our sample set, which is confirmed in TCGA melanoma data as well (www.cbioportal.org).
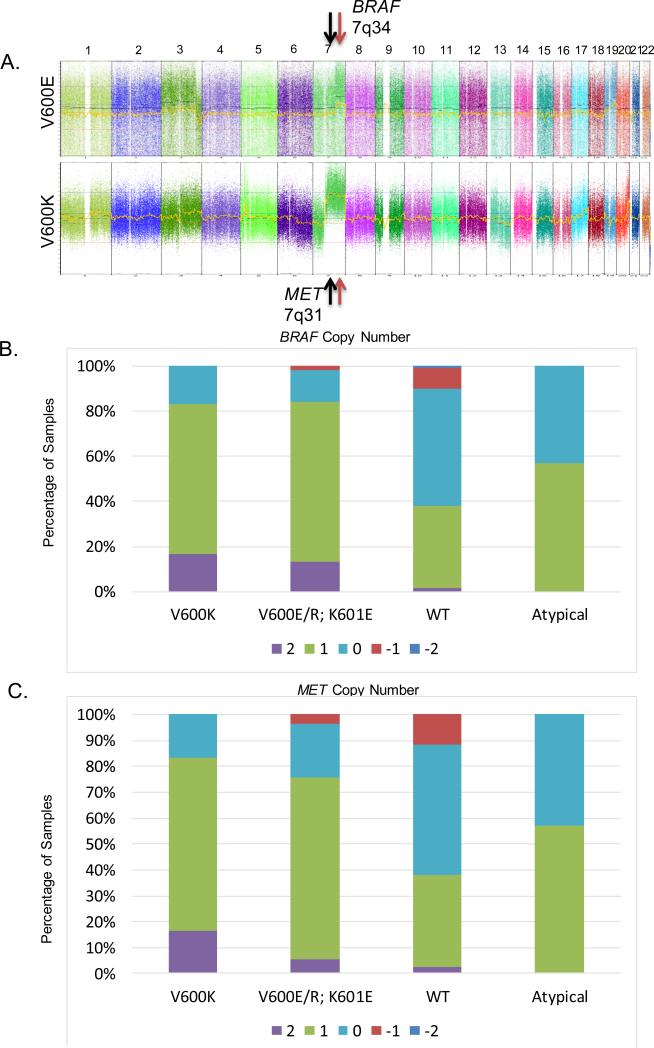
Associations with BRAF V600K tumor samples
During our analysis of copy number changes within the genome and specific genes of interest, we noted differences between the subsets of tumor samples with the BRAF V600E and V600K mutations. We observed a focal amplification of 7q34 in tumor samples with V600E mutations; however, we noted a more global amplification pattern along the q-arm in tumor samples with V600K mutations (Figure 4A). Thus, we further evaluated copy number changes in association with specific BRAF V600 mutations. We found that the BRAF gene was amplified in all BRAF somatic mutation cohorts, but amplification was greater in samples with V600K vs V600E mutations (p<0.001) (Supplemental Figure 3A). Given our observation, we did a global analysis of copy number changes and identified an increase in copy gains of MET, another gene located on chromosome 7 (7q31) in tumor samples with BRAF somatic mutations (59%) compared to NRAS somatic mutations (29%) and WT (38%) (P=0.03). Additionally, although MET was found to be amplified in both V600E and V600K mutation cohorts, we found a 2-fold increase in amplification in V600K vs. V600E (p<0.05) (Supplemental Figure 3B).
Figure 4. BRAF and MET gene amplifications are associated with BRAF V600K mutation cohort.
A. Representative plots of copy gains and losses in tumor samples with BRAF V600E and BRAF V600K mutations. BRAF and MET genomic locations are denoted with arrows. Numbers across the top designate chromosomes.
B. BRAF copy number from TCGA data in designated somatic mutation cohorts. X-axis, Designated somatic mutation cohorts. Y-axis, percentage of samples. Legend designates GISTIC copy number (CN) where +2 is high level copy gain, +1 is copy gain, 0 is diploid, −1 is copy loss, and −2 is homozygous loss.
C. MET copy number from TCGA data in designated somatic mutation cohorts. X-axis, Designated somatic mutation cohorts. Y-axis, percentage of samples. Legend designates GISTIC copy number (CN) where +2 is high level copy gain, +1 is copy gain, 0 is diploid, −1 is copy loss, and −2 is homozygous loss.
We then independently validated our finding using data from the cutaneous melanoma TCGA. We found that BRAF CN (GISTIC +2) levels were higher in BRAF V600K (17%) compared to V600E/R or K601E (13%), atypical mutants (0%) or wild-type (2%) samples (P=0.002) (Figure 4B). We demonstrated differential MET amplification in somatic mutation cohorts with copy gains observed in 76% of BRAF mutant, 27% of NRAS mutant, and 51% of WT melanoma tumor samples (P=0.003). Furthermore, MET copy gains were increased in V600K samples, as compared to V600E. It was observed that MET CN (GISTIC +2) levels are higher in BRAF V600K (17%) compared to V600E/R or K601E (6%), atypical mutants (0%) or wild-type (2%) samples (P=0.075) (Figure 4C).
DISCUSSION
We investigated the association between copy number alterations, point mutations and clinical outcome in melanoma patients treated on the E2603 randomized, phase III clinical trial of carboplatin, paclitaxel, +/− sorafenib. Copy number alterations were identified across the entire genome in the melanoma tumor samples. Similar copy gains in chromosome 1 and 6p and loss in chromosome 6q were observed in all tumor samples, although differential copy gains of chromosomes 7, 8, and 17 and copy loss of chromosome 10 were seen associated with specific somatic mutation sub-sets. As in other studies, which primarily analyzed copy number in melanoma cell lines and a small number of tumor samples, we observed global genomic gain of chromosomes 1, 6p, 7, 17q, and 20 and loss of chromosomes 4, 6q, 9, 10, 11, 13, 16, and 18 2,3,5,6,8-10. In addition, we observed a similar rate of copy number changes of individual genes including, amplifications of BRAF, CCND1, CDK4, MDM2, and MET and deletions of CDKN2A and PTEN, as well as copy number changes in additional genes including AKT1, MAP2K2, RAC1 and RAF1 3,8,10. Our results did not identify significant amplifications in NOTCH2, as were previously identified 3,8 nor global changes associated with chromosomes 8q34 and11q13 4. Gains at 8q34 and 11q13 were previously identified using fluorescence in situ hybridization probes specific for genes encoded at these loci which can account for the differences in observations. We also detected specific copy number changes specific to the different somatic mutation cohorts, which have been previously observed, including gain on chromosome 7 and loss on chromosome 10q as more frequent in tumor samples with BRAF mutations 3,6,9 and loss on chromosome 11q was more frequent in tumor samples with NRAS mutation 6,9. Our study results provide information regarding genetic alterations in a large collection of melanoma tumor samples, adding to prior work evaluating genetic aberrations identified in melanoma cell lines.
We observed that BRAF copy number gain, regardless of mutation status, was associated with worsened clinical outcomes, with decreased PFS and OS in patients, as determined by univariate analysis, although this association was no longer statistically significant in multivariate analysis. Acquisition of BRAF amplification at varying levels of copy gain (between 3-75) have recently been identified to play a role in treatment resistance to BRAF and MEK inhibitors, either alone or in combination, in melanoma 1,31-33. Additionally, copy number gains of BRAF have been shown to be associated with decreased response to BRAF inhibition 26. Thus, it has been postulated that copy gain of BRAF is a predictive marker (i.e. intrinsic copy gain or acquired amplification is associated with response to BRAF inhibition). Our data suggest that BRAF copy gain may predict for poor clinical outcome as compared to diploid. It may be that some of the prior studies suggesting that BRAF copy number gain is predictive of outcome upon treatment with BRAF inhibition were uncovering a prognostic association that was not well delineated prior to the era of BRAF targeted therapy. With advances in technology and increased attention to BRAF amplification as potential biomarker of response, we are now able to make this observation. However, this finding should not be taken to imply that high level BRAF amplification, acquired upon treatment with BRAF inhibition, is not associated with resistance to therapy 1.
We found differential amplification of the BRAF gene, with increased copy gains associated with V600K mutations, as compared to V600E mutations. We also observed an association between the BRAF V600K mutation and amplification of MET, located proximal to BRAF on chromosome 7. Both associations were validated in the TCGA data set, which shows the same pattern of increased amplification of BRAF V600K mutations, which also correlates with MET amplification. It is known that BRAF V600K mutations occur in older patients and in patients with chronic sun damage 30, which we also observed in our recent analysis of this E2603 patient cohort 25. Although our sample set was too small to formally evaluate an association between V600K mutations and genomic instability, prior data suggest that V600K mutations may be associated with more chromosomal abnormalities 29,34. Amplification of MET may be associated with treatment resistance to BRAF inhibitors, or the combination of BRAF and MEK inhibitors, particularly since studies have demonstrated that the HGF/MET pathway has been implicated in the development of treatment resistance to BRAF inhibitors 35,36, as well as in lung cancer 37,38.
Our data suggest that RAF1 copy number gain, independent of NRAS mutation status, is predictive of benefit from treatment with CPS. We found that RAF1 was amplified in 29% of our samples; in the TCGA cohort, it is gained in 16% of cases (45/278) increasing amplification correlates with increased expression (Pearson correlation 0.67) (cbioportal.org). Increased levels of CRAF lead to upregulation of the MAPK signaling pathway, known to be critically important in melanomagenesis 39. We postulate that the addition of sorafenib, a known CRAF inhibitor 15,16, to chemotherapy targets MAPK signaling resulting from increased levels of CRAF. Not surprisingly, the inhibition of the MAPK signaling pathway through CRAF appears to result in improved PFS. The improved response to treatment with CPS in this patient cohort is consistent with our previous finding that treatment with CPS increased treatment response in melanoma patients whose tumors had a NRAS mutation 25, as NRAS mutants have increased signaling through the MAPK pathway through CRAF. These results are reminiscent of those observed with addition of monoclonal antibodies trastuzimab, in breast cancer with HER2 overexpression 40, and panitumumab, in KRAS wild-type metastatic colorectal cancer 41. In these studies, distinct improvement in PFS and OS was observed in select patient cohorts, despite otherwise poor responses to standard therapies, with the addition of these monoclonal antibodies, respectively. Furthermore, improved OS with CPS treatment was identified in patients with KRAS amplification, which also signals through CRAF, strengthening the importance of CRAF inhibition in select melanoma patient cohorts. In the TCGA database, KRAS has been shown to be altered in 3% of melanoma tumor samples. Although it is unlikely that further clinical investigation will continue with sorafenib as an agent in melanoma, these results suggest that targeting of CRAF in melanoma, as defined by RAS-mutant or RAF1 amplification, may provide alternative treatment options for these select group of patients. As large scale sequencing of tumor samples becomes standard of care, this approach may become more feasible in the near future. Currently, there are ongoing clinical trials investigating pan-RAF inhibitors, as single agents or in combination with MEK inhibitors or alternative pathway inhibitors (www.clinicaltrials.gov). Correlative studies in association with these trials will be critical to identify determinants of response, and we would predict that patients with RAS-mutant or RAF1 amplification would demonstrate improved response upon treatment with these agents. Interestingly, in the TCGA data, 13% of papillary thyroid cancers and 2.6% of liver cancers have RAS mutations. One mechanism by which sorafenib may be effacious in these cancers, may be through inhibition of MAPK signaling through CRAF.
We observed that amplification of CCND1 predicted for improved PFS with treatment with CPS. These results differ from prior studies in melanoma cell lines showing that that Cyclin D1 amplification may contribute to resistance to mutant BRAF inhibitors in melanoma 42. Additionally, recent analyses of patient tumor samples also have identified an association of CCND1 copy number gain and decreased PFS upon treatment with BRAF inhibitors 26. Hweover, prior studies have demonstrated that Cyclin D1 is downregulated by sorafenib. In both hepatocellular carcinoma and prostate cancer cells, sorafenib demonstrated anti-proliferative effects through inhibition of the MAPK pathway, shown by decreased MEK and ERK phosphorylation 43,44. These effects of sorafenib were associated with increased apoptosis, along with increases in caspase-3, as well as decreased levels of Cyclin D1 upon treatment with drug 43,44. We postulate that as sorafenib is an inhibitor which targets multiple kinases 15,16; unlike specific mutant BRAF inhibitors, one of its effects is the downregulation of CCND1, as was observed in a hepatocellular carcinoma cell lines 17. Further studies are needed to determine the mechanism by which the addition of sorafenib to chemotherapy results in improved PFS in melanoma patients whose tumors have CCND1 amplification.
There are several limitations to our current study, including sample size. Initial clinical trial enrollment comprised 823 patients; however, tumor samples were not available for all patients and there were further technical limitations precluding aCGH from being done on all available samples. Nevertheless, the 119 tumors which underwent aCGH were representative of the overall clinical trial patient population. Analysis of tumor samples from the E2603 clinical trial, done prior to the implementation of the current FDA approved regimens of targeted therapy and immunomodulatory immunotherapies, provides an opportunity to evaluate prognostic markers for melanoma. Moreover, despite the fact that E2603 did not stratify patients on enrollment and did not demonstrate a difference between the two treatment arms, CP vs. CPS, we were able to identify markers associated with sorafenib as predictive of response to treatment with CPS, and which importantly, serve as a guide for analysis of future trials. In the era of targeted therapy and continual development of new treatment options, it is imperative to identify biomarkers which select patients who will benefit from particular treatments. The results of this study reinforce the critical value of correlative studies, even in negative clinical trials. Lastly, multiple comparisons are not adjusted in the study due to its exploratory nature.
In conclusion, our analysis of this large cohort of tumors unselected for somatic mutations and genomic alterations provides important information on copy number changes associated with treatment outcome. BRAF gain may be a potential prognostic biomarker, which should be investigated further in future clinical trials. In addition, RAF1 amplification predicted for improved response to CRAF inhibition, as did CCND1 and KRAS amplification, supporting the hypothesis that signaling thru CRAF is important in select melanoma cohorts. We also observed MET amplification associated with BRAF somatic mutation, and specifically increased amplification in BRAF V600K mutation cohorts, results consistent with TCGA data. These copy number changes suggest potential biomarkers that may be important in identifying prognostic markers, markers of response to treatments, or markers of mechanisms of resistance and should be evaluated further in future studies. Finally, RAS mutations have been identified in papillary thyroid cancer and RAF1 is commonly amplified in a number of cancers, including bladder cancer, that are treated with sorafenib suggesting that our results and observations may have implications in other tumor types.
Supplementary Material
Translational Relevance.
We present correlative studies for E2603, the randomized ECOG phase III clinical trial. Patients with advanced stage melanoma were randomized to carboplatin and paclitaxel, with and without sorafenib (CPS vs. CP), prior to current immunotherapies and BRAF targeted therapies. Although in the clinical trial, no overall benefit was demonstrated for CPS over CP, in the correlative studies, we identified three markers associated with significantly improved clinical outcomes upon CPS treatment. These copy number aberrations, including RAF1 (cRAF) itself, a target of sorafenib, have been associated with changes in MAPK signaling through cRAF. Identification of these markers expands upon mechanisms to stratify patients for benefit from targeted therapies, and has implications for development of pan-RAF inhibitors. Moreover, this study emphasizes the importance of correlative studies, even in the setting of a negative clinical trial, which can identify sub-sets of patients that respond to therapy.
Acknowledgments
Research support:
This study was coordinated by the Eastern Cooperative Oncology Group (Robert L. Comis, M.D., Chair) and supported in part by Public Health Service Grants CA23318, CA66636, CA21115, CA15488, CA14958, CA39229 and from the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services. Its content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute. This research was funded in part by a NCI Cancer Center Research Training Program Grant T32 CA009615 (PI: Dr. John Maris) (MAW), NIH Grant CA115756 (HMK), and CA118871 (KLN, KTF).
Footnotes
Presented in part at the American Association for Cancer Research Annual Meeting, San Diego, CA, April 2014.
Authors’ disclosures of potential conflict of interest and author contributions are found at the end of this article. The authors’ declare no conflict of interest at this time.
References
- 1.Shi H, Moriceau G, Kong X, et al. Melanoma whole-exome sequencing identifies (V600E)B-RAF amplification-mediated acquired B-RAF inhibitor resistance. Nat Commun. 2012;3:724. doi: 10.1038/ncomms1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bastian BC, LeBoit PE, Hamm H, et al. Chromosomal gains and losses in primary cutaneous melanomas detected by comparative genomic hybridization. Cancer Res. 1998;58:2170–5. [PubMed] [Google Scholar]
- 3.Gast A, Scherer D, Chen B, et al. Somatic alterations in the melanoma genome: a high-resolution array-based comparative genomic hybridization study. Genes Chromosomes Cancer. 2010;49:733–45. doi: 10.1002/gcc.20785. [DOI] [PubMed] [Google Scholar]
- 4.Gerami P, Jewell SS, Pouryazdanparast P, et al. Copy number gains in 11q13 and 8q24 [corrected] are highly linked to prognosis in cutaneous malignant melanoma. J Mol Diagn. 2011;13:352–8. doi: 10.1016/j.jmoldx.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greshock J, Nathanson K, Martin AM, et al. Cancer cell lines as genetic models of their parent histology: analyses based on array comparative genomic hybridization. Cancer Res. 2007;67:3594–600. doi: 10.1158/0008-5472.CAN-06-3674. [DOI] [PubMed] [Google Scholar]
- 6.Greshock J, Nathanson K, Medina A, et al. Distinct patterns of DNA copy number alterations associate with BRAF mutations in melanomas and melanoma-derived cell lines. Genes Chromosomes Cancer. 2009;48:419–28. doi: 10.1002/gcc.20651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hirsch D, Kemmerling R, Davis S, et al. Chromothripsis and focal copy number alterations determine poor outcome in malignant melanoma. Cancer Res. 2013;73:1454–60. doi: 10.1158/0008-5472.CAN-12-0928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonsson G, Dahl C, Staaf J, et al. Genomic profiling of malignant melanoma using tiling-resolution arrayCGH. Oncogene. 2007;26:4738–48. doi: 10.1038/sj.onc.1210252. [DOI] [PubMed] [Google Scholar]
- 9.Lazar V, Ecsedi S, Vizkeleti L, et al. Marked genetic differences between BRAF and NRAS mutated primary melanomas as revealed by array comparative genomic hybridization. Melanoma Res. 2012;22:202–14. doi: 10.1097/CMR.0b013e328352dbc8. [DOI] [PubMed] [Google Scholar]
- 10.Stark M, Hayward N. Genome-wide loss of heterozygosity and copy number analysis in melanoma using high-density single-nucleotide polymorphism arrays. Cancer Res. 2007;67:2632–42. doi: 10.1158/0008-5472.CAN-06-4152. [DOI] [PubMed] [Google Scholar]
- 11.Adolfsson J, Steineck G. Prognostic and treatment-predictive factors-is there a difference? Prostate Cancer Prostatic Dis. 2000;3:265–268. doi: 10.1038/sj.pcan.4500490. [DOI] [PubMed] [Google Scholar]
- 12.Italiano A. Prognostic or predictive? It's time to get back to definitions! J Clin Oncol. 2011;29:4718. doi: 10.1200/JCO.2011.38.3729. author reply 4718-9. [DOI] [PubMed] [Google Scholar]
- 13.Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507–16. doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380:358–65. doi: 10.1016/S0140-6736(12)60868-X. [DOI] [PubMed] [Google Scholar]
- 15.Qi RQ, He L, Zheng S, et al. BRAF exon 15 T1799A mutation is common in melanocytic nevi, but less prevalent in cutaneous malignant melanoma, in Chinese Han. J Invest Dermatol. 2011;131:1129–38. doi: 10.1038/jid.2010.405. [DOI] [PubMed] [Google Scholar]
- 16.Wilhelm SM, Adnane L, Newell P, et al. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol Cancer Ther. 2008;7:3129–40. doi: 10.1158/1535-7163.MCT-08-0013. [DOI] [PubMed] [Google Scholar]
- 17.Liu L, Cao Y, Chen C, et al. Sorafenib blocks the RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer Res. 2006;66:11851–8. doi: 10.1158/0008-5472.CAN-06-1377. [DOI] [PubMed] [Google Scholar]
- 18.Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet. 2014;384:319–28. doi: 10.1016/S0140-6736(14)60421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Escudier B, Eisen T, Stadler WM, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356:125–34. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 20.Strumberg D, Clark JW, Awada A, et al. Safety, pharmacokinetics, and preliminary antitumor activity of sorafenib: a review of four phase I trials in patients with advanced refractory solid tumors. Oncologist. 2007;12:426–37. doi: 10.1634/theoncologist.12-4-426. [DOI] [PubMed] [Google Scholar]
- 21.Strumberg D, Richly H, Hilger RA, et al. Phase I clinical and pharmacokinetic study of the Novel Raf kinase and vascular endothelial growth factor receptor inhibitor BAY 43-9006 in patients with advanced refractory solid tumors. J Clin Oncol. 2005;23:965–72. doi: 10.1200/JCO.2005.06.124. [DOI] [PubMed] [Google Scholar]
- 22.Flaherty KT, Lee SJ, Zhao F, et al. Phase III trial of carboplatin and paclitaxel with or without sorafenib in metastatic melanoma. J Clin Oncol. 2013;31:373–9. doi: 10.1200/JCO.2012.42.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flaherty KT, Schiller J, Schuchter LM, et al. A phase I trial of the oral, multikinase inhibitor sorafenib in combination with carboplatin and paclitaxel. Clin Cancer Res. 2008;14:4836–42. doi: 10.1158/1078-0432.CCR-07-4123. [DOI] [PubMed] [Google Scholar]
- 24.Hauschild A, Agarwala SS, Trefzer U, et al. Results of a phase III, randomized, placebo-controlled study of sorafenib in combination with carboplatin and paclitaxel as second-line treatment in patients with unresectable stage III or stage IV melanoma. J Clin Oncol. 2009;27:2823–30. doi: 10.1200/JCO.2007.15.7636. [DOI] [PubMed] [Google Scholar]
- 25.Wilson MA, Zhao F, Letrero R, et al. Correlation of somatic mutations and clinical outcome in melanoma patients treated with Carboplatin, Paclitaxel, and sorafenib. Clin Cancer Res. 2014;20:3328–37. doi: 10.1158/1078-0432.CCR-14-0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nathanson KL, Martin AM, Wubbenhorst B, et al. Tumor genetic analyses of patients with metastatic melanoma treated with the BRAF inhibitor dabrafenib (GSK2118436). Clin Cancer Res. 2013;19:4868–78. doi: 10.1158/1078-0432.CCR-13-0827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.StataCorp: Stata Statistical Software: Resease 11 CSTSL. 2009 [Google Scholar]
- 28.Jakob JA, Bassett RL, Ng CS, et al. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer. 2012;118:4014–23. doi: 10.1002/cncr.26724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29:1239–46. doi: 10.1200/JCO.2010.32.4327. [DOI] [PubMed] [Google Scholar]
- 30.Menzies AM, Haydu LE, Visintin L, et al. Distinguishing clinicopathologic features of patients with V600E and V600K BRAF-mutant metastatic melanoma. Clin Cancer Res. 2012;18:3242–9. doi: 10.1158/1078-0432.CCR-12-0052. [DOI] [PubMed] [Google Scholar]
- 31.Shi H, Hugo W, Kong X, et al. Acquired resistance and clonal evolution in melanoma during BRAF inhibitor therapy. Cancer Discov. 2014;4:80–93. doi: 10.1158/2159-8290.CD-13-0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Allen EM, Wagle N, Sucker A, et al. The genetic landscape of clinical resistance to RAF inhibition in metastatic melanoma. Cancer Discov. 2014;4:94–109. doi: 10.1158/2159-8290.CD-13-0617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wagle N, Van Allen EM, Treacy DJ, et al. MAP kinase pathway alterations in BRAF-mutant melanoma patients with acquired resistance to combined RAF/MEK inhibition. Cancer Discov. 2014;4:61–8. doi: 10.1158/2159-8290.CD-13-0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parisi F, Micsinai M, Strino F, et al. Integrated analysis of tumor samples sheds light on tumor heterogeneity. Yale J Biol Med. 2012;85:347–61. [PMC free article] [PubMed] [Google Scholar]
- 35.Straussman R, Morikawa T, Shee K, et al. Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature. 2012;487:500–4. doi: 10.1038/nature11183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilson TR, Fridlyand J, Yan Y, et al. Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature. 2012;487:505–9. doi: 10.1038/nature11249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benedettini E, Sholl LM, Peyton M, et al. Met activation in non-small cell lung cancer is associated with de novo resistance to EGFR inhibitors and the development of brain metastasis. Am J Pathol. 2010;177:415–23. doi: 10.2353/ajpath.2010.090863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suda K, Murakami I, Katayama T, et al. Reciprocal and complementary role of MET amplification and EGFR T790M mutation in acquired resistance to kinase inhibitors in lung cancer. Clin Cancer Res. 2010;16:5489–98. doi: 10.1158/1078-0432.CCR-10-1371. [DOI] [PubMed] [Google Scholar]
- 39.Fecher LA, Amaravadi RK, Flaherty KT. The MAPK pathway in melanoma. Curr Opin Oncol. 2008;20:183–9. doi: 10.1097/CCO.0b013e3282f5271c. [DOI] [PubMed] [Google Scholar]
- 40.Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 41.Amado RG, Wolf M, Peeters M, et al. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26:1626–34. doi: 10.1200/JCO.2007.14.7116. [DOI] [PubMed] [Google Scholar]
- 42.Smalley KS, Lioni M, Dalla Palma M, et al. Increased cyclin D1 expression can mediate BRAF inhibitor resistance in BRAF V600E-mutated melanomas. Mol Cancer Ther. 2008;7:2876–83. doi: 10.1158/1535-7163.MCT-08-0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oh SJ, Erb HH, Hobisch A, et al. Sorafenib decreases proliferation and induces apoptosis of prostate cancer cells by inhibition of the androgen receptor and Akt signaling pathways. Endocr Relat Cancer. 2012;19:305–19. doi: 10.1530/ERC-11-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sonntag R, Gassler N, Bangen JM, et al. Pro-apoptotic Sorafenib signaling in murine hepatocytes depends on malignancy and is associated with PUMA expression in vitro and in vivo. Cell Death Dis. 2014;5:e1030. doi: 10.1038/cddis.2013.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.