Abstract
Background
Alterations in glenohumeral (GH) rotation especially internal rotation and total range of motion have been associated with altered GH kinematics and susceptibility to injury. Researchers have evaluated long-term change in baseball and tennis players, and short-term changes in baseball players. However, acute (short-term) changes in GH rotation have not been evaluated in tennis players.
Hypotheses/Purpose
The purpose of this study was to quantify short-term glenohumeral rotational changes within a group of professional women's tennis players following competitive play. It was hypothesized that there would be acute alterations in passive glenohumeral internal rotation and total range of motion following episodes of tennis play.
Study Design
Cohort Study
Methods
Passive glenohumeral external rotation (GER), glenohumeral internal rotation (GIR), and total range of motion (TROM) were evaluated in a cohort of 79 professional adult female tennis players. Measurements were taken at three different time points (TP): baseline before match play (TP1), immediately after match play (TP2), and 24-hours after baseline (TP3).
Results
There was a statistically significant decrease in the mean GIR from TP1 (43 ± 11 °) to TP2 (39 ± 9 °) (p=0.002) and from TP1 to TP3 (38 ± 10 °) (p=0.001). All measures were at the level of minimal detectable change (MDC) (4 °) indicating clinical significance. There was a decrease in mean TROM from TP1 (146 ± 11 °) to TP2 (142 ± 12 °) (p=0.04), which was not above MDC (7 °). Subgroup analysis showed that 47% of the players demonstrated a decrease in GIR beyond MDC, and 37% demonstrated a decrease in TROM beyond MDC. GER remained unchanged across all time points (p>0.05).
Conclusion
Both GIR and TROM were reduced after acute exposure to tennis play. In a large subgroup of the cohort, the changes were clinically significant and approached values previously demonstrated to be associated with increased injury risk. Given the changes in glenohumeral motion following acute exposure to tennis, evaluation of players for significant motion alterations following overhead activity and intervention strategies to minimize such alterations in these players are recommended for high level tennis players.
Level of evidence
Level 3
Keywords: Glenohumeral range of motion, tennis, tournament play, shoulder
INTRODUCTION
The inherent demands of competitive tennis require high velocities and large ranges of motion at the glenohumeral (GH) joint. Rotational velocities of up to 2420 °/sec have been reported to occur during the service motion.1 These rotational velocities occur through a total range of motion of approximately 165 ° of glenohumeral internal rotation (GIR) and external rotation (GER).2 The forces and motions generated at the shoulder are essential, and must be produced for optimal performance. The anatomic structures around the shoulder have been shown to respond and adapt to these demands, with one response being alterations in motion. Alteration or loss of GIR and/or total range of motion beyond a certain point may be associated with altered joint kinematics3 and have been associated with shoulder injury in overhead athletes.4,5,6 Therefore, it is important to understand the result of tennis play on GIR and GER as a basis for rehabilitation, conditioning, and possible prevention strategies.
GER and GIR are commonly assessed both actively and passively in order to objectively quantify glenohumeral rotation. The sum of GIR and GER is referred to as the total range of motion (TROM). Several studies have shown that as GER increases, GIR decreases in the dominant arm of the asymptomatic overhead athlete.7-11 This alteration in motion appears to be an adaptive response to the imposed demands of the overhead athlete. There are several different theories regarding this rotational alteration including posterior capsule tightness,12,13 bony adaptations,7,11,13,14 and muscular weakness and tightness.13-15 Controversy exists as to which of these phenomena causes the altered motion; however, authors have documented that loss of GIR4,16,17 or TROM5,6 beyond a certain point is associated with shoulder injury. A GIR deficit ≥ 25 ° in the dominant shoulder compared to non-dominant has been identified as a risk factor for upper extremity injury in high school baseball players.17 Additionally, a TROM side-to-side deficit ≥ 5 ° has been linked to a higher risk of shoulder injury in elite baseball and handball players.5,6 However, these values have not been established in tennis athletes.
Changes in GIR and TROM have been documented within seasons in both baseball pitchers18,19 and tennis players.20,21 In addition, short-term studies have shown that GIR and TROM have been shown to decrease immediately following a throwing episode in baseball players.8,22-24 However, no information has been reported on the acute effects the overhead motion has on rotation in tennis. However, the previously mentioned studies have focused mainly on the changes in male overhead athletes. In addition to the large ranges of motion required to perform the tennis serve, the shoulder is a common site of injury in both male and female tennis players.25,26 Therefore, the purpose of this study was to quantify short-term glenohumeral rotational changes within a group of professional women's tennis players following competitive play. It is hypothesized there would be acute alterations in glenohumeral internal rotation and total range of motion following episodes of tennis play.
METHODS
Seventy-nine professional women's tennis players (age, 25 ± 4 years; height, 174 ± 6 cm; weight, 65 ± 6kg) were recruited at four professional tournaments for participation in this study. Players were excluded from the study if they reported having sustained a shoulder injury or surgery within the previous three months. All subjects read and signed an informed consent form approved by the Lexington Clinic Institutional Review Board prior to participation in the study.
One examiner (SMR) measured passive GIR and GER on the dominant shoulder using a digital inclinometer (Dualer IQ,J Tech, Salt Lake City, UT). GIR and GER measurements were obtained at three different time points (TP): baseline immediately before match play (TP1), immediately after match play (TP2), and 24-hours after baseline (TP3). TROM was calculated as the sum of GIR plus GER.
Each subject was placed in a supine position on a treatment table. The elbow was placed in 90 ° of flexion and the glenohumeral joint in 90 ° of abduction with the humerus supported by a towel to maintain proper positioning of the joint.27,28 The examiner stabilized the scapula by cupping the coracoid process and posterior spine of the scapula with one hand.29,30 The other hand placed the inclinometer just proximal to the wrist and the subject was asked to relax while the humerus was passively moved into GIR (Figure 1) and GER. GIR and GER measurements were taken to the point of tightness in which no more GH motion would occur without movement of the scapula. This procedure was performed once bilaterally at each time point. A single examiner positioned the arm, read the inclinometer, and recorded the measurements, made possible by the small size of the digital inclinometer used (Figure 1).
Figure 1.
Glenohumeral Internal Rotation Measurement: Patient is supine with the elbow placed in 90 ° of flexion and the glenohumeral joint in 90 ° of abduction. The examiner stabilizes the scapula while passively moving the humerus into GIR.
Intra-rater reliability of the examiner (SMR) was established by measuring 13 shoulders on two separate days. Intraclass correlation coefficient (ICC2,1), standard error of measure (SEM), and minimal detectable change (MDC) values were calculated for GIR (ICC2,1 = 0.801, SEM = 2.8 °, and MDC = 4.0 °) GER (ICC2,1 = 0.915, SEM = 4.7 °, and MDC = 6.6 °), and TROM (ICC2,1 = 0.919, SEM = 4.7 ° and MDC = 6.6 °). Therefore, rotational measurements greater than or equal to 4 ° for GIR and 7 ° for TROM were considered to be a meaningful change.
STATISTICAL ANALYSIS
The Shapiro-Wilk test for normality was computed, confirming that the data were normally distributed. A one-way repeated-measures ANOVA was used to determine change in GIR, GER, and TROM across time (TP1, TP2, and TP3). All data were analyzed using the Statistical Package SPSS version 21 (IBM Corp. Armonk, NY, USA). An α level of 0.05 was considered significant for all statistical analyses.
RESULTS
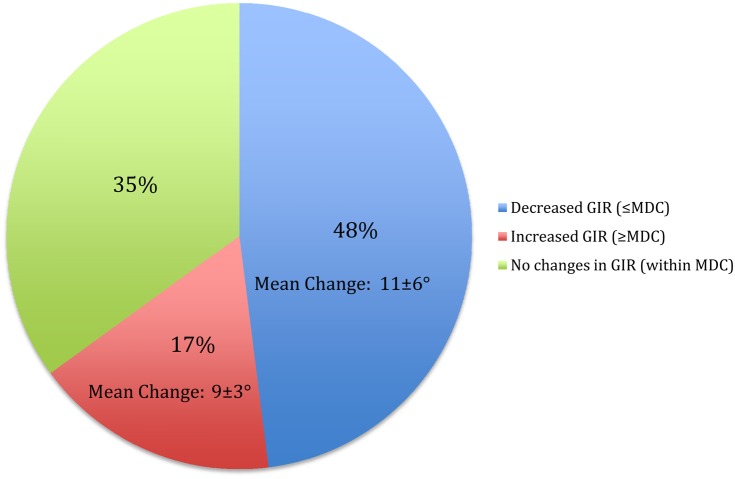
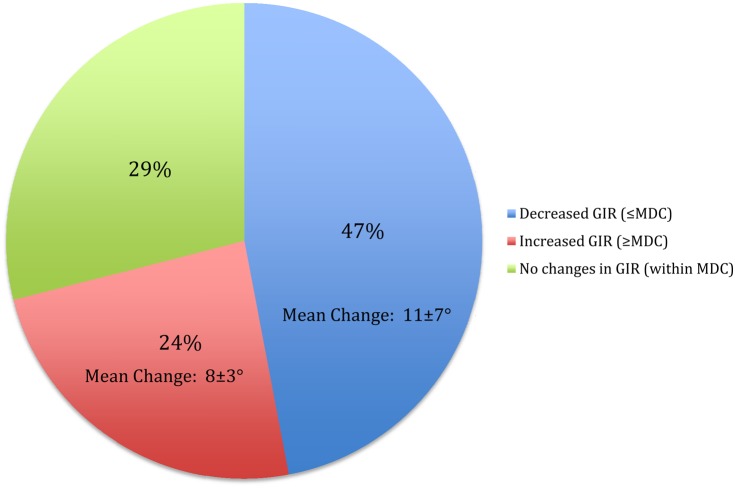
Mean GIR significantly decreased from TP1 to TP2 (p=0.002) and from TP1 to TP3 (p=0.001) (Table 1). The changes from both TP1 to TP2 and TP1 to TP3 were at or beyond the level of MDC. Further analysis subdivided the subjects into those whose GIR decreased beyond the MDC (≤4 °), increased beyond the MDC (≥4 °), or stayed within the MDC (-3 to 3). Forty-eight percent and forty-seven percent of the players demonstrated a decrease in GIR between TP1 to TP2 and TP1 to TP3, respectively. Seventeen percent and twenty-four percent of the players demonstrated an increase in GIR between TP1 to TP2 and TP1 to TP3, respectively. The mean change of players that demonstrated decreased and increased GIR beyond the MDC of 4 ° is depicted in Figure 2 and Figure 3. Thirty-five percent and twenty-nine percent of the players demonstrated changes in GIR that were within the MDC between TP1 to TP2 and TP1 to TP3, respectively.
Table 1.
Glenohumeral Range of Motion Comparisons across three time points measured in degrees
| Baseline before match play (TP1) | Immediately after match play (TP2) | 24-hours after baseline (TP3) | |
|---|---|---|---|
| Internal Rotation(°) | 43 ± 11 | 39 ± 9a | 38 ± 10 b |
| External Rotation(°) | 102 ± 9 | 102 ± 11 | 104 ± 10 |
| Total Range of Motion(°) | 146 ± 11 | 142 ± 12 c | 143 ± 11 |
Data are presented as Mean ± Standard Deviation
TP = Time Point
Significantly different from TP1 (p=0.002)
Significantly different from TP1 (p=0.001)
Significantly different from TP1 (p=0.04)
Figure 2.
This figure represents the percentages of players that decreased beyond MDC, increased beyond MDC, or stayed within MDC with respect to glenohumeral internal rotation from TP1 to TP2. The mean change is represented by the mean ± standard deviation measured in degrees, and signifies the players that demonstrated decreased or increased GIR outside the MDC of 4 °.
Figure 3.
This figure represents the percentages of players that decreased beyond MDC, increased beyond MDC, or stayed within MDC with respect to glenohumeral internal rotation from TP1 to TP3. The mean change is represented by the mean ± standard deviation measured in degrees, and signifies the players that demonstrated decreased or increased GIR outside the MDC of 4 °.
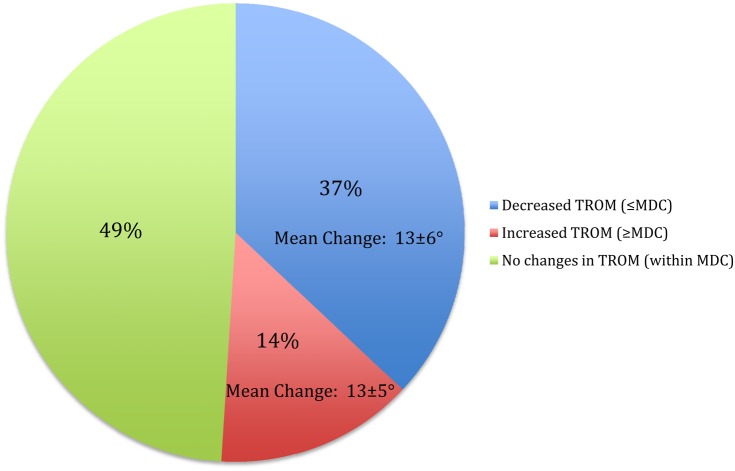
GER remained unchanged from TP1 to TP2 and TP1 to TP3 (p>0.05) (Table 1). TROM significantly decreased from TP1 to TP2 (p=0.04), but there were no significant changes from TP1 to TP3 (p=0.13) (Table 1). Thirty-seven percent of the players demonstrated a decrease beyond the MDC between TP1 to TP2 (Figure 4). Fourteen percent demonstrated an increase beyond the MDC, and 49% stayed within the MDC when investigating TROM. The mean change of players that demonstrated decreased and increased TROM beyond the MDC of 7 ° is depicted in Figure 4.
Figure 4.
This figure represents the percentages of players that decreased beyond MDC, increased beyond MDC, or stayed within MDC with respect to glenohumeral total range of motion from TP1 to TP2. The mean change is represented by the mean ± standard deviation measured in degrees, and signifies the players that demonstrated decreased or increased TROM outside the MDC of 6.6 °.
DISCUSSION
The results of this study demonstrate that acute exposure to tennis play results in change in key components of glenohumeral motion. GIR appears to be the most affected, although TROM also significantly changed from TP1 to TP2. These results are consistent with the previous literature that described adaptations to athletes in other overhead sports,18,22 which are believed to occur as a result of capsular,12,13 osseous,7,11,13,14 and musculotendinous alterations in response to repetitive overhead motion.13-15 Furthermore, this study adds novel information that subgroups of the larger tennis cohort may be more affected, and have exhibited higher levels of change.
The group mean for GIR decreased immediately after play and continued to decrease 24 hours after the acute match exposure. The group changes were only at the level of MDC, which may introduce doubt regarding the clinical significance of the changes. However, when the group changes were subdivided based on increase or decrease outside the MDC, it was found that approximately half of the athletes demonstrated decreased GIR at levels approaching concern for injury risk. The group mean for TROM also decreased immediately after play and increased by 1 ° 24-hours following match play. These group changes were below the level of MDC, which also casts doubt on the clinical significance across the group. However, subgroup analysis showed that a little over a third of players demonstrated decreases in TROM, averaging 13 ± 6 °. The data also demonstrate that tennis play does not appear to result in meaningful changes in GER following match play. This is consistent with other literature regarding changes in GH motion after acute athletic exposure. 22,23 The observed decrease in GIR coupled with a lack of change in GER may be due to the nature of the forces applied to the shoulder during the overhand motion. 1,2
Although there is still come controversy regarding the exact role of altered glenohumeral range of motion in performance and injury risk in overhead athletes, several points have been presented and discussed within the literature. First, most of the alterations involve decrease in GIR, either absolute or in relation to the opposite side, and decreased TROM in relation to the opposite side.5,6,17,22-24 Second, this alteration in GIR and TROM beyond a certain point is associated with increased injury risk at both the shoulder and elbow when assessing side-to-side deficits.5,6,17 Although exact values in GIR deficit linked to injury risk vary in the literature, it has been established that TROM deficit greater than 5 ° is associated with increased injury risk.5,6 Finally, these changes are also associated with decreased shoulder strength and increased muscle stiffness, which may be considered independent variables contributing to shoulder and elbow injury.19,31,32 Finally, current best practices from a consensus statement in baseball recommends that the acute changes in rotation be addressed by preventative strategies in order to try to avoid the documented changes in GH rotation and the consequences related to increased injury risk.33 The results of the current study add evidence showing that subgroups of tennis players can demonstrate higher levels of change.
The subgroup analysis revealed that some players decreased and some increased in motion while others remained relatively stable. However, nearly half of the players demonstrated a decrease in GIR motion across time that raises concern with the potential for adverse consequences. There are probably many factors responsible for the variability in the changes, including intensity of athletic exposure, local strength deficits, kinetic chain alterations, participation in regular conditioning activities, or the amount of previous play during the season. Until these factors are better identified, clinicians treating tennis athletes should evaluate all players for post match alterations, identify which players exhibit the significant negative changes, and implement effective interventions. This variability in motion change may also be one of the reasons behind the varied findings comparing altered motion and injury within the current body of literature.5,17,34
The researchers did not attempt to establish the anatomic or physiological basis for the changes in motion, only that they did occur. Exact mechanisms that create the acute alterations are not well established, but the amount and timing of the acute change suggest a musculoskeletal adaptation.33 This has implications for the content and timing of the interventions. Interventions should be implemented early, within the first 24 hours following tennis play, and are suggested to include dynamic warm-up, mobilization, stretching, light eccentric strengthening, and scapular retraction control.33,35-37
There are several limitations to this study. The first is that the study population was comprised of only female tennis players, so only general comparisons of the similarity of the adaptations can be made to previously studies using male baseball players, and no conclusions can be made regarding male tennis players. Second, this was an observational, cross sectional study involving change over 24 hours. More investigation is needed to examine what changes may occur in the short term (3-7 days) or long term (1-2 seasons). Third, because tennis players generally play every day or every other day, while baseball players generally pitch every 3rd to 5th day, the change over time may be different. Longer-term studies, over a weeklong tournament and over an entire season, and similar studies in male tennis players would help to provide additional missing information. Lastly, match time or other measures of match intensity were not collected during this investigation. Future reports should examine whether match time or intensity plays a role in objective glenohumeral alterations.
CONCLUSIONS
The demands of the overhead tennis serve motion result in acute adaptive changes in glenohumeral ROM in female tennis players. Female tennis players demonstrated decreased GIR and TROM, similar to the direction of change previously found in male baseball players.22 Given the concern regarding the possible impact of changes in glenohumeral ROM on shoulder and elbow injury risk in baseball players, evaluations for this change, identification of the players exhibiting the change, and intervention strategies to minimize the motion alterations should be considered in tennis players as well.
REFERENCES
- 1.Fleisig G Nicholls R Elliott B, et al. Kinematics used by world class tennis players to produce high-velocity serves. Sports Biomech. Jan 2003;2(1):51-64. [DOI] [PubMed] [Google Scholar]
- 2.Kibler WB. Biomechanical analysis of the shoulder during tennis activities. Clinics in Sports Medicine. 1995;14:79-85. [PubMed] [Google Scholar]
- 3.Borich MR Bright JM Lorello DJ, et al. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J. Orthop. Sports Phys. Ther. Dec 2006;36(12): 926-934. [DOI] [PubMed] [Google Scholar]
- 4.Myers JB Laudner KG Pasquale MR, et al. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. Mar 2006;34(3):385-391. [DOI] [PubMed] [Google Scholar]
- 5.Wilk KE Macrina LC Fleisig GS, et al. Correlation of Glenohumeral Internal Rotation Deficit and Total Rotational Motion to Shoulder Injuries in Professional Baseball Pitchers. Am. J. Sports Med. 2011;39(2):329-335. [DOI] [PubMed] [Google Scholar]
- 6.Clarsen B Bahr R Andersson SH, et al. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br. J. Sports Med. Sep 2014;48(17):1327-1333. [DOI] [PubMed] [Google Scholar]
- 7.Crockett HC Gross LB Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. American Journal of Sports Medicine. 2002;30(1):20-26. [DOI] [PubMed] [Google Scholar]
- 8.Ruotolo C Price E Panchal A. Loss of total arc of motion in collegiate baseball players. J. Shoulder Elbow Surg.. Jan-Feb 2006;15(1):67-71. [DOI] [PubMed] [Google Scholar]
- 9.Brown LP Niehues SL Harrah A, et al. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. American Journal of Sports Medicine. 1988;16(6):577-585. [DOI] [PubMed] [Google Scholar]
- 10.Ellenbecker TS Roetert EP Bailie DS, et al. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Medicine and Science in Sports and Exercise. 2002:2052-2056. [DOI] [PubMed] [Google Scholar]
- 11.Reagan KM Meister K Horodyski MB, et al. Humeral retroversion and its relationship to glenohumeral motion in the shoulder of college baseball players. American Journal of Sports Medicine. 2002;30(3):354-360. [DOI] [PubMed] [Google Scholar]
- 12.Thomas SJ Swanik CB Higginson JS, et al. A bilateral comparison of posterior capsule thickness and its correlation with glenohumeral range of motion and scapular upward rotation in collegiate baseball players. Journal Of Shoulder And Elbow Surgery / American Shoulder And Elbow Surgeons … [et al]. 2011;20(5):708-716. [DOI] [PubMed] [Google Scholar]
- 13.Shanley E Thigpen CA Clark JC, et al. Changes in passive range of motion and development of glenohumeral internal rotation deficit (GIRD) in the professional pitching shoulder between spring training in two consecutive years. J. Shoulder Elbow Surg. Nov 2012;21(11):1605-1612. [DOI] [PubMed] [Google Scholar]
- 14.Meister K Day T Horodyski M, et al. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am. J. Sports Med. May 2005;33(5):693-698. [DOI] [PubMed] [Google Scholar]
- 15.Borsa PA Wilk KE Jacobson JA, et al. Correlation of range of motion and glenohumeral translation in professional baseball pitchers. Am. J. Sports Med. Sep 2005;33(9):1392-1399. [DOI] [PubMed] [Google Scholar]
- 16.Tyler TF Nicholas SJ Roy T, et al. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28:668-673. [DOI] [PubMed] [Google Scholar]
- 17.Shanley E Rauh MJ Michener LA, et al. Shoulder Range of Motion Measures as Risk Factors for Shoulder and Elbow Injuries in High School Softball and Baseball Players. Am. J. Sports Med. Jun 17 2011;39(9):1997-2006. [DOI] [PubMed] [Google Scholar]
- 18.Freehill MT Ebel BG Archer KR, et al. Glenohumeral range of motion in major league pitchers: changes over the playing season. Sports Health. Jan 2011;3(1):97-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amin NH Ryan J Fening SD, et al. The Relationship Between Glenohumeral Internal Rotational Deficits, Total Range of Motion, and Shoulder Strength in Professional Baseball Pitchers. J. Am. Acad. Orthop. Surg. 2015;23(12):789-796. [DOI] [PubMed] [Google Scholar]
- 20.ROETERT EP ELLENBECKER TS BROWN SW. Shoulder internal and external rotation range of motion in nationally ranked junior tennis players: a longitudinal analysis. The Journal of Strength & Conditioning Research. 2000;14(2):140-143. [Google Scholar]
- 21.Kibler WB Chandler TJ. Range of Motion in Junior Tennis Players Participating in an Injury Risk Modification Program. J Sci Med Sport. 2003;6:51-62. [DOI] [PubMed] [Google Scholar]
- 22.Kibler WB Sciascia A Moore S. An acute throwing episode decreases shoulder internal rotation. Clin. Orthop. Relat. Res. Jun 2012;470(6):1545-1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reinold MM Wilk KE Macrina LC, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. Mar 2008;36(3):523-527. [DOI] [PubMed] [Google Scholar]
- 24.Kibler WB Chandler TJ Livingston BP, et al. Shoulder range of motion in elite tennis players. Effect of age and years of tournament play. Am. J. Sports Med. May-Jun 1996;24(3):279-285. [DOI] [PubMed] [Google Scholar]
- 25.Winge S Jorgensen U Lassen Nielsen A. Epidemiology of injuries in Danish championship tennis. Int. J. Sports Med. Oct 1989;10(5):368-371. [DOI] [PubMed] [Google Scholar]
- 26.Hutchinson MR Laprade RF Burnett QM, et al. Injury surveillance at the USTA Boys’ Tennis Championships: a 6-yr study. Med. Sci. Sports Exerc. 1995;27(6):826-830. [PubMed] [Google Scholar]
- 27.Moore SD Laudner KG McLoda TA, et al. The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. The Journal of orthopaedic and sports physical therapy. Jun 2011;41(6):400-407. [DOI] [PubMed] [Google Scholar]
- 28.McClure P Balaicuis J Heiland D, et al. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. The Journal of orthopaedic and sports physical therapy. Mar 2007;37(3):108-114. [DOI] [PubMed] [Google Scholar]
- 29.Wilk KE Reinold MM Macrina LC, et al. Glenohumeral Internal Rotation Measurements Differ Depending on Stabilization Techniques. Sports Health: A Multidisciplinary Approach. 2009;1(2):131-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mair SD Uhl TL Robbe RG, et al. Physeal changes and range-of-motion differences in the dominant shoulders of skeletally immature baseball players. Journal of Shoulder and Elbow Surgery. 2004;13(5):487-491. [DOI] [PubMed] [Google Scholar]
- 31.Garrison JC Cole MA Conway JE, et al. Shoulder range of motion deficits in baseball players with an ulnar collateral ligament tear. Am. J. Sports Med. Nov 2012;40(11):2597-2603. [DOI] [PubMed] [Google Scholar]
- 32.Trakis JE McHugh MP Caracciolo PA, et al. Muscle strength and range of motion in adolescent pitchers with throwing-related pain: implications for injury prevention. Am. J. Sports Med. Nov 2008;36(11):2173-2178. [DOI] [PubMed] [Google Scholar]
- 33.Kibler WB Kuhn JE Wilk K, et al. The disabled throwing shoulder: spectrum of pathology-10-year update. Arthroscopy. Jan 2013;29(1):141-161 e126. [DOI] [PubMed] [Google Scholar]
- 34.Burkhart SS Morgan CD Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2003;19(4):404-420. [DOI] [PubMed] [Google Scholar]
- 35.Laudner KG Sipes RC Wilson JT. The acute effects of sleeper stretches on shoulder range of motion. Journal of athletic training. Jul-Aug 2008;43(4):359-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tyler TF Nicholas SJ Lee SJ, et al. Correction of posterior shoulder tightness is associated with symptom resolution in patients with internal impingement. Am J Sports Med. Jan 2010;38(1):114-119. [DOI] [PubMed] [Google Scholar]
- 37.Proske U Morgan DL. Muscle damage from eccentric exercise: mechanism mechanical signs, adaptation and clinical applications. The Journal of physiology.. Dec 1 2001;537(Pt 2):333-345. [DOI] [PMC free article] [PubMed] [Google Scholar]