Abstract
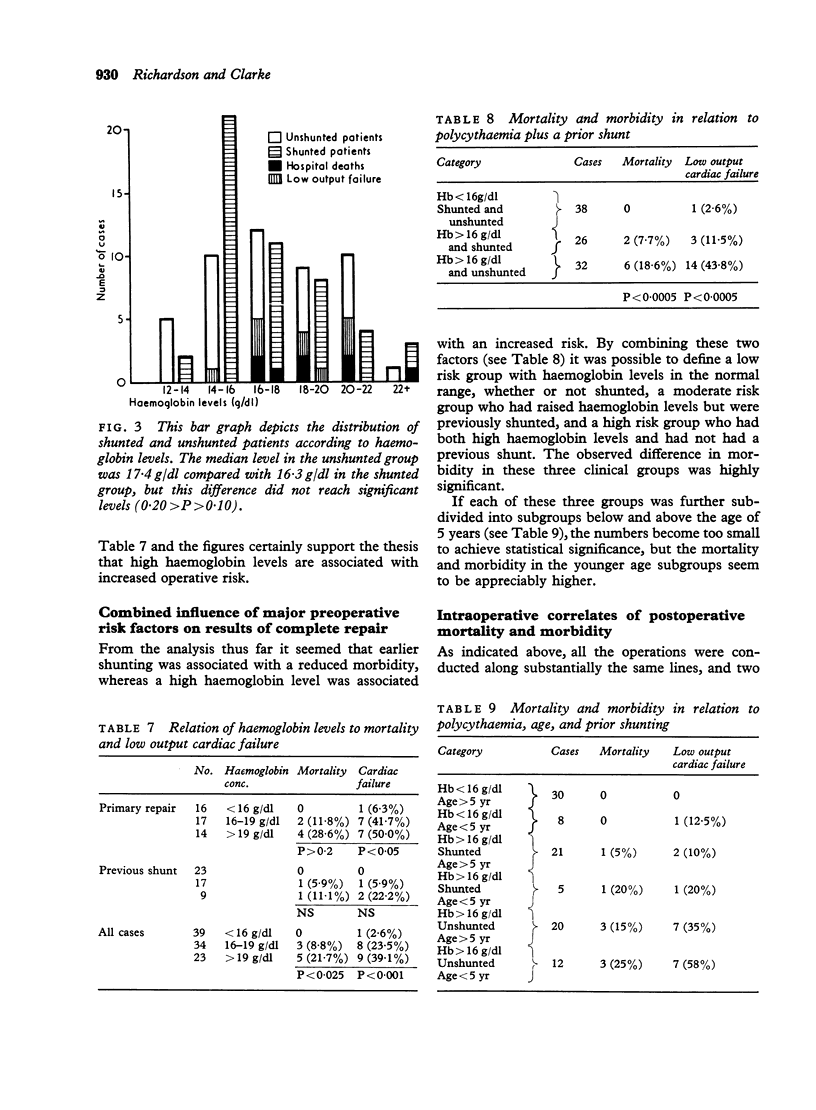
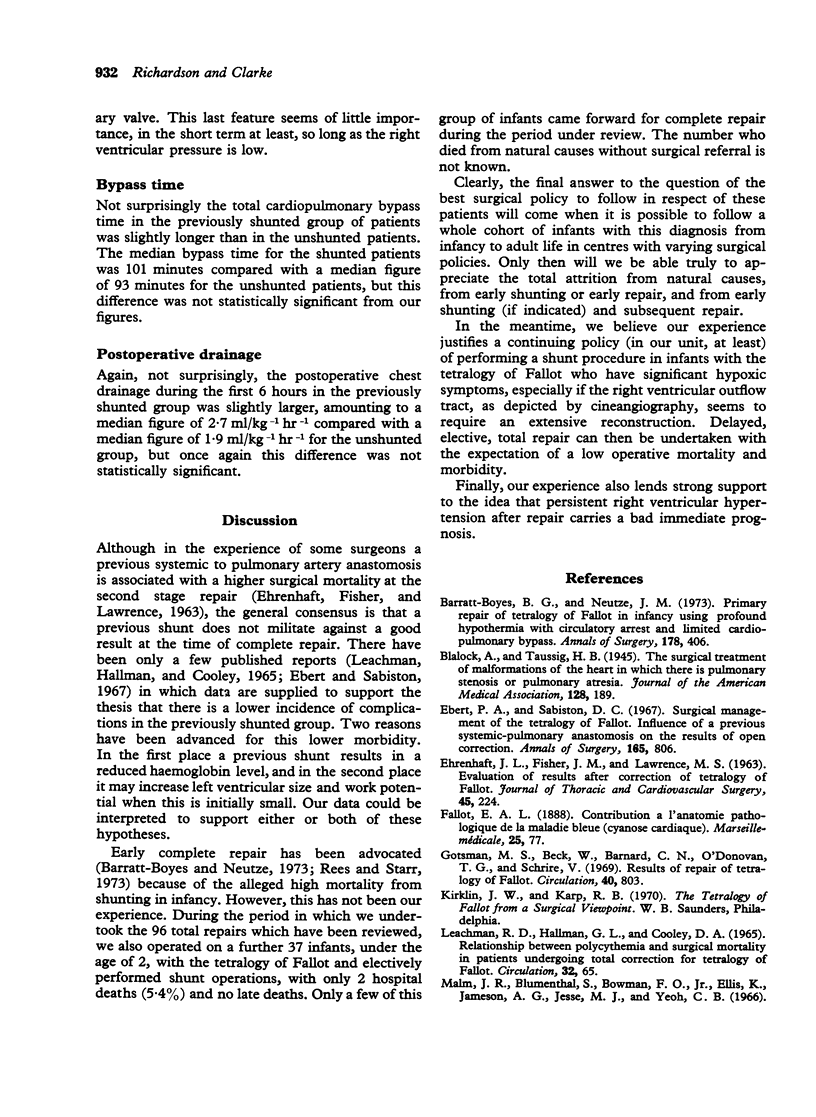
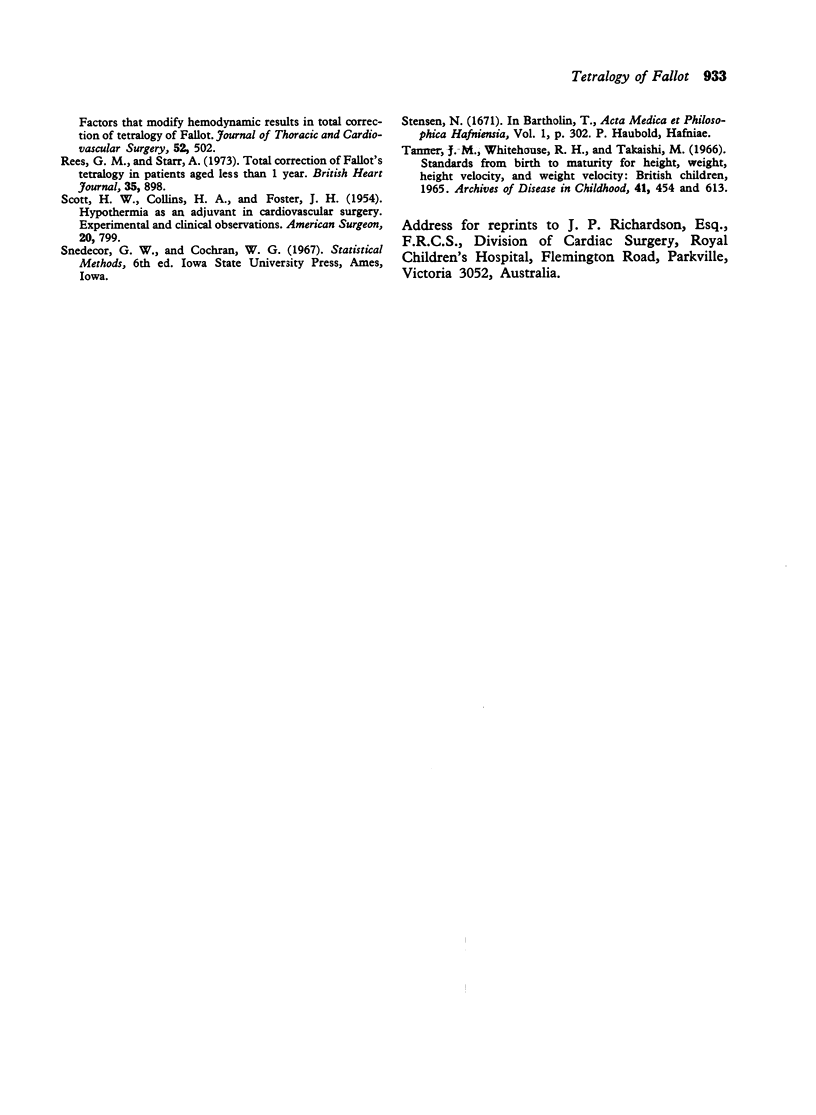
Ninety-six consecutive total repairs of the tetralogy of Fallot are reviewed. There was an overall hospital mortality of 8-3 per cent and a total incidence of low output cardiac failure of 18-8 per cent, and this was the principal cause of death and the most important source of postoperative morbidity. In 49 cases there had been a previous palliative shunt procedure and there was a strikingly lower mortality and a highly significant lower morbidity in this group. Other factors which correlated in a positive fashion with increased mortality and morbidity were chronic hypoxia (as evidenced by polycythaemia), age below 5 years, severe postoperative right ventricular hypertension, and (to a lesser extent) extensive right ventricular outflow tract reconstruction. Data are presented to support the hypothesis that a palliative shunt procedure should be considered in the severely polycythaemic child with a surgically 'unfavourable' right ventricular outflow. This policy carries a low early mortality in our hands (5-4%), and is associated with a low mortality (3-9%) at a subsequent repair. This compares with a mortality of 12-8 per cent for primary repair, and the incidence of low output cardiac failure is five times as high in the primary repair as compared to the previously shunted group.
Full text
PDF