ABSTRACT
The authors commenced research in 2005 with the goal of on constructing a health support system for primary caregivers. This ongoing study aims to develop a health support program and construct a system of regional assistance based on examining the health situation of family caregivers. Furthermore, it aims to present proposals that will put the minds of citizens at ease in respect to their ability to live in a super aging society. A survey was conducted with 213 male and female caregivers and a control group of 477 community residents not engaged in care. This paper collates the various research findings reported in journals and conference presentations by the authors. Among both male and female caregivers, blood pressure levels required regulation. Among female caregivers, grip strength and musculoskeletal symptoms were worse than those in the control group, even when participants were matched for age. We attempted to determine the characteristics of caregivers who have strong feelings of responsibility and obligation toward their provision of care. Age was a significantly higher factor in the group with stronger feelings in that regard. The group with weaker feelings of responsibility and obligation was younger. The percentage of participants who were caring for a spouse, living with a spouse, had no secondary caregivers, or were providing all-day care, was significantly higher in the group with stronger feelings of responsibility and obligation. There was no significant difference between the groups in the mean total score on the J-ZBI-8 that measures burden of care. As the aging population of Japan grows larger, support for caregivers with physical and psychological health problems, and at the very least, concern of government administrators and the general public, will assume greater importance.
Key Words: Family caregivers, Blood pressure, Grip strength, Musculoskeletal symptoms, Responsibility and obligation
INTRODUCTION
Research in Japan focused on the physical and psychological health of family caregivers has been conducted using indexes of burden of care/depression,1) quality of life (QOL),2) past medical history,3,4) and current illness.5) The majority of such studies were conducted by questionnaire. Unlike research conducted in the United States and Europe,6-9) few studies in Japan have used ecological indexes from an objective standpoint in their investigation. Even in research that has used ecological indexes, either survey samples were small or there were no specified comparative groups. Thus, the actual health of family caregivers remains unknown worldwide, not just in Japan. Since the burden of providing physical and psychological support to family caregivers is starting to become a social problem, it is necessary to investigate the actual conditions of family caregivers and to present appropriate evidence-based support strategies. The authors launched a study in 2005 centered around constructing a health support system for primary caregivers. A survey was conducted with 213 male and female caregivers and a control group of 477 community residents not engaged in care. Data collected from ecological testing resources and questionnaires were analyzed. This paper collates the various research findings reported in journals and conference presentations by the authors. SPSS15.0 J for Windows was used for all data analysis, with significance set at p<0.05.
Research related to “constructing a health support system for primary caregivers”
Rationale for the present study
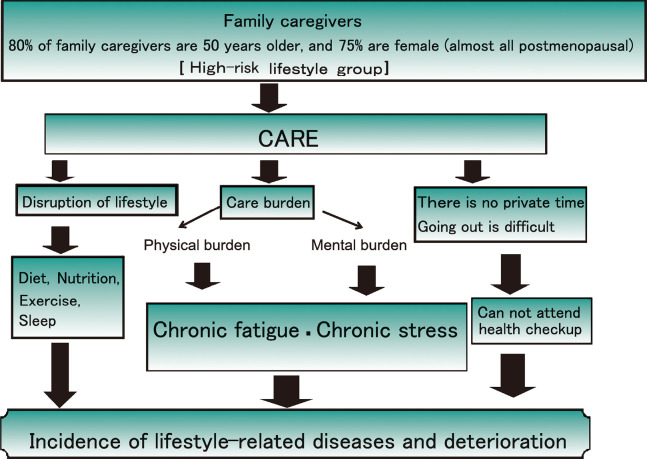
The hypotheses10) that became the driving force behind the study are shown in Figure 1. In Japan, practically all family caregivers are over 50 years of age, the time at which there is an increased likelihood of the onset of life-style related diseases. However, family caregivers invest much time in providing care, making it difficult for them to find time to care for their own health.11) Furthermore, caregivers may be unlikely to assume healthy behaviors given that a low percentage of them are reported to undergo medical check-ups,12) and there are a few opportunities for them to become aware of any illnesses they may have. The discovery of life-style related diseases in caregivers as a group has proven difficult. Additionally, lack of sleep, disturbance in lifestyle, and physical and psychological burdens from caregiving may increase the risk of the onset or exacerbation of lifestyle-related diseases among caregivers.
Fig. 1.
Research hypothesis
Purpose
The present study10) intends to develop a health support program and construct a system of regional assistance by examining the health status of family caregivers. The study also aims to present proposals which will put the minds of citizens at ease regarding their ability to live in a super aging society. The present study is based on a 2005 baseline study and is comprised of the following three sections:
1) Data collection on the effects of free home-based care (baseline survey, longitudinal survey),
2) Development of a health support program based on the results of analyses (blood pressure reduction program, laughter-inducing program),
3) Activities promoting assistance for family caregivers and the construction of a community support system that utilizes the health support counters of designated supermarkets (Fig. 2).
Fig. 2.

Health support counter in a certain supermarket
MATERIALS AND METHODS
Participants
Fliers requesting study participants were distributed at 16 facilities that included home-based care support businesses or visiting care stations, in Aichi, Gifu, and Shiga Prefectures.13) Caregivers who practiced homecare on individuals requiring care over level 3, or below level 3 but with dementia, were recruited. Written consent and valid responses were obtained from 213 participants (52 males, 161 females). The control group consisted of 477 general residents of K City in Aichi Prefecture who had undergone either a public health checkup or a basic health checkup, and had provided written consent to participate in the survey. Participants were matched 1:1 for sex and age in ten-year increments to counter the effects of age. The mean age of female family caregivers was 62.8 years (SD=1.9), while the mean age within the control group was 63.2 years (SD=12.4). There was no statistically significant difference between the groups.
Survey methods
Trained survey officials conducted the survey by visiting family caregiver homes. A self-reporting questionnaire included items on the health of caregivers, lifestyle habits, and details of care. Ecological resources were gathered through examinations using blood and urine samples primarily associated with lifestyle related diseases, as well as general measurements of grip strength and body fat. The control group survey was conducted during the public and basic health examinations of K City, Aichi Prefecture. Health examination results were provided for those items that appeared on both the survey and the health examination. For non-duplicated items, participants were surveyed by the same method as that in the experimental group.
RESULTS AND DISCUSSION
Health issues of family caregivers
Family caregivers and blood pressure
The results indicated that a means to address blood pressure levels in both men and women was required. The prevalence rate of hypertension was significantly higher in female caregivers than in controls (Table 1).13) In addition, a significant positive association was found between care giving and hypertension when other factors were controlled (rate of adjusted odds: 1.86, 95% Confidence Interval: 1.03–3.37).14) The results indicated a high likelihood of hypertension in female caregivers. Among male caregivers,15) there was no significant difference in the rate of hypertension between caregivers and controls (59.6% to 65.4%). For mean blood pressure, however, the systolic blood pressure (M=148.6, SD=42.9 mmHg vs. M=130.9, SD=20.6 mmHg, p<0.05) and diastolic blood pressure (M=91.5, SD=50.3 mmHg vs. M=74.8, SD=11.9 mmHg, p<0.01) were both significantly higher in male caregivers than in controls. This indicated that there is a greater number of male family caregivers with hypertension and higher blood pressure than in the control group. This finding warrants future examination of hypertension management among male family caregivers.
Table 1.
Characteristics of caregiver status
| Odds ratio | 95% confidence interval | multivariate odds ratio | 95% confidence interval | |
|---|---|---|---|---|
| Hypertension | 1.65 | 1.04–2.64 | 1.86 | 1.03–3.37 |
| Exercise | 0.38 | 0.24–0.61 | 0.44 | 0.25–0.78 |
| Yearly health checkup experiences | 0.23 | 0.13–0.42 | 0.26 | 0.13–0.54 |
| Health/old age-related stress | 2.62 | 1.58–4.34 | 2.53 | 1.37–4.67 |
| Carbohydrate energy ratio | 1.06 | 1.02–1.11 | 1.05 | 0.997–1.110 |
| PSQI score | 1.21 | 1.11–1.31 | 1.15 | 1.05–1.26 |
| Relaxing recreation | 0.86 | 0.79–0.93 | 0.88 | 0.79–0.97 |
Multivariate: logistic regression analysis
Dependent variable: caregiver status (0: no; 1: yes)
Explanatory variable: hypertension (0: no; 1: yes), profession (0: no; 1: yes), exercise (0: no; 1: yes), subjective health condition (0: healthy; 1: not healthy), yearly health checkup experiences (0: no; 1: yes), health/old age-related stress (0: no; 1: yes), depressive state (0: no; 1: yes), carbohydrate energy ratio, PSQI score, relaxing recreation
Family caregivers and grip strength/musculoskeletal systemic symptoms
Table 2 shows the grip strength and musculoskeletal symptoms of family caregivers. Among females,16) grip strength and musculoskeletal symptoms were worse in family caregivers than in controls, even when participants were matched for age. This indicates that such symptoms are not a product of age and that providing care is a contributing factor. On the other hand, no significant difference in mean grip strength and musculoskeletal symptoms was observed among males.17) These findings suggest that the impact of care on grip strength and musculoskeletal symptoms differs between sexes, and that future research is needed to explore possible underlying causes.
Table 2.
Compared grip and symptoms with male and female family caregivers and control
| Men (n=104) | Significance level | ||
|---|---|---|---|
| Family caregivers (n=52) | Control (n=52) | ||
| (%), Mean±SD | |||
| Age | 69.3±10.9 | 69.2±11.1 | ns |
| Grip (kg) | 33.3±6.0 | 34.4±6.7 | ns |
| Subjective symptoms | |||
| Neck, back and shoulder stiffness | 42.3 | 34.6 | ns |
| Muscle and joint pain and stiffness | 46.2 | 28.8 | ns |
| Lower back pain | 48.1 | 46.2 | ns |
| Numbness in limbs | 30.8 | 17.3 | ns |
| Women (n=320) | Significance level | ||
|---|---|---|---|
| Family caregivers (n=160) | Control (n=160) | ||
| (%), Mean±SD | |||
| Age | 62.8±11.9 | 63.0±12.2 | ns |
| Grip (kg) | 22.0±4.5 | 24.2±4.1 | * |
| Subjective symptoms | |||
| Neck, back and shoulder stiffness | 61.0 | 46.9 | * |
| Muscle and joint pain and stiffness | 43.4 | 33.1 | # |
| Lower back pain | 55.3 | 33.8 | * |
| Numbness in limbs | 23.9 | 14.4 | * |
t test, χ2 test *: p<0.05 #: p<0.1 ns: not significant
Characteristics of family caregivers with strong feelings of responsibility and obligation toward care
Ten years have passed since public nursing care insurance was put into effect. Annual increases in the number of murders and joint suicides committed by caregivers have been reported in news media, and various articles have suggested18) that many of the perpetrators held strong feelings of responsibility and obligation toward care. Although these caregivers harbored complaints and anxieties, they refused to seek help from family or others around them. Accumulated physical and psychological fatigue seems to have ultimately triggered their desperate recourse to the aforementioned events. Given this, we attempted to uncover the characteristics of people with strong feelings of responsibility and obligation toward their care provision.19) This analysis was focussed on the female caregiver.
The statement: “I feel that more than anything I alone must provide care,” was used as the index for measuring the strength of feelings of responsibility and obligation toward care. Participants who answered, “I strongly agree,” to this item were placed in the group of individuals considered to have stronger feelings of responsibility and obligation toward care. All other participants were placed in the group with “weaker feelings.” The groups were then examined and compared. Table 3 shows the differences in the background factors of both groups, while Table 4 shows the outcomes from a comparison of both groups using the short Japanese version of the Zarit Caregiver Burden Interview (J-ZBI-8).
Table 3.
Characteristics of family caregivers with strong feelings of responsibility and obligation toward care
| Feel strong (n=98) | Feel weak (n=48) | Significance level | ||
|---|---|---|---|---|
| number % | number % | |||
| Age year | 66.9±9.9 ‡ | 58.6±10.9 | *** | |
| Relationship with care receivers | ||||
| Spouse | 58 (59.2%) | 15 (31.3%) | ** | |
| Parent | 23 (23.5%) | 17 (35.4%) | ||
| Parent in law | 17 (17.3%) | 16 (33.3%) | ||
| Family housemates | ||||
| One | 47 (48.0%) | 11 (22.9%) | ** | |
| More than two | 51 (52.0%) | 37 (77.2%) | ||
| Sub-caregivers for daily home care | ||||
| Yes | 18 (18.6%) | 22 (45.8%) | *** | |
| No | 79 (81.4%) | 26 (54.2%) | ||
| Home care time per day | ||||
| all day | 44 (45.4%) | 15 (31.3%) | * | |
| half time | 19 (19.6%) | 3 (6.3%) | ||
| 2 or 3 hours | 6 (6.2%) | 8 (16.7%) | ||
| Necessity | 27 (27.1%) | 21 (43.8%) | ||
| other | 1 (1.0%) | 1 (2.1%) | ||
χ2 test, t test
†: p<0.1, *: p<0.05, **: p<0.01, ***: p<0.001
‡: Mean ± standard deviation
Subjects with unknown response were excluded.
Table 4.
Brief version of the Japanese Zarit Caregiver Burden
| Feel strong (n=98) | Feel weak (n=48) | Significance level | |
|---|---|---|---|
| Total score | 10.1±7.2 ‡ | 11.0±6.7 | |
| item 1 score | 1.6±1.3 ‡ | 1.8±1.2 | |
| item 2 score | 0.9±1.2 ‡ | 1.5±1.0 | ** |
| item 3 score | 1.4±1.4 ‡ | 1.3±1.2 | |
| item 4 score | 1.4±1.3 ‡ | 1.5±1.2 | |
| item 5 score | 1.8±1.4 ‡ | 1.4±1.3 | |
| item 6 score | 1.1±1.4 ‡ | 1.2±1.3 | |
| item 7 score | 0.7±0.9 ‡ | 1.2±1.1 | ** |
| item 8 score | 0.9±1.0 ‡ | 1.1±0.9 |
Mann-Whitney’U test
†: p<0.1, *: p<0.05, **: p<0.01, ***: p<0.001
‡: Mean ± standard deviation
Subjects with unknown response were excluded.
Age was significantly higher in the former group than in the latter. The percentage of participants who were caring for a spouse, living with a spouse, had no secondary caregivers, or provided all-day care, was significantly high in the group with stronger feelings of responsibility and obligation. There was no significant difference between the groups according to the mean total scores of the J-ZBI-8 that measures the burden of care. However, mean scores in response to item 2, “I think I’d prefer to entrust the care to someone else,” were significantly low in this group. This suggests that within the group with such strong feelings, few contemplated handing over their care responsibilities to someone else.
Furthermore, mean scores for responses to item 7, “I become irritated when I am around the person I am caring for,” were significantly low in this group, suggesting that a high number of participants do not become upset at patients in need of care.
The above findings indicate that those in the group with strong feelings toward their charges care do not become irritated with them or wish to entrust the care to others. This is despite the fact that they may live alone with an aging spouse or spend long hours giving care. The low percentage of participants with a secondary caregiver may not be related to a shortage of individuals who could potentially be caregivers, but indicates instead that caregivers do not need assistants or seek them out. These tendencies could lead caregivers to shoulder the entire burden themselves. In the future we would like to explore forms of assistance, such as social support networks, in caregiver surroundings.
LIMITATIONS
Our study has some limitations by virtue of its design. Specifically, data for the control group were taken from public health checkup records due to shortfalls in budget and research personnel. Despite its drawbacks, the study using ecological indexes, had close to 200 participants, and a control group. In this sense, it is a highly novel approach and provides valuable data in support of caregiver assistance. Future research should be of a higher quality, and conducted based on a refined design that provides a groundwork of data on health assistance for family caregivers.
CONCLUSION
Mitomi20) (2005) stated: “In Japan, Caregivers have been society abandoned, no has felt they should be saved by the government, and for that reason no one has much interest in the caregiver.”
However, as the Japanese aging population grows larger, support for caregivers with physical and psychological health problems, and, at the very least, concern on the part of government administrators and the general public, will take on greater importance. The United States and various European countries have already signed charters and law of support for caregivers. Thus, Japan can be expected to follow suit in the near future.
ACKNOWLEDGEMENTS
We wish to express our sincere gratitude to Ms. Ritsuko Hamamoto and Ms. Sanae Tsukamoto.
REFERENCES
- 1).Maruyama M, Tanji H, Arai H, Sasaki H. Burden of care and use of public services among caregivers with dementia. Japanese Journal of Geriatrics, 2005; 42: 192–194. (in Japanese). [DOI] [PubMed]
- 2).Ichimiya A, Igata R, Ogomori K, Igata T. Analysis of burden of care and QOL of elderly with dementia residing at-home, using WHO/QOL-26. Japanese Journal of Geriatric Psychiatry, 2001; 12: 1159–1167. (in Japanese).
- 3).Nishimura Y. Cardiovascular responses related to care-giving in elderly caregivers (Part 1): a focus on the care-giving behavior of female caregivers. Japan Journal of Nursing Science, 1998; 18: 87–95. (in Japanese).
- 4).Okuda M, Umemura M, Yamami N, Ogihara R, Mano Y, Hosaka T, Mizuno E, Aoyagi M. A study on fatigue and health disturbance in caregivers of the elderly at home. Japanese Journal of Primary Care, 2004; 27: 9–17. (in Japanese).
- 5).Mano Y. Disease prevalence among home caregivers: analysis of family relationships in home medical care and development of homecare support programs. pp.20–39, 2001, Health Labour Sciences Research Grant, Japanese Foundation for Aging and Health, Research Report. (in Japanese).
- 6).King AC, Oka RK, Yong DR. Ambulatory blood pressure and heart rate responses to the stress of work and caregiving in older wormen. J Gerontol, 1994; 49: 239–245. [DOI] [PubMed]
- 7).Vitaliano PP, Scanlan JM, Zhang J, Sarage MV, Hirsch IB, Sieqler IC. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med, 2002; 64: 418–435. [DOI] [PubMed]
- 8).Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med, 2003; 24: pp.113–119. [DOI] [PubMed]
- 9).Mitomi K. In Community Care and Caregivers in the United Kingdom. pp.215–220, 2008, Minerva Publishing, Inc., Tokyo. (in Japanese).
- 10).Hori Y, Hoshino J. Health issues among family caregivers. Current Medicine, 2010; 58: 349–354. (in Japanese).
- 11).Hori Y, Maekawa A, Niwa S, Sakurai S, Hamasima K, Hamamoto R, Morimoto M, Kume T, Okada T, Hoshino J. Preliminary study on primary prevention of cerebrovascular and cardiovascular diseases among primary caregivers of individuals requiring advanced home nursing care. Heisei Year 17 Aichi Nursing Research Report 2006; 32–42. (in Japanese).
- 12).Takeuchi M, Yoshida T. Issues of primary caregivers of older adults requiring nursing care. Journal of Japan Home Care, 2002; 6: 79–84. (in Japanese).
- 13).Hoshino J, Hori Y, Kondo T, Maekawa A, Tamakosi K, Sakakibara H. Physical and mental health characteristics of female caregivers. Japanese Journal of Public Health, 2009; 56 (2): 75–86. (in Japanese). [PubMed]
- 14).Hoshino J, Hori Y, Kondo T, Tamakoshi K, Onishi J, Toyoshima H, Sakakibara H. Cross-sectional study on associations between caregiving and hypertension, Japanese journal of cardiovascular disease prevention, 2011; 46 (2): 180–189. (in Japanese).
- 15).Nagai K, Hori Y, Kondo T, Hoshino J, Maekawa A, Sakakibara H, Niwa S. Health conditions and life styles among male primary caregivers of homecare (First report). Supplement to Journal of Epidemiology, 2008; 18 (1): 132. (in Japanese).
- 16).Suzuki K, Hoshino J, Hamamoto R, Hori Y. Characteristics of grip and musculoskeletal symptoms in female caregivers: comparison of female non-caregivers. Japanese Journal of Public Health, 2010; 57 (10): 201. (in Japanese).
- 17).Suzuki K, Hoshino J, Hori Y, Hamamoto R, Sugiyama T, Tamakoshi K, Kondo T, Sakakibara H. Gender differences in symptoms related to grip, muscles, bones, and joints: comparison of homecare caregivers with non-caregivers. Supplement to Journal of Epidemiology, 2011; 21 (1): 336. (in Japanese).
- 18).The Chunichi Shinbun News Crew. Writing and Editing. Tasukeai Senki. Reality of the caregiving society. Second Chapter. Only I could do it. pp.19–31, 2010, Chunichi Shinbun Corporation, Nagoya. (in Japanese).
- 19).Hamamoto R, Hoshino J, Suzuki K, Sugiyama T, Saito A, Tsuchiya H, Nakagami T, Hori Y. Association of life style and life-style diseases of female caregivers and personal awareness of the necessity of providing care. Japanese Journal of Public Health, 2010; 57 (10): 201. (in Japanese).
- 20).Mitomi K. Safeguards for care and support for caregivers in the U.S. and Europe. Introduction: research on the history and social politics of caregivers. pp.26–28, 2005, Minerva Publishing, Inc., Tokyo. (in Japanese).