Summary
Objective
A low‐carbohydrate diet can reduce body weight and some cardiovascular disease risk factors more than a low‐fat diet, but differential adherence may play a role in these effects.
Methods
Data were used from 148 adults who participated in a 12‐month clinical trial examining the effect of a low‐carbohydrate diet (<40 g d−1) and a low‐fat diet (<30% fat and <7% saturated fat) on weight and cardiovascular disease risk factors. We compared attendance at counselling sessions, deviation from nutrient goals, urinary ketone presence and composite scores representing the overall adherence based on the distribution of these individual indicators between two interventions.
Results
Composite scores were similar between the two groups. A one‐interquartile‐range increase in composite score representing better adherence to a low‐carbohydrate diet was associated with 2.2 kg or 2.3% greater weight loss, 1.1 greater reduction in percent fat mass and 1.3 greater increase in proportion of lean mass. Indicators of adherence to a low‐fat diet were not associated with changes in weight, fat mass or lean mass.
Conclusions
Despite comparable adherence between groups, a low‐carbohydrate diet was associated with greater reductions in body weight and improvement in body composition, while a low‐fat diet was not associated with weight loss.
Keywords: Carbohydrates, nutrition, weight loss
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the USA, accounting for over 30% of total deaths each year 1. Obesity is an established risk factor for CVD. The prevalence of obesity has increased dramatically until recently and remains at a high level 2, 3, 4. According to the latest estimates, 68.5% of American adults are either overweight or obese 3.
Dietary modification is a cornerstone of strategies to reduce obesity and prevent CVD 5, 6, 7, 8. For weight loss, low‐carbohydrate diets remain popular alternatives to conventional low‐fat, high‐carbohydrate diets. Relatively few studies have compared dietary regimens of differing macronutrient contents for weight loss over the course of a year or longer 9, 10, 11, and of those that have, some achieved lesser dietary differences between groups than originally planned 12, 13, 14, 15. Because of relatively small differences in results between groups in previous trials, it has been widely proposed that adherence, the extent to which participants meet or maintain the programme goals, may be more important than macronutrient composition of diets for weight loss and improvement in disease‐related outcomes 16, 17. Accordingly, it has been advised that ‘the best approach is to counsel patients to choose a dietary plan they find easiest to adhere to in the long term’ 6, 17, 18.
However, the relationship between dietary adherence and efficacy of diets with varying macronutrient compositions has not been well examined. The few previous studies that examined this issue have focused on weight loss, without assessing other aspects of dietary efficacy 19, 20, and often relied on a single measure of dietary adherence 19. In order to further address this issue, therefore, we compared multiple indicators representing behavioural, nutritional and biochemical measures of dietary adherence between a low‐carbohydrate and a low‐fat dietary intervention and examined their relationship with 12‐month changes in body weight, body composition and CVD risk factors.
Methods
Study population
The study population has been described in detail elsewhere 21. In brief, adults with obesity 22–75 years of age were recruited in the Greater New Orleans area. Participants were excluded if they were using prescription weight loss medications, had undergone or were planning to undergo weight loss surgery, were pregnant or breastfeeding, had been diagnosed with type 2 diabetes, CVD or chronic kidney disease, or were using ≥2 anti‐hypertensive or ≥2 lipid‐lowering medications. All participants provided written informed consent, and all procedures were approved by the Institutional Review Board of Tulane University Health Sciences Center.
Intervention
This parallel trial was designed to examine the effects of a low‐carbohydrate diet as compared with a low‐fat diet on body weight, composition and CVD risk factors. A total of 148 participants were randomly assigned to follow either a low‐carbohydrate diet that restricted consumption of digestible carbohydrate (total carbohydrate minus total fibre) to <40 g d−1 or a low‐fat diet that restricted total fat consumption to <30% of daily energy and saturated fat consumption to <7% of daily energy 22, 23. Neither diet included a specific calorie goal. There were a total of 20 regular dietary counselling sessions including four weekly individual sessions for the first month followed by 10 group sessions every other week for 5 months and six monthly group sessions thereafter. The format of dietary counselling sessions was identical in each group. During each counselling session, participants met with a study dietitian, weighed themselves, provided a urine specimen, received handouts including optional recipes and discussed a specific topic or behaviour of nutrition. Participants received the same behaviour curriculum on the basics of dietary nutrients, including information on dietary fibre, types of dietary fats and protein, and were instructed on food choice, portion size control and measurement of daily dietary intake in both groups throughout the study. Participants were advised to maintain their baseline levels of physical activity, which was assessed using validated measures at each follow‐up visit. For those who missed any regular counselling session (individual or group), a make‐up session was scheduled at their earliest convenience.
Data collection
As previously described, a detailed medical history including medication use and health behaviours was obtained at baseline by trained staff 21. Body composition was measured using bioelectrical impedance analysis (Quantum II analyzer, RLJ Systems, Clinton, MI, USA) at randomization and each follow‐up visit. Body weight, blood pressure, serum lipids, plasma glucose, serum insulin and high‐sensitivity C‐reactive protein were measured at baseline and at each follow‐up visit using standardized methods 21. Two 24‐h dietary recalls, one on a week day and the other on a weekend day, were obtained from each participant by a certified study dietitian at 0, 3, 6 and 12 months. Nutrient intakes were calculated using the food composition tables included in the Nutrition Data System for Research software 24. Five percent of the dietary recalls were recorded and reviewed by independent trained staff for the purposes of quality control. Physical activity was assessed by a validated questionnaire (International Physical Activity Questionnaire) and was calculated as the sum of hours per week of moderate to vigorous activities (walking, sports, dance and conditioning) multiplied by the activity's individual metabolic equivalent value 25. Urinary ketones were measured by dipstick at each dietary counselling session and each follow‐up visit. In total, urinary ketones were assessed 10 times in first 3 months, 8 times in the following 3 months and 8 times in the last 6 months. Ketones were assessed using Multistix (Siemens Healthcare Diagnostics) urinary dipsticks and analysed quantitatively on the ordinal scale using a Clintek Status+ Analyzer (Siemens Healthcare Diagnostics) in the following categories: none, trace (>0–5 mg dL−1), small (>5–40 mg dL−1), moderate (>40–80 mg dL−1) and large (>80 mg dL−1).
Statistical analysis
Attendance at dietary counselling sessions was a behavioural indicator of adherence. We calculated the percentage of attendance at individual, biweekly group and monthly group sessions, and also percentage of sessions attended by 3, 6 and 12 months. Agreement between the macronutrient goal of the assigned diet and a participant's macronutrient intake was calculated from dietary recalls. In the low‐carbohydrate diet group, we calculated scores for deviation from daily carbohydrate goal using the equation (carbohydrate intake in gram – 40 g)/40 g * 100%. In the low‐fat diet group, we calculated scores for deviation from daily total and saturated fat goals as a percentage of energy using the equation (intake of total fat in %kcal − 30% kcal)/30% kcal * 100% and (intake of saturated fat in %kcal − 7% kcal)/7% kcal * 100%, respectively. The presence of urinary ketones was considered a biochemical indicator and was used to assess the adherence to a low‐carbohydrate diet. Participants who had trace, small, moderate or large ketones detected were categorized as ketone positive, while the rest were categorized as ketone negative. For each participant, we calculated percent of ketone positive urine specimens collected by 3, 6 and 12 months.
A composite score of adherence was created based on indicators at 3, 6 and 12 months among those without missing data in any of indicators (at 12 months, N = 54 low fat and N = 58 low carbohydrate). Based on the whole sample, participants were divided into quintiles for each indicator, and a point value was assigned for each stratum. Participants received 5 points in the highest quintile, 4 points in the next stratum and so on down to participants in the lowest quintile who received 1 point. For the low‐carbohydrate diet, the composite adherence score was calculated as (points of attendance score + points of deviation score of total fat + points of deviation score of saturated fat + [6 – points of deviation score of digestible carbohydrates] + points of ketone score) /25 * 100%. For the low‐fat diet, the composite adherence score was calculated as (points of attendance score + [6 – points of deviation score of total fat] + [6 – points of deviation score of saturated fat] + points of deviation score of digestible carb + [6 – points of ketone score]) /25 * 100%.
The primary outcomes of interest to assess dietary efficacy included changes in body weight, composition and CVD risk factors at 12 months. Generalized linear regression analysis was used to model the association between dietary adherence indicators and efficacy of each diet separately. Possible interaction by race was examined. Sensitivity analyses were performed to test whether these results changed after accounting for make‐up sessions or after controlling for baseline body mass index, fat mass or lean mass. To account for the potential impact of missing data, another sensitivity analysis was performed substituting a low composite score (median in the lowest quintile) of adherence in place of missing data. All P‐values were two‐sided, and statistical significance was defined as P < 0.05. sas (version 9.3; SAS Institute Inc, Cary, NC, USA) was used for all analyses.
Results
Clinical trial characteristics
We randomized 148 individuals to a low‐fat (N = 73) diet or a low‐carbohydrate (N = 75) diet. The mean age of participants was 47 (standard deviation [SD]: 10) years; 89% were women, and 51% were African–American. At 3, 6 and 12 months, in the low‐carbohydrate group, 69, 59 and 59 participants completed the examinations. Corresponding numbers for the low‐fat group were 66, 57 and 60 participants, respectively.
Adherence indicators by diet group
Overall, participants assigned to the low‐carbohydrate diet attended an average of 56.7% (SD: 21.7%) of counselling sessions, and those assigned to the low‐fat diet attended 52.3% (SD: 21.1%) of counselling sessions. There was no significant difference in the attendance at counselling sessions between the low‐carbohydrate and low‐fat groups throughout the study (Table 1). In the low‐carbohydrate group, 73.9%, 59.7% and 44.8% of individuals met the carbohydrate goals at 3, 6 and 12 months, while those who consumed more than the carbohydrate goal had mean deviations of 145% (representing a carbohydrate intake of approximately 98 g d−1),104% (82 g d−1) and 198% (119 g d−1), respectively (Figure 1). In the low‐fat group, 59.4% and 42.2% of individuals met total and saturated fat goals at 3 months, 64.8% and 33.3% did at 6 months and 55.6% and 27.8% did at 12 months, respectively. Those who consumed more than the goal had mean deviations of 19.1% (representing an intake of about 35.7% of daily energy from total fat) and 40.6% (9.8% saturated fat) at 3 months,17.4% (35.2% total fat) and 39.8% (9.8% saturated fat) at 6 months and 23.3% (37.0% total fat) and 46.2% (10.2% saturated fat) at 12 months, respectively (Figure 1). On average, participants in the low‐carbohydrate group had significantly lower intake of digestible carbohydrates but significantly higher intakes of total fat and saturated fat, compared with those in the low‐fat group (All P < 0.001) (Supporting Information Table 1). Participants who followed a low‐carbohydrate diet tended to have higher levels of ketones at 3, 6 and 12 months compared with baseline (Figure 2). P‐values for comparison with baseline were 0.007, 0.17 and 0.04 at 3, 6 and 12 months, respectively. Throughout the study, the low‐carbohydrate group had higher cumulative percentages of ketones detected in urine, compared with the low‐fat group at 3, 6 and 12 months (at 12 months, 25% [SD: 22%] low‐carb vs. 8% [SD: 8%] low‐fat; P < 0.001; Table 1). There was no significant difference in composite adherence score between groups (Table 1).
Table 1.
Indicators of dietary attendance by intervention group [mean (standard deviation)]
| Low‐carbohydrate diet | Low‐fat diet | P‐value* | |
|---|---|---|---|
| Percent attendance at dietary sessions | |||
| By session | |||
| Individual | 96.7 (11.9) | 98.3 (6.4) | 0.30 |
| Biweekly group | 55.1 (27.7) | 50.4 (29.1) | 0.32 |
| Monthly group | 32.8 (31.1) | 24.7 (28.5) | 0.10 |
| By time | |||
| 3 months | 80.8 (17.2) | 80.7 (16.8) | 0.95 |
| 6 months | 67.0 (20.6) | 64.1 (21.0) | 0.40 |
| 12 months | 56.7 (21.7) | 52.3 (21.1) | 0.21 |
| Percent ketone positive | |||
| 3 months | 31 (28) | 9 (12) | <0.001 |
| 6 months | 27 (26) | 8 (10) | <0.001 |
| 12 months | 25 (22) | 8 (8) | <0.001 |
| Composite adherence score† | |||
| 3 months | 51.8 (11.4) | 49.3 (12.2) | 0.23 |
| 6 months | 53.1 (11.2) | 51.4 (12.2) | 0.46 |
| 12 months | 55.9 (13.6) | 54.1 (12.9) | 0.48 |
All P‐values for comparisons were from Student's t‐test.
Composite adherence score was based on attendance at dietary session, deviation from macronutrient goals and ketone presence.
Figure 1.
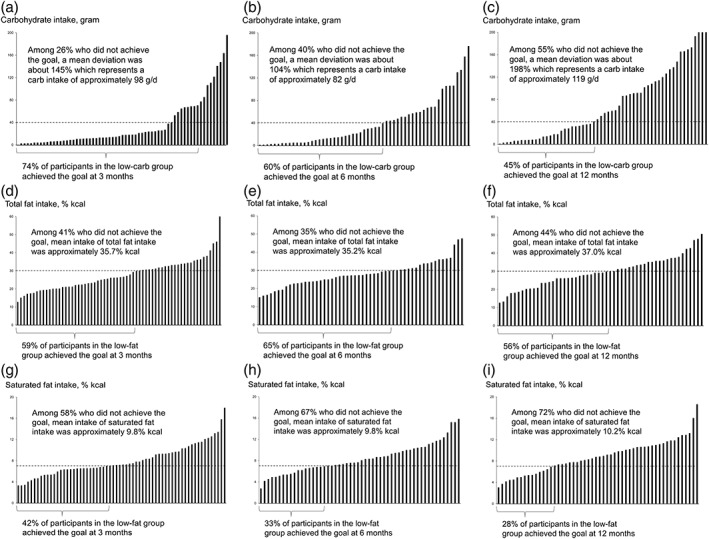
Deviation from macronutrient goal by follow‐up visit. (a–c) Carbohydrate goal at 3, 6 and 12 months, respectively, in the low‐carbohydrate group; (d–f) total fat goal at 3, 6 and 12 months, respectively, in the low‐fat group; and (g–i) saturated fat goal at 3, 6 and 12 months, respectively, in the low‐fat group.
Figure 2.
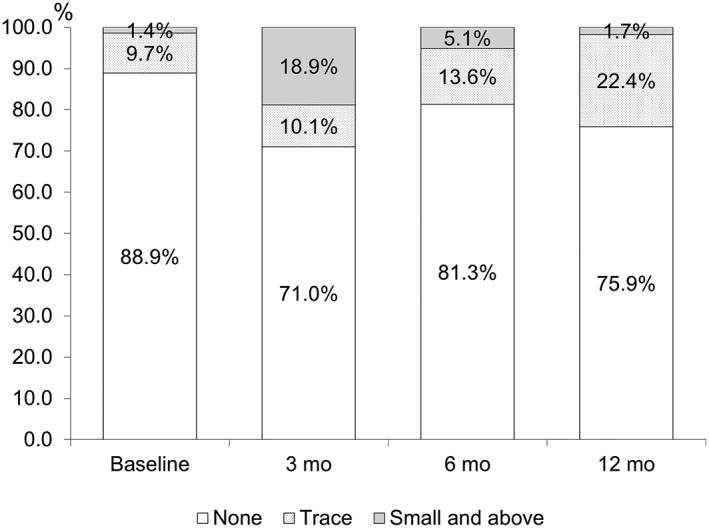
Categories of urinary ketone levels at 0, 3, 6 and 12 months in persons who followed a low‐carbohydrate diet. Ketone levels tended to be higher compared with baseline. P‐values for comparison (Fisher's exact test): 0.007 at 3 months, 0.17 at 6 months and 0.04 at 12 months.
Adherence indicators in relation to diet efficacy
In the low‐carbohydrate group, attendance at more dietary sessions, less deviation from carbohydrate goals and presence of urinary ketones at 6 and 12 months were consistently associated with greater reductions in body weight and percent fat mass and increase in percent lean mass (Table 2). Similarly, a one‐interquartile‐range increase in higher composite score reflecting adherence to a low‐carbohydrate diet was associated with more weight loss (β = −2.2 kg or 2.3%, P = 0.01), loss of fat mass (β = −1.1%, P = 0.008) and preservation of lean mass (β = 1.3%, P = 0.003). No consistent association was observed between indicators of adherence to a low‐carbohydrate diet and changes in blood pressure, lipids, glucose or C‐reactive protein at 12 months (Supporting Information Table 2). No associations between indicators of adherence and dietary efficacy were identified in the low‐fat group (Supporting Information Tables 3 and 4).
Table 2.
Regression coefficients (P‐values) for the association between adherence to diet and changes in body weight and body composition in the low‐carbohydrate diet group
| ∆ Body weight (kg) | ∆ Fat mass (%) | ∆ Lean mass (%) | |
|---|---|---|---|
| Percent attendance at dietary counselling | |||
| By session | |||
| Individual | 0.15 (0.22) | 0.01 (0.89) | −0.02 (0.68) |
| Biweekly group | −0.08 (0.03) | −0.04 (0.03) | 0.04 (0.01) |
| Monthly group | −0.08 (0.01) | −0.04 (0.005) | 0.04 (0.003) |
| By time | |||
| 3 months | −0.08 (0.21) | −0.05 (0.07) | 0.06 (0.04) |
| 6 months | −0.11 (0.04) | −0.05 (0.03) | 0.06 (0.01) |
| 12 months | −0.12 (0.01) | −0.06 (0.007) | 0.07 (0.003) |
| Mean of discrepancy of carbohydrate goal | |||
| 3 months | 5.1 (0.002) | 1.5 (0.07) | −1.5 (0.06) |
| 6 months | 4.0 (0.02) | 1.7 (0.03) | −1.6 (0.05) |
| 12 months | 5.0 (<0.001) | 1.5 (0.01) | −1.5 (0.02) |
| Percent ketones positive | |||
| 3 months | −12.0 (<0.001) | −5.1 (0.001) | 5.1 (<0.001) |
| 6 months | −14.5 (<0.001) | −6.4 (<0.001) | 6.5 (<0.001) |
| 12 months | −15.4 (<0.001) | −6.8 (0.001) | 7.0 (<0.001) |
| Composite score* | |||
| 3 months | −1.5 (0.22) | −1.1 (0.07) | 1.1 (0.04) |
| 6 months | −2.0 (0.04) | −0.9 (0.04) | 1.1 (0.01) |
| 12 months | −2.2 (0.01) | −1.1 (0.008) | 1.3 (0.003) |
A one‐interquartile‐range increase in composite adherence score, based on attendance at dietary session, deviation from macronutrient goals and ketone presence.
No significant interaction by race was detected in the associations of the composite adherence score with 12‐month changes in body weight, composition or any CVD risk factor in either diet group (all P‐values for interaction were >0.50). The results regarding the behavioural indicator were consistent after accounting for make‐up sessions in the analysis. The results were similar after replacing a low score with missing data on adherence. Further adjusting for body mass index, percent fat mass or lean mass at baseline did not change the results (data not shown).
Discussion
While it has been proposed that diets of various macronutrient compositions have similar efficacy for weight loss and CVD risk reduction and that the primary determinant of a diet's efficacy is individual adherence to dietary goals 16, the present study findings suggest that this may not entirely be the case. We observed similar measures of adherence to assigned diets in both the low‐carbohydrate and low‐fat groups throughout the trial, suggesting that differential adherence is unlikely to explain the difference in dietary efficacy between groups 21. More importantly, these findings indicate that greater adherence to a low‐fat, high‐carbohydrate diet was not associated with greater weight loss or improvement in CVD risk factors.
Diets that restrict intakes of total and saturated fat have been part of strategies for the prevention of obesity and CVD 8, 22, 23, 26. Since 1970s, the average level of fat intake as a percentage of daily energy intake has decreased from 37% and levelled off at approximately 33%, while the mean level of carbohydrate intake has correspondingly increased in the American adult population, from 42% to 48% for men and from 45% to 51% for women 27, 28. According to the data from the Women's Health Initiative, low‐fat dietary intervention was not associated with lower risk of clinical CVD events over 8 years of follow‐up, despite the achievement of dietary goals and clear separation between groups 29. Our finding that closer adherence to the low‐fat diet was not associated with greater reductions in CVD risk factors over 12 months is consistent with those of the Women's Health Initiative, which also observed only modest effects on CVD risk factors after a substantially longer period of time 29.
Adherence has been conceptualized as a multi‐dimensional construct, and no single measure of adherence has been deemed optimal 30. Attendance at counselling sessions has been widely used as an objective measure of behavioural adherence; however, it is not specific in conceptualizing dietary adherence because it is determined by many psychological and socioeconomic factors 31. Deviation from macronutrient goals as a measure of adherence is heavily dependent on self‐reported dietary recalls. The presence of urinary ketones is a widely used biochemical indicator to assess adherence to low‐carbohydrate diets; however, production of urinary ketones can be inconsistent at levels of carbohydrate intake tested in our study 32. A factor analysis using data from a weight loss trial identified two independent adherence factors clustering in the behavioural and nutritional realms and suggested the importance of integrating multiple components to describe the adherence construct more completely 31. In this study, we attempted to comprehensively describe adherence using multiple indicators. The associations we identified with primary outcomes were consistent across indicators of adherence in each within‐group analysis of our study.
Although adherence to prescribed diets that are aimed at reducing obesity and attenuating CVD seems to be important, few studies have systematically measured adherence to a low‐carbohydrate diet and examined its relationship with the success of the diet. One study examined dietary adherence as reflected by deviation from nutrient goals among premenopausal women (mostly White) who were assigned to either a prescribed commercial low‐carb diet, which included ≤20 g carbohydrate per day for first 2 months and ≤50 g carbohydrate per day thereafter, or a very low‐fat diet, which included ≤10% of total fat 19. In that study, at 12 months, participants in the most adherent tertile had significantly greater reduction in body weight than those in the least adherent tertile in the low‐carbohydrate group but not in the low‐fat group 19. Williamson and his colleagues assessed adherence to four weight loss diets with varying macronutrient compositions in the POUNDS LOST study; however, none of those diets was representative of a typical low‐carbohydrate diet 33. Our study extends previous findings by testing multiple indicators for adherence to a typical low‐carbohydrate diet and a conventional low‐fat diet, in a population with a substantial proportion of African–Americans, and further examined their relationship with changes in body composition and CVD risk factors.
Strengths of this study include a high completion rate, long duration, analysis of a relatively large, diverse population and multiple indicators of adherence to the assigned dietary regimens. Despite these strengths, some limitations are important to acknowledge. The assessment of nutritional adherence, as reflected by deviation from the nutrient goals, was based on multiple self‐reported 24‐h dietary recalls. This measurement may not represent the usual diet of the participant and thus may result in misclassification of usual intake of nutrients at the individual level. This measurement error is likely to be non‐differential. Urinary ketone sticks cannot assess ketone forms other than acetoacetate; however, urinary ketone assessment has been applied in various large dietary clinical trials for weight loss 13, 14, 15, 34. Because this is the first study to include a comprehensive list of adherence indicators, our composite adherence score has not yet been validated in other clinical trials. Given the number of tests performed in our primary analyses, statistically significant results should be interpreted with caution, particularly for those with P‐values close to 0.05. International Physical Activity Questionnaire is designed for population‐based studies rather than clinical trials. Finally, there is no validated biochemical indicator for adherence to low‐fat diets.
Our findings do not support the conclusion that all weight loss diets are equally effective and that individuals should choose a diet based on the ease of adherence. Given the profusion of low‐fat and reduced‐fat food products in the US marketplace, adherence to a low‐fat diet may be substantially easier than adherence to other dietary patterns; however, the results of our study suggest that important differences in efficacy do exist between diets. In the real practice, if a low‐carbohydrate diet is not tolerated or feasible for an individual, a low‐fat diet should not be recommended as an alternative. In conclusion, despite similar adherence between low‐carbohydrate and low‐fat diets, a low‐carbohydrate diet resulted in greater weight loss and improvement in body composition at 12 months. In contrast, a low‐fat diet was not associated with greater weight loss in this study.
Conflict of Interest Statement
No Conflict of Interest Statement
Author Contributions
T. H. and L. A. B. designed research; L. Y. and L. A. B. conducted research; T. H. and L. Y. analysed data; T. H. and L. A. B. wrote the paper; and L. Y., S. L., T. N., J. H., P. K. W. and L. M. S. revised and edited manuscript and provided critical comments. L. A. B. had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
Grants were given from the National Center for Research Resources of the National Institutes of Health (NIH/NCRR P20‐RR017659) to the Tulane University Hypertension and Renal Center of Excellence.
Disclosure
None.
Supporting information
Supporting info item
Acknowledgement
The authors thank the study participants for their cooperation.
Hu, T. , Yao, L. , Reynolds, K. , Niu, T. , Li, S. , Whelton, P. K. , He, J. , Steffen, L. M. , and Bazzano, L. A. (2016) Adherence to low‐carbohydrate and low‐fat diets in relation to weight loss and cardiovascular risk factors. Obesity Science & Practice, 2: 24–31. doi: 10.1002/osp4.23.
Trial registration: clinicaltrials.gov Identifier: NCT00609271
References
- 1. Mozaffarian D, Benjamin EJ, Go AS et al. Heart disease and stroke statistics‐2015 update: a report from the American Heart Association. Circulation 2015; 131: e29–e322. [DOI] [PubMed] [Google Scholar]
- 2. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999‐2010. JAMA 2012; 307: 491–497. [DOI] [PubMed] [Google Scholar]
- 3. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011‐2012. JAMA 2014; 311: 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960‐1994. Int J Obes Relat Metab Disord 1998; 22: 39–47. [DOI] [PubMed] [Google Scholar]
- 5. Eckel RH, Jakicic JM, Ard JD et al. AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129: 576–599. [Google Scholar]
- 6. Jensen MD, Ryan DH, Apovian CM et al. AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. Circulation 2014; 129: S108–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. NHLBI . Obesity education initiative expert panel on the identification, evaluation, and treatment of overweight and obesity in adults. Clinical Guidelines of the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults 1998; 98‐4083.
- 8. U.S. Department of Agriculture and U.S. Department of Health and Human Services . Dietary Guidelines for Americans, 2010, 7th edn December 2010. [Google Scholar]
- 9. Nordmann AJ, Nordmann A, Briel M et al. Effects of low‐carbohydrate vs low‐fat diets on weight loss and cardiovascular risk factors: a meta‐analysis of randomized controlled trials. Arch Intern Med 2006; 166: 285–293. [DOI] [PubMed] [Google Scholar]
- 10. Hu T, Mills KT, Yao L et al. Effects of low‐carbohydrate diets versus low‐fat diets on metabolic risk factors: a meta‐analysis of randomized controlled clinical trials. Am J Epidemiol 2012; 176: S44–S54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Santos FL, Esteves SS, da Costa Pereira A, Yancy WS Jr, Nunes JP. Systematic review and meta‐analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev 2012; 13: 1048–1066. [DOI] [PubMed] [Google Scholar]
- 12. de Souza RJ, Bray GA, Carey VJ et al. Effects of 4 weight‐loss diets differing in fat, protein, and carbohydrate on fat mass, lean mass, visceral adipose tissue, and hepatic fat: results from the POUNDS LOST trial. Am J Clin Nutr 2012; 95: 614–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sacks FM, Bray GA, Carey VJ et al. Comparison of weight‐loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009; 360: 859–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shai I, Schwarzfuchs D, Henkin Y et al. Weight loss with a low‐carbohydrate, Mediterranean, or low‐fat diet. New Engl J Med 2008; 359: 229–241. [DOI] [PubMed] [Google Scholar]
- 15. Foster GD, Wyatt HR, Hill JO et al. Weight and metabolic outcomes after 2 years on a low‐carbohydrate versus low‐fat diet: a randomized trial. Ann Intern Med 2010; 153: 147–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Johnston BC, Kanters S, Bandayrel K et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta‐analysis. JAMA 2014; 312: 923–933. [DOI] [PubMed] [Google Scholar]
- 17. Pagoto SL, Appelhans BM. A call for an end to the diet debates. JAMA 2013; 310: 687–688. [DOI] [PubMed] [Google Scholar]
- 18. Popular diets equally effective for losing weight. J Fam Pract 2005; 54: 306. [PubMed] [Google Scholar]
- 19. Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: results from the A TO Z weight loss study. Int J Obes (Lond) 2008; 32: 985–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Greenberg I, Stampfer MJ, Schwarzfuchs D, Shai I, DIRECT Group . Adherence and success in long‐term weight loss diets: the dietary intervention randomized controlled trial (DIRECT). J Am Coll Nutr 2009; 28: 159–168. [DOI] [PubMed] [Google Scholar]
- 21. Bazzano LA, Hu T, Reynolds K et al. Effects of low‐carbohydrate and low‐fat diets: a randomized trial. Ann Intern Med 2014; 161: 309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Cholesterol Education Program (NCEP) . Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002; 106: 3143–3421. [PubMed] [Google Scholar]
- 23. American Heart Association (AHA) . AHA Dietary Guidelines Revision 2000: a statement for healthcare professionals from the Nutrition Committee of the AHA 2000; 102: 2284‐2299. [DOI] [PubMed]
- 24. Nutrition Data System for Research . The Minnesota Nutrition Data System. University of Minnesota 2005.
- 25. Craig CL, Marshall AL, Sjostrom M et al. International physical activity questionnaire: 12‐country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395. [DOI] [PubMed] [Google Scholar]
- 26. American Heart Association Nutrition Committee , Lichtenstein AH, Appel LJ et al Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006; 114: 82–96. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Disease Control and Prevention (CDC) . Trends in intake of energy and macronutrients – United States, 1971‐2000. MMWR Morb Mortal Wkly Rep 2004; 53: 80–82. [PubMed] [Google Scholar]
- 28. Wright JD, Wang CY. Trends in intake of energy and macronutrients in adults from 1999‐2000 through 2007‐2008. NCHS Data Brief 2010; 49: 1–8. [PubMed] [Google Scholar]
- 29. Howard BV, Van Horn L, Hsia J et al. Low‐fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006; 295: 655–666. [DOI] [PubMed] [Google Scholar]
- 30. World Health Organization . Adherence to Long‐term Therapies: Evidence for Action. World Health Organization: Geneva, 2003. Switzerland 2003. [Google Scholar]
- 31. Williamson DA, Anton SD, Han H et al. Adherence is a multi‐dimensional construct in the POUNDS LOST trial. J Behav Med 2010; 33: 35–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hu T, Bazzano LA. The low‐carbohydrate diet and cardiovascular risk factors: evidence from epidemiologic studies. Nutr Metab Cardiovasc Dis 2014; 24: 337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Williamson DA, Anton SD, Han H et al. Early behavioral adherence predicts short and long‐term weight loss in the POUNDS LOST study. J Behav Med 2010; 33: 305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Laffel L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev 1999; 15: 412–426. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting info item


