Abstract
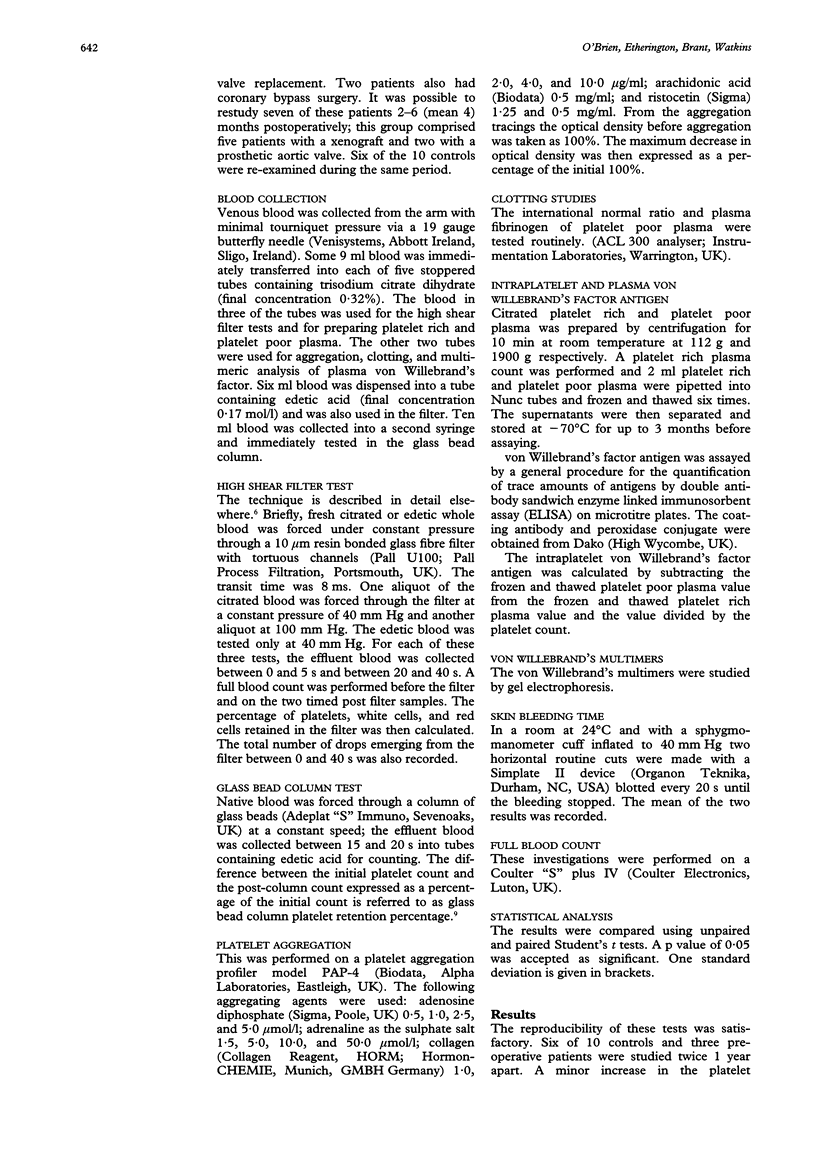
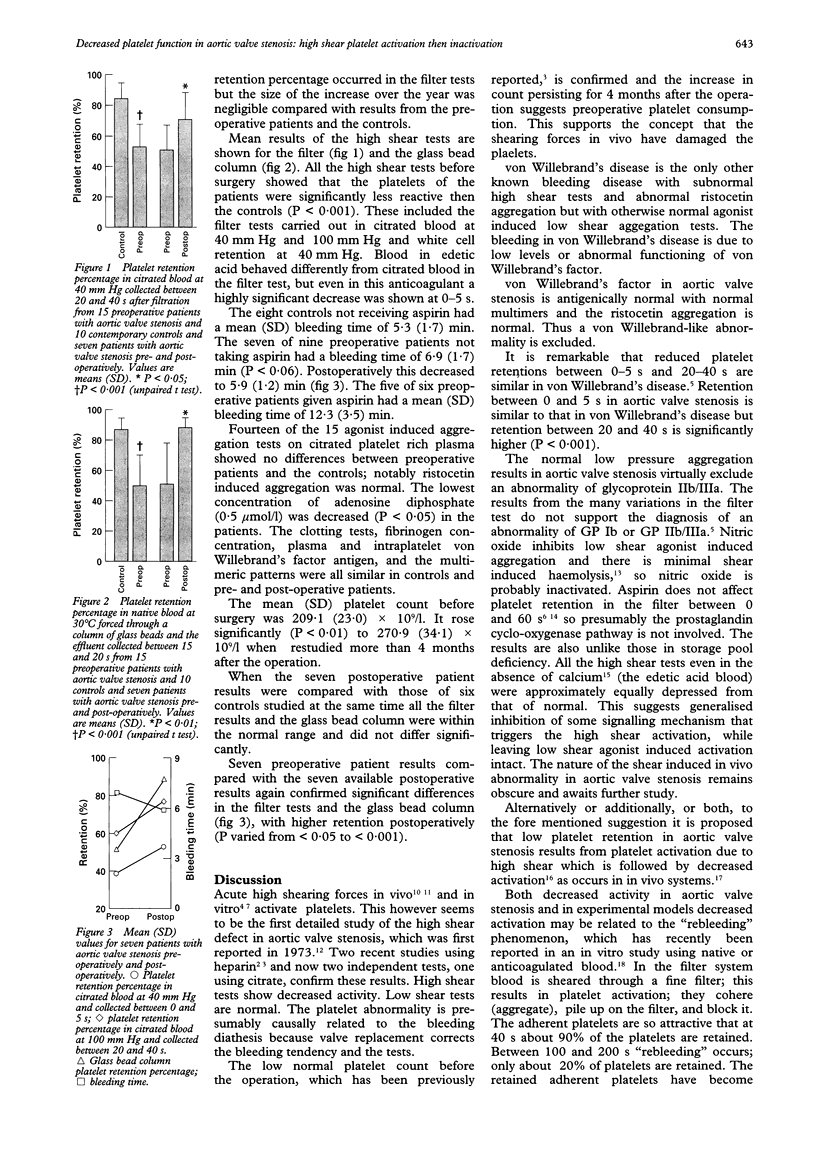
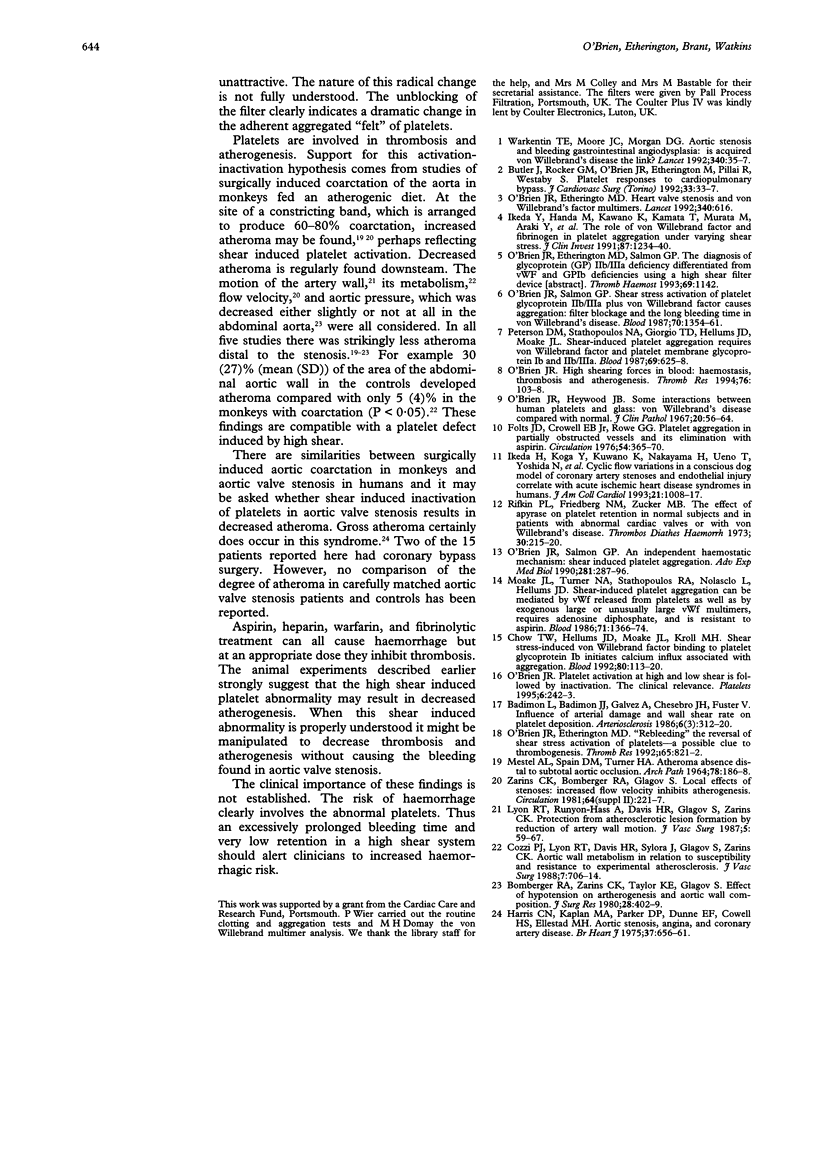
OBJECTIVE--To elucidate the mechanism of the bleeding tendency observed in patients with aortic valve stenosis. DESIGN--A prospective study of high and low shear platelet function tests in vitro in normal controls compared with that in patients with severe aortic valve stenosis with a mean (SD) systolic gradient by Doppler of 75 (18) mm Hg before and at least 4 months after aortic valve replacement. SETTING--District general hospital. RESULTS--The patients showed reduced retention in the high shear platelet function tests. (a) Platelet retention in the filter test was 53.6 (12.6)% in patients with aortic valve stenosis and 84.8 (9.6)% in the controls (P < 0.001). (b) Retention in the glass bead column test was 49.8 (19.2) in the patients and 87.4 (8.7) in the controls (P < 0.001). (c) The standard bleeding time was longer in the patients (P < 0.06). Results of the high shear tests (a, b, and c) after aortic valve replacement were within the normal range. The platelet count was low but within the normal range before surgery and increased postoperatively (P < 0.01). There were no differences in the results of standard clotting tests, plasma and intraplatelet von Willebrand's factor, or in 15 platelet aggregation tests using five agonists between patients with aortic valve stenosis and controls. CONCLUSIONS--The high shear haemodynamics of aortic valve stenosis modify platelet function in vivo predisposing to a bleeding tendency. This abnormality of platelet function is detectable only in vitro using high shear tests. The abnormal function is reversed by aortic valve replacement. High shear forces in vitro activate and then inactivate platelets. By the same mechanisms aortic valve stenosis seems to lead to high shear damage in vivo, resulting in a clinically important bleeding tendency in some patients.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Badimon L., Badimon J. J., Galvez A., Chesebro J. H., Fuster V. Influence of arterial damage and wall shear rate on platelet deposition. Ex vivo study in a swine model. Arteriosclerosis. 1986 May-Jun;6(3):312–320. doi: 10.1161/01.atv.6.3.312. [DOI] [PubMed] [Google Scholar]
- Bomberger R. A., Zarins C. K., Taylor K. E., Glagov S. Effect of hypotension on atherogenesis and aortic wall composition. J Surg Res. 1980 May;28(5):402–409. doi: 10.1016/0022-4804(80)90102-x. [DOI] [PubMed] [Google Scholar]
- Butler J., Rocker G. M., O'Brien J. R., Etherington M., Pillai R., Westaby S. Platelet responses to cardiopulmonary bypass. Assessment by a shear stress activation technique. J Cardiovasc Surg (Torino) 1992 Jan-Feb;33(1):33–37. [PubMed] [Google Scholar]
- Chow T. W., Hellums J. D., Moake J. L., Kroll M. H. Shear stress-induced von Willebrand factor binding to platelet glycoprotein Ib initiates calcium influx associated with aggregation. Blood. 1992 Jul 1;80(1):113–120. [PubMed] [Google Scholar]
- Cozzi P. J., Lyon R. T., Davis H. R., Sylora J., Glagov S., Zarins C. K. Aortic wall metabolism in relation to susceptibility and resistance to experimental atherosclerosis. J Vasc Surg. 1988 May;7(5):706–714. [PubMed] [Google Scholar]
- Folts J. D., Crowell E. B., Jr, Rowe G. G. Platelet aggregation in partially obstructed vessels and its elimination with aspirin. Circulation. 1976 Sep;54(3):365–370. doi: 10.1161/01.cir.54.3.365. [DOI] [PubMed] [Google Scholar]
- Harris C. N., Kaplan M. A., Parker D. P., Dunne E. F., Cowell H. S., Ellestad M. H. Aortic stenosis, angina, and coronary artery disease. Interrelations. Br Heart J. 1975 Jun;37(6):656–661. doi: 10.1136/hrt.37.6.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda H., Koga Y., Kuwano K., Nakayama H., Ueno T., Yoshida N., Adachi K., Park I. S., Toshima H. Cyclic flow variations in a conscious dog model of coronary artery stenosis and endothelial injury correlate with acute ischemic heart disease syndromes in humans. J Am Coll Cardiol. 1993 Mar 15;21(4):1008–1017. doi: 10.1016/0735-1097(93)90361-4. [DOI] [PubMed] [Google Scholar]
- Ikeda Y., Handa M., Kawano K., Kamata T., Murata M., Araki Y., Anbo H., Kawai Y., Watanabe K., Itagaki I. The role of von Willebrand factor and fibrinogen in platelet aggregation under varying shear stress. J Clin Invest. 1991 Apr;87(4):1234–1240. doi: 10.1172/JCI115124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon R. T., Runyon-Hass A., Davis H. R., Glagov S., Zarins C. K. Protection from atherosclerotic lesion formation by reduction of artery wall motion. J Vasc Surg. 1987 Jan;5(1):59–67. [PubMed] [Google Scholar]
- MESTEL A. L., SPAIN D. M., TURNER H. A. ATHEROMA ABSENCE DISTAL TO SUBTOTAL AORTA OCCLUSION. Arch Pathol. 1964 Sep;78:186–188. [PubMed] [Google Scholar]
- Moake J. L., Turner N. A., Stathopoulos N. A., Nolasco L., Hellums J. D. Shear-induced platelet aggregation can be mediated by vWF released from platelets, as well as by exogenous large or unusually large vWF multimers, requires adenosine diphosphate, and is resistant to aspirin. Blood. 1988 May;71(5):1366–1374. [PubMed] [Google Scholar]
- O'Brien J. R., Etherington M. D. "Rebleeding" the reversal of shear stress activation of platelets--a possible clue to thrombogenesis. Thromb Res. 1992 Mar 15;65(6):821–822. doi: 10.1016/0049-3848(92)90121-p. [DOI] [PubMed] [Google Scholar]
- O'Brien J. R., Etherington M. D. Heart valve stenosis and von Willebrand's factor multimers. Lancet. 1992 Sep 5;340(8819):616–616. doi: 10.1016/0140-6736(92)92155-9. [DOI] [PubMed] [Google Scholar]
- O'Brien J. R., Heywood J. B. Some interactions between human platelets and glass: von Willebrand's disease compared with normal. J Clin Pathol. 1967 Jan;20(1):56–64. doi: 10.1136/jcp.20.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien J. R. High shearing forces in blood: haemostasis, thrombosis and atherogenesis. Thromb Res. 1994 Oct 1;76(1):103–108. doi: 10.1016/0049-3848(94)90212-7. [DOI] [PubMed] [Google Scholar]
- O'Brien J. R., Salmon G. P. An independent haemostatic mechanism: shear induced platelet aggregation. Adv Exp Med Biol. 1990;281:287–296. doi: 10.1007/978-1-4615-3806-6_30. [DOI] [PubMed] [Google Scholar]
- O'Brien J. R., Salmon G. P. Shear stress activation of platelet glycoprotein IIb/IIIa plus von Willebrand factor causes aggregation: filter blockage and the long bleeding time in von Willebrand's disease. Blood. 1987 Nov;70(5):1354–1361. [PubMed] [Google Scholar]
- Peterson D. M., Stathopoulos N. A., Giorgio T. D., Hellums J. D., Moake J. L. Shear-induced platelet aggregation requires von Willebrand factor and platelet membrane glycoproteins Ib and IIb-IIIa. Blood. 1987 Feb;69(2):625–628. [PubMed] [Google Scholar]
- Rifkin P. L., Friedberg N. M., Zucker M. B. The effect of apyrase on platelet retention in normal subjects and in patients with abnormal cardiac valves or with von Willebrand's disease. Thromb Diath Haemorrh. 1973 Sep 15;30(1):215–220. [PubMed] [Google Scholar]
- Warkentin T. E., Moore J. C., Morgan D. G. Aortic stenosis and bleeding gastrointestinal angiodysplasia: is acquired von Willebrand's disease the link? Lancet. 1992 Jul 4;340(8810):35–37. doi: 10.1016/0140-6736(92)92434-h. [DOI] [PubMed] [Google Scholar]



