Abstract
Oligodendrocytes readily regenerate and replace myelin membranes around axons in the adult mammalian central nervous system (CNS) following injury. The ability to regenerate oligodendrocytes depends on the availability of neural progenitors called oligodendrocyte precursor cells (OPCs) in the adult CNS that respond to injury-associated signals to induce OPC expansion followed by oligodendrocyte differentiation, axonal contact and myelin regeneration (remyelination). Remyelination ensures the maintenance of axonal conduction, and the oligodendrocytes themselves provide metabolic factors that are necessary to maintain neuronal integrity. Recent advances in oligodendrocyte regeneration research are beginning to shed light on critical intrinsic signals, as well as extrinsic, environmental factors that regulate the distinct steps of oligodendrocyte lineage progression and myelin replacement under CNS injury. These studies may offer novel pharmacological targets for regenerative medicine in inflammatory demyelinating disorders in the CNS such as multiple sclerosis.
1. Introduction
Oligodendrocytes are glial cells that extend myelin membranes around axons in the central nervous system (CNS). In between myelin segments are unmyelinated axonal regions termed nodes of Ranvier, where sodium channels involved in action potential generation are clustered. This exquisite organization defines the typical vertebrate nerve fiber and is crucial for saltatory propagation of electrical impulses down the axon, enabling rapid communication between networks of nerve cells in the CNS (Bhatt et al., 2014; Frankenhaeuser, 1952; Hartline and Colman, 2007). In addition to increasing axonal conduction speed through generating myelin, oligodendrocytes secrete metabolic factors that maintain the integrity and survival of CNS neurons (Edgar et al., 2009; Fünfschilling et al., 2012; Griffiths et al., 1998; Lee et al., 2012; Oluich et al., 2012). Disturbances to oligodendrocyte function or myelination in the developing or injured brain impairs axonal conduction (Waxman, 2006) and is associated with neuronal degeneration (Haines et al., 2009), highlighting the importance of oligodendrocytes in maintaining CNS function.
One of the most intriguing features of the adult CNS is its ability to spontaneously regenerate oligodendrocytes and replace myelin (remyelination) following acute demyelination (Franklin and Ffrench-Constant, 2008). Oligodendrocyte regeneration is possible because of an abundantly distributed source of oligodendrocyte precursor cells (OPCs) in the adult CNS (Dawson et al., 2003; Horner et al., 2002; Pringle et al., 1992; van Wijngaarden and Franklin, 2013). Following demyelination, neighboring OPCs rapidly migrate to the site of injury where they differentiate into oligodendrocytes to remyelinate recently denuded axons. This spontaneous regenerative response restores saltatory conduction (Smith et al., 1979) and has been suggested to protect axons from degeneration (Irvine and Blakemore, 2008; Jeffery and Blakemore, 1997; Kornek et al., 2000). Failure to regenerate oligodendrocytes and replace myelin exacerbates axonal dysfunction from myelin loss, leading to a cascade of pathological events that ultimately concludes with neurodegeneration (Trapp and Stys, 2009). Clinical manifestations of acute CNS demyelination followed by spontaneous remyelination, as well as the progressive neurodegeneration associated with remyelination failure, are most evident in the chronically demyelinating disorder, multiple sclerosis (MS).
MS is an immune-mediated neurological disease affecting more than 2.3 million people worldwide (Milo and Kahana, 2010; Compston and Coles, 2011). For reasons that remain poorly understood, myelin membranes and oligodendrocytes are destroyed through chronic inflammation in the CNS. Although efficient oligodendrocyte regeneration and remyelination occurs in the early stages of MS, remyelination becomes inefficient and ultimately fails with disease progression (Franklin, 2008). The mechanism of remyelination failure remains unclear, however it has been hypothesized that OPCs become “stalled” and may fail to differentiate into mature oligodendrocytes at sites of lesions (for review see Franklin, 2002). Since remyelination restores axonal conduction and protects against axonal damage in rodent models of MS (Irvine and Blakemore, 2008; Jeffery and Blakemore, 1997; Kornek et al., 2000), it is hypothesized that pro-remyelination therapies may be beneficial for patients with MS. In order to understand the biology of remyelination and to develop therapies to enhance this process in MS, several models of experimental demyelination are used. We have provided an abbreviated description of the most widely used model systems in Table 1. More thorough reviews have been published elsewhere (Blakemore and Franklin, 2008; Pachner, 2011; Rodriguez, 2007; Tanaka and Yoshida, 2014). In this review we discuss the neuroprotective functions of oligodendrocytes, molecular pathways involved in regulating their regeneration, and possible therapeutic targets for promoting remyelination in the CNS.
Table 1.
Animal Models of Experimental Demyelination
| Model | Mechanism | Aspect(s) of MS Modeled |
Pros | Cons |
|---|---|---|---|---|
| Autoimmune experimental autoimmune/ allergic encephalomy- elitis (EAE) |
Co-injection of pertussis toxin and a specific myelin protein (MOG,MBP, or PLP) causes myelin destruction mediated primarily by invasion of peripheral antigen-specific T cells. |
|
||
| Theiler’s murine encephalomy elitis virus (TMEV) |
Intracerebral infection with TMEV in susceptible mouse strains leads to chronic demyelination primarily in the spinal cord. |
|
|
|
| Toxin Induced Models: | ||||
| Lysolecithin | Focal injection of 1% lysolecithin, an activator of phospholipase A2, into the spinal cord produces local demyelination. |
|
|
|
| Cuprizone | Administration of 0.2% cuprizone, a copper chelator, in the chow leads to mitochondrial complex IV dysfunction and oligodendrocyte toxicity, leading to demyelination in the corpus callosum and hippocampus. |
|
|
|
2. Role of oligodendrocytes in myelination and neuroprotection
Oligodendrocytes extend myelin sheaths around axons in a stereotyped fashion, leaving intermittent gaps of unmyelinated axon, termed nodes of Ranvier, between adjacent myelinated segments or internodes. This precise organization enables the restriction of voltage gated sodium channels to nodes of Ranvier and voltage gated potassium channels to areas called juxtaparanodes (Pedraza et al., 2001; Rasband, 2010, 2008). Demyelination disrupts ion channel segregation (Coman et al., 2006; Wolswijk and Balesar, 2003), such that sodium and potassium channels redistribute along the axon, causing overlap of paranodal and juxtaparanodal protein domains (Craner et al., 2004; England et al., 1990; Podbielska et al., 2013; Scherer and Arroyo, 2002). The diffusion of ion channels and increased membrane capacitance from myelin loss produce an impedance mismatch in demyelinated axons, which causes inefficient conduction (Waxman, 2006). In MS, the manifestation of impaired impulse conduction is frequently associated with functional and/or cognitive disabilities, highlighting the importance of intact myelin around CNS axons for mediating efficient communication between neural networks (Charil et al., 2003).
In addition to their role in myelination, recent studies have found that oligodendrocytes play a critical role in maintaining axonal integrity (Edgar et al., 2009; Griffiths et al., 1998; Lappe-Siefke et al., 2003; Nave and Trapp, 2008; Nave, 2010; Saab et al., 2013). For example, mice deficient in proteolipid protein (PLP1) or CNP, major oligodendrocyte proteins found in myelin, do not display obvious structural abnormalities in myelin, but display impaired axonal transport (Edgar et al., 2010, 2009). Moreover, targeted ablation of oligodendrocytes in mice resulted in axonal pathology (Oluich et al., 2012; Traka et al., 2010). Exactly how oligodendrocytes maintain axonal integrity remains unclear. Several studies have observed that mitochondrial density in axons increases significantly in demyelinated lesions in MS and after experimental demyelination in mice, suggesting that the presence of myelin or oligodendrocytes may be important in regulating axonal energy metabolism (Campbell et al., 2012; Kiryu-Seo et al., 2010; Mutsaers and Carroll, 1998; Traka et al., 2010; Zambonin et al., 2011). It is possible that oligodendrocytes provide metabolic factors to the axon in order to meet its high energetic demand, and that the absence of oligodendrocyte support may render neurons vulnerable to oxidative damage and cell death (Nave, 2010). Indeed, recent studies have found that lactate transport to neurons is crucial for maintaining neuronal health and survival (Fünfschilling et al., 2012; Lee et al., 2012). The downregulation of the lactate transporter MCT1 in oligodendrocytes has recently been shown to result in impaired lactate transport, leading to neuronal dysfunction and degeneration (Lee et al., 2012).
In addition to supporting axonal energy metabolism, oligodendrocytes may also regulate neuronal survival through the production of neurotrophic factors. Several previous studies have suggested that oligodendrocytes express brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), and neurotrophin-3 (NT-3) mRNA (Byravan et al., 1994; Dai et al., 2003; Dougherty et al., 2000; Gonzalez et al., 1990; Zhang et al., 2014). Moreover, BDNF and NT-3 secretion from oligodendrocytes have been shown to enhance the function of basal forebrain neurons in vitro, by increasing the expression choline acetyltransferase (ChAT) (Dai et al., 2003). Moreover, oligodendrocytes may also express glial cell line-derived neurotrophic factor (GDNF) and insulin-like growth factor type-1 (IGF1), and both factors have been shown to enhance cortical neuron survival (Wilkins et al., 2003; Zhang et al., 2014; Wilkins et al., 2001; Zhang et al., 2014; Wilkins and Compston, 2005; Wilkins et al., 2001). However, most of these studies were performed in vitro, so further studies are needed to understand the role of neurotrophic factors and IGF1 in oligodendrocyte-mediated neuronal survival in vivo.
3. Drivers of disease progression: axon damage and neurodegeneration
Considering the many roles of oligodendrocytes in supporting neuronal health, it may not be surprising that remyelination failure in progressive MS is accompanied by neurodegeneration (Compston and Coles, 2008; Dutta and Trapp, 2011; Haines et al., 2009; Nave and Trapp, 2008). It is hypothesized that the degeneration of axons in the chronically demyelinated CNS is a cause of irreversible disability (Mahad et al., 2015; Wegner et al., 2006). The evidence for axonal damage in MS is robust and comes from clinical, histopathological, biochemical, and imaging studies (for review see Haines et al., 2011; Trapp and Nave, 2008). Notably, although current immunosuppressive therapies reduce the number of relapses, they do not prevent patients from progressing (Carrithers, 2014; Rice CM, 2014) or developing significant cortical atrophy (Sailer et al., 2003). In fact, early in the disease, brain atrophy positively correlates with subsequent disability progression (Fisher et al., 2002; Rudick et al., 1999). MS patients with permanent paralysis are estimated to have between 60-70% axonal loss (Bjartmar et al., 2000; Mews et al., 1998) and this finding is closely recapitulated in the chronic EAE model, in which mice with permanent paralysis exhibit 59% and 43% axonal loss in the cervical and lumbar spinal cord, respectively (Wujek et al., 2002). Histologically, acute axon damage is characterized by the presence of varicosities and spheroid structures (Saxena and Caroni, 2007), which reflect impaired organelle transport in the axon (Williamson and Cleveland, 1999). This impairment results in the accumulation of proteins, including amyloid precursor protein (APP), along the damaged axon. APP accumulation is present in active, remyelinating, and inactive MS lesions (Bitsch et al., 2000; Ferguson et al., 1997). A second marker of neurodegeneration, non-phosphorylated neurofilament heavy chain (NFH), also accumulates in neurons in MS lesions (Dziedzic et al., 2010; Gray et al., 2012; Petzold et al., 2008; Schirmer et al., 2011).
Axon damage occurs in both acute demyelinating lesions and in chronically demyelinated lesions (Ciccarelli et al., 2014; Ferguson et al., 1997; Trapp et al., 1998), however it remains unknown whether this is a consequence of direct inflammatory attack, secreted inflammatory mediators, or is a secondary effect of demyelination (Haines et al., 2011; Trapp et al., 1998). Observations of neuronal loss and dendritic atrophy in normal appearing white matter (NAWM) (Bjartmar et al., 2000; Trapp et al., 1998; Wood et al., 2012), and in normal appearing gray matter (NAGM) (Klaver et al., 2015) suggest an early pathogenic mechanism. A growing body of evidence suggests that energetic failure and oxidative stress may be a driving factor of neurodegeneration (Trapp and Stys, 2009), as abnormalities in mitochondria density, morphology, and activity are consistently found in models of MS (Campbell et al., 2014; Fischer et al., 2012; Joshi et al., 2015; Kiryu-Seo et al., 2010; Mahad et al., 2008, 2009; Qi et al., 2006; Witte et al., 2014, 2010, 2009). The exact cause of neurodegeneration in MS remains to be seen, however the demonstration that early axonal damage can be reversed with remyelination (Bjartmar et al., 2003; Nikić et al., 2011) strengthens the rationale that pro-remyelination therapies could be beneficial for the treatment of MS.
4. Restoring function: mediators of oligodendrocyte regeneration and remyelination
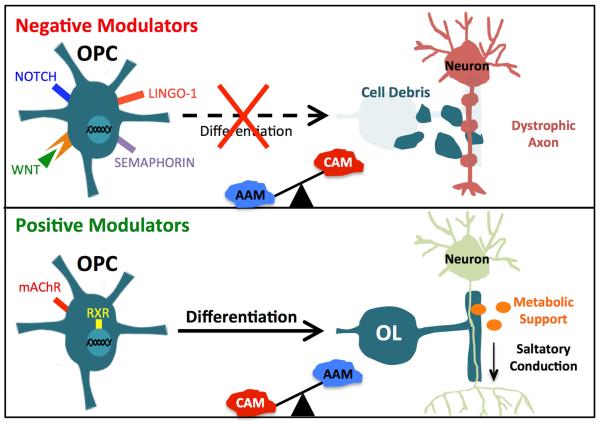
Remyelination is remarkably prolific in the early stages of MS (Franklin 2002, Goldschmidt et al., 2009; Patrikios et al., 2006), but becomes less efficient with disease progression for unknown reasons (Goldschmidt et al., 2009; Franklin 2002). While OPCs continue to be recruited to demyelinated regions in approximately 70% of lesions (Chang et al., 2002; Lucchinetti et al., 1999), their differentiation into re-myelinating cells is halted (Back et al., 2005; Charles et al., 2002, 2000; Fancy et al., 2010; Mi et al., 2005). Thus, it was hypothesized that impairment of OPC differentiation contributes to remyelination failure (Chang et al., 2002; Huang and Franklin, 2011; Kuhlmann et al., 2008; Wolswijk, 1998). Here, we will describe the role of intrinsic signaling pathways known to regulate OPC differentiation and how this process is influenced by extrinsic signals from the surrounding inflammatory milieu (Figure 1).
Figure 1.
Negative modulators of remyelination include Notch, Wnt, Lingo, and Semaphorin signaling as well as extracellular debris. Positive modulators of remyelination include muscarinic acetylcholine receptor (mAChR) and retinoid X receptor (RXR) signaling. Remyelination efficiency is also dependent on extrinsic factors, including those secreted by classically activated (CAM) and alternatively activated (AAM) macrophages/microglia, and a balance between CAM and AAM appears to modulate the regenerative process. Since myelin is necessary for saltatory conduction and oligodendrocytes provide metabolic support to neurons, chronic demyelination and oligodendrocyte loss in MS are likely to contribute to axonal dystrophy and progressive neurodegeneration.
4a. Intrinsic mediators of OPC differentiation
Several molecular pathways have been implicated in the inhibition of OPC differentiation. It is likely that transcriptional repression of these inhibitory pathways, combined with transcriptional activation of myelin genes, regulates OPC differentiation (Li et al., 2009). Here, we discuss the most widely studied inhibitory pathways including LINGO-1, canonical Notch, canonical wingless (Wnt), and semaphorin signaling. In addition, we discuss the few signaling cascades known to stimulate endogenous oligodendrocyte regeneration, including RXR and muscarinic receptor signaling pathways.
LINGO-1 Signaling
LINGO-1 (leucine-rich repeat and immunoglobulin-like domain-containing nogo receptor-interacting protein 1), a membrane protein expressed in neurons and oligodendrocytes, negatively regulates oligodendrocyte differentiation in rodent (Ji et al., 2006; Lee et al., 2007; Mi et al., 2005) and zebrafish (Yin and Hu, 2014). LINGO-1 knockout mice exhibit enhanced myelin sheath formation and recovery from EAE (Mi et al., 2007, 2005). Similarly, treatment with a LINGO-1 antagonist results in increased OPC differentiation and enhanced remyelination following EAE and lysolecithin-mediated demyelination (Mi et al., 2009), suggesting that LINGO-1 inhibition may be a useful therapeutic approach. Indeed, anti-LINGO-1 antibody promotes remyelination following lysolecithin-mediated demyelination (Zhang et al., 2015) and excitingly, has proven safe and well tolerated in patients (Tran et al., 2014). Now in a Phase II randomized clinical trial, LINGO-1 antibody may become the first available MS drug for promoting remyelination (Rudick et al., 2008). Precisely how LINGO-1 exerts its pro-regenerative effect in models of MS remains to be seen. A recent study demonstrated that LINGO-1 inhibition of oligodendrocyte differentiation may be due to decreased lipid raft translocation of the tyrosine kinase receptor ErbB2 (Lee et al., 2014). The ErbB receptor family, which also includes epidermal growth factor receptor (EGFR) and the neuregulin receptors, ErbB3 and ErbB4, has been implicated in the modulation of oligodendrocyte differentiation and myelination, albeit in a convoluted manner. ErbB2 deficiency halts oligodendrocyte lineage cells in an early stage leading to reductions in terminally differentiated oligodendrocytes (Kim et al., 2003; Park et al., 2001). While ErbB3 and ErbB4 are not required for oligodendrocyte differentiation (Brinkmann et al., 2008; Stolt et al., 2002; Sussman et al., 2005), ErbB3 may mediate experience-dependent myelination (Makinodan et al., 2012). At this point, it remains unclear whether targeting ErbB receptors would improve outcome in models of MS. Results from the anti-LINGO-1 clinical trial should inform the future direction of research in this area.
Canonical Notch Signaling
The Notch receptors are a family of transmembrane proteins that are cleaved when activated to modulate gene expression (Brosnan and John, 2009; D’Souza et al., 2008). It is generally established that canonical Notch signaling, which occurs through ligands such as Jagged, inhibits OPC differentiation during development. Activation of Notch1 receptors on OPCs inhibits their differentiation in vitro (Wang et al., 1998) and inhibition of Notch1 in OPCs disrupts the spatial and temporal regulation of oligodendrocyte differentiation in the spinal cord (Genoud et al., 2002). Further, mice heterozygous for the null allele of Notch1 exhibit premature oligodendrocyte differentiation and increased myelination (Givogri et al., 2002). Genetic inactivation of Notch1 in OPCs produces a similar phenotype characterized by premature OPC differentiation (Zhang et al., 2009). Although these studies suggest that Notch1 controls the time-course of OPC differentiation during development, its role in CNS remyelination appears more convoluted. Mice undergo complete spontaneous remyelination (Stidworthy et al., 2004) despite re-expression of Notch1 and Jagged1 in demyelinated lesions (John et al., 2002; Seifert et al., 2007; Stidworthy et al., 2004), bringing into question the role of this signaling pathway in remyelination. Genetic inactivation of Notch1 in OPCs has yielded conflicting results (Stidworthy et al., 2004; Zhang et al., 2009), however Hammond et al. recently demonstrated that OPC differentiation following lysolecithin demyelination is inhibited by Jagged1-expressing astrocytes, which directly bind to Notch1 on OPCs (Hammond et al., 2014). Reactive astrocytes express Jagged1 in MS plaques (John et al., 2002) and this expression appears to be regulated by the secreted protein endothelin-1 (ET-1) (Hammond et al., 2014), which is upregulated following lysolecithin-mediated demyelination (Gadea et al., 2008) and inhibits oligodendrocyte differentiation during development (Gadea et al., 2009). Although ET-1 directly inhibits OPC differentiation and migration in vitro (Gadea et al., 2009), it is the indirect regulation of Jagged1 expression on reactive astrocytes that is proposed to inhibit OPC differentiation following demyelination (Hammond et al., 2014). ET-2 is also implicated in the regulation of CNS remyelination, as it has been shown to promote OPC differentiation and remyelination in a model of innate immunity (Yuen et al., 2013). However, a link between ET-2 and Notch signaling has not been identified to our knowledge. Although more work is needed to identify the precise function of Notch signaling in mediating the progression of oligodendrocyte lineage cells, the majority of findings implicate this pathway in the inhibition of OPC differentiation.
Wnt Signaling
Wnt proteins are secreted ligands that play numerous roles in regulating development, including oligodendrocyte genesis (Azim and Butt, 2011; Fancy et al., 2009; Ortega et al., 2013; Shimizu et al., 2005; Ye et al., 2009). The canonical Wnt pathway is activated when extracellular Wnt binds to Frizzled membrane receptors, resulting in the stabilization of intracellular β-catenin, which enters the nucleus to promote Wnt gene transcription (Xie et al., 2014). Shimizu et al. (2005) showed that OPC differentiation in the spinal cord is inhibited by Wnt signaling through the canonical β-catenin pathway (Shimizu et al., 2005). Similarly, upregulating Wnt signaling decreases the number of proteolipid protein (PLP)-positive oligodendrocytes (Azim and Butt, 2011; Fancy et al., 2009). Interestingly, a recent study demonstrated that clustering of Frizzled receptors and the subsequent transduction of Wnt signals is modulated by Daam2-PIP5K (Lee et al., 2015). Daam2 may be a potential upstream target of Wnt as its activation inhibits OPC differentiation in development and white matter injury (WMI) (Lee et al., 2015). Although there is a general consensus that canonical Wnt signaling inhibits OPC differentiation, conflicting findings have been reported (Xie et al., 2014). Wnt/β-catenin signaling pathway is essential for myelin protein expression and myelin sheath compaction in zebrafish (Tawk et al., 2011). In addition, decreased MBP and PLP are found in mice lacking T-cell factor 4 (Fu et al., 2009), a transcription factor downstream of β-catenin that is expressed by OPCs during development and remyelination (Fancy et al., 2009). These studies suggest that Wnt/β-catenin signaling serves distinct functions in oligodendrocyte specification, differentiation, and myelination depending on timing and dosage (Xie et al., 2014). In support of this hypothesis, Wnt pathway activation was found to affect oligodendrocyte lineage cells in a dose-dependent fashion; low Wnt tone allows OPCs to differentiate and high Wnt tone after injury is associated with permanent WMI (Fancy et al., 2014). Importantly, most studies demonstrate an inhibitory role for Wnt signaling in remyelination. Mice lacking one copy of APC, a β-catenin antagonist, exhibit severely diminished PLP+ oligodendrocytes and remyelination (Fancy et al., 2009; Lang et al., 2013). Moreover, mice lacking Axin2, a Wnt target gene that promotes the degradation of β-catenin (Behrens et al., 1998; Jho et al., 2002), exhibit impaired OPC differentiation and delayed remyelination (Fancy et al., 2011b). Axin2 is expressed in OPCs in active MS lesions and in human hypoxic-ischemic white matter lesions (Fancy et al., 2011b), suggesting it may be a viable therapeutic target. More work is needed to elucidate the mechanisms by which Wnt signaling regulates oligodendrocyte lineage cells embryonically, postnatally, and following injury (Azim et al., 2014; Dai et al., 2014; Rodriguez et al., 2014) in order to resolve the ongoing debate about how and when to modulate Wnt signaling to effectively stimulate remyelination (Guo et al., 2015). Several Wnt inhibitory compounds have been identified as potential anti-cancer therapies (Le et al., 2014). Thus, inhibiting Wnt pathways as a pro-remyelination strategy may be feasible in the near future (Fancy et al., 2011a; Huang and Franklin, 2011).
Semaphorin Signaling
Failure of OPCs to migrate into demyelinated lesions may contribute to failed remyelination in approximately 30% of MS lesions which exhibit reduced OPC numbers (Chang et al., 2002; Lucchinetti et al., 1999). Semaphorins are a family of secreted and membrane proteins that have been implicated in this context. Semaphorins regulate neural development primarily by forming migratory cues through extracellular matrix binding to plexin and neuropillin receptors (for review see Jongbloets and Pasterkamp, 2014). Several members of the semaphorin family have been implicated in regulating OPC migration and differentiation, including semaphorin 3A (SEMA3A), 3F (SEMA3F), and 4D (SEMA4D). Interestingly, SEMA3A and SEMA3F play opposing roles in regulating OPC migration during development. SEMA3A serves as an inhibitory migratory cue whereas SEMA3F serves as an attractive migratory cue (Spassky et al., 2002; Sugimoto et al., 2001). While these proteins are down-regulated in the adult, SEMA3A and SEMA3F are re-expressed in active demyelinating lesions (Williams et al., 2007) where they inhibit and promote OPC migration, respectively (Piaton et al., 2011). Knockdown of SEMA3A promotes in vivo remyelination following focal demyelination of corpus callosum (Boyd et al., 2013). This effect was due to increased OPC migration into the lesion, whereas OPC proliferation, differentiation, and apoptosis were unaffected (Boyd et al., 2013). In contrast, another study found that SEMA3A directly inhibits OPC differentiation in vitro (Syed et al., 2011). While this discrepancy may be explained by different doses of SEMA3A or the use of different species, both groups show that the downstream effect of SEMA3A signaling is failed remyelination (Boyd et al., 2013; Syed et al., 2011). SEMA4D is also inhibitory, as it induces collapse of oligodendrocyte cell processes (Giraudon et al., 2004) and inhibits both OPC survival and differentiation (Smith et al., 2015). Blocking SEMA4D with a monoclonal antibody promotes OPC migration to lesions and improves myelin status following focal demyelination (Smith et al., 2015). Because diminished OPC migration likely contributes to failed remyelination in some MS lesions (Chang et al., 2002; Lucchinetti et al., 1999), inhibiting SEMA4D could be beneficial for MS. While these studies suggest that targeting semaphorins may be beneficial for promoting remyelination, further validation and human trials are needed to thoroughly assess the efficacy of this approach.
RXR Signaling
To date, only a few signaling cascades have been identified for stimulating oligodendrocyte regeneration. Among them is the nuclear retinoid X receptor (RXR) pathway, which plays an important role in cell proliferation and development (for review see Mark et al., 2009). RXRs couple with several other nuclear receptors including retinoic acid receptor, vitamin D receptor, thyroid receptor, and peroxisome proliferator-activated receptor to induce gene transcription (Rastinejad, 2001). The RXR-γ isoform is the first identified nuclear receptor to play a role in promoting remyelination. Huang et al. (2011) found that RXR-γ is differentially upregulated during remyelination in rodent and in active and remyelinated MS lesions (Huang et al., 2011). Further, knockdown of RXR-γ receptor by RNA interference/RXR-specific antagonists dramatically reduces OPC differentiation in vitro and RXR-γ knockout mice exhibit significantly less mature oligodendrocytes following demyelination (Huang et al., 2011). These studies suggest that RXR-γ signaling may regulate oligodendrocyte differentiation and open new doors for pharmacological targeting using RXR ligands, many of which are under study or already approved for the treatment of certain cancers (Ballanger et al., 2010).
Muscarinic Signaling
Acetylcholine muscarinic receptors (mAChR) have been widely studied as potential drug targets for Alzheimer’s disease, Parkinson’s disease, and schizophrenia (Langmead et al., 2008). A recent study using high-throughput screening for MBP expression in primary rat progenitor cells identified Benztropine, a selective M1 mAChR antagonist used for treating Parkinson’s Disease, as an enhancer of OPC differentiation in vitro (Deshmukh et al., 2013). Benztropine also promoted OPC differentiation in the EAE and cuprizone models of demyelination (Deshmukh et al., 2013). The beneficial effect of Benztropine is thought to result from direct anticholingeric activity on OPCs (Deshmukh et al., 2013; Eshleman et al., 1994). However, because Benztropine also has anti-histaminic activity (McKearney, 1982) and can inhibit dopamine uptake (Agoston et al., 1997), more work is needed to confirm the mechanism of action. Further, although Benztropine is still used in the clinical treatment of Parkinson’s disease (Katzenschlager et al., 2003), it is associated with severe side effects such as impaired cognition, urinary retention, nausea, and constipation (Lang and Lees, 2002; Lees, 2005). Recently, Mei et al. (2014) discovered a cluster of eight FDA-approved antimuscarinic compounds that enhance OPC differentiation and myelination using a novel micropillar assay for high-throughput screening. One drug in particular, Clemastine, readily passes the BBB and was highly effective in promoting OPC differentiation and myelination in their assay (Mei et al., 2014). Although more in vivo validation is needed, muscarinic receptors seem to be an exciting new target for the development of MS therapeutics.
4b. Influence of extrinsic inflammatory cues on OPC differentiation
Both microglia, the resident immune cells of the CNS, and peripherally derived macrophages play critical roles in neuroinflammatory disorders. Although they have different developmental origin and localization under physiological conditions, both macrophages and microglia can be polarized to acquire distinct phenotypes and functions (Colton, 2009). We will discuss the generalized activation states of macrophages/microglia as classically-activated macrophages/microglia (CAM) and alternatively-activated macrophages/microglia (AAM) because these are the most widely studied in the context of neuroinflammatory disorders. It is important to note that the distinction between CAM and AAM is not always clear, as microglia and macrophages are plastic and respond rapidly to changes in their environment and can acquire a diverse range of activation programs depending on the stimuli received (Katsumoto et al., 2014).
CAM are the first to respond to an injury or infection by secreting pro-inflammatory cytokines, reactive oxygen species (ROS), and nitrogen species to create an unfavorable (inflammatory) environment for the survival of pathogens (Cao et al., 2013, Mandovani et al., 2013). Additionally, CAM have an increased capacity for antigen-presentation. In the context of MS, this leads to widespread primary demyelination by promoting the phagocytosis of myelin fragments and dying oligodendrocytes by macrophages/microglia and reactive astrocytes (Lassmann, 2014; Sosa et al., 2013; Wu and Raine, 1992). Conversely, AAM are generally thought to suppress inflammation by promoting debris removal, angiogenesis, tissue remodeling, and wound healing (Cao et al., 2013, Mandovani et al., 2013).
Although inflammation leads to oligodendrocyte death and demyelination, depletion of immune cells including macrophages, microglia, and T cells or removal of pro-inflammatory factors including TNFα, IL-1β, and MHCII paradoxically impairs the remyelination process (Arnett et al., 2001; Bieber et al., 2003; Kotter et al., 2005; Mason et al., 2001). Interestingly, remyelination of aged mice, which exhibit impaired OPC recruitment and differentiation (Sim et al., 2002), is enhanced when blood circulation is shared with young mice via parabiosis (Miron et al., 2013; Ruckh et al., 2012). Shared circulation stimulated differentiation and remyelination of endogenous, aged OPCs in old animals following demyelination, an effect that may be partially mediated by the recruitment of young macrophages (Kotter et al., 2006; Miron et al., 2013; Ruckh et al., 2012; Shechter and Schwartz, 2013). More work is needed to elucidate the contribution of potentially additive cell types or other circulating factors to the pro-regenerative effect of young/old parabiosis, however these experiments strongly suggest that the inflammatory environment can be modulated to promote remyelination.
Activated macrophages/microglia might promote remyelination by phagocytosing myelin debris, which is known to inhibit regeneration (Copelman et al., 2001; Ousman and David, 2000; Robinson and Miller, 1999), or by secreting pro-remyelination cytokines and growth factors (Arnett et al., 2001; Hinks and Franklin, 1999; Kotter et al., 2005; Mason et al., 2001; Vela et al., 2002). AAM seem to be particularly important for the beneficial effect of inflammation on remyelination as their depletion leads to delayed oligodendrocyte differentiation following demyelination (Miron et al., 2013). Further, increasing the number of AAM attenuates symptoms in EAE mice (Denney et al., 2012; Mikita et al., 2011). The paradoxical effects of inflammation in MS suggest that it may be the balance of CAM and AAM that sets the tone for remyelination. In support of this hypothesis, Mikita et al. (2011) found that while CAM and AAM are relatively balanced after the first clinical attack following EAE induction, the CAM population significantly outnumbers the AAM population during relapse (Mikita et al., 2011). This work suggests that therapeutically manipulating the balance of CAM/AAM may be beneficial for promoting remyelination in chronic lesions. Significantly more work is needed to elucidate how CAM/AAM balance is regulated and how this balance changes with disease progression in order to test this hypothesis.
Contribution of reactive astrocytes
Astrocytes, the most abundant cells in the CNS, play numerous roles in the healthy brain as well as in disease (Mayo et al., 2014). In a process known as astrogliosis, they rapidly respond to injury by becoming ‘activated,” a phenotype characterized by altered protein expression, cell morphology remodeling, and the upregulation of proinflammatory cytokines (eg. IL6, iNOS, TNFalpha) and growth factors (eg. LIF, IGF1, PDGFalpha, CNTF) (Sofroniew, 2009). Reactive astrocytes are also characterized by increased proliferation, cellular hypertrophy, and process extension, which are thought to contribute to glial scar formation. While glial scar formation restricts infection and cell necrosis to avoid damaging adjacent tissue (Sofroniew, 2009), it can also be detrimental by contributing to chronic inflammation and blockage of oligodendrocyte lineage cell migration into the lesion (Bannerman et al., 2007; Mayo et al., 2014).
Reactive astrocytes appear to have direct and indirect effects on oligodendrocyte lineage cells. For example, expression of Jagged1 receptors on astrocytes directly inhibits OPC differentiation via Notch signaling (Hammond et al., 2014; Stidworthy et al., 2004; Zhang et al., 2009) as described in section 4a. Activated astrocytes play additional, indirect roles in regulating OPC differentiation by affecting macrophages/microglia and infiltrating T-cells. Mice lacking astrocytic NF-kB, a transcription factor that alters production of pro-inflammatory cytokines, have reduced infiltration of inflammatory cells in the spinal cord and less cytokine secretion by T cells following EAE induction (Brambilla et al., 2014, 2009). Similarly, the astrocyte-derived enzyme B4GALT6 (β-1,4-galactosyltransferase 6), has recently been identified as a driver of neuroinflammation and of microglia/macrophage activation and recruitment in chronic EAE (Mayo et al., 2014). Reactive astrocytes also indirectly affect OPC differentiation by contributing to increased BBB permeability via secretion of thymidine phosphorylase (TYMP) and vascular endothelial growth factor A (VEGF-A) (Argaw et al., 2012; Chapouly et al., 2015). Deletion of VEGF-A specifically in astrocytes improves outcome in the lysolecithin and EAE models of MS, likely by reducing the infiltration of monocytes into the CNS (Argaw et al., 2012). While it is clear that astrocytes contribute to the pathology of MS, future work should focus on identifying the mechanisms by which astrocytic signals directly affect OPC differentiation as well as regulate the inflammatory environment.
5. Conclusion
In lieu of a cure, oligodendrocyte regeneration may be a useful therapeutic approach for the treatment of MS. Remyelination restores the physiological interaction between oligodendrocyte and axon, and is hypothesized to restore the necessary structural and secreted support for axonal maintenance and efficient impulse conduction. Here we discussed several molecular pathways that regulate differentiation of OPCs into mature, myelinating oligodendrocytes that should be carefully considered as possible therapeutic targets. In conjunction, the state of inflammation must be carefully weighed. As it is now appreciated that inflammation is both damaging to myelin and necessary for myelin regeneration, combination therapies may be needed to promote remyelination across a changing inflammatory background.
Highlights.
Oligodendrocytes regenerate and remyelinate axons following injury
Remyelination is important in maintaining axonal conduction and integrity
Understanding the intrinsic and environmental signals involved in remyelination allows the identification of therapeutic targets for improving remyelination in multiple sclerosis
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agoston G, Wu J, Izenwasser S, George C, Katz J, Kline R, Newman A. Novel N-Substituted 3r-[Bis(4′-fluorophenyl)methoxy]tropane Analogues: Selective Ligands for the Dopamine Transporter. J. Med. Chem. 1997;40:4329–4339. doi: 10.1021/jm970525a. [DOI] [PubMed] [Google Scholar]
- Argaw AT, Asp L, Zhang J, Navrazhina K, Pham T, Mariani JN, Mahase S, Dutta DJ, Seto J, Kramer EG, Ferrara N, Sofroniew MV, John GR. Astrocyte-derived VEGF-A drives blood-brain barrier disruption in CNS inflammatory disease. J. Clin. Invest. 2012;122:2454–2468. doi: 10.1172/JCI60842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett H, Mason J, Marino M, Suzuki K, Matsushima GK, Ting JP. TNF alpha promotes proliferation of oligodendrocyte progenitors and remyelination. Nat. Neurosci. 2001;4:1116–1122. doi: 10.1038/nn738. [DOI] [PubMed] [Google Scholar]
- Azim K, Butt AM. GSK3β negatively regulates oligodendrocyte differentiation and myelination in vivo. Glia. 2011;59:540–553. doi: 10.1002/glia.21122. [DOI] [PubMed] [Google Scholar]
- Azim K, Rivera A, Raineteau O, Butt AM. GSK3β regulates oligodendrogenesis in the dorsal microdomain of the subventricular zone via Wnt-β-catenin signaling. Glia. 2014;62:778–789. doi: 10.1002/glia.22641. [DOI] [PubMed] [Google Scholar]
- Back S. a, Tuohy TMF, Chen H, Wallingford N, Craig A, Struve J, Luo NL, Banine F, Liu Y, Chang A, Trapp BD, Bebo BF, Rao MS, Sherman LS. Hyaluronan accumulates in demyelinated lesions and inhibits oligodendrocyte progenitor maturation. Nat. Med. 2005;11:966–972. doi: 10.1038/nm1279. [DOI] [PubMed] [Google Scholar]
- Ballanger F, Nguyen JM, Khammari a., Dréno B. Evolution of Clinical and Molecular Responses to Bexarotene Treatment in Cutaneous T-Cell Lymphoma. Dermatology. 2010;220:370–375. doi: 10.1159/000305354. [DOI] [PubMed] [Google Scholar]
- Bannerman P, Hahn A, Soulika A, Gallo V, Pleasure D. Astrogliosis in EAE Spinal Cord: Derivation from Radial Glia, and Relationships to Oligodendroglia. Glia. 2007;55:57–64. doi: 10.1002/glia. [DOI] [PubMed] [Google Scholar]
- Baxter AG. The origin and application of experimental autoimmune encephalomyelitis. Nat. Rev. Immunol. 2007;7:904–912. doi: 10.1038/nri2190. [DOI] [PubMed] [Google Scholar]
- Behrens J, Jerchow B. a, Würtele M, Grimm J, Asbrand C, Wirtz R, Kühl M, Wedlich D, Birchmeier W. Functional interaction of an axin homolog, conductin, with beta-catenin, APC, and GSK3beta. Science. 1998;280:596–599. doi: 10.1126/science.280.5363.596. [DOI] [PubMed] [Google Scholar]
- Bhatt A, Fan L, Pang Y. Strategies for myelin regeneration: lessons learned from development. Neural Regen. Res. 2014;9:1347–50. doi: 10.4103/1673-5374.137586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieber AJ, Kerr S, Rodriguez M. Efficient central nervous system remyelination requires T cells. Ann. Neurol. 2003;53:680–684. doi: 10.1002/ana.10578. [DOI] [PubMed] [Google Scholar]
- Bitsch A, Schuchardt J, Bunkowski S, Kuhlmann T, Brück W. Acute axonal injury in multiple sclerosis. Correlation with demyelination and inflammation. Brain. 2000;123(Pt 6):1174–1183. doi: 10.1093/brain/123.6.1174. [DOI] [PubMed] [Google Scholar]
- Bjartmar C, Kidd G, Mörk S, Rudick R, Trapp BD. Neurological disability correlates with spinal cord axonal loss and reduced N-acetyl aspartate in chronic multiple sclerosis patients. Ann. Neurol. 2000;48:893–901. doi: 10.1002/1531-8249(200012)48:6<893::AID-ANA10>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- Bjartmar C, Wujek JR, Trapp BD. Axonal loss in the pathology of MS: Consequences for understanding the progressive phase of the disease. J. Neurol. Sci. 2003;206:165–171. doi: 10.1016/S0022-510X(02)00069-2. [DOI] [PubMed] [Google Scholar]
- Blakemore W, Franklin R. Blakemore and Franklin_Curr Top Microbio_2008.pdf. Adv. Mult. Scler. Exp. Demyelinating Dis. Curr. Top. Microbiol. Immunol. 2008;318:193–212. doi: 10.1007/978-3-540-73677-6_8. [DOI] [PubMed] [Google Scholar]
- Boyd A, Zhang H, Williams A. Insufficient OPC migration into demyelinated lesions is a cause of poor remyelination in MS and mouse models. Acta Neuropathol. 2013;125:841–859. doi: 10.1007/s00401-013-1112-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brambilla R, Morton PD, Ashbaugh JJ, Karmally S, Lambertsen KL, Bethea JR. Astrocytes play a key role in EAE pathophysiology by orchestrating in the CNS the inflammatory response of resident and peripheral immune cells and by suppressing remyelination. Glia. 2014;62:452–467. doi: 10.1002/glia.22616. [DOI] [PubMed] [Google Scholar]
- Brambilla R, Persaud T, Hu X, Karmally S, Shestopalov VI, Dvoriantchikova G, Ivanov D, Nathanson L, Barnum SR, Bethea JR. Transgenic inhibition of astroglial NF-kappa B improves functional outcome in experimental autoimmune encephalomyelitis by suppressing chronic central nervous system inflammation. J. Immunol. 2009;182:2628–2640. doi: 10.4049/jimmunol.0802954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkmann BG, Agarwal A, Sereda MW, Garratt AN, Müller T, Wende H, Stassart RM, Nawaz S, Humml C, Velanac V, Radyushkin K, Goebbels S, Fischer TM, Franklin RJ, Lai C, Ehrenreich H, Birchmeier C, Schwab MH, Nave KA. Neuregulin-1/ErbB Signaling Serves Distinct Functions in Myelination of the Peripheral and Central Nervous System. Neuron. 2008;59:581–595. doi: 10.1016/j.neuron.2008.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosnan CF, John GR. Revisiting Notch in remyelination of multiple sclerosis lesions. J. Clin. Invest. 2009;119:10–3. doi: 10.1172/JCI37786.progressive. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byravan S, Foster LM, Phan T, Verity a N., Campagnoni a T. Murine oligodendroglial cells express nerve growth factor. Proc. Natl. Acad. Sci. U. S. A. 1994;91:8812–8816. doi: 10.1073/pnas.91.19.8812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell GR, Ohno N, Turnbull DM, Mahad DJ. Mitochondrial changes within axons in multiple sclerosis: an update. Curr. Opin. Neurol. 2012;25:221–30. doi: 10.1097/WCO.0b013e3283533a25. [DOI] [PubMed] [Google Scholar]
- Campbell GR, Worrall JT, Mahad DJ. The central role of mitochondria in axonal degeneration in multiple sclerosis. Mult. Scler. J. 2014;20:1806–1813. doi: 10.1177/1352458514544537. [DOI] [PubMed] [Google Scholar]
- Carrithers MD. Update on Disease-Modifying Treatments for Multiple Sclerosis. Clin. Ther. 2014;36:1938–1945. doi: 10.1016/j.clinthera.2014.08.006. [DOI] [PubMed] [Google Scholar]
- Chang A, Tourtellotte WW, Rudick R, Trapp BD. Premyelinating oligodendrocytes in chronic lesions of multiple sclerosis. N. Engl. J. Med. 2002;346:165–173. doi: 10.1056/NEJMoa010994. [DOI] [PubMed] [Google Scholar]
- Chapouly C, Tadesse Argaw a., Horng S, Castro K, Zhang J, Asp L, Loo H, Laitman BM, Mariani JN, Straus Farber R, Zaslavsky E, Nudelman G, Raine CS, John GR. Astrocytic TYMP and VEGFA drive blood-brain barrier opening in inflammatory central nervous system lesions. Brain. 2015:1548–1567. doi: 10.1093/brain/awv077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charil A, Zijdenbos AP, Taylor J, Boelman C, Worsley KJ, Evans AC, Dagher A. Statistical mapping analysis of lesion location and neurological disability in multiple sclerosis: Application to 452 patient data sets. Neuroimage. 2003;19:532–544. doi: 10.1016/S1053-8119(03)00117-4. [DOI] [PubMed] [Google Scholar]
- Charles P, Hernandez MP, Stankoff B, Aigrot MS, Colin C, Rougon G, Zalc B, Lubetzki C. Negative regulation of central nervous system myelination by polysialylated-neural cell adhesion molecule. Proc. Natl. Acad. Sci. U. S. A. 2000;97:7585–7590. doi: 10.1073/pnas.100076197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles P, Reynolds R, Seilhean D, Rougon G, Aigrot MS, Niezgoda A, Zalc B, Lubetzki C. Re-expression of PSA-NCAM by demyelinated axons: an inhibitor of remyelination in multiple sclerosis? Brain. 2002;125:1972–1979. doi: 10.1093/brain/awf216. [DOI] [PubMed] [Google Scholar]
- Ciccarelli O, Barkhof F, Bodini B, Stefano N. De, Golay X, Nicolay K, Pelletier D, Pouwels PJW, Smith S. a, Wheeler-Kingshott C. a M., Stankoff B, Yousry T, Miller DH. Pathogenesis of multiple sclerosis: insights from molecular and metabolic imaging. Lancet Neurol. 2014;13:807–822. doi: 10.1016/S1474-4422(14)70101-2. [DOI] [PubMed] [Google Scholar]
- Coman I, Aigrot MS, Seilhean D, Reynolds R, Girault J. a, Zalc B, Lubetzki C. Nodal, paranodal and juxtaparanodal axonal proteins during demyelination and remyelination in multiple sclerosis. Brain. 2006;129:3186–95. doi: 10.1093/brain/awl144. [DOI] [PubMed] [Google Scholar]
- Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–17. doi: 10.1016/S0140-6736(08)61620-7. [DOI] [PubMed] [Google Scholar]
- Copelman CA, Diemel LT, Gveric D, Gregson NA, Louise Cuzner M. Myelin phagocytosis and remyelination of macrophage-enriched central nervous system aggregate cultures. J. Neurosci. Res. 2001;66:1173–1178. doi: 10.1002/jnr.10026. [DOI] [PubMed] [Google Scholar]
- Craner M, Hains BC, Lo AC, Black J. a, Waxman SG. Co-localization of sodium channel Nav1.6 and the sodium-calcium exchanger at sites of axonal injury in the spinal cord in EAE. Brain. 2004;127:294–303. doi: 10.1093/brain/awh032. [DOI] [PubMed] [Google Scholar]
- D’Souza B, Miyamoto A, Weinmaster G. The many facets of Notch ligands. Oncogene. 2008;27:5148–5167. doi: 10.1038/onc.2008.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai X, Lercher LD, Clinton PM, Du Y, Livingston DL, Vieira C, Yang L, Shen MM, Dreyfus CF. The trophic role of oligodendrocytes in the basal forebrain. J. Neurosci. 2003;23:5846–53. doi: 10.1523/JNEUROSCI.23-13-05846.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Z, Sun S, Wang C, Huang H, Hu X, Zhang Z, Lu QR, Qiu M. Stage-specific regulation of oligodendrocyte development by Wnt/β-catenin signaling. J. Neurosci. 2014;34:8467–73. doi: 10.1523/JNEUROSCI.0311-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson MRL, Polito A, Levine JM, Reynolds R. NG2-expressing glial progenitor cells: An abundant and widespread population of cycling cells in the adult rat CNS. Mol. Cell. Neurosci. 2003;24:476–488. doi: 10.1016/S1044-7431(03)00210-0. [DOI] [PubMed] [Google Scholar]
- Denic a, Johnson A, Bieber A. The relevance of animal models in multiple sclerosis research. Pathophysiology. 2011;18:1–16. doi: 10.1016/j.pathophys.2010.04.004.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denney L, Kok WL, Cole SL, Sanderson S, McMichael AJ, Ho L-P. Activation of invariant NKT cells in early phase of experimental autoimmune encephalomyelitis results in differentiation of Ly6Chi inflammatory monocyte to M2 macrophages and improved outcome. J. Immunol. 2012;189:551–7. doi: 10.4049/jimmunol.1103608. [DOI] [PubMed] [Google Scholar]
- Deshmukh V, Tardif V, Lyssiotis C, Green C, Kerman B, Kim HJ, Padmanabhan K, Swoboda JG, Ahmad I, Kondo T, Gage FH, Theofilopoulos a N., Lawson BR, Schultz PG, Lairson LL. A regenerative approach to the treatment of multiple sclerosis. Nature. 2013;502:327–332. doi: 10.1038/nature12647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty KD, Dreyfus CF, Black IB. Brain-derived neurotrophic factor in astrocytes, oligodendrocytes, and microglia/macrophages after spinal cord injury. Neurobiol. Dis. 2000;7:574–585. doi: 10.1006/nbdi.2000.0318. [DOI] [PubMed] [Google Scholar]
- Dutta R, Trapp BD. Mechanisms of neuronal dysfunction and degeneration in multiple sclerosis. Prog. Neurobiol. 2011;93:1–12. doi: 10.1016/j.pneurobio.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziedzic T, Metz I, Dallenga T, König FB, Müller S, Stadelmann C, Brück W. Wallerian degeneration: A major component of early axonal pathology in multiple sclerosis. Brain Pathol. 2010;20:976–985. doi: 10.1111/j.1750-3639.2010.00401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar JM, McCulloch MC, Montague P, Brown AM, Thilemann S, Pratola L, Gruenenfelder FI, Griffiths IR, Nave K-A. Demyelination and axonal preservation in a transgenic mouse model of Pelizaeus-Merzbacher disease. EMBO Mol. Med. 2010;2:42–50. doi: 10.1002/emmm.200900057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar JM, McLaughlin M, Werner HB, McCulloch MC, Barrie J. a, Brown A, Faichney AB, Snaidero N, Nave K-A, Griffiths IR. Early ultrastructural defects of axons and axon-glia junctions in mice lacking expression of Cnp1. Glia. 2009;57:1815–24. doi: 10.1002/glia.20893. [DOI] [PubMed] [Google Scholar]
- England JD, Gamboni F, Levinson SR, Finger TE. Changed distribution of sodium channels along demyelinated axons. Proc. Natl. Acad. Sci. U. S. A. 1990;87:6777–6780. doi: 10.1073/pnas.87.17.6777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshleman a J., Henningsen R. a, Neve K. a, Janowsky a. Release of dopamine via the human transporter. Mol. Pharmacol. 1994;45:312–316. [PubMed] [Google Scholar]
- Fancy SPJ, Baranzini SE, Zhao C, Yuk DI, Irvine KA, Kaing S, Sanai N, Franklin RJM, Rowitch DH. Dysregulation of the Wnt pathway inhibits timely myelination and remyelination in the mammalian CNS. Genes Dev. 2009;23:1571–1585. doi: 10.1101/gad.1806309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancy SPJ, Chan JR, Baranzini SE, Franklin RJM, Rowitch DH. Myelin regeneration: a recapitulation of development? Annu. Rev. Neurosci. 2011a;34:21–43. doi: 10.1146/annurev-neuro-061010-113629. [DOI] [PubMed] [Google Scholar]
- Fancy SPJ, Harrington EP, Baranzini SE, Silbereis JC, Shiow LR, Yuen TJ, Huang EJ, Lomvardas S, Rowitch DH. Parallel states of pathological Wnt signaling in neonatal brain injury and colon cancer. Nat. Neurosci. 2014;17:506–12. doi: 10.1038/nn.3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancy SPJ, Harrington EP, Yuen TJ, Silbereis JC, Zhao C, Baranzini SE, Bruce CC, Otero JJ, Huang EJ, Nusse R, Franklin RJM, Rowitch DH. Axin2 as regulatory and therapeutic target in newborn brain injury and remyelination. Nat. Neurosci. 2011b;14:1009–1016. doi: 10.1038/nn.2855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancy SPJ, Kotter MR, Harrington EP, Huang JK, Zhao C, Rowitch DH, Franklin RJM. Overcoming remyelination failure in multiple sclerosis and other myelin disorders. Exp. Neurol. 2010;225:18–23. doi: 10.1016/j.expneurol.2009.12.020. [DOI] [PubMed] [Google Scholar]
- Ferguson B, Matyszak MK, Esiri MM, Perry VH. Axonal damage in acute multiple sclerosis lesions. Brain. 1997;120(Pt 3):393–399. doi: 10.1093/brain/120.3.393. [DOI] [PubMed] [Google Scholar]
- Fischer MT, Sharma R, Lim JL, Haider L, Frischer JM, Drexhage J, Mahad D, Bradl M, van Horssen J, Lassmann H. NADPH oxidase expression in active multiple sclerosis lesions in relation to oxidative tissue damage and mitochondrial injury. Brain. 2012;135:886–99. doi: 10.1093/brain/aws012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher E, Rudick R. a, Simon JH, Cutter G, Baier M, Lee J-C, Miller D, Weinstock-Guttman B, Mass MK, Dougherty DS, Simonian N. a. Eight-year follow-up study of brain atrophy in patients with MS. Neurology. 2002;59:1412–1420. doi: 10.1212/01.WNL.0000036271.49066.06. [DOI] [PubMed] [Google Scholar]
- Frankenhaeuser B. SALTATORY CONDUCTION IN MYELINATED NERVE FIBRES. J. Physiol. 1952;118:107–112. doi: 10.1113/jphysiol.1952.sp004776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin RJM. Why does remyelination fail in multiple sclerosis? Nat. Rev. Neurosci. 2002;3:705–714. doi: 10.1038/nrn917. [DOI] [PubMed] [Google Scholar]
- Franklin RJM, Ffrench-Constant C. Remyelination in the CNS: from biology to therapy. Nat. Rev. Neurosci. 2008;9:839–55. doi: 10.1038/nrn2480. [DOI] [PubMed] [Google Scholar]
- Fu H, Cai J, Clevers H, Fast E, Gray S, Greenberg R, Jain MK, Ma Q, Qiu M, Rowitch DH, Taylor CM, Stiles CD. A genome-wide screen for spatially restricted expression patterns identifies transcription factors that regulate glial development. J. Neurosci. 2009;29:11399–11408. doi: 10.1523/JNEUROSCI.0160-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fünfschilling U, Supplie LM, Mahad D, Boretius S, Saab AS, Edgar J, Brinkmann BG, Kassmann CM, Tzvetanova ID, Möbius W, Diaz F, Meijer D, Suter U, Hamprecht B, Sereda MW, Moraes CT, Frahm J, Goebbels S, Nave K-A. Glycolytic oligodendrocytes maintain myelin and long-term axonal integrity. Nature. 2012;485:517–21. doi: 10.1038/nature11007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadea A, Aguirre A, Haydar TF, Gallo V. Endothelin-1 regulates oligodendrocyte development. J. Neurosci. 2009;29:10047–10062. doi: 10.1523/JNEUROSCI.0822-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadea A, Schinelli S, Gallo V. Endothelin-1 regulates astrocyte proliferation and reactive gliosis via a JNK/c-Jun signaling pathway. J. Neurosci. 2008;28:2394–2408. doi: 10.1523/JNEUROSCI.5652-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genoud S, Lappe-Siefke C, Goebbels S, Radtke F, Aguet M, Scherer SS, Suter U, Nave KA, Mantei N. Notch1 control of oligodendrocyte differentiation in the spinal cord. J. Cell Biol. 2002;158:709–718. doi: 10.1083/jcb.200202002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraudon P, Vincent P, Vuaillat C, Verlaeten O, Cartier L, Marie-Cardine A, Mutin M, Bensussan A, Belin M-F, Boumsell L. Semaphorin CD100 from activated T lymphocytes induces process extension collapse in oligodendrocytes and death of immature neural cells. J. Immunol. 2004;172:1246–1255. doi: 10.4049/jimmunol.172.2.1246. [DOI] [PubMed] [Google Scholar]
- Givogri MI, Costa RM, Schonmann V, Silva AJ, Campagnoni AT, Bongarzone ER. Central nervous system myelination in mice with deficient expression of Notch1 receptor. J. Neurosci. Res. 2002;67:309–320. doi: 10.1002/jnr.10128. [DOI] [PubMed] [Google Scholar]
- Goldschmidt T, Antel J, König FB, Brück W, Kuhlmann T. Remyelination capacity of the MS brain decreases with disease chronicity. Neurology. 2009;72:1914–1921. doi: 10.1212/WNL.0b013e3181a8260a. [DOI] [PubMed] [Google Scholar]
- Gonzalez D, Dees W, Hiney J, Ojeda S, Saneto R. Expression of beta-nerve growth factor in cultured cells derived from the hypothalamus and cerebral cortex. Brain Res. 1990;511:249–58. doi: 10.1016/0006-8993(90)90169-c. [DOI] [PubMed] [Google Scholar]
- Gray E, Rice C, Nightingale H, Ginty M, Hares K, Kemp K, Cohen N, Love S, Scolding N, Wilkins A. Accumulation of cortical hyperphosphorylated neurofilaments as a marker of neurodegeneration in multiple sclerosis. Mult. Scler. J. 2012;19:153–161. doi: 10.1177/1352458512451661. [DOI] [PubMed] [Google Scholar]
- Griffiths I, Klugmann M, Anderson T, Yool D, Thomson C, Schwab M, Schneider A, Zimmerman F, McCulloch M, Nadon N, Nave K-A. Axonal Swellings and Degeneration in Mice Lacking the Major Proteolipid of Myelin. Science. 1998;280:1610–1613. doi: 10.1126/science.280.5369.1610. (80-. ) [DOI] [PubMed] [Google Scholar]
- Guo F, Lang J, Sohn J, Hammond E, Chang M, Pleasure D. Canonical Wnt signaling in the oligodendroglial lineage-puzzles remain. Glia. 2015 doi: 10.1002/glia.22813. [DOI] [PubMed] [Google Scholar]
- Haines J, Inglese M, Casaccia P. Axonal Damage in Multiple Sclerosis. Mt. Sinai J. Med. 2011;78:231–243. doi: 10.1002/MSJ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines JD, Inglese M, Casaccia P. Axonal Damage in Multiple Sclerosis. Mt. Sinai J. Med. 2009;76:173–181. doi: 10.1002/MSJ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond TR, Gadea A, Dupree J, Kerninon C, Nait-oumesmar B, Aguirre A. Astrocyte-Derived Endothelin-1 Inhibits Remyelination through Notch Activation. Neuron. 2014 doi: 10.1016/j.neuron.2014.03.007. [DOI] [PubMed] [Google Scholar]
- Hartline DK, Colman DR. Rapid Conduction and the Evolution of Giant Axons and Myelinated Fibers. Curr. Biol. 2007;17:29–35. doi: 10.1016/j.cub.2006.11.042. [DOI] [PubMed] [Google Scholar]
- Hinks GL, Franklin RJ. Distinctive patterns of PDGF-A, FGF-2, IGF-I, and TGF-beta1 gene expression during remyelination of experimentally-induced spinal cord demyelination. Mol. Cell. Neurosci. 1999;14:153–168. doi: 10.1006/mcne.1999.0771. [DOI] [PubMed] [Google Scholar]
- Horner P, M, T., FH, G. Defining the NG2-expressing cell of the adult CNS. J. Neurocytol. 2002;31:469–80. doi: 10.1023/a:1025739630398. [DOI] [PubMed] [Google Scholar]
- Huang JK, Franklin RJM. Regenerative medicine in multiple sclerosis: Identifying pharmacological targets of adult neural stem cell differentiation. Neurochem. Int. 2011;59:329–332. doi: 10.1016/j.neuint.2011.01.017. [DOI] [PubMed] [Google Scholar]
- Huang JK, Jarjour A. a, Nait Oumesmar B, Kerninon C, Williams A, Krezel W, Kagechika H, Bauer J, Zhao C, Baron-Van Evercooren A, Chambon P, Ffrench-Constant C, Franklin RJM. Retinoid X receptor gamma signaling accelerates CNS remyelination. Nat. Neurosci. 2011;14:45–53. doi: 10.1038/nn.2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvine KA, Blakemore WF. Remyelination protects axons from demyelination-associated axon degeneration. Brain. 2008;131:1464–1477. doi: 10.1093/brain/awn080. [DOI] [PubMed] [Google Scholar]
- Jeffery ND, Blakemore WF. Locomotor deficits induced by experimental spinal cord demyelination are abolished by spontaneous remyelination. Brain. 1997;120:27–37. doi: 10.1093/brain/120.1.27. [DOI] [PubMed] [Google Scholar]
- Jho E, Zhang T, Domon C, Joo C, Freund J, Costantini F. Wnt / β -Catenin / Tcf Signaling Induces the Transcription of Axin2 , a Negative Regulator of the Signaling Pathway Wnt / ▪ -Catenin / Tcf Signaling Induces the Transcription of Axin2 , a Negative Regulator of the Signaling Pathway. Mol. Cell. Biol. 2002;22:1172–1183. doi: 10.1128/MCB.22.4.1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji B, Li M, Wu WT, Yick LW, Lee X, Shao Z, Wang J, So KF, McCoy JM, Blake Pepinsky R, Mi S, Relton JK. LINGO-1 antagonist promotes functional recovery and axonal sprouting after spinal cord injury. Mol. Cell. Neurosci. 2006;33:311–320. doi: 10.1016/j.mcn.2006.08.003. [DOI] [PubMed] [Google Scholar]
- John G, Shankar S, Shafit-Zagardo B, Massimi A, Lee S, Raine C, Brosnan C. Multiple sclerosis: Re-expression of a developmental pathway that restricts oligodendrocyte maturation. Nat Med. 2002;8:1115–21. doi: 10.1038/nm. [DOI] [PubMed] [Google Scholar]
- Jongbloets BC, Pasterkamp RJ. Semaphorin signalling during development. Development. 2014;141:3292–3297. doi: 10.1242/dev.105544. [DOI] [PubMed] [Google Scholar]
- Joshi DC, Zhang C-L, Lin T-M, Gusain a., Harris MG, Tree E, Yin Y, Wu C, Sheng Z-H, Dempsey RJ, Fabry Z, Chiu SY. Deletion of Mitochondrial Anchoring Protects Dysmyelinating Shiverer: Implications for Progressive MS. J. Neurosci. 2015;35:5293–5306. doi: 10.1523/JNEUROSCI.3859-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katsumoto a., Lu H, Miranda a. S., Ransohoff RM. Ontogeny and Functions of Central Nervous System Macrophages. J. Immunol. 2014;193:2615–2621. doi: 10.4049/jimmunol.1400716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzenschlager R, Sampaio C, Costa J, Lees A. Anticholinergics for symptomatic management of Parkinson’s disease. Cochrane Database Syst. Rev. 2003 doi: 10.1002/14651858.CD003735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JY, Sun Q, Oglesbee M, Yoon SO. The role of ErbB2 signaling in the onset of terminal differentiation of oligodendrocytes in vivo. J. Neurosci. 2003;23:5561–5571. doi: 10.1523/JNEUROSCI.23-13-05561.2003. doi:23/13/5561 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiryu-Seo S, Ohno N, Kidd GJ, Komuro H, Trapp BD. Demyelination increases axonal stationary mitochondrial size and the speed of axonal mitochondrial transport. J. Neurosci. 2010;30:6658–66. doi: 10.1523/JNEUROSCI.5265-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaver R, Popescu V, Voorn P, Graaf YG, Valk P, Van Der, Vries H.E. De, Schenk GJ, Geurts JJG. Neuronal and Axonal Loss in Normal-Appearing Gray Matter and Subpial Lesions in Multiple Sclerosis. J Neuropathol Exp Neurol. 2015;74:453–458. doi: 10.1097/NEN.0000000000000189. [DOI] [PubMed] [Google Scholar]
- Kornek B, Storch MK, Weissert R, Wallstroem E, Stefferl a, Olsson T, Linington C, Schmidbauer M, Lassmann H. Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative quantitative study of axonal injury in active, inactive, and remyelinated lesions. Am. J. Pathol. 2000;157:267–276. doi: 10.1016/S0002-9440(10)64537-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter MR, Li W-W, Zhao C, Franklin RJM. Myelin impairs CNS remyelination by inhibiting oligodendrocyte precursor cell differentiation. J. Neurosci. 2006;26:328–332. doi: 10.1523/JNEUROSCI.2615-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter MR, Zhao C, Van Rooijen N, Franklin RJM. Macrophage-depletion induced impairment of experimental CNS remyelination is associated with a reduced oligodendrocyte progenitor cell response and altered growth factor expression. Neurobiol. Dis. 2005;18:166–175. doi: 10.1016/j.nbd.2004.09.019. [DOI] [PubMed] [Google Scholar]
- Kuhlmann T, Miron V, Cuo Q, Wegner C, Antel J, Brück W. Differentiation block of oligodendroglial progenitor cells as a cause for remyelination failure in chronic multiple sclerosis. Brain. 2008;131:1749–1758. doi: 10.1093/brain/awn096. [DOI] [PubMed] [Google Scholar]
- Lang A, Lees A. Management of Parkinson’s Disease: an Evidence Based Review. Mov. Disord. 2002;17:S1–S6. doi: 10.1002/mds.5555. [DOI] [PubMed] [Google Scholar]
- Lang J, Maeda Y, Bannerman P, Xu J, Horiuchi M, Pleasure D, Guo F. Adenomatous Polyposis Coli Regulates Oligodendroglial Development. J. Neurosci. 2013;33:3113–3130. doi: 10.1523/JNEUROSCI.3467-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langmead CJ, Watson J, Reavill C. Muscarinic acetylcholine receptors as CNS drug targets. Pharmacol. Ther. 2008;117:232–243. doi: 10.1016/j.pharmthera.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Lappe-Siefke C, Goebbels S, Gravel M, Nicksch E, Lee J, Braun PE, Griffiths IR, Nave K-A. Disruption of Cnp1 uncouples oligodendroglial functions in axonal support and myelination. Nat. Genet. 2003;33:366–74. doi: 10.1038/ng1095. [DOI] [PubMed] [Google Scholar]
- Lassmann H. Mechanisms of white matter damage in multiple sclerosis. Glia. 2014;62:1816–30. doi: 10.1002/glia.22597. [DOI] [PubMed] [Google Scholar]
- Le PN, Mcdermott JD, Jimeno A. Pharmacology & Therapeutics Targeting the Wnt pathway in human cancers : Therapeutic targeting with a focus on OMP-54F28. Pharmacol. Ther. 2014;146C:1–11. doi: 10.1016/j.pharmthera.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HK, Chaboub LS, Fancy SPJ, Deneen B, Lee HK, Chaboub LS, Zhu W, Zollinger D, Rasband MN, Fancy SPJ. Daam2-PIP5K Is a Regulatory Pathway for Wnt Signaling and Therapeutic Target for Remyelination in the CNS. Neuron. 2015;85:1227–1243. doi: 10.1016/j.neuron.2015.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee X, Shao Z, Sheng G, Pepinsky B, Mi S. LINGO-1 regulates oligodendrocyte differentiation by inhibiting ErbB2 translocation and activation in lipid rafts. Mol. Cell. Neurosci. 2014;60:36–42. doi: 10.1016/j.mcn.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Lee X, Yang Z, Shao Z, Rosenberg SS, Levesque M, Pepinsky RB, Qiu M, Miller RH, Chan JR, Mi S. NGF regulates the expression of axonal LINGO-1 to inhibit oligodendrocyte differentiation and myelination. J. Neurosci. 2007;27:220–225. doi: 10.1523/JNEUROSCI.4175-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Morrison BM, Li Y, Lengacher S, Farah MH, Hoffman PN, Liu Y, Tsingalia A, Jin L, Zhang P-W, Pellerin L, Magistretti PJ, Rothstein JD. Oligodendroglia metabolically support axons and contribute to neurodegeneration. Nature. 2012;487:443–8. doi: 10.1038/nature11314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lees A. Alternatives to levodopa in the initial treatment of early Parkinson’s disease. Drugs Aging. 2005;22:731–740. doi: 10.2165/00002512-200522090-00002. [DOI] [PubMed] [Google Scholar]
- Li H, He Y, Richardson WD, Casaccia P. Two-tier transcriptional control of oligodendrocyte differentiation. Curr. Opin. Neurobiol. 2009;19:479–485. doi: 10.1016/j.conb.2009.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucchinetti C, Brück W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. A quantitative analysis of oligodendrocytes in multiple sclerosis lesions. A study of 113 cases. Brain. 1999;122:2279–2295. doi: 10.1093/brain/122.12.2279. [DOI] [PubMed] [Google Scholar]
- Mahad D, Ziabreva I, Lassmann H, Turnbull D. Mitochondrial defects in acute multiple sclerosis lesions. Brain. 2008;131:1722–1735. doi: 10.1093/brain/awn105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahad DH, Trapp BD, Lassmann H. Series Progressive multiple sclerosis 1 Pathological mechanisms in progressive multiple sclerosis c. 2015. pp. 183–193. [DOI] [PubMed]
- Mahad DJ, Ziabreva I, Campbell G, Lax N, White K, Hanson PS, Lassmann H, Turnbull DM. Mitochondrial changes within axons in multiple sclerosis. Brain. 2009;132:1161–74. doi: 10.1093/brain/awp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makinodan M, Rosen KM, Ito S, Corfas G. A Critical Period for Social Experience–Dependent Oligodendrocyte Maturation and Myelination period for social experience. Science. 2012;337:1357–1360. doi: 10.1126/science.1220845. (80-. ) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark M, Ghyselinck NB, Chambon P. Function of retinoic acid receptors during embryonic development. Nucl. Recept. Signal. 2009;7:e002. doi: 10.1621/nrs.07002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason JL, Suzuki K, Chaplin DD, Matsushima GK. Interleukin-1beta promotes repair of the CNS. J. Neurosci. 2001;21:7046–7052. doi: 10.1523/JNEUROSCI.21-18-07046.2001. doi:21/18/7046 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo L, Trauger S. a, Blain M, Nadeau M, Patel B, Alvarez JI, Mascanfroni ID, Yeste A, Kivisäkk P, Kallas K, Ellezam B, Bakshi R, Prat A, Antel JP, Weiner HL, Quintana FJ. Regulation of astrocyte activation by glycolipids drives chronic CNS inflammation. Nat. Med. 2014;20 doi: 10.1038/nm.3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKearney J. Stimulant actions of histamine H1 antagonists on operant behavior in the squirrel monkey. Psychopharmacology (Berl) 1982;77:156–158. doi: 10.1007/BF00431939. [DOI] [PubMed] [Google Scholar]
- Mei F, Fancy SPJ, Shen Y.-A. a, Niu J, Zhao C, Presley B, Miao E, Lee S, Mayoral SR, Redmond S. a, Etxeberria A, Xiao L, Franklin RJM, Green A, Hauser SL, Chan JR. Micropillar arrays as a high-throughput screening platform for therapeutics in multiple sclerosis. Nat. Med. 2014;20:954–960. doi: 10.1038/nm.3618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mews I, Bergmann M, Bunkowski S, Gullotta F, Brück W. Oligodendrocyte and axon pathology in clinically silent multiple sclerosis lesions. Mult. Scler. 1998;4:55–62. doi: 10.1191/135245898678919582. [DOI] [PubMed] [Google Scholar]
- Mi S, Hu B, Hahm K, Luo Y, Kam Hui ES, Yuan Q, Wong WM, Wang L, Su H, Chu T-H, Guo J, Zhang W, So K-F, Pepinsky B, Shao Z, Graff C, Garber E, Jung V, Wu EX, Wu W. LINGO-1 antagonist promotes spinal cord remyelination and axonal integrity in MOG-induced experimental autoimmune encephalomyelitis. Nat. Med. 2007;13:1228–1233. doi: 10.1038/nm1664. [DOI] [PubMed] [Google Scholar]
- Mi S, Miller RH, Lee X, Scott ML, Shulag-Morskaya S, Shao Z, Chang J, Thill G, Levesque M, Zhang M, Hession C, Sah D, Trapp B, He Z, Jung V, McCoy JM, Pepinsky RB. LINGO-1 negatively regulates myelination by oligodendrocytes. Nat. Neurosci. 2005;8:745–751. doi: 10.1038/nn1460. [DOI] [PubMed] [Google Scholar]
- Mi S, Miller RH, Tang W, Lee X, Hu B, Wu W, Zhang Y, Shields CB, Zhang Y, Miklasz S, Shea D, Mason J, Franklin RJM, Ji B, Shao Z, Chédotal A, Bernard F, Roulois A, Xu J, Jung V, Pepinsky B. Promotion of central nervous system remyelination by induced differentiation of oligodendrocyte precursor cells. Ann. Neurol. 2009;65:304–315. doi: 10.1002/ana.21581. [DOI] [PubMed] [Google Scholar]
- Mikita J, Dubourdieu-Cassagno N, Deloire MS, Vekris A, Biran M, Raffard G, Brochet B, Canron M-H, Franconi J-M, Boiziau C, Petry KG. Altered M1/M2 activation patterns of monocytes in severe relapsing experimental rat model of multiple sclerosis. Amelioration of clinical status by M2 activated monocyte administration. Mult. Scler. 2011;17:2–15. doi: 10.1177/1352458510379243. [DOI] [PubMed] [Google Scholar]
- Milo R, Kahana E. Multiple sclerosis: Geoepidemiology, genetics and the environment. Autoimmun. Rev. 2010;9 doi: 10.1016/j.autrev.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Miron VE, Boyd A, Zhao J-W, Yuen TJ, Ruckh JM, Shadrach JL, van Wijngaarden P, Wagers AJ, Williams A, Franklin RJM, ffrench-Constant C. M2 microglia and macrophages drive oligodendrocyte differentiation during CNS remyelination. Nat. Neurosci. 2013;16:1211–8. doi: 10.1038/nn.3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutsaers SE, Carroll WM. Focal accumulation of intra-axonal mitochondria in demyelination of the cat optic nerve. Acta Neuropathol. 1998;96:139–43. doi: 10.1007/s004010050873. [DOI] [PubMed] [Google Scholar]
- Nave K-A. Myelination and the trophic support of long axons. Nat. Rev. Neurosci. 2010;11:275–83. doi: 10.1038/nrn2797. [DOI] [PubMed] [Google Scholar]
- Nave K-A, Trapp BD. Axon-glial signaling and the glial support of axon function. Annu. Rev. Neurosci. 2008;31:535–61. doi: 10.1146/annurev.neuro.30.051606.094309. [DOI] [PubMed] [Google Scholar]
- Nikić I, Merkler D, Sorbara C, Brinkoetter M, Kreutzfeldt M, Bareyre FM, Brück W, Bishop D, Misgeld T, Kerschensteiner M. A reversible form of axon damage in experimental autoimmune encephalomyelitis and multiple sclerosis. Nat. Med. 2011;17:495–499. doi: 10.1038/nm.2324. [DOI] [PubMed] [Google Scholar]
- Oluich L-J, Stratton JAS, Xing YL, Ng SW, Cate HS, Sah P, Windels F, Kilpatrick TJ, Merson TD. Targeted ablation of oligodendrocytes induces axonal pathology independent of overt demyelination. J. Neurosci. 2012;32:8317–30. doi: 10.1523/JNEUROSCI.1053-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega F, Gascón S, Masserdotti G, Deshpande A, Simon C, Fischer J, Dimou L, Chichung Lie D, Schroeder T, Berninger B. Oligodendrogliogenic and neurogenic adult subependymal zone neural stem cells constitute distinct lineages and exhibit differential responsiveness to Wnt signalling. Nat. Cell Biol. 2013;15:602–13. doi: 10.1038/ncb2736. [DOI] [PubMed] [Google Scholar]
- Ousman SS, David S. Lysophosphatidylcholine induces rapid recruitment and activation of macrophages in the adult mouse spinal cord. Glia. 2000;30:92–104. [PubMed] [Google Scholar]
- Pachner AR. Experimental models of multiple sclerosis. Curr. Opin. Neurol. 2011;24:291–299. doi: 10.1097/WCO.0b013e328346c226. [DOI] [PubMed] [Google Scholar]
- Park SK, Miller R, Krane I, Vartanian T. The ErbB2 gene is required for the development of terminally differentiated spinal cord oligodendrocytes. J. Cell Biol. 2001;154:1245–1258. doi: 10.1083/jcb.200104025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrikios P, Stadelmann C, Kutzelnigg A, Rauschka H, Schmidbauer M, Laursen H, Sorensen PS, Brück W, Lucchinetti C, Lassmann H. Remyelination is extensive in a subset of multiple sclerosis patients. Brain. 2006;129:3165–3172. doi: 10.1093/brain/awl217. [DOI] [PubMed] [Google Scholar]
- Pedraza L, Huang JK, Colman DR. Organizing principles of the axoglial apparatus. Neuron. 2001;30:335–44. doi: 10.1016/s0896-6273(01)00306-3. [DOI] [PubMed] [Google Scholar]
- Petzold A, Gveric D, Groves M, Schmierer K, Grant D, Chapman M, Keir G, Cuzner L, Thompson EJ. Phosphorylation and compactness of neurofilaments in multiple sclerosis: Indicators of axonal pathology. Exp. Neurol. 2008;213:326–335. doi: 10.1016/j.expneurol.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piaton G, Aigrot MS, Williams A, Moyon S, Tepavcevic V, Moutkine I, Gras J, Matho KS, Schmitt A, Soellner H, Huber AB, Ravassard P, Lubetzki C. Class 3 semaphorins influence oligodendrocyte precursor recruitment and remyelination in adult central nervous system. Brain. 2011;134:1156–1167. doi: 10.1093/brain/awr022. [DOI] [PubMed] [Google Scholar]
- Podbielska M, Banik NL, Kurowska E, Hogan EL. Myelin recovery in multiple sclerosis: the challenge of remyelination. Brain Sci. 2013;3:1282–324. doi: 10.3390/brainsci3031282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pringle NP, Mudhar HS, Collarini EJ, Richardson WD. PDGF receptors in the rat CNS: during late neurogenesis, PDGF alpha-receptor expression appears to be restricted to glial cells of the oligodendrocyte lineage. Development. 1992;115:535–551. doi: 10.1242/dev.115.2.535. [DOI] [PubMed] [Google Scholar]
- Qi X, Lewin AS, Sun L, Hauswirth WW, Guy J. Mitochondrial protein nitration primes neurodegeneration in experimental autoimmune encephalomyelitis. J. Biol. Chem. 2006;281:31950–31962. doi: 10.1074/jbc.M603717200. [DOI] [PubMed] [Google Scholar]
- Ransohoff RM. Animal models of multiple sclerosis: the good, the bad and the bottom line. Nat. Neurosci. 2012;15:1074–1077. doi: 10.1038/nn.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasband MN. Na + channels get anchored…with a little help. J. Cell Biol. 2008;183:975–977. doi: 10.1083/jcb.200811086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasband MN. Clustered K+ channel complexes in axons. Neurosci. Lett. 2010;486:101–106. doi: 10.1016/j.neulet.2010.08.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastinejad F. Retinoid X receptor and its partners in the nuclear receptor family. Curr. Opin. Struct. Biol. 2001;11:33–38. doi: 10.1016/S0959-440X(00)00165-2. [DOI] [PubMed] [Google Scholar]
- Rice CM. Disease Modification in Multiple Sclerosis: an update. Pract. Neurol. 2014;14:6–13. doi: 10.1136/practneurol-2013-000601. [DOI] [PubMed] [Google Scholar]
- Robinson S, Miller R. Contact with central nervous system myelin inhibits oligodendrocyte progenitor maturation. Dev. Biol. 1999;216:359–368. doi: 10.1006/dbio.1999.9466. [DOI] [PubMed] [Google Scholar]
- Rodriguez JP, Coulter M, Miotke J, Meyer RL, Takemaru K-I, Levine JM. Abrogation of B-Catenin Signaling in Oligodendrocyte Precursor Cells Reduces Glial Scarring and Promotes Axon Regeneration after CNS Injury. J. Neurosci. 2014;34:10285–10297. doi: 10.1523/JNEUROSCI.4915-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez M. Effectors of demyelination and remyelination in the CNS: Implications for multiple sclerosis. Brain Pathol. 2007;17:219–229. doi: 10.1111/j.1750-3639.2007.00065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruckh J, Zhao J, Shadrach J, van Wijngaarden P, Rao T, Wagers A, Franklin R. Rejuvenation of regeneration in the aging central nervous system. Cell Stem Cell. 2012;10:96–103. doi: 10.1016/j.biotechadv.2011.08.021.Secreted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudick R. a, Fisher E, Lee JC, Simon J, Jacobs L. Use of the brain parenchymal fraction to measure whole brain atrophy in relapsing-remitting MS. Multiple Sclerosis Collaborative Research Group. Neurology. 1999;53:1698–1704. doi: 10.1212/WNL.53.8.1698. [DOI] [PubMed] [Google Scholar]
- Rudick RA, Mi S, Sandrock AW. LINGO-1 antagonists as therapy for multiple sclerosis: in vitro and in vivo evidence. Expert Opin. Biol. Ther. 2008;8:1561–1570. doi: 10.1517/14712598.8.10.1561. [DOI] [PubMed] [Google Scholar]
- Saab AS, Tzvetanova ID, Nave KA. The role of myelin and oligodendrocytes in axonal energy metabolism. Curr. Opin. Neurobiol. 2013;23:1065–1072. doi: 10.1016/j.conb.2013.09.008. [DOI] [PubMed] [Google Scholar]
- Sailer M, Fischl B, Salat D, Tempelmann C, Schönfeld MA, Busa E, Bodammer N, Heinze HJ, Dale A. Focal thinning of the cerebral cortex in multiple sclerosis. Brain. 2003;126:1734–1744. doi: 10.1093/brain/awg175. [DOI] [PubMed] [Google Scholar]
- Saxena S, Caroni P. Mechanisms of axon degeneration: From development to disease. Prog. Neurobiol. 2007;83:174–191. doi: 10.1016/j.pneurobio.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Scherer SS, Arroyo EJ. Recent progress on the molecular organization of myelinated axons. J. Peripher. Nerv. Syst. 2002;7:1–12. doi: 10.1046/j.1529-8027.2002.02001.x. [DOI] [PubMed] [Google Scholar]
- Schirmer L, Antel JP, Brück W, Stadelmann C. Axonal loss and neurofilament phosphorylation changes accompany lesion development and clinical progression in multiple sclerosis. Brain Pathol. 2011;21:428–440. doi: 10.1111/j.1750-3639.2010.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert T, Bauer J, Weissert R, Fazekas F, Storch MK. Notch1 and its ligand Jagged1 are present in remyelination in a T-cell- and antibody-mediated model of inflammatory demyelination. Acta Neuropathol. 2007;113:195–203. doi: 10.1007/s00401-006-0170-9. [DOI] [PubMed] [Google Scholar]
- Shechter R, Schwartz M. Harnessing monocyte-derived macrophages to control central nervous system pathologies: No longer if’ but how'. J. Pathol. 2013;229:332–346. doi: 10.1002/path.4106. [DOI] [PubMed] [Google Scholar]
- Shimizu T, Kagawa T, Wada T, Muroyama Y, Takada S, Ikenaka K. Wnt signaling controls the timing of oligodendrocyte development in the spinal cord. Dev. Biol. 2005;282:397–410. doi: 10.1016/j.ydbio.2005.03.020. [DOI] [PubMed] [Google Scholar]
- Sim FJ, Zhao C, Penderis J, Franklin RJM. The age-related decrease in CNS remyelination efficiency is attributable to an impairment of both oligodendrocyte progenitor recruitment and differentiation. J. Neurosci. 2002;22:2451–2459. doi: 10.1097/00041327-200306000-00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ES, Jonason A, Reilly C, Veeraraghavan J, Fisher T, Doherty M, Klimatcheva E, Mallow C, Cornelius C, Leonard JE, Marchi N, Janigro D, Tadesse A, Pham T, Seils J, Bussler H, Torno S, Kirk R, Howell A, Evans EE, Paris M, Bowers WJ, John G, Zauderer M. SEMA4D compromises blood-brain barrier, activates microglia, and inhibits remyelination in neurodegenerative disease. Neurobiol. Dis. 2015;73:254–268. doi: 10.1016/j.nbd.2014.10.008. [DOI] [PubMed] [Google Scholar]
- Smith K, Blakemore W, McDonald W. Central remyelination restores secure conduction. Nature. 1979;280:395–96. doi: 10.1038/280395a0. [DOI] [PubMed] [Google Scholar]
- Sofroniew MV. Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci. 2009;32:638–647. doi: 10.1016/j.tins.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosa R. a, Murphey C, Ji N, Cardona AE, Forsthuber TG. The kinetics of myelin antigen uptake by myeloid cells in the central nervous system during experimental autoimmune encephalomyelitis. J. Immunol. 2013;191:5848–57. doi: 10.4049/jimmunol.1300771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spassky N, de Castro F, Le Bras B, Heydon K, Quéraud-LeSaux F, Bloch-Gallego E, Chédotal A, Zalc B, Thomas J-L. Directional guidance of oligodendroglial migration by class 3 semaphorins and netrin-1. J. Neurosci. 2002;22:5992–6004. doi: 10.1523/JNEUROSCI.22-14-05992.2002. doi:20026573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriram S, Steiner I. Experimental allergic encephalomyelitis: A misleading model of multiple sclerosis. Ann. Neurol. 2005;58:939–945. doi: 10.1002/ana.20743. [DOI] [PubMed] [Google Scholar]
- Stidworthy MF, Genoud S, Li WW, Leone DP, Mantei N, Suter U, Franklin RJM. Notch1 and jagged1 are expressed after CNS demyelination, but are not a major rate-determining factor during remyelination. Brain. 2004;127:1928–1941. doi: 10.1093/brain/awh217. [DOI] [PubMed] [Google Scholar]
- Stolt CC, Rehberg S, Ader M, Lommes P, Riethmacher D, Schachner M, Bartsch U, Wegner M. Terminal differentiation of myelin-forming oligodendrocytes depends on the transcription factor Sox10 service Terminal differentiation of myelin-forming oligodendrocytes depends on the transcription factor Sox10. 2002:165–170. doi: 10.1101/gad.215802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugimoto Y, Taniguchi M, Yagi T, Akagi Y, Nojyo Y, Tamamaki N. Guidance of glial precursor cell migration by secreted cues in the developing optic nerve. Development. 2001;128:3321–3330. doi: 10.1242/dev.128.17.3321. [DOI] [PubMed] [Google Scholar]
- Sussman CR, Vartanian T, Miller RH. The ErbB4 neuregulin receptor mediates suppression of oligodendrocyte maturation. J. Neurosci. 2005;25:5757–5762. doi: 10.1523/JNEUROSCI.4748-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed Y. a, Hand E, Möbius W, Zhao C, Hofer M, Nave K. a, Kotter MR. Inhibition of CNS remyelination by the presence of semaphorin 3A. J. Neurosci. 2011;31:3719–3728. doi: 10.1523/JNEUROSCI.4930-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka T, Yoshida S. Mechanisms of remyelination: recent insight from experimental models. Biomol. Concepts. 2014;5:289–298. doi: 10.1515/bmc-2014-0015. [DOI] [PubMed] [Google Scholar]
- Tawk M, Makoukji J, Belle M, Fonte C, Trousson A, Hawkins T, Li H, Ghandour S, Schumacher M, Massaad C. Wnt/beta-catenin signaling is an essential and direct driver of myelin gene expression and myelinogenesis. J. Neurosci. 2011;31:3729–3742. doi: 10.1523/JNEUROSCI.4270-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traka M, Arasi K, Avila RL, Podojil JR, Christakos A, Miller SD, Soliven B, Popko B. A genetic mouse model of adult-onset, pervasive central nervous system demyelination with robust remyelination. Brain. 2010;133:3017–29. doi: 10.1093/brain/awq247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapp BD, Nave K-A. Multiple sclerosis: an immune or neurodegenerative disorder? Annu. Rev. Neurosci. 2008;31:247–269. doi: 10.1146/annurev.neuro.30.051606.094313. [DOI] [PubMed] [Google Scholar]
- Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mörk S, Bö L. Axonal transection in the lesions of multiple sclerosis. N. Engl. J. Med. 1998;338:278–285. doi: 10.1056/NEJM199801293380502. [DOI] [PubMed] [Google Scholar]
- Trapp BD, Stys PK. Virtual hypoxia and chronic necrosis of demyelinated axons in multiple sclerosis. Lancet Neurol. 2009;8:280–291. doi: 10.1016/S1474-4422(09)70043-2. [DOI] [PubMed] [Google Scholar]
- Van Wijngaarden P, Franklin RJM. Ageing stem and progenitor cells: implications for rejuvenation of the central nervous system. Development. 2013;140:2562–75. doi: 10.1242/dev.092262. [DOI] [PubMed] [Google Scholar]
- Vela JM, Molina-Holgado E, Arévalo-Martín A, Almazán G, Guaza C. Interleukin-1 regulates proliferation and differentiation of oligodendrocyte progenitor cells. Mol. Cell. Neurosci. 2002;20:489–502. doi: 10.1006/mcne.2002.1127. [DOI] [PubMed] [Google Scholar]
- Wang S, Sdrulla AD, DiSibio G, Bush G, Nofziger D, Hicks C, Weinmaster G, Barres BA. Notch receptor activation inhibits oligodendrocyte differentiation. Neuron. 1998;21:63–75. doi: 10.1016/S0896-6273(00)80515-2. [DOI] [PubMed] [Google Scholar]
- Waxman SG. Axonal conduction and injury in multiple sclerosis: the role of sodium channels. Nat. Rev. Neurosci. 2006;7:932–941. doi: 10.1038/nrn2023. [DOI] [PubMed] [Google Scholar]
- Wegner C, Esiri MM, Chance S. a, Palace J, Matthews P. Neocortical neuronal, synaptic, and glial loss in multiple sclerosis. Neurology. 2006;67:960–967. doi: 10.1212/01.wnl.0000237551.26858.39. [DOI] [PubMed] [Google Scholar]
- Wilkins A, Chandran S, Compston A, Words KEY. A Role for Oligodendrocyte-Derived IGF-1 in Trophic Support. 2001;57:48–57. doi: 10.1002/glia.1094. [DOI] [PubMed] [Google Scholar]
- Wilkins A, Compston A. Trophic factors attenuate nitric oxide mediated neuronal and axonal injury in vitro: roles and interactions of mitogen-activated protein kinase signalling pathways. J. Neurochem. 2005;92:1487–96. doi: 10.1111/j.1471-4159.2004.02981.x. [DOI] [PubMed] [Google Scholar]
- Williams A, Piaton G, Aigrot MS, Belhadi A, Théaudin M, Petermann F, Thomas JL, Zalc B, Lubetzki C. Semaphorin 3A and 3F: Key players in myelin repair in multiple sclerosis? Brain. 2007;130:2554–2565. doi: 10.1093/brain/awm202. [DOI] [PubMed] [Google Scholar]
- Williamson TL, Cleveland DW. Slowing of axonal transport is a very early event in the toxicity of ALS-linked SOD1 mutants to motor neurons. Nat. Neurosci. 1999;2:50–56. doi: 10.1038/4553. [DOI] [PubMed] [Google Scholar]
- Witte ME, Bø L, Rodenburg RJ, Belien JA, Musters R, Hazes T, Wintjes LT, Smeitink JA, Geurts JJG, Vries HE, De, Valk P. Van Der. Enhanced number and activity of mitochondria in multiple sclerosis lesions. 2009. [DOI] [PubMed]
- Witte ME, Geurts JJG, de Vries HE, van der Valk P, van Horssen J. Mitochondrial dysfunction: A potential link between neuroinflammation and neurodegeneration? Mitochondrion. 2010;10:411–418. doi: 10.1016/j.mito.2010.05.014. [DOI] [PubMed] [Google Scholar]
- Witte ME, Mahad DJ, Lassmann H, van Horssen J. Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis. Trends Mol. Med. 2014;20:179–187. doi: 10.1016/j.molmed.2013.11.007. [DOI] [PubMed] [Google Scholar]
- Wolswijk G. Chronic stage multiple sclerosis lesions contain a relatively quiescent population of oligodendrocyte precursor cells. J. Neurosci. 1998;18:601–609. doi: 10.1523/JNEUROSCI.18-02-00601.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolswijk G, Balesar R. Changes in the expression and localization of the paranodal protein Caspr on axons in chronic multiple sclerosis. Brain. 2003;126:1638–1649. doi: 10.1093/brain/awg151. [DOI] [PubMed] [Google Scholar]
- Wood ET, Ronen I, Techawiboonwong a., Jones CK, Barker PB, Calabresi P, Harrison D, Reich DS. Investigating Axonal Damage in Multiple Sclerosis by Diffusion Tensor Spectroscopy. J. Neurosci. 2012;32:6665–6669. doi: 10.1523/JNEUROSCI.0044-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu E, Raine CS. Multiple Sclerosis Interactions between Oligodendrocytes and Hypertrophic Astrocytes and Their Occurence in Other, Nondemyelinating Conditions. Lab. Investig. 1992;67:88. [PubMed] [Google Scholar]
- Wujek JR, Bjartmar C, Richer E, Ransohoff RM, Yu M, Tuohy VK, Trapp BD. Axon loss in the spinal cord determines permanent neurological disability in an animal model of multiple sclerosis. J. Neuropathol. Exp. Neurol. 2002;61:23–32. doi: 10.1093/jnen/61.1.23. [DOI] [PubMed] [Google Scholar]
- Xie C, Li Z, Zhang GX, Guan Y. Wnt signaling in remyelination in multiple sclerosis: Friend or foe? Mol. Neurobiol. 2014;49:1117–1125. doi: 10.1007/s12035-013-8584-6. [DOI] [PubMed] [Google Scholar]
- Ye F, Chen Y, Hoang T, Montgomery RL, Zhao X, Bu H, Hu T, Taketo MM, van Es JH, Clevers H, Hsieh J, Bassel-Duby R, Olson EN, Lu QR. HDAC1 and HDAC2 regulate oligodendrocyte differentiation by disrupting the beta-catenin-TCF interaction. Nat. Neurosci. 2009;12:829–838. doi: 10.1038/nn.2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin W, Hu B. Knockdown of Lingo1b protein promotes myelination and oligodendrocyte differentiation in zebrafish. Exp. Neurol. 2014;251:72–83. doi: 10.1016/j.expneurol.2013.11.012. [DOI] [PubMed] [Google Scholar]
- Yuen TJ, Johnson KR, Miron VE, Zhao C, Quandt J, Harrisingh MC, Swire M, Williams A, McFarland HF, Franklin RJM, Ffrench-Constant C. Identification of endothelin 2 as an inflammatory factor that promotes central nervous system remyelination. Brain. 2013;136:1035–1047. doi: 10.1093/brain/awt024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambonin JL, Zhao C, Ohno N, Campbell GR, Engeham S, Ziabreva I, Schwarz N, Lee SE, Frischer JM, Turnbull DM, Trapp BD, Lassmann H, Franklin RJM, Mahad DJ. Increased mitochondrial content in remyelinated axons: implications for multiple sclerosis. Brain. 2011;134:1901–13. doi: 10.1093/brain/awr110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Argaw AT, Gurfein BT, Zameer A, Snyder BJ, Ge C, Lu QR, Rowitch DH, Raine CS, Brosnan CF, John GR. Notch1 signaling plays a role in regulating precursor differentiation during CNS remyelination. Proc. Natl. Acad. Sci. U. S. A. 2009;106:19162–19167. doi: 10.1073/pnas.0902834106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Chen K, Sloan S. a, Bennett ML, Scholze AR, Keeffe SO, Phatnani HP, Guarnieri P, Caneda C, Ruderisch N, Deng S, Liddelow S. a, Zhang C, Daneman R, Maniatis T, Barres B. a, Wu JQ. An RNA-Sequencing Transcriptome and Splicing Database of Glia , Neurons , and Vascular Cells of the Cerebral Cortex. J. Neurosci. 2014;34:1–19. doi: 10.1523/JNEUROSCI.1860-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Ping Y, Pepinsky B, Huang G, Shields LBE, Shields CB, Mi S. Inhibition of LINGO-1 promotes functional recovery after experimental spinal cord demyelination. Exp. Neurol. 2015;266:68–73. doi: 10.1016/j.expneurol.2015.02.006. [DOI] [PubMed] [Google Scholar]