Abstract
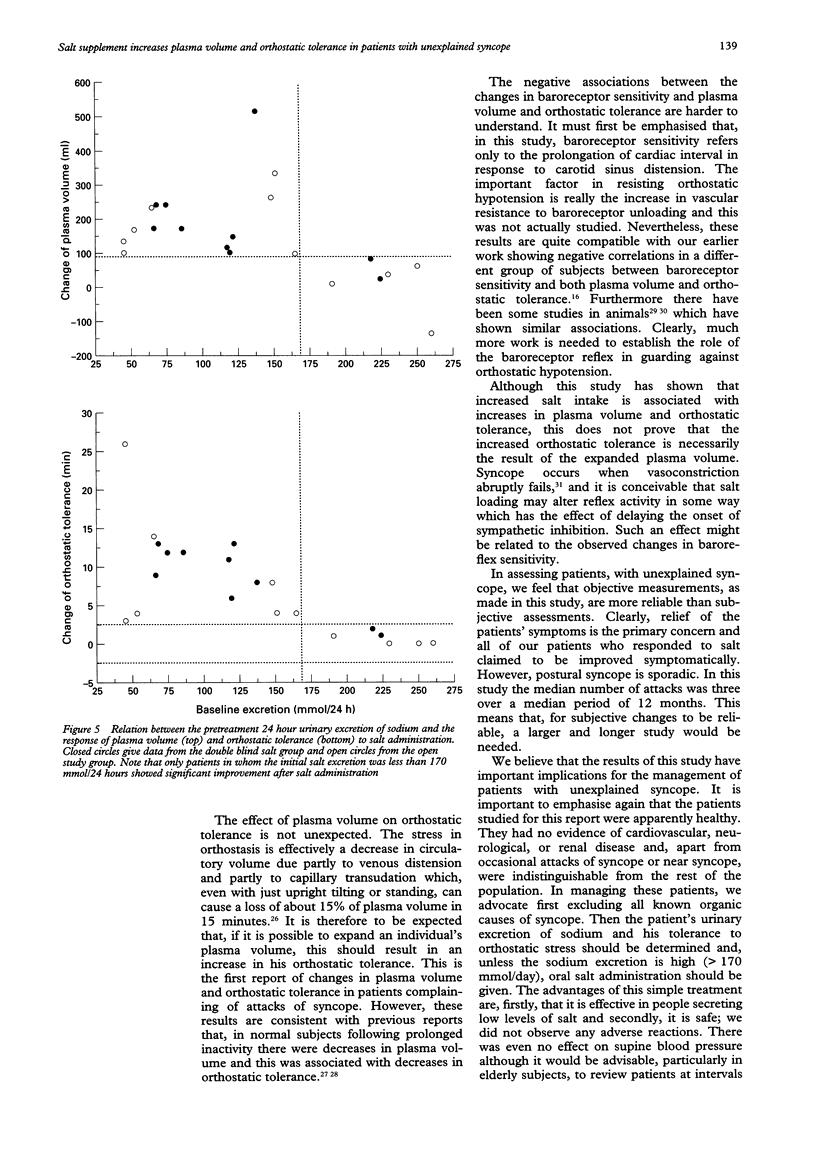
OBJECTIVE: To determine whether in patients presenting with posturally related syncope administration of salt increases plasma volume and improves orthostatic tolerance. Patients with poor tolerance of orthostatic stress tend to have lower than average plasma and blood volumes. DESIGN: A double blind placebo controlled study in 20 patients and an open study in 11 of the effects of giving 120 mmol/day of sodium chloride. PATIENTS: 31 patients presenting with episodes of syncope who had no apparent cardiac or neurological disease. Plasma volume was determined by Evans blue dye dilution, orthostatic tolerance by time to presyncope in a test of combined head-up tilt and lower body suction, and baroreceptor sensitivity by the effect of neck suction on pulse interval. RESULTS: 8 weeks after treatment, 15 (70%) of the 21 patients given salt and three (30%) of the placebo group showed increases in plasma and blood volumes and in orthostatic tolerance, and decreases in baroreceptor sensitivity. Improvement was related to initial salt excretion in that patients who responded to salt had a daily excretion below 170 mmol. The patients in the placebo group who improved also showed increases in salt excretion. CONCLUSIONS: In patients with unexplained syncope who had a relatively low salt intake administration of salt increased plasma volume and orthostatic tolerance, and in the absence of contraindications, salt is suggested as a first line of treatment.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barcroft H., Edholm O. G. On the vasodilatation in human skeletal muscle during post-haemorrhagic fainting. J Physiol. 1945 Oct 15;104(2):161–175. doi: 10.1113/jphysiol.1945.sp004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billman G. E., Dickey D. T., Teoh K. K., Stone H. L. Effects of central venous blood volume shifts on arterial baroreflex control of heart rate. Am J Physiol. 1981 Oct;241(4):H571–H575. doi: 10.1152/ajpheart.1981.241.4.H571. [DOI] [PubMed] [Google Scholar]
- Brown W. J., Jr, Brown F. K., Krishan I. Exchangeable sodium and blood volume in normotensive and hypertensive humans on high and low sodium intake. Circulation. 1971 Apr;43(4):508–519. doi: 10.1161/01.cir.43.4.508. [DOI] [PubMed] [Google Scholar]
- Bungo M. W., Charles J. B., Johnson P. C., Jr Cardiovascular deconditioning during space flight and the use of saline as a countermeasure to orthostatic intolerance. Aviat Space Environ Med. 1985 Oct;56(10):985–990. [PubMed] [Google Scholar]
- Chan W. L., Kong C. W., Chang M. S., Chiang B. N. Exacerbation of vasodepressor syncope by beta-adrenergic blockade. N Engl J Med. 1991 Apr 25;324(17):1219–1220. doi: 10.1056/NEJM199104253241716. [DOI] [PubMed] [Google Scholar]
- Day S. C., Cook E. F., Funkenstein H., Goldman L. Evaluation and outcome of emergency room patients with transient loss of consciousness. Am J Med. 1982 Jul;73(1):15–23. doi: 10.1016/0002-9343(82)90913-5. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick A. P., Theodorakis G., Vardas P., Sutton R. Methodology of head-up tilt testing in patients with unexplained syncope. J Am Coll Cardiol. 1991 Jan;17(1):125–130. doi: 10.1016/0735-1097(91)90714-k. [DOI] [PubMed] [Google Scholar]
- Freitas J., Puig J., Campos J., Garcia J. M., Cunha D. L., Carvalho M. J., Costa O., Gomes M. C., Freitas A. F. Síncope vasovagal maligna: um caso de assistolia prolongada induzida pelo teste de "tilt" e agravada pela terapêutica com bloqueador beta (caso clínico e revisão diagnóstica, fisiopatológica e terapêutica). Rev Port Cardiol. 1993 Sep;12(9):745-51, 702. [PubMed] [Google Scholar]
- Grubb B. P., Temesy-Armos P., Hahn H., Elliott L. Utility of upright tilt-table testing in the evaluation and management of syncope of unknown origin. Am J Med. 1991 Jan;90(1):6–10. doi: 10.1016/0002-9343(91)90499-n. [DOI] [PubMed] [Google Scholar]
- Gupta B. N., Linden R. J., Mary D. A., Weatherill D. The influence of high and low sodium intake on blood volume in the dog. Q J Exp Physiol. 1981 Apr;66(2):117–128. doi: 10.1113/expphysiol.1981.sp002539. [DOI] [PubMed] [Google Scholar]
- Hagan R. D., Diaz F. J., Horvath S. M. Plasma volume changes with movement to supine and standing positions. J Appl Physiol Respir Environ Exerc Physiol. 1978 Sep;45(3):414–417. doi: 10.1152/jappl.1978.45.3.414. [DOI] [PubMed] [Google Scholar]
- Hainsworth R., el-Bedawi K. M. Orthostatic tolerance in patients with unexplained syncope. Clin Auton Res. 1994 Oct;4(5):239–244. doi: 10.1007/BF01827428. [DOI] [PubMed] [Google Scholar]
- Ludwig D. A., Convertino V. A. Predicting orthostatic intolerance: physics or physiology? Aviat Space Environ Med. 1994 May;65(5):404–411. [PubMed] [Google Scholar]
- Rashtian M. Y., Bhandari A. K. Worsening of neurocardiogenic syncope by beta-blockers. Ann Intern Med. 1993 Nov 1;119(9):955–956. doi: 10.7326/0003-4819-119-9-199311010-00027. [DOI] [PubMed] [Google Scholar]
- Romero J. C., Staneloni R. J., Dufau M. L., Dohmen R., Binia A., Kliman B., Fasciolo J. C. Changes in fluid compartments, renal hemodynamics, plasma renin and aldosterone secretion induced by low sodium intake. Metabolism. 1968 Jan;17(1):10–19. doi: 10.1016/s0026-0495(68)80003-4. [DOI] [PubMed] [Google Scholar]
- Sneddon J. F., Camm A. J. Vasovagal syncope: classification, investigation and treatment. Br J Hosp Med. 1993 Mar 3;49(5):329–334. [PubMed] [Google Scholar]
- Vatner S. F., Boettcher D. H., Heyndrickx G. R., McRitchie R. J. Reduced baroreflex sensitivity with volume loading in conscious dogs. Circ Res. 1975 Aug;37(2):236–242. doi: 10.1161/01.res.37.2.236. [DOI] [PubMed] [Google Scholar]
- Wahbha M. M., Morley C. A., al-Shamma Y. M., Hainsworth R. Cardiovascular reflex responses in patients with unexplained syncope. Clin Sci (Lond) 1989 Nov;77(5):547–553. doi: 10.1042/cs0770547. [DOI] [PubMed] [Google Scholar]
- Waxman M. B., Yao L., Cameron D. A., Wald R. W., Roseman J. Isoproterenol induction of vasodepressor-type reaction in vasodepressor-prone persons. Am J Cardiol. 1989 Jan 1;63(1):58–65. doi: 10.1016/0002-9149(89)91076-x. [DOI] [PubMed] [Google Scholar]
- el-Bedawi K. M., Hainsworth R. Combined head-up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res. 1994 Apr;4(1-2):41–47. doi: 10.1007/BF01828837. [DOI] [PubMed] [Google Scholar]
- el-Bedawi K. M., Wahbha M. A., Hainsworth R. Cardiac pacing does not improve orthostatic tolerance in patients with vasovagal syncope. Clin Auton Res. 1994 Oct;4(5):233–237. doi: 10.1007/BF01827427. [DOI] [PubMed] [Google Scholar]
- el-Sayed H., Goodall S. R., Hainsworth R. Re-evaluation of Evans blue dye dilution method of plasma volume measurement. Clin Lab Haematol. 1995 Jun;17(2):189–194. [PubMed] [Google Scholar]
- el-Sayed H., Hainsworth R. Relationship between plasma volume, carotid baroreceptor sensitivity and orthostatic tolerance. Clin Sci (Lond) 1995 Apr;88(4):463–470. doi: 10.1042/cs0880463. [DOI] [PubMed] [Google Scholar]


