Abstract
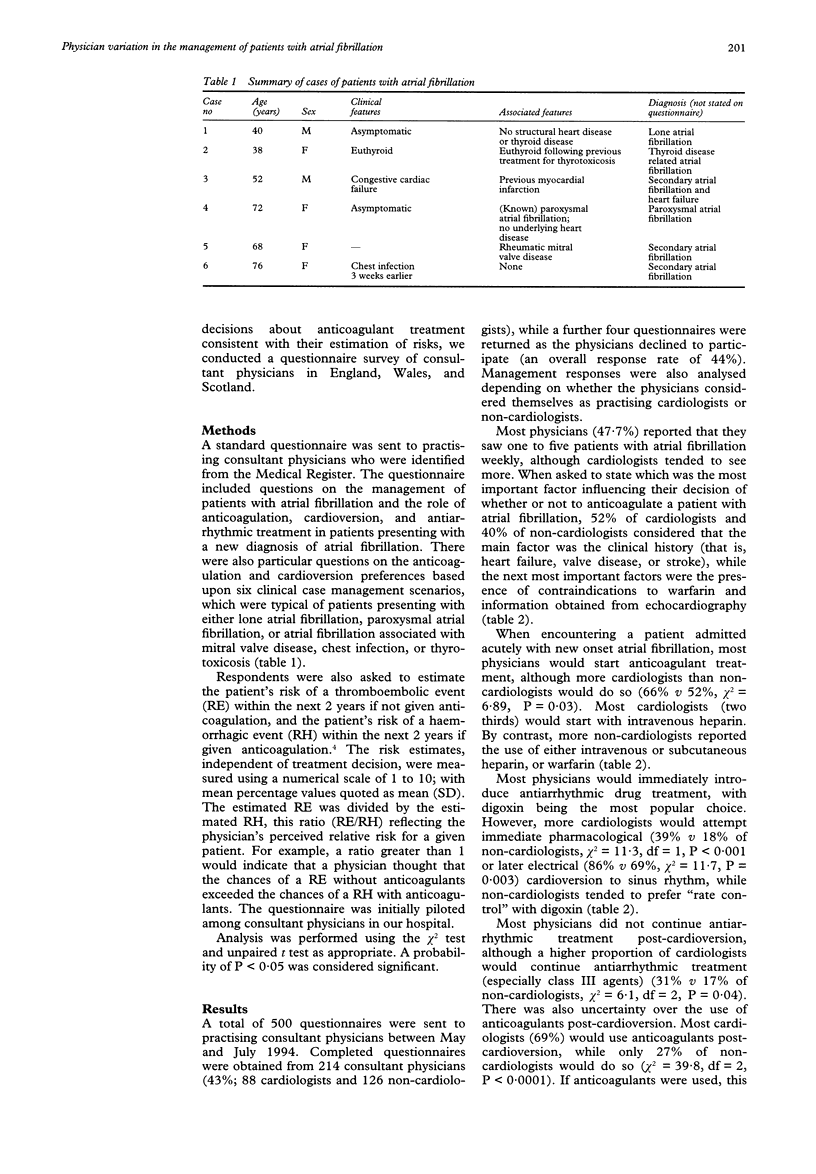
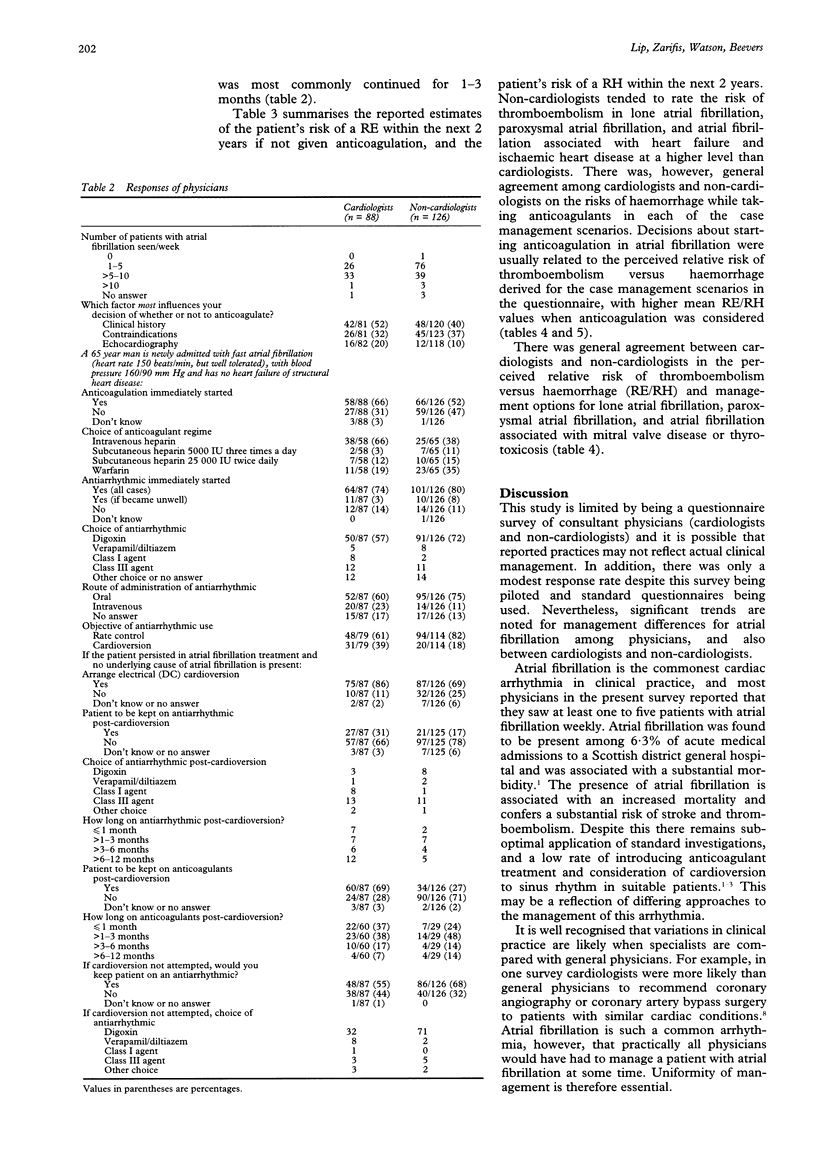
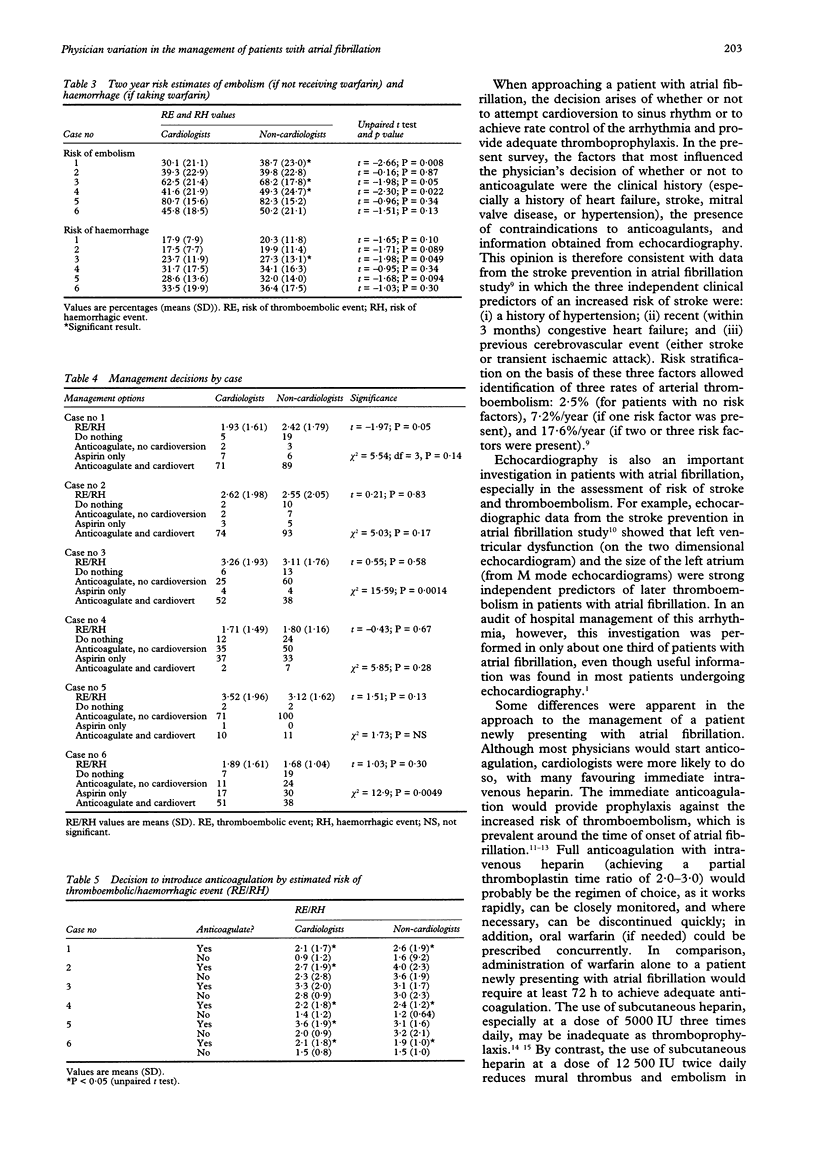
OBJECTIVE: To investigate variations in the management of patients with atrial fibrillation among consultant physicians. DESIGN: Questionnaire survey. SUBJECTS: Consultant physicians in England, Wales, and Scotland. RESULTS: 214 consultant physicians (88 cardiologists and 126 non-cardiologists) were surveyed between May and July 1994. Most physicians (47.7%) reported that they saw one to five patients with atrial fibrillation weekly. Some 52% of cardiologists and 40% of non-cardiologists considered that the main factor influencing their decision of whether or not to anticoagulate was the clinical history--that is, heart failure, valve disease, or stroke. When encountering a patient admitted acutely with new onset atrial fibrillation, significantly more cardiologists (66% v 52%, chi 2 = 6.89, P = 0.03) would immediately start anticoagulant treatment, most favouring intravenous heparin. Most physicians would also introduce antiarrhythmic treatment or digoxin, but more cardiologists would attempt immediate pharmacological (39% v 18% of non-cardiologists, P < 0.001) or later electrical (86% v 69%, chi 2 = 11.7, P = 0.003) cardioversion to sinus rhythm, while non-cardiologists tended to prefer "rate control" with digoxin. Although many physicians would not continue antiarrhythmic treatment post-cardioversion, more cardiologists than non-cardiologists would do so (the commonest choice being class III agents) (31% v 17%, P = 0.04). Fewer non-cardiologists would continue anticoagulant treatment post-cardioversion (27% v 69% of cardiologists, chi 2 = 39.8, P < 0.0001). When treating patients with atrial fibrillation, decisions about anticoagulation were usually related to the perceived relative risk of thromboembolism versus haemorrhage derived for each of six case management scenarios in the questionnaire. There was, however, general agreement between cardiologists and non-cardiologists in the use of antithrombotic treatment in the management of lone atrial fibrillation, paroxysmal atrial fibrillation, and patients with atrial fibrillation and mitral valve disease or thyrotoxicosis. CONCLUSION: There is considerable variation in the management of atrial fibrillation, with more cardiologists than non-cardiologists considering cardioversion to sinus rhythm (and the use of antiarrhythmic and anticoagulant treatment post-cardioversion) and thrombo-prophylaxis with anticoagulation. Guidelines on the management of this common arrhythmia are clearly required.
Full text
PDF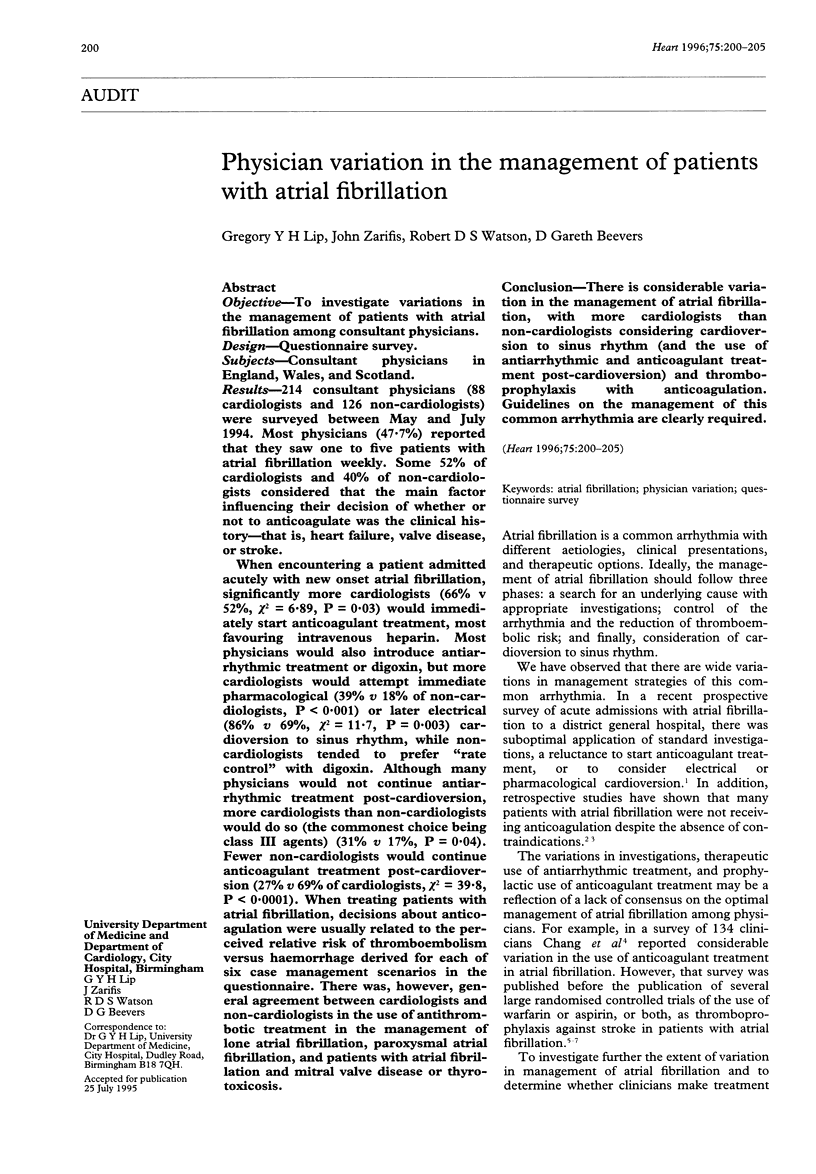
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alpert J. S., Petersen P., Godtfredsen J. Atrial fibrillation: natural history, complications, and management. Annu Rev Med. 1988;39:41–52. doi: 10.1146/annurev.me.39.020188.000353. [DOI] [PubMed] [Google Scholar]
- Bath P. M., Prasad A., Brown M. M., MacGregor G. A. Survey of use of anticoagulation in patients with atrial fibrillation. BMJ. 1993 Oct 23;307(6911):1045–1045. doi: 10.1136/bmj.307.6911.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand F. N., Abbott R. D., Kannel W. B., Wolf P. A. Characteristics and prognosis of lone atrial fibrillation. 30-year follow-up in the Framingham Study. JAMA. 1985 Dec 27;254(24):3449–3453. [PubMed] [Google Scholar]
- Brook R. H., Kosecoff J. B., Park R. E., Chassin M. R., Winslow C. M., Hampton J. R. Diagnosis and treatment of coronary disease: comparison of doctors' attitudes in the USA and the UK. Lancet. 1988 Apr 2;1(8588):750–753. doi: 10.1016/s0140-6736(88)91550-4. [DOI] [PubMed] [Google Scholar]
- Caro J. J., Groome P. A., Flegel K. M. Atrial fibrillation and anticoagulation: from randomised trials to practice. Lancet. 1993 May 29;341(8857):1381–1384. doi: 10.1016/0140-6736(93)90950-l. [DOI] [PubMed] [Google Scholar]
- Chang H. J., Bell J. R., Deroo D. B., Kirk J. W., Wasson J. H. Physician variation in anticoagulating patients with atrial fibrillation. Dartmouth Primary Care COOP Project. Arch Intern Med. 1990 Jan;150(1):83–86. [PubMed] [Google Scholar]
- Dittrich H. C., Erickson J. S., Schneiderman T., Blacky A. R., Savides T., Nicod P. H. Echocardiographic and clinical predictors for outcome of elective cardioversion of atrial fibrillation. Am J Cardiol. 1989 Jan 15;63(3):193–197. doi: 10.1016/0002-9149(89)90284-1. [DOI] [PubMed] [Google Scholar]
- Hendry A., Campbell A. M., Campbell G., Macdonald J. B., Williams B. O. Antithrombotic therapy prescribed for patients with non-rheumatic atrial fibrillation. Scott Med J. 1994 Aug;39(4):110–111. doi: 10.1177/003693309403900404. [DOI] [PubMed] [Google Scholar]
- Kopecky S. L., Gersh B. J., McGoon M. D., Whisnant J. P., Holmes D. R., Jr, Ilstrup D. M., Frye R. L. The natural history of lone atrial fibrillation. A population-based study over three decades. N Engl J Med. 1987 Sep 10;317(11):669–674. doi: 10.1056/NEJM198709103171104. [DOI] [PubMed] [Google Scholar]
- Lip G. Y., Tean K. N., Dunn F. G. Treatment of atrial fibrillation in a district general hospital. Br Heart J. 1994 Jan;71(1):92–95. doi: 10.1136/hrt.71.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe G. D. Antithrombotic treatment and atrial fibrillation. BMJ. 1992 Dec 12;305(6867):1445–1446. doi: 10.1136/bmj.305.6867.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning W. J., Silverman D. I., Katz S. E., Riley M. F., Come P. C., Doherty R. M., Munson J. T., Douglas P. S. Impaired left atrial mechanical function after cardioversion: relation to the duration of atrial fibrillation. J Am Coll Cardiol. 1994 Jun;23(7):1535–1540. doi: 10.1016/0735-1097(94)90652-1. [DOI] [PubMed] [Google Scholar]
- O'Neill P. G., Puleo P. R., Bolli R., Rokey R. Return of atrial mechanical function following electrical conversion of atrial dysrhythmias. Am Heart J. 1990 Aug;120(2):353–359. doi: 10.1016/0002-8703(90)90079-d. [DOI] [PubMed] [Google Scholar]
- Petersen P. Thromboembolic complications in atrial fibrillation. Stroke. 1990 Jan;21(1):4–13. doi: 10.1161/01.str.21.1.4. [DOI] [PubMed] [Google Scholar]
- Turpie A. G., Robinson J. G., Doyle D. J., Mulji A. S., Mishkel G. J., Sealey B. J., Cairns J. A., Skingley L., Hirsh J., Gent M. Comparison of high-dose with low-dose subcutaneous heparin to prevent left ventricular mural thrombosis in patients with acute transmural anterior myocardial infarction. N Engl J Med. 1989 Feb 9;320(6):352–357. doi: 10.1056/NEJM198902093200604. [DOI] [PubMed] [Google Scholar]


