Abstract
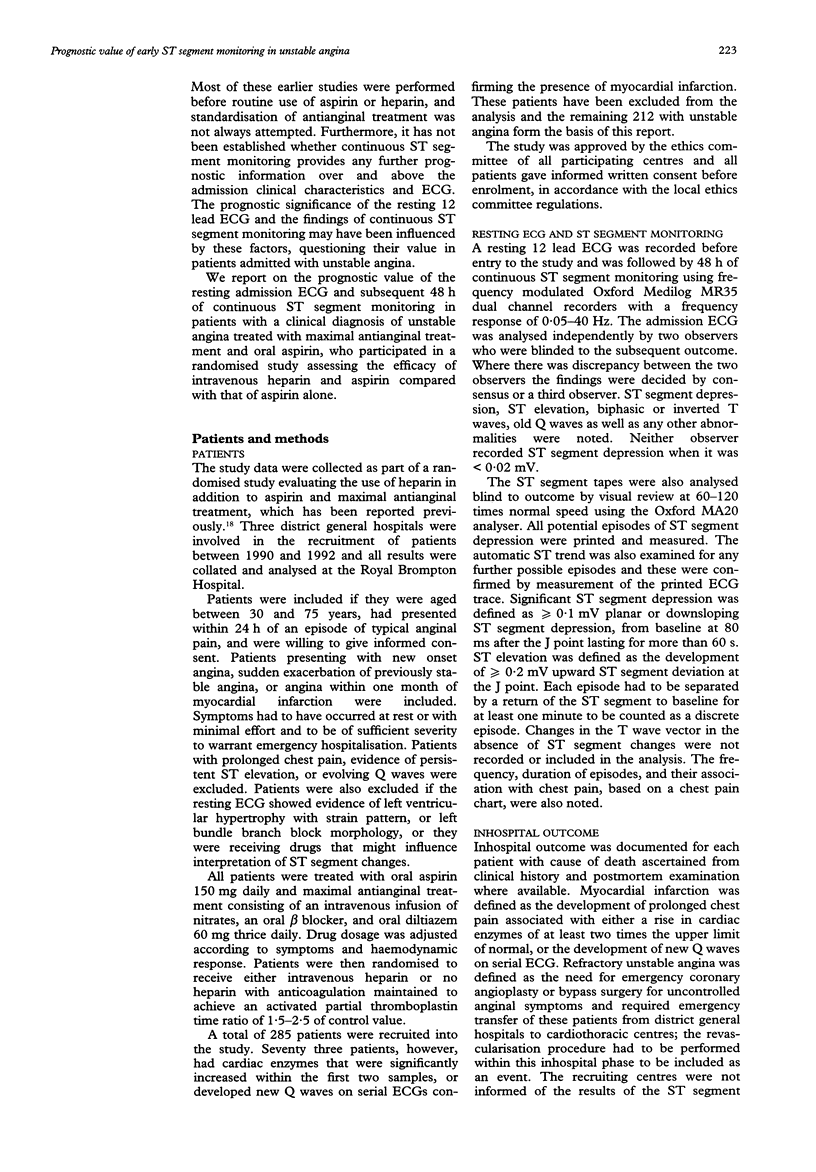
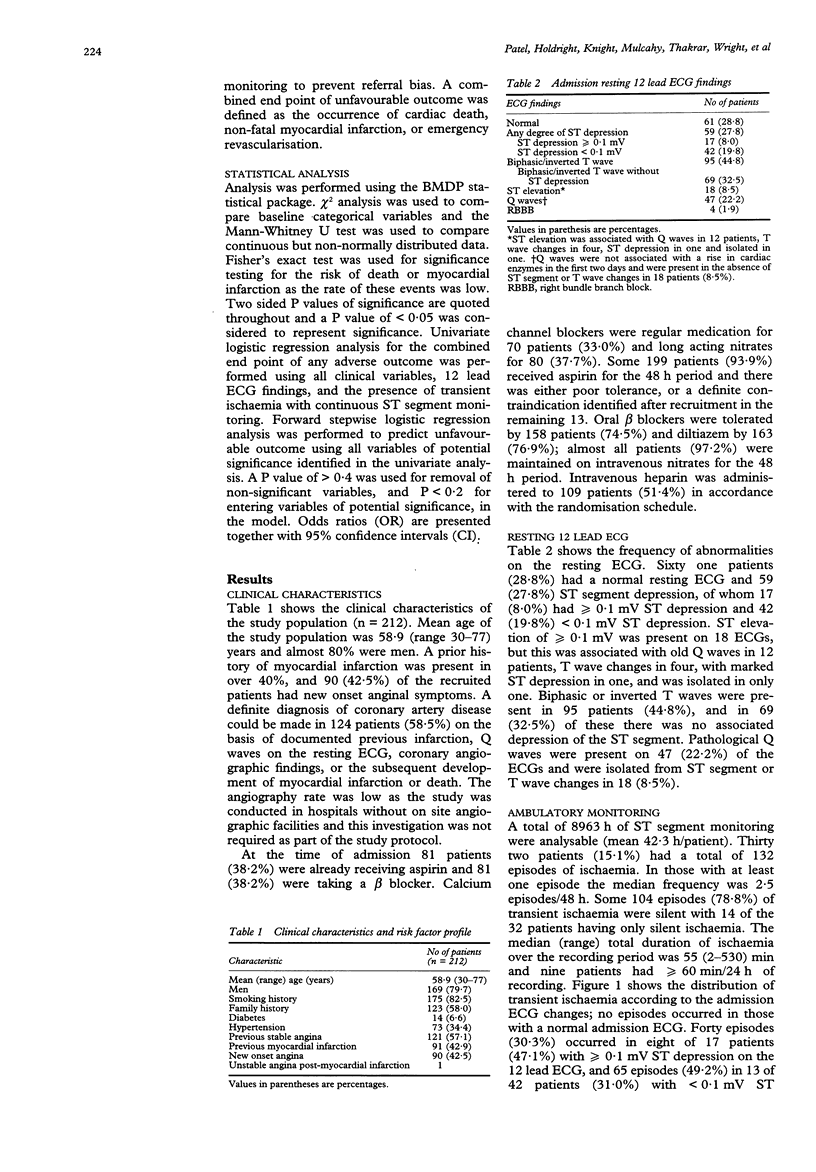
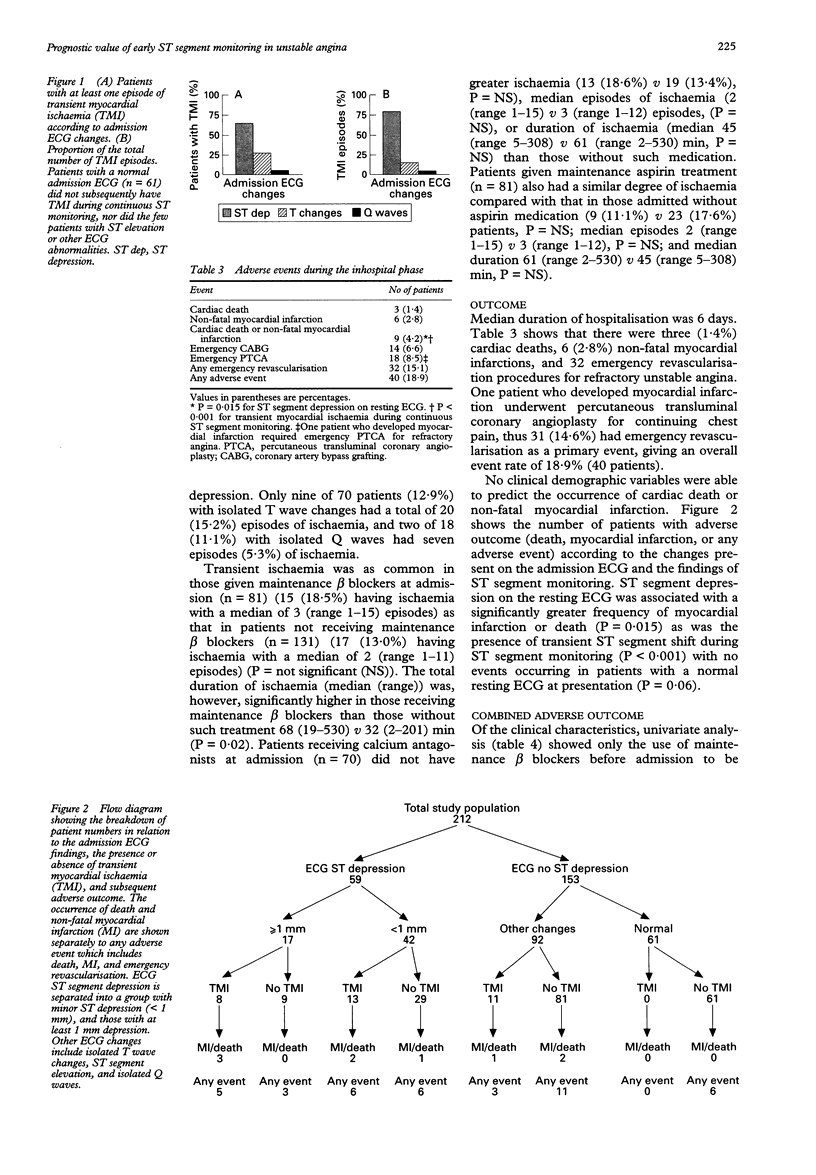
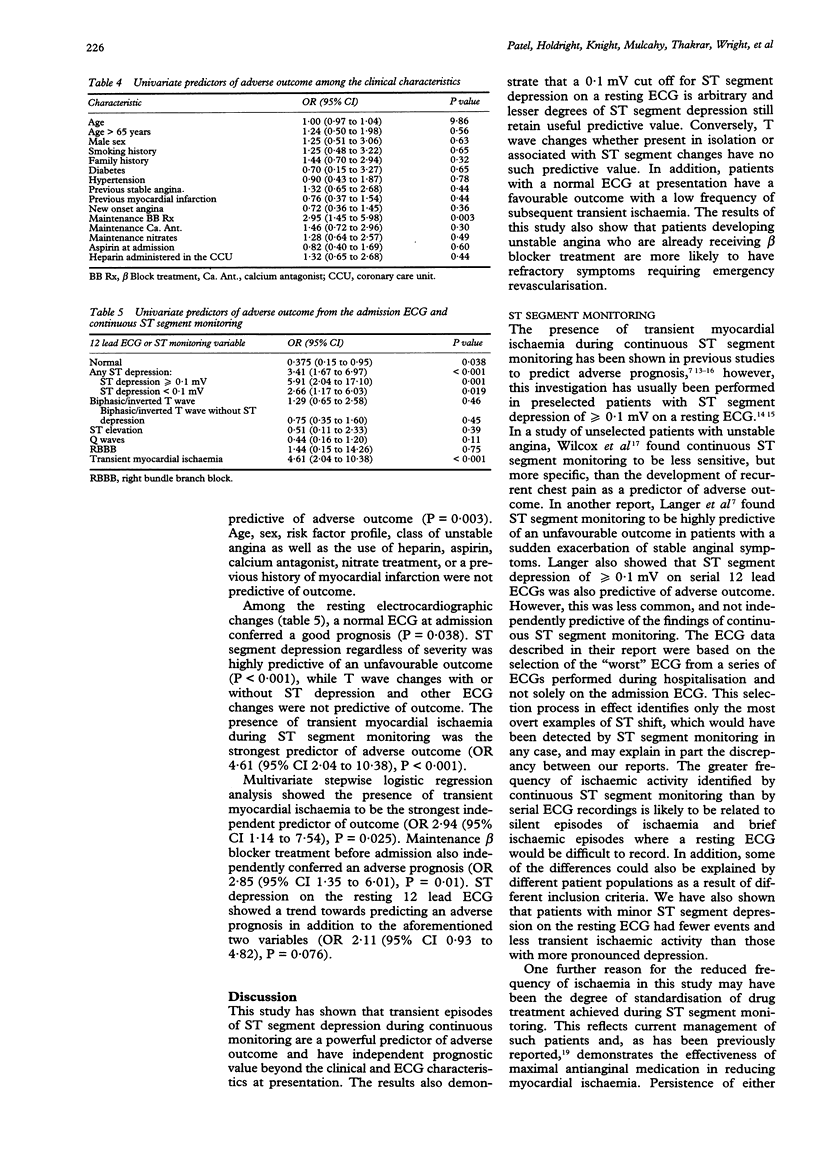
BACKGROUND AND OBJECTIVE: In unstable angina, clinical characteristics, resting electrocardiography, and early continuous ST segment monitoring have been individually reported to identify subgroups at increased risk of adverse outcome. It is not known, however, whether continuous ST monitoring provides additional prognostic information in such a setting. DESIGN: Observational study of 212 patients with unstable angina without evidence of acute myocardial infarction admitted to district general hospitals, who had participated in a randomised study comparing heparin and aspirin treatment versus aspirin alone. METHODS: Clinical variables and a 12 lead electrocardiogram (ECG) were recorded at admission, and treatment was standardised to include aspirin, atenolol, diltiazem, and intravenous glyceryl trinitrate, in addition to intravenous heparin (randomised treatment). Continuous ST segment monitoring was performed for 48 h and all inhospital adverse events were recorded. RESULTS: The admission ECG was normal in 61 patients (29%), showed ST depression in 59 (28%) (17 > or = 0.1 mV), and T wave changes in a further 69 (33%). The remaining 23 had Q waves (18), right bundle branch block (four), or ST elevation (one). During 8963 h of continuous ST segment monitoring (mean 42.3 h/patient), 132 episodes of transient myocardial ischaemia (104 silent) were recorded in 32 patients (15%). Forty patients (19%) had an adverse event (cardiac deaths (n = 3), non-fatal myocardial infarction (n = 6) and, emergency revascularisation (n = 31)). Both admission ECG ST depression (P = 0.02), and transient ischaemia (P < 0.001) predicted an increased risk of non-fatal myocardial infarction or death, while no patients with a normal ECG died or had a myocardial infarction. Adverse outcome was predicted by admission ECG ST depression (regardless of severity) (odds ratio (OR) 3.41) (P < 0.001), and maintenance beta blocker treatment (OR 2.95) (P < 0.01). A normal ECG predicted a favourable outcome (OR 0.38) (P = 0.04), while T wave or other ECG changes were not predictive of outcome. Transient ischaemia was the strongest predictor of adverse prognosis (OR 4.61) (P < 0.001), retaining independent predictive value in multivariate analysis (OR 2.94) (P = 0.03), as did maintenance beta blocker treatment (OR 2.85) (P = 0.01) and admission ECG ST depression, which showed a trend towards independent predictive value (OR 2.11) (P = 0.076). CONCLUSIONS: Patients with unstable angina and a normal admission ECG have a good prognosis, while ST segment depression predicts an adverse outcome. Transient myocardial ischaemia detected by continuous ST segment monitoring in such patients receiving optimal medical treatment provides prognostic information additional to that gleaned from the clinical characteristics or the admission ECG.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cairns J. A., Gent M., Singer J., Finnie K. J., Froggatt G. M., Holder D. A., Jablonsky G., Kostuk W. J., Melendez L. J., Myers M. G. Aspirin, sulfinpyrazone, or both in unstable angina. Results of a Canadian multicenter trial. N Engl J Med. 1985 Nov 28;313(22):1369–1375. doi: 10.1056/NEJM198511283132201. [DOI] [PubMed] [Google Scholar]
- Cohen M., Hawkins L., Greenberg S., Fuster V. Usefulness of ST-segment changes in greater than or equal to 2 leads on the emergency room electrocardiogram in either unstable angina pectoris or non-Q-wave myocardial infarction in predicting outcome. Am J Cardiol. 1991 Jun 15;67(16):1368–1373. doi: 10.1016/0002-9149(91)90467-y. [DOI] [PubMed] [Google Scholar]
- Gazes P. C., Mobley E. M., Jr, Faris H. M., Jr, Duncan R. C., Humphries G. B. Preinfarctional (unstable) angina--a prospective study--ten year follow-up. Prognostic significance of electrocardiographic changes. Circulation. 1973 Aug;48(2):331–337. doi: 10.1161/01.cir.48.2.331. [DOI] [PubMed] [Google Scholar]
- Gottlieb S. O., Weisfeldt M. L., Ouyang P., Mellits E. D., Gerstenblith G. Silent ischemia as a marker for early unfavorable outcomes in patients with unstable angina. N Engl J Med. 1986 May 8;314(19):1214–1219. doi: 10.1056/NEJM198605083141903. [DOI] [PubMed] [Google Scholar]
- Grambow D. W., Topol E. J. Effect of maximal medical therapy on refractoriness of unstable angina pectoris. Am J Cardiol. 1992 Sep 1;70(6):577–581. doi: 10.1016/0002-9149(92)90194-4. [DOI] [PubMed] [Google Scholar]
- Haines D. E., Raabe D. S., Gundel W. D., Wackers F. J. Anatomic and prognostic significance of new T-wave inversion in unstable angina. Am J Cardiol. 1983 Jul;52(1):14–18. doi: 10.1016/0002-9149(83)90061-9. [DOI] [PubMed] [Google Scholar]
- Holdright D., Patel D., Cunningham D., Thomas R., Hubbard W., Hendry G., Sutton G., Fox K. Comparison of the effect of heparin and aspirin versus aspirin alone on transient myocardial ischemia and in-hospital prognosis in patients with unstable angina. J Am Coll Cardiol. 1994 Jul;24(1):39–45. doi: 10.1016/0735-1097(94)90539-8. [DOI] [PubMed] [Google Scholar]
- Johnson S. M., Mauritson D. R., Winniford M. D., Willerson J. T., Firth B. G., Cary J. R., Hillis L. D. Continuous electrocardiographic monitoring in patients with unstable angina pectoris: Identification of high-risk subgroup with severe coronary disease, variant angina, and/or impaired early prognosis. Am Heart J. 1982 Jan;103(1):4–12. doi: 10.1016/0002-8703(82)90522-1. [DOI] [PubMed] [Google Scholar]
- Karlson B. W., Herlitz J., Pettersson P., Hallgren P., Strömbom U., Hjalmarson A. One-year prognosis in patients hospitalized with a history of unstable angina pectoris. Clin Cardiol. 1993 May;16(5):397–402. doi: 10.1002/clc.4960160506. [DOI] [PubMed] [Google Scholar]
- Langer A., Freeman M. R., Armstrong P. W. ST segment shift in unstable angina: pathophysiology and association with coronary anatomy and hospital outcome. J Am Coll Cardiol. 1989 Jun;13(7):1495–1502. doi: 10.1016/0735-1097(89)90338-0. [DOI] [PubMed] [Google Scholar]
- Mulcahy R., Al Awadhi A. H., de Buitleor M., Tobin G., Johnson H., Contoy R. Natural history and prognosis of unstable angina. Am Heart J. 1985 Apr;109(4):753–758. doi: 10.1016/0002-8703(85)90634-9. [DOI] [PubMed] [Google Scholar]
- Muller J. E., Turi Z. G., Pearle D. L., Schneider J. F., Serfas D. H., Morrison J., Stone P. H., Rude R. E., Rosner B., Sobel B. E. Nifedipine and conventional therapy for unstable angina pectoris: a randomized, double-blind comparison. Circulation. 1984 Apr;69(4):728–739. doi: 10.1161/01.cir.69.4.728. [DOI] [PubMed] [Google Scholar]
- Sclarovsky S., Rechavia E., Strasberg B., Sagie A., Bassevich R., Kusniec J., Mager A., Agmon J. Unstable angina: ST segment depression with positive versus negative T wave deflections--clinical course, ECG evolution, and angiographic correlation. Am Heart J. 1988 Oct;116(4):933–941. doi: 10.1016/0002-8703(88)90143-3. [DOI] [PubMed] [Google Scholar]
- Severi S., Orsini E., Marraccini P., Michelassi C., L'Abbate A. The basal electrocardiogram and the exercise stress test in assessing prognosis in patients with unstable angina. Eur Heart J. 1988 Apr;9(4):441–446. doi: 10.1093/oxfordjournals.eurheartj.a062522. [DOI] [PubMed] [Google Scholar]
- Théroux P., Waters D., Qiu S., McCans J., de Guise P., Juneau M. Aspirin versus heparin to prevent myocardial infarction during the acute phase of unstable angina. Circulation. 1993 Nov;88(5 Pt 1):2045–2048. doi: 10.1161/01.cir.88.5.2045. [DOI] [PubMed] [Google Scholar]
- Wilcox I., Ben Freedman S., Kelly D. T., Harris P. J. Clinical significance of silent ischemia in unstable angina pectoris. Am J Cardiol. 1990 Jun 1;65(20):1313–1316. doi: 10.1016/0002-9149(90)91319-2. [DOI] [PubMed] [Google Scholar]
- de Zwaan C., Bär F. W., Wellens H. J. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982 Apr;103(4 Pt 2):730–736. doi: 10.1016/0002-8703(82)90480-x. [DOI] [PubMed] [Google Scholar]
- von Arnim T., Gerbig H. W., Krawietz W., Höfling B. Prognostic implications of transient--predominantly silent--ischaemia in patients with unstable angina pectoris. Eur Heart J. 1988 Apr;9(4):435–440. doi: 10.1093/oxfordjournals.eurheartj.a062521. [DOI] [PubMed] [Google Scholar]


