Abstract
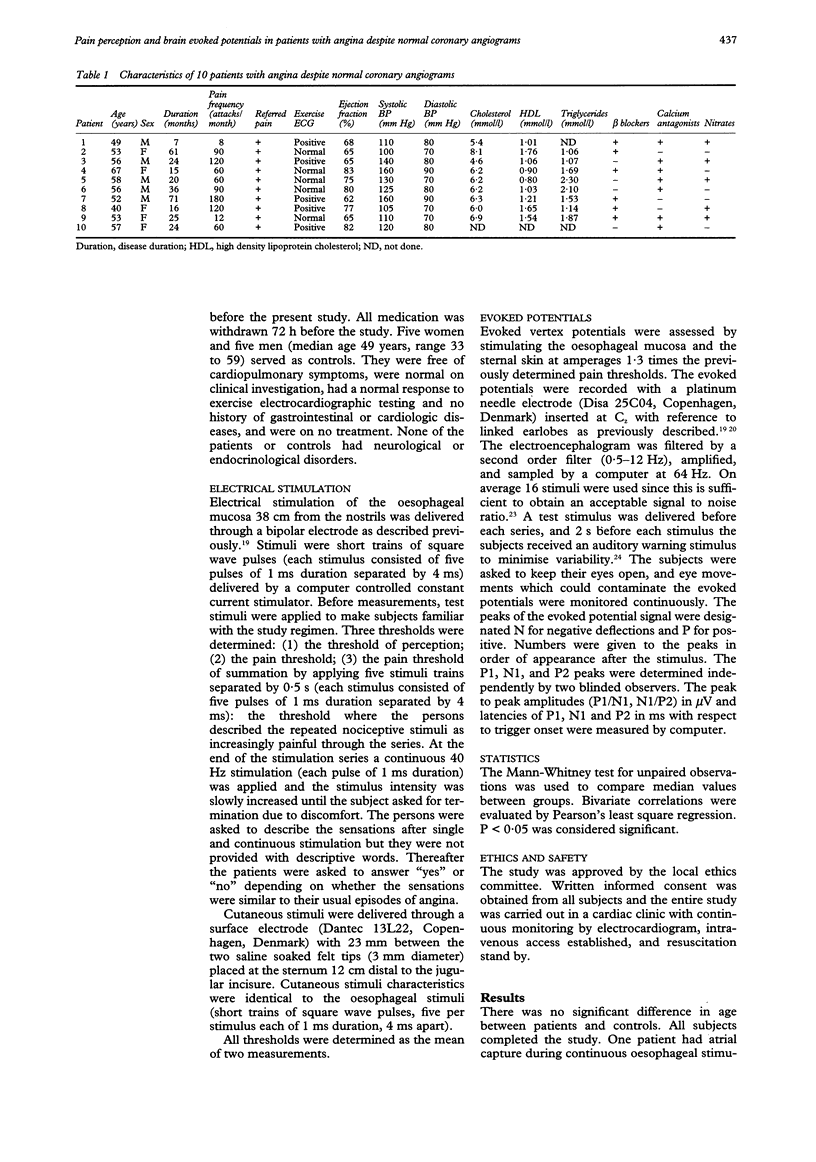
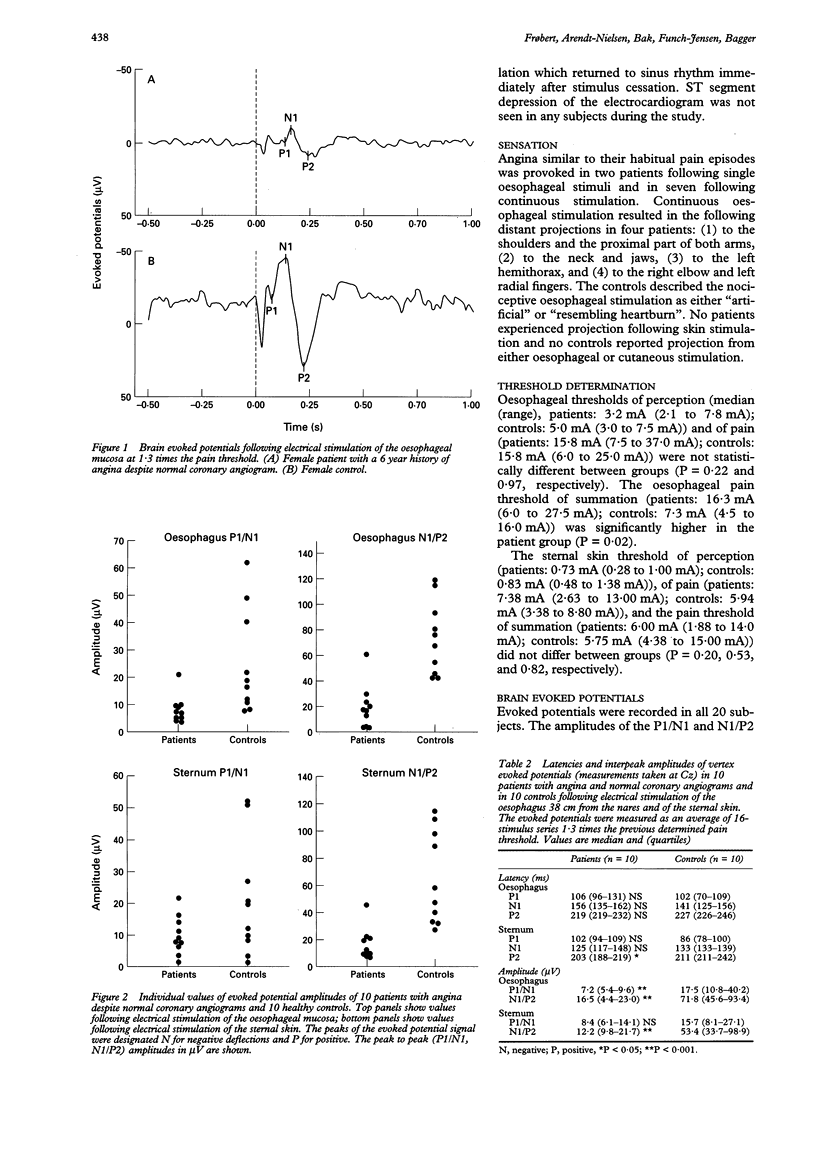
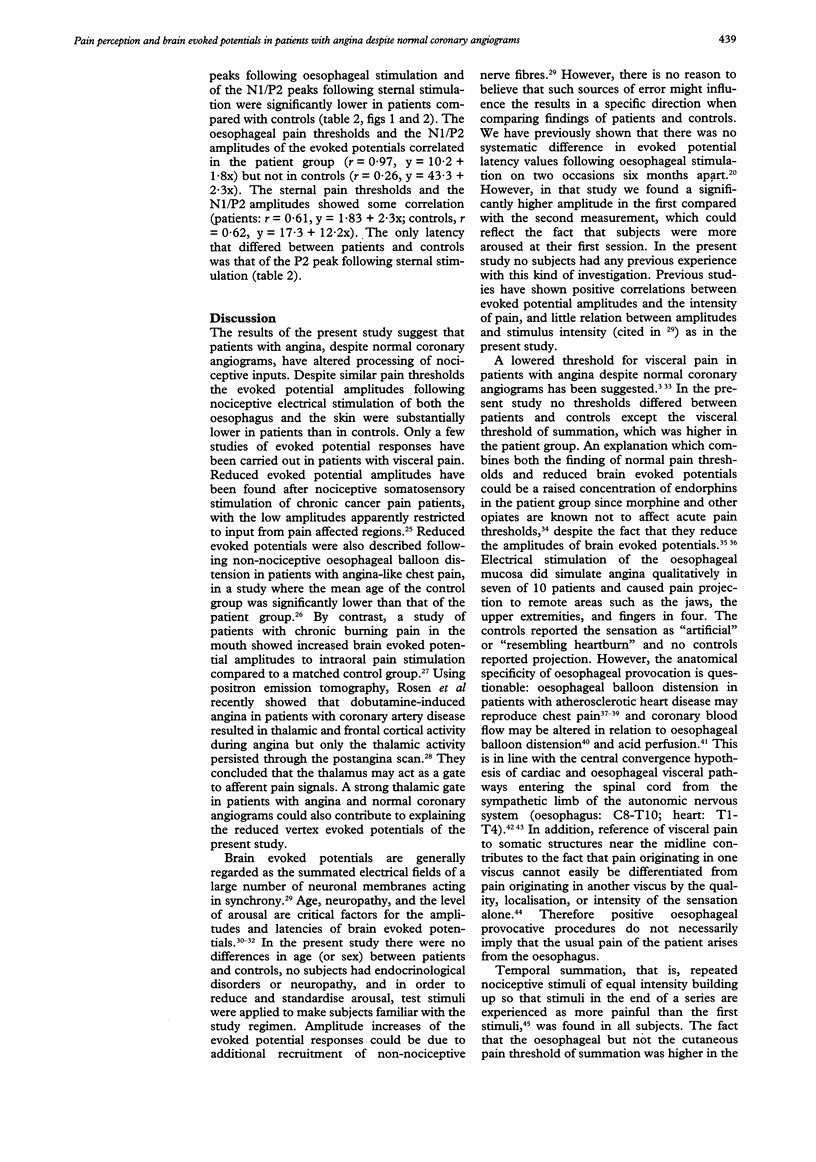
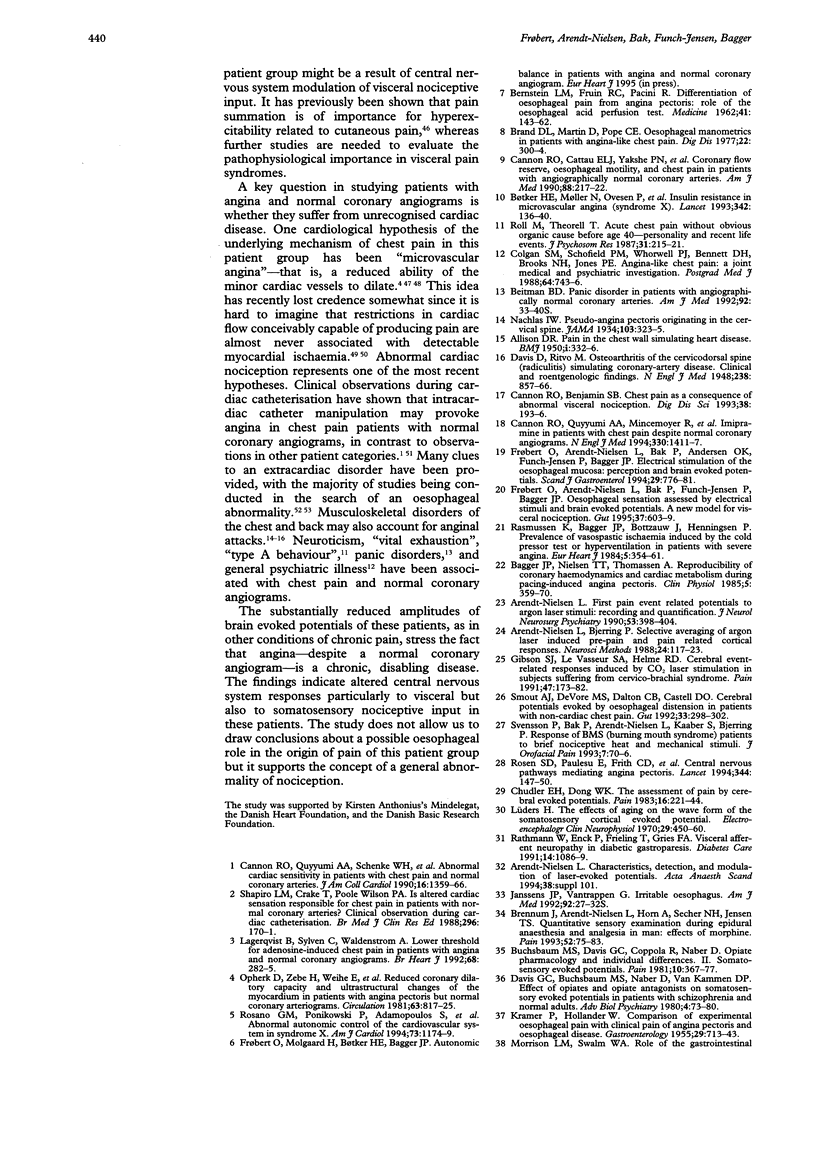
OBJECTIVE: To evaluate the role of nociception in patients with angina despite normal coronary angiograms and to investigate whether any abnormality is confined to visceral or somatosensory perception. METHODS: Perception, pain threshold, and brain evoked potentials to nociceptive electrical stimuli of the oesophageal mucosa and the sternal skin were investigated in 10 patients who had angina but normal coronary angiograms, no other signs of cardiac disease, and normal upper endoscopy. Controls were 10 healthy volunteers. The peaks of the evoked potential signal were designated N for negative deflections and P for positive. Numbers were given to the peaks in order of appearance after the stimulus. The peak to peak amplitudes (P1/N1, N1/P2) were measured in microV. RESULTS: (1) Angina pectoris was provoked in seven patients following continuous oesophageal stimulation. (2) Distant projection of pain occurred after continuous electrical stimulation of the oesophagus in four patients and in no controls. (3) Patients had higher oesophageal pain thresholds (median 16.3 mA v 7.3 mA, P = 0.02) to repeated stimuli than controls, whereas the values did not differ with respect to the skin. There were no intergroup differences in thresholds to single stimuli. (4) Patients had substantially reduced brain evoked potential amplitudes after both single oesophageal (P1/N1, median values: 7.2 microV, controls: 29.0 microV; N1/P2: 16.5 microV, controls: 66.0 microV; P < 0.001 for both) and skin (N1/P2: 13.5 microV; controls: 76.0 microV; P < 0.001) stimuli despite the similar pain thresholds. CONCLUSION: Central nervous system responses to visceral and somatosensory nociceptive input are altered in patients who have angina despite normal coronary angiograms.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ALLISON D. R. Pain in the chest wall simulating heart disease. Br Med J. 1950 Feb 11;1(4649):332–336. doi: 10.1136/bmj.1.4649.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arendt-Nielsen L., Bjerring P. Selective averaging of argon laser induced pre-pain and pain related cortical responses. J Neurosci Methods. 1988 Jun;24(2):117–123. doi: 10.1016/0165-0270(88)90054-4. [DOI] [PubMed] [Google Scholar]
- Arendt-Nielsen L., Brennum J., Sindrup S., Bak P. Electrophysiological and psychophysical quantification of temporal summation in the human nociceptive system. Eur J Appl Physiol Occup Physiol. 1994;68(3):266–273. doi: 10.1007/BF00376776. [DOI] [PubMed] [Google Scholar]
- Arendt-Nielsen L. First pain event related potentials to argon laser stimuli: recording and quantification. J Neurol Neurosurg Psychiatry. 1990 May;53(5):398–404. doi: 10.1136/jnnp.53.5.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BERNSTEIN L. M., FRUIN R. D., PACINI R. Differentiation of esophageal pain from angina pectoris: role of the esophageal acid perfusion test. Medicine (Baltimore) 1962 May;41:143–162. doi: 10.1097/00005792-196205000-00002. [DOI] [PubMed] [Google Scholar]
- Bagger J. P., Nielsen T. T., Thomassen A. Reproducibility of coronary haemodynamics and cardiac metabolism during pacing-induced angina pectoris. Clin Physiol. 1985 Aug;5(4):359–370. doi: 10.1111/j.1475-097x.1985.tb00756.x. [DOI] [PubMed] [Google Scholar]
- Beitman B. D. Panic disorder in patients with angiographically normal coronary arteries. Am J Med. 1992 May 27;92(5A):33S–40S. doi: 10.1016/0002-9343(92)80054-4. [DOI] [PubMed] [Google Scholar]
- Brand D. L., Martin D., Pope C. E., 2nd Esophageal manometrics in patients with angina-like chest pain. Am J Dig Dis. 1977 Apr;22(4):300–304. doi: 10.1007/BF01072186. [DOI] [PubMed] [Google Scholar]
- Brennum J., Arendt-Nielsen L., Horn A., Secher N. H., Jensen T. S. Quantitative sensory examination during epidural anaesthesia and analgesia in man: effects of morphine. Pain. 1993 Jan;52(1):75–83. doi: 10.1016/0304-3959(93)90117-8. [DOI] [PubMed] [Google Scholar]
- Buchsbaum M. S., Davis G. C., Coppola R., Naber D. Opiate pharmacology and individual differences. II. Somatosensory evoked potentials. Pain. 1981 Jun;10(3):367–377. doi: 10.1016/0304-3959(81)90098-1. [DOI] [PubMed] [Google Scholar]
- Bøtker H. E., Møller N., Ovesen P., Mengel A., Schmitz O., Orskov H., Bagger J. P. Insulin resistance in microvascular angina (syndrome X) Lancet. 1993 Jul 17;342(8864):136–140. doi: 10.1016/0140-6736(93)91344-l. [DOI] [PubMed] [Google Scholar]
- Camici P. G., Gistri R., Lorenzoni R., Sorace O., Michelassi C., Bongiorni M. G., Salvadori P. A., L'Abbate A. Coronary reserve and exercise ECG in patients with chest pain and normal coronary angiograms. Circulation. 1992 Jul;86(1):179–186. doi: 10.1161/01.cir.86.1.179. [DOI] [PubMed] [Google Scholar]
- Cannon R. O., 3rd, Benjamin S. B. Chest pain as a consequence of abnormal visceral nociception. Dig Dis Sci. 1993 Feb;38(2):193–196. doi: 10.1007/BF01307534. [DOI] [PubMed] [Google Scholar]
- Cannon R. O., 3rd, Cattau E. L., Jr, Yakshe P. N., Maher K., Schenke W. H., Benjamin S. B., Epstein S. E. Coronary flow reserve, esophageal motility, and chest pain in patients with angiographically normal coronary arteries. Am J Med. 1990 Mar;88(3):217–222. doi: 10.1016/0002-9343(90)90145-4. [DOI] [PubMed] [Google Scholar]
- Cannon R. O., 3rd, Epstein S. E. "Microvascular angina" as a cause of chest pain with angiographically normal coronary arteries. Am J Cardiol. 1988 Jun 1;61(15):1338–1343. doi: 10.1016/0002-9149(88)91180-0. [DOI] [PubMed] [Google Scholar]
- Cannon R. O., 3rd, Quyyumi A. A., Mincemoyer R., Stine A. M., Gracely R. H., Smith W. B., Geraci M. F., Black B. C., Uhde T. W., Waclawiw M. A. Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 1994 May 19;330(20):1411–1417. doi: 10.1056/NEJM199405193302003. [DOI] [PubMed] [Google Scholar]
- Cannon R. O., 3rd, Quyyumi A. A., Schenke W. H., Fananapazir L., Tucker E. E., Gaughan A. M., Gracely R. H., Cattau E. L., Jr, Epstein S. E. Abnormal cardiac sensitivity in patients with chest pain and normal coronary arteries. J Am Coll Cardiol. 1990 Nov;16(6):1359–1366. doi: 10.1016/0735-1097(90)90377-2. [DOI] [PubMed] [Google Scholar]
- Chauhan A., Mullins P. A., Thuraisingham S. I., Taylor G., Petch M. C., Schofield P. M. Abnormal cardiac pain perception in syndrome X. J Am Coll Cardiol. 1994 Aug;24(2):329–335. doi: 10.1016/0735-1097(94)90284-4. [DOI] [PubMed] [Google Scholar]
- Chauhan A., Petch M. C., Schofield P. M. Effect of oesophageal acid instillation on coronary blood flow. Lancet. 1993 May 22;341(8856):1309–1310. doi: 10.1016/0140-6736(93)90817-z. [DOI] [PubMed] [Google Scholar]
- Chudler E. H., Dong W. K. The assessment of pain by cerebral evoked potentials. Pain. 1983 Jul;16(3):221–244. doi: 10.1016/0304-3959(83)90111-2. [DOI] [PubMed] [Google Scholar]
- Colgan S. M., Schofield P. M., Whorwell P. J., Bennett D. H., Brooks N. H., Jones P. E. Angina-like chest pain: a joint medical and psychiatric investigation. Postgrad Med J. 1988 Oct;64(756):743–746. doi: 10.1136/pgmj.64.756.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubner R. Pain and hyperalgesia following tissue injury: new mechanisms and new treatments. Pain. 1991 Mar;44(3):213–214. doi: 10.1016/0304-3959(91)90087-E. [DOI] [PubMed] [Google Scholar]
- Frøbert O., Arendt-Nielsen L., Bak P., Andersen O. K., Funch-Jensen P., Bagger J. P. Electric stimulation of the esophageal mucosa. Perception and brain-evoked potentials. Scand J Gastroenterol. 1994 Sep;29(9):776–781. doi: 10.3109/00365529409092509. [DOI] [PubMed] [Google Scholar]
- Frøbert O., Arendt-Nielsen L., Bak P., Funch-Jensen P., Bagger J. P. Oesophageal sensation assessed by electrical stimuli and brain evoked potentials--a new model for visceral nociception. Gut. 1995 Nov;37(5):603–609. doi: 10.1136/gut.37.5.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison D. W., Chandler M. J., Foreman R. D. Viscerosomatic convergence onto feline spinal neurons from esophagus, heart and somatic fields: effects of inflammation. Pain. 1992 Jun;49(3):373–382. doi: 10.1016/0304-3959(92)90245-7. [DOI] [PubMed] [Google Scholar]
- Gayheart P. A., Gwirtz P. A., Bravenec J. S., Longlet N., Jones C. E. An alpha-adrenergic coronary constriction during esophageal distention in the dog. J Cardiovasc Pharmacol. 1991 May;17(5):747–753. doi: 10.1097/00005344-199105000-00009. [DOI] [PubMed] [Google Scholar]
- Gibson S. J., LeVasseur S. A., Helme R. D. Cerebral event-related responses induced by CO2 laser stimulation in subjects suffering from cervico-brachial syndrome. Pain. 1991 Nov;47(2):173–182. doi: 10.1016/0304-3959(91)90202-9. [DOI] [PubMed] [Google Scholar]
- Hewson E. G., Dalton C. B., Richter J. E. Comparison of esophageal manometry, provocative testing, and ambulatory monitoring in patients with unexplained chest pain. Dig Dis Sci. 1990 Mar;35(3):302–309. doi: 10.1007/BF01537406. [DOI] [PubMed] [Google Scholar]
- Janssens J. P., Vantrappen G. Irritable esophagus. Am J Med. 1992 May 27;92(5A):27S–32S. doi: 10.1016/0002-9343(92)80053-3. [DOI] [PubMed] [Google Scholar]
- Lagerqvist B., Sylvén C., Waldenström A. Lower threshold for adenosine-induced chest pain in patients with angina and normal coronary angiograms. Br Heart J. 1992 Sep;68(3):282–285. doi: 10.1136/hrt.68.9.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüders H. The effect of aging on the wave form of the somatosensory cortical evoked potential. Electroencephalogr Clin Neurophysiol. 1970 Nov;29(5):450–460. doi: 10.1016/0013-4694(70)90062-3. [DOI] [PubMed] [Google Scholar]
- Ness T. J., Gebhart G. F. Visceral pain: a review of experimental studies. Pain. 1990 May;41(2):167–234. doi: 10.1016/0304-3959(90)90021-5. [DOI] [PubMed] [Google Scholar]
- Opherk D., Zebe H., Weihe E., Mall G., Dürr C., Gravert B., Mehmel H. C., Schwarz F., Kübler W. Reduced coronary dilatory capacity and ultrastructural changes of the myocardium in patients with angina pectoris but normal coronary arteriograms. Circulation. 1981 Apr;63(4):817–825. doi: 10.1161/01.cir.63.4.817. [DOI] [PubMed] [Google Scholar]
- Rasmussen K., Bagger J. P., Bøttzauw J., Henningsen P. Prevalence of vasospastic ischaemia induced by the cold pressor test or hyperventilation in patients with severe angina. Eur Heart J. 1984 May;5(5):354–361. doi: 10.1093/oxfordjournals.eurheartj.a061668. [DOI] [PubMed] [Google Scholar]
- Rathmann W., Enck P., Frieling T., Gries F. A. Visceral afferent neuropathy in diabetic gastroparesis. Diabetes Care. 1991 Nov;14(11):1086–1089. doi: 10.2337/diacare.14.11.1086. [DOI] [PubMed] [Google Scholar]
- Roll M., Theorell T. Acute chest pain without obvious organic cause before age 40--personality and recent life events. J Psychosom Res. 1987;31(2):215–221. doi: 10.1016/0022-3999(87)90078-x. [DOI] [PubMed] [Google Scholar]
- Rosano G. M., Ponikowski P., Adamopoulos S., Collins P., Poole-Wilson P. A., Coats A. J., Kaski J. C. Abnormal autonomic control of the cardiovascular system in syndrome X. Am J Cardiol. 1994 Jun 15;73(16):1174–1179. doi: 10.1016/0002-9149(94)90177-5. [DOI] [PubMed] [Google Scholar]
- Rosen S. D., Paulesu E., Frith C. D., Frackowiak R. S., Davies G. J., Jones T., Camici P. G. Central nervous pathways mediating angina pectoris. Lancet. 1994 Jul 16;344(8916):147–150. doi: 10.1016/s0140-6736(94)92755-3. [DOI] [PubMed] [Google Scholar]
- Rosen S. D., Uren N. G., Kaski J. C., Tousoulis D., Davies G. J., Camici P. G. Coronary vasodilator reserve, pain perception, and sex in patients with syndrome X. Circulation. 1994 Jul;90(1):50–60. doi: 10.1161/01.cir.90.1.50. [DOI] [PubMed] [Google Scholar]
- Sax F. L., Cannon R. O., 3rd, Hanson C., Epstein S. E. Impaired forearm vasodilator reserve in patients with microvascular angina. Evidence of a generalized disorder of vascular function? N Engl J Med. 1987 Nov 26;317(22):1366–1370. doi: 10.1056/NEJM198711263172202. [DOI] [PubMed] [Google Scholar]
- Shapiro L. M., Crake T., Poole-Wilson P. A. Is altered cardiac sensation responsible for chest pain in patients with normal coronary arteries? Clinical observation during cardiac catheterisation. Br Med J (Clin Res Ed) 1988 Jan 16;296(6616):170–171. doi: 10.1136/bmj.296.6616.170-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smout A. J., DeVore M. S., Dalton C. B., Castell D. O. Cerebral potentials evoked by oesophageal distension in patients with non-cardiac chest pain. Gut. 1992 Mar;33(3):298–302. doi: 10.1136/gut.33.3.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvén C. Angina pectoris. Clinical characteristics, neurophysiological and molecular mechanisms. Pain. 1989 Feb;36(2):145–167. doi: 10.1016/0304-3959(89)90019-5. [DOI] [PubMed] [Google Scholar]
- Vantrappen G., Janssens J., Ghillebert G. The irritable oesophagus--a frequent cause of angina-like pain. Lancet. 1987 May 30;1(8544):1232–1234. doi: 10.1016/s0140-6736(87)92686-9. [DOI] [PubMed] [Google Scholar]


