Abstract
Background
Although patients with peripheral artery disease (PAD) are known to have an increased risk of adverse prognosis, simple techniques to further risk‐stratify PAD patients would be clinically useful. A plausible but unexplored factor to predict such risk would be greater disease burden, manifested as multiple lower extremity lesions. The aim of this study was to examine the association between having multiple versus isolated lower extremity PAD lesions and long‐term prognosis.
Methods and Results
A prospective cohort of 756 newly diagnosed PAD patients underwent duplex ultrasound testing to determine the number of lower extremity lesions. Cox regression models examined the independent association of lesion number (≥3 and 2 versus 1) and adverse prognosis (defined as a composite end point comprising first occurrence of either lower extremity amputation, admission for heart failure, nonfatal stroke, myocardial infarction, or unstable angina or mortality), adjusting for demographic and clinical risk factors. Analyses were replicated using an advanced Cox‐based model for multiple events. A total of 173 patients (23%) had ≥3 lesions, 197 (26%) had 2 lesions, and 386 (51%) had 1 lesion. After a median follow‐up of 3.2 years, patients with ≥3 lesions had an increased risk of experiencing a first adverse event (adjusted hazard ratio 1.60, 95% CI 1.08–2.38, P=0.020) and an increased risk of having multiple events (adjusted hazard ratio 1.53, 95% CI 1.08–2.18, P=0.018). Patients with 2 lesions had a prognosis similar to those with 1 lesion.
Conclusions
Among PAD patients, a greater number of lesions is associated with an increased risk of an adverse prognosis over 3 years of follow‐up. Assessing the number of lower extremity lesions might serve as a simple risk‐stratification tool at initial PAD diagnosis.
Keywords: claudication, peripheral artery disease, prognosis, statistics, survival
Introduction
Patients with peripheral arterial disease (PAD) are a vulnerable population because they not only experience functional impairment1, 2 but also face an excess risk of an adverse prognosis (eg, myocardial infarction [MI], angina, stroke, heart failure, lower extremity amputation, and death) due to concomitant coronary and cerebrovascular disease.3, 4, 5
This risk of an adverse prognosis is applicable to the whole spectrum of PAD patients and thus mandates aggressive cardiovascular risk factor control through the prescription of statins, antiplatelet therapy, and smoking cessation.6, 7, 8 There have been few efforts, however, to further risk‐stratify patients with PAD at the time of their initial presentation. A simple marker of a worse prognosis could be the extent of disease, as suggested by the number of obstructive lesions identified at presentation. The clinical logic is that a greater number of lesions may reflect a more aggressive disease process, not only in the peripheral arteries but also in the coronary and cerebral vasculature. Risk‐stratifying PAD patients may be clinically useful so that more intensive follow‐up and more aggressive treatment might be considered, including a more thorough workup and screening for occult coronary or cerebrovascular disease.
It is expected that patients presenting with multiple lower extremity arterial lesions are more likely to be at increased risk of having any or multiple adverse events than those having a single lesion; however, this assumption has not been thoroughly quantified in PAD patients.9 Initial evidence to support our hypothesis is provided by secondary analyses of the BASIL trial, in which the number of detectable ankle pressures in critical limb ischemia patients—a more advanced presentation of PAD—was positively associated with better 2‐year survival outcomes.10 To further address this gap in knowledge in patients with earlier stages of PAD, our objectives were to document patient risk of experiencing a first adverse event and multiple adverse events (defined as a composite end point of either lower extremity amputation, admission for heart failure, nonfatal stroke, MI, or unstable angina or mortality) after an initial PAD diagnosis (Rutherford grade I, including patients with mild, moderate, and severe claudication) as a function of the number of lower extremity arterial lesions identified. We also explored whether the risk associated with number of lesions differed by the type of adverse event (lower extremity amputation, unstable angina, MI, heart failure, stroke, or death). This information could support better quantification of PAD patient risk for subsequent events and may provide clinicians with an easy way to risk‐stratify patients with new onset or worsening symptoms of PAD.
Methods
Patients and Study Design
A total of 756 PAD patients were systematically followed for a median of 3.2 years (±1.6 years, interquartile range 1.7 to 4.5 years; verification of adverse prognosis information occurred up to January 1, 2012). Patients were consecutively enrolled from 2 vascular surgery outpatient clinics (St. Elisabeth Hospital and TweeSteden Hospital, Tilburg, Netherlands) between March 2006 and October 2011 if they presented with new‐onset PAD symptoms or exacerbation of existing PAD requiring re‐evaluation and treatment. Other inclusion criteria were abnormal resting ankle‐brachial index (ABI; ≤0.90) or a decrease in postexercise ABI ≥15% following a distance‐limited treadmill test. Patients with critical limb ischemia were excluded because their clinical trajectories, treatments, and outcomes look vastly different from those of patients with PAD who present with earlier stages of the disease. Patients were also excluded if they had a noncompressible ABI (≥1.30), severe cognitive impairment, or severe psychiatric or somatic comorbidities (eg, psychosis or active cancer treatment) or if they did not have sufficient knowledge of the Dutch language. Because the focus of this study was on the number of lower extremity lesions, patients were excluded if no preprocedural duplex ultrasound examination was available from their medical records within 3 months of enrollment (Figure S1 provides an overview of exclusions).
All patients underwent noninvasive vascular laboratory testing as part of their clinical evaluation for PAD including resting and postexercise ABI measurements and a duplex ultrasound examination. Information on demographic and socioeconomic factors was obtained from patients at baseline through purpose‐designed questionnaires, and information on clinical factors was collected through medical chart abstraction. Finally, up‐to‐date vital status information until January 1, 2012, was retrieved from patients’ electronic medical records, which contained information on in‐hospital deaths and deaths that occurred outside the hospital because records are linked to the regional social security death index of the Tilburg community. Information on deaths occurring outside the Tilburg community was provided by patients’ general practitioners.
The study was designed in accordance with the Helsinki Declaration and approved by the local institutional review board of each participating site. All participants provided written informed consent.
Measures
Adverse prognosis
The primary outcome of this study was a combination of any of the following events, as documented by patients’ hospital or death records: (1) PAD‐related major lower extremity amputation, (2) heart failure, (3) nonfatal stroke, (4) nonfatal MI or unstable angina, (5) fatal MI or stroke, (6) other cardiovascular deaths (cardiac arrest, heart failure, sepsis), and (7) other causes of death (exacerbation of chronic obstructive pulmonary disease, cancer). Data on adverse events were abstracted from patients’ medical records based on the diagnosis and treatment discharge codes and discharge notes and adjudicated by a team of 3 physicians (surgical fellow and 2 vascular surgeons).
Vascular laboratory assessments
Patient ABI was read from a handheld Doppler instrument (Imexlab 9000; Imex Medical Systems Inc) used by trained vascular technicians. Both resting and postexercise ABIs were obtained in both legs. The lowest resting ABI value was used in our analyses. The exercise protocol included a distance‐limited treadmill test (1000 m) from which the pain‐free walking and maximum walking distances were derived.
Duplex ultrasound examination protocol
Information on number of lesions, anatomical lesion location, and lesion severity, as indicated by the peak systolic velocity (PSV) ratio (in cm/s), was derived from duplex ultrasound examinations prior to the initiation of any treatment. A detailed description of the duplex ultrasound examination protocol was published previously.11
A team of 3 physicians (surgical fellow and 2 vascular surgeons) adjudicated the duplex information; they quantified and classified patients based on the number of peripheral arterial lesions. Lesions with a PSV ratio ≥2.5 or total occlusions were considered significant, and lesions with a PSV ratio >0 to <2.5 were considered nonsignificant.6, 11, 12, 13 The numbers of nonsignificant and significant lesions were documented from duplex ultrasound readings. The number of significant lower extremity lesions at the patient level was used in our analyses. When determining the number of lesions, each significant lesion was counted as 1 lesion, regardless of its anatomical location in the peripheral arteries. If a patient had, for example, multiple lesions in the superficial femoral artery, then all significant lesions were counted.
The peripheral vascular lesions were categorized into 3 categories: (1) proximal lesions (aortoiliac segments including the distal abdominal aorta, right and left common iliac artery, right and left external iliac artery, and bifurcation of the right and left internal iliac artery); (2) distal lesions (femoropopliteal segments including the right and left common femoral artery, bifurcation of the right and left deep femoral artery, the right and left superficial femoral artery, and right and left popliteal artery and crural segments including the right and left posterior tibial artery, right and left peroneal artery, and right and left anterior tibial artery); and (3) both proximal and distal lesions, which included lesions or occlusions that presented at both proximal and distal locations. Because these 3 categories were not mutually exclusive, each lesion location category was compared against all patients who were not in that category. In our multivariable analyses, having any proximal lesions was compared against having distal lesions only. Duplex ultrasonography has a median sensitivity of 88% (95% CI 80% to 98%) and a specificity of 96% (95% CI 89% to 99%) to detect a stenosis of ≥50% or an occlusion when imaging the whole leg versus the standard of contrast angiography.14
Patient characteristics
Information on clinical factors was abstracted from patients’ medical records and included cardiovascular history (prior angina, MI, coronary artery bypass grafting, percutaneous coronary intervention, heart failure, stroke, and transient ischemic attack), other clinical risk factors (current smoking status, diabetes mellitus, hypertension, dyslipidemia, chronic obstructive pulmonary disease, body mass index [in kg/m2], renal dysfunction, total cholesterol levels [in mg/dL], high‐density lipoprotein cholesterol [in mg/dL], systolic brachial blood pressure [ie, the highest of 2 arms in mm Hg], back pain, and hip or knee osteoarthritis), and medications that patients were on following their vascular workup.
Demographic factors were obtained from patients’ medical records and included age and sex. Socioeconomic factors were derived from purpose‐designed questionnaires and included patients’ marital status (no partner versus partner), education (less than a high school degree versus high school degree or higher), and work status (nonactive versus active).
Statistical Analysis
The analyses conducted for this study were patient based, meaning that the counts of lesions were cumulative across lower extremities within a patient. Patients were categorized by the number of significant lower extremity lesions, as derived from the duplex ultrasound readings, as ≥3 lesions (≥3 lesions with a PSV ratio ≥2.5 and/or total occlusions), 2 lesions (2 lesions with a PSV ratio ≥2.5 and/or total occlusions), or 1 lesion (1 lesion with a PSV ratio ≥2.5 or 1 occlusion, or nonsignificant lesions with a PSV ratio >0 to <2.5).
Baseline patient characteristics were described for the total population and compared among the 3 groups. Categorical variables were analyzed by the chi‐square test, and 1‐way ANOVA was used to analyze continuous variables.
Due to power considerations, the association between the number of lesions (≥3 or 2 versus 1) and adverse events was analyzed using a composite end point (ie, amputation, unstable angina, MI, heart failure, stroke, and death). In addition, a multivariate analysis examined the association between the number of lesions and adverse event type.
Time‐to‐first‐event analysis
Patients were followed for a median of 3.2 years (±1.6 years, interquartile range 1.7–4.5 years). The incidence of adverse events by ≥3 or 2 versus 1 lesion (reference) was plotted by Kaplan–Meier curves, and survival curves were tested by the log‐rank test. Risk estimates (hazard ratios [HRs] and their 95% CIs) for the association between having ≥3 or 2 versus 1 (reference) lower extremity lesion and experiencing a first major adverse event at 3.2‐year follow‐up were calculated using a traditional time‐to‐first‐event Cox regression model. Multivariable analyses were adjusted for the following a priori selected covariates: demographics (age, sex), resting ABI, cardiovascular history (angina, MI, percutaneous coronary intervention, coronary artery bypass grafting, heart failure, stroke, transient ischemic attack), other clinical risk factors (body mass index, chronic obstructive pulmonary disease, hypertension, hyperlipidemia, diabetes, renal dysfunction, smoking status, total cholesterol, high‐density lipoprotein cholesterol, systolic blood pressure), and presence of proximal versus nonproximal lesions (reference). Baseline hazards were also stratified by hospital. Effects of continuous variables (age, body mass index, ABI) were tested for linearity using restricted cubic splines. Proportional hazards assumptions were evaluated using Schoenfeld residuals.
Sensitivity analysis
A sensitivity analysis was performed to evaluate the association between having ≥3 or 2 versus 1 lesion (reference) and 3.2‐year risk of multiple adverse events, as opposed to the main time‐to‐first‐event analysis, using an unadjusted and adjusted Cox‐based intensity‐elapsed time model15 including the same covariates as in the time‐to‐first‐event analysis. This model assumes that all events are equally likely to occur, independent of prior events, with the risk of each event starting from “time zero,” the time of initial enrollment.15 The within‐patient correlation was modeled by a frailty term (ie, a random component to account for within‐patient correlation). The mean cumulative incidence of events was also calculated, stratified by the number of lesions (≥3 or 2 versus 1 lesion [reference]).
Event‐specific analyses
Given the composite nature of the outcome, a multivariate Cox regression model was constructed to evaluate whether the risk associated with number of lesions varied by event type. This analysis modeled time to first event separately for each type of event, with event‐specific baseline hazard functions, an interaction between number of lesions and event type, adjustment for other covariates as described above, and a frailty term to model within‐patient correlation. A secondary analysis was performed to evaluate the association between the number of arterial lesions and cumulative incidence of major adverse cardiac events, including fatal or nonfatal MI or stroke. Deaths due to other causes were treated as competing risk events. Because only 12 patients experienced multiple events of the same type, this analysis modeled only time to first event.
The follow‐up data for adverse events were complete. Covariate data were complete except for body mass index, total cholesterol, high‐density lipoprotein cholesterol, and systolic blood pressure, which were missing on 16%, 12%, 12%, and 4% of patients, respectively. For modeling purposes, missing values were imputed using single regression imputation on all other available covariates and outcomes.
All statistical analyses were performed with SAS software version 9.3 (SAS Institute Inc) and R software version 2.14.1 (R Foundation). All tests were 2‐tailed, and P values <0.05 were considered statistically significant.
Results
Baseline Characteristics by Number of Lesions
Of the 756 included patients, 173 (23%) presented with ≥3 lesions, 197 (26%) had 2 significant lesions, and 386 (51%) had a nonsignificant lesion (n=77) or 1 significant lesion (n=309).
Table 1 summarizes patient characteristics for the total study population stratified by the number of lower extremity arterial lesions. The mean age of the population was 65 years (±10 years, range 37–92 years), and 65% were male. Patients with ≥3 lesions were older; lower rates of having a partner were noted, whereas higher rates of prior cardiovascular history and use of cardiovascular medications, antidepressants, and hypnotics were observed. Patients with ≥3 lesions presented with higher proportions of distal lesions and lesions in both proximal and distal segments. Finally, patient maximum walking distance, resting ABI, and postexercise ABI values were also lower in patients with ≥3 lesions as compared with patients having fewer lesions.
Table 1.
Baseline Characteristics for the Total Sample Stratified by the Number of Lower Extremity PAD Lesions (≥3 or 2 Versus 1 Lesion)
| Total Sample (n=756) | ≥3 Lesions (n=173) | 2 Lesions (n=197) | 1 Lesion (n=386) | P Value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (mean±SD), y | 65.0±9.8 | 68.0±10.2 | 64.9±9.6 | 63.8±9.5 | <0.001 |
| Age <50 years, n (%) | 50 (6.6) | 6 (3.5) | 14 (7.1) | 30 (7.8) | 0.002 |
| Age 50 to 69 years, n (%) | 430 (56.9) | 82 (47.4) | 114 (57.9) | 234 (60.6) | |
| Age ≥70 years, n (%) | 276 (36.5) | 85 (49.1) | 69 (35.0) | 122 (31.6) | |
| Male sex, n (%) | 489 (64.7) | 117 (67.6) | 136 (69.0) | 236 (61.1) | 0.11 |
| Socioeconomic factors | |||||
| No partner, n (%) | 162 (21.4) | 51 (34.9) | 40 (23.7) | 71 (21.5) | 0.007 |
| Less than high school degree, n (%) | 165 (21.8) | 42 (29.2) | 45 (26.6) | 78 (23.8) | 0.45 |
| Active working status, n (%) | 163 (21.6) | 25 (18.2) | 48 (28.7) | 90 (28.1) | 0.06 |
| Cardiovascular risk factors | |||||
| Prior angina, n (%) | 112 (14.8) | 39 (22.5) | 19 (9.6) | 54 (14.0) | 0.002 |
| Prior myocardial infarction, n (%) | 140 (18.5) | 48 (27.7) | 35 (17.8) | 57 (14.8) | 0.001 |
| Prior coronary artery bypass grafting, n (%) | 82 (10.8) | 26 (15.0) | 17 (8.6) | 39 (10.1) | 0.11 |
| Prior percutaneous coronary intervention, n (%) | 70 (9.3) | 15 (8.7) | 21 (10.7) | 34 (8.8) | 0.73 |
| Heart failure, n (%) | 36 (4.8) | 9 (5.2) | 8 (4.1) | 19 (4.9) | 0.86 |
| Prior transient ischemic attack, n (%) | 66 (8.7) | 24 (13.9) | 13 (6.6) | 29 (7.5) | 0.023 |
| Prior stroke, n (%) | 59 (7.8) | 16 (9.2) | 16 (8.1) | 27 (7.0) | 0.64 |
| Clinical factors | |||||
| Body mass index, mean±SD | 26.8±4.9 | 26.4±4.6 | 26.5±3.9 | 27.1±5.5 | 0.25 |
| Total cholesterol, mg/dL (mean±SD) | 193.3±46.0 | 186.8±45.1 | 194.0±45.4 | 195.9±46.5 | 0.13 |
| High‐density lipoprotein cholesterol, mg/dL (mean±SD) | 49.2±14.3 | 48.8±13.0 | 51.0±17.4 | 48.5±12.9 | 0.15 |
| Systolic blood pressure, mm Hg (mean±SD) | 158.7±22.6 | 161.6 ±25.4 | 159.2±21.1 | 157.2±21.8 | 0.10 |
| Smoking, n (%) | 375 (49.6) | 75 (43.4) | 99 (50.3) | 201 (52.1) | 0.16 |
| Diabetes mellitus, n (%) | 183 (24.2) | 43 (24.9) | 47 (23.9) | 93 (24.1) | 0.97 |
| Hyperlipidemia, n (%) | 512 (67.7) | 126 (72.8) | 127 (64.5) | 259 (67.1) | 0.21 |
| Hypertension, n (%) | 452 (59.8) | 113 (65.3) | 115 (58.4) | 224 (58.0) | 0.24 |
| Chronic obstructive pulmonary disease, n (%) | 136 (18.0) | 29 (16.8) | 36 (18.3) | 71 (18.4) | 0.89 |
| Renal dysfunction, n (%) | 69 (9.1) | 22 (12.7) | 18 (9.1) | 29 (7.5) | 0.14 |
| Back pain, n (%) | 113 (14.9) | 19 (11.0) | 34 (17.3) | 60 (15.5) | 0.22 |
| Hip or knee osteoarthritis, n (%) | 156 (20.6) | 33 (19.1) | 43 (21.8) | 80 (20.7) | 0.81 |
| Medication use | |||||
| Aspirin, n (%) | 586 (77.5) | 137 (79.2) | 149 (75.6) | 300 (77.7) | 0.71 |
| Statins, n (%) | 616 (81.5) | 145 (83.8) | 164 (83.2) | 307 (79.5) | 0.37 |
| Beta blocker, n (%) | 315 (41.7) | 79 (45.7) | 72 (36.5) | 164 (42.5) | 0.19 |
| Diuretics, n (%) | 190 (25.1) | 57 (32.9) | 50 (25.4) | 83 (21.5) | 0.016 |
| Angiotensin‐converting enzyme inhibitor, n (%) | 234 (31.0) | 68 (39.3) | 62 (31.5) | 104 (26.9) | 0.014 |
| Calcium antagonist, n (%) | 167 (22.1) | 45 (26.0) | 47 (23.9) | 75 (19.4) | 0.18 |
| Nitroglycerin, n (%) | 67 (8.9) | 25 (14.5) | 16 (8.1) | 26 (6.7) | 0.011 |
| Anticoagulants, n (%) | 125 (16.5) | 40 (23.1) | 30 (15.2) | 55 (14.2) | 0.028 |
| Digoxin, n (%) | 18 (2.4) | 9 (5.2) | 3 (1.5) | 6 (1.6) | 0.042 |
| Antiarrhythmics, n (%) | 21 (2.8) | 8 (4.6) | 4 (2.0) | 9 (2.3) | 0.27 |
| Antidepressives, n (%) | 45 (6.0) | 13 (7.5) | 3 (1.5) | 29 (7.5) | 0.009 |
| Anxiolytics, n (%) | 31 (4.1) | 9 (5.2) | 4 (2.0) | 18 (4.7) | 0.22 |
| Hypnotics, n (%) | 34 (4.5) | 16 (9.2) | 3 (1.5) | 15 (3.9) | 0.001 |
| Anatomical lesion location | <0.001 | ||||
| Nonsignificant lesion, n (%) | 71 (9.4) | 0 (0.0) | 0 (0.0) | 71 (19.2) | |
| Proximal lesions, n (%) | 219 (29.0) | 31 (19.3) | 69 (36.7) | 119 (32.2) | |
| Distal lesions, n (%) | 363 (48.0) | 89 (55.3) | 94 (50.0) | 180 (48.6) | |
| Proximal and distal lesions, n (%) | 66 (8.7) | 14 (25.5) | 25 (13.3) | 0 (0.0) | |
| Vascular laboratory assessment | |||||
| Pain‐free walking distance, median (IQR), m | 80.0 (40.0–130.0) | 70.0 (40.0–130.0) | 80.0 (50.0–140.0) | 70.0 (30.0–130.0) | 0.69 |
| Maximum walking distance, median (IQR), m | 250.0 (140.0–500.0) | 230 (120.0–400.0) | 250.0 (140.0–520.0) | 280.0 (160.0–500.0) | 0.028 |
| Resting ankle‐brachial index, median % (IQR) | 65.0 (53.0–79.0) | 55.5 (48.0–67.0) | 64.0 (53.0–75.0) | 71.0 (59.0–83.0) | <0.001 |
| Postexercise ankle‐brachial index, median % (IQR) | 35.0 (26.0–54.0) | 28.0 (20.0–39.0) | 32.0 (25.0–46.0) | 41.0 (30.0–62.0) | <0.001 |
Overall P values for each comparison are provided. IQR indicates interquartile range; PAD, peripheral arterial disease.
Adverse Events
A total of 218 adverse events occurred among 155 patients (20%) who experienced at least 1 event and among 41 patients (5%) who had at least 2 events during follow‐up. Table 2 summarizes the crude cumulative incidence rates stratified by event type; deaths (n=87) were the most commonly documented events.
Table 2.
Total Number of Patients and Events by Event Category for the Total Sample Stratified by the Number of Lesions
| Event Category | Total Sample (n=756), Patients/Events | ≥3 Lesions (n=173), Patients/Events | 2 Lesions (n=197), Patients/Events | 1 Lesion (n=386), Patients/Events |
|---|---|---|---|---|
| Major amputation, % | 5/8 | 2/3 | 1/2 | 2/3 |
| Unstable angina, % | 34/36 | 8/8 | 9/11 | 17/17 |
| Myocardial infarction, % | 33/37 | 14/14 | 4/5 | 15/18 |
| Heart failure, % | 22/28 | 6/10 | 7/7 | 9/11 |
| Cerebrovascular accident, % | 22/23 | 7/7 | 7/7 | 8/9 |
| Death, % | 87/87 | 33/33 | 18/18 | 36/36 |
Time‐to‐First‐Event Analysis
Figure 1 presents the cumulative incidence over time for experiencing a first adverse event, illustrating that the cumulative incidence was higher for patients presenting with ≥3 lesions (log‐rank test P<0.0001). Results from the time‐to‐first‐event Cox regression analysis indicated that patients presenting with ≥3 lesions were more likely to experience a first adverse event during 3.2‐year follow‐up compared with those presenting with 1 lesion in the unadjusted model (unadjusted HR 2.05, 95% CI 1.43–2.93, P≤0.0001). No increased risk of experiencing a first adverse event was observed among patients presenting with 2 versus 1 lesion (unadjusted HR 0.93, 95% CI 0.62–1.42, P=0.75).
Figure 1.
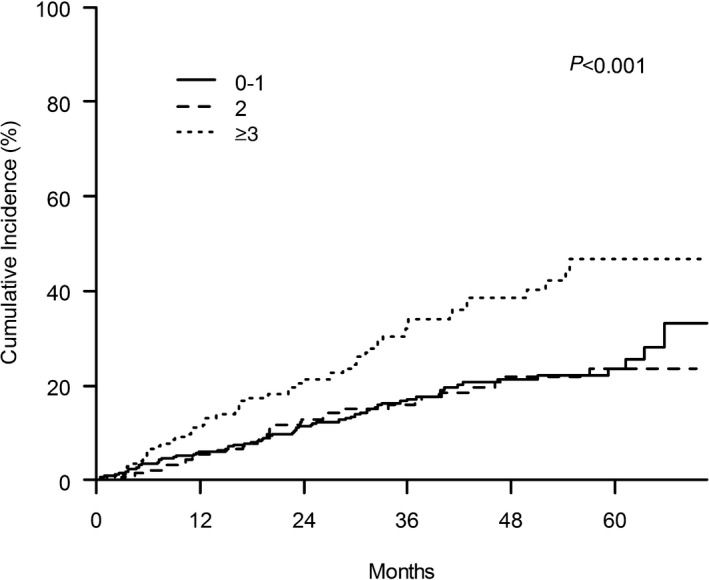
The cumulative incidence of a first adverse event by number of lesions during median follow‐up of 3.2 years. The comparison of ≥3 lesions vs 0 to 1 lesion (reference category) was statistically significant at the P<0.001 level.
Results from the multivariable time‐to‐first‐event analysis are listed in Table 3. The presence of ≥3 lesions (HR 1.60, 95% CI 1.08–2.38, P=0.020) remained an independent predictor of experiencing an adverse event. Other significant covariates included age (HR per +10 years 1.32, 95% CI 1.08–1.62, P=0.006) and chronic obstructive pulmonary disease (HR 2.11, 95% CI 1.46–3.06, P≤0.001). The c‐index for the multivariable model was 0.69.
Table 3.
The Association Between the Number of Lesions and 3.2‐Year First Adverse Event Risk
| Hazard Ratio | 95% CI | P Value | |
|---|---|---|---|
| Number of lesions | |||
| 2 vs 1 | 0.85 | 0.55–1.31 | 0.46 |
| ≥3 vs 1 | 1.60* | 1.08–2.38 | 0.020 |
| Resting ankle‐brachial index (per +10%) | 0.93 | 0.84–1.04 | 0.19 |
| Age (per +10 years) | 1.32* | 1.08–1.62 | 0.006 |
| Female | 1.05 | 0.73.1.50 | 0.81 |
| Body mass index | 1.01 | 0.97–1.04 | 0.79 |
| Prior angina | 1.49 | 0.95–2.33 | 0.08 |
| Prior myocardial infarction | 1.52 | 1.00–2.31 | 0.05 |
| Heart failure | 1.46 | 0.81–2.62 | 0.21 |
| Prior coronary artery bypass grafting | 0.84 | 0.50–1.40 | 0.49 |
| Prior percutaneous coronary intervention | 1.32 | 0.78–2.21 | 0.30 |
| Prior stroke | 1.20 | 0.66–2.20 | 0.55 |
| Prior transient ischemic attack | 0.82 | 0.46–1.47 | 0.50 |
| Chronic obstructive pulmonary disease | 2.11 | 1.46– 3.06 | <0.001 |
| Hypertension | 1.16 | 0.79–1.68 | 0.45 |
| Dyslipidemia | 1.21 | 0.83–1.75 | 0.32 |
| Diabetes mellitus | 1.11 | 0.75–1.63 | 0.61 |
| Renal dysfunction | 1.03 | 0.62–1.71 | 0.91 |
| Smoking | 1.35 | 0.94–1.94 | 0.11 |
| Total cholesterol, mg/dL | 1.00 | 0.99–1.00 | 0.19 |
| High‐density lipoprotein cholesterol, mg/dL | 1.00 | 0.99–1.02 | 0.81 |
| Systolic blood pressure, mm Hg | 1.00 | 0.99–1.01 | 0.78 |
| Proximal lesion | 0.98 | 0.68–1.42 | 0.93 |
Sensitivity Analyses
A total of 41 patients (5%) experienced >1 adverse event over time. Sensitivity analyses were performed to calculate the cumulative 3.2‐year risk of experiencing multiple adverse events by the number of lesions (≥3 or 2 versus 1 lesion [reference]) using an unadjusted and multivariable adjusted Cox‐based intensity‐elapsed time model. The mean cumulative incidence of multiple adverse events by the number of lesions was significantly higher for patients with ≥3 lesions (log‐rank test P=0.0001) (Figure S2). Apart from the risk of experiencing a first adverse event, having ≥3 lesions (HR 1.68, 95% CI 1.20–2.36, P=0.003) was also associated with an increased cumulative risk of experiencing >1 adverse event during 3.2 years of follow‐up. Other relevant indicators of an increased cumulative risk were age, prior MI, chronic obstructive pulmonary disease, heart failure, and smoking (Table S1 shows full model results).
Event‐Specific Analyses
Results from the multivariate Cox regression analysis of time to first event, stratified by event type, demonstrated that prior MI (HR 2.65, 95% CI 1.26–5.55, P=0.018) and death (HR 2.50, 95% CI 1.53–4.08, P=0.002) were the events more likely to occur in patients presenting with ≥3 lesions compared with those having 1 lesion (Figures 2 and 3); however, because of the low number of individual event types, the interaction between number of lesions and event type was not significant (P=0.62). Results from the secondary analysis that evaluated the association between the number of arterial lesions and major adverse cardiac events indicated that patients having a higher number of arterial lesions had higher cumulative incidence of major adverse cardiac events compared with those having fewer arterial lesions (Figure 4).
Figure 2.
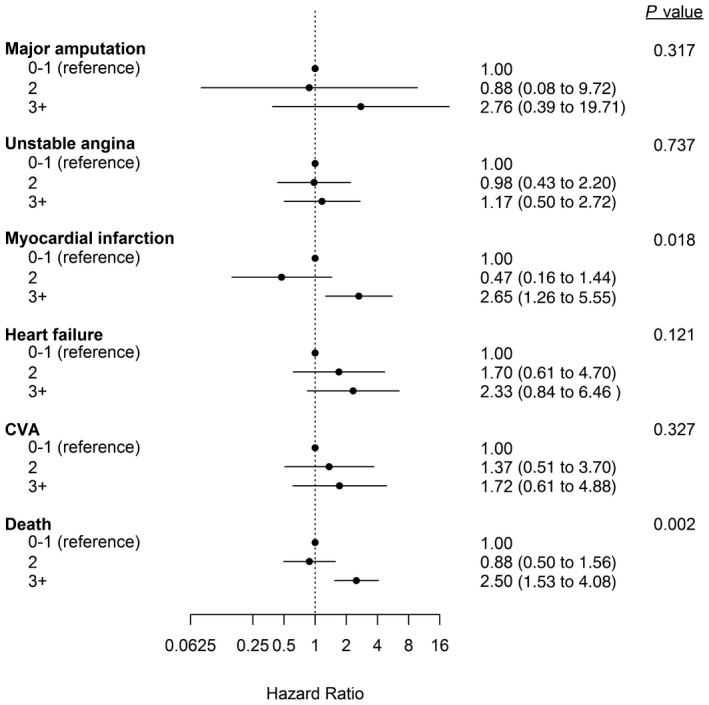
The association between number of lesions and first adverse event risk, stratified by event type. The hazard ratios and 95% CIs are depicted for lower extremity amputation, unstable angina, myocardial infarction, heart failure, stroke, and mortality. The reference group for the comparisons was the group of patients having nonsignificant lesions or 1 significant lesion (0–1 lesion). Overall P values for each comparison are provided. CVA indicates cerebrovascular accident.
Figure 3.
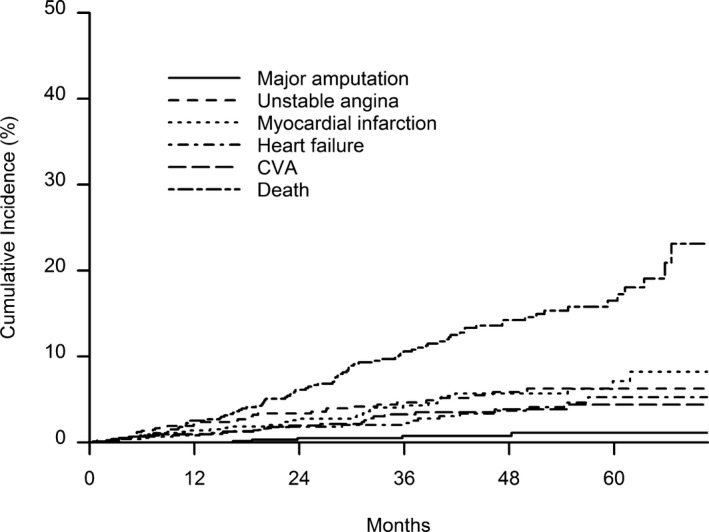
The cumulative incidence of experiencing multiple adverse events in patients stratified by event type (lower extremity amputation, unstable angina, myocardial infarction, heart failure, stroke, and mortality) during median follow‐up of 3.2 years. CVA indicates cerebrovascular accident.
Figure 4.
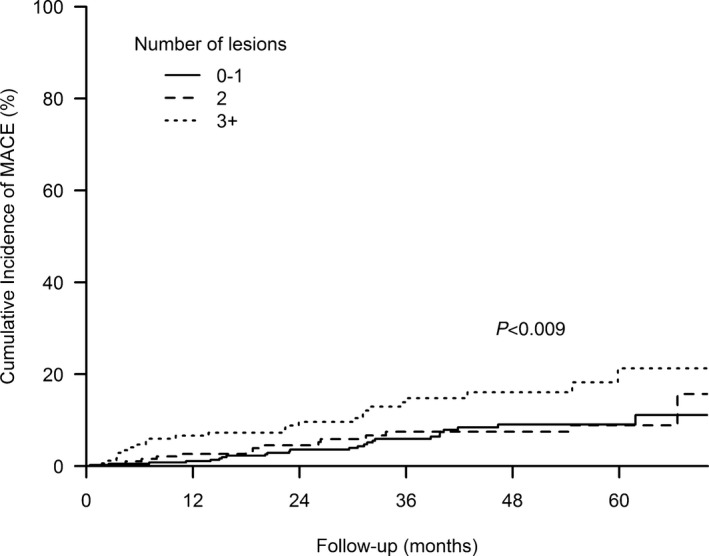
The association between the number of lesions and cumulative incidence of major adverse cardiac events (MACE) during median follow‐up of 3.2 years. Multiple MACE occurring at any time in patients are taken into account. The reference group for the comparisons was the group of patients having nonsignificant lesions or 1 significant lesion (0 to 1 lesion). The overall P value for the comparisons was P<0.009.
Discussion
This study in patients with new diagnosis of PAD (Rutherford grade I; patients with mild, moderate, and severe claudication) provides further insight into strategies that can potentially help risk‐stratify these patients based on a simple comparison by the number of lower extremity arterial lesions identified at presentation. In addition, this study is the first, of which we are aware, to estimate PAD patient risks of experiencing multiple adverse events over time, using novel multiple‐event modeling techniques. In a vascular specialty setting, we found that half of our patients presented with 1 lesion, whereas a quarter had ≥3 lesions on diagnosis. At least 1 adverse event was observed in a quarter of the population, and only a minority (5%) experienced ≥2 events during the 3‐year study follow‐up. Having more lower extremity lesions (≥3) was not only predictive of an increased risk of experiencing a first adverse event, as assessed by a traditional time‐to‐first‐event Cox regression model, but also was associated with experiencing multiple events over time compared with patients having an isolated lesion, as modeled with a Cox‐based intensity‐elapsed time model. In addition, the results remained consistent throughout our analyses despite adjusting for known traditional PAD risk factors.
Although it seems obvious to assume that patients with multiple lower extremity arterial lesions have poorer prognosis compared with those having a single lesion, prior studies demonstrated only that PAD patients with concomitant coronary or carotid disease (ie, having several arterial beds affected) have increased risks of experiencing adverse events compared with those having a single arterial bed affected.3, 5, 16 These studies were unable to perform comparisons based on the number of lesions within 1 arterial bed (lower extremity arteries) for patients with PAD.3, 5, 16 Only 1 small study of 224 younger nondiabetic patients recruited in 1985 demonstrated that patients with multiple lower extremity arterial lesions had lower 6‐year survival rates compared with patients having a single lesion.9 Because of its many limitations, including a nondiabetic population that is not necessarily representative of the PAD population, lack of visualization of arterial segments, and limited sample size, this older study did not draw any firm conclusions about the prognostic association of the number of lesions in lower extremity PAD with outcomes. Other research supporting our findings comes from the BASIL trial data, in which the number of ankle‐pressure measurements that could be detected (dorsalis pedis, posterior tibial, and perforating peroneal; range 0–3) was included in a prediction model to predict 2‐year survival in critical limb ischemia patients—a more advanced expression of PAD. The number of detectable ankle‐pressure measurements was associated with 2‐year survival in a dose‐response–related way in which the highest survival rates were noted among patients with 3 pressures and the lowest survival rates were seen among patients without detectible pressures.10 In the current study, we had a unique chance to examine the association between arterial lesions and prognosis in a larger cohort of patients with earlier stages of PAD in which adverse risk factors were proportionally represented in accordance with their prevalence in a real‐world clinical setting.3, 5 Lesions were documented with modern duplex ultrasound techniques on diagnosis. Detailed and complete follow‐up information was available for first and multiple events. Our study maximized the use of information on multiple events into state‐of‐the‐art analytic models and has the potential to significantly advance our understanding of different subpopulations of patients with PAD.
Our results suggest that the risk of adverse events may increase along with the number of lower extremity lesions. This raises the question whether it is possible that the manifestation of atherosclerosis may present differentially among individual patients’ arteries. More aggressive expression of atherosclerosis has been found in patients with distal versus aortoiliac disease and in patients in whom higher inflammation markers can be found.17, 18, 19 These studies suggested which concomitant factors could be associated with a more aggressive underlying atherosclerotic process but were unable to document whether this could be linked to the number of lower extremity lesions and patient outcomes.17, 18 Consequently, future work needs to verify whether having more lower extremity lesions is associated with a more aggressive underlying atherosclerotic process expressed by higher inflammation markers or undergoing multiple lower extremity revascularizations to better characterize PAD subpopulations that are at increased risk of an adverse prognosis.
Apart from investigating the potential pathophysiological underpinnings for the adverse prognosis associated with having more arterial lesions, our results indicate that information on the number of lesions—as derived from various radiological imaging instruments—adds to the prognostic information derived from traditional PAD risk factors that we adjusted for in our models. It may also offer some predictive information beyond the established risk stratification based on patient ABI20; we found in our preliminary analyses that the number of lesions remained predictive of patient prognosis after adjusting for ABI. Nevertheless, further validation work in this area is needed. Future studies need to evaluate whether implementing quality‐of‐care protocols specifically directed at the subgroups of patients presenting with multiple lesions (eg, closer patient monitoring in combination with aggressive adverse risk management and more proactive screening for coronary or cerebrovascular disease) may be able to curb the adverse risk observed in patients with PAD presenting with multiple lesions. Assessing patients’ true cumulative risk of having multiple adverse events over time is becoming more standard within cardiovascular research21, 22 but rarely has been applied for research investigating PAD populations. Future efforts should focus on ways in which we can more accurately predict patients’ overall risk of experiencing multiple future events following a diagnosis of PAD, using state‐of‐the‐art analyses.15 Although we did not observe a great number of multiple adverse events during the limited 3‐year study follow‐up, these techniques seem even more relevant when investigating longer term outcomes and the need for recurrent procedures in this vulnerable patient group.
Our results should be interpreted in the context of the following potential limitations. Not all arterial segments were visualized because duplex ultrasound testing was guided by the vascular surgeon's clinical evaluation, including history taking, ABI assessment, and physical examination, thereby checking the presence of arterial pulses; however, chances that lesions were missed are minimal because duplex ultrasound testing was performed using a systematic approach (ie, segments were additionally visualized if a lesion was expected elsewhere due to flow disturbances). Information on individual lesion complexity or length of the stenosis was not accounted for in our analyses, and future research remains to be done on whether this granular anatomical lesion information may further improve the risk stratification of patients with PAD. Although duplex ultrasonography has been shown to have a median sensitivity of 88% and a specificity of 96% to detect a stenosis of ≥50% or an occlusion when imaging the whole leg versus the standard of contrast angiography, we acknowledge the potential for misclassification of arterial lesions.14 To maximize our power, we explored patient risk of adverse events by use of a composite end point, but we also explored patient risk by event type, using a multivariate analysis, and further ran sensitivity analyses by restricting our end point to fatal or nonfatal MI or stroke; for all of these analyses, the association between the number of arterial lesions and adverse prognosis persisted. In addition, because patients were recruited from 2 vascular surgery outpatient clinics and patients with critical limb ischemia were excluded, our results may not necessarily be generalizable to the whole spectrum of PAD patients and to patients with PAD seen in other settings. Future formal validation work is needed in similar, larger cohorts to establish firm clinical management guidelines based on the discriminatory ability of the number of lesions to better risk‐stratify patients with PAD. Furthermore, we did not adjust for treatments that patients received after their baseline visit. Finally, although we adjusted for clinically important factors, we cannot rule out the possibility of residual confounding due to the observational nature of our study.
Conclusions
This study demonstrated that PAD patients presenting with more lower extremity arterial lesions on diagnosis were at increased risk of experiencing a first and multiple adverse events over time compared with those having only 1 lesion. Comparing PAD outcomes as a function of patients’ number of lower extremity lesions may offer a new paradigm that may serve clinicians to better determine patient risk for an adverse prognosis at initial PAD diagnosis. Our findings also may open up new possibilities to develop and evaluate care innovations directed specifically at patients who present with ≥3 lesions within their lower extremity arteries, possibly representing a phenotype that is associated with a more aggressive form of atherosclerotic disease.
Data Access and Responsibility
Drs Smolderen and van Zitteren had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Sources of Funding
Dr Smolderen was supported by the Patient‐Centered Outcomes Research Institute [CE‐1304‐6677].
Disclosures
None.
Supporting information
Figure S1. Flow chart of the study population.
Figure S2. The mean cumulative incidence for experiencing multiple adverse events by the number of lesions during a median follow‐up of 3.2‐years. The estimated cumulative incidence curves for 0 to 1 and 2 lesions were virtually identical; therefore, they are labeled as 1 curve 0 to 2 lesions. The P value for the comparison of 0 to 2 lesions vs ≥3 lesions was P=0.001.
Table S1. The Association Between the Number of Lesions and 3.2‐Year Multiple Adverse Events Risk
(J Am Heart Assoc. 2015;4:e001823 doi: 10.1161/JAHA.115.001823)
Accompanying Figures S1, S2 and Table S1 are available at http://jaha.ahajournals.org/content/4/10/e001823/suppl/DC1
Part of these data (abstract) were presented at the Quality of Care and Outcome Research (QCOR) in Cardiovascular Disease and Stroke Scientific Sessions of the American Heart Association, Washington DC, USA, May 12 to 14, 2011.
References
- 1. McDermott MM, Guralnik JM, Tian L, Ferrucci L, Liu K, Liao Y, Criqui MH. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Cardiol. 2007;50:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McDermott MM, Liu K, Ferrucci L, Tian L, Guralnik JM, Liao Y, Criqui MH. Decline in functional performance predicts later increased mobility loss and mortality in peripheral arterial disease. J Am Coll Cardiol. 2011;57:962–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bhatt DL, Eagle KA, Ohman EM, Hirsch AT, Goto S, Mahoney EM, Wilson PW, Alberts MJ, D'Agostino R, Liau CS, Mas JL, Rother J, Smith SC Jr, Salette G, Contant CF, Massaro JM, Steg PG. Comparative determinants of 4‐year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA. 2010;304:1350–1357. [DOI] [PubMed] [Google Scholar]
- 4. Saw J, Bhatt DL, Moliterno DJ, Brener SJ, Steinhubl SR, Lincoff AM, Tcheng JE, Harrington RA, Simoons M, Hu T, Sheikh MA, Kereiakes DJ, Topol EJ. The influence of peripheral arterial disease on outcomes: a pooled analysis of mortality in eight large randomized percutaneous coronary intervention trials. J Am Coll Cardiol. 2006;48:1567–1572. [DOI] [PubMed] [Google Scholar]
- 5. Steg PG, Bhatt DL, Wilson PW, D'Agostino R Sr, Ohman EM, Rother J, Liau CS, Hirsch AT, Mas JL, Ikeda Y, Pencina MJ, Goto S. One‐year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–1206. [DOI] [PubMed] [Google Scholar]
- 6. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM Jr, White CJ, White J, White RA, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; Transatlantic Inter‐Society Consensus; and Vascular Disease Foundation. Circulation. 2006;113:e463–e654. [DOI] [PubMed] [Google Scholar]
- 7. Olin JW, Allie DE, Belkin M, Bonow RO, Casey DE Jr, Creager MA, Gerber TC, Hirsch AT, Jaff MR, Kaufman JA, Lewis CA, Martin ET, Martin LG, Sheehan P, Stewart KJ, Treat‐Jacobson D, White CJ, Zheng ZJ, Masoudi FA. ACCF/AHA/ACR/SCAI/SIR/SVM/SVN/SVS 2010 performance measures for adults with peripheral artery disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures, the American College of Radiology, the Society for Cardiac Angiography and Interventions, the Society for Interventional Radiology, the Society for Vascular Medicine, the Society for Vascular Nursing, and the Society for Vascular Surgery (Writing Committee to Develop Clinical Performance Measures for Peripheral Artery Disease). Circulation. 2010;122:2583–2618. [DOI] [PubMed] [Google Scholar]
- 8. Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, Golzarian J, Gornik HL, Halperin JL, Jaff MR, Moneta GL, Olin JW, Stanley JC, White CJ, White JV, Zierler RE. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients with Peripheral Artery Disease (updating the 2005 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58:2020–2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jonason T, Ringqvist I. Mortality and morbidity in patients with intermittent claudication in relation to the location of the occlusive atherosclerosis in the leg. Angiology. 1985;36:310–314. [DOI] [PubMed] [Google Scholar]
- 10. Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FG, Gillespie I, Ruckley CV, Raab GM, Participants BT. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: a survival prediction model to facilitate clinical decision making. J Vasc Surg. 2010;51:52S–68S. [DOI] [PubMed] [Google Scholar]
- 11. van Zitteren M, Vriens PW, Heyligers JM, Burger DH, Nooren MJ, de Fijter WM, Denollet J, Smolderen KG. Self‐reported symptoms on questionnaires and anatomic lesions on duplex ultrasound examinations in patients with peripheral arterial disease. J Vasc Surg. 2012;55:1025–1034. [DOI] [PubMed] [Google Scholar]
- 12. Diagnostics and treatment of arterial disease in the lower extremities. ISBN 90‐8523‐072‐1. 2005.
- 13. Leiner T, Kessels AG, Nelemans PJ, Vasbinder GB, de Haan MW, Kitslaar PE, Ho KY, Tordoir JH, van Engelshoven JM. Peripheral arterial disease: comparison of color duplex US and contrast‐enhanced MR angiography for diagnosis. Radiology. 2005;235:699–708. [DOI] [PubMed] [Google Scholar]
- 14. Collins R, Burch J, Cranny G, Aguiar‐Ibanez R, Craig D, Wright K, Berry E, Gough M, Kleijnen J, Westwood M. Duplex ultrasonography, magnetic resonance angiography, and computed tomography angiography for diagnosis and assessment of symptomatic, lower limb peripheral arterial disease: systematic review. BMJ. 2007;334:1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kelly PJ, Lim LL. Survival analysis for recurrent event data: an application to childhood infectious diseases. Stat Med. 2000;19:13–33. [DOI] [PubMed] [Google Scholar]
- 16. Mahoney EM, Wang K, Keo HH, Duval S, Smolderen KG, Cohen DJ, Steg G, Bhatt DL, Hirsch AT. Vascular hospitalization rates and costs in patients with peripheral artery disease in the United States. Circ Cardiovasc Qual Outcomes. 2010;3:642–651. [DOI] [PubMed] [Google Scholar]
- 17. Aboyans V, Criqui MH, Denenberg JO, Knoke JD, Ridker PM, Fronek A. Risk factors for progression of peripheral arterial disease in large and small vessels. Circulation. 2006;113:2623–2629. [DOI] [PubMed] [Google Scholar]
- 18. Aboyans V, Desormais I, Lacroix P, Salazar J, Criqui MH, Laskar M. The general prognosis of patients with peripheral arterial disease differs according to the disease localization. J Am Coll Cardiol. 2010;55:898–903. [DOI] [PubMed] [Google Scholar]
- 19. Chen Q, Smith CY, Bailey KR, Wennberg PW, Kullo IJ. Disease location is associated with survival in patients with peripheral arterial disease. J Am Heart Assoc. 2013;2:e000304 doi: 10.1161/JAHA.113.000304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G, Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton‐Tyrrell K, Lee AJ, Price JF, d'Agostino RB, Murabito JM, Norman PE, Jamrozik K, Curb JD, Masaki KH, Rodriguez BL, Dekker JM, Bouter LM, Heine RJ, Nijpels G, Stehouwer CD, Ferrucci L, McDermott MM, Stoffers HE, Hooi JD, Knottnerus JA, Ogren M, Hedblad B, Witteman JC, Breteler MM, Hunink MG, Hofman A, Criqui MH, Langer RD, Fronek A, Hiatt WR, Hamman R, Resnick HE, Guralnik J. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta‐analysis. JAMA. 2008;300:197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Borer JS, Bohm M, Ford I, Komajda M, Tavazzi L, Sendon JL, Alings M, Lopez‐de‐Sa E, Swedberg K. Effect of ivabradine on recurrent hospitalization for worsening heart failure in patients with chronic systolic heart failure: the SHIFT study. Eur Heart J. 2012;33:2813–2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Anker SD, McMurray JJ. Time to move on from ‘time‐to‐first’: should all events be included in the analysis of clinical trials? Eur Heart J. 2012;33:2764–2765. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Flow chart of the study population.
Figure S2. The mean cumulative incidence for experiencing multiple adverse events by the number of lesions during a median follow‐up of 3.2‐years. The estimated cumulative incidence curves for 0 to 1 and 2 lesions were virtually identical; therefore, they are labeled as 1 curve 0 to 2 lesions. The P value for the comparison of 0 to 2 lesions vs ≥3 lesions was P=0.001.
Table S1. The Association Between the Number of Lesions and 3.2‐Year Multiple Adverse Events Risk


