Abstract
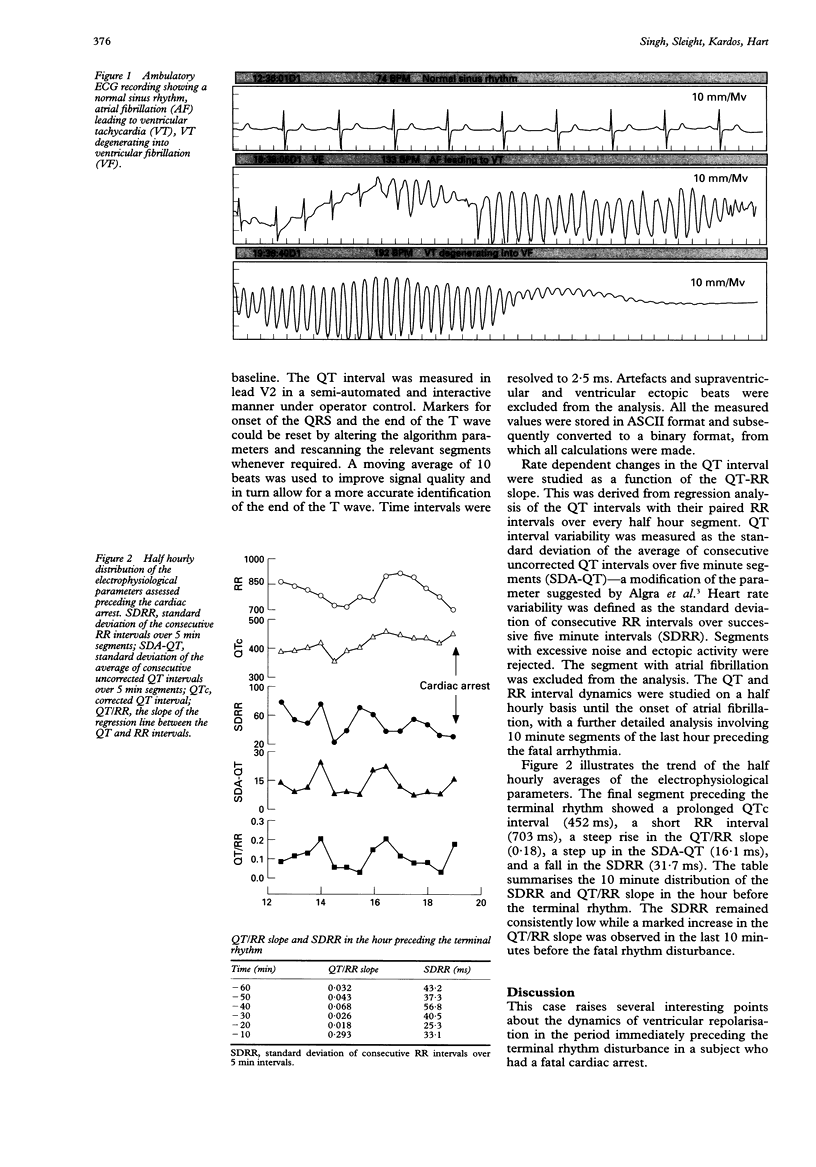
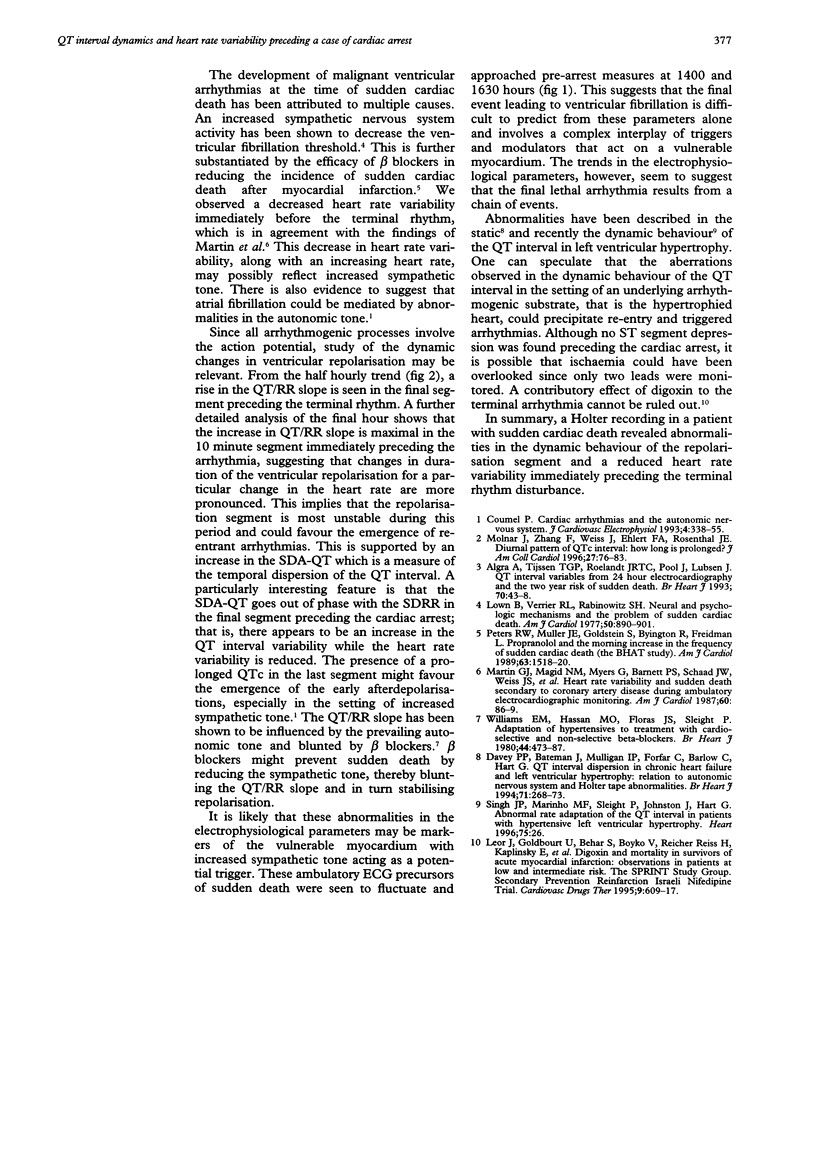
A 71 year old man with hypertensive heart disease and chronic renal failure was wearing a Holter monitor when he had a cardiac arrest. He had ventricular fibrillation (VF) and died despite prompt resuscitation. In the 15 minutes preceding the VF there was a sudden increase in heart rate, followed by a brief period of atrial fibrillation leading to ventricular tachycardia, which in turn rapidly degenerated into VF. The QT interval and heart rate variability were studied half hourly over the seven hours preceding the cardiac arrest, using a computerised Holter system. A further detailed analysis was performed over the final hour before the cardiac arrest. An abrupt increase in the steepness of the QT/RR slope, a prolonged QTc, and a reduction in the heart rate variability were observed in the interval that immediately preceded the onset of the terminal rhythm disturbance.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Algra A., Tijssen J. G., Roelandt J. R., Pool J., Lubsen J. QT interval variables from 24 hour electrocardiography and the two year risk of sudden death. Br Heart J. 1993 Jul;70(1):43–48. doi: 10.1136/hrt.70.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coumel P. Cardiac arrhythmias and the autonomic nervous system. J Cardiovasc Electrophysiol. 1993 Jun;4(3):338–355. doi: 10.1111/j.1540-8167.1993.tb01235.x. [DOI] [PubMed] [Google Scholar]
- Davey P. P., Bateman J., Mulligan I. P., Forfar C., Barlow C., Hart G. QT interval dispersion in chronic heart failure and left ventricular hypertrophy: relation to autonomic nervous system and Holter tape abnormalities. Br Heart J. 1994 Mar;71(3):268–273. doi: 10.1136/hrt.71.3.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leor J., Goldbourt U., Behar S., Boyko V., Reicher-Reiss H., Kaplinsky E., Rabinowitz B. Digoxin and mortality in survivors of acute myocardial infarction: observations in patients at low and intermediate risk. The SPRINT Study Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. Cardiovasc Drugs Ther. 1995 Aug;9(4):609–617. doi: 10.1007/BF00878094. [DOI] [PubMed] [Google Scholar]
- Lown B., Verrier R. L., Rabinowitz S. H. Neural and psychologic mechanisms and the problem of sudden cardiac death. Am J Cardiol. 1977 May 26;39(6):890–902. doi: 10.1016/s0002-9149(77)80044-1. [DOI] [PubMed] [Google Scholar]
- Martin G. J., Magid N. M., Myers G., Barnett P. S., Schaad J. W., Weiss J. S., Lesch M., Singer D. H. Heart rate variability and sudden death secondary to coronary artery disease during ambulatory electrocardiographic monitoring. Am J Cardiol. 1987 Jul 1;60(1):86–89. doi: 10.1016/0002-9149(87)90990-8. [DOI] [PubMed] [Google Scholar]
- Molnar J., Zhang F., Weiss J., Ehlert F. A., Rosenthal J. E. Diurnal pattern of QTc interval: how long is prolonged? Possible relation to circadian triggers of cardiovascular events. J Am Coll Cardiol. 1996 Jan;27(1):76–83. doi: 10.1016/0735-1097(95)00426-2. [DOI] [PubMed] [Google Scholar]
- Peters R. W., Muller J. E., Goldstein S., Byington R., Friedman L. M. Propranolol and the morning increase in the frequency of sudden cardiac death (BHAT Study). Am J Cardiol. 1989 Jun 15;63(20):1518–1520. doi: 10.1016/0002-9149(89)90019-2. [DOI] [PubMed] [Google Scholar]
- Williams E. M., Hassan M. O., Floras J. S., Sleight P., Jones J. V. Adaptation of hypertensives to treatment with cardioselective and non-selective beta-blockers. Absence of correlation between bradycardia and blood pressure control, and reduction in slope of the QT/RR relation. Br Heart J. 1980 Nov;44(5):473–487. doi: 10.1136/hrt.44.5.473. [DOI] [PMC free article] [PubMed] [Google Scholar]


