Abstract
Background
Although substantial effort has been devoted to reducing readmissions among heart failure (HF) patients, little is known about factors identified by patients and caregivers that may contribute to readmissions. The goal of this study was to compare the perspectives of HF patients, their caregivers, and their care team on HF management and hospital admissions. Understanding these perspectives may lead to better strategies for improving care during the post-hospital transition and reducing preventable readmissions.
Methods and Results
We performed freelisting—an anthropological technique in which participants list items in response to a question—with hospitalized HF patients (n=58), their caregivers (n=32), and clinicians (n=67). We asked about home HF management tasks, difficulties in managing HF, and perceived reasons for hospital admission. Results were analyzed in Anthropac©. Salience indices (measures of the most important words for defining the domain of interest) were calculated. Patients and clinicians described similar home HF management tasks, while caregivers described tasks related to activities of daily living. Clinicians cited socio-economic factors as challenges to HF management, while patients and caregivers cited limited functional status and daily activities. When asked about reasons for hospitalization, patients and caregivers listed distressing symptoms and illness, while clinicians viewed patient behaviors as primarily responsible for admission.
Conclusions
These findings highlight that, although some similarities exist, there are important differences among patients, caregivers, and clinicians in how they perceive the challenges of HF management and reasons for readmission. Understanding these differences may be critical to developing strategies to reduce readmissions.
Keywords: heart failure, readmissions, patient-centered care, transitional care, qualitative research
Introduction
Heart failure (HF) has an enormous impact on health and the health care system in America. It afflicts approximately 5.1 million Americans and is the primary diagnosis in more than one million admissions yearly.1 In 2012, the estimated total cost of HF was $30.7 billion, with projected growth to $69.7 billion by 2030.1 Readmissions also contribute substantially to the high costs of HF care. The estimated cost of 30-day readmissions is approximately $17.4 billion.2 Among Medicare patients who are admitted for various conditions, HF patients have the highest 30-day readmission rate at 27%.2
In light of the high prevalence and costs of HF, substantial resources and research have been devoted to improving outpatient HF care and reducing hospitalizations. In particular, efforts directed toward reducing readmissions by improving transitional care have accelerated due to financial penalties enacted by the Centers for Medicare and Medicaid Services (CMS) for institutions with higher readmission rates.3,4
Several interventions have been shown to reduce HF readmissions.5–7 However, a better understanding of the perspectives among patients, caregivers, and clinicians and the etiologies of hospital admissions may inform improvements in interventions. Although numerous qualitative and quantitative studies have examined barriers to HF care from the patient and caregiver perspectives, relatively few studies have used qualitative methods to triangulate perspectives of patients, caregivers, and clinicians on HF management and factors for hospital admission.8–13 Comparing perspectives becomes crucial because the ways that patients and their families experience illness is often very different from the ways that their health care providers understand that experience.14,15 Therefore, we hypothesized that qualitative interviews would better inform our understanding of HF management after hospital discharge and across the continuum of care. Qualitative interviews provide a medium through which patients and caregivers can describe their experiences from their own perspective, unconstrained by expert points of view. These voices become particularly important after hospitalization during the transitional period, which appears to be a time of increased risk for various adverse health events.4,16 Identifying areas of concordance and discordance in perspectives may be helpful in improving communication among patients, caregivers, and clinicians. In addition, this knowledge could be used to inform the design of HF interventions by ensuring that barriers identified by each stakeholder are addressed.
To evaluate similarities and discrepancies among the patient- and caregiver-experience and perceptions of experienced care teams, we used freelisting, a qualitative research strategy that elicits participants’ ideas about concepts that belong in a particular domain.17–19 Using freelisting, wherein participants generate a list of words in response to a prompt, we sought to characterize the patient and caregiver experience of managing HF at home by interviewing admitted patients and their caregivers. We also interviewed physicians, registered nurses (RNs), nurse practitioners (NPs), physician assistants (PAs), social workers, and care coordinators with expertise in managing HF patients.
Methods
Study Overview
We designed a qualitative study using a purposive sample20 of HF patients, their caregivers, and clinicians. The study sites were the Hospital of the University of Pennsylvania (a large, urban academic health center) and Penn Presbyterian Medical Center (an urban, teaching, community hospital affiliated with the University of Pennsylvania Health System). The Institutional Review Board of the University of Pennsylvania approved this study, and all participants provided informed consent.
Patient and Caregiver Samples
Patients were eligible for this study if they were admitted to a cardiology or general medicine service at either site with a primary diagnosis related to HF. The exclusion criteria were: 1) current long-term facility residents or prisoners; 2) non-English speaking; 3) unable or unwilling to provide consent; 4) severe cognitive impairment; and 5) patients with or scheduled for left ventricular assist device, cardiac transplantation, or home inotrope therapy. Heart failure patients were identified by a combination of an electronic health record query that generated a daily census of patients admitted with a HF or HF-related diagnosis, chart review by research assistants, and direct contact with floor nurses. Cognitive impairment was screened by chart review, and patients with documented cognitive impairment were excluded. Caregivers were identified by the patient and asked if they were able to participate. We purposively sampled to achieve a mix of patients from cardiology and medicine floors and patients with and without recent hospital admission. Patients were consented and interviewed in-person. Caregivers were contacted, consented, and interviewed separately either via telephone or in-person during a hospital visit.
Clinician Sample
Clinician participants were those working on interdisciplinary teams caring for HF patients at the two hospitals. These included physicians, NPs, RNs, PAs, social workers, and care coordinators (nurses who provide case management and discharge planning services). Multiple mechanisms were used to identify clinicians. We obtained lists of all of the general cardiology, HF, and hospital medicine interdisciplinary teams. We contacted these individuals either via email or in person, and then scheduled an interview time, either in person or over the phone. We identified inpatient registered nurses while on the inpatient floors with admitted HF patients. We purposively sampled to create a mix of clinicians from different training disciplines.
Data Collection
The research team developed freelist interview guides based on their expertise, review of the literature, and input from a patient with HF. The guides consisted of an initial description of the study, instructions for freelisting, and a warm-up exercise. To enhance consistency across interviews, the guide included a written script for the interviewer. The participants were asked to generate a list of words or short phrases in response to three separate questions as shown in Supplemental Material, Table S1. The questions were designed to identify perceptions of: 1) how patients manage their HF at home; 2) barriers to effective management; and 3) reasons for hospitalization.
Interviews were conducted from October 2012 to April 2013. All interviews were performed by either a research assistant or one of the study authors (FSA, BP) and typically lasted thirty minutes. All interviewers underwent training in conducting freelisting interviews by a medical anthropologist (FKB). The interviewers met regularly with the medical anthropologist and the project manager (MA) to address any questions about or concerns with the interview process. The interviewer audio recorded all responses by participants, and the interviews were transcribed for analysis. The interviewers collected additional socio-demographic and clinical variables either directly from the participant or from chart review.
Data Management and Analysis
Individual lists were inspected to combine synonyms and similar ideas and to standardize word forms or phrases. For example, if Participant A listed “watch my weight” and Participant B listed “weigh myself daily,” both of these would be categorized under “check weight.” The “cleaned” lists were reviewed and validated by at least three additional members of the research team, which included a patient with HF. Then the medical anthropologist and her research assistant (BP) reviewed the comments from other team members and revised the lists. The list of standardized words and phrases were then entered into Anthropac© 4.98 (Analytic Technologies, Lexington, KY). A data list was created for each of the three questions for each role (patient, caregiver, and provider) for a total of 9 data lists.
Using Anthropac, a salience index (Smith’s S) was calculated for each term using the formula S = ((Σ((L−Rj + 1))/L)/N, where L = the length of each list, Rj is the rank of item j in the list, and N = the number of lists in the sample.17,21 Saliency describes the words that are most important for defining the domain of interest among members of a group. Saliency scores are then plotted as scree plots. The graphs are inspected to select the elbow that demarcates a flattening of the slope. All words with saliency scores greater than or equal to that elbow value are retained as the list of salient terms (for example, see Supplemental Material, Figure S1).17 We have focused in this paper on the salient terms because they represent the words or phrases that most people prioritized.
Our primary analyses focused on describing salient terms for the group as a whole, and then comparing salient terms for patients, for caregivers, for clinicians, and for subgroups of clinicians. Two additional subgroup analyses were performed. First, we compared salient terms between patients with caregivers to those without caregivers. Second, we also compared responses between MDs, NPs/RNs/PAs and social workers/care coordinators because we hypothesized these groups would have different perspectives due to their training and roles in the care team. NPs and PAs were grouped with RNs because, at the participating institutions, these providers directly provide clinical care but have a different role from physicians, who oversee the overall care plan and decide on the timing of discharge. Care coordinators work directly with the social workers to coordinate post-discharge, and thus they were grouped together.
In qualitative research, sampling continues until saturation, when no new important themes arise. A freelist sample size of 17 per group is typically adequate to obtain reliable results, but we sought to obtain 20 to 25 per group in case there was heterogeneity of responses within groups.22 We tested for saturation by analyzing the freelist results when approximately 80% of the data were collected and then rerunning the analyses when the sample was complete. There were no new words or concepts that arose between the sets of results. Because we purposively sampled patients and caregivers to achieve a mix from medicine and cardiology floors and with and without recent hospital admission, our sample of patients and caregivers was greater than 25.
Results
Participants
The demographic and clinical characteristics of the 58 enrolled patients are shown in Table 1. The mean age of the patient sample was 64±19 years old with 28% of patients older than 70 years old. Males comprised 64% of the sample, and 41% of the participants were black participants. Only 10% of patients had commercial insurance, while the remaining sample had either government insurance or were uninsured. Twenty-two percent of patients had been admitted two or more times within the year prior to the admission during which enrollment occurred.
Table 1.
Patient Characteristics
| Patient Characteristics (n = 58) | |
|---|---|
| Age, years, n (%) | |
| < 31 | 0 (0) |
| 31–50 | 8 (13) |
| 51–70 | 34 (59) |
| 71+ | 16 (28) |
| Male, n (%) | 37 (64) |
| Race, n (%) | |
| White | 34 (59) |
| Black | 24 (41) |
| Ethnicity, n (%) | |
| Non-Hispanic | 55 (95) |
| Hispanic | 3 (5) |
| Identified caregiver, n (%) | 45 (78) |
| Marital status, n (%) | |
| Married | 24 (41) |
| Divorced/Separated/Widowed | 18 (31) |
| Single | 16 (28) |
| Education, n (%) | |
| Attended grade school or high school | 12 (21) |
| Completed high school | 22 (38) |
| Attended college | 10 (17) |
| Graduated College/Post-graduate education | 14 (24) |
| Insurance, n (%) | |
| Medicare/Supplemental Security Insurance | 12 (21) |
| Medicaid | 16 (28) |
| Commercial | 6 (10) |
| Medicare & Other | 22 (38) |
| None | 2 (3) |
| Employment Status, n (%) | |
| Retired | 25 (43) |
| Disabled | 21 (36) |
| Full-time employed | 7 (12) |
| Unemployed/Other | 5 (8) |
| Income, n (%) | |
| $0 – $19,999 | 16 (27) |
| $20 – $39,999 | 13 (22) |
| $40 – $49,999 | 4 (7) |
| >$50,000 | 11 (19) |
| Refused | 13 (22) |
| Not available | 1 (2) |
| Sodium, serum, mmol/L, mean ±STD | 137±4.4 |
| Creatinine, serum, mg/dL, mean ±STD | 1.9±1.8 |
| Left ventricular ejection fraction, %, mean ±STD | 41±18.6 |
| Self-Reported Health Status, n (%) | |
| Excellent | 2 (4) |
| Very Good | 6 (11) |
| Good | 15 (28) |
| Fair | 16 (30) |
| Poor | 15 (28) |
We enrolled 32 caregivers, 66% of whom were female (Table 2). Slightly more than half of the caregivers were spouses of the patient, and the second-largest group of caregivers was patients’ adult children (31%). There was a broad range of educational background, and 47% were employed full-time or part-time. The median number of hours of care was 35 per week.
Table 2.
Caregiver Characteristics
| Caregiver Characteristics (n=32) | |
|---|---|
| Age, years, mean (min-max) | 54 (27–80) |
| Male, n (%) | 11 (34) |
| Race, n (%) | |
| White | 18 (56) |
| Black | 14 (44) |
| Ethnicity, n (%) | |
| Non-Hispanic | 32 (100) |
| Hispanic | 0 (0) |
| Education, n (%) | |
| Attended grade school or high school | 3 (9) |
| Completed high school | 10 (31) |
| Attended college | 7 (22) |
| Graduated College/Post-graduate education | 12 (37) |
| Employment status, n (%) | |
| Full-time Employed | 12 (38) |
| Part-time Employed | 3 (9) |
| Unemployed/retired | 15 (47) |
| Other (disability) | 2 (6) |
| Relationship to patient | |
| Spouse | 17 (53) |
| Child | 10 (31) |
| Friend/sibling/parent/other | 5 (15) |
| Hours per week of caregiving, n (%) | |
| 0 to 10 | 5 (16) |
| 11 to 20 | 5 (16) |
| 21 to 30 | 3 (9) |
| 31 to 40 | 6 (19) |
| Greater than 40 | 13 (41) |
| Self-Reported Health Status, n (%) | |
| Excellent | 8 (25) |
| Very Good | 6 (19) |
| Good | 9 (28) |
| Fair | 7 (22) |
| Poor | 2 (6) |
Of the 67 enrolled clinicians, there were 25 physicians; 25 RNs, NPs, and PAs; and 17 social workers and care coordinators. Sixty-three percent of the sample was female, 78% were white, and 58% had 6 or more years of experience working with HF patients (Table 3).
Table 3.
Clinician Characteristics
| Clinician Characteristics (n=67) | |
|---|---|
| Discipline, n (%) | |
| Physician | 25 (37) |
| Registered Nurse/Nurse Practitioner/Physician Assistant | 25 (37) |
| Social Worker/Care Coordinator | 17 (25) |
| Age, years, n (%) | |
| < 31 | 12 (18) |
| 31–40 | 26 (39) |
| 41–50 | 11 (16) |
| 51–60 | 11 (16) |
| > 60 | 6 (10) |
| Male, n (%) | 18 (27) |
| Race/ethnicity, n (%) | |
| White | 52 (78) |
| Black | 5 (7) |
| Asian | 10 (15) |
| Ethnicity, n (%) | |
| Non-Hispanic | 63 (94) |
| Hispanic | 4 (6) |
| Years working with HF patients, n (%) | |
| < 6 | 27 (40) |
| 6–10 | 16 (24) |
| 11–20 | 15 (22) |
| >20 | 8 (12) |
| Not available | 1 (1.5) |
Freelisting Results
For Question 1, patients and clinicians were asked: What words describe things a patient (you) does to manage your HF at home? Caregivers were asked: What words describe things you do to help (patient’s name) manage HF at home? Figure 1 presents the salient terms identified by participants. Taking medications and healthy diet were salient for all three groups. Patients and clinicians similarly identified watching sodium and checking weight, while caregivers listed tasks that defined their role in the patients’ lives, such as cooking, household chores, shopping, and transportation. Fluids and not overdoing it were salient terms for both patients and caregivers.
Figure 1.
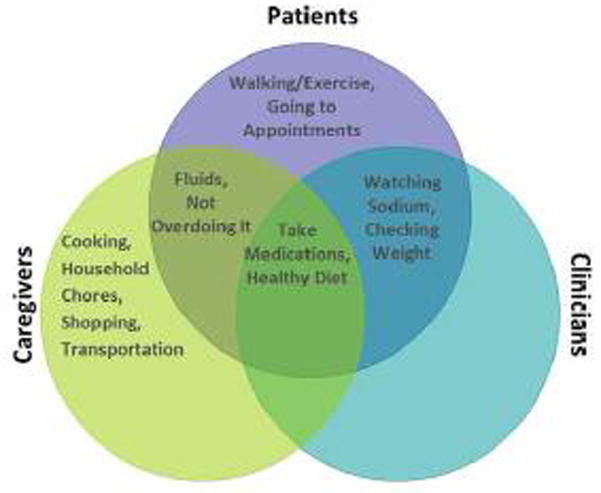
Home HF Management
For Question 2, participants were asked: What words describe things that make it difficult for a patient (you) to manage HF at home? The results varied among groups (See Figure 2). Patients and caregivers jointly identified physical limitations, activities of daily living, and diet as salient terms. Additionally, steps and exercise were unique salient terms for patients. Caregivers cited reduced independence, stress, and personal characteristics, such as “stubbornness,” “not listening,” and “laziness,” as barriers to HF management for patients. Two terms were salient for clinicians: No caregiver or social support and financial constraints. No caregiver or social support was also a salient term for caregivers.
Figure 2.
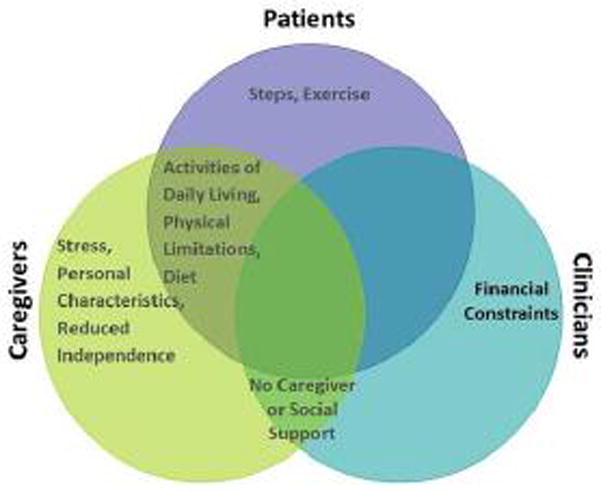
Challenges to Home HF Management
For Question 3, participants were asked: What words describe the things that led to the patient’s (your) hospitalization this time? For this question, there was greater differentiation between clinicians and patients/caregivers. As illustrated in Figure 3, patients and caregivers similarly identified symptoms such as trouble breathing and swelling and their diseases as the primary reasons for admission. Clinicians identified non-adherence to diet and medications, the progression of HF, and various socioeconomic factors, such as lack of social support and access to medications, as the reasons for HF admissions.
Figure 3.
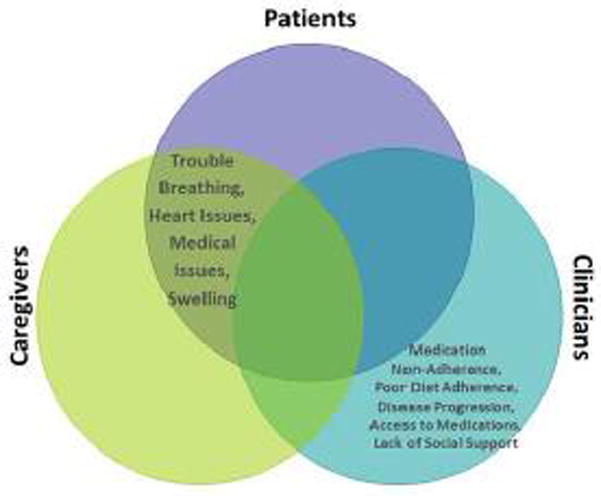
Reasons for Hospital Admission
Subgroup Analyses
Freelisting responses by patients with and without caregivers were compared. Salient terms for question 1 (home HF management) were largely similar (See Supplemental Material, Figure S2). For Question 2 (challenges to home HF management), there were some similarities; however, patients without caregivers uniquely listed obtaining and taking medications as salient terms (See Supplemental Material, Figure S3). For Question 3 (reasons for hospital admission), there was a small amount of overlap between the two groups (See Supplemental Material, Figure S4).
Freelisting responses by clinicians were analyzed by discipline. Salient terms for Question 1 (home HF management) were similar among the groups (See Supplemental Material, Figure S5). For Question 2 (challenges to home HF management), there were expected differences in responses reflecting the different perspectives in each group (See Supplemental Material, Figure S6). For Question 3 (reasons for hospital admission), there was general agreement about adherence to diet and medication, while other expected differences were based on provider perspective (See Supplemental Material, Figure S7).
Discussion
Triangulating patient, caregiver, and clinician perspectives is an important step in better understanding the reasons for HF readmissions. Freelisting is a technique that allows patients and their caregivers to provide spontaneous, qualitative descriptions of their experiences and a quantitative indicator of their relative importance based on the frequency of mention and the order of the list. To our knowledge, this study is the first application of freelisting to cardiovascular health services research. The results demonstrate similarities and significant differences among patient, caregiver, and clinician perspectives (See Table 4).
Table 4.
Key Potential Targets for Intervention to Address Areas of Discordance
| Area of Discordance | Potential Targets for Intervention |
|---|---|
| Home HF Management |
|
| Challenges to Home HF Management |
|
| Reasons for Hospital Admission |
|
When asked about home HF management, the only two shared salient terms among all three groups were take medications and healthy diet, which is consistent with the central importance of medication adherence and diet in managing HF. Clinicians and patients shared several salient terms, such as watching sodium and checking weight, which likely represents the results of patient education efforts. Although caregivers did cite some HF specific tasks, they did not cite two important HF specific tasks: checking weights and watching sodium. Caregivers primarily enumerated tasks related to taking care of daily needs of the patient, while clinicians did not mention any of these tasks. Based on these results, clinicians do not emphasize the role caregivers play in patient lives, and caregivers do not prioritize the importance of health maintenance tasks such as weight monitoring and sodium reduction. Clinical teaching could be restructured to focus on the relationship of HF maintenance care on managing the tasks that caregivers see as salient. Similarly, while acknowledging the essential roles of the caregiver, discussing HF-specific tasks with them may improve HF management across the continuum of care.
When describing things that make it difficult for HF management, clinicians focused on socio-economic factors, including financial constraints, lack of caregiver and social support, difficulties with access to care and medications, lack of knowledge about HF, and poor health literacy. In contrast, patients and caregivers had several salient terms related to limited functional status, activities of daily living, reduced independence, and stress. The discordance among clinicians, patients, and caregivers suggests that clinicians may not recognize some of the biggest challenges facing HF patients from the patient and caregiver perspective. Additionally, as suggested in other studies,23,24 obtaining and taking medications appear to be greater challenges for patients without a caregiver. This population of patients may particularly benefit from interventions designed to ensure access to medications and improve adherence.
When asked about the reasons for hospitalization, patients and caregivers viewed distressing symptoms and illness as the drivers for hospitalization. In contrast, clinicians included patient behaviors such as diet and medication adherence as being primarily responsible for admission. This suggests that patients see the reasons for hospital readmission as simply due to the fact that they became sicker and not necessarily that it might be connected with their health maintenance tasks of medication taking, weight management, or diet. The model of HF self-care, developed by Riegel et al.,25 defines the key components of self-care as falling into two domains: “Self-care maintenance” including symptom monitoring, treatment adherence, and symptom recognition; and “Self-care management” including symptom evaluation, treatment implementation, and treatment evaluation. Our findings fall mainly into the self-care maintenance domain with very little mention of self-care management tasks such as evaluating symptoms, implementing treatments, or evaluating how the treatments are working. These tend to be higher-level tasks performed by “self-care experts.”26 In addition, several factors, including comorbidities, depression, anxiety, age, impaired cognition, sleep disturbances, problems with the health system, and poor health literacy have been described as challenges to self-care,27 but these were not mentioned by our study subjects. These findings reinforce the importance of educating clinicians about the components of self-care including maintenance and management to help them develop personalized action plans to address barriers, self-efficacy, skills in symptom recognition, and monitoring and management of signs and symptoms.26
Numerous studies have examined patient, provider, and systemic barriers to care for HF patients using quantitative, qualitative, or mixed-methods approaches.8 We found some similarities to barriers identified in prior studies, but our novel approach has provided additional insights. Ghali et al.13 categorized precipitants for readmission using a “detailed personal interview” and found medication and dietary non-adherence as the major contributors to readmission. However, the details of the interview guide and analysis of qualitative data were not published, and our study used a more rigorous qualitative approach. Strunin et al.12 interviewed 21 hospitalized HF patients and found that “difficult life circumstances,” including lack of social support, lack of financial resources, and lack of transportation, and depression created barriers to recuperation after hospitalization. We identified similar factors for hospital admission to the Strunin et al.12 study; however, our study was larger and identified additional factors.
In the Netherlands, Annema et al.10 asked patients, caregivers, and clinicians the reasons for hospital HF readmission and found that providers disagreed with patients and their caregivers 64% of the time. Our study found some similar reasons for readmission and the presence of discordant perspectives using a different methodology in a sample with greater racial and ethnic diversity.
Retrum et al.,11 using semi-structured interviews, found that patient-identified reasons for HF readmission fell under five broad categories: distressing symptoms, unavoidable progression of illness, influence of psychosocial factors, good but imperfect self-care adherence, and health system failures. Our study adds additional perspectives of patients and the perspectives of caregivers and clinicians using freelisting and identifies key areas where perspectives differ.
Several clinical investigators have developed prediction models as a way to identify either high-risk individuals that require resource-intensive follow-up care or subgroups that might respond differently to particular forms of interventions. These models are built mostly from administrative or retrospective clinical data with variables selected by experts and generally have only moderate predictive accuracy.28,29 In three studies, the addition of psychosocial variables improved the predictive ability of the model.30–32 However, none of these studies interviewed patients using qualitative methods to select potential predictors of readmission. One potential explanation for the limited success of readmission risk prediction models is the lack of inclusion of patient-centered factors.
In this study, freelisting demonstrated several strengths. Freelisting explicitly elicits the perspectives of patients, caregivers, and clinicians to identify key similarities and differences in their perspectives. Unlike many qualitative studies that create semi-structured interview guides based on author expertise and literature review, freelisting can be used to develop an interview protocol derived from the perspectives of the major stakeholders involved in HF care. As a result, several areas of discordant perspectives among patient and caregiver dyads and clinicians were identified. A better understanding for the reasons underlying the discordant areas and developing strategies to increase concordance may help improve HF management across the continuum of care (See Table 4). Strategies to increase concordance may include restructuring patient and caregiver education around patient- and caregiver-identified tasks and barriers and conveying to clinicians the priorities and barriers expressed by patients and caregivers. Moreover, these findings suggest potential targets for strategies to improve transitional care by highlighting the importance of longitudinal follow-up of functional status, the ability to perform activities of daily living, and medication adherence.
The main limitation of this study is that all participants were identified within a single, urban health system. Additional studies in other health care systems and populations are needed. This includes the need for additional investigations in physician populations with greater diversity of racial and ethnic background and years of experience. In addition, the ability to quantify the factors identified and their predictive ability for hospital readmission remain untested. The challenges to HF management identified in this study now need to be better characterized. The next steps for this research study include open-ended, semi-structured interviews with patients using an interview guide based on these findings, and then testing prospectively challenges for predictive ability of hospital readmission.
Conclusion
There has been an increasing emphasis on the importance of measuring patient health status and patient-centered outcomes in cardiac patients.33 To our knowledge, this is the first application of freelisting to cardiovascular health services research. This method yielded insights into the difficulties of managing HF at home and revealed similarities and key discrepancies among clinician, patient, and caregiver perspectives. There appears to be some agreement on how to manage HF at home, less agreement on challenges to HF management, and almost no agreement on reasons for admissions. These findings may help clinicians frame evidence-based recommendations around items that are salient to patients and caregivers. Moreover, these results may prove useful in better predicting hospital readmission and tailoring interventions to patient and caregiver-specific barriers to maintaining their health after hospital discharge.
Supplementary Material
Highlights.
Patients, caregivers, and clinicians view challenges to HF management differently
Patients/caregivers cite very different reasons for readmission than clinicians
Patients/caregivers state distressing symptoms as the cause of admission
In contrast, clinicians cite patient behaviors as the primary drivers
Understanding these differences may help to reduce readmissions
Acknowledgments
We would like to thank Rebecca Henderson and Shimrit Keddem for contributions to data collection, management, and analysis. Dr. Ahmad was at the University of Pennsylvania when the study was performed.
Funding/Support: This study was funded by the Patient-Centered Outcomes Research Institute pilot grant 1IP2PI000186-02. Dr. Ahmad is supported by the National Heart, Lung and Blood Institute of the National Institutes of Health under Award number T32HL069771 and by a 2015 Research Fellowship Award from the Heart Failure Society of America.
The statements presented in this article are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient -Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Footnotes
Conflicts of Interests/Financial Disclosures: None of the authors report any conflicts of interests or financial disclosures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services (CMS), HHS. Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and FY 2012 rates; hospitals’ FTE resident caps for graduate medical education payment. Final rules. Fed Regist. 2011;76(160):51476–51846. [PubMed] [Google Scholar]
- 4.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Health Aff (Millwood) 2011;30(4):746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 5.Fleming LM, Kociol RD. Interventions for heart failure readmissions: successes and failures. Curr Heart Fail Rep. 2014;11(2):178–187. doi: 10.1007/s11897-014-0192-x. [DOI] [PubMed] [Google Scholar]
- 6.Feltner C, Jones CD, Cené CW, et al. Transitional Care Interventions to Prevent Readmissions for People with Heart Failure. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. [PubMed] [Google Scholar]
- 7.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 8.McEntee ML, Cuomo LR, Dennison CR. Patient-, Provider-, and System-Level Barriers to Heart Failure Care. J Cardiovasc Nurs. 2009;24(4):290–298. doi: 10.1097/JCN.0b013e3181a660a0. [DOI] [PubMed] [Google Scholar]
- 9.Saunders MM. Perspectives from family caregivers receiving home nursing support: findings from a qualitative study of home care patients with heart failure. Home Healthc Nurse. 2012;30(2):82–90. doi: 10.1097/NHH.0b013e3182429337. [DOI] [PubMed] [Google Scholar]
- 10.Annema C, Luttik ML, Jaarsma T. Reasons for readmission in heart failure: perspectives of patients, caregivers, cardiologists, and heart failure nurses. Heart Lung. 2009;38:427–34. doi: 10.1016/j.hrtlng.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Retrum JH, Boggs J, Hersh A, et al. Patient-Identified Factors Related to Heart Failure Readmissions. Circulation: Cardiovascular Quality and Outcomes. 2013;6(2):171–177. doi: 10.1161/CIRCOUTCOMES.112.967356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strunin L, Stone M, Jack B. Understanding rehospitalization risk: Can hospital discharge be modified to reduce recurrent hospitalization? J Hosp Med. 2007;2(5):297–304. doi: 10.1002/jhm.206. [DOI] [PubMed] [Google Scholar]
- 13.Ghali JK. Precipitating Factors Leading to Decompensation of Heart Failure. Archives of internal medicine. 1988;148(9):2013. doi: 10.1001/archinte.1988.00380090087021. [DOI] [PubMed] [Google Scholar]
- 14.Kleinman A. The Illness Narratives: Suffering, Healing and the Human Condition. New York: Basic Books; 1988. [Google Scholar]
- 15.Bhui K, Bhugra D. Explanatory models for mental distress: implications for clinical practice and research. The British Journal of Psychiatry. 2002;181(1):6–7. doi: 10.1192/bjp.181.1.6. [DOI] [PubMed] [Google Scholar]
- 16.Krumholz HM. Post-Hospital Syndrome — An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borgatti SP. Elicitation techniques for cultural domain analysis. In: Schensul JJ, LeCompte MD, editors. Enhanced Ethnographic Methods: Audiovisual Techniques, Focused Group Interviews, and Elicitation Techniques. Ethnographer Toolkit. Vol. 3. Walnut Creek: AltaMira Press; 1999. pp. 115–151. [Google Scholar]
- 18.Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative Approaches. 4. Walnut Creek, CA: Alta Mira Press; 2002. [Google Scholar]
- 19.Schrauf RW, Sanchez J. Using freelisting to identify, assess, and characterize age differences in shared cultural domains. J Gerontol B Psychol Sci Soc Sci. 2008;63(6):S385–93. doi: 10.1093/geronb/63.6.S385. [DOI] [PubMed] [Google Scholar]
- 20.Bernard HR, Ryan GW. Analyzing Qualitative Data: Systematic Approaches. Walnut Creek, California: Sage Publications; 2010. [Google Scholar]
- 21.Smith JJ, Borgatti SP. Salience Counts And So Does Accuracy: Correcting and Updating a Measure for Free-List-Item Salience. Journal of Linguistic Anthropology. 1997;7(2):208–209. doi: 10.1525/jlin.1997.7.2.208. [DOI] [Google Scholar]
- 22.Weller SC. Cultural Consensus Theory: Applications and Frequently Asked Questions. Field Methods. 2007;19(4):339–368. doi: 10.1177/1525822X07303502. [DOI] [Google Scholar]
- 23.Oosterom-Calo R, van Ballegooijen AJ, Terwee CB, et al. Determinants of adherence to heart failure medication: a systematic literature review. Heart Fail Rev. 2013;18(4):409–427. doi: 10.1007/s10741-012-9321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strachan PH, Currie K, Harkness K, Spaling M, Clark AM. Context Matters in Heart Failure Self-Care: A Qualitative Systematic Review. Journal of Cardiac Failure. 2014;20(6):448–455. doi: 10.1016/j.cardfail.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 25.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. J Cardiovasc Nurs. 2009;24(6):485–497. doi: 10.1097/JCN.0b013e3181b4baa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riegel B, Lee CS, Dickson VV. Medscape. Self care in patients with chronic heart failure. Nature Reviews Cardiology. 2011;8(11):644–654. doi: 10.1038/nrcardio.2011.95. [DOI] [PubMed] [Google Scholar]
- 27.Riegel B, Moser DK, Anker SD, et al. State of the science promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 28.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahimi K, Bennett D, Conrad N, et al. Risk Prediction in Patients With Heart Failure: A Systematic Review and Analysis. JACC: Heart Failure. 2014;2(5):440–446. doi: 10.1016/j.jchf.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 30.Coleman EA, Min S-J, Chomiak A, Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Services Research. 2004;39(5):1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48(11):981–988. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 32.Watson AJ, O’Rourke J, Jethwani K, et al. Linking electronic health record-extracted psychosocial data in real-time to risk of readmission for heart failure. Psychosomatics. 2011;52(4):319–327. doi: 10.1016/j.psym.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rumsfeld JS, Alexander KP, Goff DC, et al. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127(22):2233–2249. doi: 10.1161/CIR.0b013e3182949a2e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


