Abstract
Thiazide-induced hyponatremia is one of the main causes of decreased sodium levels in elderly individuals. This review presents the current evidence regarding the thiazide-associated hyponatremia. Thiazide-associated hyponatremia is observed mainly in patients with certain risk factors such as those receiving large doses of thiazides, having much comorbidity, such as heart failure, liver disease or malignancy, and taking several medications, such as non-steroidal anti-inflammatory drugs, selective serotonin re-uptake inhibitors or tricyclic antidepressants. Sodium concentration should be monitored in patients with risk factors for developing thiazide-associated hyponatremia and clinicians should measure promptly serum sodium levels in patients with neurologic signs indicating reduced sodium levels. The clinical and biochemical profile of patients with thiazide-associated hyponatremia may be that of extracellular volume depletion or the syndrome of inappropriate antidiuretic hormone secretion (SIADH). The investigation of possible thiazide-associated hyponatremia includes the exclusion of other causes of decreased sodium levels and the identification of the characteristics of hyponatremia due to thiazides (extracellular volume depletion-related or SIADH-like). Treatment should be carefully monitored to avoid serious neurologic complications due to overcorrection. Clinicians should discourage prescribing thiazides in patients with a history of diuretic-associated hyponatremia and should prefer low doses of thiazides in patients with risk factors for developing thiazide-associated hyponatremia.
Keywords: Antidiuretic hormone, Diuretics, Hyponatremia, Potassium, Sodium, Thiazides
1. Introduction
Hyponatremia (serum sodium < 136 mEq/L) is the most common electrolyte imbalance observed in clinical practice. This common electrolyte disorder is even more frequent in older patients and, indeed, increased age (> 60 years) represents a risk factor for the development of hyponatremia.[1]–[3] Moreover, the most common symptoms associated with acute hyponatremia (developed in less than 48 h), such as nausea, vomiting, headache, and/or seizures, as well as conditions associated with chronic hyponatremia due to any cause (even mild), such as fatigue, cognition impairment, gait deficits, falls and fractures and even increased mortality, are more frequent and severe in elderly patients.[4]–[6]
Among the various causes of drug-induced hyponatremia, thiazide-induced hyponatremia comprises a main cause, while loop diuretics only occasionally induce hyponatremia.[3],[7]–[17] The incidence of thiazide–induced hyponatremia has not been clearly determined, since in many cases other potential risk factors for low serum sodium levels are concurrently present. Hence, the reported incidence of thiazide-induced hyponatremia in various studies depended on several variables such as the definition of hyponatremia, the studied population (for example more frequent in the elderly), the healthcare setting, and differences in diuretic choice and dosage. In this context, a study reported that approximately 14% of 951 thiazide-treated outpatients had hyponatremia (serum sodium concentration < 135 mmol/L), whereas age > 70 years was associated with a fourfold increase in hyponatremia risk.[18] On the other hand, the Systolic Hypertension in the Elderly Program (SHEP) study reported hyponatremia (serum sodium concentration < 130 mmol/L) in 4.1% of patients taking chlorthalidone compared with 1.3% in the control group.[19] Generally, thiazide-associated hyponatremia (serum sodium concentration < 136 mmol/L) is a relatively frequent condition in elderly individuals. The aim of this review is to practically present the current evidence regarding the thiazide-induced hyponatremia in elderly patients.
2. Risk factors for thiazide-induced hyponatremia
The risk factors for the development of thiazide–associated hyponatremia are shown in Table 1.[11],[20],[21] Even though hyponatremia is usually observed within the first few weeks of treatment, it can also be observed after years of treatment especially when concomitant contributory factors shown in Table 1 supervene.[20],[22],[23]
Table 1. Risk factors for thiazide-associated hyponatremia in the elderly.
| Low-normal or unmeasured baseline sodium levels |
| Many comorbidities (> 5) |
| Low body mass |
| Low-sodium diet-tube feeding |
| Habitual increased water intake |
| Concominant administration of drugs affecting water homeostasis, such as SSRIs, NSAIDs or even benzodiazepines |
| Underlying psychiatric diseases associated with polydipsia |
| Female gender |
| Type 2 diabetes mellitus |
| Hypokalemia |
| Increased dose of thiazides |
| Co-administration of amiloride/spironolactone |
SSRIs: selective serotonin re-uptake inhibitors; NSAIDs: non-steroidal anti-inflammatory drugs.
Low-normal or unmeasured baseline sodium levels and increased comorbidity burden (≥ 5 comorbidities), such as heart failure, depression, dementia, respiratory diseases, chronic kidney disease, nausea, vomiting and/or malignancy, have been reported as strong predictors of hyponatremia in older adults.[24] Additionally, female gender or type 2 diabetes mellitus are significant risk factors for reduced sodium levels in patients receiving hydrochlorothiazide or indapamide.[22]
Thiazide-associated hyponatremia is more commonly encountered in elderly individuals with low body mass or low-sodium diet.[7]–[10],[20],[25] Furthermore, patients with habitual increased water intake (such as those with underlying psychiatric disorders, beer drinkers, etc) are particularly prone to the development of hyponatremia.[20] Concomitant administration of drugs affecting water homeostasis, such as selective serotonin reuptake inhibitors (SSRIs), serotonin–norepinephrine re-uptake inhibitors (SNRIs), non-steroidal anti-inflammatory drugs (NSAIDs) or benzodiazepines, is frequent in elderly patients with thiazide-associated hyponatremia.
The presence of hypokalemia is frequent in patients with thiazide-induced hyponatremia. However, hypokalemia is not only a risk factor for the development of hyponatremia but also for difficulty in the correction of hyponatremia.[26],[27]
A study reported that only 10% of elderly hypertensive women with diuretic-associated hyponatremia received a low dose of hydrochlorothiazide (12.5 mg/day), suggesting that the effects of thiazides are dose-dependent.[28] Interestingly, hyponatremia seems to be more common in patients treated with chlorthalidone compared with hydrochlorothiazide both in young and elderly individuals.[29],[30] A retrospective population-based cohort study of 29,873 individuals aged ≥ 66 years showed that chlorthalidone was associated with an increased hospitalizations due to hyponatremia by approximately 1.7 times compared with hydrochlorothiazide.[30] Indapamide administration may also be related with the development of hyponatremia.[31] Even the low dose of indapamide (sustained release 1.5 mg daily) can induce severe hyponatremia (serum sodium < 125 mmol/L) in elderly individuals.[32] However, indapamide, although not consistently, has been associated with less hyponatremia compared with hydrochlorothiazide in elderly hypertensive patients.[22],[33] It should be mentioned that the risk of hyponatremia increases with the concomitant administration of thiazides with amiloride or spironolactone.[34]
3. Biochemical characteristics of thiazide-associated hyponatremia
Patients with thiazide-associated hyponatremia are broadly divided into two subgroups according to their biochemical profile; a subgroup with laboratory results consistent with extracellular volume depletion (increased serum urea/creatinine ratio, increased uric acid levels, urine Na+ < 20 mmol/L after discontinuation of the thiazide) and a subgroup with a biochemical profile suggesting the syndrome of inappropriate antidiuretic hormone secretion (SIADH) (low to normal serum creatinine and urea, decreased uric acid levels, increased urine Na+).[35] However, in many cases the distinction of these subgroups is difficult since they may have features from both entities.[25],[36]
4. Pathogenetic mechanisms of thiazide–associated hyponatremia
A number of interrelated mechanisms are implicated in the pathogenesis of thiazide–induced hyponatremia in the elderly (Table 2).
Table 2. Pathogenetic mechanisms of thiazide-induced hyponatremia in the elderly.
| Decreased free water excretion (diminished urine diluting ability) due to the reduced NaCl reabsorption in the renal tubules |
| Excess renal losses of electrolytes (K+ + Na+) as compared to water excretion (hypertonic losses) |
| Aging and associated smaller muscle mass impair renal diluting capacity |
| Decreased intrarenal generation of prostaglandins |
| Decreased glomerular filtration rate |
| Increased water intake |
| Extracellular volume depletion leading to ADH-mediated water retention (non-osmotic baroceptor mediated) and to activation of thirst-stimulation of water intake |
| Coexistent diuretic–induced hypokalemia leading to transcellular cation exchange (K+ leaves the cells, while Na+ moves into cells) |
| Inappropriate secretion of ADH (thiazides can exacerbate hyponatremia in patients with underlying SIADH or can increase the secretion of ADH) |
| Direct upregulation of aquaporin-2 receptors expression in the renal tubules resulting in increased water permeability in the collecting duct |
ADH: antidiuretic hormone; SIADH: syndrome of inappropriate antidiuretic hormone secretion.
(1) The propensity of thiazides to promote hyponatremia is explained by the inhibition of urinary dilution due to reduced reabsorption of NaCl in the distal renal tubules.[25] In contrast, loop diuretics do not impair urinary dilution and are not associated with reduction of sodium levels.[37] Indeed, loop diuretics generally cause hypotonic renal losses and are used to treat euvolemic and hypervolemic hyponatremia. Furthermore, hypernatremia rather than hyponatremia may develop if renal water losses induced by loop diuretics are not sufficiently replaced.[3]
(2) Elderly patients usually have decreased muscle mass, which is associated with impairment of the renal diluting capacity.[38] In fact, decreased body mass is an independent risk factor for the development of thiazide–associated hyponatremia.[20],[24],[28] In this context, it has been proposed that the higher incidence of thiazide-associated hyponatremia in women may be mediated by body size.[21] It should be noted that serum sodium concentration is associated with exchangeable total (sodium + potassium)/total body water ratio. Hence, fluctuations in serum sodium concentration occur more frequently in subjects with less total body water. Additionally, low body mass in elderly subjects may be related to an underlying illness, which can also be associated with the development of hyponatremia. Decreased protein intake (habitually or due to superimposed illness) also affects water excretion and may play a role in the development of hyponatremia.[39]
(3) A decreased intrarenal generation of prostaglandins may also be involved in the impaired ability of elderly individuals to excrete water. In fact, a defect in water excretion due to prostaglandin deficiency would be amplified by thiazides, since the reabsorption of NaCl without water at the thiazide-sensitive site in the distal tubule normally lowers the urine osmolality.[38]
(4) The high prevalence of decreased glomerular filtration rate (GFR) in elderly individuals may also play a role in the thiazide-induced impaired water excretion. In this context, a study showed that patients who developed thiazide-associated hyponatremia had lower baseline GFR compared with patients who remained normonatremic during therapy.[39]
(5) Thiazide–induced extracellular volume depletion results in increased non-osmotic baroreceptor-mediated secretion of antidiuretic hormone (ADH). The increased ADH induces water retention in renal tubules and activates thirst–stimulation water intake.[25],[39]
(6) The thiazide-induced electrolyte excretion leads to loss of effective solutes (K+ + Na+), which in association with the excess of water due to ADH-mediated water retention results in hypertonic losses.[9]
(7) Increased water intake is a prominent factor related with hyponatremia, especially in patients with an acute idiosyncratic reduction in serum sodium concentration.[8],[40],[41] The role of drugs causing xerostomia, such as anticholinergics, SSRIs, tricyclic antidepressants, phenothiazines, is important in many elderly patients.[42]
(8) The thiazide-induced hypokalemia may play a significant role in the development of hyponatremia, since it promotes a transcellular exchange between K+ (exits from cells) and Na+ (moves into cells).[26],[27]
(9) Thiazides are associated in some cases with the development of euvolemic hyponatremia due to inappropriate secretion of ADH. Usually in these cases hyponatremia occurs acutely after thiazide initiation.[35],[43] It should also be mentioned that enhanced ADH release may also be induced by nausea or other neurological symptoms.
(10) It has been reported that the idiopathic SIADH (a relatively rare phenomenon) is more common among the elderly.[44] The increased incidence of idiopathic SIADH in older subjects may be due to a higher sensitivity to osmotic stimuli.[45]
(11) It is important to note that thiazides can also exacerbate hyponatremia in patients with underlying SIADH due to drugs (SSRIs, SNRIs, NSAIDs, benzodiazepines, tricyclic antidepressants) or other causes.[20] Moreover, various drug categories that elderly patients frequently take (e.g., NSAIDs, SSRIs, SNRIs, benzodiazepins, angiotensin converting enzyme inhibitors, sartans) impair water excretion. A multidrug regimen including some of these drugs is a risk factor for the development of thiazide-induced hyponatremia.
(12) Elderly individuals frequently follow a low salt diet, especially if they have hypertension or heart failure, and suffer from diseases (e.g., diabetes mellitus, infections, heart failure) that stimulate water intake or ADH release.
(13) A direct effect of thiazides on aquaporin-2 receptor expression in the renal tubules has also been proposed as a mediating mechanism promoting hyponatremia. In some cases, these receptors are acutely up-regulated by thiazides resulting in increased water permeability in the collecting duct and, hence, water retention and decreased sodium concentration.[46]–[48] Indeed, it has been shown in vitro that thiazides increase water permeability and water reabsorption in the inner medullary collecting duct in an ADH-independent manner.[46]–[48]
5. Diagnosis of thiazide-induced hyponatremia
Thiazide-induced hyponatremia should be considered when the hyponatremic patient takes a thiazide. However, it is necessary to distinguish the thiazide-induced hyponatremia from the other causes of reduced serum sodium concentration. A thorough medical history helps to identify the presence of underlying diseases, polydipsia or concurrent administration of drugs that may be related with reduced serum sodium levels.[20],[36],[49] Moreover, a detailed physical examination should focus on signs of extracellular volume depletion.
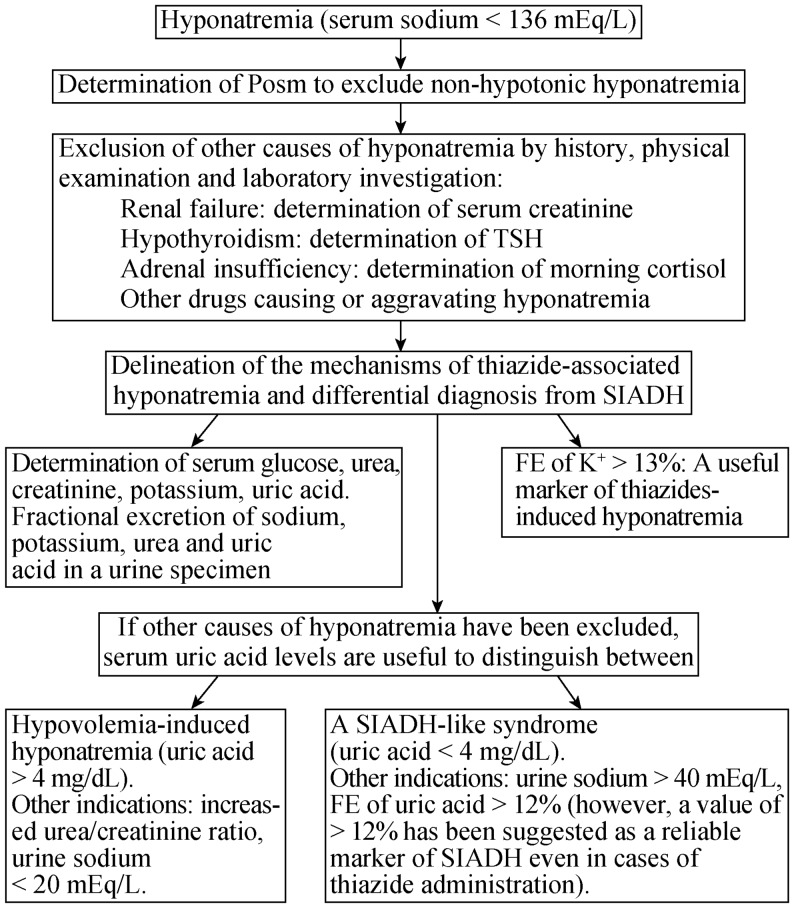
Laboratory investigation should be initiated with the measurement of serum osmolarity (Posm) (Figure 1). It is crucial to differentiate non-hypotonic hyponatremia from the “true” hypotonic (Posm < 280 mOsm/kg) hyponatremia.[50] When the latter has been confirmed, serum urea, creatinine, potassium, uric acid as well as thyroid stimulating hormone and cortisol levels (for the exclusion of endocrine diseases-associated hyponatremia) should be determined.[51]–[54] Additionally, urine urea, sodium, potassium, creatinine and uric acid should be measured in a spot urine sample and the fractional excretion of sodium, urea, potassium and uric acid levels should be appropriately calculated.
Figure 1. Laboratory investigation of possible thiazide-associated hyponatremia.
FE: fractional excretion; Posm: serum osmolarity; SIADH: syndrome of inappropriate antidiuretic hormone secretion; TSH: thyroid stimulating hormone.
The evaluation of laboratory tests for the diagnosis of thiazide-induced hyponatremia is presented in Table 3. It is important to note that although low uric acid levels combined with increased urate fractional excretion [fractional excretion (FE) of urate > 12%] favor the diagnosis of SIADH even in patients on diuretics,[55] these abnormalities may also point to a subgroup of patients with thiazide–induced hyponatremia. This subgroup of patients is presented with a SIADH-like picture with euvolemia, but usually with a quick onset of severe hyponatremia.[35] It should be noted that increased potassium excretion (FE of K+ >13%) is a useful marker for the diagnosis of thiazide-induced hyponatremia.[56]
Table 3. Diagnosis of thiazide-induced hyponatremia.
| Coexistent hypokalemia with kaliuria (FE of K+ >13%). FE of K can help to differentiate hyponatremia due to thiazides from other causes |
| A low FE of uric acid (< 12%) is usually observed in thiazides-associated hyponatremia |
| Urine sodium is < 20 mEq/L in patients with extracellular volume depletion-induced hyponatremia when the diuretic effect has warned off. However, values > 20 mEq/L are not diagnostic |
| Serum uric acid levels can differentiate between two subgroups of patients with thiazide-associated hyponatremia: patients with serum uric acid levels < 4 mg/dL usually exhibit a biochemical profile coexistent with a SIADH-like state, whereas patients with uric acid levels > 4 mg/dL usually have extracellular volume depletion |
FE: fractional excretion; SIADH: syndrome of inappropriate antidiuretic hormone secretion.
The restoration of normonatremia after thiazide withdrawal aids to the accurate diagnosis of thiazide-induced hyponatremia. However, up to two weeks may be needed after stopping the thiazide for full recovery of the diluting capacity and serum sodium normalization. This delay should be taken into account when investigating the subgroup of patients with possible thiazide-associated hyponatremia and a SIADH-like profile. In these patients, a thorough diagnostic work up for the presence of other causes for underlying SIADH should be done only if mild hyponatremia persists 2–3 weeks after the discontinuation of the thiazide.
6. Treatment of thiazide-induced hyponatremia
Hyponatremia, especially when attributed to diuretics, should be carefully managed.[57] The first step is the discontinuation of the possible offending agent. The drug withdrawal results in restoration of urinary diluting ability leading to increased water diuresis. This effect increases the risk of rapid or even dangerous correction of hyponatremia. The measurement of urine electrolytes and calculation of urine/plasma electrolyte ratio [(urine Na+ + urine K+)/serum Na+] are helpful. An urine/serum electrolyte ratio < 0.5 is indicative of increased water excretion, which is associated with potentially dangerous overtreatment of hyponatremia. In any case, frequent (every few hours) determination of serum electrolytes and careful evaluation of diuresis are mandatory for the safe and effective correction of hyponatremia.[53],[54],[58],[59]
Acute hyponatremia (developed in less than 48 h) may produce neurological symptoms, from simple such as nausea, vomiting, or headache to serious such as seizures, coma or death, which are associated with the degree of brain edema. In cases of acute symptomatic hyponatremia, administration of 100 mL of 3% NaCl (2 mL/kg body weight) should be immediately given. If it is needed, up to two additional infusions at 10-min intervals may be given.[60] Target of treatment is an increase of serum sodium by 4–6 mEq/L within the first 6 h for symptoms to subside. However, the increase in serum sodium should not exceed the 8 mEq/L during the first 24 h, the 12–14 mEq/L during the first 48 h, and the 14–16 mEq/L during the first 72 h. More rapid correction of hyponatremia increases the risk of developing the osmotic demyelination syndrome (ODS), a disorder involving central demyelinating lesions, particularly in the pons, and major neurologic disability or even fatal outcome.[61]–[63] Brain magnetic resonance imaging is sensitive to diagnose the demyelination in the brainstem pons.[64],[65] Elderly patients with hypokalemia, malnutrition, underlying liver disease and hypoxia are at particularly increased risk for the development of ODS.[53],[54],[58],[66] Moreover, it has been shown that elderly women are more susceptible to develop neurological complications as a result of rapid correction of hyponatremia.[62],[67],[68]
In cases of chronic oligosymptomatic hyponatremia, therapy is based mainly on patients' extracellular volume status. In euvolemic states, discontinuation of thiazide and water restriction (up to 1 L/day) are usually enough to correct serum sodium levels. In hypovolemic hyponatremia, normal saline (0.9% sodium chloride solution) should be administered.[60] The rate of infusion of normal saline should be individualized and special attention should be given in elderly patients with underlying heart failure.[69]
Importantly, the potassium depletion that is frequently observed in thiazide-related hyponatremia should also be corrected. However, clinicians should be very careful in this setting. First, potassium anions should be taken into account in the calculation of the tonicity of the infused solutions. Thus, when intravenous potassium administration is required, potassium chloride should be added in hypotonic fluids. The administration of potassium chloride in normal saline should be avoided because it can result in rapid correction of hyponatremia and circulatory overload.[69] Second, the correction of hypovolemia and hypokalemia may be followed by an increased water diuresis, which increases substantially the risk of overcorrection of hyponatremia and its devastating consequences.[53],[54],[58],[59] In these cases, careful and frequent monitoring (every few hours) of serum sodium concentration and diuresis is mandatory. The correction rate in serum sodium, which should be < 8 meq/L in the first 24 h of therapy in patients with chronic hyponatremia, should be even lower (i.e., < 4–6 mmol/L per 24 h) in the presence of hypokalemia.[70] It should be noted that vasopressin receptor inhibitors (Vaptans) do not have any role in hypovolemic hyponatremia due to thiazide administration.[71]
7. Prevention of thiazide–induced hyponatremia
Since thiazide-induced hyponatremia, even mild, is associated with a considerable increase in patients' morbidity, special attention should be given to the prevention of this abnormality in elderly patients (Table 4).[34],[57]–[59],[72] A low dose of diuretic (equivalent to 12.5 mg hydrochlorothiazide) should be preferred if additional risk factors coexist. A calcium channel blocker or beta-blockers are useful choices for patients who need an alternative antihypertensive treatment. Finally, in patients with a history of thiazide-associated hyponatremia who need to take diuretics, furosemide may be used without risk of recurrent hyponatremia.[73]
Table 4. Measures for the prevention of thiazide-induced hyponatremia.
| Thiazides should not be prescribed in elderly individuals with a history of diuretic-induced hyponatremia |
| Careful assessment of water intake especially in patients with underlying psychiatric disease and xerostomia |
| Careful administration of thiazides in patients taking drugs affecting water homeostasis, such as SSRIs and NSAIDs |
| A loop diuretic, which does not impair renal diluting ability, is desirable in patients with heart failure |
| Careful assessment of symptoms suggestive of decreased sodium levels (neurological symptoms, instability, frequent falls, decreased attention) shortly after thiazides prescription and regularly during therapy is mandatory |
| Measurement of serum creatinine and electrolyte values within the first days of thiazide initiation to identify an idiosyncratic acute decrease in serum sodium levels |
| Periodic laboratory investigation of patients on diuretics as well as on other drugs affecting renal function and electrolyte balance |
| Rapid discontinuation of diuretics as well as of other drugs affecting renal function and electrolyte balance in cases of an acute illness associated with decreased water intake, renal or extra-renal water losses, nausea or other conditions leading to increased ADH secretion |
ADH: antidiuretic hormone; NSAIDs: non-steroidal anti-inflammatory drugs; SSRIs: selective serotonine re-uptake inhibitors.
8. Conclusions
Thiazide-induced hyponatremia is frequent in elderly individuals. Clinicians should be aware for neurologic signs indicating decreased sodium levels and should monitor sodium concentration in patients with risk factors for thiazide-associated hyponatremia. The investigation of possible thiazide-associated hyponatremia includes the exclusion of other causes of reduced sodium levels and the identification of the characteristics of hyponatremia due to thiazides (extracellular volume depletion-related or SIADH-like). Serum sodium levels should be carefully monitored to avoid overcorrection, which is associated with serious neurologic complications. Clinicians should avoid prescribing thiazides in patients with a history of diuretic-associated hyponatremia.
Acknowledgments
This review was written independently, no company or institution supported it financially. Elisaf M has received speaker honoraria, consulting fees, and research funding from AstraZeneca, Schering Plough, Merck, Pfizer, Solvay, Abbott, Boehringer Ingelheim and Fournier, and has participated in clinical trials with AstraZeneca, Merck, Sanofi-Synthelabo, Solvay, Glaxo, Novartis, Pfizer and Fournier. The authors have given talks and attended conferences sponsored by various pharmaceutical companies, including Bristol-Myers Squibb, Pfizer, Lilly, Abbott, Amgen, Astrazeneca, Novartis, Vianex, Teva and MSD.
References
- 1.Hawkins RC. Age and gender as risk factors for hyponatremia and hypernatremia. Clin Chim Acta. 2003;337:169–172. doi: 10.1016/j.cccn.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Lindner G, Pfortmuller CA, Leichtle AB, et al. Age-related variety in electrolyte levels and prevalence of dysnatremias and dyskalemias in patients presenting to the emergency department. Gerontology. 2014;60:420–423. doi: 10.1159/000360134. [DOI] [PubMed] [Google Scholar]
- 3.Liamis G, Rodenburg EM, Hofman A, et al. Electrolyte disorders in community subjects: prevalence and risk factors. Am J Med. 2013;126:256–263. doi: 10.1016/j.amjmed.2012.06.037. [DOI] [PubMed] [Google Scholar]
- 4.Gankam Kengne F, Andres C, Sattar L, et al. Mild hyponatremia and risk of fracture in the ambulatory elderly. QJM. 2008;101:583–588. doi: 10.1093/qjmed/hcn061. [DOI] [PubMed] [Google Scholar]
- 5.Renneboog B, Musch W, Vandemergel X, et al. Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med. 2006;119:71 e71–78. doi: 10.1016/j.amjmed.2005.09.026. [DOI] [PubMed] [Google Scholar]
- 6.Hoorn EJ, Rivadeneira F, van Meurs JB, et al. Mild hyponatremia as a risk factor for fractures: the Rotterdam Study. J Bone Miner Res. 2011;26:1822–1828. doi: 10.1002/jbmr.380. [DOI] [PubMed] [Google Scholar]
- 7.Sonnenblick M, Friedlander Y, Rosin AJ. Diuretic-induced severe hyponatremia. Review and analysis of 129 reported patients. Chest. 1993;103:601–606. doi: 10.1378/chest.103.2.601. [DOI] [PubMed] [Google Scholar]
- 8.Friedman E, Shadel M, Halkin H, et al. Thiazide-induced hyponatremia. Reproducibility by single dose rechallenge and an analysis of pathogenesis. Ann Intern Med. 1989;110:24–30. doi: 10.7326/0003-4819-110-1-24. [DOI] [PubMed] [Google Scholar]
- 9.Ashraf N, Locksley R, Arieff AI. Thiazide-induced hyponatremia associated with death or neurologic damage in outpatients. Am J Med. 1981;70:1163–1168. doi: 10.1016/0002-9343(81)90822-6. [DOI] [PubMed] [Google Scholar]
- 10.Fichman MP, Vorherr H, Kleeman CR, et al. Diuretic-induced hyponatremia. Ann Intern Med. 1971;75:853–863. doi: 10.7326/0003-4819-75-6-853. [DOI] [PubMed] [Google Scholar]
- 11.Chow KM, Szeto CC, Wong TY, et al. Risk factors for thiazide-induced hyponatraemia. QJM. 2003;96:911–917. doi: 10.1093/qjmed/hcg157. [DOI] [PubMed] [Google Scholar]
- 12.Chow KM, Kwan BC, Szeto CC. Clinical studies of thiazide-induced hyponatremia. J Natl Med Assoc. 2004;96:1305–1308. [PMC free article] [PubMed] [Google Scholar]
- 13.Sardar GK, Eilbert WP. Severe hyponatremia associated with thiazide diuretic use. J Emerg Med. 2015;48:305–309. doi: 10.1016/j.jemermed.2014.09.054. [DOI] [PubMed] [Google Scholar]
- 14.Cohen DL, Townsend RR. Hyponatremia and thiazides. J Clin Hypertens (Greenwich) 2012;14:653. doi: 10.1111/j.1751-7176.2012.00673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Upadhyay A, Jaber BL, Madias NE. Epidemiology of hyponatremia. Semin Nephrol. 2009;29:227–238. doi: 10.1016/j.semnephrol.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Ellison DH, Loffing J. Thiazide effects and adverse effects: insights from molecular genetics. Hypertension. 2009;54:196–202. doi: 10.1161/HYPERTENSIONAHA.109.129171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119:S30–S35. doi: 10.1016/j.amjmed.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Clayton JA, Rodgers S, Blakey J, et al. Thiazide diuretic prescription and electrolyte abnormalities in primary care. Br J Clin Pharmacol. 2006;61:87–95. doi: 10.1111/j.1365-2125.2005.02531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 20.Hix JK, Silver S, Sterns RH. Diuretic-associated hyponatremia. Semin Nephrol. 2011;31:553–566. doi: 10.1016/j.semnephrol.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Rodenburg EM, Hoorn EJ, Ruiter R, et al. Thiazide-associated hyponatremia: a population-based study. Am J Kidney Dis. 2013;62:67–72. doi: 10.1053/j.ajkd.2013.02.365. [DOI] [PubMed] [Google Scholar]
- 22.Al Qahtani M, Alshahrani A, Alskaini A, et al. Prevalence of hyponatremia among patients who used indapamide and hydrochlorothiazide: a single center retrospective study. Saudi J Kidney Dis Transpl. 2013;24:281–285. doi: 10.4103/1319-2442.109574. [DOI] [PubMed] [Google Scholar]
- 23.Mori M, Koide T, Imanishi Y, et al. Duloxetine-induced hyponatremia in an elderly patient treated with thiazide diuretics. Indian J Pharmacol. 2014;46:657–659. doi: 10.4103/0253-7613.144947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Makam AN, Boscardin WJ, Miao Y, et al. Risk of thiazide-induced metabolic adverse events in older adults. J Am Geriatr Soc. 2014;62:1039–1045. doi: 10.1111/jgs.12839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hwang KS, Kim GH. Thiazide-induced hyponatremia. Electrolyte Blood Press. 2010;8:51–57. doi: 10.5049/EBP.2010.8.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aird W, Douek K, Halperin ML. Profound hypokalemia secondary to modest potassium depletion in a patient with coexisting hyponatremia: therapeutic implications. Am J Kidney Dis. 1988;12:164–166. doi: 10.1016/s0272-6386(88)80014-3. [DOI] [PubMed] [Google Scholar]
- 27.Liamis G, Mitrogianni Z, Liberopoulos EN, et al. Electrolyte disturbances in patients with hyponatremia. Intern Med. 2007;46:685–690. doi: 10.2169/internalmedicine.46.6223. [DOI] [PubMed] [Google Scholar]
- 28.Sharabi Y, Illan R, Kamari Y, et al. Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens. 2002;16:631–635. doi: 10.1038/sj.jhh.1001458. [DOI] [PubMed] [Google Scholar]
- 29.van Blijderveen JC, Straus SM, Rodenburg EM, et al. Risk of hyponatremia with diuretics: chlorthalidone versus hydrochlorothiazide. Am J Med. 2014;127:763–771. doi: 10.1016/j.amjmed.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 30.Dhalla IA, Gomes T, Yao Z, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158:447–455. doi: 10.7326/0003-4819-158-6-201303190-00004. [DOI] [PubMed] [Google Scholar]
- 31.Chapman MD, Hanrahan R, McEwen J, et al. Hyponatraemia and hypokalaemia due to indapamide. Med J Aust. 2002;176:219–221. doi: 10.5694/j.1326-5377.2002.tb04377.x. [DOI] [PubMed] [Google Scholar]
- 32.Yong TY, Huang JE, Lau SY, et al. Severe hyponatremia and other electrolyte disturbances associated with indapamide. Curr Drug Saf. 2011;6:134–137. doi: 10.2174/157488611797579249. [DOI] [PubMed] [Google Scholar]
- 33.Plante GE, Dessurault DL. Hypertension in elderly patients. A comparative study between indapamide and hydrochlorothiazide. Am J Med. 1988;84:98–103. [PubMed] [Google Scholar]
- 34.Arampatzis S, Gaetcke LM, Funk GC, et al. Diuretic-induced hyponatremia and osteoporotic fractures in patients admitted to the emergency department. Maturitas. 2013;75:81–86. doi: 10.1016/j.maturitas.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 35.Liamis G, Christidis D, Alexandridis G, et al. Uric acid homeostasis in the evaluation of diuretic-induced hyponatremia. J Investig Med. 2007;55:36–44. doi: 10.2310/6650.2007.06027. [DOI] [PubMed] [Google Scholar]
- 36.Liamis G, Milionis H, Elisaf M. A review of drug-induced hyponatremia. Am J Kidney Dis. 2008;52:144–153. doi: 10.1053/j.ajkd.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 37.Szatalowicz VL, Miller PD, Lacher JW, et al. Comparative effect of diuretics on renal water excretion in hyponatraemic oedematous disorders. Clin Sci (Lond) 1982;62:235–238. doi: 10.1042/cs0620235. [DOI] [PubMed] [Google Scholar]
- 38.Clark BA, Shannon RP, Rosa RM, et al. Increased susceptibility to thiazide-induced hyponatremia in the elderly. J Am Soc Nephrol. 1994;5:1106–1111. doi: 10.1681/ASN.V541106. [DOI] [PubMed] [Google Scholar]
- 39.Frenkel NJ, Vogt L, De Rooij SE, et al. Thiazide-induced hyponatraemia is associated with increased water intake and impaired urea-mediated water excretion at low plasma antidiuretic hormone and urine aquaporin-2. J Hypertens. 2015;33:627–633. doi: 10.1097/HJH.0000000000000423. [DOI] [PubMed] [Google Scholar]
- 40.Kennedy RM, Earley LE. Profound hyponatremia resulting from a thiazide-induced decrease in urinary diluting capacity in a patient with primary polydipsia. N Engl J Med. 1970;282:1185–1186. doi: 10.1056/NEJM197005212822107. [DOI] [PubMed] [Google Scholar]
- 41.Beresford HR. Polydipsia, hydrochlorothiazide, and water intoxication. JAMA. 1970;214:879–883. [PubMed] [Google Scholar]
- 42.Visvanathan V, Nix P. Managing the patient presenting with xerostomia: a review. Int J Clin Pract. 2010;64:404–407. doi: 10.1111/j.1742-1241.2009.02132.x. [DOI] [PubMed] [Google Scholar]
- 43.Decaux G, Schlesser M, Coffernils M, et al. Uric acid, anion gap and urea concentration in the diagnostic approach to hyponatremia. Clin Nephrol. 1994;42:102–108. [PubMed] [Google Scholar]
- 44.Shapiro DS, Sonnenblick M, Galperin I, et al. Severe hyponatraemia in elderly hospitalized patients: prevalence, aetiology and outcome. Intern Med J. 2010;40:574–580. doi: 10.1111/j.1445-5994.2010.02217.x. [DOI] [PubMed] [Google Scholar]
- 45.Helderman JH, Vestal RE, Rowe JW, et al. The response of arginine vasopressin to intravenous ethanol and hypertonic saline in man: the impact of aging. J Gerontol. 1978;33:39–47. doi: 10.1093/geronj/33.1.39. [DOI] [PubMed] [Google Scholar]
- 46.Kim GH, Lee JW, Oh YK, et al. Antidiuretic effect of hydrochlorothiazide in lithium-induced nephrogenic diabetes insipidus is associated with upregulation of aquaporin-2, Na-Cl co-transporter, and epithelial sodium channel. J Am Soc Nephrol. 2004;15:2836–2843. doi: 10.1097/01.ASN.0000143476.93376.04. [DOI] [PubMed] [Google Scholar]
- 47.Glover M, O'Shaughnessy KM. Molecular insights from dysregulation of the thiazide-sensitive WNK/SPAK/NCC pathway in the kidney: Gordon syndrome and thiazide-induced hyponatraemia. Clin Exp Pharmacol Physiol. 2013;40:876–884. doi: 10.1111/1440-1681.12115. [DOI] [PubMed] [Google Scholar]
- 48.Tiwari S, Packer RK, Hu X, et al. Increased renal alpha-ENaC and NCC abundance and elevated blood pressure are independent of hyperaldosteronism in vasopressin escape. Am J Physiol Renal Physiol. 2006;291:F49–F57. doi: 10.1152/ajprenal.00390.2005. [DOI] [PubMed] [Google Scholar]
- 49.Filippatos TD, Elisaf MS. Hyponatremia in patients with heart failure. World J Cardiol. 2013;5:317–328. doi: 10.4330/wjc.v5.i9.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liamis G, Tsimihodimos V, Elisaf M. Hyponatremia in diabetes mellitus: Clues to diagnosis and treatment. J Diabetes Metab. 2015;6:6. [Google Scholar]
- 51.Leung AA, Wright A, Pazo V, et al. Risk of thiazide-induced hyponatremia in patients with hypertension. Am J Med. 2011;124:1064–1072. doi: 10.1016/j.amjmed.2011.06.031. [DOI] [PubMed] [Google Scholar]
- 52.Liamis G, Milionis HJ, Elisaf M. Endocrine disorders: causes of hyponatremia not to neglect. Ann Med. 2011;43:179–187. doi: 10.3109/07853890.2010.530680. [DOI] [PubMed] [Google Scholar]
- 53.Maxwell AP. Diagnosis and management of hyponatraemia: AGREEing the guidelines. BMC Med. 2015;13:31. doi: 10.1186/s12916-015-0277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nagler EV, Vanmassenhove J, van der Veer SN, et al. Diagnosis and treatment of hyponatremia: a systematic review of clinical practice guidelines and consensus statements. BMC Med. 2014;12:1. doi: 10.1186/s12916-014-0231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fenske W, Stork S, Koschker AC, et al. Value of fractional uric acid excretion in differential diagnosis of hyponatremic patients on diuretics. J Clin Endocrinol Metab. 2008;93:2991–2997. doi: 10.1210/jc.2008-0330. [DOI] [PubMed] [Google Scholar]
- 56.Musch W, Thimpont J, Vandervelde D, et al. Combined fractional excretion of sodium and urea better predicts response to saline in hyponatremia than do usual clinical and biochemical parameters. Am J Med. 1995;99:348–355. doi: 10.1016/s0002-9343(99)80180-6. [DOI] [PubMed] [Google Scholar]
- 57.Gross P, Palm C. Thiazides: do they kill? Nephrol Dial Transplant. 2005;20:2299–2301. doi: 10.1093/ndt/gfi109. [DOI] [PubMed] [Google Scholar]
- 58.Adrogue HJ, Madias NE. Diagnosis and treatment of hyponatremia. Am J Kidney Dis. 2014;64:681–684. doi: 10.1053/j.ajkd.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 59.Liamis G, Elisaf M. Treatment of hyponatremia: what the clinician needs to know. J Nephrol Res. 2015;1:19–21. [Google Scholar]
- 60.Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013;126:S1–42. doi: 10.1016/j.amjmed.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 61.Adrogue HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581–1589. doi: 10.1056/NEJM200005253422107. [DOI] [PubMed] [Google Scholar]
- 62.Karp BI, Laureno R. Pontine and extrapontine myelinolysis: a neurologic disorder following rapid correction of hyponatremia. Medicine (Baltimore) 1993;72:359–373. [PubMed] [Google Scholar]
- 63.Kumar S, Fowler M, Gonzalez-Toledo E, et al. Central pontine myelinolysis, an update. Neurol Res. 2006;28:360–366. doi: 10.1179/016164106X110346. [DOI] [PubMed] [Google Scholar]
- 64.Graff-Radford J, Fugate JE, Kaufmann TJ, et al. Clinical and radiologic correlations of central pontine myelinolysis syndrome. Mayo Clin Proc. 2011;86:1063–1067. doi: 10.4065/mcp.2011.0239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hart BL, Eaton RP. Osmotic Myelinolysis. N Engl J Med. 1995;333:1259. doi: 10.1056/NEJM199511093331905. [DOI] [PubMed] [Google Scholar]
- 66.Lauriat SM, Berl T. The hyponatremic patient: practical focus on therapy. J Am Soc Nephrol. 1997;8:1599–1607. doi: 10.1681/ASN.V8101599. [DOI] [PubMed] [Google Scholar]
- 67.Verbalis JG, Martinez AJ. Neurological and neuropathological sequelae of correction of chronic hyponatremia. Kidney Int. 1991;39:1274–1282. doi: 10.1038/ki.1991.161. [DOI] [PubMed] [Google Scholar]
- 68.Sterns RH, Cappuccio JD, Silver SM, et al. Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective. J Am Soc Nephrol. 1994;4:1522–1530. doi: 10.1681/ASN.V481522. [DOI] [PubMed] [Google Scholar]
- 69.Liamis G, Filippatos TD, Elisaf MS. Correction of hypovolemia with crystalloid fluids: Individualizing infusion therapy. Postgrad Med. 2015;127:405–412. doi: 10.1080/00325481.2015.1029421. [DOI] [PubMed] [Google Scholar]
- 70.Arany I, Safirstein RL. Cisplatin nephrotoxicity. Semin Nephrol. 2003;23:460–464. doi: 10.1016/s0270-9295(03)00089-5. [DOI] [PubMed] [Google Scholar]
- 71.Liamis G, Filippatos TD, Elisaf MS. Treatment of hyponatremia: the role of lixivaptan. Expert Rev Clin Pharmacol. 2014;7:431–441. doi: 10.1586/17512433.2014.911085. [DOI] [PubMed] [Google Scholar]
- 72.Hoorn EJ, Liamis G, Zietse R, et al. Hyponatremia and bone: an emerging relationship. Nat Rev Endocrinol. 2012;8:33–39. doi: 10.1038/nrendo.2011.173. [DOI] [PubMed] [Google Scholar]
- 73.Fadel S, Karmali R, Cogan E. Safety of furosemide administration in an elderly woman recovered from thiazide-induced hyponatremia. Eur J Intern Med. 2009;20:30–34. doi: 10.1016/j.ejim.2008.04.006. [DOI] [PubMed] [Google Scholar]