Abstract
Importance
Estimates of the relative mortality risks associated with normal weight, overweight, and obesity may help to inform decision making in the clinical setting.
Objective
To perform a systematic review of reported hazard ratios (HRs) of all-cause mortality for overweight and obesity relative to normal weight in the general population.
Data Sources
PubMed and EMBASE electronic databases were searched through September 30, 2012, without language restrictions.
Study Selection
Articles that reported HRs for all-cause mortality using standard body mass index (BMI) categories from prospective studies of general populations of adults were selected by consensus among multiple reviewers. Studies were excluded that used nonstandard categories or that were limited to adolescents or to those with specific medical conditions or to those undergoing specific procedures. PubMed searches yielded 7034 articles, of which 141 (2.0%) were eligible. An EMBASE search yielded 2 additional articles. After eliminating overlap, 97 studies were retained for analysis, providing a combined sample size of more than 2.88 million individuals and more than 270 000 deaths.
Data Extraction
Data were extracted by 1 reviewer and then reviewed by 3 independent reviewers. We selected the most complex model available for the full sample and used a variety of sensitivity analyses to address issues of possible overadjustment (adjusted for factors in causal pathway) or underadjustment (not adjusted for at least age, sex, and smoking).
Results
Random-effects summary all-cause mortality HRs for overweight (BMI of 25–<30), obesity (BMI of ≥30), grade 1 obesity (BMI of 30–<35), and grades 2 and 3 obesity (BMI of ≥35) were calculated relative to normal weight (BMI of 18.5–<25). The summary HRs were 0.94 (95% CI, 0.91–0.96) for overweight, 1.18 (95% CI, 1.12–1.25) for obesity (all grades combined), 0.95 (95% CI, 0.88–1.01) for grade 1 obesity, and 1.29 (95% CI, 1.18–1.41) for grades 2 and 3 obesity. These findings persisted when limited to studies with measured weight and height that were considered to be adequately adjusted. The HRs tended to be higher when weight and height were self-reported rather than measured.
Conclusions and Relevance
Relative to normal weight, both obesity (all grades) and grades 2 and 3 obesity were associated with significantly higher all-cause mortality. Grade 1 obesity overall was not associated with higher mortality, and overweight was associated with significantly lower all-cause mortality. The use of predefined standard BMI groupings can facilitate between-study comparisons.
The topic of the mortality differences between weight categories has sometimes been described as controversial.1 The appearance of controversy may arise in part because studies of body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) and mortality have used a wide variety of BMI categories and varying reference categories, which can make findings appear more variable than when standard categories are used and also can make it difficult to compare and synthesize studies. A report2 in 1997 from the World Health Organization Consultation on Obesity defined BMI-based categories of underweight, normal weight, preobesity, and obesity. The same cutoff BMI values were adopted by the National Heart, Lung, and Blood Institute in 1998.3
In this study, we used the National Heart, Lung, and Blood Institute’s terminology with categories of underweight (BMI of <18.5), normal weight (BMI of 18.5–<25), overweight (BMI of 25–<30), and obesity (BMI of ≥30). Grade 1 obesity was defined as a BMI of 30 to less than 35; grade 2 obesity, a BMI of 35 to less than 40; and grade 3 obesity, a BMI of 40 or greater. These standard categories have been increasingly used in published studies of BMI and mortality, but the literature reporting these results has not been systematically reviewed.
The purpose of this study was to compile and summarize published analyses of BMI and all-cause mortality that provide hazard ratios (HRs) for standard BMI categories. We followed the guidelines in the Meta-analysis of Observational Studies in Epidemiology (MOOSE) statement4 for reporting of systematic reviews.
METHODS
Articles were identified by searches of PubMed and EMBASE through September 30, 2012. Details of search strategies appear in eTable 1 at http://www.jama.com. No language restrictions were applied. All articles were reviewed for inclusion by 1 reviewer (K.M.F.). An independent review of all articles was conducted by a second set of reviewers (B.K.K., H.O., and B.I.G.). The articles were reviewed to identify those that used standard BMI categories in prospective, observational cohort studies of all-cause mortality among adults with BMI measured or reported at baseline. Studies that addressed these relationships only in adolescents, only in institutional settings, or only among those with specific medical conditions or undergoing specific medical procedures were excluded. We included multiple articles from a given data set only when there was little overlap between articles by sex, age group, or some other factor.
In some cases, authors used standard BMI categories for overweight and obesity but had used a slightly broader reference BMI category of less than 25 or a slightly narrower reference BMI category of 20 to less than 25 rather than the standard normal BMI category of 18.5 to less than 25. We included these articles but have noted the cases in which the reference BMI category was less than 25 or 20 to less than 25. We classified studies that included a mix of self-reported and measured weight and height according to the preponderant type.
Abstracted items included sample size, number of deaths, age at baseline, length of follow-up, HRs and 95% confidence intervals, sex, age, type of weight and height data (measured or self-reported), country or region, source of study sample, adjustment factors, exclusion and inclusion criteria, and sensitivity analyses. Authors of screened articles were queried for additional information when necessary. In studies that only presented results stratified by smoking or health condition, we selected results for nonsmokers or never smokers or for those without the health condition. We selected the most complex model available for the full sample and used a variety of sensitivity analyses to address issues of possible over-adjustment or underadjustment.
We categorized HRs into 2 age groupings either as limited solely to people aged 65 years or older or as a mixed-age category (eg, aged 25–64 years or 40–80 years). We classified articles as adequately adjusted, possibly overadjusted, or possibly underadjusted. We categorized HRs by adjustment level, by whether the data were measured or self-reported, by whether the analysis was performed separately for men and women or for both sexes combined, and by region (North America, Europe, and other).
We used a random-effects model5 to summarize the results overall and within subgroups and based statistically significant heterogeneity on a P value of less than .05. We calculated the quantity I2 to describe the degree of heterogeneity with values of 25%, 50%, and 75% considered low, moderate, and high, respectively.6 We also used a sequential approach similar to that described by Patsopoulos et al7 to assess consistency of findings when heterogeneity was reduced. All analyses were performed with SAS version 9.3 (SAS Institute Inc).
For sensitivity analyses, we examined the effects on HRs of incorporating results from a recent large pooled study for overweight.8 For comparative purposes, we also constructed approximate HRs relative to normal weight from several recent large studies9–14 that had used finer BMI groupings and thus did not meet our inclusion criteria. To do this, we averaged HRs from the finer BMI groupings over groups corresponding to the standard BMI categories, weighting the HRs by the number of deaths.
RESULTS
As shown in the eFigure at http://www.jama.com, the primary search strategy for PubMed yielded 4142 articles, of which 128 met our criteria. A second PubMed search yielded 2892 additional articles, of which 13 met our criteria. A search of EMBASE yielded 2 additional eligible articles. In total, 143 eligible studies were identified.
After exclusion of 41 articles with overlapping data sets and of 5 articles lacking sufficient information, 97 articles remained for analysis; all of which had been identified through systematic search procedures. The selected studies are shown in eTable 2 with additional information in eTable 3 regarding exclusions and adjustment factors. Regions of origin of participants included the United States or Canada (n=41 studies), Europe (n=37), Australia (n=7), China or Taiwan (n=4), Japan (n=2), Brazil (n=2), Israel (n=2), India (n=1), and Mexico (n=1). The tabulated studies included more than 2.88 million participants and more than 270 000 deaths.
Not all studies reported the specific categories of interest. There were 93 studies for the BMI category of 25 to less than 30 (overweight), 61 studies for the BMI category of 30 or greater (obesity), and 32 studies for the BMI categories of 30 to less than 35 (grade 1 obesity) and 35 and greater (grades 2 and 3 obesity).
We considered the results adequately adjusted if they were adjusted for age, sex, and smoking and not adjusted for factors in the causal pathway between obesity and mortality, or if they had reported or demonstrated that adjustments or exclusions to avoid bias had shown little effect on their findings. A number of studies (for example15–29) reported qualitatively that such adjustments had little or no effect without showing quantitative details.
Other studies (for example30–32) demonstrated little effect through a series of sensitivity analyses. We considered the available full sample results from such studies to also be adequately adjusted. Otherwise, we considered studies as possibly overadjusted if they adjusted for factors such as hypertension that are considered to be in the causal pathway between obesity and mortality or as possibly underadjusted if they did not adjust for age, sex, and smoking. We classified 53 studies as adequately adjusted, 34 studies as possibly overadjusted, and 10 studies as possibly underadjusted.
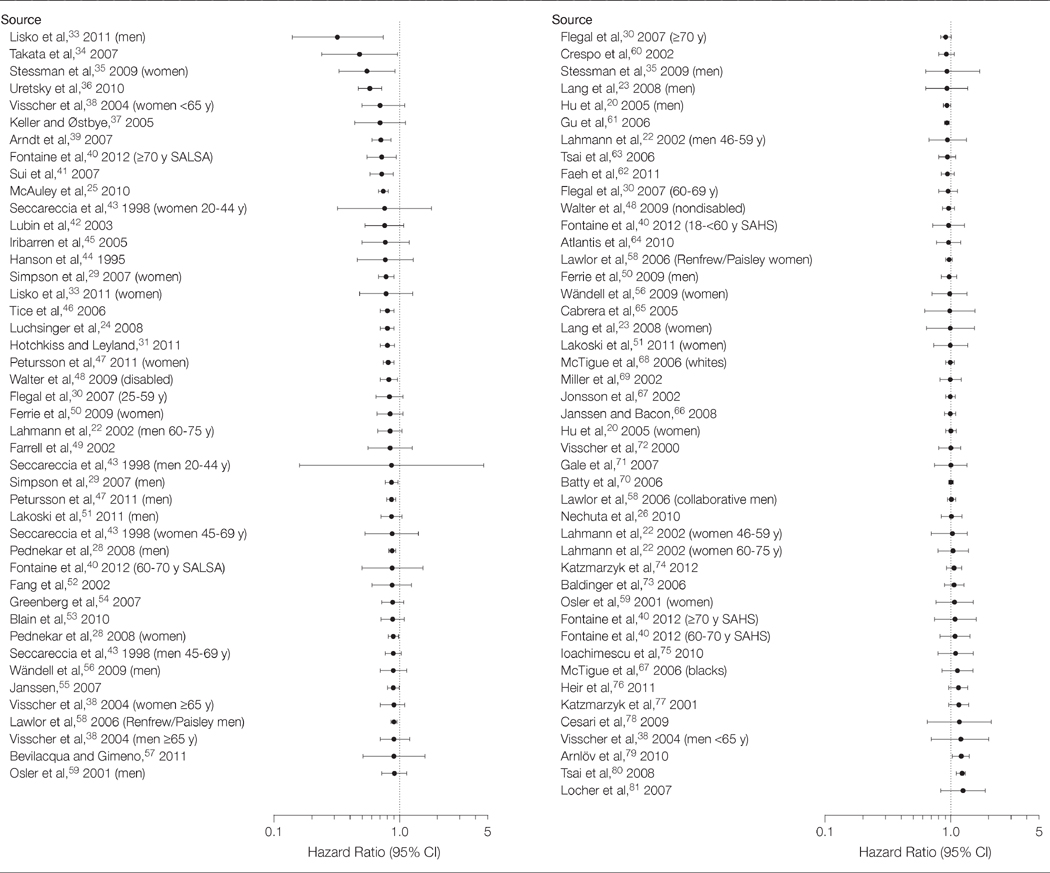
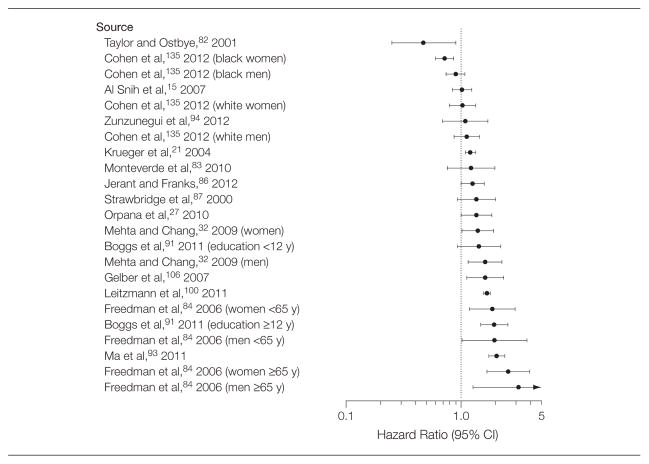
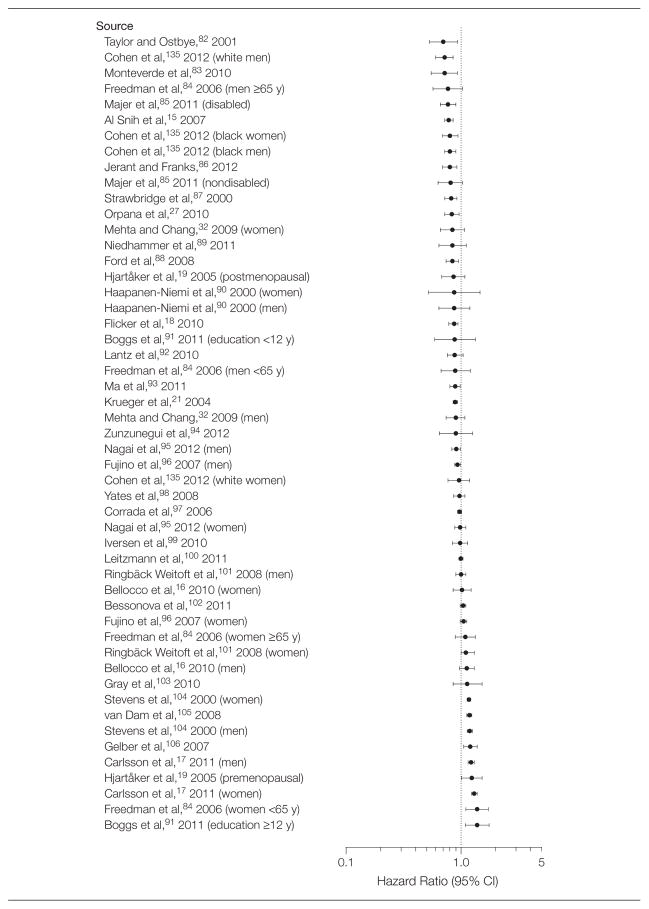
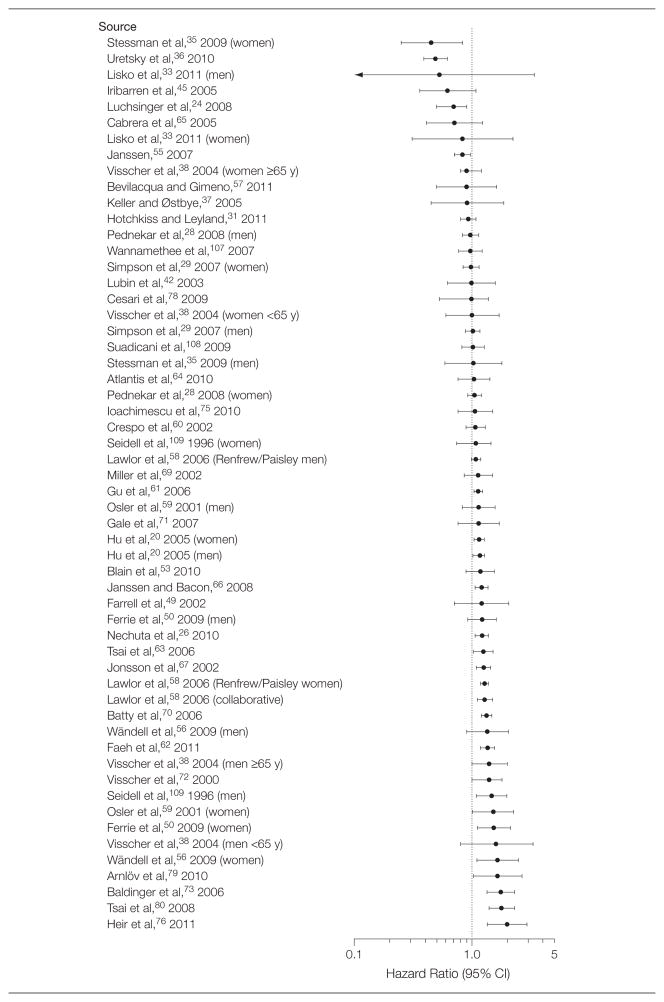
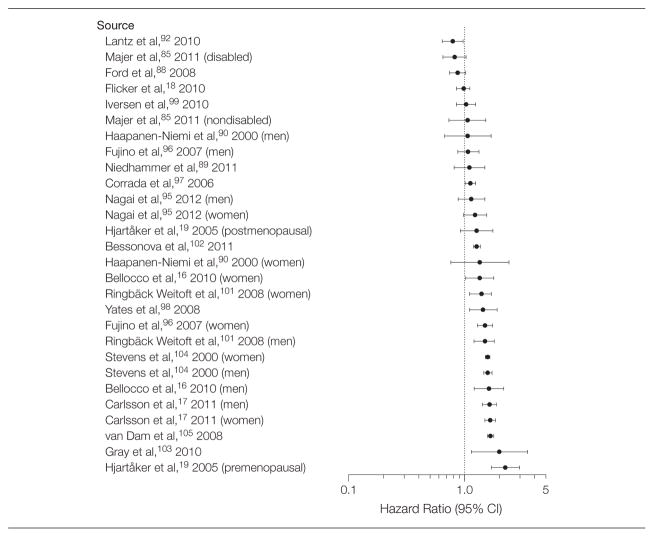
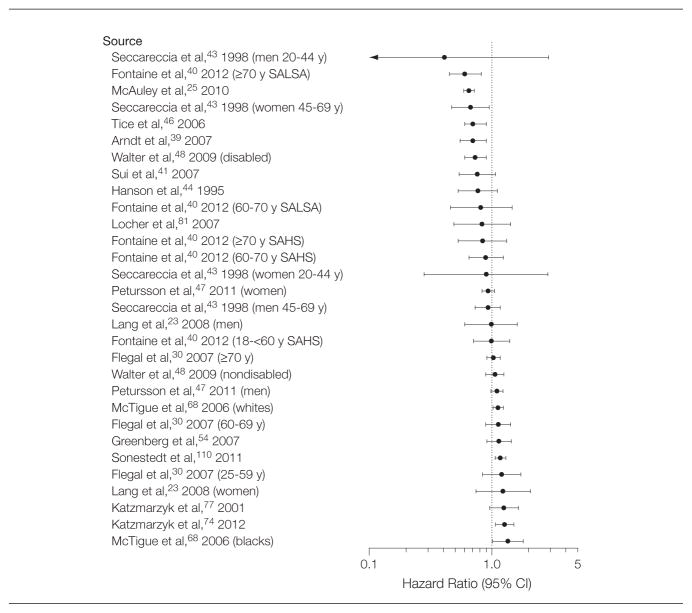
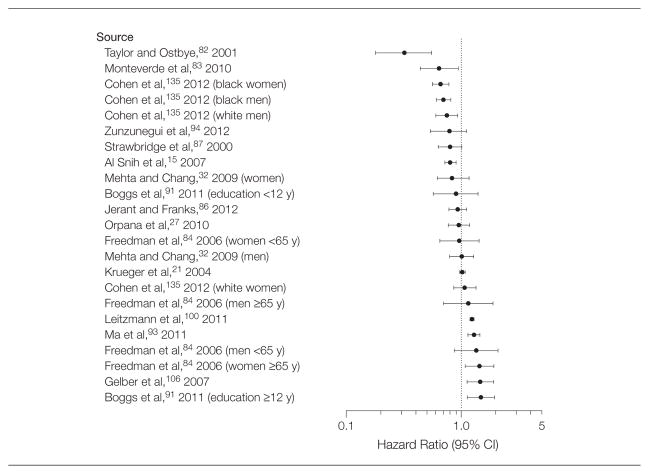
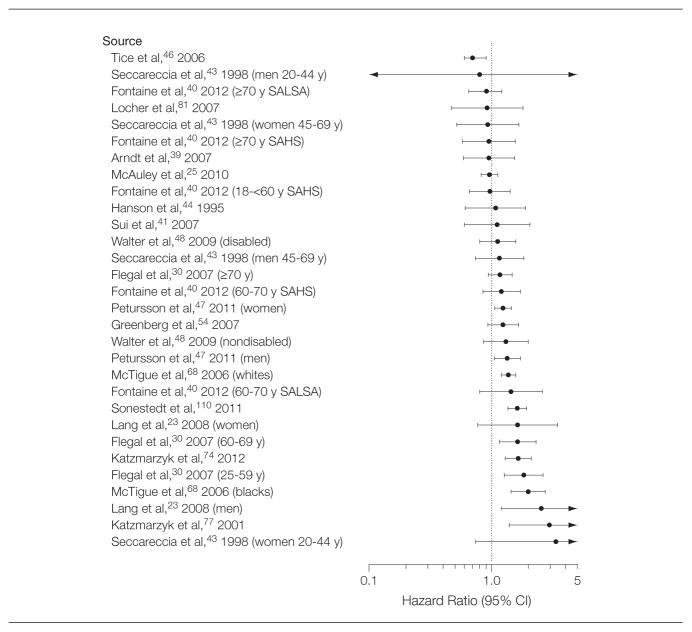
Summary HRs are shown in Table 1 overall, by age group, and by whether data were measured or self-reported. The summary HRs were 0.94 (95% CI, 0.91–0.96) for overweight, 1.18 (95% CI, 1.12–1.25) for obesity (all grades), 0.95 (95% CI, 0.88–1.01) for grade 1 obesity, and 1.29 (95% CI, 1.18–1.41) for grades 2 and 3 obesity. Plots of HRs for these categories are shown in Figures 1–8.33–110 Additional details are shown in eTables 4–7, which show summary HRs by age, sex, region, and measurement type.
Table 1.
Summary Random-Effects Hazard Ratios (HRs) of All-Cause Mortality for Overweight and Obesity Relative to Normal Weight
| Self-reported or Measured Height and Weight | Height and Weight | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Measured | Self-reported | ||||||||
|
|
|
|
|||||||
| No. of HRs | Summary HR (95% CI) | I2, % | No. of HRs | Summary HR (95% CI) | I2, % | No. of HRs | Summary HR (95% CI) | I2, % | |
| BMI of 25–<30 | |||||||||
| All ages | 140 | 0.94 (0.91–0.96)a | 85.0 | 89 | 0.93 (0.89–0.95)a | 75.8 | 51 | 0.96 (0.92–1.00)a | 90.4 |
|
| |||||||||
| Mixed ages | 107 | 0.95 (0.92–0.98)a | 86.8 | 67 | 0.93 (0.89–0.96)a | 79.6 | 40 | 0.98 (0.93–1.03)a | 90.7 |
|
| |||||||||
| Age ≥65 y only | 33 | 0.90 (0.86–0.94)a | 51.2 | 22 | 0.90 (0.84–0.95) | 31.2 | 11 | 0.90 (0.84–0.96)a | 71.0 |
|
| |||||||||
| BMI of ≥30 | |||||||||
| All ages | 84 | 1.18 (1.12–1.25)a | 86.7 | 56 | 1.13 (1.06–1.19)a | 73.4 | 28 | 1.29 (1.18–1.41)a | 89.7 |
|
| |||||||||
| Mixed ages | 63 | 1.23 (1.16–1.31)a | 87.2 | 41 | 1.16 (1.10–1.24)a | 74.6 | 22 | 1.36 (1.25–1.48)a | 86.1 |
|
| |||||||||
| Age ≥65 y only | 21 | 1.03 (0.94–1.12)a | 61.5 | 15 | 0.98 (0.86–1.12)a | 61.1 | 6 | 1.09 (0.96–1.23)a | 67.0 |
|
| |||||||||
| BMI of 30–<35 | |||||||||
| All ages | 53 | 0.95 (0.88–1.01)a | 86.8 | 30 | 0.94 (0.86–1.03)a | 80.5 | 23 | 0.95 (0.85–1.06)a | 90.1 |
|
| |||||||||
| Mixed ages | 42 | 0.96 (0.89–1.04)a | 87.7 | 24 | 0.95 (0.86–1.06)a | 83.2 | 18 | 0.97 (0.87–1.09)a | 90.0 |
|
| |||||||||
| Age ≥65 y only | 11 | 0.87 (0.72–1.05)a | 76.3 | 6 | 0.89 (0.71–1.11) | 56.2 | 5 | 0.83 (0.58–1.20)a | 85.7 |
|
| |||||||||
| BMI of ≥35 | |||||||||
| All ages | 53 | 1.29 (1.18–1.41)a | 81.7 | 30 | 1.25 (1.13–1.39)a | 65.4 | 23 | 1.34 (1.16–1.55)a | 88.3 |
|
| |||||||||
| Mixed ages | 42 | 1.32 (1.19–1.45)a | 82.8 | 24 | 1.28 (1.14–1.44)a | 68.9 | 18 | 1.35 (1.16–1.58)a | 89.0 |
|
| |||||||||
| Age ≥65 only | 11 | 1.20 (0.94–1.52)a | 70.6 | 6 | 1.10 (0.89–1.34) | 25.1 | 5 | 1.29 (0.77–2.17)a | 85.2 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Indicates significant heterogeneity (P<.05).
Figure 1.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Measured Data for Participants With a Body Mass Index of 25 to Less Than 30
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals. SAHS indicates San Antonio Heart Study; and SALSA, Sacramento Area Latino Study on Aging.
Figure 8.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Self-reported Data for Participants With a Body Mass Index of 35 or Greater
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals.
Results for studies that we considered adequately adjusted are shown in Table 2. This more select group showed the same general pattern of overweight associated with reduced mortality, grade 1 obesity not significantly associated with increased mortality, and the higher grades of obesity significantly associated with increased mortality. The summary HRs were 0.94 (95% CI, 0.90–0.97) for overweight, 1.21 (95% CI, 1.12–1.31) for obesity (all grades), 0.97 (95% CI, 0.90–1.04) for grade 1 obesity, and 1.34 (95% CI, 1.21–1.47) for grades 2 and 3 obesity. For overweight, the results from possibly overadjusted studies and from adequately adjusted studies were similar (eTable 8). However, for obesity, the possibly overadjusted studies tended to have lower HRs than the adequately adjusted studies.
Table 2.
Summary Hazard Ratios (HRs) of All-Cause Mortality for Overweight and Obesity Relative to Normal Weight From Studies Considered Adequately Adjusted
| Self-reported or Measured Height and Weight | Height and Weight | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Measured | Self-reported | ||||||||
|
|
|
|
|||||||
| No. of HRs | Summary HR (95% CI) | I2, % | No. of HRs | Summary HR (95% CI) | I2, % | No. of HRs | Summary HR (95% CI) | I2, % | |
| BMI of 25–<30 | |||||||||
| All ages | 86 | 0.94 (0.90–0.97)a | 87.6 | 45 | 0.92 (0.88–0.96)a | 74.8 | 41 | 0.95 (0.90–1.01)a | 91.0 |
|
| |||||||||
| Mixed ages | 68 | 0.95 (0.91–0.99)a | 89.3 | 34 | 0.93 (0.88–0.98)a | 79.2 | 34 | 0.96 (0.91–1.02)a | 91.8 |
|
| |||||||||
| Age ≥65 y only | 18 | 0.90 (0.86–0.95) | 27.9 | 11 | 0.90 (0.84–0.96) | 23.4 | 7 | 0.91 (0.84–0.98) | 42.9 |
|
| |||||||||
| BMI of ≥30 | |||||||||
| All ages | 42 | 1.21 (1.12–1.31)a | 89.3 | 22 | 1.11 (1.03–1.20)a | 67.1 | 20 | 1.33 (1.21–1.47)a | 88.0 |
|
| |||||||||
| Mixed ages | 33 | 1.26 (1.16–1.37)a | 89.7 | 16 | 1.13 (1.04–1.23)a | 66.7 | 17 | 1.39 (1.27–1.53)a | 84.3 |
|
| |||||||||
| Age ≥65 y only | 9 | 1.05 (0.92–1.21)a | 63.9 | 6 | 1.02 (0.81–1.29)a | 73.1 | 3 | 1.08 (0.93–1.25) | 39.7 |
|
| |||||||||
| BMI of 30–<35 | |||||||||
| All ages | 42 | 0.97 (0.90–1.04)a | 83.8 | 21 | 1.00 (0.92–1.09)a | 64.2 | 21 | 0.94 (0.84–1.05)a | 89.6 |
|
| |||||||||
| Mixed ages | 33 | 0.98 (0.91–1.06)a | 84.8 | 16 | 1.03 (0.94–1.12)a | 64.8 | 17 | 0.95 (0.85–1.07)a | 90.3 |
|
| |||||||||
| Age ≥65 y only | 9 | 0.88 (0.69–1.12)a | 78.0 | 5 | 0.90 (0.70–1.16)a | 64.1 | 4 | 0.82 (0.46–1.47)a | 88.1 |
|
| |||||||||
| BMI of ≥35 | |||||||||
| All ages | 42 | 1.34 (1.21–1.47)a | 81.2 | 21 | 1.32 (1.20–1.46)a | 46.6 | 21 | 1.35 (1.16–1.57)a | 88.7 |
|
| |||||||||
| Mixed ages | 33 | 1.35 (1.22–1.50)a | 82.2 | 16 | 1.37 (1.24–1.52) | 40.4 | 17 | 1.34 (1.14–1.57)a | 89.6 |
|
| |||||||||
| Age ≥65 y only | 9 | 1.28 (0.93–1.76)a | 75.2 | 5 | 1.12 (0.89–1.43) | 37.8 | 4 | 1.40 (0.64–3.07)a | 86.8 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Indicates significant heterogeneity (P<.05).
Between-study heterogeneity was statistically significant in most categories. According to Higgins et al,6 this test may have “excessive power when there are many studies, especially when those studies are large.” Heterogeneity (as indicated by the value of I2) was less for studies with measured height and weight and was lower for studies limited to those older than 65 years. The value of I2 was reduced by limiting findings to adequately adjusted studies with measured data.
Higher levels of heterogeneity, however, do not necessarily lead to dissimilar results that would affect the conclusions. For example, the summary HR for overweight for older ages (≥65 years) was identical (0.90) for measured height and weight (I2=31.2%) and for self-reported height and weight (I2 =71.0%). For adequately adjusted studies, we sequentially excluded HRs within age and measurement categories as needed to reduce the I2 value to below 25%. Within the 4 age-measurement groups, this required exclusion of 9% to 22% of studies for measured data and 14% to 39% of studies for self-reported data.
For overweight, excluding these studies led to a uniformly lower HR of 0.89 for both age groups and for both measured and self-reported data. For obesity, the effects of excluding these studies were more variable and led to an overall increase of the summary HR from 1.21 to 1.24. Corresponding values were from 0.97 to 1.05 (neither significantly different from 1) for grade 1 obesity and from 1.34 to 1.39 for grades 2 and 3 obesity. Thus, heterogeneity appeared to have had little effect on the conclusions of the meta-analysis.
The excluded studies varied across outcome categories; inspection of the excluded studies did not suggest specific reasons why they had contributed to heterogeneity. Taken together, the findings suggest that contributors to heterogeneity across all studies include adjustment levels, type of measurement data, and age group. Some degree of heterogeneity may also result from the variation in BMI levels within the broad BMI categories used, as well as from variations in the type of cohorts studied.
Sensitivity Analyses
For the overweight category only, we also repeated analyses including the results from a study that pooled data from 19 cohorts. After excluding ever smokers and those with a history of cancer or heart disease, Berrington de Gonzalez et al8 found a HR of 1.11 (95% CI, 1.07–1.16) for men and 1.13 (95% CI, 1.09–1.16) for women with a BMI of 25 to 29.9 relative to those with a BMI of 20 to less than 25 (Amy Berrington de Gonzalez, DPhil, written communication, June 16, 2011).
Our analysis included published studies using 6 of the same cohorts, representing about 60% of the original Berrington de Gonzalez et al8 sample. Excluding those studies from our analysis and substituting the above results from Berrington de Gonzalez et al did not change the summary HR for overweight.
We also repeated the analyses after excluding the studies that had used slightly different reference categories. Excluding studies with a reference BMI category of less than 25 had no effect on the HRs for overweight and decreased the HR for obesity by 0.02. Excluding studies with a reference BMI category of 20 to less than 25 increased the HR for overweight by 0.005 and had no effect on the HR for obesity.
Beyond these slight differences in the reference category, studies that used nonstandard BMI categories were excluded. However, we were able to construct approximate HRs from some recent large studies that had used nonstandard BMI categories (eTable 9). This approach does not allow for construction of appropriate standard errors or confidence intervals. The approximate HRs were consistent with our findings from our analyses of individual studies, showing similar minor variation.
COMMENT
This study presents comprehensive estimates (derived from a systematic review) of the association of all-cause mortality in adults with current standard BMI categories used in the United States and internationally. Estimates of the relative mortality risks associated with normal weight, overweight, and obesity may help to inform decision making in the clinical setting.
The most recent data from the United States show that almost 40% of adult men and almost 30% of adult women fall into the overweight category with a BMI of 25 to less than 30.111 Comparable figures for Canada are 44% of men and 30% of women112 and for England are 42% of men and 32% of women.113
According to the results presented herein, overweight (defined as a BMI of 25–<30) is associated with significantly lower mortality overall relative to the normal weight category with an overall summary HR of 0.94. For overweight, 75% of HRs with measured weight and height and 67% of HRs with self-reported weight and height were below 1. These results are broadly consistent with 2 previous meta-analyses114,115 that used standard categories. In a pooled analysis of 26 observational studies, McGee et al114 found summary relative risks of all-cause mortality for overweight of 0.97 (95% CI, 0.92–1.01) for men and 0.97 (95% CI, 0.93–0.99) for women relative to normal weight.
Recent estimates for the prevalence of obesity (defined as a BMI of ≥30) among adults are 36% in the United States,111 24% in Canada,112 and 26% in England.113 Obesity was associated with significantly higher all-cause mortality relative to the normal weight BMI category with an overall summary HR of 1.18. Corresponding estimates for obesity from McGee et al114 were 1.20 (95% CI, 1.12–1.29) for men and 1.28 (95% CI, 1.18–1.37) for women. In the United States and Canada, more than half of those who are obese fall into the grade 1 category (BMI of 30–<35). We did not find significant excess mortality associated with grade 1 obesity, suggesting that the main contribution to excess mortality in obesity comes from higher levels of BMI.
Our findings are consistent with observations of lower mortality among overweight and moderately obese patients.116–119 Possible explanations have included earlier presentation of heavier patients,120 greater likelihood of receiving optimal medical treatment,121–123 cardioprotective metabolic effects of increased body fat,124,125 and benefits of higher metabolic reserves.118
The results presented herein provide little support for the suggestion126 that smoking and preexisting illness are important causes of bias. Most studies that addressed the issue found that adjustments or exclusions for these factors had little or no effect. However, overadjustment for factors in the causal pathway appears to decrease HRs for obesity but not for overweight.
An important source of bias appears to be the errors in self-reported weight and height data. Such errors have been shown to vary by age, sex, race, measured values, and data collection method.127,128 The systematic error of self-reported data rather than measured data can result in substantial misclassification of individuals into incorrect BMI categories,129 create errors that are difficult to correct,130 and lead to upward bias in the estimates.131 We found a generally lower summary HR and less heterogeneity in studies using measured data than in studies using self-reported data. The differences were more pronounced in analyses stratified by sex than in analyses that combined both men and women. Because the errors in self-reported data tend to differ by sex, there may be an offsetting effect when analyses combine men and women.
Publication bias can potentially affect systematic reviews. Studies that find little or no association of overweight or obesity with mortality risk sometimes only mention these results in passing without providing details. For example, He et al132 did not include terms for overweight or obesity in their models, reporting only that overweight and obesity were not associated with increased mortality. Studies of BMI and mortality sometimes selectively report analyses of certain subgroups, an approach that can lead to bias.133,134
The study by Berrington de Gonzalez et al8 and the overlapping study by Adams et al1 found results similar to ours in their full sample but based their final results on a subgroup with less than half of their original sample, arguing that this subgroup provided more valid results than the full sample. The validity of this assertion has not been demonstrated, and such large-scale exclusions may introduce additional bias, particularly when using self-reported data. Other studies* have shown little or no effect of similar exclusions.
Strengths and Limitations
One of the strengths of our study is the large sample size and number of studies included, which make the findings robust to the effects of any single study. Additionally, we used a comprehensive search strategy and prespecified standard categories. Although standard BMI categories were developed by the World Health Organization and by the National Institutes of Health in the 1990s, not all studies of BMI and mortality use standard categories as part of their analyses. The combination of flexible categorization and selective reporting can lead to wide variations in HRs even within a single data set.136 Categorization of BMI has both advantages and disadvantages.137,138 However, the use of predefined standard groupings avoids issues of post hoc and ad hoc selection of categories and reference categories.
Our study also has limitations. It addresses only all-cause mortality and not morbidity or cause-specific mortality. It addresses only findings related to BMI and not to other aspects of body composition such as visceral fat or fat distribution. Our census of these articles may be incomplete. Our coding and data abstraction procedures may have introduced errors. Our information on age was limited. Because of publication bias and selective reporting, null or negative HRs may have been less likely to be published. Geographical coverage was limited.
CONCLUSIONS
Relative to normal weight, obesity (all grades) and grades 2 and 3 obesity were both associated with significantly higher all-cause mortality. Grade 1 obesity was not associated with higher mortality, suggesting that the excess mortality in obesity may predominantly be due to elevated mortality at higher BMI levels. Overweight was associated with significantly lower all-cause mortality. The use of predefined standard BMI groupings can facilitate between-study comparisons.
Supplementary Material
Figure 2.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Self-reported Data for Participants With a Body Mass Index of 25 to Less Than 30
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals.
Figure 3.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Measured Data for Participants With a Body Mass Index of 30 or Greater
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals.
Figure 4.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Self-reported Data for Participants With a Body Mass Index of 30 or Greater
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals.
Figure 5.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Measured Data for Participants With a Body Mass Index of 30 to Less Than 35
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals. SAHS indicates San Antonio Heart Study; and SALSA, Sacramento Area Latino Study on Aging.
Figure 6.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Self-reported Data for Participants With a Body Mass Index of 30 to Less Than 35
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals.
Figure 7.
Hazard Ratios for All-Cause Mortality Relative to Normal Weight in Studies That Used Measured Data for Participants With a Body Mass Index of 35 or Greater
Data markers indicate hazard ratios and error bars indicate 95% confidence intervals. SAHS indicates San Antonio Heart Study; and SALSA, Sacramento Area Latino Study on Aging.
Acknowledgments
Funding/Support: There was no external funding for this work. The Centers for Disease Control and Prevention and the National Cancer Institute reviewed and approved the manuscript before submission.
Footnotes
Author Contributions: Dr Flegal had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Flegal, Kit, Graubard.
Acquisition of data: Flegal, Kit, Orpana, Graubard.
Analysis and interpretation of data: Flegal, Kit, Orpana, Graubard.
Drafting of the manuscript: Flegal.
Critical revision of the manuscript for important intellectual content: Flegal, Kit, Orpana, Graubard.
Statistical analysis: Flegal, Graubard.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The findings and conclusions in this report are those of the authors and not necessarily the official views of the Centers for Disease Control and Prevention or the National Cancer Institute.
Online-Only Material: The Author Video Interview, eTables 1 through 9, eFigure, and eReferences are available at http://www.jama.com.
Additional Contributions: We thank Amy Berrington de Gonzalez, DPhil (National Cancer Institute), Marselle Bevilacqua (Universidade Federal de São Paulo, Brazil), Michael Bursztyn, MD (Hadassah-Hebrew University Medical Center), Sarah Cohen, PhD (International Epidemiology Institute), Jane Ferrie, PhD (University College, London), Trond Heir, MD (Oslo University Hospital), Heather Keller, PhD (University of Waterloo), Patrick Krueger, PhD (University of Colorado), Petra Lahmann, PhD (Queensland Institute of Medical Research), Iain Lang, MD (Peninsula College of Medicine and Dentisty), Malena Monteverde, PhD (National Council of Scientific and Technical Research, Argentina), Mangesh Pednekar, PhD (Sekhsaria Institute for Public Health), Julie Simpson, PhD (University of Melbourne), and Joachanan Stessman, MD (Hadassah-Hebrew University Medical Center), for providing additional information about their studies; Yinong Chong, PhD (Centers for Disease Control and Prevention), for assistance with an article in Chinese; Eduardo Simoes, MD (Centers for Disease Control and Prevention), for assistance with an article in Portuguese; and David Check, BS (National Cancer Institute), for assistance with the figures. No financial compensation was provided to any of these individuals.
References
- 1.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 2.Obesity: preventing and managing the global epidemic: report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 3.Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 4.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting: Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 5.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170(15):1293–1301. doi: 10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- 10.Jee SH, Sull JW, Park J, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355(8):779–787. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 11.Klenk J, Nagel G, Ulmer H, et al. VHM&PP Study Group. Body mass index and mortality: results of a cohort of 184,697 adults in Austria. Eur J Epidemiol. 2009;24(2):83–91. doi: 10.1007/s10654-009-9312-4. [DOI] [PubMed] [Google Scholar]
- 12.Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359(20):2105–2120. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 13.Whitlock G, Lewington S, Sherliker P, et al. Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364(8):719–729. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al Snih S, Ottenbacher KJ, Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007;167(8):774–780. doi: 10.1001/archinte.167.8.774. [DOI] [PubMed] [Google Scholar]
- 16.Bellocco R, Jia C, Ye W, Lagerros YT. Effects of physical activity, body mass index, waist-to-hip ratio and waist circumference on total mortality risk in the Swedish National March Cohort. Eur J Epidemiol. 2010;25(11):777–788. doi: 10.1007/s10654-010-9497-6. [DOI] [PubMed] [Google Scholar]
- 17.Carlsson S, Andersson T, de Faire U, Lichtenstein P, Michaëlsson K, Ahlbom A. Body mass index and mortality: is the association explained by genetic factors? Epidemiology. 2011;22(1):98–103. doi: 10.1097/EDE.0b013e3181fce2a2. [DOI] [PubMed] [Google Scholar]
- 18.Flicker L, McCaul KA, Hankey GJ, et al. Body mass index and survival in men and women aged 70 to 75. J Am Geriatr Soc. 2010;58(2):234–241. doi: 10.1111/j.1532-5415.2009.02677.x. [DOI] [PubMed] [Google Scholar]
- 19.Hjartåker A, Adami HO, Lund E, Weiderpass E. Body mass index and mortality in a prospectively studied cohort of Scandinavian women: the women’s lifestyle and health cohort study. Eur J Epidemiol. 2005;20(9):747–754. doi: 10.1007/s10654-005-2145-x. [DOI] [PubMed] [Google Scholar]
- 20.Hu G, Tuomilehto J, Silventoinen K, Barengo NC, Peltonen M, Jousilahti P. The effects of physical activity and body mass index on cardiovascular, cancer and all-cause mortality among 47 212 middle-aged Finnish men and women. Int J Obes (Lond) 2005;29(8):894–902. doi: 10.1038/sj.ijo.0802870. [DOI] [PubMed] [Google Scholar]
- 21.Krueger PM, Rogers RG, Hummer RA, Boardman JD. Body mass, smoking, and overall and cause-specific mortality among older US adults. Res Aging. 2004;26(1):82–107. [Google Scholar]
- 22.Lahmann PH, Lissner L, Gullberg B, Berglund G. A prospective study of adiposity and all-cause mortality: the Malmö Diet and Cancer Study. Obes Res. 2002;10(5):361–369. doi: 10.1038/oby.2002.50. [DOI] [PubMed] [Google Scholar]
- 23.Lang IA, Llewellyn DJ, Alexander K, Melzer D. Obesity, physical function, and mortality in older adults. J Am Geriatr Soc. 2008;56(8):1474–1478. doi: 10.1111/j.1532-5415.2008.01813.x. [DOI] [PubMed] [Google Scholar]
- 24.Luchsinger JA, Patel B, Tang MX, Schupf N, Mayeux R. Body mass index, dementia, and mortality in the elderly. J Nutr Health Aging. 2008;12(2):127–131. doi: 10.1007/BF02982565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McAuley PA, Kokkinos PF, Oliveira RB, Emerson BT, Myers JN. Obesity paradox and cardiorespiratory fitness in 12,417 male veterans aged 40 to 70 years. Mayo Clin Proc. 2010;85(2):115–121. doi: 10.4065/mcp.2009.0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nechuta SJ, Shu XO, Li HL, et al. Combined impact of lifestyle-related factors on total and cause-specific mortality among Chinese women: prospective cohort study. PLoS Med. 2010;7(9) doi: 10.1371/journal.pmed.1000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Orpana HM, Berthelot JM, Kaplan MS, Feeny DH, McFarland B, Ross NA. BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring) 2010;18(1):214–218. doi: 10.1038/oby.2009.191. [DOI] [PubMed] [Google Scholar]
- 28.Pednekar MS, Hakama M, Hebert JR, Gupta PC. Association of body mass index with all-cause and cause-specific mortality: findings from a prospective cohort study in Mumbai (Bombay), India. Int J Epidemiol. 2008;37(3):524–535. doi: 10.1093/ije/dyn001. [DOI] [PubMed] [Google Scholar]
- 29.Simpson JA, MacInnis RJ, Peeters A, Hopper JL, Giles GG, English DR. A comparison of adiposity measures as predictors of all-cause mortality: the Melbourne Collaborative Cohort Study. Obesity (Silver Spring) 2007;15(4):994–1003. doi: 10.1038/oby.2007.622. [DOI] [PubMed] [Google Scholar]
- 30.Flegal KM, Graubard BI, Williamson DF, Gail MH. Impact of smoking and preexisting illness on estimates of the fractions of deaths associated with underweight, overweight, and obesity in the US population. Am J Epidemiol. 2007;166(8):975–982. doi: 10.1093/aje/kwm152. [DOI] [PubMed] [Google Scholar]
- 31.Hotchkiss JW, Leyland AH. The relationship between body size and mortality in the linked Scottish Health Surveys: cross-sectional surveys with follow-up. Int J Obes (Lond) 2011;35(6):838–851. doi: 10.1038/ijo.2010.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehta NK, Chang VW. Mortality attributable to obesity among middle-aged adults in the United States. Demography. 2009;46(4):851–872. doi: 10.1353/dem.0.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lisko I, Tiainen K, Stenholm S, Luukkaala T, Hervonen A, Jylhä M. Body mass index, waist circumference, and waist-to-hip ratio as predictors of mortality in nonagenarians: the Vitality 90+ Study. J Gerontol A Biol Sci Med Sci. 2011;66(11):1244–1250. doi: 10.1093/gerona/glr147. [DOI] [PubMed] [Google Scholar]
- 34.Takata Y, Ansai T, Soh I, et al. Association between body mass index and mortality in an 80-year-old population. J Am Geriatr Soc. 2007;55(6):913–917. doi: 10.1111/j.1532-5415.2007.01170.x. [DOI] [PubMed] [Google Scholar]
- 35.Stessman J, Jacobs JM, Ein-Mor E, Bursztyn M. Normal body mass index rather than obesity predicts greater mortality in elderly people: the Jerusalem Longitudinal Study. J Am Geriatr Soc. 2009;57(12):2232–2238. doi: 10.1111/j.1532-5415.2009.02567.x. [DOI] [PubMed] [Google Scholar]
- 36.Uretsky S, Supariwala A, Singh P, et al. Impact of weight on long-term survival among patients without known coronary artery disease and a normal stress SPECT MPI. J Nucl Cardiol. 2010;17(3):390–397. doi: 10.1007/s12350-010-9214-6. [DOI] [PubMed] [Google Scholar]
- 37.Keller HH, Østbye T. Body mass index (BMI), BMI change and mortality in community-dwelling seniors without dementia. J Nutr Health Aging. 2005;9(5):316–320. [PubMed] [Google Scholar]
- 38.Visscher TL, Rissanen A, Seidell JC, et al. Obesity and unhealthy life-years in adult Finns: an empirical approach. Arch Intern Med. 2004;164(13):1413–1420. doi: 10.1001/archinte.164.13.1413. [DOI] [PubMed] [Google Scholar]
- 39.Arndt V, Rothenbacher D, Zschenderlein B, Schuberth S, Brenner H. Body mass index and premature mortality in physically heavily working men—a ten-year follow-up of 20,000 construction workers. J Occup Environ Med. 2007;49(8):913–921. doi: 10.1097/JOM.0b013e31814544fe. [DOI] [PubMed] [Google Scholar]
- 40.Fontaine KR, McCubrey R, Mehta T, et al. Body mass index and mortality rate among Hispanic adults: a pooled analysis of multiple epidemiologic data sets. Int J Obes (Lond) 2012;36(8):1121–1126. doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sui X, LaMonte MJ, Laditka JN, et al. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. JAMA. 2007;298(21):2507–2516. doi: 10.1001/jama.298.21.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lubin F, Lusky A, Chetrit A, Dankner R. Lifestyle and ethnicity play a role in all-cause mortality. J Nutr. 2003;133(4):1180–1185. doi: 10.1093/jn/133.4.1180. [DOI] [PubMed] [Google Scholar]
- 43.Seccareccia F, Lanti M, Menotti A, Scanga M. Role of body mass index in the prediction of all cause mortality in over 62,000 men and women: the Italian RIFLE Pooling Project: Risk Factor and Life Expectancy. J Epidemiol Community Health. 1998;52(1):20–26. doi: 10.1136/jech.52.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hanson RL, McCance DR, Jacobsson LT, et al. The U-shaped association between body mass index and mortality: relationship with weight gain in a Native American population. J Clin Epidemiol. 1995;48(7):903–916. doi: 10.1016/0895-4356(94)00217-e. [DOI] [PubMed] [Google Scholar]
- 45.Iribarren C, Jacobs DR, Kiefe CI, et al. Causes and demographic, medical, lifestyle and psychosocial predictors of premature mortality: the CARDIA Study. Soc Sci Med. 2005;60(3):471–482. doi: 10.1016/j.socscimed.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 46.Tice JA, Kanaya A, Hue T, et al. Risk factors for mortality in middle-aged women. Arch Intern Med. 2006;166(22):2469–2477. doi: 10.1001/archinte.166.22.2469. [DOI] [PubMed] [Google Scholar]
- 47.Petursson H, Sigurdsson JA, Bengtsson C, Nilsen TI, Getz L. Body configuration as a predictor of mortality: comparison of five anthropometric measures in a 12 year follow-up of the Norwegian HUNT 2 Study. PLoS One. 2011;6(10):e26621. doi: 10.1371/journal.pone.0026621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Walter S, Kunst A, Mackenbach J, Hofman A, Tiemeier H. Mortality and disability: the effect of overweight and obesity. Int J Obes (Lond) 2009;33(12):1410–1418. doi: 10.1038/ijo.2009.176. [DOI] [PubMed] [Google Scholar]
- 49.Farrell SW, Braun L, Barlow CE, Cheng YJ, Blair SN. The relation of body mass index, cardiorespiratory fitness, and all-cause mortality in women. Obes Res. 2002;10(6):417–423. doi: 10.1038/oby.2002.58. [DOI] [PubMed] [Google Scholar]
- 50.Ferrie JE, Singh-Manoux A, Kivimäki M, et al. Cardiorespiratory risk factors as predictors of 40-year mortality in women and men. Heart. 2009;95(15):1250–1257. doi: 10.1136/hrt.2008.164251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lakoski SG, Le AH, Muntner P, et al. Adiposity, inflammation, and risk for death in black and white men and women in the United States: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. J Clin Endocrinol Metab. 2011;96(6):1805–1814. doi: 10.1210/jc.2010-3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fang X, Tang Z, Xiang M, et al. The relationship between body mass index, hypertension and all-cause mortality in the populaton over 55 year old in Beijing. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23(1):28–31. [PubMed] [Google Scholar]
- 53.Blain H, Carriere I, Sourial N, et al. Balance and walking speed predict subsequent 8-year mortality independently of current and intermediate events in well-functioning women aged 75 years and older. J Nutr Health Aging. 2010;14(7):595–600. doi: 10.1007/s12603-010-0111-0. [DOI] [PubMed] [Google Scholar]
- 54.Greenberg JA, Fontaine K, Allison DB. Putative biases in estimating mortality attributable to obesity in the US population. Int J Obes (Lond) 2007;31(9):1449–1455. doi: 10.1038/sj.ijo.0803615. [DOI] [PubMed] [Google Scholar]
- 55.Janssen I. Morbidity and mortality risk associated with an overweight BMI in older men and women. Obesity (Silver Spring) 2007;15(7):1827–1840. doi: 10.1038/oby.2007.217. [DOI] [PubMed] [Google Scholar]
- 56.Wändell PE, Carlsson AC, Theobald H. The association between BMI value and long-term mortality. Int J Obes (Lond) 2009;33(5):577–582. doi: 10.1038/ijo.2009.36. [DOI] [PubMed] [Google Scholar]
- 57.Bevilacqua MR, Gimeno SG. Abdominal obesity in Japanese-Brazilians: which measure is best for predicting all-cause and cardiovascular mortality? Cad Saude Publica. 2011;27(10):1986–1996. doi: 10.1590/s0102-311x2011001000012. [DOI] [PubMed] [Google Scholar]
- 58.Lawlor DA, Hart CL, Hole DJ, Davey Smith G. Reverse causality and confounding and the associations of overweight and obesity with mortality. Obesity (Silver Spring) 2006;14(12):2294–2304. doi: 10.1038/oby.2006.269. [DOI] [PubMed] [Google Scholar]
- 59.Osler M, Heitmann BL, Høidrup S, Jørgensen LM, Schroll M. Food intake patterns, self rated health and mortality in Danish men and women: a prospective observational study. J Epidemiol Community Health. 2001;55(6):399–403. doi: 10.1136/jech.55.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Crespo CJ, Palmieri MR, Perdomo RP, et al. The relationship of physical activity and body weight with all-cause mortality: results from the Puerto Rico Heart Health Program. Ann Epidemiol. 2002;12(8):543–552. doi: 10.1016/s1047-2797(01)00296-4. [DOI] [PubMed] [Google Scholar]
- 61.Gu D, He J, Duan X, et al. Body weight and mortality among men and women in China. JAMA. 2006;295(7):776–783. doi: 10.1001/jama.295.7.776. [DOI] [PubMed] [Google Scholar]
- 62.Faeh D, Braun J, Tarnutzer S, Bopp M. Obesity but not overweight is associated with increased mortality risk. Eur J Epidemiol. 2011;26(8):647–655. doi: 10.1007/s10654-011-9593-2. [DOI] [PubMed] [Google Scholar]
- 63.Tsai SP, Donnelly RP, Wendt JK. Obesity and mortality in a prospective study of a middle-aged industrial population. J Occup Environ Med. 2006;48(1):22–27. doi: 10.1097/01.jom.0000184866.49000.e5. [DOI] [PubMed] [Google Scholar]
- 64.Atlantis E, Browning C, Kendig H. Body mass index and unintentional weight change associated with all-cause mortality in older Australians: the Melbourne Longitudinal Studies on Healthy Ageing (MELSHA) Age Ageing. 2010;39(5):643–646. doi: 10.1093/ageing/afq073. [DOI] [PubMed] [Google Scholar]
- 65.Cabrera MA, Wajngarten M, Gebara OC, Diament J. Relationship between body mass index, waist circumference, and waist-to-hip ratio and mortality in elderly women: a 5-year follow-up study. Cad Saude Publica. 2005;21(3):767–775. doi: 10.1590/s0102-311x2005000300010. [DOI] [PubMed] [Google Scholar]
- 66.Janssen I, Bacon E. Effect of current and midlife obesity status on mortality risk in the elderly. Obesity (Silver Spring) 2008;16(11):2504–2509. doi: 10.1038/oby.2008.400. [DOI] [PubMed] [Google Scholar]
- 67.Jonsson S, Hedblad B, Engström G, Nilsson P, Berglund G, Janzon L. Influence of obesity on cardiovascular risk: twenty-three-year follow-up of 22,025 men from an urban Swedish population. Int J Obes Relat Metab Disord. 2002;26(8):1046–1053. doi: 10.1038/sj.ijo.0802060. [DOI] [PubMed] [Google Scholar]
- 68.McTigue K, Larson JC, Valoski A, et al. Mortality and cardiac and vascular outcomes in extremely obese women. JAMA. 2006;296(1):79–86. doi: 10.1001/jama.296.1.79. [DOI] [PubMed] [Google Scholar]
- 69.Miller MD, Crotty M, Giles LC, et al. Corrected arm muscle area: an independent predictor of long-term mortality in community-dwelling older adults? J Am Geriatr Soc. 2002;50(7):1272–1277. doi: 10.1046/j.1532-5415.2002.50316.x. [DOI] [PubMed] [Google Scholar]
- 70.Batty GD, Shipley MJ, Jarrett RJ, Breeze E, Marmot MG, Davey Smith G. Obesity and overweight in relation to disease-specific mortality in men with and without existing coronary heart disease in London: the original Whitehall Study. Heart. 2006;92(7):886–892. doi: 10.1136/hrt.2005.072637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gale CR, Martyn CN, Cooper C, Sayer AA. Grip strength, body composition, and mortality. Int J Epidemiol. 2007;36(1):228–235. doi: 10.1093/ije/dyl224. [DOI] [PubMed] [Google Scholar]
- 72.Visscher TL, Seidell JC, Menotti A, et al. Underweight and overweight in relation to mortality among men aged 40–59 and 50–69 years: the Seven Countries Study. Am J Epidemiol. 2000;151(7):660–666. doi: 10.1093/oxfordjournals.aje.a010260. [DOI] [PubMed] [Google Scholar]
- 73.Baldinger B, Schwarz C, Jaggy C. Cardiovascular risk factors, BMI and mortality in a cohort of Swiss males (1976–2001) with high-sum-assured life insurance cover. J Insur Med. 2006;38(1):44–53. [PubMed] [Google Scholar]
- 74.Katzmarzyk PT, Reeder BA, Elliott S, et al. Body mass index and risk of cardiovascular disease, cancer and all-cause mortality. Can J Public Health. 2012;103(2):147–151. doi: 10.1007/BF03404221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ioachimescu AG, Brennan DM, Hoar BM, Hoogwerf BJ. The lipid accumulation product and all-cause mortality in patients at high cardiovascular risk: a PreCIS database study. Obesity (Silver Spring) 2010;18(9):1836–1844. doi: 10.1038/oby.2009.453. [DOI] [PubMed] [Google Scholar]
- 76.Heir T, Erikssen J, Sandvik L. Overweight as predictor of long-term mortality among healthy, middle-aged men: a prospective cohort study. Prev Med. 2011;52(3–4):223–226. doi: 10.1016/j.ypmed.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 77.Katzmarzyk PT, Craig CL, Bouchard C. Original article underweight, overweight and obesity: relationships with mortality in the 13-year follow-up of the Canada Fitness Survey. J Clin Epidemiol. 2001;54(9):916–920. doi: 10.1016/s0895-4356(01)00356-0. [DOI] [PubMed] [Google Scholar]
- 78.Cesari M, Pahor M, Lauretani F, et al. Skeletal muscle and mortality results from the InCHIANTI Study. J Gerontol A Biol Sci Med Sci. 2009;64(3):377–384. doi: 10.1093/gerona/gln031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Arnlöv J, Ingelsson E, Sundström J, Lind L. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation. 2010;121(2):230–236. doi: 10.1161/CIRCULATIONAHA.109.887521. [DOI] [PubMed] [Google Scholar]
- 80.Tsai SP, Wen CP, Chan HT, Chiang PH, Tsai MK, Cheng TY. The effects of pre-disease risk factors within metabolic syndrome on all-cause and cardiovascular disease mortality. Diabetes Res Clin Pract. 2008;82(1):148–156. doi: 10.1016/j.diabres.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 81.Locher JL, Roth DL, Ritchie CS, et al. Body mass index, weight loss, and mortality in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2007;62(12):1389–1392. doi: 10.1093/gerona/62.12.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Taylor DH, Jr, Ostbye T. The effect of middle- and old-age body mass index on short-term mortality in older people. J Am Geriatr Soc. 2001;49(10):1319–1326. doi: 10.1046/j.1532-5415.2001.49259.x. [DOI] [PubMed] [Google Scholar]
- 83.Monteverde M, Noronha K, Palloni A, Novak B. Obesity and excess mortality among the elderly in the United States and Mexico. Demography. 2010;47(1):79–96. doi: 10.1353/dem.0.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, Ron E. The mortality risk of smoking and obesity combined. Am J Prev Med. 2006;31(5):355–362. doi: 10.1016/j.amepre.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 85.Majer IM, Nusselder WJ, Mackenbach JP, Kunst AE. Life expectancy and life expectancy with disability of normal weight, overweight, and obese smokers and nonsmokers in Europe. Obesity (Silver Spring) 2011;19(7):1451–1459. doi: 10.1038/oby.2011.46. [DOI] [PubMed] [Google Scholar]
- 86.Jerant A, Franks P. Body mass index, diabetes, hypertension, and short-term mortality: a population-based observational study, 2000–2006. J Am Board Fam Med. 2012;25(4):422–431. doi: 10.3122/jabfm.2012.04.110289. [DOI] [PubMed] [Google Scholar]
- 87.Strawbridge WJ, Wallhagen MI, Shema SJ. New NHLBI clinical guidelines for obesity and overweight: will they promote health? Am J Public Health. 2000;90(3):340–343. doi: 10.2105/ajph.90.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ford J, Spallek M, Dobson A. Self-rated health and a healthy lifestyle are the most important predictors of survival in elderly women. Age Ageing. 2008;37(2):194–200. doi: 10.1093/ageing/afm171. [DOI] [PubMed] [Google Scholar]
- 89.Niedhammer I, Bourgkard E, Chau N Lorhandicap Study Group. Occupational and behavioural factors in the explanation of social inequalities in premature and total mortality: a 12.5-year follow-up in the Lorhandicap Study. Eur J Epidemiol. 2011;26(1):1–12. doi: 10.1007/s10654-010-9506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Haapanen-Niemi N, Miilunpalo S, Pasanen M, Vuori I, Oja P, Malmberg J. Body mass index, physical inactivity and low level of physical fitness as determinants of all-cause and cardiovascular disease mortality—16 y follow-up of middle-aged and elderly men and women. Int J Obes Relat Metab Disord. 2000;24(11):1465–1474. doi: 10.1038/sj.ijo.0801426. [DOI] [PubMed] [Google Scholar]
- 91.Boggs DA, Rosenberg L, Cozier YC, et al. General and abdominal obesity and risk of death among black women. N Engl J Med. 2011;365(10):901–908. doi: 10.1056/NEJMoa1104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of US adults. Soc Sci Med. 2010;70(10):1558–1566. doi: 10.1016/j.socscimed.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ma J, Flanders WD, Ward EM, Jemal A. Body mass index in young adulthood and premature death: analyses of the US National Health Interview Survey linked mortality files. Am J Epidemiol. 2011;174(8):934–944. doi: 10.1093/aje/kwr169. [DOI] [PubMed] [Google Scholar]
- 94.Zunzunegui MV, Sanchez MT, Garcia A, Casado JM, Otero A. Body mass index and long-term mortality in an elderly Mediterranean population. J Aging Health. 2012;24(1):29–47. doi: 10.1177/0898264311408419. [DOI] [PubMed] [Google Scholar]
- 95.Nagai M, Kuriyama S, Kakizaki M, et al. Impact of obesity, overweight and underweight on life expectancy and lifetime medical expenditures: the Ohsaki Cohort Study. BMJ Open. 2012;2(3) doi: 10.1136/bmjopen-2012-000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fujino Y Japan Collaborative Cohort Study for Evaluation of Cancer. Anthropometry, development history and mortality in the Japan Collaborative Cohort Study for Evaluation of Cancer ( JACC) Asian Pac J Cancer Prev. 2007;8(suppl):105–112. [PubMed] [Google Scholar]
- 97.Corrada MM, Kawas CH, Mozaffar F, Paganini-Hill A. Association of body mass index and weight change with all-cause mortality in the elderly. Am J Epidemiol. 2006;163(10):938–949. doi: 10.1093/aje/kwj114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yates LB, Djoussé L, Kurth T, Buring JE, Gaziano JM. Exceptional longevity in men: modifiable factors associated with survival and function to age 90 years. Arch Intern Med. 2008;168(3):284–290. doi: 10.1001/archinternmed.2007.77. [DOI] [PubMed] [Google Scholar]
- 99.Iversen L, Hannaford PC, Lee AJ, Elliott AM, Fielding S. Impact of lifestyle in middle-aged women on mortality: evidence from the Royal College of General Practitioners’ Oral Contraception Study. Br J Gen Pract. 2010;60(577):563–569. doi: 10.3399/bjgp10X515052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Leitzmann MF, Moore SC, Koster A, et al. Waist circumference as compared with body-mass index in predicting mortality from specific causes. PLoS One. 2011;6(4):e18582. doi: 10.1371/journal.pone.0018582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ringbäck Weitoft G, Eliasson M, Rosén M. Underweight, overweight and obesity as risk factors for mortality and hospitalization. Scand J Public Health. 2008;36(2):169–176. doi: 10.1177/1403494807085080. [DOI] [PubMed] [Google Scholar]
- 102.Bessonova L, Marshall SF, Ziogas A, et al. The association of body mass index with mortality in the California Teachers Study. Int J Cancer. 2011;129(10):2492–2501. doi: 10.1002/ijc.25905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gray L, Hart CL, Smith GD, Batty GD. What is the predictive value of established risk factors for total and cardiovascular disease mortality when measured before middle age? pooled analyses of two prospective cohort studies from Scotland. Eur J Cardiovasc Prev Rehabil. 2010;17(1):106–112. doi: 10.1097/HJR.0b013e3283348ed9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Stevens J, Cai J, Juhaeri, Thun MJ, Wood JL. Evaluation of WHO and NHANES II standards for overweight using mortality rates. J Am Diet Assoc. 2000;100(7):825–827. doi: 10.1016/s0002-8223(00)00238-8. [DOI] [PubMed] [Google Scholar]
- 105.van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ. 2008;337:a1440. doi: 10.1136/bmj.a1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gelber RP, Kurth T, Manson JE, Buring JE, Gaziano JM. Body mass index and mortality in men: evaluating the shape of the association. Int J Obes (Lond) 2007;31(8):1240–1247. doi: 10.1038/sj.ijo.0803564. [DOI] [PubMed] [Google Scholar]
- 107.Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Decreased muscle mass and increased central adiposity are independently related to mortality in older men. Am J Clin Nutr. 2007;86(5):1339–1346. doi: 10.1093/ajcn/86.5.1339. [DOI] [PubMed] [Google Scholar]
- 108.Suadicani P, Hein HO, von Eyben FE, Gyntelberg F. Metabolic and lifestyle predictors of ischemic heart disease and all-cause mortality among normal weight, overweight, and obese men: a 16-year follow-up in the Copenhagen Male Study. Metab Syndr Relat Disord. 2009;7(2):97–104. doi: 10.1089/met.2008.0041. [DOI] [PubMed] [Google Scholar]
- 109.Seidell JC, Verschuren WM, van Leer EM, Kromhout D. Overweight, underweight, and mortality: a prospective study of 48,287 men and women. Arch Intern Med. 1996;156(9):958–963. doi: 10.1001/archinte.156.9.958. [DOI] [PubMed] [Google Scholar]
- 110.Sonestedt E, Gullberg B, Ericson U, Wirfält E, Hedblad B, Orho-Melander M. Association between fat intake, physical activity and mortality depending on genetic variation in FTO. Int J Obes (Lond) 2011;35(8):1041–1049. doi: 10.1038/ijo.2010.263. [DOI] [PubMed] [Google Scholar]
- 111.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 112.Public Health Agency of Canada and the Canadian Institute for Health Information. [Accessibility verified December 6, 2012];Obesity in Canada: a joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information. http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/oic-oac/assets/pdf/oic-oac-eng.pdf.
- 113.National Health Service Information Centre. [Accessed April 9, 2012];Health survey for England: 2010 trend tables. http://www.ic.nhs.uk/pubs/hse10trends.
- 114.McGee DL Diverse Populations Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15(2):87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 115.Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev. 2007;8(1):41–59. doi: 10.1111/j.1467-789X.2006.00248.x. [DOI] [PubMed] [Google Scholar]
- 116.Carnethon MR, De Chavez PJ, Biggs ML, et al. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012;308(6):581–590. doi: 10.1001/jama.2012.9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 118.Doehner W, Clark A, Anker SD. The obesity paradox: weighing the benefit. Eur Heart J. 2010;31(2):146–148. doi: 10.1093/eurheartj/ehp339. [DOI] [PubMed] [Google Scholar]
- 119.Lainscak M, von Haehling S, Doehner W, Anker SD. The obesity paradox in chronic disease: facts and numbers. J Cachexia Sarcopenia Muscle. 2012;3(1):1–4. doi: 10.1007/s13539-012-0059-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Oreopoulos A, McAlister FA, Kalantar-Zadeh K, et al. The relationship between body mass index, treatment, and mortality in patients with established coronary artery disease: a report from APPROACH. Eur Heart J. 2009;30(21):2584–2592. doi: 10.1093/eurheartj/ehp288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chang VW, Asch DA, Werner RM. Quality of care among obese patients. JAMA. 2010;303(13):1274–1281. doi: 10.1001/jama.2010.339. [DOI] [PubMed] [Google Scholar]
- 122.Schenkeveld L, Magro M, Oemrawsingh RM, et al. The influence of optimal medical treatment on the “obesity paradox,” body mass index and long-term mortality in patients treated with percutaneous coronary intervention: a prospective cohort study. BMJ Open. 2012;2:e000535. doi: 10.1136/bmjopen-2011-000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Steinberg BA, Cannon CP, Hernandez AF, Pan W, Peterson ED, Fonarow GC. Medical therapies and invasive treatments for coronary artery disease by body mass: the “obesity paradox” in the Get With The Guidelines database. Am J Cardiol. 2007;100(9):1331–1335. doi: 10.1016/j.amjcard.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 124.Hastie CE, Padmanabhan S, Slack R, et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Eur Heart J. 2010;31(2):222–226. doi: 10.1093/eurheartj/ehp317. [DOI] [PubMed] [Google Scholar]
- 125.Auyeung TW, Lee JS, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese—a 5-year follow-up study in 4,000 older adults using DXA. J Gerontol A Biol Sci Med Sci. 2010;65(1):99–104. doi: 10.1093/gerona/glp099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Manson JE, Stampfer MJ, Hennekens CH, Willett WC. Body weight and longevity: a reassessment. JAMA. 1987;257(3):353–358. [PubMed] [Google Scholar]
- 127.Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutr J. 2005;4:27. doi: 10.1186/1475-2891-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nyholm M, Gullberg B, Merlo J, Lundqvist-Persson C, Råstam L, Lindblad U. The validity of obesity based on self-reported weight and height: implications for population studies. Obesity (Silver Spring) 2007;15(1):197–208. doi: 10.1038/oby.2007.536. [DOI] [PubMed] [Google Scholar]
- 129.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002;5(4):561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- 130.Plankey MW, Stevens J, Flegal KM, Rust PF. Prediction equations do not eliminate systematic error in self-reported body mass index. Obes Res. 1997;5(4):308–314. doi: 10.1002/j.1550-8528.1997.tb00556.x. [DOI] [PubMed] [Google Scholar]
- 131.Chiolero A, Peytremann-Bridevaux I, Paccaud F. Associations between obesity and health conditions may be overestimated if self-reported body mass index is used. Obes Rev. 2007;8(4):373–374. doi: 10.1111/j.1467-789X.2007.00375.x. [DOI] [PubMed] [Google Scholar]
- 132.He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353(11):1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 133.Hahn S, Williamson PR, Hutton JL, Garner P, Flynn EV. Assessing the potential for bias in meta-analysis due to selective reporting of subgroup analyses within studies. Stat Med. 2000;19(24):3325–3336. doi: 10.1002/1097-0258(20001230)19:24<3325::aid-sim827>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 134.Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine—reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357(21):2189–2194. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- 135.Cohen SS, Signorello LB, Cope EL, et al. Obesity and all-cause mortality among black adults and white adults. Am J Epidemiol. 2012;176(5):431–442. doi: 10.1093/aje/kws032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ioannidis JP. Why most discovered true associations are inflated. Epidemiology. 2008;19(5):640–648. doi: 10.1097/EDE.0b013e31818131e7. [DOI] [PubMed] [Google Scholar]
- 137.Welch HG, Schwartz LM, Woloshin S. The exaggerated relations between diet, body weight and mortality: the case for a categorical data approach. CMAJ. 2005;172(7):891–895. doi: 10.1503/cmaj.1041310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Frøslie KF, Røislien J, Laake P, Henriksen T, Qvigstad E, Veierød MB. Categorisation of continuous exposure variables revisited: a response to the Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) Study. BMC Med Res Methodol. 2010;10:103. doi: 10.1186/1471-2288-10-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.