Abstract
Endoscopic ultrasound (EUS) of the mediastinum was pioneered by gastroenterologists, and it was taken up by pulmonologists when the smaller-diameter endobronchial ultrasound (EBUS) scope was designed after a few years. The pulmonologists’ approach remained largely confined to entry from the trachea, but they soon realized that the esophagus was an alternative route of entry by the EBUS scope. The new generations of interventionists are facing the challenge of learning two techniques (EUS and EBUS) from two routes (esophagus and trachea). The International Association for the Study of Lung Cancer (IASLC) proposed a classification of mediastinal lymph nodes at different stations that lie within the boundaries of specific spaces. These interventionists need clear definitions of landmarks and clear techniques to identify the spaces. There are enough descriptions of spaces of the neck and the mediastinum in the literature, yet the topic mentioned above has never been discussed separately. The anatomical structures, landmarks, and boundaries of spaces will be important to interventionists in the near future during performances of endosonography. This article combines the baseline anatomy of the spaces with the actual imaging during EUS.
KEY WORDS: Endoscopic ultrasound, mediastinum, neck, spaces
BACKGROUND
The neck and the mediastinum contain a number of connective tissue spaces that are continuous with each other. These spaces have no universally accepted nomenclature or boundaries.[1] The available descriptions of spaces in the neck are generally with relation to layers of fascia.[2] The mediastinum has no limiting fascial layers like the neck, and the spaces of mediastinum are generally described with relation to the trachea.[3] Clinicians need to know about these spaces as they are potential pathways for the spread of disease and contain normal, regional, or metastatic lymph nodes.[4,5] Each malignancy has its unique first echelon and pattern of spread to different nodal stations.[6] Proper staging of diseased lymph nodes at different stations is possible by computed tomography (CT), positron emission tomography (PET), and PET-CT.[4,7] Ultrasonography (US) also assumes importance in the routine diagnosis, treatment, and follow-up of diseases of the head, neck, and chest.[8,9,10,11] Imaging of hollow organs by endoscopic ultrasound (EUS) and EUS-guided fine-needle aspiration cytology (FNAC) has improved accuracy in the assessment of local lymph node metastases in malignancies of the neck, esophagus, and lung when compared with CT.[12,13,14] Currently, EUS is increasingly used in the evaluation of metastatic disease, posttreatment assessment, and the detection of recurrent disease, and it offers a distinct advantage in EUS-FNAC of lymph nodes or masses that are not accessible to CT.[15,16,17]
Anatomical knowledge of the spaces of the neck and mediastinum can help in EUS examination from the pharynx and esophagus. This article describes the normal EUS anatomy of the neck and mediastinum.
PROCEDURE
Applied anatomy of spaces of neck
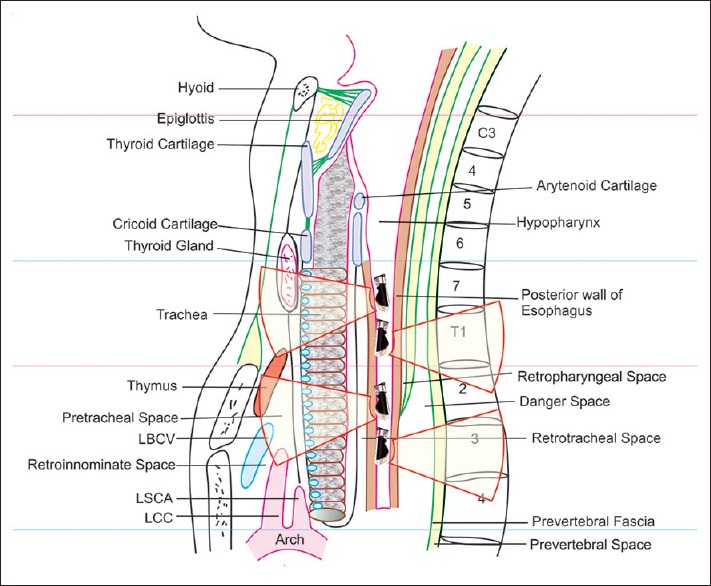
The pharynx extends from the base of the skull to the level of cricoid cartilage (C6), and the esophagus extends from the lower margin of cricoid cartilage to the abdomen (T11) [Figure 1]. The neck is generally subdivided into the suprahyoid and infrahyoid regions by the hyoid bone. The deep neck spaces (submandibular space, sublingual space, parotid space, parapharyngeal space, and masticator space) are present only in the suprahyoid region. Visceral space, anterior cervical space, and posterior cervical space are present only in the infrahyoid region.[2] The carotid, retropharyngeal, perivertebral, and danger spaces extend up to the base of the skull and are present in both the suprahyoid and infrahyoid regions [Figure 1]. The infrahyoid region of the neck can be evaluated through the anterior lateral or posterior wall of the pharynx and esophagus by EUS [Figure 2].
Figure 1.
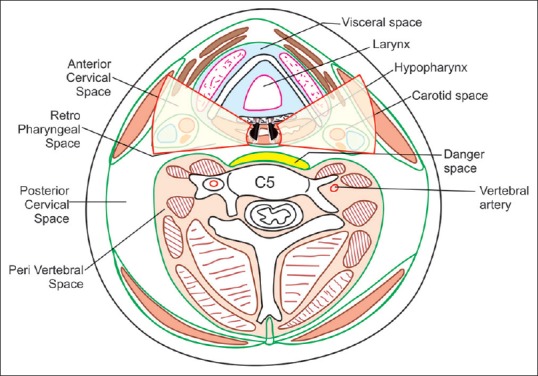
The spaces in the neck are formed from the three layers of cervical fascia, i.e., a superficial, a pretracheal, and a prevertebral layer. The superficial layer surrounds all the important structures in the neck, the prevertebral layer surrounds the vertebral column and the nearby muscles, and the pretracheal layer forms a visceral compartment around the trachea and esophagus. On either side of the cervical esophagus are the carotid spaces, and behind are the retropharyngeal and perivertebral spaces. The anterior and posterior cervical space lie anterior and posterior to the carotid space
Figure 2.
EUS through the anterior and lateral wall of the esophagus allows examination of visceral, carotid, anterior cervical, and posterior cervical spaces. EUS through the posterior esophageal wall allows the examination of retropharyngeal (retroesophageal), danger, and prevertebral spaces
The anterior cervical space is a paired space lying lateral to the visceral space and anterior to the carotid space in the anterior triangle of the neck deep to the sternocleidomastoid muscle [Figures 3 and 4]
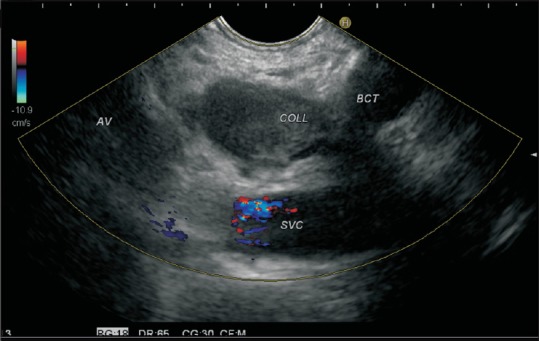
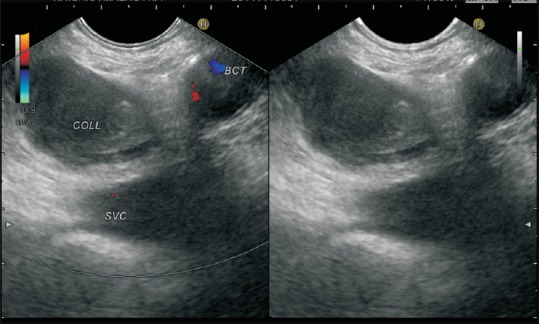
The posterior cervical space is a paired, adipose-tissue space located posterior to the sternocleidomastoid muscle in the lower part of the posterior triangle (supraclavicular triangle) of the neck [Figures 5–8]
The visceral space is a median space delimited anterolaterally by the anterior cervical space, posterolaterally by the carotid space, and posteriorly by the retropharyngeal space [Figures 9 and 10][18]
The carotid space is a paired space containing the main neurovascular bundle of the neck including the common carotid artery, the internal carotid artery, and the internal jugular vein [Figures 11–13]
The retropharyngeal (retroesophageal space) is a median space present behind the pharynx and cervical esophagus. The retropharyngeal space extends to the level of C6 in the upper neck and the retroesophageal space extends to the lower neck and the posterior mediastinum up to the level of T2 vertebra [Figure 14]
The danger space is a potential median space between the alar and prevertebral layers of the deep cervical fascia, which extends downward throughout the thorax. It contains no lymph nodes
The perivertebral space is encased by the prevertebral layer of deep cervical fascia and is subdivided into a median prevertebral space in front of the vertebrae and paraspinal spaces on either side of the vertebrae [Figures 15 and 16] [Table 1].
Figure 3.
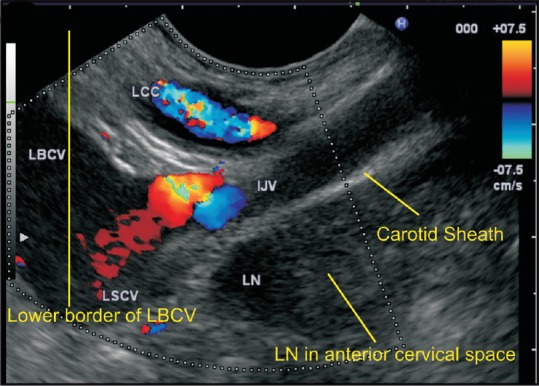
A lymph node is seen in the lowermost part of the supraclavicular fossa belonging to the lower jugular group. This lies in the anterior cervical space anterior to the carotid sheath
Figure 4.
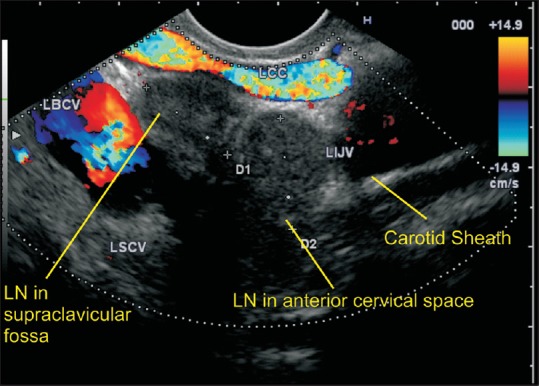
A lymph node is seen in the lowermost part of the neck belonging to the lower jugular group of lymph nodes both anterior and posterior to the carotid sheath. The lymph node in the supraclavicular fossa lies in the posterior cervical space
Figure 5.
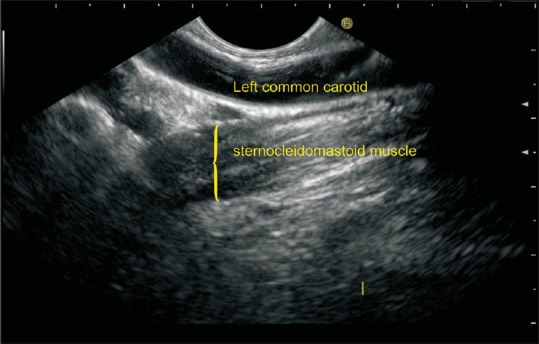
The left common carotid artery lies in the carotid sheath in anterolateral relation to the esophagus, and the sternocleidomastoid muscle lies beyond the carotid sheath
Figure 8.
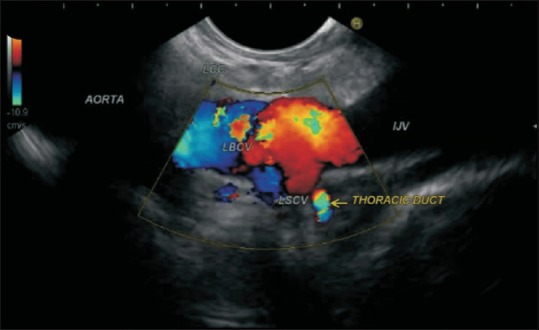
The thoracic duct is seen joining the junction of the left brachiocephalic vein with the left subclavian vein in the posterior cervical space
Figure 9.
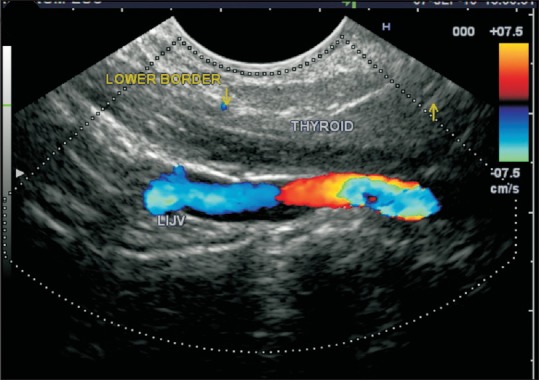
The thyroid gland is seen in the visceral space. The internal jugular vein is seen in the carotid sheath beyond the thyroid gland
Figure 10.
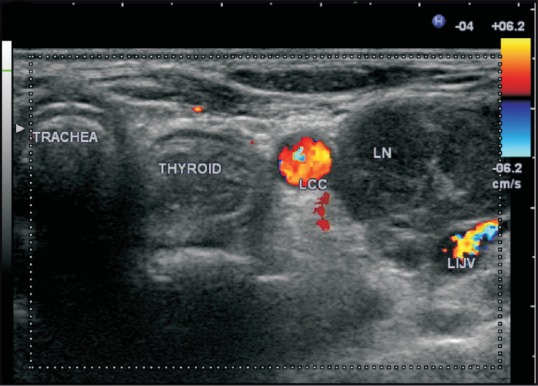
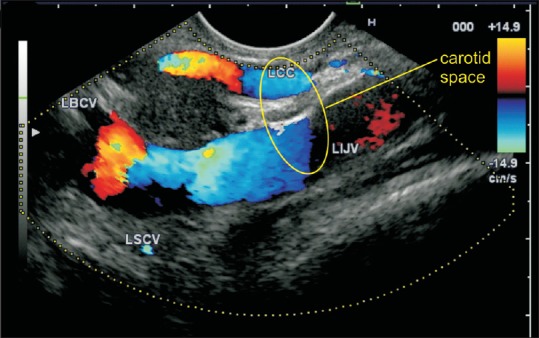
Anterior (central) compartment group VI lymph nodes include the pre- and paratracheal nodes, the precricoid (Delphian) node, and the perithyroidal nodes. A transverse section of ultrasound from the neck shows the thyroid gland and a lymph node lateral to thyroid gland between the LCC and LIJV. LCC = Left common carotid, LIJV = Left internal jugular vein
Figure 11.
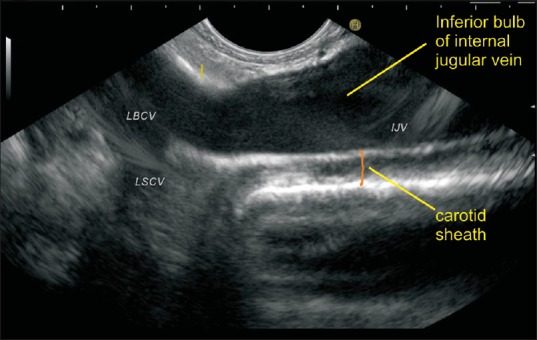
The carotid sheath is made of contributions from pretracheal, precervical, and superficial fascia. The union of the two veins is seen in the base of the neck, and the dilated lower part of the internal jugular vein is called the inferior bulb
Figure 13.
The carotid sheath in the neck includes the internal jugular vein and the common carotid artery. In this case, lymph nodes are seen within the carotid sheath
Figure 14.
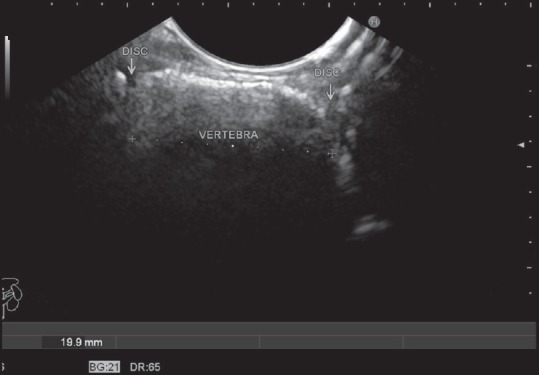
The alternating pattern of hyperechoic spine and hypoechoic intervertebral disc can be traced all the way to the base of the skull by a pullout along the posterior wall of the esophagus and pharynx
Figure 15.
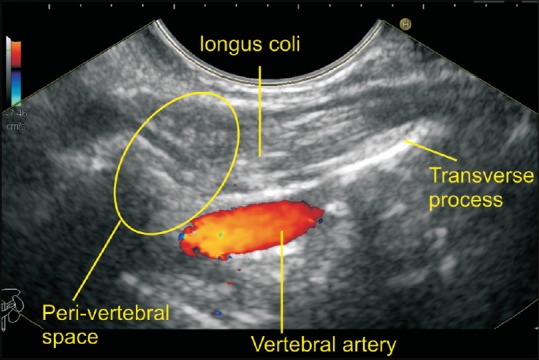
The vertebral artery is seen in the areas between the two adjacent transverse processes of vertebrae. The longus colli muscle is seen between the probe and the vertebral artery
Figure 16.
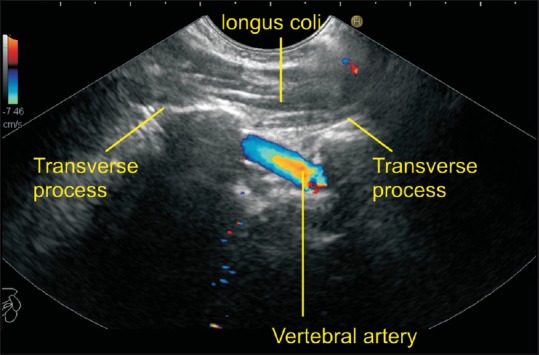
The longus colli muscle is seen in the paravertebral area. The transverse processes interrupt the visualization of the entire course of the artery
Table 1.
Spaces in infrahyoid region of neck
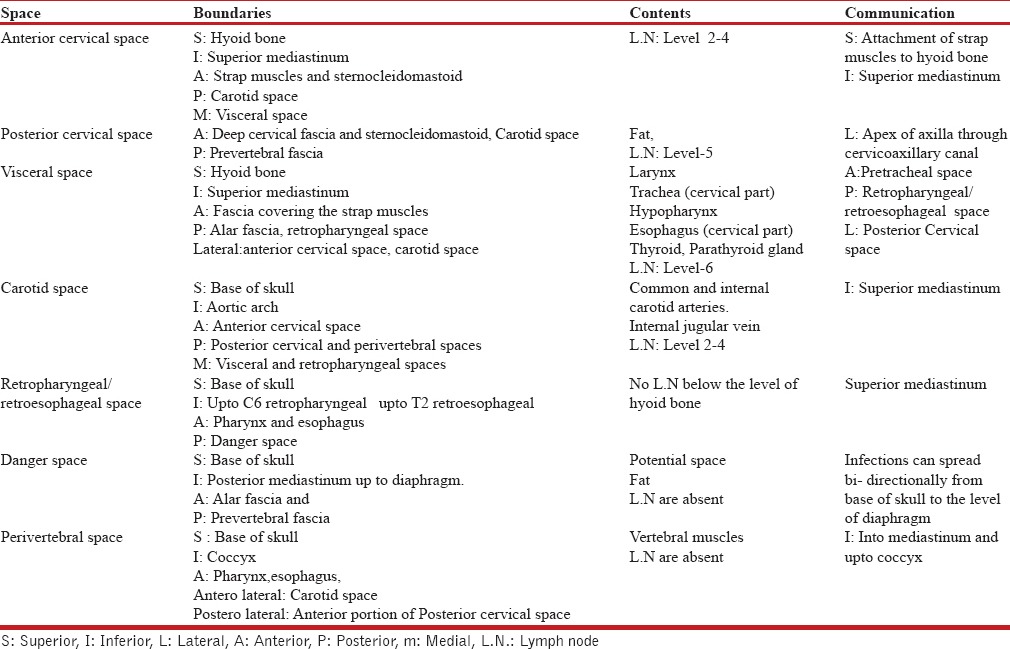
Figure 6.
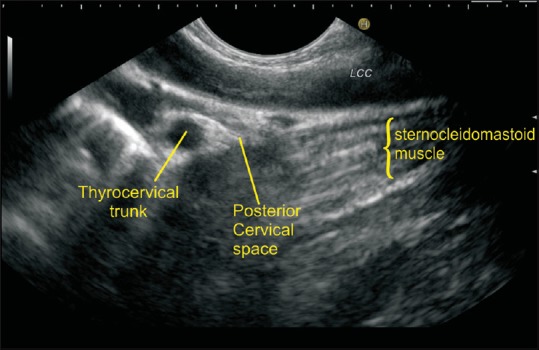
The thyrocervical trunk is a branch of the first portion of the subclavian artery arising between the origin of the subclavian artery and the inner border of the scalenus anterior muscle. The thyrocervical trunk is located in the supraclavicular fossa in the posterior cervical space surrounded by hyperechoic adipose tissue
Figure 7.
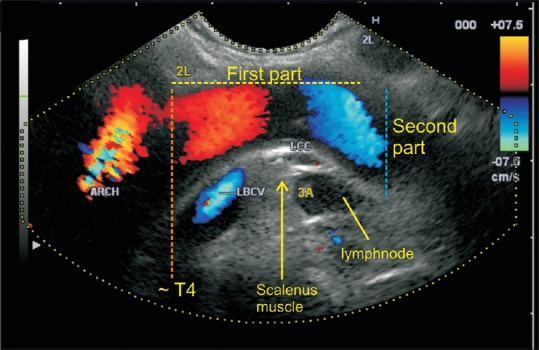
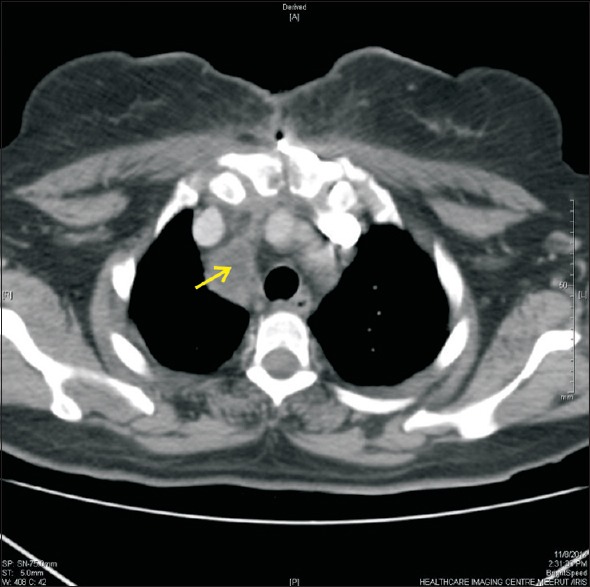
The left subclavian artery arises from the arch of the aorta at the level of the T4 vertebra (orange dotted line). The scalenus anterior (SA) muscle (yellow arrow) divides this artery into three parts. The first part extends from the origin to the medial border of the SA and ascends in the superior mediastinal cavity to the root of the neck (yellow dotted line). The second part lies behind the SA, forms the highest part of the arch, and arches laterally (blue dotted line). A lymph node belonging to station 3a (by IASLC classification) is seen lying in the prevascular space
Figure 12.
A union of the left subclavian vein and the left internal jugular vein is seen. This union lies in the cervical part of the mediastinum anterior to the cupola. The left subclavian vein arches upward and reaches almost to the lower boundary of the supraclavicular triangle. The area above the subclavian vein can be considered the supraclavicular triangle, whereas the internal jugular vein enters the carotid sheath within the carotid triangle
Applied anatomy of spaces of mediastinum
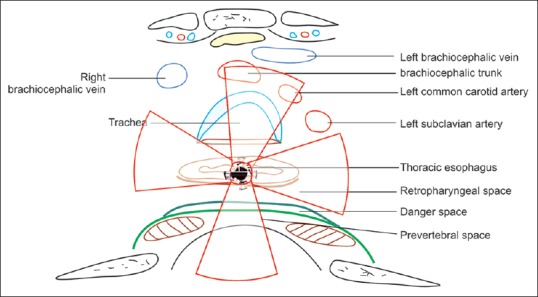
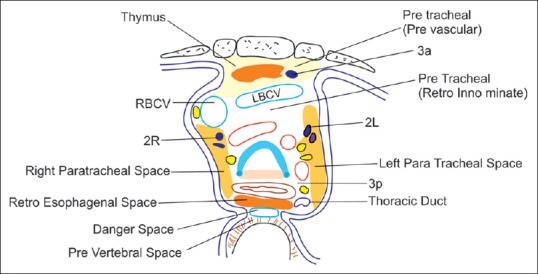
The esophagus is divided into the cervical and thoracic portions. The cervical esophagus ends at the thoracic inlet. The rest of the esophagus is divided into three regions.[12] The upper thoracic portion extends from the thoracic inlet to the carina, the midthoracic portion extends from the carina to esophageal hiatus of the diaphragm, and the lower esophagus includes the intraabdominal esophagus and the gastroesophageal junction.[1] The heart and major vessels divide the mediastinum into central and anterior zones.[19] CT images obtained after pneumomediastinography have also demonstrated several compartments of the mediastinum where spread of gas occurs from one space to another [Figure 17].[3,20] Different methods of imaging of the posterior mediastinum have been described and standard techniques of imaging of the different lymph node stations have been described by the International Association for the Study of Lung Cancer (IASLC).[21,22,23,24,25] The mediastinal spaces are described in this article as having boundaries, but in reality they are all continuous with each other directly or indirectly [Tables 2 and 3].
Figure 17.
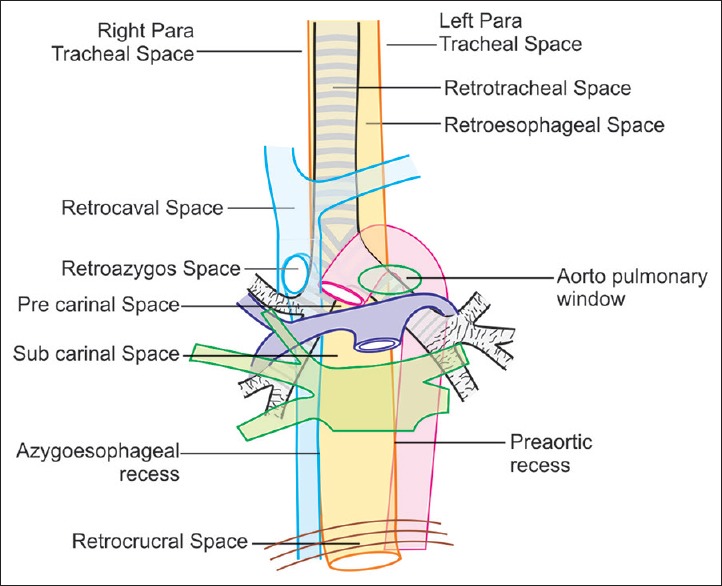
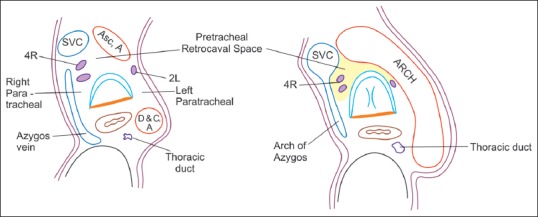
A coronal view of spaces around trachea and esophagus is seen. The trachea and esophagus divide the central zone of the mediastinum into left-sided and right-sided compartments. The tracheal bifurcation and the main bronchi divide the central zone into supracarinal and subcarinal areas. The spaces in the supracarinal area include the paratracheal spaces (on the right and left sides of the upper trachea), the pretracheal space, the AP window, and the retrotracheal space. The spaces in the subcarinal areas include the precarinal and the subcarinal spaces in continuity with the azygoesophageal and preaortic recesses
Table 2.
Spaces Anterior, lateral and posterior to trachea
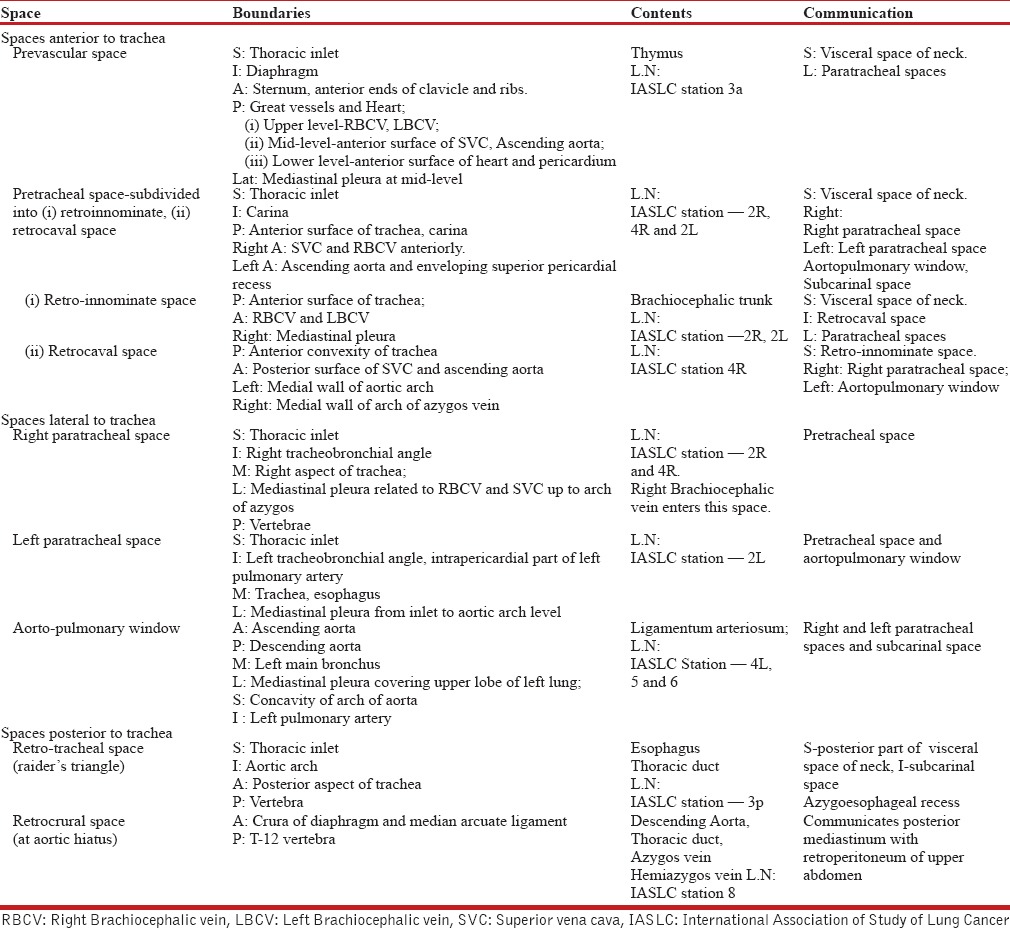
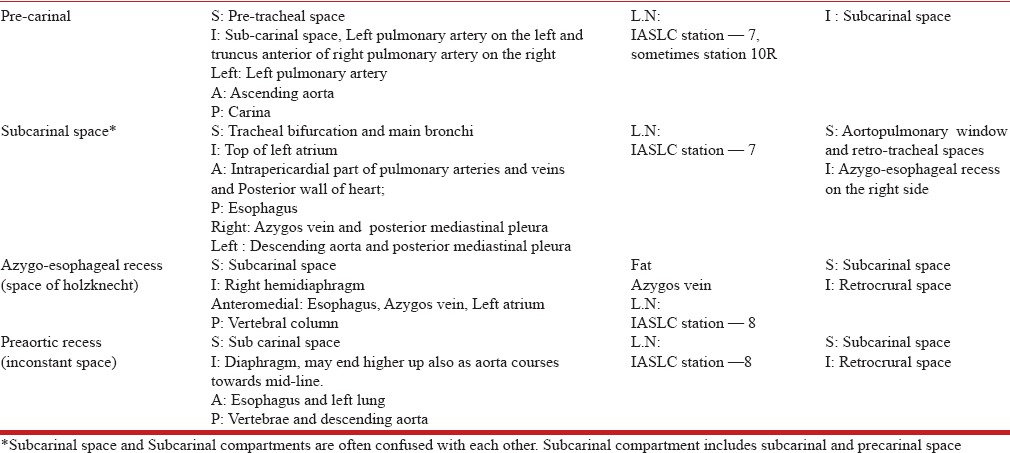
Table 3.
Spaces below trachea
Spaces anterior to trachea
The pretracheal space lies in front of trachea and has been subdivided into the retroinnominate and retrocaval spaces [Figures 18–20].[26] The pretracheal spaces are generally retrovascular in location.
Prevascular space (anterior junctional area) represents the junction areas where the two lungs approximate each other and by the apposition of the visceral and parietal pleura of the lungs with intervening mediastinal fat.[25] The anterior junctional area lies anterosuperior to the aorta and pulmonary artery and is also known as the prevascular space. The anterior junction area cannot be seen by EUS. The thymus lies in this space.
Figure 18.
A cross-sectional view of spaces around the trachea
Figure 20.
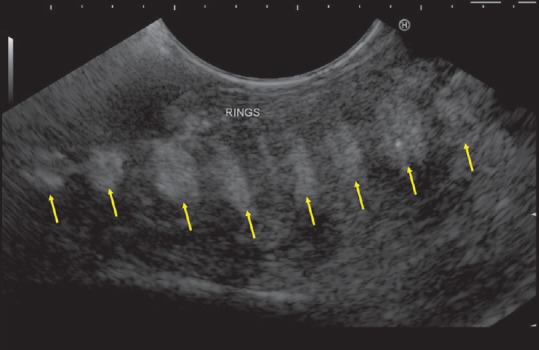
On a clockwise rotation to either side the rings of the trachea can be more easily appreciated (yellow arrows). The pretracheal space lies in front of the trachea and may be difficult to visualize by EUS; a transcutaneous ultrasound can give more information
Figure 19.
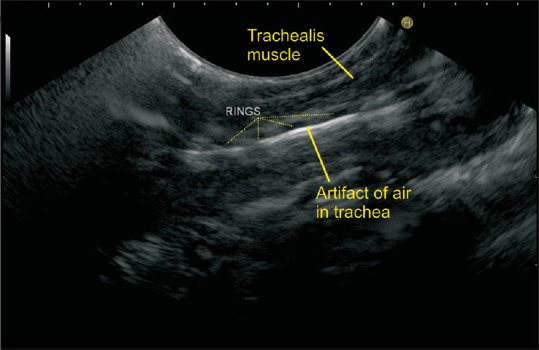
It is difficult to see the pretracheal space because of air in the trachea, which lies in front of the esophagus, and the presence of air in the trachea creates reverberation artifacts. The sound waves are transmitted through the trachealis muscle, which lies in the posterior wall of the trachea
Spaces lateral to trachea
The right paratracheal space is wider than the left and becomes gradually narrower as it goes down toward the tracheal bifurcation [Figures 21–26].
The left paratracheal space lies to the left of the trachea and the esophagus. In a thin patient, the left paratracheal space is narrow and becomes broader as it goes down, particularly at the level of the aortopulmonary window [Figures 27–29].
The aortopulmonary window is specifically called a window (and not space), and it is created by the formation of an aortic arch over the left pulmonary artery in the left paratracheal region [Figures 30–34].
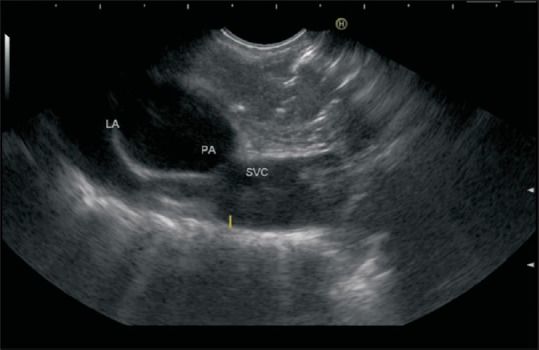
Figure 21.
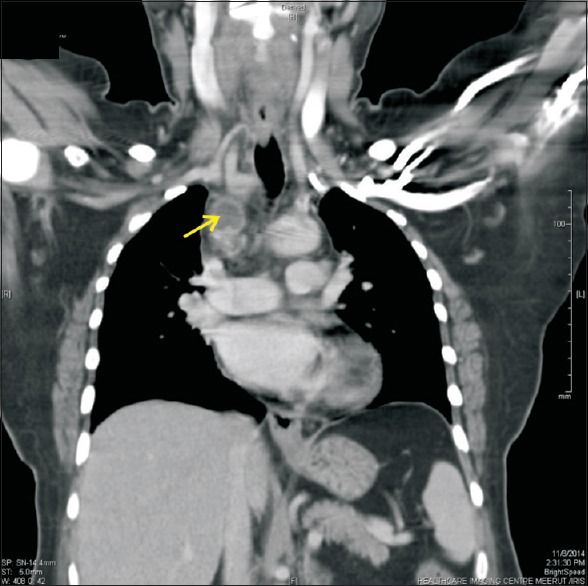
A follow-up case of large retrosternal thyroid goiter who underwent excision developed fever and retrosternal chest pain radiating to the right shoulder. CT coronal scan revealed a small, hypodense peripherally enhancing collection of 32 × 33 mm2 size in the right paratracheal region abutting the SVC
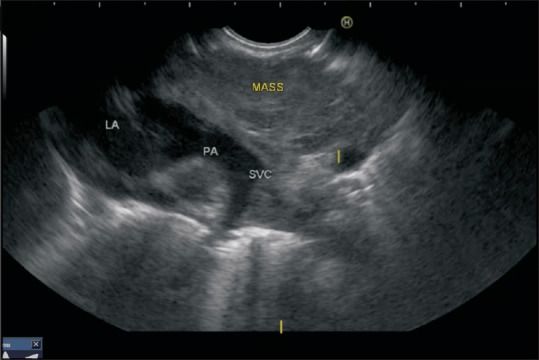
Figure 26.
In this case, the union of the azygos vein with SVC is seen and a mass is seen between the azygos vein and the union of SVC
Figure 27.
This figure shows the continuity of spaces around the trachea with each other
Figure 29.
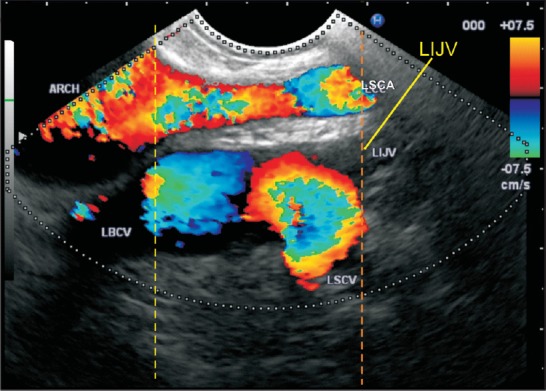
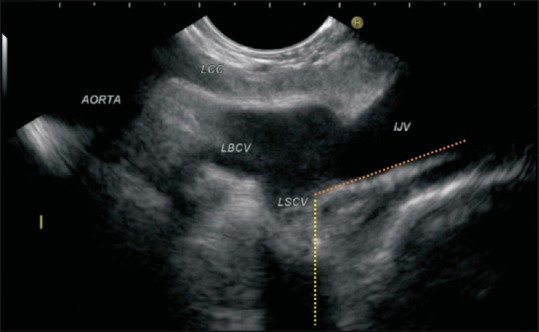
The EUS image shows the origin of the left subclavian artery from the arch of the aorta. The formation of the left brachiocephalic vein is observed by the union of the left internal jugular vein and the left subclavian vein near the lower part of the supraclavicular triangle. In general, the venous system is larger and lies more laterally, and is observed beyond the left common carotid artery in this image. The yellow line represents the upper border of the aortic arch and the orange line shows the lowermost point of the supraclavicular triangle. LBCV = left brachiocephalic vein; LCC = left common carotid artery; LIJV = left internal jugular vein; LSCV = left subclavian vein
Figure 30.
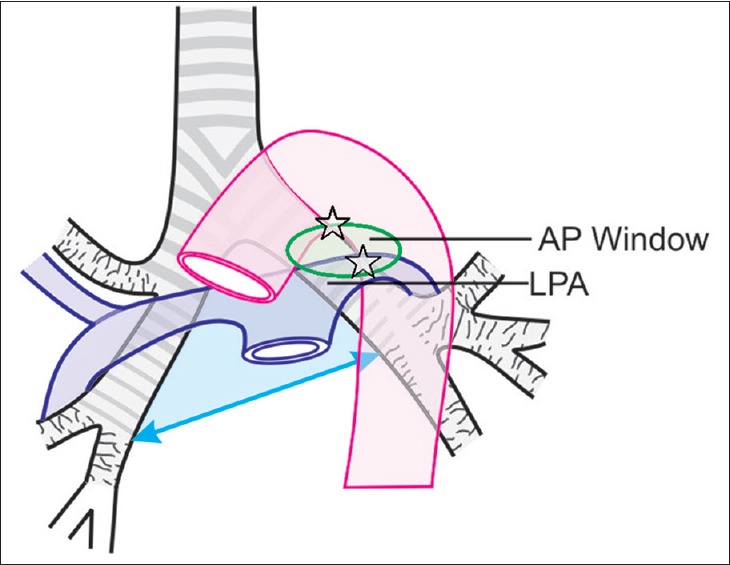
The aortopulmonary (AP) window lies immediately below the arch of the aorta above the left pulmonary artery (oval green circle). It is bounded superiorly by the inferior margin of the aortic arch; inferiorly by the superior margin of the left pulmonary artery; anteriorly by the posterior wall of the ascending aorta; posteriorly by the anterior wall of the descending aorta; medially by the trachea and the left main bronchus, and esophagus; and laterally by the left lung and left upper-lobe pleurae. The AP window merges with the subcarinal space
Figure 34.
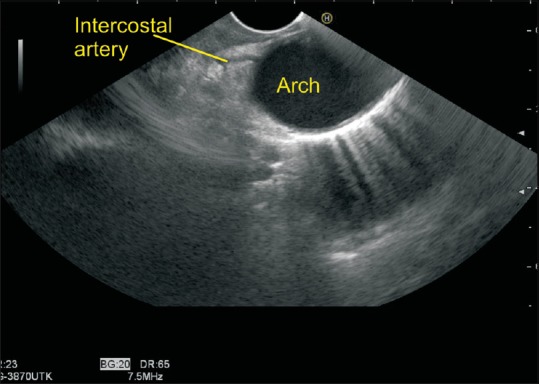
The contents of the aortopulmonary window include the bronchial arteries; in this case a bronchial artery is seen going from the lower aspect of the aortic arch into the aortopulmonary window. Label in figure
Figure 22.
The transverse section of the same case as in Figure 21
Figure 23.
EUS was able to show the same collection in right paratracheal space. The collection lies between the esophagus and SVC and can be also called as retrocaval in location
Figure 24.
The right paratracheal area is generally considered to be a difficult area for imaging by EUS, but in this case it was easily visualized by EUS. The brachiocephalic trunk is also seen
Figure 25.
The right paratracheal space is a continuation of pretracheal space. It is generally bigger and wider
Figure 28.
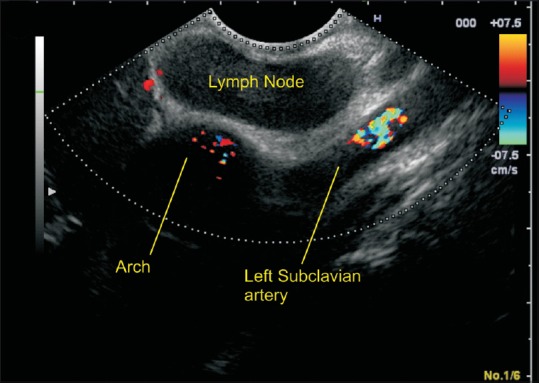
The examination of the arch of the aorta shows the origin of the left subclavian artery and a lymph node belonging to a metastatic station of head and neck malignancy
Figure 31.
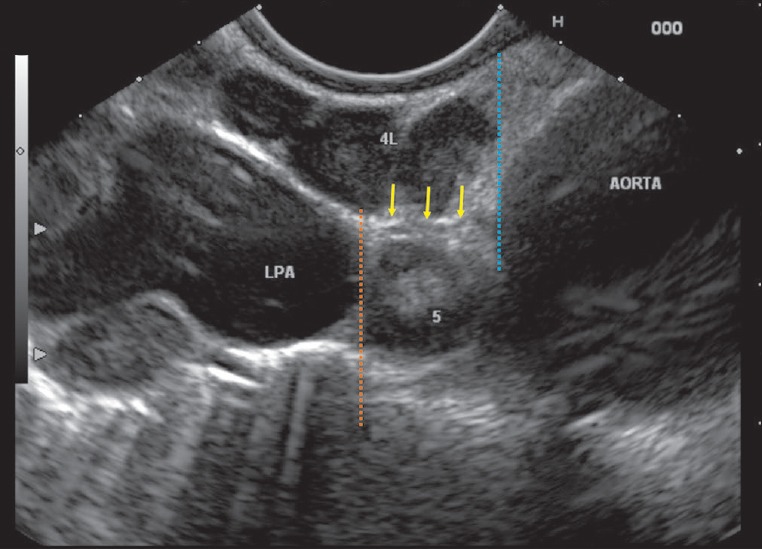
The AP window is bounded superiorly by the inferior margin of the aortic arch (dotted blue line) and inferiorly by the superior margin of the left pulmonary artery (dotted orange line); the ligamentum arteriosum is seen in an imaginary line between the arch of the aorta and the left pulmonary artery. In this case the ligamentum arteriosum is indicated by yellow arrows. The lymph node line medial to ligamentum arteriosum is labelled as station 4L and the lymph node lateral to the ligament is labelled as station 5
Figure 32.

A mass is seen in the AP window
Figure 33.
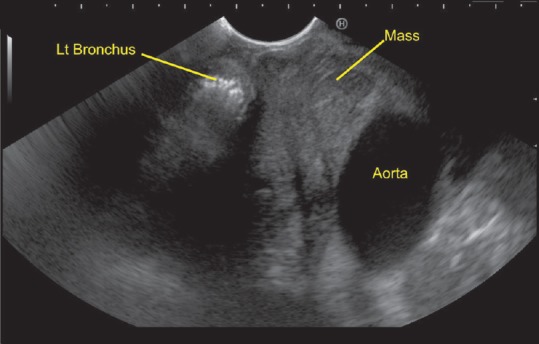
The same case as Figure 32. The left bronchus is seen just below the mass, can be traced going toward the left hilum of the lung on anticlockwise rotation, and shows the extension of mass up to the lower limit of the AP window
Spaces posterior to trachea
Most of the spaces behind the trachea are continuations of the neck spaces and have been already described.
The retrotracheal space (or Raider triangle) lies between the esophagus and the trachea and is normally triangular in shape [Figures 35 and 36].[27]
The posterior junctional area lies posterior to the trachea and esophagus, is formed by the apposition of the lungs posterior to the esophagus, and lies anterior to the vertebral bodies of T3 to T5 vertebrae.[28,29,30,31,32] The posterior junction line can be seen above the level of the azygos vein and the aorta by EUS.
Figure 35.
The figure shows a coronal section of different spaces and the technique of EUS imaging. The retrotracheal space is seen
Figure 36.
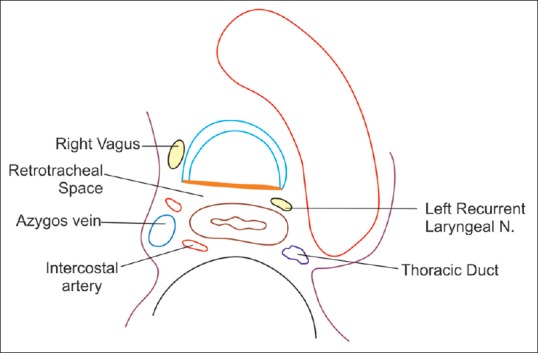
The area of arches shows the position of different spaces at T4 vertebral level
Spaces below trachea
This space is ideally called the subcarinal compartment but is sometimes described as two intercommunicating spaces that are partly separated by the right pulmonary artery. One is called the precarinal space and the other is called the subcarinal space. The subcarinal compartment is continuous below with the azygoesophageal and preaortic recesses.
The precarinal space merges imperceptibly with the aortopulmonary window on the left and continues below into the subcarinal area [Figure 37]
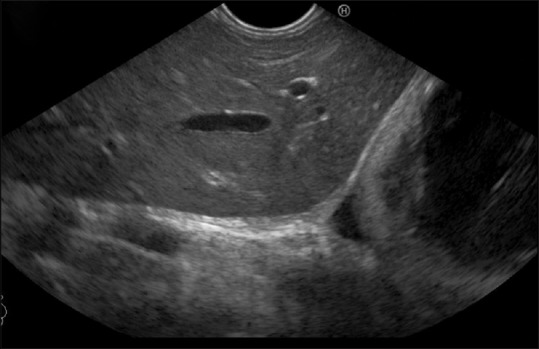
The subcarinal space is sometimes described as the area below the carina and sometimes as the area below the right pulmonary artery. It commonly contains benign triangular lymph nodes [Figures 38–43]
The azygoesophageal recess (also called “Holzknecht space” or “retroesophageal recess/pouch”) is the interface between the right lower lobe of the lung and the mediastinal reflection inferior to the arch of the azygos vein [Figures 44 and 45]
The preaortic recess is an inconstant space analogous to the azygoesophageal recess and is present in individuals whose left lung is able to extend anterior to the descending aorta [Figure 46]
The retrocrural space lies between the diaphragmatic crura and the T12 vertebra.[18]
Figure 37.
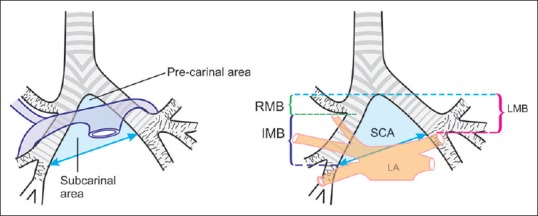
IASLC classification defines subcarinal window/area (light blue triangular area) as a pyramidal space, the tip of which lies at the tracheal bifurcation. The right boundary (~5 cm) is formed by the right bronchus (~2.5 cm) and intermediate bronchus (~2.5 cm), and the left boundary is formed by left main bronchus (~5 cm). The lower limit of the SCA is formed by an oblique line drawn from the lower border of the intermediate bronchus to the lower border of the left main bronchus and is also defined by the upper border of the left atrium (~3–4 cm in breadth). RMB = Right main bronchus, LMB = Left main bronchus, IMB = Intermediate bronchus, SCA = Subcarinal area shown in blue triangle. RMB = Right main bronchus, LMB = Left main bronchus, IMB = Intermediate bronchus
Figure 38.
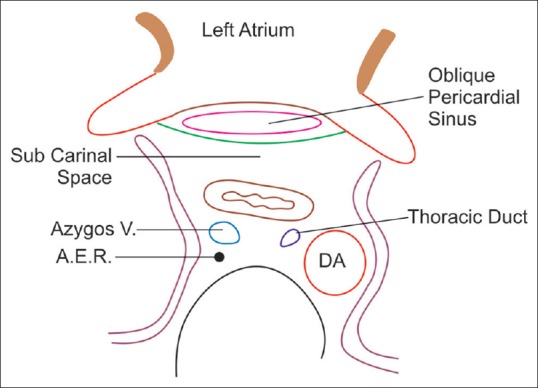
This figure shows the relationship of the subcarinal space with the oblique sinus of the pericardium, and the pathway of communication with the azygoesophageal and preaortic recesses
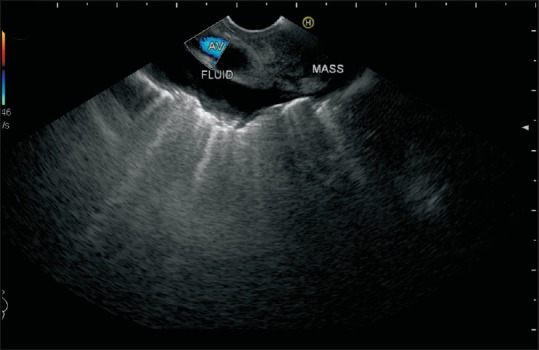
Figure 43.
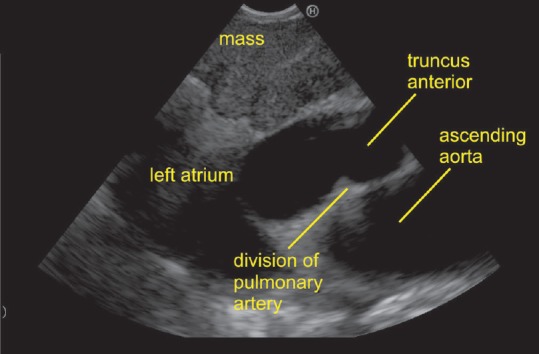
The imaging of subcarinal area can be done at ~ 27 cm distance in the esophagus. The lower boundary of station 7 is made by the left atrium. In this case, the right pulmonary artery is seen dividing into two branches. The division of the right pulmonary artery into two branches occurs after crossing the bronchus. The upper branch is known as truncus anterior
Figure 44.
The esophagus contacts the upper lobe of both lungs, and only the pleural sacs intervene between the esophagus and lung. The pleural sacs may be filled with fluid, which can come up posteriorly below the azygos vein, which arches above the right bronchus to join the SVC. In this case, there is a tumor involving the arch of the azygos vein and pleural effusion close to the azygos vein. The esophagus goes through the superior mediastinum and remains in contact with both upper lobe of lungs, whereas the trachea gets separated from the lung on the left side by the branches of the aorta
Figure 45.

The azygos vein runs close to esophagus, and in this case the esophageal tumor is extending into the azygoesophageal recess. The reflection of the sound waves from the right lung is seen as a white line along the distal border of the azygos vein
Figure 46.
The aortoesophageal recess generally lies in the area between the esophagus and the adjacent aorta. In this case, a mass is seen beyond the aorta and lies within the close-to-posterior basal segment of the left lung
Figure 39.
The right boundary of the subcarinal space can be defined with ease if the right pulmonary artery is followed up to its bifurcation. In this image, the division of the right pulmonary artery and the right bronchus defines the right boundary of the subcarinal space
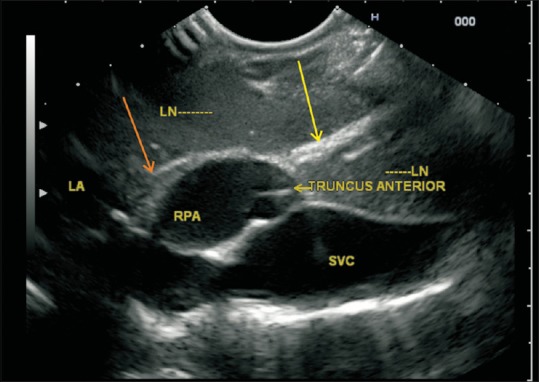
Figure 40.
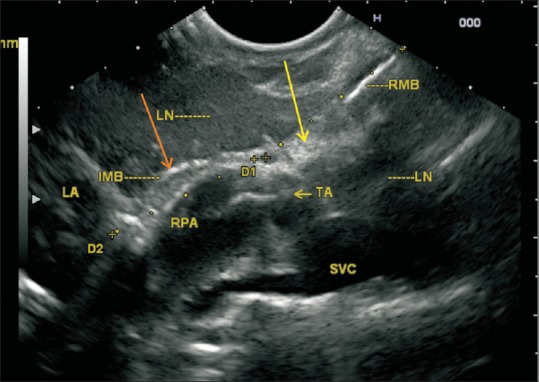
The right pulmonary artery divides into two branches near the right main bronchus (yellow arrow) and intermediate bronchus (orange arrow). The upper branch of the right pulmonary artery goes to the right upper lobe and is called truncus anterior. On the right, the truncus anterior courses inferior to the right upper lobe bronchus at the hilum and then passes anterosuperior to the bronchus as it exits the hilum. The upper border of the right pulmonary artery at the point of this division corresponds to the lower border of the right main bronchus and the lower limit of the paratracheal space on the right side. Yellow arrow = Right main bronchus, RMB = Right main bronchus, Orange arrow = Intermediate bronchus, IMB = Intermediate bronchus, RPA = Right pulmonary artery, SVC = Superior vena cava, LA = Left atrium
Figure 41.
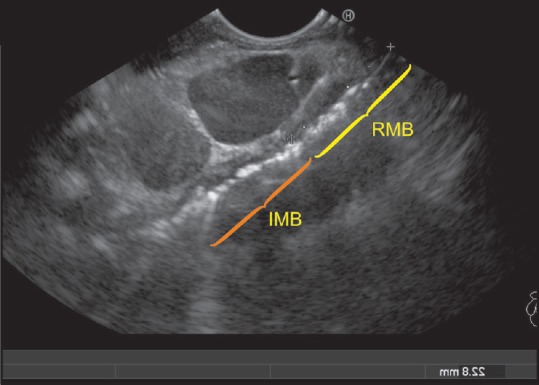
The right boundary of the subcarinal area is approximately 5 cm in length and is formed by right main bronchus, which is about 2.5 cm in length, and intermediate bronchus, which is about 2.5 cm in length. Air is seen within the right main bronchus and the intermediate bronchus. In this case, two lymph nodes are seen and one of them lies close to the right main bronchus, whereas the other lies close to the intermediate bronchus. (yellow arrow indicates RMB = Right main bronchus, orange arrow indicates IMB = Intermediate bronchus)
Figure 42.
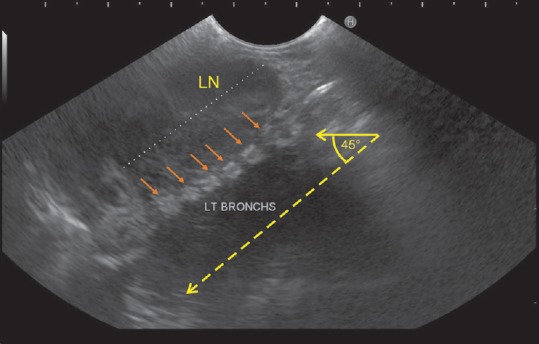
The right bronchus takes an angle of about 45° from midline as it proceeds toward the hilum of the left lung (dotted yellow arrow). It is seen in the subcarinal window anterior to the esophagus and can be traced from the lower margin of the trachea with clockwise rotation. As the scope is rotated clockwise, the left bronchus proceeds in an angle of about 45° from midline and in this case is seen as multiple interrupted rings (small orange arrows). The subcarinal space is the entire space between the probe and the left bronchus
Spaces related to pericardium
The pericardium surrounds the heart and extends cranially to cover the pulmonary trunk, superior vena cava (SVC), and ascending aorta. On EUS the normal amount of 15–20 mL of pericardial fluid can produce well-circumscribed contours with a variety of shapes including triangular, crescent-shaped, oval, or beaklike extensions.[33] The pericardial cavity contains the pericardial cavity proper and two major pericardial sinuses, the transverse and oblique sinuses [Figures 47 and 48].[34]
Figure 47.
The superior aortic recess is an extension of transverse sinus, which extends upward along the right side of the ascending aorta usually to the level of the sternal angle, and can mimic adenopathy at the right and left paratracheal stations
Figure 48.
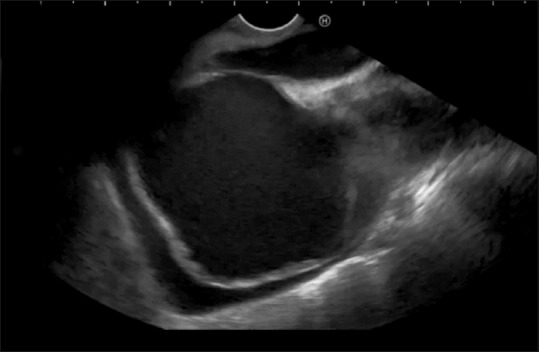
A small amount of fluid is seen in the tip of the pericardial cavity
The transverse sinus is located cephalad to the left atrium. It gives origin to the superior and inferior aortic recesses and the left and right pulmonic recesses [Figure 49][35,36,37,38]
The oblique sinus is the most posterior pericardial space. Fluid in the oblique sinus can simulate abnormalities in the esophagus, descending thoracic aorta, and subcarinal and bronchopulmonary lymph nodes [Figure 50].
Figure 49.
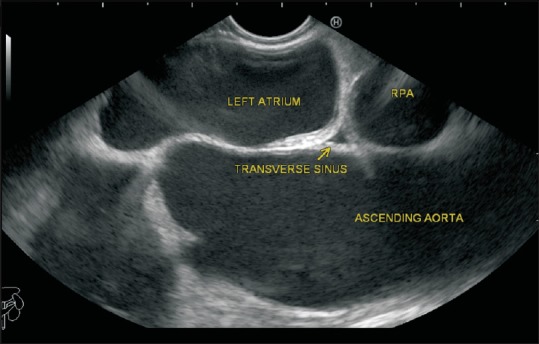
A larger amount of fluid is seen in the pericardial cavity, as indicated by yellow arrows
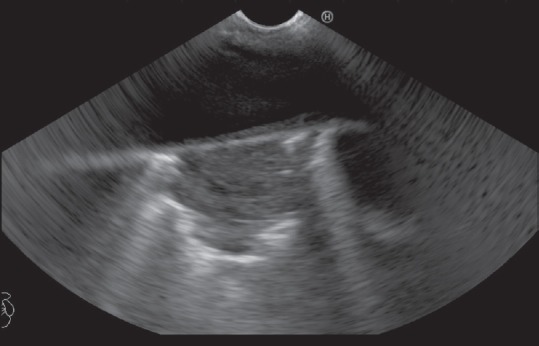
Figure 50.
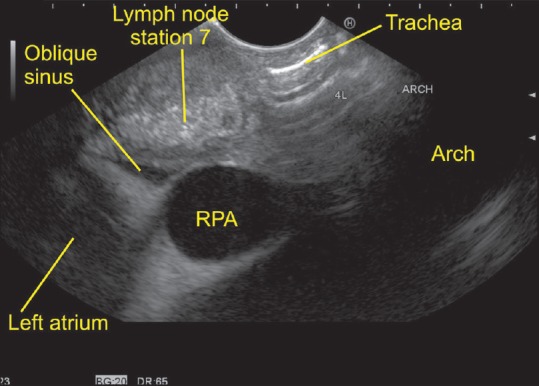
The oblique sinus of the pericardium is seen between the right pulmonary artery and the left atrium
CONCLUSION
The trachea and the esophagus pass through the center of the mediastinum and are responsible for the formation of many spaces. These spaces are continuous with the potential space in the neck. The description of the spaces in the neck generally coincides with the presence of lymph node stations as described for head and neck cancers. The description of the spaces in the mediastinum generally coincides with lymph node stations as described in IASLC classification. Knowledge of the spaces is important to head, neck, and thoracic surgeons because these anatomic areas are used daily for radiographic interpretation as well as for the performance of surgical procedures.[28] The evolution of CT technology has improved detection of these spaces, and more detailed imaging is now routinely pursued before planning management strategies. Knowledge of the typical locations and of typical and atypical appearances on EUS can prevent misdiagnosis and help in appropriate management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Heitzman ER. Radiologic Correlations with Anatomy and Pathology. St. Louis: Mosby; 1977. The Mediastinum. [Google Scholar]
- 2.Gervasio A, Mujahed I, Biasio A, Alessi S. Ultrasound anatomy of the neck: The infrahyoid region. J Ultrasound. 2010;13:85–9. doi: 10.1016/j.jus.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sone S, Higashihara T, Morimoto S, Yokota K, Ikezoe J, Oomine H, et al. Potential spaces of the mediastinum: CT pneumomediastinography. AJR Am J Roentgenol. 1982;138:1051–7. doi: 10.2214/ajr.138.6.1051. [DOI] [PubMed] [Google Scholar]
- 4.Dammann F, Bootz F, Cohnen M, Hassfeld S, Tatagiba M, Kösling S. Diagnostic imaging modalities in head and neck disease. Dtsch Arztebl Int. 2014;111:417–23. doi: 10.3238/arztebl.2014.0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nair S, Mohan S, Nilakantan A, Gupta A, Malik A, Gupta A. Impact of (18) f-fluorodeoxyglucose positron emission tomography/computed tomography scan on initial evaluation of head and neck squamous cell carcinoma: Our experience at a tertiary care center in India. World J Nucl Med. 2015;14:19–24. doi: 10.4103/1450-1147.150519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reimann K, Horger M, Schulze M. TMN classification of hypopharynx carcinoma-hypopharynx carcinoma: TNM classification. Rofo. 2013;185:1119–23. doi: 10.1055/s-0033-1346795. [DOI] [PubMed] [Google Scholar]
- 7.Subesinghe M, Scarsbrook AF, Sourbron S, Wilson DJ, McDermott G, Speight R, et al. Alterations in anatomic and functional imaging parameters with repeated FDG PET-CT and MRI during radiotherapy for head and neck cancer: A pilot study. BMC Cancer. 2015;15:137. doi: 10.1186/s12885-015-1154-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraft M, Bruns N, Hügens-Penzel M, Arens C. Clinical value of endosonography in the assessment of laryngeal cancer. Head Neck. 2013;35:195–200. doi: 10.1002/hed.22949. [DOI] [PubMed] [Google Scholar]
- 9.Arens C, Weigt J, Schumacher J, Kraft M. Ultrasound of the larynx, hypopharynx and upper esophagus. HNO. 2011;59:145–54. doi: 10.1007/s00106-010-2211-x. [DOI] [PubMed] [Google Scholar]
- 10.Bozzato A. Interpretation of ultrasound findings in otorhinolaryngology: Skin, soft tissue of the neck, lymph nodes, and oncologic follow-up. HNO. 2015;63:139–54. doi: 10.1007/s00106-014-2961-y. [DOI] [PubMed] [Google Scholar]
- 11.Mavrogenis G, Hassaini H, Sibille A, Feloni S, Deprez PH, Gillain C, et al. Expanding the horizons of endoscopic ultrasound: Diagnosis of non-digestive pathologies. Gastroenterol Rep (Oxf) 2014;2:63–9. doi: 10.1093/gastro/got033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallace MB, Pascual JM, Raimondo M, Woodward TA, Mccomb BL, Johnson MM, et al. Complete “medical mediastinoscopy” under conscious sedation: A prospective blinded comparison of endoscopic and endobronchial ultrasound to bronchoscopic fine needle aspiration for malignant mediastinal lymph nodes. Gastrointest Endosc. 2006;63:AB96. [Google Scholar]
- 13.Sharma A, Fidias P, Hayman LA, Loomis SL, Taber KH, Aquino SL. Patterns of lymphadenopathy in thoracic malignancies. Radiographics. 2004;24:419–34. doi: 10.1148/rg.242035075. [DOI] [PubMed] [Google Scholar]
- 14.van Zoonen M, van Oijen MG, van Leeuwen MS, van Hillegersberg R, Siersema PD, Vleggaar FP. Low impact of staging EUS for determining surgical resectability in esophageal cancer. Surg Endosc. 2012;26:2828–34. doi: 10.1007/s00464-012-2254-z. [DOI] [PubMed] [Google Scholar]
- 15.Hwang HS, Perez DA, Orloff LA. Comparison of positron emission tomography/computed tomography imaging and ultrasound in staging and surveillance of head and neck and thyroid cancer. Laryngoscope. 2009;119:1958–65. doi: 10.1002/lary.20594. [DOI] [PubMed] [Google Scholar]
- 16.Wang SJ. Surveillance radiologic imaging after treatment of oropharyngeal cancer: A review. World J Surg Oncol. 2015;13:94. doi: 10.1186/s12957-015-0481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wierzbicka M, Popko M, Piskadło K, Czepczyński R, Stankowska A, Piętka T, et al. Comparison of positron emission tomography/computed tomography imaging and ultrasound in surveillance of head and neck cancer-The 3-year experience of the ENT Department in Poznan. Rep Pract Oncol Radiother. 2011;16:184–8. doi: 10.1016/j.rpor.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balboni GC. 3rd ed. Vol. 2. Edi-Hermes; 1994. Human Anatomy; pp. 578–94. [Google Scholar]
- 19.Hansell DM, Lynch DA, McAdams HP, Bankier AA. Conventionally These Spaces Contain Specific Group of L.N. As Per the Classification Described by IASLC [Google Scholar]
- 20.Frias Vilaça A, Reis AM, Vidal IM. The anatomical compartments and their connections as demonstrated by ectopic air. Insights Imaging. 2013;4:759–72. doi: 10.1007/s13244-013-0278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma M, Rameshbabu CS, Mohan P. Standard techniques of imaging of IASLC borders by endoscopic ultrasound. J Bronchology Interv Pulmonol. 2011;18:99–110. doi: 10.1097/LBR.0b013e318207e6d5. [DOI] [PubMed] [Google Scholar]
- 22.Sharma M, Arya CL, Somasundaram A, Rameshbabu CS. Techniques of linear endobronchial ultrasound imaging. J Bronchology Interv Pulmonol. 2010;17:177–87. doi: 10.1097/LBR.0b013e3181dca122. [DOI] [PubMed] [Google Scholar]
- 23.Ziyade S, Pinarbasili NB, Ziyade N, Akdemir OC, Sahin F, Soysal Ö, et al. J Determination of standard number, size and weight of mediastinal lymph nodes in postmortem examinations: Reflection on lung cancer surgery. J Cardiothorac Surg. 2013;8:94. doi: 10.1186/1749-8090-8-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rong F, Xiao S. Location of mediastinal lymph nodes for conventional transbronchial needle aspiration. Zhonghua Jie He He Hu Xi Za Zhi. 2014;37:588–91. [PubMed] [Google Scholar]
- 25.Occhipinti M, Heidinger BH, Franquet E, Eisenberg RL, Bankier AA. Imaging the posterior mediastinum: A multimodality approach. Diagn Interv Radiol. 2015;21:293–306. doi: 10.5152/dir.2014.14467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schnyder PA, Gamsu G. CT of the pretracheal retrocaval space. AJR Am J Roentgenol. 1981;136:303–8. doi: 10.2214/ajr.136.2.303. [DOI] [PubMed] [Google Scholar]
- 27.Franquet T, Erasmus JJ, Giménez A, Rossi S, Prats R. The retrotracheal space: Normal anatomic and pathologic appearances. Radiographics. 2002;22:S231–46. doi: 10.1148/radiographics.22.suppl_1.g02oc16s231. [DOI] [PubMed] [Google Scholar]
- 28.Gibbs JM, Chandrasekhar CA, Ferguson EC, Oldham SA. Lines and stripes: Where did they go?–From conventional radiography to CT. Radiographics. 2007;27:33–48. doi: 10.1148/rg.271065073. [DOI] [PubMed] [Google Scholar]
- 29.Bertin F, Deslauriers J. Anatomy of the pleura: Reflection lines and recesses. Thorac Surg Clin. 2011;21:165–71. doi: 10.1016/j.thorsurg.2010.12.002. vii. [DOI] [PubMed] [Google Scholar]
- 30.Pfister RC, Oh KS, Ferrucci JT., Jr Retrosternal density. A radiological evaluation of the retrosternal-premediastinal space. Radiology. 1970;96:317–24. doi: 10.1148/96.2.317. [DOI] [PubMed] [Google Scholar]
- 31.Whalen JP, Meyers MA, Oliphant M, Caragol WJ, Evans JA. The retrosternal line. A new sign of an anterior mediastinal mass. Am J Roentgenol Radium Ther Nucl Med. 1973;117:861–72. doi: 10.2214/ajr.117.4.861. [DOI] [PubMed] [Google Scholar]
- 32.McComb BL. Reflecting upon the left superior mediastinum. J Thorac Imaging. 2001;16:56–64. doi: 10.1097/00005382-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Truong MT, Erasmus JJ, Gladish GW, Sabloff BS, Marom EM, Madewell JE, et al. Anatomy of pericardial recesses on multidetector CT: Implications for oncologic imaging. AJR Am J Roentgenol. 2003;181:1109–13. doi: 10.2214/ajr.181.4.1811109. [DOI] [PubMed] [Google Scholar]
- 34.O’Leary SM, Williams PL, Williams MP, Edwards AJ, Roobottom CA, Morgan-Hughes GJ, et al. Imaging the pericardium: Appearances on ECG-gated 64-detector row cardiac computed tomography. Br J Radiol. 2010;83:194–205. doi: 10.1259/bjr/55699491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Basile A, Bisceglie P, Giulietti G, Calcara G, Figuera M, Mundo E, et al. Prevalence of “high-riding” superior pericardial recesses on thin-section 16-MDCT scans. Eur J Radiol. 2006;59:265–9. doi: 10.1016/j.ejrad.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 36.Choi YW, McAdams HP, Jeon SC, Seo HS, Hahm CK. The “High-Riding” superior pericardial recess: CT findings. AJR Am J Roentgenol. 2000;175:1025–8. doi: 10.2214/ajr.175.4.1751025. [DOI] [PubMed] [Google Scholar]
- 37.Alraiyes AH, Almeida FA, Mehta AC. Pericardial recess through the eyes of endobronchial ultrasound. Endosc Ultrasound. 2015;4:162–3. doi: 10.4103/2303-9027.156764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shroff GS, Viswanathan C, Godoy MC, Marom EM, Sabloff BS, Truong MT. Pitfalls in oncologic imaging: Pericardial recesses mimicking adenopathy. Semin Roentgenol. 2015;50:235–40. doi: 10.1053/j.ro.2015.01.013. [DOI] [PubMed] [Google Scholar]


