ABSTRACT
CD4 tropism is conserved among all primate lentiviruses and likely contributes to viral pathogenesis by targeting cells that are critical for adaptive antiviral immune responses. Although CD4-independent variants of human immunodeficiency virus (HIV) and simian immunodeficiency virus (SIV) have been described that can utilize the coreceptor CCR5 or CXCR4 in the absence of CD4, these viruses typically retain their CD4 binding sites and still can interact with CD4. We describe the derivation of a novel CD4-independent variant of pathogenic SIVmac239, termed iMac239, that was used to derive an infectious R5-tropic SIV lacking a CD4 binding site. Of the seven mutations that differentiate iMac239 from wild-type SIVmac239, a single change (D178G) in the V1/V2 region was sufficient to confer CD4 independence in cell-cell fusion assays, although other mutations were required for replication competence. Like other CD4-independent viruses, iMac239 was highly neutralization sensitive, although mutations were identified that could confer CD4-independent infection without increasing its neutralization sensitivity. Strikingly, iMac239 retained the ability to replicate in cell lines and primary cells even when its CD4 binding site had been ablated by deletion of a highly conserved aspartic acid at position 385, which, for HIV-1, plays a critical role in CD4 binding. iMac239, with and without the D385 deletion, exhibited an expanded host range in primary rhesus peripheral blood mononuclear cells that included CCR5+ CD8+ T cells. As the first non-CD4-tropic SIV, iMac239-ΔD385 will afford the opportunity to directly assess the in vivo role of CD4 targeting on pathogenesis and host immune responses.
IMPORTANCE CD4 tropism is an invariant feature of primate lentiviruses and likely plays a key role in pathogenesis by focusing viral infection onto cells that mediate adaptive immune responses and in protecting virions attached to cells from neutralizing antibodies. Although CD4-independent viruses are well described for HIV and SIV, these viruses characteristically retain their CD4 binding site and can engage CD4 if available. We derived a novel CD4-independent, CCR5-tropic variant of the pathogenic molecular clone SIVmac239, termed iMac239. The genetic determinants of iMac239's CD4 independence provide new insights into mechanisms that underlie this phenotype. This virus remained replication competent even after its CD4 binding site had been ablated by mutagenesis. As the first truly non-CD4-tropic SIV, lacking the capacity to interact with CD4, iMac239 will provide the unique opportunity to evaluate SIV pathogenesis and host immune responses in the absence of the immunomodulatory effects of CD4+ T cell targeting and infection.
INTRODUCTION
The primate lentiviruses human immunodeficiency virus type 1 (HIV-1), HIV-2, and simian immunodeficiency virus (SIV) share a mechanism of target cell entry by interacting with CD4 and a member of the chemokine receptor family (1–3). CD4 binding to the envelope glycoprotein (Env) trimer initiates a cascade of conformational changes, resulting in the formation and exposure of the coreceptor binding site on the gp120 subunit of Env. Following coreceptor binding, the gp41 subunit is released to interact with the target cell membrane, leading to the formation of a fusion intermediate and, ultimately, the 6-helix bundle, which drives membrane fusion and viral entry (1, 3–9). While CCR5, CXCR4, and, less commonly, other coreceptors can be used by these viruses during entry, CD4 tropism, mediated by a highly conserved binding site on gp120, is an invariant feature (1, 10), indicating that it plays a major role in pathogenesis. CD4 binding enables HIV-1 to evade host neutralizing antibody responses by limiting antibody access to neutralizing epitopes once the virion has attached to CD4 on the cell surface (11, 12). In addition, CD4 tropism in vivo focuses viral infection onto CD4+ T cell subsets that are critical in mediating adaptive antiviral immunity (13–16). These cells include Th1, Th17, T follicular helper, and T regulatory cells that collectively contribute to the coordinated induction, maturation, and maintenance of cellular and humoral immune responses (17–26) and (for Th17 cells) to the integrity of the epithelial barrier at mucosal surfaces (20, 27, 28).
Although CD4 tropism is conserved, rare examples of CD4-independent viruses have been described that can utilize coreceptors, either CCR5 or CXCR4, for entry in the absence of CD4. These viruses, through mutations in gp120 and/or gp41, preform and expose a functional coreceptor binding site that typically is present only after CD4 binding occurs (29–40). By cryoelectron microscopy, Env trimers on CD4-independent viruses exhibit more open conformations than CD4-dependent viruses, and in the absence of CD4 they acquire conformations typically seen only after CD4 binding and triggering occur (41, 42). Although CD4-independent viruses have been derived in vitro (29–37, 43), they have only rarely been observed in vivo, as in rhesus macaques during late-stage disease or following the depletion of CD4+ T cells prior to infection with anti-CD4 antibodies (44–46). CD4-independent viruses typically are highly neutralization sensitive as a result of their more open Env trimer conformations and exposure of neutralization epitopes on cell-free virions that are poorly accessible after binding to the cell surface (12, 32, 39, 40, 47). Thus, CD4-independent viruses likely are strongly selected against in vivo (32, 48, 49). Nonetheless, although not strictly CD4 independent, HIVs and SIVs with the ability to utilize low levels of CD4 for entry are well described, and this phenotype has been proposed to contribute to the infection of macrophages and microglial cells, which exhibit a lower density of CD4 than T cells (32, 43–45, 50–57). For one neuropathic SIV isolate, its ability to cause AIDS encephalopathy in macaques correlated with the infection of brain-derived endothelial cells that expressed CCR5 but not CD4 (58). In addition, CD4-independent infection has been proposed to contribute to SIV infection of macrophages in the context of cell-to-cell transmission (59, 60). Of note, viruses that are CD4 independent typically retain their CD4 binding site and the ability to engage CD4, if present (30, 34, 58, 61, 62), and have been shown to exhibit faster fusion kinetics in the presence of CD4 than CD4-dependent viruses (63).
For HIV-1, the CD4 binding site has been resolved at the atomic level and shown to be a deeply recessed pocket on gp120 formed by regions within the inner and outer domains that interact cooperatively with CD4 and gp41 during CD4 binding (1, 4, 41, 64, 65). Among HIV-1 and SIV isolates, some variability exists in these interactions. For SIVmac, the bulky side chain at Trp-375 has been shown to fill a space in the CD4 binding pocket, reducing its dependency on CD4 binding, while HIV-1, containing a serine at this position, requires additional contributions from a layer on the gp120 inner domain (64). In HIV-1, residues Asp-368, Glu-370, and Trp-427 are highly conserved and make multiple contacts with CD4, particularly amino acids Phe-43 and Arg-59 in its outermost D1 domain. Among these, Arg-59 forms a salt bridge with Asp-368 on gp120, and mutations in gp120 (10, 66) or CD4 (67, 68) that disrupt this bond ablate CD4 binding. Although crystallographic resolution of an SIV gp120 in complex with CD4 has not been determined, an aspartic acid at the analogous position (i.e., amino acid 385 for SIVmac) is conserved in all SIVs except for two SIV mandrill env clones that contain a glutamic acid residue, suggesting that this aspartic acid also is critical for SIV gp120 interactions with CD4 (10) (see Fig. S1 in the supplemental material). Indeed, a brain-derived Env clone from an SIVmac239-infected macaque with an asparagine at this position exhibited a 40-fold reduction in CD4 binding and CD4-independent use of CCR5 in a cell-cell fusion assay (69).
We describe the in vitro derivation of a novel variant of SIVmac239 that is both CD4 independent and unable to interact with CD4. This variant was adapted to replicate in a CD4-negative clone of SupT1 cells that expressed rhesus CCR5. Four mutations in gp120 and 2 in the gp41 ectodomain were associated with CD4 independence, and of these, a D178G mutation in the region analogous to the HIV-1 V1/V2 loops was shown to be necessary for this phenotype, while additional mutations were required to enable a spreading infection to occur. Although iMac239, like other CD4-independent viruses, was highly neutralization sensitive, mutations in gp120 were identified that conferred CD4 independence in the absence of increased neutralization sensitivity. Notably, when Asp-385 was deleted to disrupt the CD4 binding site, fusion and infectivity of parental SIVmac239 were ablated while iMac239 remained fully replication competent on CD4+, CCR5+, and CD4−, CCR5+ cell lines and primary macaque lymphocytes. In addition, iMac239 with and without the Asp-385 deletion exhibited an expanded host range in primary macaque peripheral mononuclear cells that included CCR5+, CD8+ T cells. Thus, iMac239 will provide a novel platform for exploring the molecular and structural determinants for CD4 independence and neutralization sensitivity and has enabled a novel non-CD4-tropic SIV variant to be derived that can be used to directly explore the role of CD4 binding and tropism in pathogenesis and in modulating host immune responses.
MATERIALS AND METHODS
Cell lines.
Human SupT1 and BC7 cell lines (29) were transfected with a lentiviral vector to express rhesus CCR5 (RhCCR5) (70). SupT1/RhCCR5, BC7/RhCCR5, CEMx174, and HUT-78 cell lines were maintained in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS), 2 mM glutamine, and 2 mM penicillin-streptomycin (RPMI-complete). The Japanese quail fibrosarcoma cell line QT6, the human embryonic kidney cell line 293T, and the human HeLa cell line TZM-bl engineered to express CD4 and CCR5 (obtained through the AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH, from John C. Kappes) were cultured in Dulbecco's modified Eagle medium supplemented with 10% FBS, 2 mM glutamine, and 2 mM penicillin-streptomycin (DMEM-complete).
Env cloning and mutagenesis.
Adapted env clones from SIV-infected BC7/RhCCR5 cultures were isolated as described previously (71). Mutant env genes were created using the QuikChange site-directed mutagenesis kit (Stratagene) by following the manufacturer's protocol. To repair a premature stop codon in the cytoplasmic tail of env at position 734, this codon was reverted to the wild-type (WT) Q by QuikChange. To generate recombinant molecular clones of the SIVmac239 genome containing adapted and mutant env genes, env clones were cloned into the previously described pHVP-2 construct (also known as p239SpSp3′) containing an open nef reading frame with a corrected HindIII site at position 602, and containing the 3′ half of the viral genome, following HindIII/SacI digestion (72). Full-length genome constructs then were generated by cloning pVP-2 with p239SpSp5′ as previously described (71) (p239SpSp5′ was obtained through the AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH, from Ronald Desrosiers). The identities of the recombinant clones were confirmed using restriction analysis and DNA sequencing. For the generation of Env-pseudotyped viruses, SIV env genes with a premature stop codon in the cytoplasmic tail (CT) coding region (Q734Stop) in pCR2.1 were digested with KpnI and XbaI and cloned into the similarly digested pCDNA3.1(−) expression construct.
Fusion assays.
Env fusion was assessed quantitatively on quail QT6 cells using a cell-cell fusion assay and expression constructs for CD4 and various coreceptors, and the use of a reporter plasmid encoding luciferase under the control of a T7 promoter has been previously described (71, 73, 74). Rhesus CD4 and coreceptors CCR5, CXCR6, APJ, GPR1, GPR15, CCR2, and CCR8 were kindly provided by Ronald Collman and Robert Doms.
Pseudotype viruses.
Pseudotyped viruses were generated as previously described (75) by cotransfecting 293T cells with 8 μg of plasmid encoding the SG3 Δenv-based virus backbone and 4 μg of the appropriate env expression vector for 3 to 8 h with the FuGENE6 transfection agent (Promega). Cell supernatants were collected at 48 h posttransfection and stored at −80°C.
Virus production.
To generate molecularly cloned viruses, 293T cells were transfected with full-length viral genome constructs for 5 h using calcium phosphate. Cell supernatants were collected 48 or 72 h posttransfection and stored at −80°C. The uncloned iMac239 swarm was generated from supernatants of acutely infected BC7RhR5 cells and stored at −80°C.
Viral replication assays.
Virus concentrations were determined by enzyme-linked immunosorbent assay for viral p27 Gag antigen (Advanced Bioscience Laboratories). SupT1/RhCCR5 and BC7/RhCCR5 were inoculated with equivalent amounts of p27-containing virus. Following overnight incubation at 37°C, infected cells were washed in RPMI supplemented with 5% FBS to remove excess virus and then maintained in RPMI-complete medium. Viral replication was monitored by viral reverse transcriptase (RT) activity in the culture supernatants (29, 76).
Neutralization assays.
The sensitivity of pseudotyped viruses bearing Envs of interest to neutralization by sera or plasma samples from SIVmac251-infected rhesus macaques, soluble CD4, or monoclonal antibodies to SIVmac Envs, including murine antibodies 7D3, 11F2, 17A11, 5B11, 4E11, 171C2, and 36D5 (77), human antibodies 1.4H, 6.10F, 6.10B, 9.1A, and 1.7A, or rhesus antibodies 1.10A, 3.11H (78–81), and 4.10F (unpublished data; produced as described in reference 79), was assessed in a TZM-bl pseudotype assay as previously described (75). Briefly, pseudotyped viruses were incubated for 1 h at 37°C with various dilutions of serum, plasma, soluble CD4 (sCD4), or monoclonal antibodies and then used to infect TZM-bl cells pretreated with DEAE-dextran. Cells were incubated at 37°C for 48 h and then lysed with the BriteLite plus luminescence reporter assay system (PerkinElmer). A long terminal repeat (LTR)-driven luciferase reporter gene in TZM-bl cells generated the luciferase signal. Infection was quantified by measuring luciferase activity with a Thermo LabSystems Luminoskan Ascent luminometer. Neutralization was measured as the reduction in luciferase activity compared to that of untreated controls.
Infection of PBMCs.
Purified peripheral blood mononuclear cells (PBMCs) from rhesus macaques stored at −140°C were thawed and stimulated for 3 days with 5 μg/ml concanavalin A (ConA) at a concentration of 106 cells/ml in RPMI-complete medium. Cells (5 × 106) then were inoculated with viruses (125 ng of p27 Gag) and medium supplemented with interleukin-2 (IL-2) (100 U/ml). After 24 h, cells were washed to remove the viral inoculum and cultured in fresh RPMI-complete medium supplemented with IL-2 (100 U/ml).
Antibody reagents.
Antibodies used for surface staining included anti-CD14 BV650, anti-CD20 BV605, anti-CD8 BV570 (BioLegend), anti-CD16 APC Cy7, anti-CD95 PECy5, anti-CCR5 PE (BD Biosciences), anti-CD4 PECy5.5 (Invitrogen Life Technologies), and anti-CD28 ECD (Beckman Coulter). Antibodies used for intracellular staining included anti-CD3 V450 (BD Biosciences) and anti-p27 fluorescein isothiocyanate (FITC; kindly provided by E. Rakasz, WNPRC).
Flow cytometry staining assay.
At peaks of viral replication, infected rhesus PBMCs were identified by p27 Gag positivity and flow cytometry. Aliquots of cells (1 × 106 per sample) were washed once with PBS and stained for viability with Aqua amine-reactive dye (Invitrogen) for 10 min in the dark at room temperature. A mixture of surface marker antibodies was added and kept at room temperature for 30 min in the dark. Cells then were washed with PBS containing 1% bovine serum albumin (BSA) and 0.1% sodium azide and permeabilized for 17 min at room temperature using the Cytofix/Cytoperm kit (BD Biosciences). Immediately following permeabilization, cells were washed in Perm/Wash buffer (BD Biosciences), a cocktail of antibodies for intracellular markers was added, and the cells were incubated in the dark for 1 h at room temperature. Cells then were washed with Perm/Wash buffer, fixed with PBS containing 2% paraformaldehyde, and stored at 4°C until flow cytometric analysis. For flow cytometric analysis, 3 × 105 events were acquired on an LSRII flow cytometer (BD Immunocytometry Systems) modified to detect up to 18 fluorophores. Antibody capture beads (BD Biosciences) were used to prepare compensation tubes for each individual antibody used in the experiment. Data analysis was performed using FlowJo software, version 9.0.1 (TreeStar).
Nucleotide sequence accession number.
The iMac239 env sequence has been deposited in GenBank under accession number KT959233.
RESULTS
Adaptation of SIVmac239 to CD4-negative BC7/RhR5 cells.
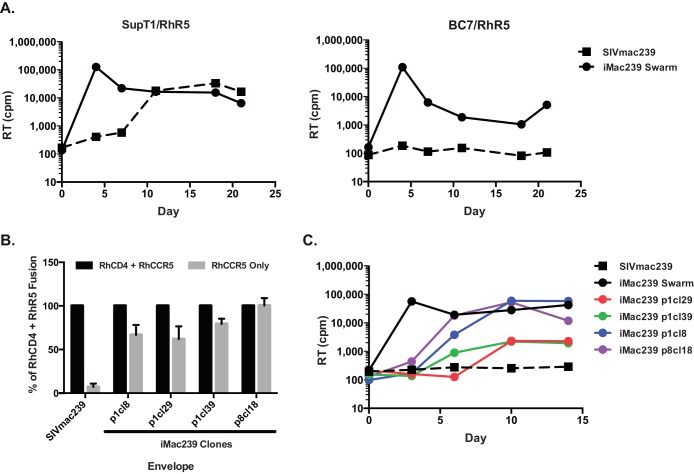
We derived a CD4-independent strain of SIV by serially passaging SIVmac239 on a 1:10 mixture of CD4-positive SupT1 cells and a CD4-negative variant of this line, BC7 (62), each of which stably expressed rhesus CCR5 (designated SupT1/RhR5 and BC7/RhR5, respectively). After 13 passages the virus could infect a pure culture of BC7/RhR5 cells and then was passaged an additional eight times in this cell line. The resulting viral swarm was able to replicate with high efficiency both in SupT1/RhR5 and in BC7/RhR5, while parental SIVmac239 could replicate only in the CD4+ SupT1/RhR5 cells (Fig. 1A). Env clones PCR amplified from genomic DNA of infected BC7/RhR5 cells were derived, and their ability to mediate CD4-independent fusion using rhesus CCR5 was evaluated on quail QT6 cells (73) (Fig. 1B). One clone (p8cl18) mediated comparable levels of fusion in the presence or absence of rhesus CD4 and was selected for further characterization. When this Env was inserted into a SIVmac239 backbone, the resulting virus (iMac239 p8cl18 in Fig. 1C) was able to replicate with rapid growth kinetics in both SupT1/RhR5 (data not shown) and BC7/RhR5 cells (Fig. 1C), while parental SIVmac239 was only able to replicate in SupT1/RhR5 (Fig. 1A). CD4-independent replication in BC7/RhR5 cells was retained when the expected premature stop codon acquired during passaging of this SIVmac in human cell lines (82) was corrected (data not shown), and this Env was used to construct a virus containing a full-length cytoplasmic tail, designated iMac239, that was employed in all subsequent experiments, except for the production of Env-pseudotyped viruses, for which Envs with a short cytoplasmic tail were used.
FIG 1.
Replication and fusion of CD4-independent variants of SIVmac239. (A) Replication of parental SIVmac239 and an uncloned CD4-independent viral swarm is shown in CD4+ SupT1/RhR5 cells (left) and CD4− BC7/RhR5 cells (right), each of which stably expressed rhesus CCR5. RT, reverse transcriptase activity. (B) Fusion activity of SIVmac239 and four iMac239 env clones on QT6 cells using a cell-cell fusion assay. For each env gene, the level of CD4-independent fusion on rhesus CCR5 is shown as a percentage of fusion (luciferase activity) in the presence of rhesus CD4. Background fusion levels on cells expressing GFP only were subtracted. The data shown are the means of three experiments plus the standard errors of the means (SEM). (C) Growth curves in CD4-negative, BC7/RhR5 cells are shown for wild-type (WT) SIVmac239, the iMac239 viral swarm, and four recombinant SIVmac239-based viruses bearing the indicated iMac239 env clones. RT activity in culture supernatants was measured at the indicated time points. Results from a representative experiment are shown.
Mutations required for iMac239 CD4 independence.
Sequencing of the iMac239 p18cl8 env gene revealed seven coding changes from SIVmac239, four in gp120 and three in gp41 (Table 1; also see Fig. S2 in the supplemental material). None of the gp120 mutations occurred in regions analogous to those of HIV-1 gp120 that contribute to the CD4 binding site in HIV-1, indicating that although the iMac239 Env and virus were CD4 independent, they likely retained the ability to interact with CD4. For gp120, three mutations (D178G, D337Y, and R427K) occurred within variable loop regions V1/V2, V3, and V4, respectively, while a single mutation (H224Q) occurred in a region analogous to the HIV-1 C2 region flanking the V1/V2 stem. In gp41, two mutations in the ectodomain (K573T and N673I) were located within regions comparable to HIV-1 heptad-repeat regions 1 and 2 (HR1 and HR2), respectively, while one (L820M) occurred in the cytoplasmic tail.
TABLE 1.
Amino acid differences in envelope glycoproteins between SIVmac239 and CD4-independent iMac239a
| Virus | Env region and amino acid position |
||||||
|---|---|---|---|---|---|---|---|
| gp120 |
gp41 |
||||||
| V1/V2 | C2 | V3 | V4 | HR1 | HR2 | CT | |
| 178 | 224 | 337 | 427 | 573 | 673 | 820 | |
| SIVmac239 | D | H | D | R | K | N | L |
| iMac239 | G | Q | Y | K | T | I | M |
Also see Fig. S2 in the supplemental material.
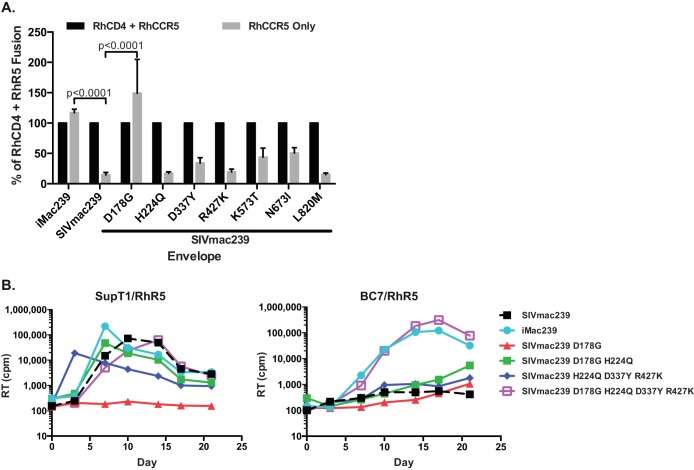
The contributions of these mutations to CD4 independence first were evaluated in a cell-cell fusion assay (Fig. 2A). In the absence of CD4 the iMac239 Env generated fusion levels on CCR5 that were comparable to or slightly greater than those in the presence of CD4, while parental SIVmac239 exhibited <10% fusion. When iMac239 mutations were introduced singly into the SIVmac239 Env, D178G in the V1/V2 loop was sufficient to confer CD4-independent fusion at levels approximately 50% greater than those in the presence of CD4, although gp41 mutations K573T and N673I each produced modest increases in fusion to levels 40 to 50% of the fusion in the presence of CD4.
FIG 2.
Determinants for iMac239 Env CD4 independence in cell-cell fusion and viral replication assays. (A) Fusion activity on rhesus CCR5 in the presence or absence of rhesus CD4 is shown for SIVmac239 Envs containing the indicated single mutations from iMac239. Data from 3 experiments plus SEM are shown as described for Fig. 1B. Two-way analysis of variance (ANOVA) with multiple comparisons was used to determine significance. (B) Replication of SIVmac239-based viruses bearing the indicated Envs is shown in CD4+ SupT1/RhR5 (left) and CD4− BC7/RhR5 (right) cells. Four changes in gp120 are sufficient to confer CD4-independent replication. A virus with D178G alone was unable to replicate in either cell type but was rescued for replication in SupT1 by H224Q. RT activity was measured at the indicated time points. Results from a representative experiment are shown.
We next evaluated CD4 independence in an infection assay on SupT1/RhR5 and BC7/RhR5 cells using viruses containing Envs with various combinations of iMac239 mutations (Fig. 2B). When all 4 gp120 mutations were introduced into the SIVmac239 Env (SIVmac239 D178G H224Q D337Y R427K in Fig. 2B), robust CD4-independent replication was observed in BC7/RhR5 cells with kinetics and levels that were comparable to those of a virus with the full iMac239 Env. However, a virus containing only the gp41 K573T and N673I mutations replicated poorly in both cell types (not shown). Interestingly, although the D178G mutation alone was sufficient to confer CD4 independence in the cell-cell fusion assay, a virus containing only this mutation replicated poorly in BC7/RhR5 cells and was noninfectious on CD4+ SupT1/RhR5 cells (Fig. 2B). Virions from this virus exhibited levels of Env similar to those of both SIVmac239 WT and iMac239 virus, as measured by Western blotting, indicating that this defect was not the result of a failure of Env incorporation into virions (data not shown). However, when viruses contained the D178G mutation in combination with the gp120 H224Q mutation, replication was restored in both SupT1/RhR5 and BC7/RhR5 cells, although CD4-independent replication occurred more slowly in the latter (Fig. 2B). This apparent rescue of infectivity for virus containing the D178G mutation alone was not seen when the other gp120 mutations were inserted individually (not shown). Significantly, the removal of the D178G mutation from the iMac239 Env with all four gp120 changes resulted in a virus (SIVmac239 H224Q D337Y R427K) that was replication competent on SupT1/RhR5 cells but no longer CD4 independent and unable to infect BC7/RhR5 cells (Fig. 2B). Thus, among the gp120 mutations that conferred CD4 independence to SIVmac239, while D178G in V1/V2 was critical, this mutation alone resulted in a virus that was noninfectious in both CD4-positive and -negative cell types but could be rescued by the H224Q change in gp120.
Neutralization sensitivity of iMac239.
For HIV-1 and SIV, CD4-independent Envs typically are highly neutralization sensitive, owing to their more open conformation of the Env trimer on virions (41, 42) and formation of highly immunogenic epitopes that typically are induced only in the presence of CD4 (11, 32, 39, 40). Given the well-described neutralization resistance of the SIVmac239 Env, we were interested in determining the neutralization sensitivity of the iMac239 Env to a panel of sera and plasma samples from SIVmac-infected rhesus macaques and to a panel of anti-SIVmac gp120 monoclonal antibodies previously shown to potently neutralize laboratory-adapted SIVmac251 but not SIVmac239 (77). Neutralization assays were performed on TZM-bl cells using viral particles pseudotyped with Envs. In addition to iMac239, we also evaluated SIVmac239 Envs containing the four gp120 changes that were sufficient to confer CD4 independence (Fig. 2B) in viral replication assays and an Env containing only the D178G mutation, which was CD4 independent in the cell-cell fusion assay (Fig. 2A).
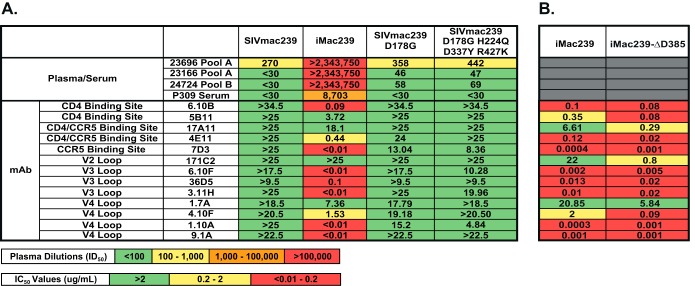
As expected, whereas SIVmac239 was resistant to neutralization by anti-SIV sera or plasma, with reciprocal 50% inhibitory dilutions (ID50) of ≤270, iMac239 was highly sensitive, with ID50 values of >2 million for plasma and 8,703 for sera (Fig. 3A). We sought to determine if iMac239's neutralization sensitivity could be mapped to particular epitopes; thus, we utilized a panel of monoclonal antibodies to SIVmac variable loops (V2, V3, and V4) and to the CD4 and CCR5 binding sites (77–81) in TZM-bl cell neutralization assays. As with the plasma and serum samples, SIVmac239 was highly resistant to all of the antibodies in the panel, while iMac239 was highly sensitive to 7 of 13 antibodies and resistant only to an anti-CD4 binding site (5B11), anti-CD4/CCR5 binding site (17A11), anti-V2 (171C2), and anti-V4 loop (1.7A) antibody (Fig. 3A). Surprisingly, iMac239 Envs containing the minimum number of mutations in gp120 that conferred CD4 independence in either cell-cell fusion or viral infection assays (Fig. 2) remained neutralization resistant at levels comparable to those of parental SIVmac239. These findings indicate that although typically associated, CD4 independence and increased neutralization sensitivity can be dissociated. Moreover, these findings also suggest that changes in the iMac239 gp41 that were selected for in vitro and were not present in the SIVmac239 D178G H224Q D337Y R427K Env used in this assay were key determinants for its marked neutralization sensitivity.
FIG 3.
Neutralization sensitivity of Envs with iMac239 mutations. Viral pseudotypes containing the indicated Envs were preincubated with various dilutions of plasma, serum, or monoclonal antibodies prior to infection of TZM-bl cells. Reciprocal 50% inhibitory dilutions (ID50) for plasma and serum are color coded (<100, green; 100 to 1,000, yellow; 1,000 to 100,000, orange; >100,000, red). Fifty percent inhibitory concentrations (IC50) of monoclonal antibodies (mAb) are color coded (>2 μg/ml, green; 0.2 to 2 μg/ml, yellow; <0.01 to 0.2 μg/ml, red). (A) Neutralization of SIVmac239 and iMac239 relative to two viruses (SIVmac239 D178G and SIVmac239 D179G H224Q D337Y R427K), each containing the indicated mutations in gp120. (B) Neutralization of iMac239 and iMac239-ΔD385, containing a deletion of Asp-385 within the CD4 binding site. Gray-shaded areas indicate assays that were not tested.
CD4 independence of iMac239 is retained following ablation of the CD4 binding site.
Although CD4-independent Envs are structurally altered and expose or form neutralization epitopes (32, 39–42, 47), as noted above, these Envs retain the ability to bind and use CD4. In order to determine if the iMac239 Env would remain competent for fusion and infection even after its CD4 binding site had been ablated, we introduced a 3-nucleotide deletion removing a codon for an aspartic acid at amino acid position 385 that is highly conserved throughout HIV and SIV phylogeny (10) (see Fig. S1 in the supplemental material). For HIV-1, the analogous aspartic acid at position 368 (HXB numbering) forms a salt bridge with arginine 59 of CD4 (1, 2), and a D368R mutation in HIV-1 gp120 ablates CD4 binding and most CD4 binding site antibody epitopes (10, 66).
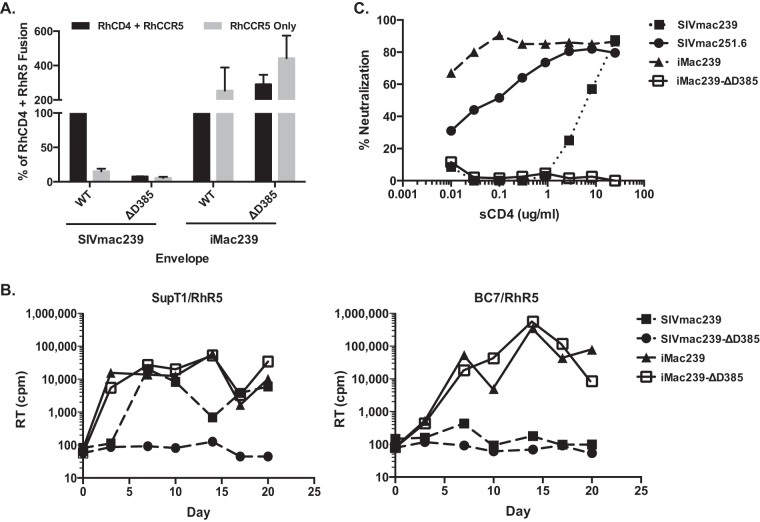
The effects of the D385 deletion (ΔD385) on SIVmac239 and iMac239 Envs were assessed in cell-cell fusion assays and on viral replication on CD4-positive and CD4-negative cell lines. Remarkably, whereas ΔD385 largely ablated the fusion of SIVmac239 Env on target cells bearing CD4 and CCR5 to levels of <10% of the wild type, iMac239 fusion was unaffected and actually was enhanced in the presence of this mutation (Fig. 4A). When viral replication was assessed in SupT1/RhR5 and BC7/RhR5 cells, SIVmac239 containing the ΔD385 mutation was unable to replicate in either cell type, whereas iMac239 with or without the ΔD385 mutation replicated in both cell types with similar kinetics (Fig. 4B, left and right). We confirmed that viruses used in these infection assays expressed comparable amounts of gp120 relative to p27 Gag (not shown).
FIG 4.
Effect of the ΔD385 mutation in cell-cell fusion, viral replication, and neutralization assays. (A) Fusion activities of SIVmac239, SIVmac239-ΔD385, iMac239, and iMac239-ΔD385 on rhesus CCR5 only are shown for each Env as the percentage of fusion in the presence of rhesus CD4. Background was subtracted as described for Fig. 1B. The data shown are the means from four experiments plus SEM. (B) Replication of SIVmac239, SIVmac239-ΔD385, iMac239, and iMac239-ΔD385 viruses in CD4+ SupT1/RhR5 cells (left) and CD4− BC7/RhR5 cells (right). RT activity in culture supernatants was measured at the indicated time points. Results from a representative experiment are shown. (C) Soluble CD4 (sCD4) neutralization of viral pseudotypes containing SIVmac239, SIVmac251.6, iMac239, and iMac239-ΔD385 Envs is shown on TZM-bl cells. Percent neutralization was calculated using luciferase activity normalized to infection in the absence of sCD4. Results from a representative experiment are shown.
The sensitivity of viral pseudotypes bearing these Envs to neutralization by sCD4 also was assessed as an indicator of CD4 binding to Env trimers on virions. The infectivity of pseudotypes containing SIVmac239, SIVmac251.6 (a laboratory-adapted SIVmac), iMac239, or iMac239-ΔD385 Envs was evaluated on TZM-bl cells in the presence of various concentrations of sCD4. While sCD4 sensitivity was observed for SIVmac239 (IC50, 7.8 μg/ml) and was markedly enhanced for SIVmac251.6 (IC50, 0.1 μg/ml) and iMac239 (IC50 <0.01 μg/ml), iMac239 containing the ΔD385 mutation was highly resistant (IC50, >20 μg/ml) (Fig. 4C). Collectively these findings indicate that although the iMac239 Env retained a CD4 binding site and was highly sensitive to sCD4 neutralization, this Env could mediate entry while lacking a CD4 binding site.
Identifying neutralization epitopes on iMac239 and iMac239-ΔD385.
Given the exquisite sensitivity of iMac239 Env to sera from SIVmac-infected macaques and monoclonal antibodies to gp120 epitopes (Fig. 3A) and the ability of iMac239 virus to replicate without a functional CD4 binding site (Fig. 4B), we sought to determine if conformational changes associated with its altered antigenicity were affected by the loss of the CD4 binding site. Neutralization of viral particles pseudotyped with Envs from iMac239 or iMac239-ΔD385 was assessed on TZM-bl cells using the same panel of monoclonal antibodies as that shown in Fig. 3A. As seen previously (Fig. 3A), the iMac239-ΔD385 Env also was highly neutralization sensitive at levels that were comparable to or greater than those of iMac239 (Fig. 3B). Thus, relative to SIVmac239, CD4-independent iMac239 was globally neutralization sensitive to multiple antibodies, and this sensitivity was further enhanced by the ΔD385 mutation. These findings also indicate that while the ΔD385 mutation largely ablated CD4 binding function, it did not disrupt the antigenicity of the CD4 binding site, as determined by the antibodies in our panel.
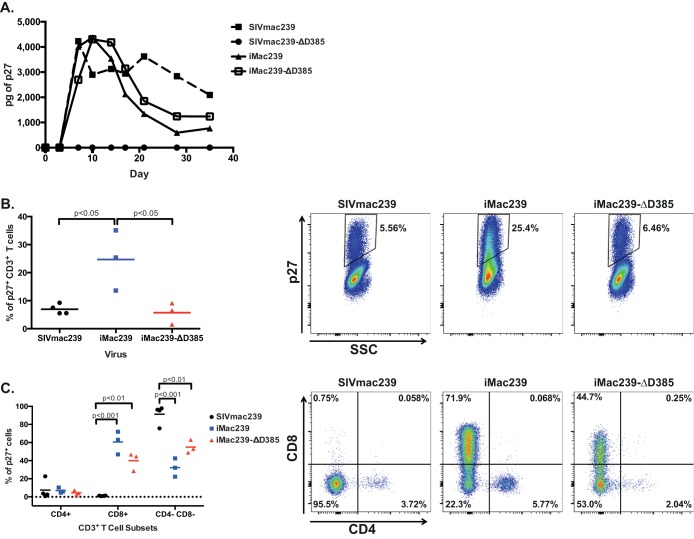
Replication of iMac239 and iMac239-ΔD385 in primary rhesus macaque PBMC.
Given the ability of CD4-independent iMac239 to replicate in T cell lines with or without a CD4 binding site, we assessed the infectivity of iMac239 and iMac239-ΔD385 on ConA/IL-2-stimulated primary rhesus PBMCs. Similar to T cell lines, parental SIVmac239 containing the ΔD385 mutation was completely noninfectious. However, both iMac239 and iMac239-ΔD385 replicated to levels identical to those of SIVmac239. Peak intracellular viral p27 Gag expression occurred at different days postinoculation, with SIVmac239 infection peaking at 4 days postinfection and iMac239 and iMac239-ΔD385 peaking at 10 days (Fig. 5A). These data indicate that while CD4 binding could facilitate iMac239 replication, a CD4 binding site was not required for this virus to infect primary cells.
FIG 5.
Replication of SIVmac239 and iMac239 with and without the ΔD385 mutation in rhesus PBMCs. Replication of SIVmac239, SIVmac239-ΔD385, iMac239, and iMac239-ΔD385 in ConA/IL-2-stimulated rhesus PBMCs is shown. p27 Gag in culture supernatants was quantified by ELISA at the indicated time points. (A) Results from a representative experiment are shown. (B, left) For each virus, the percentage of total CD3+ T cells that are positive for p27 Gag are indicated. (Right) Flow cytometry cytograms from a representative experiment show the percentage of p27 Gag+ CD3+ T cells. (C, left) The percentage of p27 Gag+ CD3+ T cells that express CD4 and/or CD8 at peak infection is shown. (Right) Cytograms from a representative experiment show that for iMac239 and iMac239-ΔD385, a marked increase in p27 Gag is detectable in CD8+ T cells. One-way analysis of variance (ANOVA) was used to determine significance.
Given the potential for CD4-independent iMac239 and iMac239-ΔD385 to have an expanded cellular tropism, we next assessed their infectivity for different cell types in the stimulated rhesus macaque PBMC population using flow cytometry with a panel of antibodies to T cells, B cells, and monocyte subsets and to CCR5. Gating strategies were performed with uninfected cells (see Fig. S3 in the supplemental material). Among CD3+ T cells assayed at the viral peak, iMac239 infection produced a significant increase in p27 Gag-positive cells compared to both SIVmac239 and iMac239-ΔD385 (i.e., 25.4% versus 5.56% and 6.46%, respectively, in the representative experiment shown in Fig. 5B). Among p27 Gag+ CD3+ T cells, the vast majority (>90%) of SIVmac239-infected cells were negative for CD4 and CD8, most likely reflecting CD4+ T cells from which CD4 was downregulated by the effects of Nef and Env expression (83–86), and only rare cells (<1%) expressed CD8. In marked contrast, for iMac239 and iMac239-ΔD385 infections, on average 60% and 40% of p27 Gag+ cells, respectively, expressed CD8 (Fig. 5C). The infection of monocytes (CD16+ and CD14+) or B cells (CD20+) was not observed (data not shown), although we note that culture conditions did not support the expansion of these cell types. Further analysis will be required to determine if any additional CD4-negative cell types in rhesus PBMC populations are infected by iMac239 and iMac239-ΔD385. Collectively, these data indicate that both CD4-independent iMac239 and iMac239-ΔD385 have expanded tropism on primary cells, which includes CD8+ T cells.
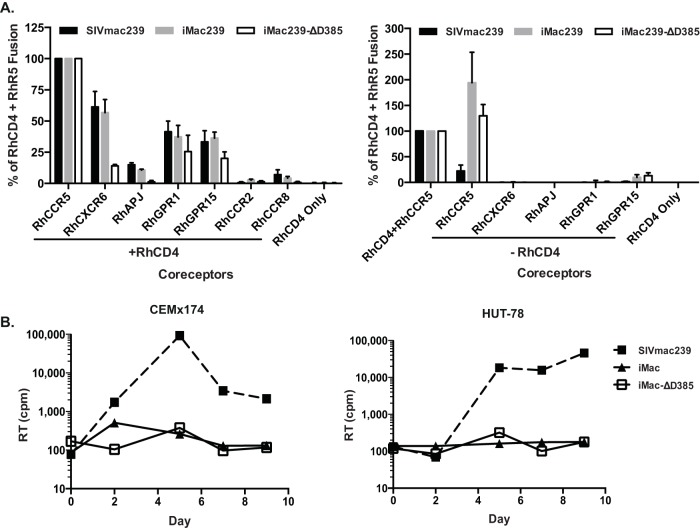
No use of alternative coreceptors by iMac239 and iMac239-ΔD385.
SIVmac239 and other SIVs have been shown to use coreceptors in addition to CCR5, including CXCR6, APJ, GPR1, GPR15, CCR2, and CCR8 (87–91). To determine if CD4-independent use of CCR5 by iMac239 and iMac239-ΔD385 affected CD4-dependent or -independent use of alternative coreceptors, a cell-cell fusion assay was used to assess fusion on target cells expressing rhesus CXCR6, APJ, GPR1, GPR15, CCR2, and CCR8 with or without rhesus CD4. In the presence of CD4, SIVmac239, iMac239, and iMac239-ΔD385 exhibited some capacity to use CXCR6, GPR1, and GPR15, although the levels of fusion were less than those for CCR5 (Fig. 6A, left). However, in the absence of CD4, only iMac239 and iMac-ΔD385 exhibited CD4-independent fusion, and only on CCR5 (Fig. 6A, right). We also assessed the infection of two CD4+, CCR5-negative cell lines, CEMx174 and HUT-78, previously shown to be permissive for SIVmac infection, most likely through their expression of GPR15 (91–96). In contrast to SIVmac239, both iMac239 and iMac239-ΔD385 were unable to replicate in these cell lines (Fig. 6B). Thus, while adapted for the CD4-independent use of rhesus CCR5, these findings suggest that iMac239 and iMac239-ΔD385 are strictly CCR5 tropic and unable to use alternative coreceptors for infection in the presence or absence of CD4.
FIG 6.
Use of alternative coreceptors by SIVmac239, iMac239, and iMac239-ΔD385. (A) Fusion activity of the indicated Envs on rhesus coreceptors in the presence (left) or absence (right) of rhesus CD4 was assessed in a cell-cell fusion assay. In each panel, luciferase activity was normalized to values for rhesus CCR5. Background fusion levels were subtracted prior to normalization. Data shown are the means from three experiments plus SEM. (B) Replication of SIVmac239, iMac239, and iMac239-ΔD385 viruses in CD4+ CCR5− CEMx174 (left) and HUT-78 (right) cells. RT activity in culture supernatants was measured at the indicated time points. Results from a representative experiment are shown.
DISCUSSION
CD4 tropism is conserved among all primate lentiviruses and has been proposed to play a key role in protecting viruses from neutralizing antibodies that are sterically restricted from accessing the Env trimer once virions have bound to the cell surface (11, 12). However, by focusing infection onto cells that are critical to host adaptive immune responses, CD4 tropism likely also exerts potent immunomodulatory effects that contribute to disease progression and/or viral persistence. Although CD4-independent viruses have been observed in vivo, particularly in nonhuman primate models of pathogenic SIV infection, they typically appear in the setting of highly immunocompromised hosts with advanced neurological or pulmonary complications (44, 58, 69) at sites where nonlymphoid cells (primarily macrophages) with little or no CD4 are infected. In rhesus macaques depleted of CD4 T cells with anti-CD4 antibodies prior to SIVmac infection, CD4-independent viruses rapidly appeared, in association with SIV encephalitis and macrophage infection (46, 53), indicating that this phenotype can readily emerge in vivo. Because CD4-independent viruses are characteristically neutralization sensitive, it is likely that they are strongly selected against during typical pathogenic infection (32, 48, 49, 97). Recent publications by Yen et al. have suggested that CD4-independent entry serves as a mechanism of cell-cell viral spread in tissue macrophages, which is more efficient and can shield virus from neutralizing antibodies than cell-free transmission, thereby allowing CD4-independent variants to circulate in compartments such as the brain (59, 60). Interestingly, primary isolates of HIV-2, which is less pathogenic than HIV-1 (reviewed in reference 98), have been reported to exhibit CD4 independence in vitro (61, 99). However, for HIV-1 (and as we show for SIVmac239), extensive passaging is required to derive CD4-independent viruses in vitro, indicating that for these viruses there likely are additional barriers to their emergence (29, 30, 34, 36, 37, 39, 47). Of note, CD4-independent Envs typically retain their CD4 binding site, and their infectivity generally is enhanced in the presence of CD4 (30, 32, 46, 61). Thus, while CD4-independent viruses arising in vivo or in vitro provide potentially useful tools to understand conformational changes associated with coreceptor engagement and viral entry (34, 35, 39, 40, 63), their applicability to questions of what role CD4 interactions play in pathogenesis and on host immune responses has been limited.
In this report, we describe the derivation and characterization of a CD4-independent and truly non-CD4-tropic variant of SIVmac239 that lacks the ability to interact with CD4. A CD4-independent virus, iMac239, was first derived in vitro and shown to be highly competent in mediating fusion and infection of cells bearing rhesus CCR5 in the absence of CD4. Unlike SIVmac316, a macrophage tropic variant of SIVmac239 that was CD4 independent in cell-cell fusion assays (32, 44), the determinants for iMac239's altered tropism resided solely within gp120, and this virus did not require a truncated cytoplasmic tail to exhibit this phenotype. Notably, after deletion of the codon for a highly conserved aspartic acid in the CD4 binding loop on gp120, shown for HIV-1 to be critical for CD4 binding, iMac239 remained fully infectious on CD4-negative cell lines expressing rhesus CCR5 and on primary peripheral blood lymphocytes. This mutation in parental SIVmac239 completely ablated its function in cell-cell fusion and infection assays. Moreover, whereas SIVmac239 and especially iMac239 were sensitive to neutralization by soluble CD4, iMac239 containing the ΔD385 deletion was completely resistant, consistent with the view that CD4 binding for this virus was ablated or at least markedly reduced (Fig. 4).
Among the seven mutations in the iMac239 Env, four changes in gp120 were sufficient to confer CD4-independent infection of CCR5-expressing cells. A D178G mutation in the iMac239 V1/V2 loop was critical in that this change alone conferred CD4-independent fusion to the SIVmac239 Env, and correction of this change alone ablated CD4-independent infection by a virus bearing the minimum set of gp120 mutations required for CD4 independence. For HIV-1 and SIV, changes in V1/V2 frequently are associated with CD4 independence (30, 33–35, 43, 100–102) and/or an enhanced ability to infect cells that express low levels of CD4 (60, 99). Structural studies of HIV-1 soluble SOSIP timers (7, 9, 103–105) and cryoelectron microscopic analyses of virion-associated trimers have shown, in the absence of CD4, V1/V2 loops to be oriented toward the apex of the trimer, in contrast to their more lateral positioning upon CD4 activation (8, 41). Given that soluble gp120 even in the absence of CD4 is thermodynamically favored to assume a CD4-bound conformation as an apparent default structure (106) but that its conformation is likely restrained by the V1/V2 and V3 variable loops (104–106), changes in V1/V2 that perturb its quaternary interactions within or between adjacent protomers could favor the spontaneous opening of the trimer to a CD4-bound conformation and promote CD4-independent function. Interestingly, although D178G alone enabled the SIVmac239 Env to fuse independently of CD4 and a viral pseudotype bearing this Env could permit infection in a single-round entry assay, SIVmac239 virus containing only this change was not replication competent on either CD4-positive or -negative cells. However, this Env could be rescued by iMac239's H224Q mutation distal from the V1/V2 stem. Because the Env trimer has been modeled as a metastable structure with the potential to assume conformations that are either favorable or nonpermissive for fusion (107, 108), we interpret these results to indicate that D178G, while necessary for CD4-independent fusion and entry, requires H224Q to guide conformational changes and/or promote Env stability during fusion and to prevent fusion-incompetent conformations from being formed, as described for HIV-1 Envs after cold treatment (107) and/or small-molecule CD4 binding site agonists (108–110).
As noted, it is likely that the enhanced neutralization sensitivity of CD4-independent viruses results from a more open structure, as their Env trimers assume conformations that typically occur only in the presence of CD4, exposing epitopes that are shielded on resting virions (41). In addition, CD4-induced epitopes that contribute to the coreceptor binding site and are highly immunogenic (11) are poorly formed in the absence of CD4 binding and inaccessible to antibodies on cell-bound virions but are able to be targeted on CD4-independent viruses on which they are formed and exposed (39) or sampled more frequently in the absence of CD4 (111). As we demonstrated, iMac239 as well as its non-CD4 binding derivative, iMac239-ΔD385, were globally neutralization sensitive to sera from SIVmac-infected animals and to monoclonal antibodies to CD4-induced and noninduced epitopes (Fig. 3). However, an Env containing only the iMac239 gp120 changes, while CD4 independent, remained highly neutralization resistant, similar to parental SIVmac239. Similar findings were reported by Yen and coworkers, in which the loss of a glycosylation site in the SIVmac239 V2 loop (Asn-173) conferred the ability to infect macrophages in the context of cell-to-cell transmission while retaining the neutralization-resistant phenotype of SIVmac239 (59, 60). In addition to indicating that CD4 independence and enhanced neutralization sensitivity can be dissociated, our findings also suggest that changes in the gp41 ectodomain that arose with iMac239's CD4 independence contribute to its neutralization sensitivity. The effect of gp41 mutations on gp120 neutralization sensitivity has been more extensively characterized in HIV-1 (112–115). Our finding also is consistent with the model of intrinsic reactivity of the Env trimer proposed by Haim et al. (107), in which changes in gp41 enhanced the spontaneous formation/exposure of the HR1 coiled coil, decreasing the threshold for Env to transition upon activation from a high-energy to a lower-energy state.
As described, CD4-independent iMac239 virus, following deletion of Asp-385, remained fully infectious on CCR5-expressing cell lines and on primary lymphocytes. Although the structure of the SIVmac gp120 in complex with CD4 has not been resolved at the crystallographic level, for HIV-1 this residue forms a covalent bond with Arg-59 on human CD4 (corresponding to Lys-59 on rhesus CD4) and is highly conserved across nearly all HIV and SIV isolates (see Fig. S1 in the supplemental material) (10). While we cannot rule out the possibility that iMac239 containing this mutation maintained some low-level interactions with CD4, the finding that it became completely resistant to soluble CD4 while iMac239 was exquisitely sensitive strongly supports the view that CD4 binding was markedly impaired (Fig. 4). We chose to introduce a deletion rather than a point mutation at this position to create a CD4-binding site mutant that would be less likely to revert in vivo in macaques. In vitro, when iMac239-ΔD385 was serially passaged up to 20 times in CD4+ SupT1/RhR5 cells, this mutation remained stable (not shown), indicating that the loss of CD4 binding function, at least in cell lines, did not confer a major fitness cost during long-term propagation in vitro.
In rhesus PBMCs cultured with T cell mitogens, SIVmac has been shown to infect CD4 effector and central memory T cells, consistent with the expression of CCR5 on these cells and SIVmac's highly efficient use of this coreceptor for entry (49, 116, 117). Although alternative coreceptors can be used by SIVs in vivo (87, 118), it is likely that levels of CCR5 expression are a key determinant of tropism and pathogenicity. Consistent with this hypothesis, sooty mangabeys, a natural host for nonpathogenic SIVsm infection, exhibit low CCR5 expression on central memory CD4 T cells, likely accounting for the sparing of this subset in the context of SIVsmm infection (117, 119). Among peripheral blood cells stimulated with T cell mitogens, iMac239 with and without the ΔD385 deletion exhibited an expanded host range that included CD8+ T cells, most likely through their expression of CCR5 (Fig. 5). We observed that 30 to 65% of CD8+ T cells in these cultures expressed CCR5 (not shown), which was associated with the infection of approximately 20% and 4% of CD3+ CD8+ T cells by iMac239 and non-CD4-tropic iMac239-ΔD385, respectively, in contrast to <0.15% for SIVmac239. The adaptation of SIVmac239 for CD4-independent use of CCR5 led to a reduced capacity to utilize alternative coreceptors (Fig. 6), suggesting that its expanded tropism in vitro was driven largely by CCR5 expression. Collectively, these findings clearly show that the tropism of SIVmac239 on primary cells can be altered and redirected from its exclusive infection of CD4+ target cells. Whether these viruses can infect additional cell types, such as NK, B cells, or monocytes, remains to be determined.
The ability to remove CD4 tropism from SIVmac creates new opportunities to assess the role of CD4 in pathogenesis. Nonhuman primate models of AIDS have clearly shown that during early SIV infection, CD4+ T cells that express CCR5 and reside in mucosal tissues are selectively and rapidly depleted (116, 120, 121), associated with a disruption in the epithelial barrier that contributes to microbial translocation and systemic immune activation (20, 27, 28, 122, 123). In addition, by focusing infection onto T cell subsets that provide help for adaptive immune responses, including Th1, Th17, and Tfh cells, it is likely that CD4 tropism has profound effects on antiviral immune responses, which ultimately are inadequate to contain viral replication and disease progression. Binding of gp120 to CD4 also has the potential to disrupt CD4's physiologic interaction with HLA class II on antigen-presenting cells, which underlies T-cell immunologic helper functions. Although iMac239-ΔD385 exhibited expanded cell tropism in vitro, its inability to selectively target CD4+ T cell subsets raises the possibility that T cell help for cytotoxic CD8 and CD4 cellular responses will be qualitatively or quantitatively altered and that B cell maturation and memory responses, which are dependent on interactions with Tfh cells, will lead to improved antibody responses. Future studies that assess the quality of anti-SIV responses in the context of a CD4-sparing infection will provide new insights into pathogenesis and possibly inform interventions that can be directed to improve host immune responses to infection and vaccines.
Supplementary Material
ACKNOWLEDGMENTS
We thank Emily Roberts (University of Pennsylvania) for technical assistance with flow cytometry assays and Robert Doms, Ronald Collman, and members of their laboratories at the University of Pennsylvania for supplying rhesus receptors. We also acknowledge assistance from the University of Pennsylvania Center for AIDS Research (CFAR) Viral/Molecular and Non-Human Primate Cores. We thank Meredith Hunter and Tessa Williams at the Tulane National Primate Research Center (TNPRC) for assistance with rhesus PMBC infections. We thank Mira Bilska at the Duke Central Reference Laboratory for excellent technical assistance with neutralization assays. We thank Vicky Coalter, Adam Wiles, Rodney Wiles, and Donald Johnson at NCI-Frederick for the acquisition and preparation of rhesus PBMCs. We thank Ronald Swanstrom at the University of North Carolina for helpful discussions.
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
Funding Statement
The Nonhuman Primate Humoral Immunology Core Laboratory also received funds through National Institute of Allergy and Infectious Diseases contract HHSN27201100016C. Extensive assistance was provided by the Viral/Molecular and Nonhuman Primate Cores of the Penn Center for AIDS Research (P30-AI045008).
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JVI.02851-15.
REFERENCES
- 1.Kwong PD, Wyatt RA, Robinson J, Sweet RW, Sodroski J, Hendrickson WA. 1998. Structure of an HIV gp120 envelope glycoprotein in complex with the CD4 receptor and a neutralizing human antibody. Nature 393:648–659. doi: 10.1038/31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wyatt R, Sodroski J. 1998. The HIV-1 envelope glycoproteins: fusogens, antigens, and immunogens. Science 280:1884–1888. doi: 10.1126/science.280.5371.1884. [DOI] [PubMed] [Google Scholar]
- 3.Wilen CB, Tilton JC, Doms RW. 2012. HIV: cell binding and entry, p 23–36. In Bushman FD, Nabel GJ, Swanstrom R (ed), HIV: from biology to prevention and treatment. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu J, Bartesaghi A, Borgnia MJ, Sapiro G, Subramaniam S. 2008. Molecular architecture of native HIV-1 gp120 trimers. Nature 455:109–113. doi: 10.1038/nature07159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myszka DG, Sweet RW, Hensley P, Brigham-Burke M, Kwong PD, Hendrickson WA, Wyatt R, Sodroski J, Doyle ML. 2000. Energetics of the HIV gp120-CD4 binding reaction. Proc Natl Acad Sci U S A 97:9026–9031. doi: 10.1073/pnas.97.16.9026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park HE, Gruenke JA, White JM. 2003. Leash in the groove mechanism of membrane fusion. Nat Struct Biol 10:1048–1053. doi: 10.1038/nsb1012. [DOI] [PubMed] [Google Scholar]
- 7.Kwon YD, Pancera M, Acharya P, Georgiev IS, Crooks ET, Gorman J, Joyce MG, Guttman M, Ma X, Narpala S, Soto C, Terry DS, Yang Y, Zhou T, Ahlsen G, Bailer RT, Chambers M, Chuang G-Y, Doria-Rose NA, Druz A, Hallen MA, Harned A, Kirys T, Louder MK, O'Dell S, Ofek G, Osawa K, Prabhakaran M, Sastry M, Stewart-Jones GBE, Stuckey J, Thomas PV, Tittley T, Williams C, Zhang B, Zhao H, Zhou Z, Donald BR, Lee LK, Zolla-Pazner S, Baxa U, Schön A, Freire E, Shapiro L, Lee KK, Arthos J, Munro JB, Blanchard SC, Mothes W, Binley JM, McDermott AB, Mascola JR, Kwong PD. 2015. Crystal structure, conformational fixation and entry-related interactions of mature ligand-free HIV-1 Env. Nat Struct Mol Biol 22:522–531. doi: 10.1038/nsmb.3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartesaghi A, Merk A, Borgnia MJ, Milne JLS, Subramaniam S. 2013. Pre-fusion structure of trimeric HIV-1 envelope glycoprotein determined by cryo-electron microscopy. Nat Struct Mol Biol 20:1352–1357. doi: 10.1038/nsmb.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pancera M, Zhou T, Druz A, Georgiev IS, Soto C, Gorman J, Huang J, Acharya P, Chuang G, Ofek G, Stewart-jones GBE, Stuckey J, Bailer RT, Joyce MG, Louder MK, Tumba N, Yang Y, Zhang B, Cohen MS, Haynes BF, Mascola JR, Morris L, Munro JB, Blanchard SC, Mothes W, Connors M, Kwong PD. 2014. Structure and immune recognition of trimeric pre-fusion HIV-1 Env. Nature 514:455–461. doi: 10.1038/nature13808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olshevsky U, Helseth E, Furman C, Li J, Haseltine W, Sodroski J. 1990. Identification of individual human immunodeficiency virus type 1 gp120 amino acids important for CD4 receptor binding. J Virol 64:5701–5707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Decker JM, Bibollet-Ruche F, Wei X, Wang S, Levy DN, Wang W, Delaporte E, Peeters M, Derdeyn CA, Allen S, Hunter E, Saag MS, Hoxie JA, Hahn BH, Kwong PD, Robinson JE, Shaw GM. 2005. Antigenic conservation and immunogenicity of the HIV coreceptor binding site. J Exp Med 201:1407–1419. doi: 10.1084/jem.20042510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Labrijn AF, Poignard P, Raja A, Zwick MB, Delgado K, Franti M, Binley J, Vivona V, Grundner C, Huang C-C, Venturi M, Petropoulos CJ, Wrin T, Dimitrov DS, Robinson J, Kwong PD, Wyatt RT, Sodroski J, Burton DR. 2003. Access of antibody molecules to the conserved coreceptor binding site on glycoprotein gp120 is sterically restricted on primary human immunodeficiency virus type 1. J Virol 77:10557–10565. doi: 10.1128/JVI.77.19.10557-10565.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalams SA, Walker BD. 1998. The critical need for CD4 help in maintaining effective cytotoxic T lymphocyte responses. J Exp Med 188:2199–2204. doi: 10.1084/jem.188.12.2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Onabajo OO, Mattapallil JJ. 2013. Expansion or depletion of T follicular helper cells during HIV infection: consequences for B cell responses. Curr HIV Res 11:595–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heeney JL. 2002. The critical role of CD4+ T-cell help in immunity to HIV. Vaccine 20:1961–1963. doi: 10.1016/S0264-410X(02)00078-6. [DOI] [PubMed] [Google Scholar]
- 16.Altfeld M, Rosenberg ES. 2000. The role of CD4(+) T helper cells in the cytotoxic T lymphocyte response to HIV-1. Curr Opin Immunol 12:375–380. doi: 10.1016/S0952-7915(00)00103-5. [DOI] [PubMed] [Google Scholar]
- 17.Yamane H, Paul WE. 2013. Early signaling events that underlie fate decisions of naive CD4+ T cells towards distinct T-helper cell subsets. Immunol Rev 252:12–23. doi: 10.1111/imr.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu J, Paul WE. 2010. Peripheral CD4 T cell differentiation regulated by networks of cytokines and transcription factors. Immunol Rev 238:247–262. doi: 10.1111/j.1600-065X.2010.00951.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekkens MJ, Shedlock DJ, Jung E, Troy A, Pearce EL, Shen H, Pearce EJ. 2007. Th1 and Th2 cells help CD8 T-cell responses. Infect Immun 75:2291–2296. doi: 10.1128/IAI.01328-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klatt NR, Brenchley JM. 2010. Th17 cell dynamics in HIV infection. Curr Opin HIV AIDS 5:135–140. doi: 10.1097/COH.0b013e3283364846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crotty S. 2011. Follicular helper CD4 T cells (TFH). Annu Rev Immunol 29:621–663. doi: 10.1146/annurev-immunol-031210-101400. [DOI] [PubMed] [Google Scholar]
- 22.Liu X, Nurieva RI, Dong C. 2013. Transcriptional regulation of folicular T-helper (Tfh) cells. Immunol Rev 252:139–145. doi: 10.1111/imr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linterman MA, Liston A, Vinuesa CG. 2012. T-follicular helper cell differentiation and the co-option of this pathway by non-helper cells. Immunol Rev 247:143–159. doi: 10.1111/j.1600-065X.2012.01121.x. [DOI] [PubMed] [Google Scholar]
- 24.Vinuesa CG. 2012. HIV and T follicular helper cells: a dangerous relationship. J Clin Investig 122:3059–3062. doi: 10.1172/JCI65175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKinstry KK, Strutt TM, Swain SL. 2010. Regulation of CD4+ T-cell contraction during pathogen challenge. Immunol Rev 236:110–124. doi: 10.1111/j.1600-065X.2010.00921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bour-Jordan H, Bluestone JA. 2009. Regulating the regulators: costimulatory signals control the homeostatsis and function of regulatory T cells. Immunol Rev 229:41–66. doi: 10.1111/j.1600-065X.2009.00775.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brenchley JM, Paiardini M, Knox KS, Asher AI, Cervasi B, Asher TE, Scheinberg P, Price DA, Hage CA, Kholi LM, Khoruts A, Frank I, Else J, Schacker T, Silvestri G, Douek DC. 2008. Differential Th17 CD4 T-cell depletion in pathogenic and nonpathogenic lentiviral infections. Blood 112:2826–2835. doi: 10.1182/blood-2008-05-159301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Estes JD, Harris LD, Klatt NR, Tabb B, Pittaluga S, Paiardini M, Barclay GR, Smedley J, Pung R, Oliveira KM, Hirsch VM, Silvestri G, Douek DC, Miller CJ, Haase AT, Lifson J, Brenchley JM. 2010. Damaged intestinal epithelial integrity linked to microbial translocation in pathogenic simian immunodeficiency virus infections. PLoS Pathog 6:e1001052. doi: 10.1371/journal.ppat.1001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Endres MJ, Clapham PR, Marsh M, Ahuja M, Turner JD, McKnight A, Thomas JF, Stoebenau-Haggarty B, Choe S, Vance PJ, Wells TN, Power CA, Sutterwala SS, Doms RW, Landau NR, Hoxie JA. 1996. CD4-independent infection by HIV-2 is mediated by fusin/CXCR4. Cell 87:745–756. doi: 10.1016/S0092-8674(00)81393-8. [DOI] [PubMed] [Google Scholar]
- 30.LaBranche CC, Hoffman TL, Romano J, Haggarty BS, Edwards TG, Matthews TJ, Doms RW, Hoxie JA. 1999. Determinants of CD4 independence for a human immunodeficiency virus type 1 variant map outside regions required for coreceptor specificity. J Virol 73:10310–10319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin G, Lee B, Haggarty BS, Doms RW, Hoxie JA. 2001. CD4-independent use of rhesus CCR5 by human immunodeficiency virus type 2 implicates an electrostatic interaction between the CCR5 N terminus and the gp120 C4 domain. J Virol 75:10766–10778. doi: 10.1128/JVI.75.22.10766-10778.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puffer BA, Pöhlmann S, Edinger AL, Carlin D, Sanchez MD, Reitter J, Watry DD, Fox HS, Desrosiers RC, Doms RW. 2002. CD4 Independence of simian immunodeficiency virus Envs is associated with macrophage tropism, neutralization sensitivity, and attenuated pathogenicity. J Virol 76:2595–2605. doi: 10.1128/JVI.76.6.2595-2605.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puffer BA, Altamura LA, Pierson TC, Doms RW. 2004. Determinants within gp120 and gp41 contribute to CD4 independence of SIV Envs. Virology 327:16–25. doi: 10.1016/j.virol.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 34.Kolchinsky P, Mirzabekov T, Farzan M, Kiprilov E, Cayabyab M, Mooney LJ, Choe H, Sodroski J. 1999. Adaptation of a CCR5-using, primary human immunodeficiency virus type 1 isolate for CD4-independent replication. J Virol 73:8120–8126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kolchinsky P, Kiprilov E, Bartley P, Rubinstein R, Sodroski J. 2001. Loss of a single N-linked glycan allows CD4-independent human immunodeficiency virus type 1 infection by altering the position of the gp120 V1/V2 variable loops. J Virol 75:3435–3443. doi: 10.1128/JVI.75.7.3435-3443.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dumonceaux J, Nisole S, Chanel C, Quivet L, Amara A, Baleux F, Briand P, Hazan U. 1998. Spontaneous mutations in the env gene of the human immunodeficiency virus type 1 NDK isolate are associated with a CD4-independent entry phenotype. J Virol 72:512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dumonceaux J, Goujon C, Joliot V, Briand P, Hazan U. 2001. Determination of essential amino acids involved in the CD4-independent tropism of the X4 human immunodeficiency virus type 1 m7NDK isolate: role of potential N glycosylations in the C2 and V3 regions of gp120. J Virol 75:5425–5428. doi: 10.1128/JVI.75.11.5425-5428.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boyd DF, Peterson D, Haggarty BS, Jordan APO, Hogan MJ, Goo L, Hoxie JA, Overbaugh J. 2015. Mutations in HIV-1 envelope that enhance entry with the macaque CD4 receptor alter antibody recognition by disrupting quaternary interactions within the trimer. J Virol 89:894–907. doi: 10.1128/JVI.02680-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoffman TL, LaBranche CC, Zhang W, Canziani G, Robinson J, Chaiken I, Hoxie JA, Doms RW. 1999. Stable exposure of the coreceptor-binding site in a CD4-independent HIV-1 envelope protein. Proc Natl Acad Sci USA 96:6359–6364. doi: 10.1073/pnas.96.11.6359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edwards TG, Hoffman TL, LaBranche CC, Romano J, Adkinson J, Sharron M, Hoxie JA, Doms RW. 2001. Relationships between CD4 independence, neutralization sensitivity, and exposure of a CD4-induced epitope in a human immunodeficiency virus type 1 envelope protein. J Virol 75:5230–5239. doi: 10.1128/JVI.75.11.5230-5239.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.White TA, Bartesaghi A, Borgnia MJ, Meyerson JR, de la Cruz MJV, Bess JW, Nandwani R, Hoxie JA, Lifson JD, Milne JLS, Subramaniam S. 2010. Molecular architectures of trimeric SIV and HIV-1 envelope glycoproteins on intact viruses: strain-dependent variation in quaternary structure. PLoS Pathog 6:e1001249. doi: 10.1371/journal.ppat.1001249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.White TA, Bartesaghi A, Borgnia MJ, de la Cruz MJV, Nandwani R, Hoxie JA, Bess JW, Lifson JD, Milne JLS, Subramaniam S. 2011. Three-dimensional structures of soluble CD4-bound states of trimeric simian immunodeficiency virus envelope glycoproteins determined by using cryo-electron tomography. J Virol 85:12114–12123. doi: 10.1128/JVI.05297-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flaherty MT, Hauer DA, Mankowski JL, Zink MC, Clements JE. 1997. Molecular and biological characterization of a neurovirulent molecular clone of simian immunodeficiency virus. J Virol 71:5790–5798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mori K, Ringler DJ, Kodama T, Desrosiers RC. 1992. Complex determinants of macrophage tropism in env of simian immunodeficiency virus. J Virol 66:2067–2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banapour B, Marthas ML, Ramos RA, Lohman BL, Unger RE, Gardner MB, Pedersen NC, Luciw PA. 1991. Identification of viral determinants of macrophage tropism for simian immunodeficiency virus SIVmac. J Virol 65:5798–5805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ortiz AM, Klatt NR, Li B, Yi Y, Tabb B, Hao XP, Sternberg L, Lawson B, Carnathan PM, Cramer EM, Engram JC, Little DM, Ryzhova E, Gonzalez-scarano F, Paiardini M, Ansari AA, Ratcliffe S, Else JG, Brenchley JM, Collman RG, Estes JD, Derdeyn CA, Silvestri G. 2011. Depletion of CD4+ T cells abrogates post-peak decline of viremia in SIV-infected rhesus macaques. J Clin Investig 121:4433–4445. doi: 10.1172/JCI46023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kolchinsky P, Kiprilov E. 2001. Increased neutralization sensitivity of CD4-independent human immunodeficiency virus variants. J Virol 75:2041–2050. doi: 10.1128/JVI.75.5.2041-2050.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Francella N, Gwyn SE, Yi Y, Li B, Xiao P, Elliott STC, Ortiz AM, Hoxie JA, Paiardini M, Silvestri G, Derdeyn CA, Collman RG. 2013. CD4+ T cells support production of simian immunodeficiency virus Env antibodies that enforce CD4-dependent entry and shape tropism in vivo. J Virol 87:9719–9732. doi: 10.1128/JVI.01254-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Francella N, Elliott ST, Yi Y, Gwyn SE, Ortiz AM, Li B, Silvestri G, Paiardini M, Derdeyn CA, Collman RG. 2013. Decreased plasticity of coreceptor use by CD4-independent SIV Envs that emerge in vivo. Retrovirology 10:133. doi: 10.1186/1742-4690-10-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mori K, Rosenzweig M, Desrosiers RC. 2000. Mechanisms for adaptation of simian immunodeficiency virus to replication in alveolar macrophages. J Virol 74:10852–10859. doi: 10.1128/JVI.74.22.10852-10859.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mankowski JL, Flaherty MT, Spelman JP, Hauer DA, Didier PJ, Amedee AM, Murphey-Corb M, Kirstein LM, Muñoz A, Clements JE, Zink MC. 1997. Pathogenesis of simian immunodeficiency virus encephalitis: viral determinants of neurovirulence. J Virol 71:6055–6060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Banapour B, Marthas ML, Munn RJ, Luciw PA. 1991. In vitro macrophage tropism of pathogenic and nonpathogenic molecular clones of simian immunodeficiency virus (SIVmac). Virology 183:12–19. doi: 10.1016/0042-6822(91)90113-P. [DOI] [PubMed] [Google Scholar]
- 53.Micci L, Alvarez X, Iriele RI, Ortiz AM, Ryan ES, McGary CS, Deleage C, McAtee BB, He T, Apetrei C, Easley K, Pahwa S, Collman RG, Derdeyn CA, Davenport MP, Estes JD, Silvestri G, Lackner AA, Paiardini M. 2014. CD4 Depletion in SIV-infected macaques results in macrophage and microglia infection with rapid turnover of infected cells. PLoS Pathog 10:e1004467. doi: 10.1371/journal.ppat.1004467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Joseph SB, Arrildt KT, Swanstrom AE, Schnell G, Lee B, Hoxie JA, Swanstrom R. 2014. Quantification of entry phenotypes of macrophage-tropic HIV-1 across a wide range of CD4 densities. J Virol 88:1858–1869. doi: 10.1128/JVI.02477-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gorry PR, Taylor J, Holm GH, Mehle A, Morgan T, Cayabyab M, Farzan M, Wang H, Bell JE, Kunstman K, Moore JP, Wolinsky SM, Gabuzda D. 2002. Increased CCR5 affinity and reduced CCR5/CD4 dependence of a neurovirulent primary human immunodeficiency virus type 1 isolate. J Virol 76:6277–6292. doi: 10.1128/JVI.76.12.6277-6292.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li G-H, Anderson C, Jaeger L, Do T, Major EO, Nath A. 2015. Cell-to-cell contact facilitates HIV transmission from lymphocytes to astrocytes via CXCR4. AIDS 29:755–766. doi: 10.1097/QAD.0000000000000605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bhattacharya J, Peters PJ, Clapham PR. 2003. CD4-independent infection of HIV and SIV: implications for envelope conformation and cell tropism in vivo. AIDS 17:S35–S43. doi: 10.1097/00002030-200317004-00004. [DOI] [PubMed] [Google Scholar]
- 58.Edinger AL, Mankowski JL, Doranz BJ, Margulies BJ, Lee B, Rucker J, Sharron M, Hoffman TL, Berson JF, Zink MC, Hirsch VM, Clements JE, Doms RW. 1997. CD4-independent, CCR5-dependent infection of brain capillary endothelial cells by a neurovirulent simian immunodeficiency virus strain. Proc Natl Acad Sci U S A 94:14742–14747. doi: 10.1073/pnas.94.26.14742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yen P-J, Mefford ME, Hoxie JA, Williams KC, Desrosiers RC, Gabuzda D. 2014. Identification and characterization of a macrophage-tropic SIV envelope glycoprotein variant in blood from early infection in SIVmac251-infected macaques. Virology 458-459:53–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yen P-J, Herschhorn A, Haim H, Salas I, Gu C, Sodroski J, Gabuzda D. 2014. Loss of a conserved N-linked glycosylation site in the simian immunodeficiency virus envelope glycoprotein V2 region enhances macrophage tropism by increasing CD4-independent cell-to-cell transmission. J Virol 88:5014–5028. doi: 10.1128/JVI.02785-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reeves JD, Hibbitts S, Simmons G, McKnight A, Azevedo-Pereira JM, Moniz-Pereira J, Clapham PR. 1999. Primary human immunodeficiency virus type 2 (HIV-2) isolates infect CD4-negative cells via CCR5 and CXCR4: comparison with HIV-1 and simian immunodeficiency virus and relevance to cell tropism in vivo. J Virol 73:7795–7804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hoxie JA, Labranche CC, Endres MJ, Turner JD, Berson JF, Doms RW, Matthews TJ. 1998. CD4-independent utilization of the CXCR4 chemokine receptor by HIV-1 and HIV-2. J Reprod Immunol 41:197–211. doi: 10.1016/S0165-0378(98)00059-X. [DOI] [PubMed] [Google Scholar]
- 63.Gallo SA, Puri A, Blumenthal R. 2001. HIV-1 gp41 six-helix bundle formation occurs rapidly after the engagement of gp120 by CXCR4 in the HIV-1 Env-mediated fusion process. Biochemistry 40:12231–12236. doi: 10.1021/bi0155596. [DOI] [PubMed] [Google Scholar]
- 64.Finzi A, Pacheco B, Xiang S-H, Pancera M, Herschhorn A, Wang L, Zeng X, Desormeaux A, Kwong PD, Sodroski J. 2012. Lineage-specific differences between human and simian immunodeficiency virus regulation of gp120 trimer association and CD4 binding. J Virol 86:8974–8986. doi: 10.1128/JVI.01076-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pancera M, Majeed S, Ban Y-EA, Chen L, Huang C, Kong L, Kwon Y Do, Stuckey J, Zhou T, Robinson JE, Schief WR, Sodroski J, Wyatt R, Kwong PD. 2010. Structure of HIV-1 gp120 with gp41-interactive region reveals layered envelope architecture and basis of conformational mobility. Proc Natl Acad Sci U S A 107:1166–1171. doi: 10.1073/pnas.0911004107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li Y, Migueles SA, Welcher B, Svehla K, Phogat A, Louder MK, Wu X, Shaw GM, Connors M, Wyatt RT, Mascola JR. 2007. Broad HIV-1 neutralization mediated by CD4-binding site antibodies. Nat Med 13:1032–1034. doi: 10.1038/nm1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Arthos J, Deen KC, Chaikin MA, Fornwald JA, Sathe G, Sattentau QJ, Clapham PR, Weiss RA, McDougal JS, Pietropaolo C. 1989. Identification of the residues in human CD4 critical for the binding of HIV. Cell 57:469–481. doi: 10.1016/0092-8674(89)90922-7. [DOI] [PubMed] [Google Scholar]
- 68.Wu H, Myszka DG, Tendian SW, Brouillette CG, Sweet RW, Chaiken IM, Hendrickson WA. 1996. Kinetic and structural analysis of mutant CD4 receptors that are defective in HIV gp120 binding. Proc Natl Acad Sci U S A 93:15030–15035. doi: 10.1073/pnas.93.26.15030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ryzhova E, Whitbeck JC, Canziani G, Westmoreland SV, Cohen GH, Eisenberg RJ, Lackner A, González-Scarano F. 2002. Rapid progression to simian AIDS can be accompanied by selection of CD4-independent gp120 variants with impaired ability to bind CD4. J Virol 76:7903–7909. doi: 10.1128/JVI.76.15.7903-7909.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Del Prete GQ, Leslie GJ, Haggarty B, Jordan APO, Romano J, Hoxie JA. 2010. Distinct molecular pathways to X4 tropism for a V3-truncated human immunodeficiency virus type 1 lead to differential coreceptor interactions and sensitivity to a CXCR4 antagonist. J Virol 84:8777–8789. doi: 10.1128/JVI.00333-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Del Prete GQ, Haggarty B, Leslie GJ, Jordan APO, Romano J, Wang N, Wang J, Holmes MC, Montefiori DC, Hoxie JA. 2009. Derivation and characterization of a simian immunodeficiency virus SIVmac239 variant with tropism for CXCR4. J Virol 83:9911–9922. doi: 10.1128/JVI.00533-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kestler H, Kodama T, Ringler D, Marthas M, Pedersen N, Lackner AA, Regier D, Sehgal P, Daniel M, King N. 1990. Induction of AIDS in rhesus monkeys by molecularly cloned simian immunodeficiency virus. Science 248:1109–1112. doi: 10.1126/science.2160735. [DOI] [PubMed] [Google Scholar]
- 73.Rucker J, Doranz BJ, Edinger AL, Long D, Berson JF, Doms RW. 1997. Cell-cell fusion assay to study the role of chemokine receptors in human immunodeficiency virus type 1 entry. Methods Enzymol 288:118–133. [DOI] [PubMed] [Google Scholar]
- 74.Edinger A, Doms RW. 1999. A cell-cell fusion assay to monitor HIV-1 Env interactions with chemokine receptors. Methods Mol Med 17:41–49. [DOI] [PubMed] [Google Scholar]
- 75.Montefiori DC. 2005. Evaluating neutralizing antibodies against HIV, SIV, and SHIV in luciferase reporter gene assays. Curr Protoc Immunol Chapter 12:Unit 12.11. [DOI] [PubMed] [Google Scholar]
- 76.LaBranche CC, Sauter MM, Haggarty BS, Vance PJ, Romano J, Hart TK, Bugelski PJ, Hoxie JA. 1994. Biological, molecular, and structural analysis of a cytopathic variant from a molecularly cloned simian immunodeficiency virus. J Virol 68:7665–7667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Edinger AL, Ahuja M, Sung T, Baxter KC, Haggarty B, Doms RW, Hoxie JA. 2000. Characterization and epitope mapping of neutralizing monoclonal antibodies produced by immunization with oligomeric simian immunodeficiency virus envelope protein. J Virol 74:7922–7935. doi: 10.1128/JVI.74.17.7922-7935.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Robinson JE, Cole KS, Elliott DH, Lam H, Amedee AM, Means R, Desrosiers RC, Clements J, Montelaro RC, Murphey-Corb M. 1998. Production and characterization of SIV envelope-specific rhesus monoclonal antibodies from a macaque asymptomatically infected with a live SIV vaccine. AIDS Res Hum Retrovir 14:1253–1262. doi: 10.1089/aid.1998.14.1253. [DOI] [PubMed] [Google Scholar]
- 79.Cole KS, Alvarez M, Elliott DH, Lam H, Martin E, Chau T, Micken K, Rowles JL, Clements JE, Murphey-Corb M, Montelaro RC, Robinson JE. 2001. Characterization of neutralization epitopes of simian immunodeficiency virus (SIV) recognized by rhesus monoclonal antibodies derived from monkeys infected with an attenuated SIV strain. Virology 290:59–73. doi: 10.1006/viro.2001.1144. [DOI] [PubMed] [Google Scholar]
- 80.Robinson JE, Holton D, Pacheco-Morell S, Liu J, McMurdo H. 1990. Identification of conserved and variant epitopes of human immunodeficiency virus type 1 (HIV-1) gp120 by human monoclonal antibodies produced by EBV-transformed cell lines. AIDS Res Hum Retrovir 6:567–579. doi: 10.1089/aid.1990.6.567. [DOI] [PubMed] [Google Scholar]
- 81.Kong R, Li H, Georgiev I, Changela A, Bibollet-Ruche F, Decker JM, Rowland-Jones SL, Jaye A, Guan Y, Lewis GK, Langedijk JPM, Hahn BH, Kwong PD, Robinson JE, Shaw GM. 2012. Epitope mapping of broadly neutralizing HIV-2 human monoclonal antibodies. J Virol 86:12115–12128. doi: 10.1128/JVI.01632-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kodama T, Wooley DP, Naidu YM, Kestler HW, Daniel MD, Li Y, Desrosiers RC. 1989. Significance of premature stop codons in env of simian immunodeficiency virus. J Virol 63:4709–4714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lock M, Greenberg ME, Lafrate AJ, Swigut T, Muench J, Kirchhoff F, Shohdy N, Skowronski J. 1999. Two elements target SIV Nef to the AP-2 clathrin adaptor complex, but only one is required for the induction of CD4 endocytosis. EMBO J 18:2722–2733. doi: 10.1093/emboj/18.10.2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen BK, Gandhi R, Baltimore D. 1996. CD4 down-modulation during infection of human T cells with human immunodeficiency virus type 1 involves independent activities of vpu, env, and nef. J Virol 70:6044–6053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aiken C, Konner J, Landau NR, Lenburg ME, Trono D. 1994. Nef induces CD4 endocytosis: requirement for a critical dileucine motif in the membrane-proximal CD4 cytoplasmic domain. Cell 76:853–864. doi: 10.1016/0092-8674(94)90360-3. [DOI] [PubMed] [Google Scholar]
- 86.Piguet V, Schwartz O, Le Gall S, Trono D. 1999. The downregulation of CD4 and MHC-I by primate lentiviruses: a paradigm for the modulation of cell surface receptors. Immunol Rev 168:51–63. doi: 10.1111/j.1600-065X.1999.tb01282.x. [DOI] [PubMed] [Google Scholar]
- 87.Elliott STC, Wetzel KS, Francella N, Bryan S, Romero DC, Riddick NE, Shaheen F, Vanderford T, Derdeyn CA, Silvestri G, Paiardini M, Collman RG. 2015. Dualtropic CXCR6/CCR5 simian immunodeficiency virus (SIV) infection of sooty mangabey primary lymphocytes: distinct coreceptor use in natural versus pathogenic hosts of SIV. J Virol 89:9252–9261. doi: 10.1128/JVI.01236-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Puffer BA, Sharron M, Coughlan CM, Baribaud F, McManus CM, Lee B, David J, Price K, Horuk R, Tsang M, Doms RW. 2000. Expression and coreceptor function of APJ for primate immunodeficiency viruses. Virology 276:435–444. doi: 10.1006/viro.2000.0557. [DOI] [PubMed] [Google Scholar]
- 89.Rucker J, Edinger AL, Sharron M, Samson M, Lee B, Berson JF, Yi Y, Margulies B, Collman RG, Doranz BJ, Parmentier M, Doms RW. 1997. Utilization of chemokine receptors, orphan receptors, and herpesvirus-encoded receptors by diverse human and simian immunodeficiency viruses. J Virol 71:8999–9007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gautam R, Gaufin T, Butler I, Gautam A, Barnes M, Mandell D, Pattison M, Tatum C, Macfarland J, Monjure C, Marx PA, Pandrea I, Apetrei C. 2009. Simian immunodeficiency virus SIVrcm, a unique CCR2-tropic virus, selectively depletes memory CD4+ T cells in pigtailed macaques through expanded coreceptor usage in vivo. J Virol 83:7894–7908. doi: 10.1128/JVI.00444-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Edinger AL, Hoffman TL, Sharron M, Lee B, Dowd BO, Doms RW. 1998. Use of GPR1, GPR15, and STRL33 as coreceptors by diverse human immunodeficiency virus type 1 and simian immunodeficiency virus envelope proteins. Pathology 249:367–378. [DOI] [PubMed] [Google Scholar]
- 92.Deng HK, Unutmaz D, Kewal-Ramani VN, Littman DR. 1997. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature 388:296–300. doi: 10.1038/40894. [DOI] [PubMed] [Google Scholar]
- 93.Vodros D, Thorstensson R, Doms RW, Fenyo EM, Reeves JD. 2003. Evolution of coreceptor use and CD4-independence in envelope clones derived from SIVsm-infected macaques. Virology 316:17–28. doi: 10.1016/S0042-6822(03)00579-8. [DOI] [PubMed] [Google Scholar]
- 94.Johnston PB, Dubay JW, Hunter E. 1993. Truncations of the simian immunodeficiency virus transmembrane protein confer expanded virus host range by removing a block to virus entry into cells. J Virol 67:3077–3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kiene M, Marzi A, Urbanczyk A, Bertram S, Fisch T, Nehlmeier I, Gnirss K, Karsten CB, Palesch D, Münch J, Chiodi F, Pöhlmann S, Steffen I. 2012. The role of the alternative coreceptor GPR15 in SIV tropism for human cells. Virology 433:73–84. doi: 10.1016/j.virol.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 96.Margulies BJ, Hauer DA, Clements JE. 2001. Identification and comparison of eleven rhesus macaque chemokine receptors. AIDS Res Hum Retrovir 17:981–986. doi: 10.1089/088922201750290104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stephens EB, Galbreath D, Liu ZQ, Sahni M, Li Z, Lamb-Wharton R, Foresman L, Joag SV, Narayan O. 1997. Significance of macrophage tropism of SIV in the macaque model of HIV disease. J Leukoc Biol 62:12–19. [DOI] [PubMed] [Google Scholar]
- 98.Nyamweya S, Hegedus A, Jaye A, Rowland-Jones S, Flanagan KL, Macallan DC. 2013. Comparing HIV-1 and HIV-2 infection: Lessons for viral immunopathogenesis. Rev Med Virol 23:221–240. doi: 10.1002/rmv.1739. [DOI] [PubMed] [Google Scholar]
- 99.Clapham PR, McKnight A, Weiss RA. 1992. Human immunodeficiency virus type 2 infection and fusion of CD4-negative human cell lines: induction and enhancement by soluble CD4. J Virol 66:3531–3537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Musich T, Peters PJ, Duenas-Decamp MJ, Gonzalez-Perez MP, Robinson J, Zolla-Pazner S, Ball JK, Luzuriaga K, Clapham PR. 2011. A conserved determinant in the v1 loop of HIV-1 modulates the V3 loop to prime low CD4 use and macrophage infection. J Virol 85:2397–2405. doi: 10.1128/JVI.02187-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Luciw PA, Shaw KE, Unger RE, Planelles V, Stout MW, Lackner JE, Pratt-Lowe E, Leung NJ, Banapour B, Marthas ML. 1992. Genetic and biological comparisons of pathogenic and nonpathogenic molecular clones of simian immunodeficiency virus (SIVmac). AIDS Res Hum Retrovir 8:395–402. doi: 10.1089/aid.1992.8.395. [DOI] [PubMed] [Google Scholar]
- 102.Reeves JD, Schulz TF. 1997. The CD4-independent tropism of human immunodeficiency virus type 2 involves several regions of the envelope protein and correlates with a reduced activation threshold for envelope-mediated fusion. J Virol 71:1453–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sanders RW, Derking R, Cupo A, Julien J-P, Yasmeen A, de Val N, Kim HJ, Blattner C, de la Peña AT, Korzun J, Golabek M, de Los Reyes K, Ketas TJ, van Gils MJ, King CR, Wilson IA, Ward AB, Klasse PJ, Moore JP. 2013. A next-generation cleaved, soluble HIV-1 Env trimer, BG505 SOSIP.664 gp140, expresses multiple epitopes for broadly neutralizing but not non-neutralizing antibodies. PLoS Pathog 9:e1003618. doi: 10.1371/journal.ppat.1003618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lyumkis D, Julien J-P, de Val N, Cupo A, Potter CS, Klasse PJ, Burton DR, Sanders RW, Moore JP, Carragher B, Wilson IA, Ward AB. 2013. Cryo-EM structure of a fully glycosylated soluble cleaved HIV-1 Env trimer. Science 342:1484–1490. doi: 10.1126/science.1245627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Julien J-P, Cupo A, Sok D, Stanfield RL, Lyumkis D, Deller MC, Klasse P-J, Burton DR, Sanders RW, Moore JP, Ward AB, Wilson IA. 2013. Crystal structure of a soluble cleaved HIV-1 envelope trimer. Science 342:1477–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kwon YD, Finzi A, Wu X, Dogo-Isonagie C, Lee LK, Moore LR, Schmidt SD, Stuckey J, Yang Y, Zhou T, Zhu J, Vicic DA, Debnath AK, Shapiro L, Bewley CA, Mascola JR, Sodroski JG, Kwong PD. 2012. Unliganded HIV-1 gp120 core structures assume the CD4-bound conformation with regulation by quaternary interactions and variable loops. Proc Natl Acad Sci U S A 109:5663–5668. doi: 10.1073/pnas.1112391109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Haim H, Strack B, Kassa A, Madani N, Wang L, Courter JR, Princiotto A, McGee K, Pacheco B, Seaman MS, Smith AB, Sodroski J. 2011. Contribution of intrinsic reactivity of the HIV-1 envelope glycoproteins to CD4-independent infection and global inhibitor sensitivity. PLoS Pathog 7:e1002101. doi: 10.1371/journal.ppat.1002101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Haim H, Si Z, Madani N, Wang L, Courter JR, Princiotto A, Kassa A, DeGrace M, McGee-Estrada K, Mefford M, Gabuzda D, Smith AB, Sodroski J. 2009. Soluble CD4 and CD4-mimetic compounds inhibit HIV-1 infection by induction of a short-lived activated state. PLoS Pathog 5:e1000360. doi: 10.1371/journal.ppat.1000360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Courter JR, Madani N, Sodroski J, Schön A, Freire E, Kwong PD, Hendrickson WA, Chaiken IM, LaLonde JM, Smith AB. 2014. Structure-based design, synthesis and validation of CD4-mimetic small molecule inhibitors of HIV-1 entry: conversion of a viral entry agonist to an antagonist. Acc Chem Res 47:1228–1237. doi: 10.1021/ar4002735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kamanna K, Aneja R, Duffy C, Kubinski P, Rodrigo MD, Bailey LD, McFadden K, Schon A, Holmes A, Tuzer F, Contarino M, Freire E, Chaiken IM. 2013. Non-natural peptide triazole antagonists of HIV-1 envelope gp120. Chem Med Chem 8:322–328. doi: 10.1002/cmdc.201200422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Munro JB, Gorman J, Ma X, Zhou Z, Arthos J, Burton DR, Koff WC, Courter JR, Smith AB III, Kwong PD, Blanchard SC, Mothes W. 2014. Conformational dynamics of single HIV-1 envelope trimers on the surface of native virions. Science 346:759–763. doi: 10.1126/science.1254426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Blish CA, Nguyen M-A, Overbaugh J. 2008. Enhancing exposure of HIV-1 neutralization epitopes through mutations in gp41. PLoS Med 5:e9. doi: 10.1371/journal.pmed.0050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lovelace E, Xu H, Blish CA, Strong R, Overbaugh J. 2011. The role of amino acid changes in the human immunodeficiency virus type 1 transmembrane domain in antibody binding and neutralization. Virology 421:235–244. doi: 10.1016/j.virol.2011.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Thali M, Charles M, Furman C, Cavacini L, Posner M, Robinson J, Sodroski J. 1994. Resistance to neutralization by broadly reactive antibodies to the human immunodeficiency virus type 1 gp120 glycoprotein conferred by a gp41 amino acid change. J Virol 68:674–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Reitz MS, Wilson C, Naugle C, Gallo RC, Robert-Guroff M. 1988. Generation of a neutralization-resistant variant of HIV-1 is due to selection for a point mutation in the envelope gene. Cell 54:57–63. doi: 10.1016/0092-8674(88)90179-1. [DOI] [PubMed] [Google Scholar]
- 116.Mattapallil JJ, Douek DC, Hill B, Nishimura Y, Martin M, Roederer M. 2005. Massive infection and loss of memory CD4+ T cells in multiple tissues during acute SIV infection. Nature 434:1093–1097. doi: 10.1038/nature03501. [DOI] [PubMed] [Google Scholar]
- 117.Paiardini M, Cervasi B, Reyes-Aviles E, Micci L, Ortiz AM, Chahroudi A, Vinton C, Gordon SN, Bosinger SE, Francella N, Hallberg PL, Cramer E, Schlub T, Chan ML, Riddick NE, Collman RG, Apetrei C, Pandrea I, Else J, Munch J, Kirchhoff F, Davenport MP, Brenchley JM, Silvestri G. 2011. Low levels of SIV infection in sooty mangabey central memory CD4+ T cells are associated with limited CCR5 expression. Nat Med 17:830–836. doi: 10.1038/nm.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Riddick NE, Hermann EA, Loftin LM, Elliott ST, Wey WC, Cervasi B, Taaffe J, Engram JC, Li B, Else JG, Li Y, Hahn BH, Derdeyn CA, Sodora DL, Apetrei C, Paiardini M, Silvestri G, Collman RG. 2010. A novel CCR5 Mutation common in sooty mangabeys reveals SIVsmm infection of CCR5-null natural hosts and efficient alternative coreceptor use in vivo. PLoS Pathog 6:e1001064. doi: 10.1371/journal.ppat.1001064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pandrea I, Apetrei C, Gordon S, Barbercheck J, Dufour J, Bohm R, Sumpter B, Roques P, Marx PA, Hirsch VM, Kaur A, Lackner AA, Veazey RS, Silvestri G. 2007. Paucity of CD4+ CCR5+ T cells is a typical feature of natural SIV hosts. Blood 109:1069–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Veazey RS, DeMaria M, Chalifoux LV, Shvetz DE, Pauley DR, Knight HL, Rosenzweig M, Johnson RP, Desrosiers RC, Lackner AA. 1998. Gastrointestinal tract as a major site of CD4+ T cell depletion and viral replication in SIV infection. Science 280:427–431. doi: 10.1126/science.280.5362.427. [DOI] [PubMed] [Google Scholar]
- 121.Ling B, Veazey RS, Luckay A, Penedo C, Xu K, Lifson JD, Marx PA. 2002. SIV(mac) pathogenesis in rhesus macaques of Chinese and Indian origin compared with primary HIV infections in humans. AIDS 16:1489–1496. doi: 10.1097/00002030-200207260-00005. [DOI] [PubMed] [Google Scholar]
- 122.Klatt NR, Harris LD, Vinton CL, Sung H, Briant JA, Morcock D, McGinty JW, Lifson JD, Lafont BA, Martin A, Levine AD, Estes JD, Brenchley JM. 2010. Compromised gastrointestinal integrity in pigtail macaques is associated with increased microbial translocation, immune activation and IL-17 production in the absence of SIV infection. Mucosal Immun 3:387–398. doi: 10.1038/mi.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Brenchley JM. 2013. Mucosal immunity in human and simian immunodeficiency lentivirus infections. Mucosal Immunol 6:657–665. doi: 10.1038/mi.2013.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.