Abstract
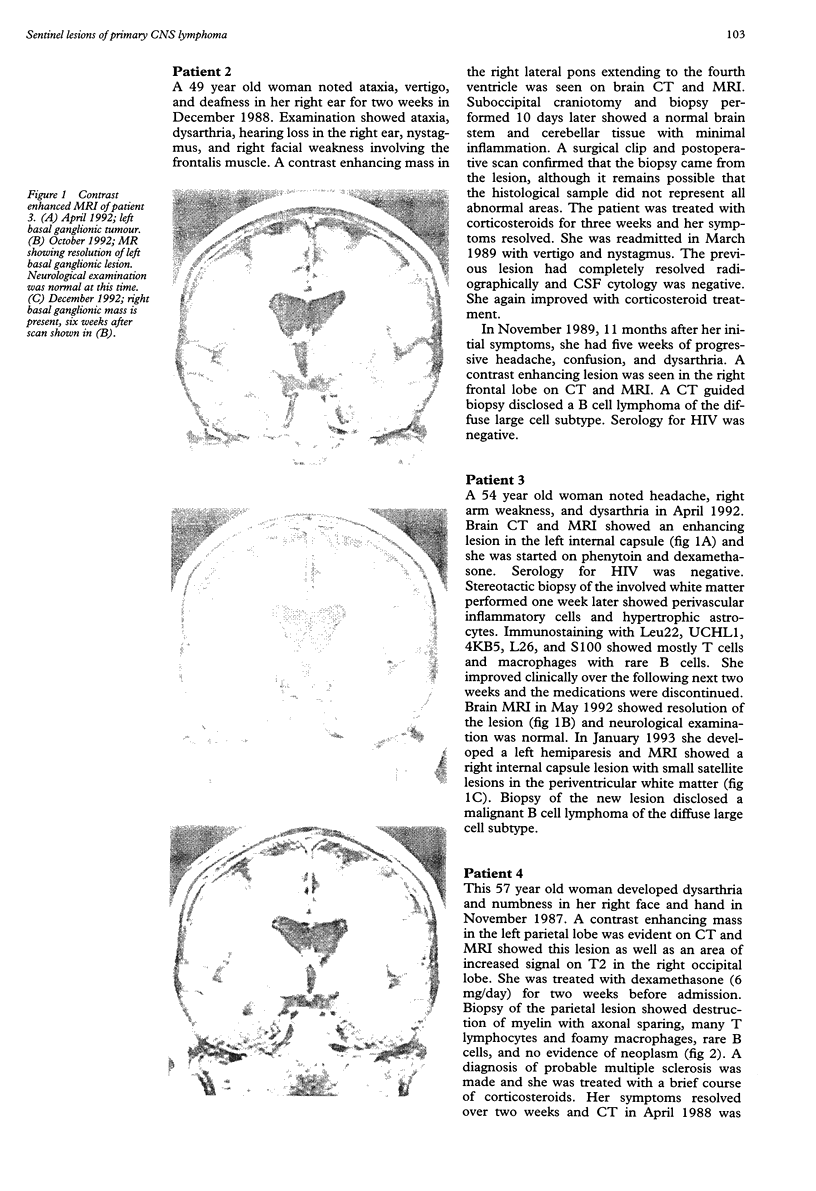
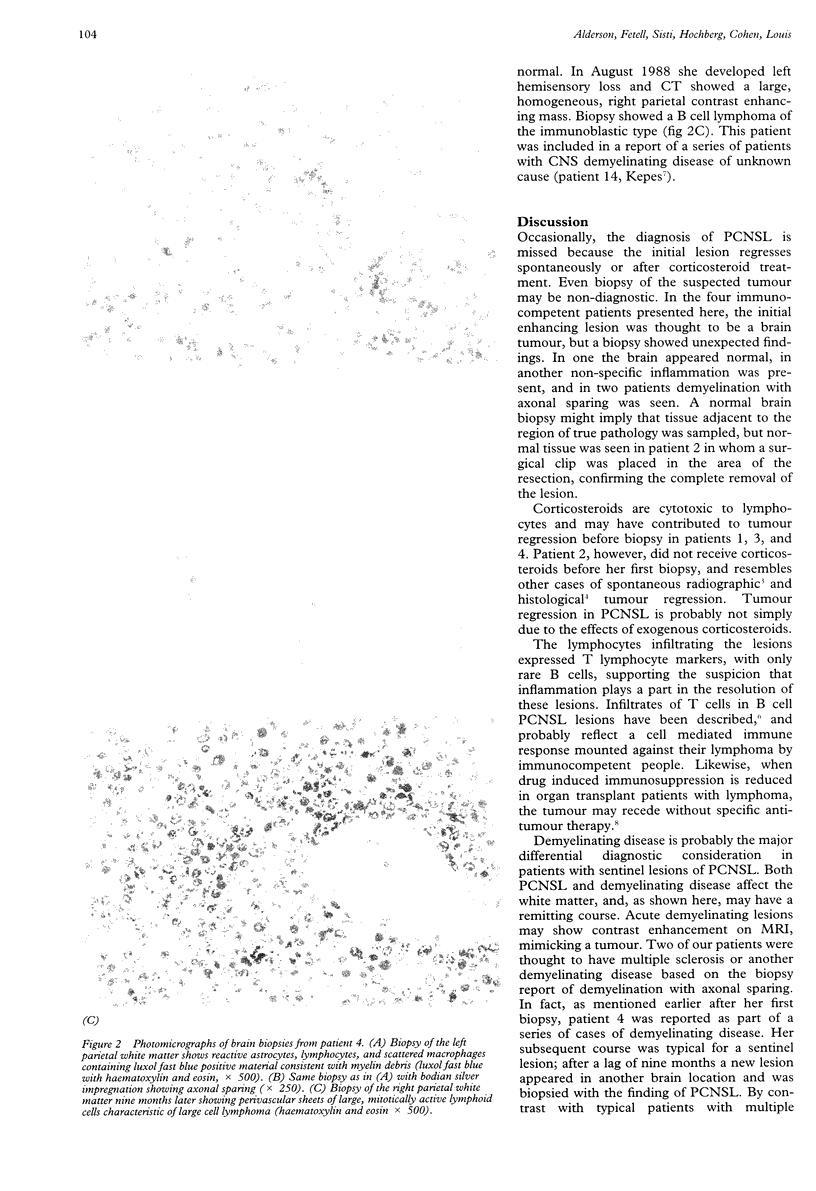
Some patients ultimately diagnosed with primary CNS lymphoma (PCNSL) have transient symptomatic contrast enhancing lesions. These "sentinel lesions" of PCNSL recede spontaneously or with corticosteroid treatment and present an important diagnostic dilemma because they show variable, but non-diagnostic histopathological features. Four previously healthy, immunocompetent patients aged 49 to 58 years had contrast enhancing intraparenchymal brain lesions. Before biopsy, three of the four were treated with corticosteroids. Initial biopsies showed demyelination with axonal sparing in two, non-specific inflammation in one, and normal brain in one. Infiltrating lymphocytes predominantly expressed T cell markers with rare B cells. All four patients recovered within two to four weeks after the initial biopsy and imaging studies showed resolution of the lesions. The CSF was normal in three of the four patients tested; oligoclonal bands were absent in both of the two tested. After seven to 11 months, each patient developed new symptomatic lesions in a different region of the brain, biopsy of which showed a B cell PCNSL. The mechanism of spontaneous involution of sentinel lesions is not understood, but may represent host immunity against the tumour. Sentinel lesions of PCNSL should be considered in patients with contrast enhancing focal parenchymal lesions that show non-specific or demyelinative histopathological changes. Close clinical and radiographic follow up is essential if PCNSL is to be diagnosed early in such patients.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bender G. P., Schapiro R. T. Primary CNS lymphoma presenting as multiple sclerosis. A case study. Minn Med. 1989 Mar;72(3):157–160. [PubMed] [Google Scholar]
- DeAngelis L. M. Primary central nervous system lymphoma imitates multiple sclerosis. J Neurooncol. 1990 Oct;9(2):177–181. doi: 10.1007/BF02427840. [DOI] [PubMed] [Google Scholar]
- Eby N. L., Grufferman S., Flannelly C. M., Schold S. C., Jr, Vogel F. S., Burger P. C. Increasing incidence of primary brain lymphoma in the US. Cancer. 1988 Dec 1;62(11):2461–2465. doi: 10.1002/1097-0142(19881201)62:11<2461::aid-cncr2820621135>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Kepes J. J. Large focal tumor-like demyelinating lesions of the brain: intermediate entity between multiple sclerosis and acute disseminated encephalomyelitis? A study of 31 patients. Ann Neurol. 1993 Jan;33(1):18–27. doi: 10.1002/ana.410330105. [DOI] [PubMed] [Google Scholar]
- Kuroda Y., Kawasaki T., Haraoka S., Fujiyama F., Kakigi R., Abe M., Tabuchi K., Kuroiwa T., Kishikawa T., Sugihara H. Autopsy report of primary CNS B-cell lymphoma indistinguishable from multiple sclerosis: diagnosis with the immunoglobulin gene rearrangements analysis. J Neurol Sci. 1992 Sep;111(2):173–179. doi: 10.1016/0022-510x(92)90065-s. [DOI] [PubMed] [Google Scholar]
- Meeker T., Lowder J., Cleary M. L., Stewart S., Warnke R., Sklar J., Levy R. Emergence of idiotype variants during treatment of B-cell lymphoma with anti-idiotype antibodies. N Engl J Med. 1985 Jun 27;312(26):1658–1665. doi: 10.1056/NEJM198506273122602. [DOI] [PubMed] [Google Scholar]
- Penn I. Cancers complicating organ transplantation. N Engl J Med. 1990 Dec 20;323(25):1767–1769. doi: 10.1056/NEJM199012203232510. [DOI] [PubMed] [Google Scholar]
- Starzl T. E., Nalesnik M. A., Porter K. A., Ho M., Iwatsuki S., Griffith B. P., Rosenthal J. T., Hakala T. R., Shaw B. W., Jr, Hardesty R. L. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet. 1984 Mar 17;1(8377):583–587. doi: 10.1016/s0140-6736(84)90994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaquero J., Martínez R., Rossi E., López R. Primary cerebral lymphoma: the "ghost tumor". Case report. J Neurosurg. 1984 Jan;60(1):174–176. doi: 10.3171/jns.1984.60.1.0174. [DOI] [PubMed] [Google Scholar]
- Weingarten K. L., Zimmerman R. D., Leeds N. E. Spontaneous regression of intracerebral lymphoma. Radiology. 1983 Dec;149(3):721–724. doi: 10.1148/radiology.149.3.6359262. [DOI] [PubMed] [Google Scholar]
- Williams R. S., Crowell R. M., Fisher C. M., Davis K., Lavyne M. H., Ropper A. H., Bremer A. M. Clinical and radiologic remission in reticulum cell sarcoma of the brain. Arch Neurol. 1979 Apr;36(4):206–210. doi: 10.1001/archneur.1979.00500400060009. [DOI] [PubMed] [Google Scholar]
- Yefenof E., Picker L. J., Scheuermann R. H., Tucker T. F., Vitetta E. S., Uhr J. W. Cancer dormancy: isolation and characterization of dormant lymphoma cells. Proc Natl Acad Sci U S A. 1993 Mar 1;90(5):1829–1833. doi: 10.1073/pnas.90.5.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]