Abstract
Nutritional strategies are vitally needed to aid in the management of obesity. Cross-sectional and epidemiologic studies consistently demonstrate that breakfast consumption is strongly associated with a healthy body weight. However, the intervention-based long-term evidence supporting a causal role of breakfast consumption is quite limited and appears to be influenced by several key dietary factors, such as dietary protein, fiber, and energy content. This article provides a comprehensive review of the intervention-based literature that examines the effects of breakfast consumption on markers of weight management and daily food intake. In addition, specific focus on the composition and size (i.e., energy content) of the breakfast meal is included. Overall, there is limited evidence supporting (or refuting) the daily consumption of breakfast for body weight management and daily food intake. In terms of whether the type of breakfast influences these outcomes, there is accumulating evidence supporting the consumption of increased dietary protein and fiber content at breakfast, as well as the consumption of more energy during the morning hours. However, the majority of the studies that manipulated breakfast composition and content did not control for habitual breakfast behaviors, nor did these studies include a breakfast-skipping control arm. Thus, it is unclear whether the addition of these types of breakfast plays a causal role in weight management. Future research, including large randomized controlled trials of longer-term (i.e., ≥6 mo) duration with a focus on key dietary factors, is critical to begin to assess whether breakfast recommendations are appropriate for the prevention and/or treatment of obesity.
Keywords: breakfast, weight loss, breakfast skipping, obesity, increased dietary protein, meal omission
Introduction
Obesity is the greatest threat to global health this century, affecting the lives of >1.4 billion adults (1). In the United States, ∼167 million adults (69%) are overweight/obese (2). The health consequences related to obesity can begin as early as childhood (3), and many overweight children and adolescents already have at least one, if not multiple, cardiovascular disease risk factors (4). Thus, there is a great need to develop successful nutrition strategies that target weight management to reverse the obesity epidemic and prevent or delay serious health complications. One factor that has received substantial attention is the dietary habit of skipping breakfast. Although breakfast was once thought to be the most important meal of the day, several investigators have challenged this notion because of the limited amount of existing scientific evidence (5, 6).
Breakfast consumption previously was considered a staple of the American diet (7–9); however, there has been an increased prevalence of skipping breakfast over the past 50 y, with as many as 30% of young people skipping breakfast every day and up to 60% eating breakfast infrequently (7, 10, 11). The increased frequency of skipping breakfast has occurred concomitant with the increased rise in obesity (8), raising the question of whether breakfast plays a causal role in weight management. The myriad epidemiologic, observational, and cross-sectional data document strong associations between breakfast consumption and markers of healthy weight management such that increased frequency of breakfast consumption is associated with lower BMI, lower weight and weight gain, and lower body fat (5, 12–17). In a recent meta-analysis (5), breakfast consumers were shown to display a greater OR of being classified as healthy weight than were those who skipped breakfast (P = 10−42). Despite the consistent evidence supporting the relation between breakfast consumption and weight management, there is a paucity of intervention-based evidence assessing whether the addition of breakfast improves weight-management outcomes (5). It is also unclear whether the composition and size of breakfast affect weight outcomes. Because current research demonstrates improvements in weight management with increased dietary protein, whole-grain/fiber consumption, and timing of food intake (18–20), it is plausible that these factors also might influence any proposed breakfast-related effects.
This article provides a comprehensive review of the intervention-based literature that examines the effects of breakfast consumption on weight management and daily food intake, with specific focus on breakfast composition and size.
Methodology for the Comprehensive Review
Breakfast is the first eating occasion of the day, before 1000; this was described previously by Timlin and Pereira (21). The search terms included breakfast (skipping) and morning fast, along with the following outcomes: weight (loss), fat mass (loss), percent body fat, BMI, waist circumference, and daily energy (food) intake.
Searches of electronic databases were carried out between 26 June 2014 and 28 July 2014, and included PubMed and Scopus. In addition, references from existing reviews and select articles were examined to supplement the electronic search.
This review was limited to articles published in English in peer-reviewed journals, and included the following criteria: 1) all age groups; 2) all diseases/conditions; 3) any breakfast intervention of ≥8 wk (for weight and body composition outcomes) and any duration for daily food intake; and 4) studies that included outcomes of weight, fat mass, body fat, lean mass/fat-free mass, BMI, waist circumference, or daily food (energy) intake. Epidemiologic, observational, and cross-sectional studies were excluded. The search flow diagrams for the weight outcomes and daily food intake are presented in Figures 1 and 2, respectively. All data is presented as mean ± SEM.
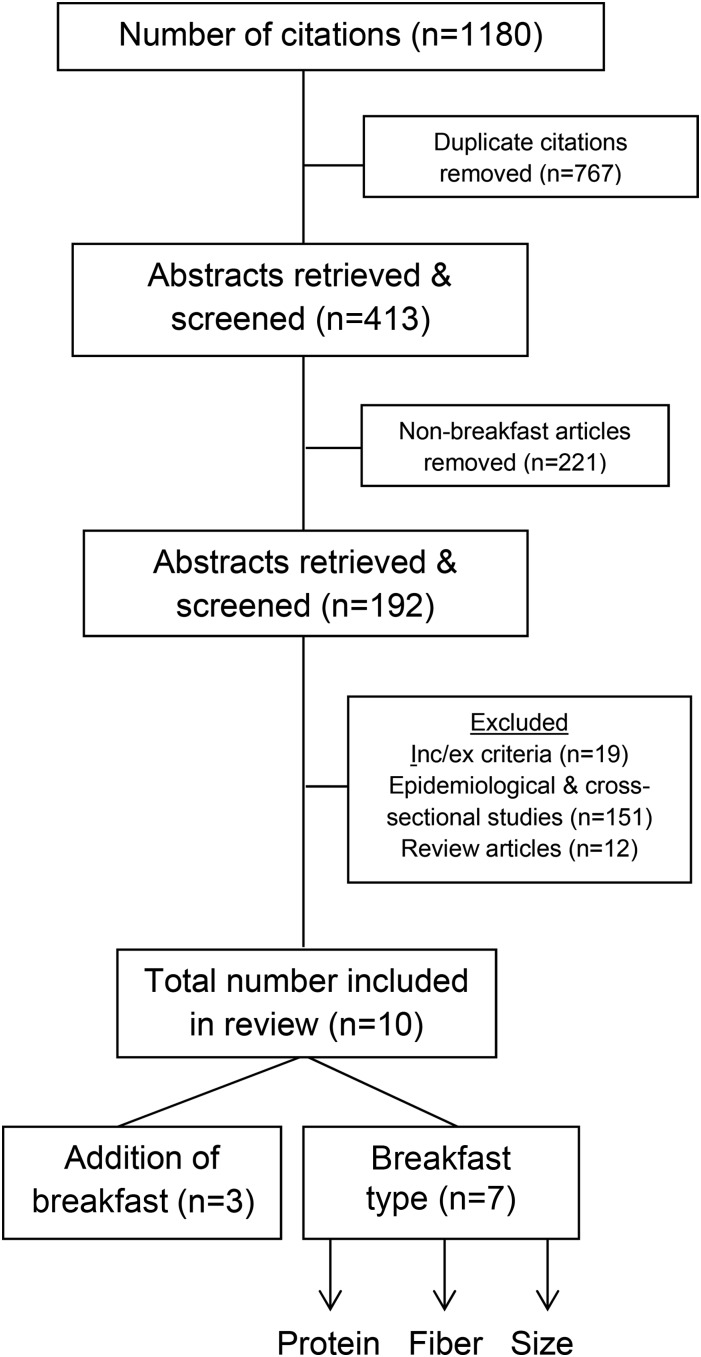
FIGURE 1.
Flow diagram of the selection process for the articles containing breakfast interventions and weight outcomes. Inc/ex, inclusion/exclusion.
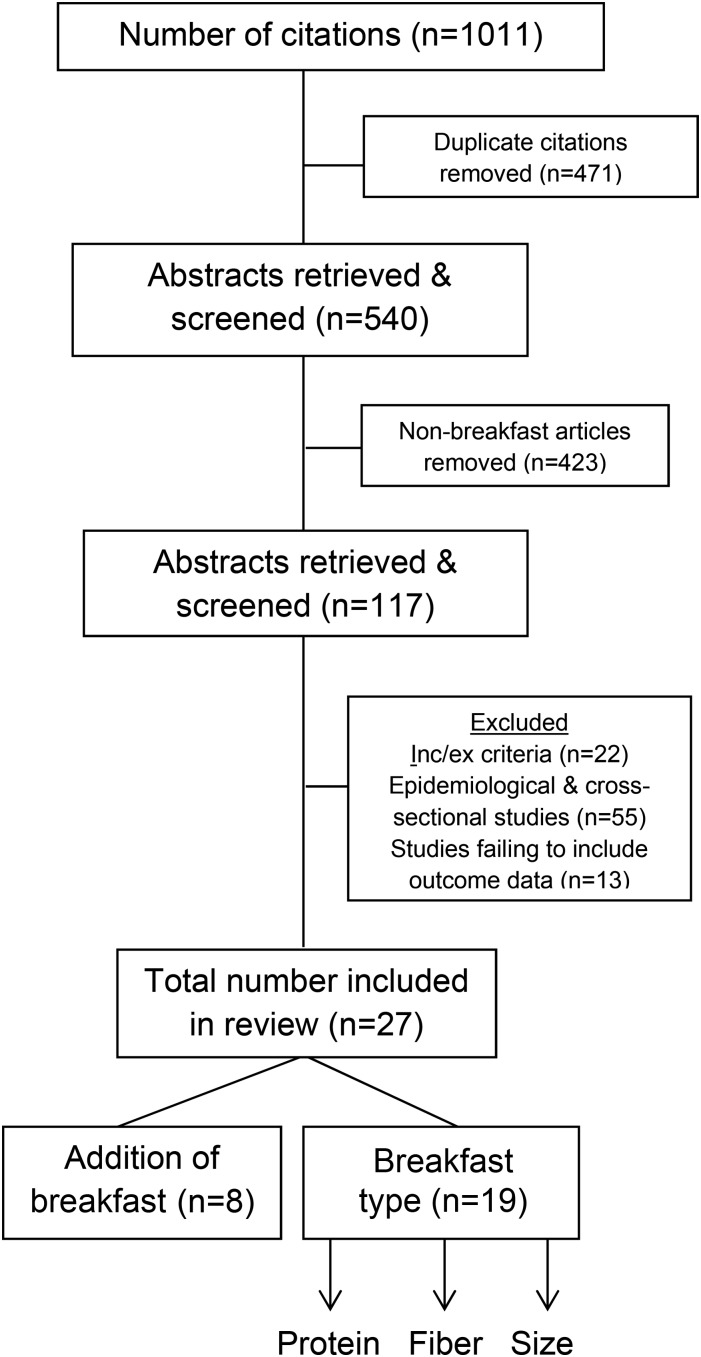
FIGURE 2.
Flow diagram of the selection process for the articles containing breakfast interventions and daily energy intake. Inc/ex, inclusion/exclusion.
Each article was graded based on the Academy of Nutrition and Dietetics’ article evaluation found within The Evidence Analysis Manual (22).
Intervention-Based Clinical Trials Including Weight Outcomes
Addition of breakfast
Only 3 long-term studies [albeit all randomized controlled trials (RCTs)] were identified that assessed whether the addition of breakfast influenced weight outcomes (Table 1). Schlundt et al. (23) examined the effects of consuming breakfast compared with skipping breakfast during a 12-wk energy-restricted diet in 52 obese adult women [age: 18–55 y; BMI (in kg/m2): 30–31). The women were initially stratified according to habitual breakfast behaviors, with skipping breakfast defined as having skipped breakfast on ≥3 occasions/wk. The participants then began the weight-reduction program, in which they were prescribed a 1200-kcal/d diet (50–55% carbohydrates, 15–20% protein, and 25–30% fat), and were randomly assigned to a breakfast-skipping group or a 400-kcal breakfast group. Although both groups consumed the isocaloric diets, the breakfast-skipping group was prescribed 400-kcal lunch and 800-kcal dinner meals, whereas the breakfast group was prescribed 400-kcal breakfast, 300-kcal lunch, and 500-kcal dinner meals. Weight loss was assessed at baseline and poststudy. Both groups lost weight throughout the 12-wk energy restriction (P < 0.001). However, no differences in weight loss were observed between the women who ate breakfast throughout the 12 wk (−7.7 ± 3.3 kg) and those who skipped breakfast (−6.1 ± 3.9 kg). In addition, habitual breakfast behavior (at baseline) did not significantly influence weight loss. The study included a 6-mo follow-up, which led to similar findings (data not shown).
TABLE 1.
Long-term trials lasting ≥8 wk investigating the effects of breakfast consumption on indexes of body weight and body composition1
| Study (reference) | Type of trial | Study length, wk | Characteristics | Study results | Important limitations |
| Breakfast skipping | |||||
| Schlundt et al. (23) | Randomized controlled trial | 12 | Breakfast skipping: no breakfast, lunch (400 kcal), dinner (800 kcal) | Breakfast skipping vs. breakfast and changes in weight: −7.7 ± 3.3 vs. −6.1 ± 3.9 kg; P > 0.05 (NS) | This was not a tightly controlled study, because the breakfasts were not provided. Also, the investigators wanted to maintain a 2-meal vs. 3-meal comparison. To do this, snacking was not permitted and, thus, habitual eating patterns were altered. |
| Breakfast: breakfast (400 kcal), lunch (300 kcal), dinner (500 kcal) | |||||
| Menus were given as guidelines and participants were taught to use food exchanges to plan meals | |||||
| Rosado et al. (24) | Randomized controlled trial | 12 | Control breakfast: habitual breakfast | Control vs. breakfast and changes in weight: +1.2 kg (0.4, 2.0 kg) vs. +1.03 kg (0.3, 0.7 kg); P > 0.05 (NS) | This was not a tightly controlled study, because the breakfasts were not provided in the breakfast group or documented in the control group. Also, the control group included habitual breakfast skippers and consumers. Finally, the dropout rate was fairly high at 31%. |
| Breakfast: 250 kcal; 14 g PRO, 47 g CHO, 1 g fat | Percentage fat: +0.4 (−0.5, 1.4) vs. +0.4 (−0.4, 1.1); P > 0.05 (NS) | ||||
| Prescribed 1 serving of ready-to-eat cereal with 250 mL skim milk | BMI (in kg/m2): +0.01 (−0.4, 0.4) vs. +0.1 (−0.3, 0.4); P > 0.05 (NS) | ||||
| Dhurandhar et al. (25) | Randomized controlled trial | 16 | Breakfast skipping: USDA pamphlet with instructions not to consume any calories before 1100 | Breakfast skipping, control breakfast, and breakfast, and changes in weight: −0.66 ± 1.18 kg, −0.62 ± 1.16 kg, and −0.68 ± 1.16 kg, respectively | This was not a tightly controlled study, because the breakfasts were not provided or prescribed. |
| Control: USDA pamphlet with instructions to maintain habitual breakfast habit | |||||
| Breakfast: USDA pamphlet with instructions to consume breakfast before 1000 every day; no specific restrictions | No main effect of breakfast was detected (P > 0.05, NS). | ||||
| Breakfast composition—protein | |||||
| Wang et al. (26) | Parallel design | 12 | High protein: 386 kcal; 12 g PRO, 29 g CHO, 16 g fat | High protein vs. normal protein and changes in weight: −3.9% vs. −0.2% of initial body weight (P < 0.001) | Breakfasts were not provided. The data are not presented with SD/SE. The protein differential between meals was extremely small (4 g) and the high-protein meal only contained 12 g PRO. |
| Normal protein: 386 kcal; 8 g PRO, 45 g CHO, 12 g fat | |||||
| Both meals contained white rice and milk. The high-protein breakfast included eggs; the normal protein included bread. | |||||
| Rueda and Khosla (27) | Parallel design | 14 | High protein: 1 serving eggs (2 whole eggs) | High protein vs. normal protein and changes in weight: no values given, P < 0.05 | Breakfasts were not provided. The breakfast prescription only included eggs and thus was not protein-specific, although the treatments ended up differing in protein content by ∼10 g. |
| Normal protein: no eggs | Fat mass: No values given, P < 0.05 | ||||
| Although consumption of eggs/no eggs was prescribed, the remainder of the breakfast meals in each group was otherwise uncontrolled. | |||||
| Jakubowicz et al. (28) | Parallel design | 12 | High protein: 600 kcal; 45 g PRO, 60 g CHO, 20 g fat | High protein vs. normal protein and changes in weight: −13.6 ± 2.3 kg vs. −15.3 ± 1.9 kg; P > 0.05 (NS) | Breakfasts were not provided. Energy content was also permitted to vary between meals, as were carbohydrate and fat content. |
| Normal protein: 300 kcal; 30 g PRO, 10 g CHO, 16 g fat | BMI: −4.8 vs. −5.4; P > 0.05 (NS) | ||||
| No recommendations outside of energy and macronutrient content were provided. | Waist circumference: −7.4 cm vs. −7.9 cm; P > 0.05 (NS) | ||||
| Rabinovitz et al. (29) | Parallel design | 12 | High protein: 430 kcal; 23 g PRO, 42 g CHO, 19 g fat | High protein vs. normal protein and changes in weight: −2.43 ± 0.46 kg vs. −1.86 ± 0.4 kg; P > 0.05 (NS) | Breakfasts were not provided. Energy content was also permitted to vary between meals, as were carbohydrate and fat content. |
| Normal protein: 210 kcal; 8 g PRO, 29 g CHO, 7 g fat | BMI: −0.88 ± 0.17 vs. −0.69 ± 0.15; P > 0.05 (NS) | ||||
| No recommendations outside of energy and macronutrient content were provided. | Waist circumference: −2.65 ± 0.66 cm vs. −2.2 ± 0.47 cm; P > 0.05 (NS) | ||||
| Breakfast composition—fiber | |||||
| Hu et al. (30) | Randomized controlled trial | 12 | High fiber: 309 kcal; 27.5 g fiber, 15 g PRO, 32 g CHO, 7 g fat | High fiber vs. low fiber and changes in weight: −0.68 ± 0.32 kg vs. −1.39 ± 0.36 kg; (P < 0.05) | Palatability of the biscuits was not directly assessed |
| Low fiber: 375 kcal; 3.2 g fiber, 12 g PRO, 62 g CHO, 7 g fat | Fat mass: −0.40 ± 0.14 kg vs. −0.71 ± 0.29 kg; P > 0.05 (NS) | ||||
| Biscuits were provided each day. The high-fiber biscuits contained soy fiber, whereas the low-fiber biscuits did not. | Waist circumference: −0.41 ± 0.15 cm vs. −1.75 ± 0.48 cm; P > 0.05 (NS) | ||||
| Breakfast size2 | |||||
| Jakubowicz et al. (31) | Parallel design | 12 | High calorie: 700 kcal; 54 g PRO, 84 g CHO | High calorie vs. low calorie and changes in weight: −8.7 ± 1.4 kg vs. −3.6 ± 1.5 kg; P < 0.0001 | Breakfasts were not provided |
| Low calorie: 200 kcal; 35 g PRO, 5.7 CHO | BMI: −3.1 vs. −1.3; P < 0.0001 | ||||
| No recommendations outside of energy and macronutrient content were provided. | Waist circumference: −8.5 ± 1.9 cm vs. −3.9 ± 1.4 cm; P < 0.0001 | ||||
| Lombardo et al. (32) | Parallel design | 12 | High calorie: 70% of daily calories in the morning (25% breakfast; ∼495 kcal; 31 g PRO, 56 g CHO, 16 g fat; 10% morning snack; 35% lunch); 10% afternoon snack; 20% dinner. | High calorie vs. low calorie and changes in weight: −8.2 ± 3.0 kg vs. −6.5 ± 3.4 kg; P < 0.03 | Breakfasts were not provided |
| Low calorie: 55% of daily calories in the morning (15% breakfast; ∼300 kcal; 19 g PRO, 34 g CHO, 10 g fat; 5% morning snack; 35% lunch); 15% afternoon snack; 30% dinner. | Fat mass: −6.8 ± 2.1 kg vs. −4.5 ± 2.9 kg; P < 0.03 | ||||
| No recommendations outside of energy and macronutrient content were provided. | BMI: −3.1 ± 0.2 vs. −1.8 ± 0.4; P < 0.05 | ||||
| Waist circumference: −7.0 ± 0.6 vs. −5.0 ± 0.3 cm; P < 0.05 | |||||
Rosado et al. (24) completed a 12-wk RCT in 147 children who were overweight or at risk of overweight (age: 9 ± 1 y; 90th BMI percentile for age). The breakfast group was prescribed 1 serving/d ready-to-eat cereals with milk (∼250 kcal; 14 g protein, 47 g carbohydrates, and 1 g fat), whereas the control group continued the breakfast habit to which they were accustomed. Changes in body weight, body fat [through bioelectrical impedance analysis (BIA)], and BMI were assessed at baseline and poststudy. Both groups gained weight over the 12 wk [breakfast group: +0.9 kg (95% CI: 0.4, 1.4 kg) and control group: +1.2 kg (95% CI: 0.4, 2.0 kg); both P < 0.05] with no differences between groups. In addition, no differences in BMI or percentage body fat changes were detected between groups (Table 1).
More recently, Dhurandhar et al. (25) completed a 16-wk study in 309 overweight/obese adults (age: 40 ± 0.3 y; BMI: 25–40). The participants initially were stratified according to habitual breakfast behaviors, with skipping breakfast defined as having skipped breakfast on ≥3 occasions/wk, and then were randomly assigned to the breakfast recommendations to eat breakfast, skip breakfast, or maintain their habitual breakfast behaviors. All groups were provided with the USDA “Let’s Eat for the Health of It” pamphlet, which included a general description of good nutrition habits (but did not discuss breakfast consumption). Along with this pamphlet, the breakfast group received an additional handout instructing them to eat breakfast before 1000. The handout suggested healthy food items to consume, but the participants could choose whatever they wished to eat. The breakfast-skipping group was also provided with a handout instructing the participants to avoid the consumption of any foods or drinks (besides water or zero-calorie beverages) before 1100. Again, no differences in weight loss were observed in those who ate breakfast throughout the 16 wk (−0.68 ± 1.16 kg) compared with those who skipped breakfast (−0.66 ± 1.18 kg) or those who continued their respective breakfast patterns (−0.62 ± 1.16 kg). Also, habitual breakfast behaviors (at baseline) did not influence the amount of weight lost throughout the study.
Collectively, the current evidence, albeit limited in study numbers and quality of study, does not support an effect of breakfast on weight outcomes. Although these findings suggest that breakfast does not play a causal role in weight management, the data should be viewed with caution because of several limitations. First, the small number of RCTs available during the time of the review (n = 3) presents challenges for developing conclusions regarding the role of breakfast in preventing and/or reducing weight gain. Furthermore, none of these studies tightly controlled key breakfast factors, including energy content, macronutrients, and/or breakfast quality (23–25), which might influence weight outcomes. Last, only the study by Rosado et al. (24) included other weight-related outcomes outside of weight loss, such as body composition and BMI. Thus, it is unclear whether substantial improvements in weight management would be observed after long-term studies that include tightly controlled breakfast meals varying in key dietary factors, such as macronutrient and/or energy content.
To provide additional support for the continuation of this line of research, we recently published a tightly controlled study to examine whether the daily consumption of high-protein compared with normal-protein breakfast meals improved weight management in overweight/obese breakfast-skipping young people (33). In this study, 57 adolescents (age: 19 ± 1 y; BMI: 29.7 ± 4.6) were randomly assigned to 1 of 3 patterns: 1) a high-protein breakfast (350 kcal; 35 g carbohydrates, 35 g protein, and 8 g fat); 2) a normal-protein breakfast (350 kcal; 57 g carbohydrates, 13 g protein, and 8 g fat); or 3) no breakfast (control). All breakfast meals were provided throughout the 12 wk. Weight loss and body composition (through DXA) were assessed at baseline and poststudy. No differences in weight loss were observed between groups. However, the high-protein breakfast prevented fat-mass gains over the 12 wk (−0.4 ± 0.5 kg) compared with continuing to skip breakfast (+1.6 ± 0.9 kg, P < 0.03), whereas the normal-protein breakfast did not prevent fat-mass gains (+0.3 ± 0.5 kg). Although preliminary, these data suggest a beneficial effect of including a protein-rich breakfast on weight management in individuals who habitually skip the morning meal. However, it is important to note that this was a 12-wk pilot study and was not powered to detect differences in weight loss and body composition. Further research exploring the effects of increased dietary protein at breakfast for a longer duration and in a larger sample size is necessary to strengthen these findings.
Breakfast composition and size
Whereas the previous section focused on the comparison between skipping breakfast and consuming breakfast, this section examines the effects of breakfast meals that vary in protein, fiber, and energy content.
Dietary protein.
Only 4 long-term studies were identified that tested whether increased protein consumption at breakfast improved weight outcomes. Wang et al. (26) compared the effects of a prescribed normal-protein, bread-based breakfast (386 kcal; 45 g carbohydrates, 8 g protein, and 12 g fat) and an isocaloric high-protein, egg-based breakfast (29 g carbohydrates, 12 g protein, and 16 g fat) in 156 obese adolescents (age: 14 ± 2 y; BMI: 32.1 ± 1.7). The bread breakfast consisted of steamed bread, white rice, and milk, whereas the egg breakfast consisted of boiled eggs (50 g), white rice, and milk. Weight loss was assessed at baseline and at 12 wk. The egg breakfast led to ∼4% more weight loss than did the bread breakfast (P < 0.001) (Table 1), which was a difference of ∼2.25 kg between groups (P < 0.001).
In a similar study, Rueda and Khosla (27) compared a non-egg breakfast and an egg breakfast in 73 college students (age: 17–20 y; BMI: 26.0 ± 3.4). The non-egg group was given a recommendation to simply avoid eating eggs 5 d/wk for 14 wk, whereas the egg group was instructed to eat 1 serving of eggs (i.e., equivalent to 2 whole eggs) 5 d/wk for 14 wk. Both groups were permitted to eat other breakfast foods ad libitum during breakfast. Breakfast energy and macronutrient content, weight loss, and changes in BMI and body composition (through BIA) were assessed at baseline and poststudy. On average, both groups consumed ∼640-kcal breakfasts. The non-egg breakfasts contained ∼104 g carbohydrates, 19 g protein, and 4 g fat, whereas the egg breakfasts contained ∼76 g carbohydrates, 26 g protein, and 26 g fat. Although both groups gained weight and fat mass throughout the study, no differences were observed between groups.
Finally, the remaining 2 studies (28, 29) manipulated protein content and breakfast size within an energy-restricted diet. As described in Jakubowicz et al. (28), 193 obese adults (age: 47 ± 7 y; BMI: 32.2 ± 1.0) were prescribed an energy-restricted diet (∼1500 kcal/d) and were randomly assigned to either a large high-protein/high-carbohydrate breakfast (600 kcal; 60 g carbohydrates, 45 g protein, and 20 g fat) or a small lower-protein/low-carbohydrate breakfast (300 kcal; 10 g carbohydrates, 30 g protein, and 16 g fat) for 16 wk followed by a 32-wk follow-up. Weight loss and changes in BMI and waist circumference were assessed at baseline, poststudy, and follow-up. Although both energy-restricted diets led to significant (P < 0.05) reductions in weight (−14.4 kg), BMI (−5.1), and waist circumference (−7.7 cm), no differences were detected between groups throughout the intervention (Table 1). However, at the end of the follow-up period, the group consuming the large high-protein/high-carbohydrate breakfast lost more weight (−20.6 kg) than did the group consuming the small lower-protein/low-carbohydrate breakfast (−3.5 kg, P < 0.001). The group consuming the large high-protein/high-carbohydrate breakfast also displayed greater reductions in BMI and waist circumference during the follow-up period than did the group consuming the small lower-protein/low-carbohydrate breakfast (data not shown).
In a similar study, Rabinovitz et al. (29) included 59 overweight and obese adults with type 2 diabetes (age: 60.7 ± 6.4 y; BMI: 32.4 ± 3.7) and implemented an energy-restricted diet (∼1400 kcal/d) for 12 wk. The participants were randomly assigned to either a large high-protein/high-fat breakfast (430 kcal; 42 g carbohydrates, 23 g protein, and 19 g fat) or a small lower-protein/low-fat breakfast (210 kcal; 29 g carbohydrates, 8 g protein, and 7 g fat). Weight loss and changes in body composition (through BIA), BMI, and waist circumference were assessed at baseline and poststudy. No differences in any of these weight indexes were observed between groups (Table 1).
In summary, although limited, there is some evidence illustrating modest improvements in weight management after the consumption of breakfast meals containing increased dietary protein compared with lower-protein versions. However, several limitations exist that greatly influence the study findings and implications. First, none of the studies included within this section of the review were RCTs, thus weakening the quality of the research. Second, in several studies (26, 27), the protein content of the high-protein breakfasts was fairly low (12 g protein) and/or the protein differential between the breakfast comparisons was quite small (i.e., only a 4- to 7-g protein difference between the lower and higher protein meals). In a recent review, ∼30 g protein (with a differential of ∼15 g protein between treatments) was suggested as eliciting effects on indexes of weight management (18). Thus, the reduced protein content included within these studies likely reduced the ability to identify a protein effect at breakfast. In addition, habitual breakfast behaviors were not assessed in any of these studies, which may have influenced the participants’ responses to the study breakfast interventions. Furthermore, none of the studies provided the breakfast foods for the participants to consume throughout the study, making it difficult to assess adherence accurately. Finally, 3 (27–29) of the 4 studies neglected to match key dietary characteristics, including fiber, energy density, and/or energy content. Thus, additional work involving full-feeding RCTs are needed to assess whether the implementation of a single dietary strategy, such as increased protein consumption at breakfast, improves weight management.
Dietary fiber.
The search with respect to the effect of increased dietary fiber at breakfast on weight outcomes yielded only one report (Table 1). Hu et al. (30) completed a 12-wk RCT in 39 overweight adults (age: 21 ± 5 y; BMI: 26 ± 0.5) in which a breakfast was provided each day consisting of either low-fiber (375 kcal; 3 g wheat fiber) or high-fiber (309 kcal; 28 g soy fiber) biscuits. Changes in body weight, body composition (through DXA), BMI, and waist circumference were assessed at baseline and poststudy. The high-fiber breakfast group experienced a 2% greater weight loss over the 12 wk than did the low-fiber breakfast controls (P < 0.05, Table 1). Furthermore, although no additional differences were detected between groups, only the high-fiber group displayed greater reductions in BMI, waist circumference, fat mass, and percentage body fat throughout the study (poststudy–prestudy, all P < 0.05). Although this is the only published study, to our knowledge, examining the long-term effects of fiber consumption at breakfast on weight management, the findings suggest a potential effect of fiber, specifically soy fiber, on weight loss and improvements in body composition. Additional RCTs are needed to replicate these data, as well as to explore whether similar findings occur with the incorporation of other types of fiber.
Breakfast size.
Our search identified 4 studies addressing breakfast size and weight management. All 4 studies included dietary energy restrictions in overweight/obese adults and were between 12 and 16 wk in duration (28, 29, 31, 32). Two of the studies (28, 29) were described previously, because protein content, along with energy content, were manipulated. Of those studies, only the one by Jakubowicz et al. (28) reported greater weight loss and greater reductions in BMI and waist circumference after the large breakfasts than after the small breakfasts; however, these differences were only detected at the end of the 32-wk follow-up period.
In a subsequent study (31), 93 overweight/obese women (age: 45.8 ± 7.1 y; BMI: 32.4 ± 1.8) with metabolic syndrome were assigned to an energy-restricted lower-carbohydrate diet (∼1400 kcal/d) for 12 wk and were randomly assigned to high-calorie (700 kcal) or low-calorie (200 kcal) breakfast groups. To make the diets isocaloric, the high-calorie breakfast group was prescribed a lower-calorie dinner (200 kcal), whereas the low-calorie breakfast group was prescribed a higher-calorie dinner (700 kcal). Lunch was matched at 500 kcal for both groups. The diets were also matched for macronutrient content (32% carbohydrates, 41% protein, and 27% fat). Weight loss and changes in BMI and waist circumference were assessed at baseline and poststudy. The group consuming the high-calorie breakfast experienced a 2.5-fold greater weight loss than did the group consuming the low-calorie breakfast (Table 1). In addition, greater reductions in BMI and waist circumference were observed with the high-calorie breakfast than with the low-calorie breakfast (both, P < 0.05; Table 1).
The last study in this section (32) included a 12-wk energy-restricted (600 kcal/d less than weight maintenance) Mediterranean-style diet (55% carbohydrates, 15% protein, and 30% fat) in 42 overweight/obese women (age: 60.7 ± 6.4 y; BMI: 32.4 ± 3.7). Unlike in the previous studies, Lombardo et al. (32) assessed the distribution of calories throughout the day instead of simply assessing breakfast per se. In this study, the participants were randomly prescribed a large or small morning distribution pattern. The large morning pattern contained 70% of daily calories with 25% (∼495 kcal) at breakfast, 10% at the morning snack, and 35% at lunch, whereas the small morning pattern contained 55% of daily calories with 15% (∼300 kcal) at breakfast, 5% during the morning snack, and 35% at lunch. Changes in body weight, body composition (through DXA), BMI, and waist circumference were assessed at baseline and poststudy. The large morning pattern led to 20% more weight loss over the 12 wk than did the small morning pattern (P < 0.03; Table 1). Furthermore, the large morning pattern led to greater reductions in BMI, waist circumference, and fat mass than did the small morning pattern (all, P < 0.05; Table 1).
Strong evidence is emerging to support the effect of redistributing calories toward the morning, particularly including a higher-calorie breakfast, for improvement in outcomes of weight management. However, it is important to note that these studies were not RCTs and did not tightly control the diet interventions. In addition, only 2 studies manipulated macronutrient content (in addition to breakfast size) and demonstrated a modest protein effect (28, 29). Regardless of the limitations, these studies provide a framework for future clinical trials to explore the timing and distribution of food intake for the prevention and/or treatment of obesity.
Intervention-Based Trials Including Daily Food Intake
The regulation of energy intake has been proposed as serving as one mediator of weight management. Subsequently, numerous studies have explored whether breakfast consumption reduces body weight through alterations in daily intake. The studies in this section include assessments of daily energy intake that were either directly measured through ad libitum consumption or estimated through dietary recalls and/or food records or diaries. In addition, the majority of these studies (n = 19; 83%) were acute trials in which the intervention occurred over a single day. A few studies (n = 3) (34–37) included subchronic durations between 1 and 6 wk, and only one of the studies was >8 wk (29).
Addition of breakfast.
The search yielded 8 studies in which breakfast skipping was compared with breakfast consumption, and many of the studies included different types of breakfasts within each study.
Approximately 21% of the comparisons (34, 35, 38, 39) demonstrated greater daily intake when consuming breakfast than when skipping breakfast; 5% (36) demonstrated lower daily intake with breakfast consumption than with skipping breakfast; and 74% (34, 40–42) elicited no differences in daily intake (Table 2). Although these summary data suggest that the effects of breakfast on daily intake remain uncertain, there are a few issues that must be considered.
TABLE 2.
Acute and long-term trials investigating the effects of breakfast consumption on daily energy intake1
| Study (reference) | Type of trial | Study length | Characteristics | Results of daily food intake, kcal/d |
| Leidy et al. (34) | Crossover design | 1-wk acclimation followed by the respective 8-h testing day/treatment | Breakfast skipping: 0 kcal; nothing before lunch | Breakfast skipping vs. normal protein: 2002 ± 111 vs. 2292 ± 115; P < 0.003 |
| Normal protein: 350 kcal; 13 g PRO, 57 g CHO, and 8 g fat | ||||
| High protein: 350 kcal; 35 g PRO, 35 g CHO, and 8 g fat | Breakfast skipping vs. high protein: 2002 ± 111 vs. 2123 ± 71; P > 0.05 (NS) | |||
| All meals provided | ||||
| Betts et al. (35) | Randomized controlled trial | 6 wk/treatment | Breakfast skipping: 0 kcal; nothing before 1200 | Breakfast skipping vs. breakfast: 2191 ± 494 vs. 2730 ± 573; P < 0.0007 |
| Breakfast: ≥700 kcal (before 1100; 50% within 2 h of waking) | ||||
| Meals were not provided | ||||
| Farshchi et al. (36) | Crossover design | 2-wk acclimation followed by the respective 4-h testing day/treatment | Breakfast skipping: 0 kcal | Breakfast skipping vs. breakfast: 1756 ± 155 vs. 1665 ± 141; P = 0.001 |
| Breakfast: 10 kcal/kg body weight | ||||
| 15% PRO, 50% CHO, and 35% fat | ||||
| All meals provided | ||||
| Kral et al. (38) | Crossover design | One 4-h testing day/treatment | Breakfast skipping: 0 kcal | Breakfast skipping vs. breakfast: 1830 vs. 2191; P < 0.05 |
| Breakfast cereals: 350 kcal; 11 g PRO, 69 g CHO, 4 g fat | ||||
| All breakfast meals provided | ||||
| Levitsky and Pacanowski (39) | Crossover design | 1 d/treatment | Breakfast skipping: 0 kcal | Breakfast skipping vs. breakfast: 400 fewer kcal consumed by breakfast skipping vs. breakfast; P < 0.01 |
| Breakfast: ad libitum; total offered: 218 kcal | ||||
| All foods provided | ||||
| Leidy and Racki (40) | Crossover design | 1 d/treatment | Breakfast skipping: 0 kcal; nothing before lunch | Breakfast skipping vs. normal protein: 2259 ± 280 vs. 2530 ± 212; P > 0.05 (NS) |
| Normal protein: 513 ± 26 kcal; 18 g PRO, 95 g CHO, 8 g fat | ||||
| High protein: 512 ± 26 kcal; 49 g PRO, 63 g CHO, 8 g fat | Breakfast skipping vs. high protein: 2259 ± 280 vs. 2505 ± 284; P > 0.05 (NS) | |||
| All meals provided | ||||
| Irvine et al. (41) | Crossover design | 1 d/treatment | Breakfast skipping: 0 kcal | Breakfast skipping vs. normal protein: 1488 ± 385 vs. 1663 ± 331, P > 0.05 (NS) |
| Normal protein: 250 kcal; 4 g PRO, 39 g CHO, 9 g fat | ||||
| High protein: 250 kcal; 20 g PRO, 39 g CHO, 2 g fat | Breakfast skipping vs. high protein: 1488 ± 385 vs. 1672 ± 368; P > 0.05 (NS) | |||
| All meals provided | ||||
| De Graaf et al. (42) | Crossover design | 1 d/treatment | Breakfast skipping: 8 kcal | Breakfast skipping vs. breakfasts: all comparisons, P > 0.05 (NS) |
| Breakfasts: high energy (400 kcal); medium energy (250 kcal); low energy (100 kcal) and high protein (70%); high carbohydrate (99%); and high fat (92%) | Numerical data not presented | |||
| All breakfast meals provided | ||||
| Breakfast composition—protein2 | ||||
| Stubbs et al. (43) | Randomized controlled trial | One 24-h testing day/treatment | High carbohydrate: 1237 kcal; 57 g PRO, 188 g CHO, and 29 g fat | High carbohydrate vs. high protein: 4006 ± 160 vs. 4022 ± 160, P > 0.05 (NS) |
| High fat: 1251 kcal; 64 g PRO, 70 g CHO, and 79 g fat | ||||
| High protein: 1263 kcal; 186 g PRO, 69 g CHO, and 27 g fat | High fat vs. high protein: 3867 ± 160 vs. 4022 ± 160; P > 0.05 (NS) | |||
| All meals provided | ||||
| Karhunen et al. (44) | Crossover design | 1 d/treatment | Low fiber–low protein: 300 kcal; 3 g PRO, 33 g CHO, and 14 g fat; 7.6 g fiber | Normal-protein versions vs. high-protein versions: P > 0.05 (NS) |
| Low fiber–high protein: 300 kcal; 20 g PRO, 23 g CHO, and 13 g fat; 6.2 g fiber | Numerical data not presented | |||
| High fiber–low protein: 300 kcal; 3 g PRO, 32 g CHO, and 16 g fat; 27.3 g fiber | ||||
| High fiber–high protein: 300 kcal; 18 g PRO, 21 g CHO, and 14 g fat; 25.8 g fiber | ||||
| All breakfast meals provided | ||||
| Fallaize et al. (45) | Crossover design | 1 d/treatment | Normal-protein cereal: 330 kcal; 9 g PRO, 53 g CHO, and 10 g fat | Normal-protein groups vs. high protein: greater intake in normal-protein vs. high protein; P < 0.007 |
| Normal-protein croissant: 330 kcal; 5 g PRO, 8 g CHO, and 18 g fat | Numerical data not presented | |||
| High protein: 330 kcal; 18 g PRO, 18 g CHO, and 21 g fat | ||||
| All meals provided | ||||
| Vander Wal et al. 2005 (46) | Crossover design | 1.5 d/treatment | Normal protein: 344 ± 11 kcal; 14 g PRO, 48 g CHO, and 11 g fat | Normal protein vs. high protein: 2048 ± 487 vs. 1784 ± 427; P < 0.05 |
| High protein: 353 ± 2 kcal; 18 g PRO, 33 g CHO, 17 g fat | ||||
| All breakfast meals provided | ||||
| Ratliff et al. (47) | Crossover design | 1 d/treatment | Normal protein: 396 kcal; 16 g PRO, 71 g CHO, and 5 g fat | Normal protein vs. high protein: 2229 ± 528 vs. 1826 ± 603; P < 0.05 |
| High protein: 396 kcal; 22 g PRO, 22 g CHO, and 24 g fat | ||||
| All breakfast meals provided | ||||
| Breakfast composition—fiber | ||||
| Mattes (37) | Crossover design | 5 d/treatment | Low fiber: 207 kcal; 5 g PRO, 39 g CHO, and 4 g fat; 0.62 g wheat fiber | Low fiber vs. high fiber: P > 0.05 (NS) |
| High-fiber alginate/guar gum: 196 kcal; 6 g PRO, 38 g CHO, and 4 g fat; 4.49 g guar fiber | Numerical data not presented | |||
| All breakfast meals provided | ||||
| Delargy et al. (48) | Crossover design | 1 d/treatment | No fiber: 92 kcal; 2 g PRO, 21 g CHO, and 1 g fat; 0g fiber | No fiber: 3355 ± 698 |
| Low fiber: 537 kcal; 16 g PRO, 95 g CHO, and 11 g fat; 1 g insoluble fiber and 2.2 g soluble fiber | Low fiber: 3389 ± 542 | |||
| High fiber—insoluble: 537 kcal; 23 g PRO, 84 g CHO, and 13 g fat; 18 g insoluble fiber and 3.8 g soluble fiber | High fiber—insoluble: 3548 ± 557 | |||
| High fiber—soluble: 537 kcal; 16 g PRO, 96 g CHO, and 11 g fat; 4.2 g insoluble fiber and 17.5 g soluble fiber | High fiber—soluble: 3535 ± 570 | |||
| All meals provided | No main effect of fiber was detected (P > 0.05, NS) | |||
| Juvonen et al. (49) | Crossover design | 1 d/treatment | Low fiber: 299 kcal; 4 g PRO, 57 g CHO, and 4 g fat; 1.5 g insoluble fiber | Low-fiber versions vs. high-fiber versions: all comparisons, P > 0.05 (NS) |
| High fiber—wheat bran: 299 kcal; 6 g PRO, 54 g CHO, and 4 g fat; 10.3 g insoluble fiber | Numerical data not presented | |||
| High fiber—oat bran: 299 kcal; 8 g PRO, 53 g CHO, and 4 g fat; 5.5 g insoluble fiber and 5.1 g soluble fiber | ||||
| High fiber—wheat and oat breakfast: 299 kcal; 7 g PRO, 57 g CHO, and 4 g fat; 7.6 g insoluble fiber and 2.5 g soluble fiber | ||||
| All breakfast meals provided | ||||
| Klosterbuer et al. (50) | Crossover design | 1 d/treatment | Low fiber: 591 kcal; 10 g PRO, 105 g CHO, and 13 g fat; 2.8 g wheat fiber | Low-fiber versions vs. high-fiber versions: all comparisons, P > 0.05 (NS) |
| High fiber—corn: 617 kcal; 10 g PRO, 104 g CHO, and 13 g fat; 27.8 g corn fiber | Numerical data not presented | |||
| High fiber—corn and pullalan: 641 kcal; 10 g PRO, 104 g CHO, and 13 g fat; 27.8 g corn and pullalan fiber | ||||
| High fiber—resistant starch: 589 kcal; 10 g PRO, 106 g CHO, and 13 g fat; 27.2 g resistant starch fiber | ||||
| High fiber—resistant starch and pullalan: 568 kcal; 10 g PRO, 106 g CHO, and 13 g fat; 27.2 g resistant starch and pullalan fiber | ||||
| All breakfast meals provided | ||||
| Willis et al. (51) | Crossover design | 1 d/treatment | Low fiber: 502 kcal; 11 g PRO, 74 g CHO, and 20g fat; <1 g fiber | All comparisons, P > 0.05 (NS) |
| 4 g fiber: 488 kcal; 12 g PRO, 81 g CHO, and 13 g fat; 5.7 g fiber | Numerical data not presented | |||
| 8 g fiber: 493 kcal; 12 g PRO, 89 g CHO, and 10 g fat; 8.9 g fiber | ||||
| 12 g fiber: 544 kcal; 13 g PRO, 93 g CHO, and 13 g fat; 12.8 g fiber | ||||
| All breakfast meals provided | ||||
| Archer et al. (52) | Crossover design | 1 d/treatment | No fiber: 427 kcal; 27 g PRO, 34 g CHO, and 21 g FAT; 0 g fiber | No fiber vs. high fiber—inulin: greater intake in no fiber vs. high fiber—inulin; P < 0.05 |
| High fiber—inulin: 362 kcal; 27 g PRO, 34 g CHO, and 13 g fat; 24 g fiber | Numerical data not presented | |||
| High fiber—lupin: 360 kcal; 28 g PRO, 34 g CHO, 13 g fat; 24 g fiber | No fiber vs. high fiber—lupin: greater intake in no fiber vs. high fiber—lupin; P < 0.05 | |||
| All breakfast meals provided | Numerical data not presented | |||
| Yannakoula et al. (53) | Crossover design | 1 d/treatment | Low fiber: 456 kcal; 17 g PRO, 74 g CHO, and 11 g fat; 0.7 g fiber | Low fiber vs. high fiber: 3359 ± 669 vs. 2989 ± 602; P < 0.005 |
| High fiber: 465 kcal; 18 g PRO, 73 g CHO, and 11 g fat; 14.9 g fiber | ||||
| All breakfast meals provided | ||||
| Barone Lumaga et al. (54) | Crossover design | 1 d/treatment | No fiber: 149 kcal/250 mL; 0 g PRO, 37 g CHO, and 0 g fat; 0 g fiber | No fiber vs. high-fiber groups: greater intake vs. high-fiber groups; P < 0.05 |
| High fiber—β-glucan: 148 kcal/250 mL; 0 g PRO, 34 g CHO, and 0 g fat; 3 g β-glucan fiber | Numerical data not presented | |||
| High fiber—pectin: 149 kcal/250 mL; 1 g PRO, 34 g CHO, and 0 g fat; 2.5 g pectin fiber | ||||
| All treatments were part of an isocaloric breakfast: ∼536.3 kcal; all breakfasts were provided | ||||
| Karhunen et al. (44) | Crossover design | 1 d/treatment | Low fiber–low protein: 300 kcal; 3 g PRO, 33 g CHO, and 14 g fat; 7.6 g fiber | Low-fiber groups vs. high-fiber groups: all comparisons, P > 0.05 (NS) |
| Low fiber–high protein: 300 kcal; 20 g PRO, 23 g CHO, and 13 g fat; 6.2 g fiber | Numerical data not presented | |||
| High fiber–low protein: 300 kcal; 3 g PRO, 32 g CHO, and 16 g fat; 27.3 g fiber | ||||
| High fiber–high protein: 300 kcal; 18 g PRO, 21 g CHO, and 14 g fat; 25.8 g fiber | ||||
| All breakfast meals provided | ||||
| Breakfast composition—size3 | ||||
| Rabinovitz, et al. (29) | Parallel design | 12 wk | High calorie: 430 kcal; 23 g PRO, 42 g CHO, and 19 g fat | Low calorie vs. high calorie: P > 0.05 (NS) |
| Low calorie: 210 kcal; 8 g PRO, 29 g CHO, and 7 g fat | Numerical data not presented | |||
| No recommendations outside of energy and macronutrient content were provided | ||||
The breakfast characteristics within and between studies may have contributed to the conflicting findings. For example, Leidy et al. (34) reported an additional 290 kcal/d after a normal-protein breakfast compared with skipping breakfast (P < 0.003), whereas the high-protein breakfast did not increase daily intake. These findings are also supported by those studies that included only normal-protein breakfasts and reported increased daily intake compared with skipping breakfast (35, 38, 39). However, it is important to note that, although increased protein at breakfast may not increase daily intake, none of the studies reported a decrease in daily intake with the high-protein breakfasts compared with skipping breakfast (34, 40–42). Based on these data, it is unclear whether a single high-protein meal elicits changes in daily intake. However, in our recent pilot study, the group consuming a high-protein breakfast had an ∼400 kcal reduction in daily intake throughout the 12-wk period, whereas the breakfast-skipping group did not experience this reduction (33). In fact, those who continued skipping breakfast increased their daily intake by ∼370 kcal.
Beyond the breakfast characteristics, habitual breakfast behaviors might also influence the study findings. Adding breakfast to the diet of those who habitually skip the morning meal is quite a different experience from removing breakfast from the diet of someone who habitually eats breakfast. For example, the study by Farshchi et al. (36) only included habitual breakfast consumers and was the only study to report higher daily intake (by ∼90 kcal, P < 0.001) when breakfast was removed (i.e., skipped) than when breakfast continued to be consumed. However, in the studies that only included habitual breakfast skippers, the addition of breakfast generally did not increase daily intake despite the additional calories consumed from the breakfast meal (34, 40). These data suggest that although incorporating additional calories at the breakfast meal does not increase daily intake, omitting breakfast from one’s diet may lead to overeating later in the day.
The last factor that may influence intake data involves the specific modality of assessing intake. Three of the studies (34, 39, 41) used a full-feeding design in which all foods and beverages were provided and weighed, whereas the remaining studies included dietary food records and/or recalls. Although dietary records and recalls typically lead to under-reporting of daily intake, eating behavior is compromised within a full-feeding laboratory setting and can lead to purposeful reductions in daily food intake (55). Because of the limitations with collecting viable intake data, it is challenging to accurately identify a breakfast effect.
Breakfast composition and size.
The search yielded 9 studies that compared high-protein with normal-protein breakfasts, 8 studies that compared high-fiber with normal/no-fiber breakfasts, and 2 studies that compared small with large breakfasts (Table 2).
The protein studies included a fairly large range of protein intake within the breakfast meals. Specifically, the normal-protein meals contained between 3 and 64 g protein/meal, whereas the high-protein meals included 18–186 g protein. Although the normal- and high-protein meals were isocaloric within each study, protein sources and types of breakfasts in these meals varied within and/or between studies. Specifically, a variety of protein sources were included within the high-protein breakfasts, including eggs, dairy, beef, and soy. On average, consumption of the high-protein breakfasts led to a daily intake of 2440 ± 335 kcal, whereas consumption of the normal-protein breakfasts led to a daily intake of 2530 ± 335 kcal, a difference of ∼90 kcal. When the study findings were summarized, 62% of the comparisons elicited similar daily intake (40–44), 38% reported a reduction in daily intake (34, 45–47), and 0% reported an increase in daily intake with the consumption of a high-protein compared with normal-protein breakfast (Table 2).
The fiber studies included a fairly large range of fiber intake within the breakfast meals. Specifically, the normal-fiber meals contained between 0 and 3 g fiber/meal, whereas the high-fiber meals included 2.5–28 g fiber. Energy content, source of fiber, and types of breakfast varied within and/or between studies. On average, the consumption of the high-fiber breakfasts led to a daily intake of 2350 ± 210 kcal, whereas consumption of the normal-fiber breakfasts led to a daily intake of 2460 ± 210 kcal (i.e., a difference of ∼110 kcal). When the study findings were summarized, 80% of the comparisons elicited similar daily intake (37, 44, 48–51), 20% reported a reduction in daily intake (52–54), and 0% reported an increase in daily intake with the consumption of a high-fiber compared with a normal-fiber breakfast (Table 2).
With respect to the effects of breakfast size, both studies led to similar intake when comparing the large with the smaller breakfast meals, averaging 1850 ± 450 kcal/d (Table 2) (29, 42).
In summary, the current evidence is conflicting as to whether breakfast consumption influences daily intake. Although the discrepant data might be due to the limitations of assessing daily intake, it is important to note that daily intake was generally lower after the consumption of breakfast meals high in dietary protein or fiber. Further research including more tightly controlled breakfast components throughout randomized, controlled, longer-term studies are required to strengthen these findings.
Summary and Conclusions
The strength of the evidence supporting the consumption of breakfast for weight management and daily food intake is shown in Supplemental Table 1. Based on the Academy of Nutrition and Dietetics Evidence Analysis criteria (22), there is limited evidence supporting the addition of breakfast for body weight management and daily food intake. Regarding the type of breakfast, accumulating evidence exists supporting the consumption of increased protein and fiber at breakfast, as well as consuming more energy during the morning hours. However, the majority of the studies that manipulated breakfast composition and content did not control for habitual breakfast behaviors; nor did those studies include a breakfast-skipping control. Thus, it is unclear whether the addition of these types of breakfast meals affects weight management.
Future research, including large RCTs of longer-term duration (≥6 mo) with a focus on key dietary factors, is critical to begin to assess whether breakfast recommendations are appropriate for the prevention and/or treatment of obesity across the lifespan.
Acknowledgments
Responsibility for the design, analyses, and interpretation of the information presented in this review was that of the authors. All authors read and approved the final manuscript.
References
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, Robinson TN, Scott BJ, St Jeor S, Williams CL. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 2005;111:1999–2012. [DOI] [PubMed] [Google Scholar]
- 4.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics 1999;103:1175–82. [DOI] [PubMed] [Google Scholar]
- 5.Brown AW, Bohan Brown MM, Allison DB. Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am J Clin Nutr 2013;98:1298–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casazza K, Brown A, Astrup A, Bertz F, Baum C, Bohan Brown M, Dawson J, Durant N, Dutton G, Fields DA, et al. Weighing the evidence of common beliefs in obesity research. Crit Rev Food Sci Nutr 2015;55:2014–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deshmukh-Taskar PR, Nicklas TA, O’Neil CE, Keast DR, Radcliffe JD, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999–2006. J Am Diet Assoc 2010;110:869–78. [DOI] [PubMed] [Google Scholar]
- 8.Siega-Riz AM, Popkin BM, Carson T. Trends in breakfast consumption for children in the United States from 1965–1991. Am J Clin Nutr 1998;67:748S–56S. [DOI] [PubMed] [Google Scholar]
- 9.Song WO, Chun OK, Kerver J, Cho S, Chung CE, Chung SJ. Ready-to-eat breakfast cereal consumption enhances milk and calcium intake in the US population. J Am Diet Assoc 2006;106:1783–9. [DOI] [PubMed] [Google Scholar]
- 10.Moag-Stahlberg A. 2010 ADAF Family nutrition and physical activity survey background data [Internet]. 2010 [cited 2011 Jan 1]. Available from: www.Eatright.org.
- 11.Warmoth B. Breakfast habits by the numbers (Hint: It isn't good for breakfast) [Internet]. 2013 [cited 2013 Sep 26]. Available from: http://www.fooddive.com/news/breakfast-habits-by-the-numbers-hint-it-isnt-good-for-breakfast/175630/.
- 12.Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005;105:743–60, quiz 761–2. [DOI] [PubMed] [Google Scholar]
- 13.Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008;121:e638–45. [DOI] [PubMed] [Google Scholar]
- 14.Fiore H, Travis S, Whalen A, Auinger P, Ryan S. Potentially protective factors associated with healthful body mass index in adolescents with obese and nonobese parents: a secondary data analysis of the third national health and nutrition examination survey, 1988–1994. J Am Diet Assoc 2006;106:55–64, quiz 76–9. [DOI] [PubMed] [Google Scholar]
- 15.Barton BA, Eldridge AL, Thompson D, Affenito SG, Striegel-Moore RH, Franko DL, Albertson AM, Crockett SJ. The relationship of breakfast and cereal consumption to nutrient intake and body mass index: the National Heart, Lung, and Blood Institute Growth and Health Study. J Am Diet Assoc 2005;105:1383–9. [DOI] [PubMed] [Google Scholar]
- 16.Niemeier HM, Raynor HA, Lloyd-Richardson EE, Rogers ML, Wing RR. Fast food consumption and breakfast skipping: predictors of weight gain from adolescence to adulthood in a nationally representative sample. J Adolesc Health 2006;39:842–9. [DOI] [PubMed] [Google Scholar]
- 17.Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord 2003;27:1258–66. [DOI] [PubMed] [Google Scholar]
- 18.Leidy HJ, Clifton PM, Astrup A, Wycherley TP, Westerterp-Plantenga MS, Luscombe-Marsh ND, Woods SC, Mattes RD. The role of protein in weight loss and maintenance. Am J Clin Nutr 2015. Apr 29 (Epub ahead of print; DOI: ajcn084038. [DOI] [PubMed] [Google Scholar]
- 19.Pol K, Christensen R, Bartels EM, Raben A, Tetens I, Kristensen M. Whole grain and body weight changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr 2013;98:872–84. [DOI] [PubMed] [Google Scholar]
- 20.Garaulet M, Gomez-Abellan P. Timing of food intake and obesity: a novel association. Physiol Behav 2014;134:44–50. [DOI] [PubMed] [Google Scholar]
- 21.Timlin MT, Pereira MA. Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr Rev 2007;65:268–81. [DOI] [PubMed] [Google Scholar]
- 22.Dietetics ANa. Evidence analysis manual: steps in the academy evidence analysis process, ed. 2012.
- 23.Schlundt DG, Hill JO, Sbrocco T, Pope-Cordle J, Sharp T. The role of breakfast in the treatment of obesity: a randomized clinical trial. Am J Clin Nutr 1992;55:645–51. [DOI] [PubMed] [Google Scholar]
- 24.Rosado JL, del R.Arellano M, Montemayor K, García P, Caamaño Mdel C. An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: a randomized controlled trial. Nutr J 2008;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dhurandhar EJ, Dawson J, Alcorn A, Larsen LH, Thomas EA, Cardel M, Bourland AC, Astrup A, St-Onge MP, Hill JO, et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014;100:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S, Yang L, Lu J, Mu Y. High-Protein Breakfast Promotes Weight Loss by Suppressing Subsequent Food Intake and Regulating Appetite Hormones in Obese Chinese Adolescents. Horm Res Paediatr 2015;83:19–25. [DOI] [PubMed] [Google Scholar]
- 27.Rueda JM, Khosla P. Impact of breakfasts (with or without eggs) on body weight regulation and blood lipids in university students over a 14-week semester. Nutrients 2013;5:5097–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jakubowicz D, Froy O, Wainstein J, Boaz M. Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids 2012;77:323–31. [DOI] [PubMed] [Google Scholar]
- 29.Rabinovitz HR, Boaz M, Ganz T, Jakubowicz D, Matas Z, Madar Z, Wainstein J. Big breakfast rich in protein and fat improves glycemic control in type 2 diabetics. Obesity (Silver Spring) 2014;22:E46–54. [DOI] [PubMed] [Google Scholar]
- 30.Hu X, Gao J, Zhang Q, Fu Y, Li K, Zhu S, Li D. Soy fiber improves weight loss and lipid profile in overweight and obese adults: a randomized controlled trial. Mol Nutr Food Res 2013;57:2147–54. [DOI] [PubMed] [Google Scholar]
- 31.Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity (Silver Spring) 2013;21:2504–12. [DOI] [PubMed] [Google Scholar]
- 32.Lombardo M, Bellia A, Padua E, Annino G, Guglielmi V, D’Adamo M, Iellamo F, Sbraccia P. Morning meal more efficient for fat loss in a 3-month lifestyle intervention. J Am Coll Nutr 2014;33:198–205. [DOI] [PubMed] [Google Scholar]
- 33.Leidy HJ, Hoertel HA, Douglas SM, Higgins KA, Shafer RS. A high-protein breakfast prevents body fat gain, through reductions in daily intake and hunger, in “breakfast skipping” adolescents. Obesity (Silver Spring) 2015;23:1761–4. [DOI] [PubMed] [Google Scholar]
- 34.Leidy HJ, Ortinau LC, Douglas SM, Hoertel HA. Beneficial effects of a higher-protein breakfast on the appetitive, hormonal, and neural signals controlling energy intake regulation in overweight/obese, “breakfast-skipping,” late-adolescent girls. Am J Clin Nutr 2013;97:677–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr 2014;100:539–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 2005;81:388–96. [DOI] [PubMed] [Google Scholar]
- 37.Mattes RD. Effects of a combination fiber system on appetite and energy intake in overweight humans. Physiol Behav 2007;90:705–11. [DOI] [PubMed] [Google Scholar]
- 38.Kral TV, Whiteford LM, Heo M, Faith MS. Effects of eating breakfast compared with skipping breakfast on ratings of appetite and intake at subsequent meals in 8- to 10-y-old children. Am J Clin Nutr 2011;93:284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levitsky DA, Pacanowski CR. Effect of skipping breakfast on subsequent energy intake. Physiol Behav 2013;119:9–16. [DOI] [PubMed] [Google Scholar]
- 40.Leidy HJ, Racki EM. The addition of a protein-rich breakfast and its effects on acute appetite control and food intake in ‘breakfast-skipping’ adolescents. Int J Obes (Lond) 2010;34:1125–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Irvine P, Mouzet JB, Marteau C, Salle A, Genaitay M, Favreau AM, Berrut G, Ritz P. Short-term effect of a protein load on appetite and food intake in diseased mildly undernourished elderly people. Clin Nutr 2004;23:1146–52. [DOI] [PubMed] [Google Scholar]
- 42.de Graaf C, Hulshof T, Weststrate JA, Jas P. Short-term effects of different amounts of protein, fats, and carbohydrates on satiety. Am J Clin Nutr 1992;55:33–8. [DOI] [PubMed] [Google Scholar]
- 43.Stubbs RJ, van Wyk MC, Johnstone AM, Harbron CG. Breakfasts high in protein, fat or carbohydrate: effect on within-day appetite and energy balance. Eur J Clin Nutr 1996;50:409–17. [PubMed] [Google Scholar]
- 44.Karhunen LJ, Juvonen KR, Flander SM, Liukkonen KH, Lahteenmaki L, Siloaho M, Laaksonen DE, Herzig KH, Uusitupa MI, Poutanen KS. A psyllium fiber-enriched meal strongly attenuates postprandial gastrointestinal peptide release in healthy young adults. J Nutr 2010;140:737–44. [DOI] [PubMed] [Google Scholar]
- 45.Fallaize R, Wilson L, Gray J, Morgan LM, Griffin BA. Variation in the effects of three different breakfast meals on subjective satiety and subsequent intake of energy at lunch and evening meal. Eur J Nutr 2013;52:1353–9. [DOI] [PubMed] [Google Scholar]
- 46.Vander Wal JS, Marth JM, Khosla P, Jen KL, Dhurandhar NV. Short-term effect of eggs on satiety in overweight and obese subjects. J Am Coll Nutr 2005;24:510–5. [DOI] [PubMed] [Google Scholar]
- 47.Ratliff J, Leite JO, de Ogburn R, Puglisi MJ, VanHeest J, Fernandez ML. Consuming eggs for breakfast influences plasma glucose and ghrelin, while reducing energy intake during the next 24 hours in adult men. Nutr Res 2010;30:96–103. [DOI] [PubMed] [Google Scholar]
- 48.Delargy HJ, O’Sullivan KR, Fletcher RJ, Blundell JE. Effects of amount and type of dietary fibre (soluble and insoluble) on short-term control of appetite. Int J Food Sci Nutr 1997;48:67–77. [DOI] [PubMed] [Google Scholar]
- 49.Juvonen KR, Salmenkallio-Marttila M, Lyly M, Liukkonen KH, Lahteenmaki L, Laaksonen DE, Uusitupa MI, Herzig KH, Poutanen KS, Karhunen LJ. Semisolid meal enriched in oat bran decreases plasma glucose and insulin levels, but does not change gastrointestinal peptide responses or short-term appetite in healthy subjects. Nutr Metab Cardiovasc Dis 2011;21:748–56. [DOI] [PubMed] [Google Scholar]
- 50.Klosterbuer AS, Thomas W, Slavin JL. Resistant starch and pullulan reduce postprandial glucose, insulin, and GLP-1, but have no effect on satiety in healthy humans. J Agric Food Chem 2012;60:11928–34. [DOI] [PubMed] [Google Scholar]
- 51.Willis HJ, Thomas W, Eldridge AL, Harkness L, Green H, Slavin JL. Increasing doses of fiber do not influence short-term satiety or food intake and are inconsistently linked to gut hormone levels. Food Nutr Res 2010;54:5135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Archer BJ, Johnson SK, Devereux HM, Baxter AL. Effect of fat replacement by inulin or lupin-kernel fibre on sausage patty acceptability, post-meal perceptions of satiety and food intake in men. Br J Nutr 2004;91:591–9. [DOI] [PubMed] [Google Scholar]
- 53.Yannakoulia M, Aggelopoulou D, Skenderi K, Koinaki S, Yiannakouris N. A Mediterranean-like breakfast affects energy intake and appetite-related feelings. Int J Food Sci Nutr 2014;65:899–902. [DOI] [PubMed] [Google Scholar]
- 54.Barone Lumaga R, Azzali D, Fogliano V, Scalfi L, Vitaglione P. Sugar and dietary fibre composition influence, by different hormonal response, the satiating capacity of a fruit-based and a beta-glucan-enriched beverage. Food Funct 2012;3:67–75. [DOI] [PubMed] [Google Scholar]
- 55.Sawaya AL, Tucker K, Tsay R, Willett W, Saltzman E, Dallal GE, Roberts SB. Evaluation of four methods for determining energy intake in young and older women: comparison with doubly labeled water measurements of total energy expenditure. Am J Clin Nutr 1996;63:491–9. [DOI] [PubMed] [Google Scholar]