Abstract
Background. In obesity there is a subclinical chronic low-grade inflammatory response where insulin resistance (IR) may develop. Chemerin is secreted in white adipose tissue and promotes low-grade inflammatory process, where it expressed CMKLR1 receptor. The role of chemerin and CMKLR1 in inflammatory process secondary to obesity is not defined yet. Methods. Cross-sectional study with 134 individuals classified as with and without obesity by body mass index (BMI) and IR. Body fat storage measurements and metabolic and inflammatory markers were measured by routine methods. Soluble chemerin and basal levels of insulin by ELISA and relative expression of CMKLR1 were evaluated with qPCR and 2−ΔΔCT method. Results. Differences (P < 0.05) were observed between obesity and lean individuals in body fat storage measurements and metabolic-inflammatory markers. Both CMKLR1 expression and chemerin levels were increased in obesity without IR. Soluble chemerin levels correlate with adiposity and metabolic markers (r = 8.8% to 38.5%), P < 0.05. Conclusion. The increment of CMKLR1 expression was associated with insulin production. Increased serum levels of chemerin in obesity were observed, favoring a dysmetabolic response. The results observed in this study suggest that both chemerin and CMKLR1 have opposite expression in the context of low-grade inflammatory response manifested in the development of IR.
1. Introduction
Obesity which is the excess storage of white adipose tissue (WAT) and low-grade inflammation are the key factors for development of insulin resistance (IR) [1–4].
In WAT primed immune cells are recruited as adiposity increases, and these cells became resident cells (mainly macrophages) and secrete proinflammatory adipokines that promote further recruitment of circulating monocytes [4–7]. Later, they polarize towards M1 macrophages, favoring an inflammatory subclinical chronic state [6, 8–10].
Chemerin is an adipokine secreted by adipocytes; it is closely associated with amount of fat and distribution. As a chemoattractant protein, chemerin acts as a ligand for the coupled G-receptor protein (ChemR23) and participates in both adaptive and innate immunity [11]. In humans, chemerin gene (RRARES2) is highly expressed in WAT and to a lesser extent in liver and lungs. On immune cells, chemerin is known to stimulate chemotaxis of dendritic cells, macrophages, and NK cells. Meanwhile, its receptor, ChemR23 gene (CMKLR1), is expressed in dendritic cells, monocyte/macrophages, and endothelial cells [11–14]. ChemR23 is involved in the differentiation of adipocytes and increased intracellular glucose or lipids promote its expression [14].
The interaction of chemerin/ChemR23 has been shown to reduce cytokines, chemokines, and phagocytosis, proving to be important in the inflammatory process associated with obesity [12, 14, 15].
In this context, chemerin/ChemR23 axis has been shown to impact IR development, which influences the clinical course and severity of obesity-related diseases [10]. However, the association with immunometabolic markers and chemerin and its receptor ChemR23 is scarce. Therefore, the aim of this study was to characterize the inflammatory and metabolic phenotype of subjects with obesity-IR state based on the chemerin soluble levels and its receptor CMKLR1 expression.
2. Material and Methods
2.1. Study Design
In this cross-sectional study a total of 134 adults, aged 20 to 59 years, were recruited from general population in the west of Mexico. We included individuals who at the time of enrollment did not present glucose intolerance, infectious diseases, hypertension, pregnancy, anemia, cardiovascular disease, malignancy, and renal and metabolic diseases such as type 2 diabetes mellitus (T2DM). Subjects with current medication use were excluded.
Subjects were classified in two forms, based on obesity and then by IR. First, they were classified according to the recommendations' of World Health Organization, by body mass index (BMI), waist circumference (WC), waist-hip ratio (WHR), and waist to height ratio (WHtR), in two groups: subjects with obesity, if any of the following conditions were present: BMI ≥ 30.0 kg/m2, WC ≥ 90.0 cm, WHR ≥ 0.90, and WHtR ≥ 52.5 in Men and WC ≥ 80.0 cm, WHR ≥ 0.80, and WHtR ≥ 53.0 in women, and lean subjects that are lower in these measurements. For detection of IR in subjects with obesity they were secondly classified according to Gayoso criteria in two groups: with and without IR [16].
For ethical purposes, participants were informed about the study and signed a consent form following the Helsinki declaration guidelines [17] and the institutional (Guadalajara University) review boards' committees.
2.2. Subjects' Medical History and Physical Examination
All individuals who satisfied inclusion criteria were clinically evaluated by a physician who performed a complete medical history. Assessment of general health status and vital signs were included: blood pressure (measured 3 times with the subject in the sitting position for 15 minutes before the evaluation), heart and respiratory rate, and body temperature.
2.3. Subjects' Body Fat Storage Measurements
We evaluated height, which was measured to the nearest 1 mm by using a stadiometer (Seca GmbH & Co. KG. Hamburg, Germany); body weight and total and trunk body fat mass (absolute, kg, and relative, %) were determined by bioelectrical impedance analysis (TANITA BC-418 Segmental Body Composition Analyzer, Tokyo, JPN) to the nearest 0.1 kg. WC, hip circumference (HC), and coronal abdominal diameter were measured by using an anthropometric fiberglass tape (GULICK® length 0–180 cm precision ±0.1; USA). At the level of the iliac crest (L4-5) sagittal abdominal diameter was measured using a sliding-beam, abdominal caliper (precision ±0.1 cm, Holtain Ltd. Crosswell, Crymych, Pembs., SA41 3UF, UK) with the patient lying in a supine position on the examination table [18]. Five measures of skinfold thickness (i.e., abdominal, bicipital, tricipital, subscapular, and suprailiac) were obtained on the right side of the body by using a Harpenden skinfold caliper (opened 80 mm with precision of ±0.2 mm, constant pressure: 10 g/mm2; Holtain Ltd. Crosswell, Crymych, Pembs., SA41 3UF, UK). All these measurements were carried out by the same Physician, in duplicate following the procedures recommended by anthropometric indicators measurement guide [19, 20].
To determine obesity and adiposity indexes the following calculations were used: BMI, kg/m2 = weight (kg)/height2 (m); WHtR = WC (cm)/height (cm) [21]; WHR = WC (cm)/HC (cm); conicity index (CI) = WC (cm)/; BFR = total body fat mass (kg)/height (cm); total adipose area (TAA, cm2) = WC2/4π; visceral area (VA, cm2) = π(WC/2π − abdominal skinfold)2; subcutaneous abdominal area (cm2) = TAA − VA [18]; visceral adiposity index (VAI): for males, VAI = (WC/36.58 + (1.896BMI))6(TG/0.81)6(1.52/HDLc) and females, VAI = (WC/39.68 + (1.886BMI)) 6(TG/1.03)6(1.31/HDLc) [22]; homeostasis model assessment-insulin resistance (HOMA-IR) = [basal glucose mg/dL × (basal insulin μUI/mL)/405] [23, 24].
2.4. Metabolic, Inflammatory Markers, and Chemerin Levels Measurements
Individuals included in the study were fasting 12 hours before the blood samples were taken, allowing them to clot at room temperature, and then were centrifuged at 1509 RCF (Rotanta 460R, Andreas Hettich GmbH & Co. KG.) for 10 minutes at 20°C. Serum was collected and stored at −86°C until further analysis.
We quantified serum concentration of glucose and nonesterified fatty acids (NEFA) with routine enzymatic methods; triglycerides (TG) and total cholesterol (TC) with routine colorimetric methods, high and low density lipoprotein cholesterol (HDLc and LDLc, resp.), apolipoproteins A1 (Apo-A1) and B (Apo-B), and high sensitivity C reactive protein (CRP) with immunoturbidimetry methods (Randox Laboratories 55 Diamond Road, Crumlin Co. Antrim, Northern Ireland, UK); and erythrocyte sedimentation rate (ESR) with Wintrobe method [25]. And the low density lipoprotein cholesterol (VLDLc) was obtained with the Friedewald formula [26].
Through using commercial enzyme-linked immunoabsorbent assays (ELISA) soluble levels of insulin were determined (sensitivity of 0.399 μUI/mL) (ALPCO 26-G Keewaydin Drive, Salem, NH 03079), and chemerin was determined with a limit of detection of 1.08–7.8 ng/mL (R&D Systems, Minneapolis, USA).
2.5. CMKLR1 Relative Expression Analysis
Mononuclear cells from the subjects studied were isolated by density gradient media with separating solution Lymphoprep™ (AXIS-SHIELD PO Box 6863 Rodelokka, 0504 Oslo, Norway). Total RNA was isolated from purified mononuclear cells, using TRIzol® LS Reagent (Ambion RNA Life Technologies, 5791 Van Allen Way, Carlsbad, CA 92008) based on the single-step RNA isolation modified method reported by Chomczynski [27]. Complementary DNA synthesis (cDNA) was performed with 2 μg of each total RNA sample using a reaction size of 20 μL, with oligo (dT) 18 primer (100 ng/μL), RNase free, DEPC treated water, and SuperScript Reverse Transcriptase III kit (Applied Biosystems, 850 Lincoln Centre Drive, Foster City, CA 94404) and stored at −20°C until used for expression analyses.
Real-Time Quantitative Polymerase Chain Reaction (qPCR) was conducted using the StepOne™ detection system, EXPRESS SYBR® GreenER™, and ROX™ qPCR SuperMix Universal, and sequence detector software v2.3 (Applied Biosystems, 850 Lincoln Centre Drive, Foster City, CA 94404) was used for data analysis. A threshold cycle (CT) value was determined from each amplification plot.
In brief, CMKLR1 mRNA expression was performed in a final reaction volume of 20 μL (10 μM forward and reverse primer, 500 nM ROX, 1X SYBR Green qPCR master mix, and cDNA 1000 ng). The conditions of the reaction were as follows: holding 95°C/10 min, cycling (35 cycles of 95°C/15 s, 60°C/60 s), and melt curves 95°C/15 s, 60°C/60 s, and 95°C/15 s. Expression of target genes was normalized by the endogenous reference gen RPS28; sequence specific primers were forward: 5′-GGTCTGTCACAGTCTGCTCC-3′, and reverse 5′-CATCTCAGTTACGTGTGGCG-3′ and for CMKLR1 target gen forward: 5′-GTGGTGGTCTACAGCATCGT-3′ and reverse: 5′-ATGGCGGCATAGGTGATATGG-3′.
The relative expression fold change of target gene was calculated using the comparative CT method with 2−ΔΔCT equation [28]. To ensure accuracy of data, experiments were done in duplicate, blank, internal controls and melt curve data were collected with applications of StepOne detector software (Cat. 4376357).
2.6. Statistical Analysis
Data were analyzed with statistics software SPSS v21 (IBM Inc., Chicago, IL, USA) and GraphPad Prism v6.01 (2014 Inc. 2236 Beach Avenue Jolla, CA 92037). Results are given as mean ± standard deviation (SD). The data distribution of clinical and laboratory variables was evaluated with Z Kolmogorov-Smirnov test. The clinical and laboratory characteristics of study group were compared with one way ANOVA with Tukey post hoc. Data from serum concentrations of chemerin and insulin, laboratorial assessment, and adiposity variables were subjected to Pearson correlation tests. A two-tailed P value < 0.05 was considered statistically significant.
3. Results
3.1. Status Assessment of Body Fat Showed High Adiposity and IR
In this study, the observed frequency of obesity and IR was 63% and 39%, respectively, while IR was not present in lean individuals (with average BMI of 21.6 kg/m2, 18.0 to 24.7). For individuals classified with obesity, IR prevalence was 62%. The adiposity measurements are shown in Table 1.
Table 1.
Status of body fat storage in individuals in the study group.
| Study group | Lean | Obesity without IR | Obesity with IR |
|---|---|---|---|
| BMI (kg/m2) | [21.6 (18.5–24.7)] | [32.0 (30.1–34.7)] | [32.6 (30.2–34.9)] |
| n = 134 | 49 | 32 | 53 |
|
| |||
| Measurement | |||
| Height (cm) | 166.0 ± 8.4 | 162.8 ± 7.8 | 163.8 ± 9.0 |
| Body weight (kg) | 60.0 ± 9.9 | 90.1 ± 12.8a | 97.3 ± 18.9a |
| Total body fat mass (%) | 20.3 ± 5.9 | 40.3 ± 6.8a | 40.6 ± 6.9a |
| Total body fat mass (kg) | 12.0 ± 3.6 | 36.6 ± 8.8a | 39.8 ± 12.4a |
| Trunk body fat mass (%) | 23.8 ± 10.6 | 38.1 ± 11.4a | 35.4 ± 10.5a |
| Trunk body fat mass (kg) | 5.9 ± 2.4b,c | 18.4 ± 3.9a,c | 19.4 ± 6.1a,b |
| Waist circumference (cm) | 78.3 ± 6.6 | 109.6 ± 11.9a | 113.7 ± 13.2a |
| Hip circumference (cm) | 93.3 ± 4.8 | 115.7 ± 12.4a | 118.8 ± 10.8a |
| Coronal abdominal diameter (cm) | 30.2 ± 6.4b,c | 38.0 ± 8.7a,c | 44.9 ± 12.0a,b |
| Sagittal abdominal diameter (cm) | 16.7 ± 2.1 | 24.6 ± 3.4a | 25.9 ± 4.4a |
| Total adipose area (cm2) | 491.2 ± 82.3 | 967.9 ± 216.6a | 1042.5 ± 249.6a |
| Visceral area (cm2) | 227.4 ± 373.0 | 292.7 ± 516.4 | 599.7 ± 836.1a |
| Subcutaneous abdominal area (cm2) | 314.2 ± 324.0 | 696.8 ± 560.8a | 562.6 ± 908.7 |
BMI: body mass index [ (min–max)]. Data are shown in ± SD. aDifference versus lean. bDifference versus obesity without IR. cDifference versus obesity with IR (P < 0.05, ANOVA, Tukey post hoc). IR: insulin resistance.
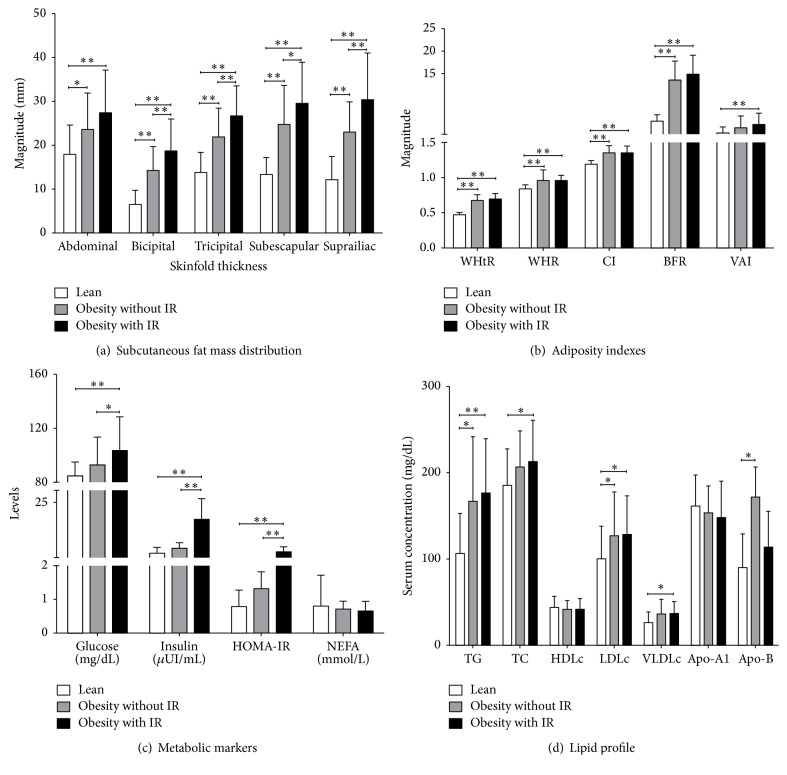
The fat distribution assessed by the skinfold thicknesses showed magnitudes as follows: the group with obesity and IR > obesity without IR group > lean group (Figure 1(a)). Adiposity indexes were increased in both groups with obesity versus lean subjects, except VAI whose increase is observed in individuals with IR versus lean subjects (Figure 1(b)).
Figure 1.
Body fat mass distribution, adiposity indexes, and metabolic markers in the study groups. Lean: [BMI: 21.4 (18.5–24.7) kg/m2] n = 49; obesity without IR: [BMI: 32.0 (30.1–34.7) kg/m2] n = 32; obesity with IR: [BMI: 32.6 (30.2–34.9) kg/m2] n = 53. IR: insulin resistance. WHtR: waist to height ratio; WHR waist-hip ratio; CI: conicity index; VAI: visceral adiposity index; BFR: body fat ratio; HOMA-IR: homeostatic model assessment of insulin resistance; NEFA: none esterified fatty acids; TG: triglycerides; TC: total cholesterol; HDLc, LDLc, and VLDLc (lipoproteins of high, low, and very low density cholesterol, resp.). Data are shown in . ∗∗ P < 0.001, ∗ P < 0.05 (ANOVA, Tukey post hoc).
3.2. Individuals with Obesity and IR Presented a Subclinical Inflammatory State and Dyslipidemia
Lean individuals presented lower levels of glucose, insulin, and HOMA-IR when compared with individuals with and without IR, whereas NEFA presented no changes in different groups (Figure 1(c)); lean individuals showed lower levels of triglycerides and LDLc compared to subjects with and without IR, also lean individuals presented lower levels of total cholesterol and VLDLc when compared to obesity group with IR. Lean subjects also presented lower levels of Apo-B compared with individuals without IR whereas HDLc and Apo-A1 presented no statistical changes (Figure 1(d)). Levels of CRP and ESR were higher in obesity with IR versus lean (6.83 ± 5.65, 17.46 ± 11.67, P < 0.001; resp.).
3.3. Obesity without IR Showed a Contrasting Context on Chemerin Levels
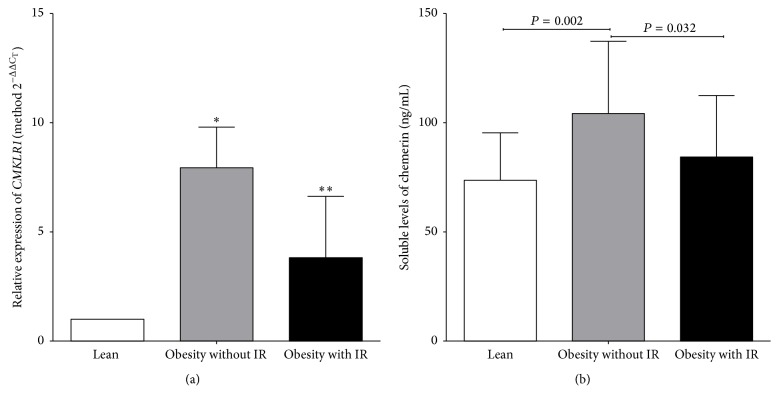
Increased levels of soluble chemerin were observed in obese individuals without IR compared to obese individuals with IR and lean subjects groups (Figure 2(a)).
Figure 2.
Levels of soluble chemerin and relative expression of CMKLR1 in the study groups. (a) Relative expression of CMKLR1. Method 2−ΔΔCT: ∗difference between obesity without IR and lean (7.9-fold; P = 0.003), and ∗∗obesity with IR versus lean (3.8-fold; P < 0.001). (b) Serum levels of chemerin (ANOVA, Tukey post hoc). IR: insulin resistance.
3.4. Chemerin and Insulin Levels Were Associated with Dysmetabolic Phenotype and Body Fat Adiposity Markers
Positive correlations of chemerin and insulin were observed with the increase in the status of body fat and subcutaneous fat accumulation with lipid profile (Table 2).
Table 2.
Correlation of chemerin and insulin serum levels with the dysmetabolic phenotype and body fat adiposity markers status in the study groups.
| Measurements | Chemerin (ng/mL) | Insulin (μUI/mL) |
|---|---|---|
| Correlation (%) | ||
| Body weight (kg) | −2.8 | 34.7∗∗ |
| BMI (kg/m2) | 15.3 | 46.2∗∗ |
| Body fat mass (%) | 38.5∗∗ | 41.5∗∗ |
| Total body fat mass (kg) | 26.1∗∗ | 46.7∗∗ |
| Waist circumference (cm) | 18.8∗ | 36.4∗∗ |
| Hip circumference (cm) | 21.6∗∗ | 41.5∗∗ |
| Waist-hip ratio | 5.8 | 16.9∗∗ |
| Body fat ratio | 31.5∗∗ | 47.1∗∗ |
| Waist to height ratio | 26.6∗∗ | 38.8∗∗ |
| Conicity index | 30.7∗∗ | 18.3∗∗ |
| Coronal abdominal diameter (cm) | 8.4 | 13.0∗ |
| Sagittal abdominal diameter (cm) | 15.7 | 46.4∗∗ |
| Total adipose area (cm2) | 18.8∗ | 36.4∗∗ |
| Visceral area (cm2) | 19.2∗ | 37.0∗∗ |
| Subcutaneous abdominal area (cm2) | 17.6 | 19.4∗∗ |
| Glucose (mg/dL) | −6.3 | 22.5∗∗ |
| Skinfold thickness (mm): | ||
| Abdominal | −10.3 | 17.3∗∗ |
| Bicipital | 32.7∗∗ | 45.8∗∗ |
| Tricipital | 30.4∗∗ | 39.0∗∗ |
| Subscapular | 11.1 | 38.8∗∗ |
| Suprailiac | 16.1∗ | 36.5∗∗ |
| Triglycerides (mg/dL) | 20.4∗ | 26.1∗∗ |
| LDLc (mg/dL) | 13.0 | 12.5∗ |
| VLDLc (mg/dL) | 20.4∗ | 20.9∗∗ |
| HDLc (mg/dL) | 17.4∗ | 10.1 |
| NEFA (mmol/L) | 30.2∗∗ | 9.0 |
| CRP (mg/L) | 14.1 | 31.5∗∗ |
| ESR (mm/h) | 30.2∗∗ | 1.8 |
IR: insulin resistance. HDLc, LDLc, and VLDLc (lipoproteins of high, low, and very low density cholesterol, resp.); NEFA: nonesterified fatty acids; CRP: C reactive protein; ESR: erythrocyte sedimentation rate. ∗∗ P < 0.001, ∗ P < 0.05, Pearson correlation test.
3.5. Higher CMKLR1 Relative Expression Was Associated with Obesity without IR
Increased expression levels of CMKLR1 receptor were observed in individuals with obesity without IR versus lean and obesity with IR individuals (Figure 2(b)).
A detailed test by tertiles was performed (describing the first tertile as lower expression, second tertile as intermediate expression, and third tertile as higher expression); we found increased accumulation of abdominal fat mass and metabolic markers between individuals with high expression versus individuals with low expression of CMKLR1, independent of the presence of IR and/or obesity. Other relevant information provided in this analysis is that there is an inverse correspondence in insulin levels, HOMA-IR, and NEFA regarding the expression of CMKLR1 (Table 3).
Table 3.
Adiposity and metabolic markers in the relative expression levels of CMKLR1.
| Tertile | First | Second | Third |
|---|---|---|---|
| CMKLR1 relative expression | [0.546 (0.034–1.060)] | [4.148 (1.148–8.934)] | [69.787 (9.009–473.260)] |
| % obesity | 48.7 | 44.1 | 51.7 |
| % IR | 59.0 | 52.9 | 48.3 |
|
| |||
| Measurement | |||
| Trunk body fat mass (%) | 26.02 ± 12.0 | 32.32 ± 9.0a | 33.37 ± 6.4a |
| Coronal abdominal diameter | 35.15 ± 12.0 | 42.18 ± 10.5a | 40.97 ± 8.9 |
| VAI | 2.44 ± 2.6 | 3.33 ± 2.3 | 4.54 ± 2.41a |
| Insulin (μUI/mL) | 15.22 ± 11.4 | 13.08 ± 8.4 | 8.74 ± 5.1a |
| HOMA-IR | 3.49 ± 2.5 | 3.05 ± 1.9 | 2.13 ± 1.4a |
| NEFA | 0.725 ± 0.2 | 0.618 ± 0.26 | 0.500 ± 0.25a |
The expression levels of CMKLR1 are in relative units [ (min–max)]. Data are shown in ± SD and were classified by tertiles. aDifference versus first tertile (P < 0.05, ANOVA, Tukey post hoc). IR: insulin resistance. VAI: visceral adiposity index; HOMA-IR: homeostatic model assessment of insulin resistance; NEFA: nonesterified fatty acids.
4. Discussion
Two main findings emerge from this study: first, the CMKLR1 receptor expression was associated with obesity and its features, and second, its ligand chemerin was associated not only with obesity, but also with metabolic dysfunction such as dyslipidemia and IR.
Adipose tissue has been suggested to be an important source of low-grade inflammation based on three biological aspects: quantity (total mass and relative proportion), anatomical distribution, and phenotype of resident cells [10, 29].
Regarding the quantity and site, our study supported that dysfunctional WAT may play an important role in low-grade inflammation, because the individuals with obesity shown increased accumulation of fat manly in the abdominal region along with low-grade inflammation and dysmetabolic phenotype (represented by dyslipidemic state and increased adiposity indexes), although not all individuals with obesity were IR.
Another important point from this study is that it supports the fact that the IR is a component for developing a chronic-degenerative disease. The IR first promotes dyslipidemia (as an intermediate event) leading to metabolic syndrome and subsequently development of T2DM [1, 3, 30].
The dysmetabolic phenotype observed in individuals with obesity in our study can be explained in the context of immune system dysregulation that exists in IR by the development of two alternative mechanisms not exclusive: in one the WAT of individuals with obesity have increased resident M1 macrophages able to produce chemokines and in additional one, it has been found that high concentrations of fatty acids induce expression of TNFα and Toll-like receptor-4 signaling [4, 30]. This pathway converges with insulin signaling in adipocytes affecting positively glucose transport, glycogen synthesis, and cell differentiation while negatively affecting the lipolysis and gluconeogenesis [8, 31, 32].
The polarization of monocytes/macrophages to M1 in WAT is favored by coupling of chemerin through ChemR23 that in turn displayed a proinflammatory profile, where chemotactic ligand-receptor interaction regulates continued migration of monocytes to WAT [13, 14]. Soluble chemerin produced by adipocytes and resident macrophages M1 in WAT binds to ChemR23 with high affinity, and its levels decrease as recruited circulating monocytes differentiate into macrophages [12–14, 33, 34].
This study evaluated the gene expression of CMKLR1 receptor in circulating monocytes. It presented 7.9- or 3.8-fold higher expression in individuals with obesity without IR or obesity with IR, respectively, than lean individuals. Interestingly the increase in expression levels was directly associated with the proportion of abdominal fat mass and body dimensions, whereas an inverse association was observed with the production of insulin, nonesterified free fatty acids, and HOMA-IR.
In this regard, previous study showed that the chemerin/ChemR23 signaling does not affect the inflammatory response in ex vivo human macrophages [35]. The expression levels of CMKLR1 found in our study suggest that the level of expression is higher in early activation of primed circulating monocytes but decreases at later stages, which can be explained based on the reports in other studies in animal models [31, 36], although changes of CMKLR1 expression in human macrophage differentiation/polarization still remain to be established.
The association of CMKLR1 expression levels, observed in our study, can be explained due to IR being closely associated with excess in abdominal accumulation of WAT [30] and based on other reports in which an adipocyte cell line expression of CMKLR1 was analyzed during differentiation process where upregulation was in the early stage whereas a downregulation was observed in late stages [37, 38]. Proinflammatory stimulus such as TNFα or adiponectin has been shown to upregulate gene expression of CMKLR1 in differentiated adipocytes [39]. This shows the complexity of the CMKLR1 expression and functionality that is not dependent on the expression of its ligand but also dependent on the cell type presented on the disease.
Nevertheless, the limitations of this study were that protein levels of the ChemR23 in monocyte were not assessed, limiting complementary studies about the functional receptor. Another limitation that should be taken in consideration is that this same receptor is known to bind with the same affinity to the lipid mediator resolving E1, which has anti-inflammatory properties. The quantification of such ligand was not done.
One of the main findings was the increased serum levels of chemerin in individuals with obesity without IR versus individuals with IR and lean. In parallel correlation with indicators of adiposity and metabolic markers was observed.
In this regard, previous studies report conflicting results on chemerin levels in different diseases with an inflammatory component such as chronic pancreatitis (94.0 ng/mL) [40], T2DM individuals (179.0 ng/mL) [41], lipodystrophy (234.3 ng/mL) [42], and obesity without diabetes (590.08 ng/mL) [43]. Chemerin levels were increased, except for the levels reported in rheumatoid arthritis (35.0 ng/mL) [44] (an inflammatory disease per se), although this can be explained based on treatment; however, other studies have suggested that chemerin may be the functional link between chronic inflammation and obesity-related T2DM and cardiovascular disease [45].
Our results can be explained because monocytes/macrophages are decisive in the pathogenic process of IR, based on the fact that they are an important source of proinflammatory markers (TNFα, IL-6, chemerin, and C reactive protein), along with increased levels of expression of adipokines, chemokines, and proinflammatory cytokines associated with an equivalent increase in hyperplastic and hypertrophic adipocytes [13, 30, 46].
One important observation from this study is that, in the context of obesity, soluble chemerin levels enhanced both the inflammation and dysmetabolic phenotype, showing how an opposite change in the expression of CMKLR1 takes place once IR is established.
In previous reports it is postulated that chemerin production has a dual profile pro/anti-inflammatory [9, 15]. In this context we suggest that, in the initial stage of IR, the increase in chemerin levels promotes dysmetabolic profile arising from the dysfunctional adipose tissue [36]. Although in the setting of obesity during the process of establishment of IR the levels of chemerin can be decreased, the dysmetabolic profile is maintained. Its scenery might be explained due to that action of chemerin where it regulates the insulin metabolism [6].
5. Conclusions
This is the first study that links the increment of CMKLR1 expression with insulin production, showing an association with fat mass and corporal dimensions, while the increased serum levels of chemerin in obesity were observed, favoring a dysmetabolic response.
Taking together, the results observed in this study suggest that both chemerin and CMKLR1 have opposite expression in the context of low-grade inflammatory response, manifested in the development of IR.
Functional studies are necessary to clarify the biological functions of chemerin signaling in the pathogenesis of IR.
Acknowledgments
This work was supported by Grant PRODEP no. 220214 to UDG-CA-701: Academic group “Aging, Immunometabolism and Oxidative Stress.”
Competing Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contributions
Fernanda-Isadora Corona-Meraz and Rosa-Elena Navarro-Hernández equally contributed to this work.
References
- 1.Makki K., Froguel P., Wolowczuk I. Adipose tissue in obesity-related inflammation and insulin resistance: cells, cytokines, and chemokines. ISRN Inflammation. 2013;2013:12. doi: 10.1155/2013/139239.139239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Luca C., Olefsky J. M. Inflammation and insulin resistance. FEBS Letters. 2008;582(1):97–105. doi: 10.1016/j.febslet.2007.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ye J. Mechanisms of insulin resistance in obesity. Frontiers of Medicine. 2013;7(1):14–24. doi: 10.1007/s11684-013-0262-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Z., Nakayama T. Inflammation, a link between obesity and cardiovascular disease. Mediators of Inflammation. 2010;2010:17. doi: 10.1155/2010/535918.535918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ouchi N., Parker J. L., Lugus J. J., Walsh K. Adipokines in inflammation and metabolic disease. Nature Reviews Immunology. 2011;11(2):85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chawla A., Nguyen K. D., Goh Y. P. S. Macrophage-mediated inflammation in metabolic disease. Nature Reviews Immunology. 2011;11(11):738–749. doi: 10.1038/nri3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourlier V., Bouloumie A. Role of macrophage tissue infiltration in obesity and insulin resistance. Diabetes & Metabolism. 2009;35(4):251–260. doi: 10.1016/j.diabet.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 8.McNelis J., Olefsky J. Macrophages, immunity, and metabolic disease. Immunity. 2014;41(1):36–48. doi: 10.1016/j.immuni.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 9.Yao L., Herlea-Pana O., Heuser-Baker J., Chen Y., Barlic-Dicen J. Roles of the chemokine system in development of obesity, insulin resistance, and cardiovascular disease. Journal of Immunology Research. 2014;2014:11. doi: 10.1155/2014/181450.181450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schipper H. S., Prakken B., Kalkhoven E., Boes M. Adipose tissue-resident immune cells: key players in immunometabolism. Trends in Endocrinology and Metabolism. 2012;23(8):407–415. doi: 10.1016/j.tem.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Zabel B. A., Kwitniewski M., Banas M., Zabieglo K., Murzyn K., Cichy J. Chemerin regulation and role in host defense. American Journal of Clinical and Experimental Immunology. 2014;3(1):1–19. [PMC free article] [PubMed] [Google Scholar]
- 12.Ernst M. C., Sinal C. J. Chemerin: at the crossroads of inflammation and obesity. Trends in Endocrinology and Metabolism. 2010;21(11):660–667. doi: 10.1016/j.tem.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Bondue B., Wittamer V., Parmentier M. Chemerin and its receptors in leukocyte trafficking, inflammation and metabolism. Cytokine and Growth Factor Reviews. 2011;22(5-6):331–338. doi: 10.1016/j.cytogfr.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Mariani F., Roncucci L. Chemerin/chemR23 axis in inflammation onset and resolution. Inflammation Research. 2014;64(2):85–95. doi: 10.1007/s00011-014-0792-7. [DOI] [PubMed] [Google Scholar]
- 15.Yoshimura T., Oppenheim J. J. Chemokine-like receptor 1 (CMKLR1) and chemokine (C-C motif) receptor-like 2 (CCRL2); two multifunctional receptors with unusual properties. Experimental Cell Research. 2011;317(5):674–684. doi: 10.1016/j.yexcr.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gayoso-Diz P., Otero-González A., Rodriguez-Alvarez M. X., et al. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocrine Disorders. 2013;13, article 47 doi: 10.1186/1472-6823-13-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Council for International Organizations of Medical Sciences. International Ethical Guidelines for Epidemiological Studies. Geneva, Switzerland: CIOMS; 2009. [Google Scholar]
- 18.Garaulet M., Hernández-Morante J. J., Tébar F. J., Zamora S., Canteras M. Two-dimensional predictive equation to classify visceral obesity in clinical practice. Obesity. 2006;14(7):1181–1191. doi: 10.1038/oby.2006.135. [DOI] [PubMed] [Google Scholar]
- 19.NHANES. Anthropometry Procesures Manual. CDC/National Center for Health Statistics; 2012. (Edited by N.C.f.H. Statistics). [Google Scholar]
- 20.Ness-Abramof R., Apovian C. M. Waist circumference measurement in clinical practice. Nutrition in Clinical Practice. 2008;23(4):397–404. doi: 10.1177/0884533608321700. [DOI] [PubMed] [Google Scholar]
- 21.Zeng Q., He Y., Dong S., et al. Optimal cut-off values of BMI, waist circumference and waist: height ratio for defining obesity in Chinese adults. British Journal of Nutrition. 2014;112(10):1735–1744. doi: 10.1017/s0007114514002657. [DOI] [PubMed] [Google Scholar]
- 22.Amato M. C., Giordano C., Galia M., et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–922. doi: 10.2337/dc09-1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matthews D. R., Hosker J. P., Rudenski A. S., Naylor B. A., Treacher D. F., Turner R. C. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/bf00280883. [DOI] [PubMed] [Google Scholar]
- 24.Wallace T. M., Matthews D. R. The assessment of insulin resistance in man. Diabetic Medicine. 2002;19(7):527–534. doi: 10.1046/j.1464-5491.2002.00745.x. [DOI] [PubMed] [Google Scholar]
- 25.Wintrobe M. M., Landsberg J. W. A standardized technique for the blood sedimentation test 1935. The American Journal of the Medical Sciences. 2013;346(2):148–153. doi: 10.1097/MAJ.0b013e31826caf12. [DOI] [PubMed] [Google Scholar]
- 26.Friedewald W. T., Levy R. I., Fredrickson D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 27.Chomczynski P. A reagent for the single-step simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. BioTechniques. 1993;15(3):532–537. [PubMed] [Google Scholar]
- 28.Pfaffl M. W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Research. 2001;29(9, article e45) doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee M.-J., Wu Y., Fried S. K. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Molecular Aspects of Medicine. 2013;34(1):1–11. doi: 10.1016/j.mam.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fuentes E., Fuentes F., Vilahur G., Badimon L., Palomo I. Mechanisms of chronic state of inflammation as mediators that link obese adipose tissue and metabolic syndrome. Mediators of Inflammation. 2013;2013:11. doi: 10.1155/2013/136584.136584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo S. Insulin signaling, resistance, and metabolic syndrome: insights from mouse models into disease mechanisms. Journal of Endocrinology. 2014;220(2):T1–T23. doi: 10.1530/joe-13-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson A. M. F., Olefsky J. M. The origins and drivers of insulin resistance. Cell. 2013;152(4):673–684. doi: 10.1016/j.cell.2013.01.041. [DOI] [PubMed] [Google Scholar]
- 33.Herová M., Schmid M., Gemperle C., Hersberger M. ChemR23, the receptor for chemerin and resolvin E1, is expressed and functional on M1 but not on M2 Macrophages. The Journal of Immunology. 2015;194(5):2330–2337. doi: 10.4049/jimmunol.1402166. [DOI] [PubMed] [Google Scholar]
- 34.Ernst M. C., Haidl I. D., Zuńĩga L. A., et al. Disruption of the chemokine-like receptor-1 (CMKLR1) gene is associated with reduced adiposity and glucose intolerance. Endocrinology. 2012;153(2):672–682. doi: 10.1210/en.2011-1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bondue B., de Henau O., Luangsay S., et al. The chemerin/ChemR23 system does not affect the pro-inflammatory response of mouse and human macrophages ex vivo. PLoS ONE. 2012;7(6) doi: 10.1371/journal.pone.0040043.e40043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takahashi M., Okimura Y., Iguchi G., et al. Chemerin regulates β-cell function in mice. Scientific Reports. 2011;1, article 123 doi: 10.1038/srep00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suzuki Y., Hong Y. H., Song S. H., et al. The regulation of chemerin and CMKLR1 genes expression by TNF-α, adiponectin, and chemerin analog in bovine differentiated adipocytes. Asian-Australasian Journal of Animal Sciences. 2012;25(9):1316–1321. doi: 10.5713/ajas.2012.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Takahashi M., Takahashi Y., Takahashi K., et al. Chemerin enhances insulin signaling and potentiates insulin-stimulated glucose uptake in 3T3-L1 adipocytes. FEBS Letters. 2008;582(5):573–578. doi: 10.1016/j.febslet.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 39.Goralski K. B., McCarthy T. C., Hanniman E. A., et al. Chemerin, a novel adipokine that regulates adipogenesis and adipocyte metabolism. The Journal of Biological Chemistry. 2007;282(38):28175–28188. doi: 10.1074/jbc.m700793200. [DOI] [PubMed] [Google Scholar]
- 40.Adrych K., Stojek M., Smoczynski M., Sledzinski T., Sylwia S.-W., Swierczynski J. Increased serum chemerin concentration in patients with chronic pancreatitis. Digestive and Liver Disease. 2012;44(5):393–397. doi: 10.1016/j.dld.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 41.Neuparth M. J., Proença J. B., Santos-Silva A., Coimbra S. The positive effect of moderate walking exercise on chemerin levels in portuguese patients with type 2 diabetes mellitus. Journal of Investigative Medicine. 2014;62(2):350–353. doi: 10.231/JIM.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 42.Miehle K., Ebert T., Kralisch S., et al. Circulating serum chemerin levels are elevated in lipodystrophy. Clinical Endocrinology. 2015 doi: 10.1111/cen.12976. [DOI] [PubMed] [Google Scholar]
- 43.Lórincz H., Katkõ M., Harangi M., et al. Strong correlations between circulating chemerin levels and lipoprotein subfractions in nondiabetic obese and nonobese subjects. Clinical Endocrinology. 2014;81(3):370–377. doi: 10.1111/cen.12363. [DOI] [PubMed] [Google Scholar]
- 44.Dessein P. H., Tsang L., Woodiwiss A. J., Norton G. R., Solomon A. Circulating concentrations of the novel adipokine chemerin are associated with cardiovascular disease risk in rheumatoid arthritis. Journal of Rheumatology. 2014;41(9):1746–1754. doi: 10.3899/jrheum.140122. [DOI] [PubMed] [Google Scholar]
- 45.Fülöp P., Seres I., Lorincz H., Harangi M., Somodi S., Paragh G. Association of chemerin with oxidative stress, inflammation and classical adipokines in non-diabetic obese patients. Journal of Cellular and Molecular Medicine. 2014;18(7):1313–1320. doi: 10.1111/jcmm.12282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheng C., Daskalakis C. Association of adipokines with insulin resistance, microvascular dysfunction, and endothelial dysfunction in healthy young adults. Mediators of Inflammation. 2015;2015:9. doi: 10.1155/2015/594039.594039 [DOI] [PMC free article] [PubMed] [Google Scholar]