Abstract
Vascular superoxide (O2•) and inflammation contribute to hypertension. The mitochondria are an important source of O2•; however, the regulation of mitochondrial O2• and the antihypertensive potential of targeting the mitochondria remain poorly defined. Angiotensin II and inflammatory cytokines such as IL17A and TNFα significantly contribute to hypertension. We hypothesized that angiotensin II and cytokines co-operatively induce cyclophilin D (CypD)-dependent mitochondrial O2• production in hypertension. We tested if CypD inhibition attenuates endothelial oxidative stress and reduces hypertension. CypD depletion in CypD−/− mice prevents overproduction of mitochondrial O2• in angiotensin II infused mice, attenuates hypertension by 20 mm Hg and improves vascular relaxation compared with wild-type C57Bl/6J mice. Treatment of hypertensive mice with the specific CypD inhibitor Sanglifehrin A reduces blood pressure by 28 mm Hg, inhibits production of mitochondrial O2• by 40%, and improves vascular relaxation. Angiotensin II-induced hypertension was associated with CypD redox-activation by S-glutathionylation and expression of the mitochondria-targeted H2O2 scavenger, catalase, abolished CypD S-glutathionylation, prevented stimulation mitochondrial O2• and attenuated hypertension. The functional role of cytokine-angiotensin II interplay was confirmed by co-operative stimulation of mitochondrial O2• by 3-fold in cultured endothelial cells and impairment of aortic relaxation incubated with combination of angiotensin II, IL17A and TNFα which was prevented by CypD depletion or expression of mitochondria-targeted SOD2 and catalase. These data support a novel role of CypD in hypertension and demonstrate that targeting CypD decreases mitochondrial O2•, improves vascular relaxation and reduces hypertension.
Keywords: mitochondria, endothelial oxidative stress, vasorelaxation, cyclophilin D, angiotensin II, inflammatory cytokines, hypertension
INTRODUCTION
Hypertension is a multifactorial disorder involving perturbations of the vasculature, the kidney and the central nervous system.1 This disease represents a major risk factor for stroke, myocardial infarction, and heart failure.2 Despite treatment with multiple drugs, 24% of hypertensive patients remain hypertensive,3 likely due to the mechanisms contributing to blood pressure elevation that are not affected by current treatments. In almost all experimental models of hypertension, production of reactive oxygen species (ROS: O2• and H2O2) is increased in multiple organs.4 In the vasculature ROS promote vasoconstriction and remodeling, thus increasing systemic vascular resistance.5 Systemic vascular resistance is increased in virtually all cases of adult hypertension,6 and thus understanding alterations of vascular function in hypertension remains of utmost importance.
The mitochondria are an important source of O2• 7 and we have recently shown that over-expression of mitochondrial superoxide dismutase (SOD2) or scavenging of mitochondrial ROS with mitochondria-targeted antioxidants attenuate hypertension.8, 9 Regulation of mitochondrial O2• and therapeutic potential of targeting the mitochondria however is poorly defined. 10
We previously reported that inhibition of mitochondrial Cyclophilin D (CypD) in isolated endothelial mitochondria reduces O2• production and recent studies have shown that CypD deficiency reduced O2• production in leukocytes.11, 12 CypD is a regulatory subunit of the mitochondrial permeability transition pore (mPTP) and acts as Ca2+ sensitizer for mPTP opening 13 which is implicated in the regulation of cell death.14, 15 CypD has been targeted for reducing ischemic heart injury and transplant rejection using the non-specific CypD inhibitor cyclosporine A.16 However, the off-target effects of cyclosporine A paradoxically lead to increased sympathetic outflow, endothelin production, vasoconstriction and hypertension which is likely associated with calcineurin inhibition.17 Indeed, genetic CypD depletion did not alter the basal blood pressure.12 We therefore hypothesized that CypD contributes to O2• overproduction in mitochondria, vascular oxidative stress and hypertension, and that targeting CypD decreases mitochondrial O2• and reduces hypertension. To test this hypothesis, we studied CypD depleted human aortic endothelial cells and CypD−/− mice. We also studied redox activation of CypD and the potential interplay in this process between angiotensin II, IL17A and TNFα which significantly contribute to hypertension. 18–20 Finally, we examined the therapeutic potential of targeting CypD in hypertension by treatment of hypertensive mice with the CypD inhibitor Sanglifehrin A (SFA).21
Materials and Methods
Reagents
Angiotensin II (Ang II), TNFα and IL17A were purchased from Sigma (St Luis, MO), Thermo Scientific (Rockford, IL) and Ebioscience (San Diego, CA). MitoSOX and DHE were supplied by Invitrogen (Grand Island, NY). CypD, SOD2 and GSH antibodies were obtained from Abcam (San Francisco, CA). mitoEbselen was purchased from Enzo Life Sciences (San Diego, CA).
Cell culture
Human aortic endothelial cells (HAECs) were purchased from Lonza (Chicago, IL) and cultured in EGM-2 medium supplemented with 2% fetal bovine serum but without antibiotics. On the day before the study, the fetal bovine serum concentration was reduced to 1%. Potential interplay between Ang II, IL17A and TNFα was tested in HAECs treated for 24 hours with Ang II (Sigma, A9525), TNFα (Thermo Scientific, 1857619) and/or IL17A (Ebioscience, 14-8171).
Animal experiments
Hypertension was induced by Ang II infusion (0.7 mg/kg/day, Sigma A6402) in 2–3 months old male mice as described previously 22 using mCAT (Stock# 016197), TgSOD2 23 and CypD−/− (Stock# 022308) mice which have C57Bl/6J genetic background (Jackson Labs). In some experiments, six days after saline or Ang II minipump placement, C57Bl/6J mice received a second minipump for infusion with saline as vehicle or the CypD inhibitor SFA (i.p. 10 mg/kg/day). In order to test the pro-hypertensive role of IL17A some mice were infused with recombinant mouse IL17A (i.p. 1.5 μg/day, Ebioscience, 14-8171). The role of TNFα was tested by i.p. treatment with TNFα blocker Etanercept (i.p. 0.2 mg/day, Amgen Inc.). Blood pressure was monitored by the telemetry and tail cuff methods as previously described.24, 25
Superoxide measurements using HPLC
Cells were cultured up to 80% confluence. Stock solutions of MitoSOX (4 mM) and DHE (10 mM) were dissolved in DMSO and were diluted in KHB buffer to a final concentration of 2 μM MitoSOX and 10 μM DHE. Cells loaded with dye were incubated in a tissue culture incubator for 20 minutes. Next, buffer was aspirated and scraped cells were mixed with methanol (300 μl) and homogenized with a glass pestle. The cell homogenates were passed through a 0.22 μm syringe filter and methanol filtrates were analyzed by HPLC according to previously published protocols.26 DHE and MitoSOX oxidation products, 2-hydroxyethidium and ethidium, were separated using a C-18 reverse-phase column (Nucleosil 250 to 4.5 mm) and a mobile phase containing 0.1% trifluoroacetic acid and an acetonitrile gradient (from 37% to 47%) at a flow rate of 0.5 ml/min. Ethidium and 2-hydroxyethidium were detected with a fluorescence detector using an emission wavelength of 580 nm and an excitation of 480 nm. Production of cytoplasmic and mitochondrial O2• was measured as accumulation of 2-hydroxyethidium and mito-2-hydroxyethidium in DHE or mitSOX supplemented samples as described previously.8
Nitric oxide measurements by Electron Spin Resonance
NO• levels in endothelial cells and vessels were quantified by ESR and colloid Fe(DETC)2 as described previously.27 ESR spectra were recorded by EMX ESR spectrometer (Bruker Biospin Corp., Billerica, MA) with super high Q microwave cavity using suprasil nitrogen Dewar flask (Wilmad-Labglass, Vineland, NJ). The ESR settings for NO measurements were as follows: field sweep, 100 Gauss; microwave frequency, 9.43 GHz; microwave power, 10 milliwatts; modulation amplitude, 2 Gauss; conversion time, 70 msec; time constant, 5.24 sec; scan number, 4.
Vascular relaxation study
Isometric tension studies were performed on 2 mm mouse aortic rings dissected free of perivascular fat from C57B/6J, mCAT, tgSOD2 and CypD−/− mice (Jackson Lab). Studies were performed in a horizontal wire myograph (DMT, Aarhus, Denmark, models 610M and 620M) containing physiological salt solution with the composition of 118 mM NaCl, 4.7 mM KCl, 1.2 mM MgSO4, 1.2 mM KH2PO4, 25 mM NaHCO3, 11 mM glucose, and 1.8 mM CaCl2. The isometric tone of each vessel was recorded using LabChart Pro v7.3.7 (AD Instruments, Australia). The aortic rings were equilibrated over a 2-hour period by heating and stretching the vessels to an optimal baseline tension of 36 millinewtons before contracting them with three cycles of 60 mM KCl physiological saline solution. Endothelium-dependent and independent vascular relaxation was tested following pre-constriction with 1uM phenylephrine. Once the vessels reached a steady state contraction, increasing concentrations of acetylcholine were administered, and the response to each concentration of drug was recorded.
Statistics
Experiments were analyzed using the Student Neuman Keuls post-hoc test and analysis of variance (ANOVA). P levels < 0.05 were considered significant.
Results
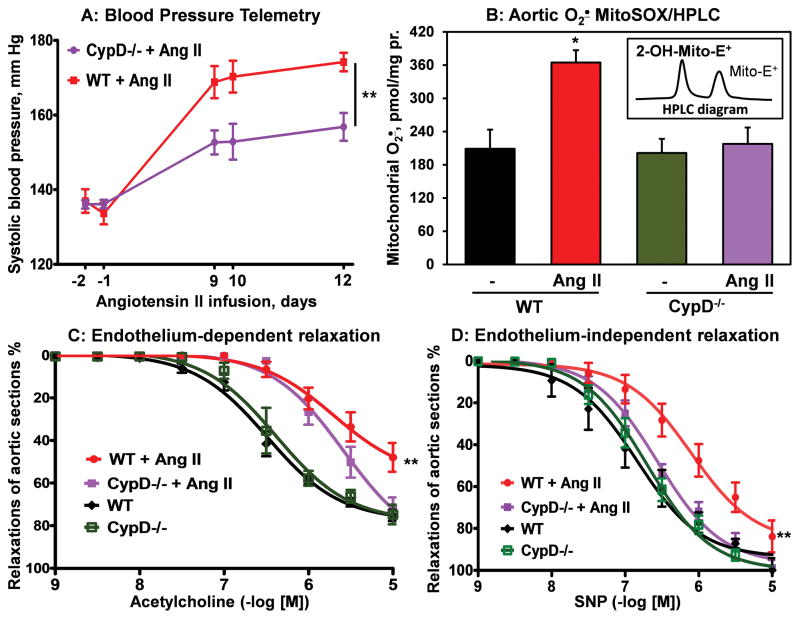
Effect of CypD depletion on angiotensin II-induced hypertension, vascular O2• and vasodilation
In initial studies we sought to determine if CypD deletion in the CypD−/− mice decreases vascular oxidative stress, improves vascular relaxation and attenuates Ang II-induced hypertension compared with wild-type C57Bl/6J mice. Indeed, CypD−/− mice infused with Ang II (0.7 mg/kg/day) had lower blood pressure compared with wild type mice while basal blood pressure was not different (Figure 1A). Following 14 days of Ang II infusion, mice were sacrificed and aortas were isolated for the measurement of mitochondrial O2• and the analysis of vascular relaxation. As expected, CypD deficiency prevented overproduction of mitochondrial O2• in Ang II infused mice (Figure 1B) and improved endothelium-dependent and endothelium-independent relaxation (Figure 1C and 1D) compared with Ang II-infused wild-type mice.
Figure 1.
Effect of CypD depletion on angiotensin II-induced hypertension, vascular O2•, and vasorelaxation. (A) Blood pressure was measured by telemetry in CypD−/− or C57Bl/6J wild type mice infused with either saline (Sham) or Ang II (0.7 mg/kg/ml). (B) Mitochondrial O2• in aorta isolated from Sham or Ang II-infused mice was measured by mitochondria-targeted probe MitoSOX and HPLC following accumulation of O2•-specific product 2-OH-MitoE+. (C) Endothelium-dependent relaxation to acetylcholine. (D) Endothelium-independent relaxation to NO donor SNP. Results are mean ± SEM (n=8). *P<0.05 vs Sham, **P<0.01 vs CypD−/−+Ang II (n=8).
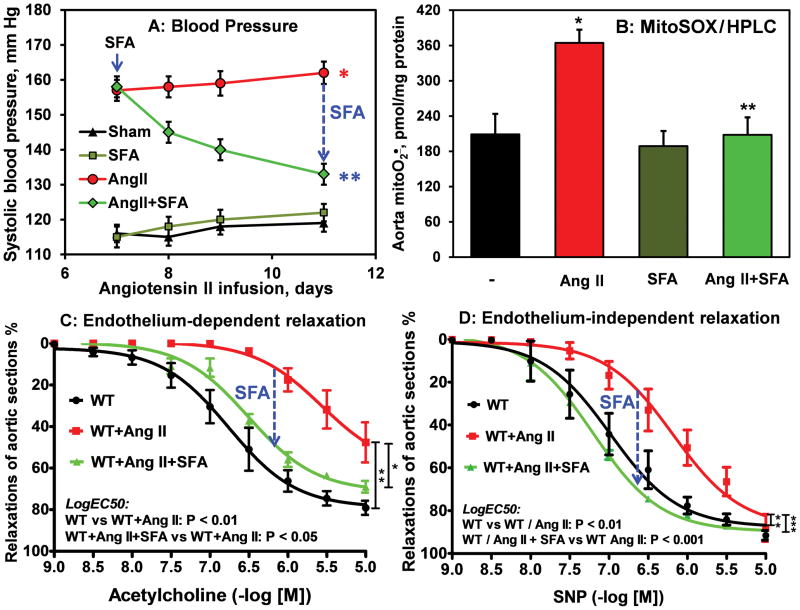
Therapeutic potential of targeting CypD after onset of hypertension
Based on the above results with genetic depletion of CypD, we tested if the specific CypD inhibitor Sanglifehrin A (SFA) can lower blood pressure, reduce mitochondrial O2•, and improve vascular relaxation. To accomplish this we implanted wild-type mice with osmotic minipump containing Ang II and started treatment with Sanglifehrin A after the onset of Ang II-induced hypertension (Figure 2A). Indeed, treatment of hypertensive mice with CypD inhibitor Sanglifehrin A reduced blood pressure (Figure 2A), normalized mitochondrial O2• production (Figure 2B) and improved endothelium-dependent and endothelium-independent relaxation (Figure 2C and 2D). These data support the therapeutic potential of targeting CypD in hypertension.
Figure 2.
Treatment of hypertensive mice with CypD inhibitor Sanglifehrin A. C57Bl/6J wild type mice were implanted with angiotensin II osmotic pumps (0.7 mg/kg/ml) and seven days later received Sanglifehrin A (SFA) (i.p. 10 mg/kg/day) after onset of Ang II-induced hypertension. (A) Blood pressure was measured by tail-cuff method. Following 14 days of saline or Ang II infusion, mice were sacrificed for isolation of aorta to study mitochondrial O2• using MitoSOX and HPLC (B) or to study vasodilation.8 (C) Endothelium-dependent relaxation to acetylcholine. (D) Endothelium-independent relaxation to NO donor SNP. Results are mean ± SEM (n=8). *P<0.05 vs Sham, **P<0.01 vs Ang II, ***P<0.001 vs Ang II+SFA (n=8).
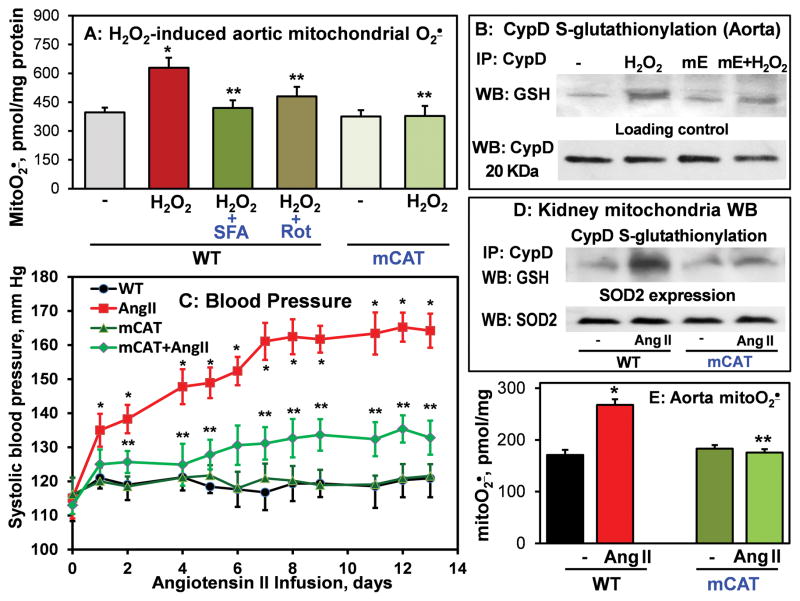
The role of CypD S-glutathionylation in stimulation of mitochondrial O2• and hypertension
CypD is exquisitely H2O2-sensitive via its cysteine 203 residue, which acts as a redox switch when it is S-glutathionylated.28 We propose that mitochondrial H2O2 activates CypD by S-glutathionylation and this induces overproduction of mitochondrial O2• in the electron transport chain. The potential role of mitochondrial H2O2 in hypertension, CypD S-glutathionylation and stimulation of mitochondrial O2• was studied in transgenic mice expressing mitochondria targeted catalase (mCAT) and aortic vessels treated with H2O2. Treatment of isolated aortic segments with H2O2 (100 μM, Krebs-Hepes buffer, 60 min at 37 °C) significantly increased mitochondrial O2• and induced CypD S-glutathionylation (Figure 3A,B). Supplementation with the specific CypD inhibitor Sanglifehrin A (1 μM) or treatment with the complex I inhibitor rotenone blocked H2O2-induced mitochondrial O2• production (Figure 3A). Scavenging mitochondrial H2O2 using mitoEbselen or mitochondrial-targeted catalase in aorta isolated from mCAT mice completely prevented CypD S-glutathionylation and reduced mitochondrial O2•.
Figure 3.
Redox activation of CypD by S-glutathionylation in vascular oxidative stress and hypertension. (A) Mitochondrial O2• in mouse aorta isolated from WT or mCAT mice and treated with H2O2 (100 μM, 30 min). Sanglifehrin A (SFA, 1 μM) was added prior to H2O2 and complex I inhibitor rotenone (ROT, 1 μM) was added after H2O2. **P<0.01 vs H2O2 (N=6). (B) Western blot analysis of CypD S-glutathionylation in C57Blk/6J mouse aorta treated with H2O2 in the presence of mitoEbselen (mE, 1 nM) or DMSO as a vehicle.9 (C) Tail-cuff blood pressure measurements in C57Blk/6J (WT) or mCAT mice infused with Ang II (0.7 mg/kg/day). (D) Western blot study of CypD S-glutathionylation and SOD2 expression in mitochondria isolated from C57Blk/6J (WT) or mCAT Ang II-infused mice. (E) Following 14 days of saline or Ang II infusion, mice were sacrificed for isolation of aorta to study mitochondrial O2• using MitoSOX and HPLC.8 *P<0.05 vs Sham, **P<0.01 vs Ang II (n=8).
A potential role of CypD S-glutathionylation in hypertension was studied in Ang II-infused mCAT and wild-type mice. Ang II-induced hypertension was inhibited in mCAT mice compared with C57Bl/6J wild type mice (Figure 3C). Following 14-days of Ang II infusion mice were sacrificed and we analyzed CypD S-glutathionylation, SOD2 expression and mitochondrial O2• production. Western blot analysis revealed significant CypD S-glutathionylation in tissue isolated from wild-type mice infused with Ang II while expression of mitochondrial-targeted H2O2 scavenger catalase in mCAT mice significantly attenuated CypD S-glutathionylation (Figure 3D). Furthermore, production of mitochondrial O2• was substantially increased in aorta from Ang II-infused wild-type mice but not in aorta from Ang II-infused mCAT mice (Figure 3E). Of note, Western blot showed no change in mitochondrial superoxide dismutase level between wild-type and mCAT mice; therefore, the lack of mitochondrial O2• overproduction in mCAT mice is not due to elevated SOD2 level (Figure 3D). These data support a potential role of CypD S-glutathionylation in stimulation of mitochondrial O2• and hypertension.
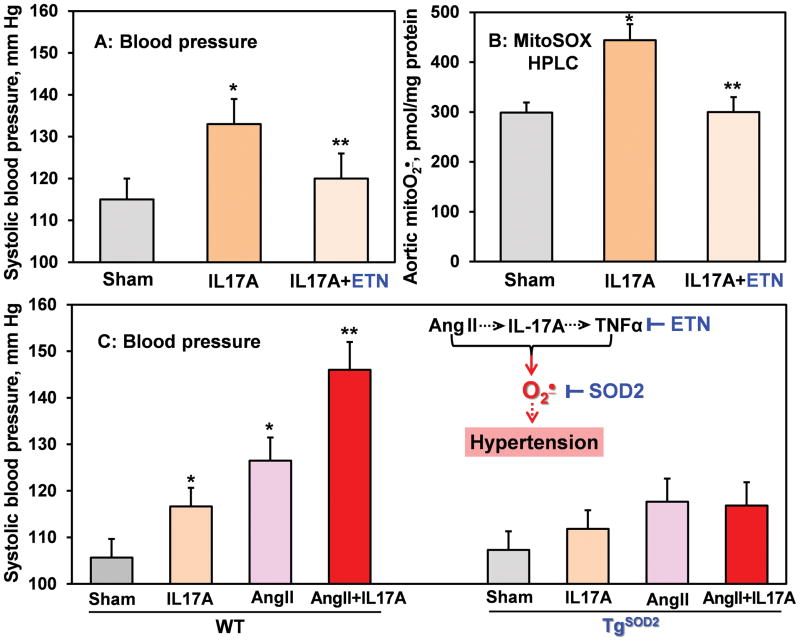
Interplay between angiotensin II and inflammatory cytokines IL17A and TNFα in hypertension
Given that Ang II and inflammatory cytokines IL17A and TNFα increase vascular ROS, 19, 20, 29, 30 we hypothesized that Ang II, IL17A and TNFα may co-operatively activate redox-dependent CypD and increase mitochondrial O2• production. In order to test this hypothesis we infused mice with IL17A or IL17A+TNFα blocker, Etanercept (Amgen Inc.). IL17A increased blood pressure to 133 mmHg and vascular mitochondrial O2• while Etanercept attenuated hypertensive response to IL17A and inhibited IL17A induced mitochondrial O2• (Figure 4A and 4B). These data support the important role of IL17A and TNFα in the stimulation of mitochondrial O2• and hypertension.
Figure 4.
Angiotensin II - cytokine interplay in hypertension. Blood pressure (A) and aortic mitochondrial O2• (B) in C57Bl/6J mice infused with IL17A (1.5 μg/day) and Etanercept (ETN, i.p. 0.2 mg/day). *P<0.05 vs Sham, **P<0.01 vs Ang II (N=8). (C) Tail-cuff blood pressure measurements in C57Bl/6J and TgSOD2 mice infused for 7 days with Ang II (0.3 mg/kg/day), IL17A (1 μg/day) or both. *P<0.05 vs Sham, **P<0.001 vs Ang II (N=6).
In additional experiments we tested the potential interplay between Ang II and inflammatory cytokines in hypertension in mice infused with low dose of Ang II (0.3 mg/kg/day) and IL17A (1 μg/day).20, 31 In wild-type mice, infusion of low doses of either Ang II or IL17A caused small increases of blood pressure, but combined treatment with IL17A and low dose Ang II co-operatively induced severe hypertension. SOD2 overexpression abrogated this hypertensive response to Ang II and IL17A (Figure 4C). These data support an important role of the interplay between Ang II and cytokines in stimulation of mitochondrial O2• in hypertension.
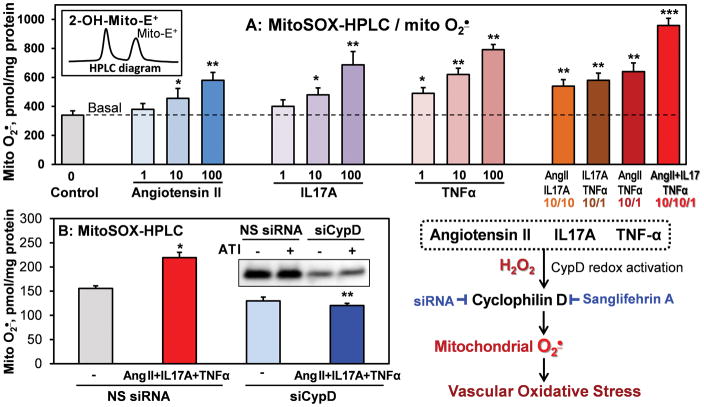
Co-operative stimulation of CypD-dependent mitochondrial O2• by angiotensin II, IL17A and TNFα
The above studies in intact mice demonstrate Ang II and inflammatory cytokines act in concert to increase blood pressure and that this is likely mediated by mitochondrial O2• (Figure 4). We therefore hypothesized that Ang II, IL17A and TNFα co-operatively induce CypD-dependent production of mitochondrial O2•. To further test this hypothesis and extend our findings to human cells, we studied mitochondrial O2• in human aortic endothelial cells (HAECs) treated with low doses of Ang II, IL17A, TNFα either separately or in combination using HPLC analysis of O2• specific MitoSOX product 2-OH-Mito-E+ (Figure 5A, insert).32 Treatment of endothelial cells with Ang II and cytokines induced mitochondrial O2• in a dose-dependent manner. The lowest concentration of TNFα that increased mitochondrial O2• was 1 nM while Ang II and IL17A required 10 nM. We then tested if the combination of these low doses of Ang II, IL17A and TNFα co-operatively increased mitochondrial O2• production. We found that the combinations of Ang II+17A, Ang II+TNFα and IL17A+TNFα modestly increased mitochondrial O2• above the basal level; however, the triple combination of Ang II, IL17A and TNFα co-operatively increased mitochondrial O2• above maximal levels compared to each single stimulation (Figure 5A).
Figure 5.
Production of mitochondrial O2• in human aortic endothelial cells (HAECs). (A) HAECs were treated with Ang II, IL17A and TNFα (1–100 ng/ml) or their combinations for 24 hours prior to measurements of mitochondrial O2• by MitoSOX and HPLC (A).8 *P<0.05 vs Control, **P<0.01 vs Control, ***P<0.001 vs double treatments (N=4–6). (B) Measurements of mitochondrial O2• in CypD depleted cells. HAECs were transfected with non-silencing (NS) or CypD siRNA prior to stimulation with Ang II (10 nM), IL17A (10 ng/ml) and TNFα (1 ng/ml). CypD depletion was confirmed by Western blot analysis (Insert). *P<0.05 vs Control, **P<0.01 vs Ang II+IL17A+TNFα (ATI) (N=6).
To directly confirm a role of CypD in stimulation of mitochondrial O2• in human cells, we employed siRNA against CypD. Transfection of HAECs with CypD siRNA reduced CypD expression and abolished the stimulation of mitochondrial O2• (Figure 5B). These data support the interplay between Ang II and cytokines in the stimulation of CypD-dependent mitochondrial O2• overproduction and show that CypD has a role in the production of mitochondrial O2• by human endothelial cells.
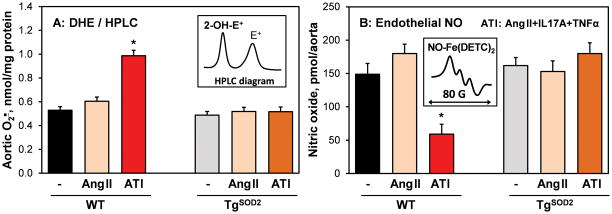
Role of CypD and mitochondrial ROS in impaired vasodilation by angiotensin II, IL17A and TNFα
We have previously shown that Ang II stimulates cytokine production 33 and that Ang II causes blunted hypertension in RAG1 KO mice lacking lymphocytes, mice deficient in the cytokine IL17, or in mice co-treated with the TNFα antagonist Etanercept.34 We hypothesized that inflammatory cytokines such as TNFα and IL17A act in concert with Ang II to stimulate O2• production in vessels leading to inactivation of endothelial nitric oxide and impaired vascular relaxation. Indeed, ex vivo incubation of aorta with Ang II did not significantly affect aortic O2• or NO levels while the combination of Ang II, IL17A and TNFα caused a 2-fold increase in O2• and a 3-fold reduction of NO (Figure 6). We directly tested the role of mitochondrial O2• in cytokine-induced vascular oxidative stress and impaired NO production using transgenic mice that overexpress mitochondrial superoxide dismutase (TgSOD2).23 SOD2 overexpression completely abolished vascular oxidative stress and prevented loss of endothelial NO (Figure 6).
Figure 6.
Angiotensin II - cytokine interplay in vascular oxidative stress. in C57Bl/6J (WT) or TgSOD2 mouse aorta Isolated three mm aortic segments were placed in RPMI tissue culture and treated ex vivo with Ang II (10 nM) or Ang II + IL17A (10 ng/ml) + TNFα (1 ng/ml) for 24 hours. Following incubation, aortic segments were used for O2• and nitric oxide analysis. (A) Vascular O2• was measured in by DHE probe and HPLC. 26 (B) endothelial nitric oxide was measured by Fe-DETC probe and ESR.27 in C57Bl/6J (WT) or TgSOD2 mouse aorta vascular NO was measured by ESR and specific NO spin trap Fe(DETC)2.27 *P<0.05 vs Control (N=6).
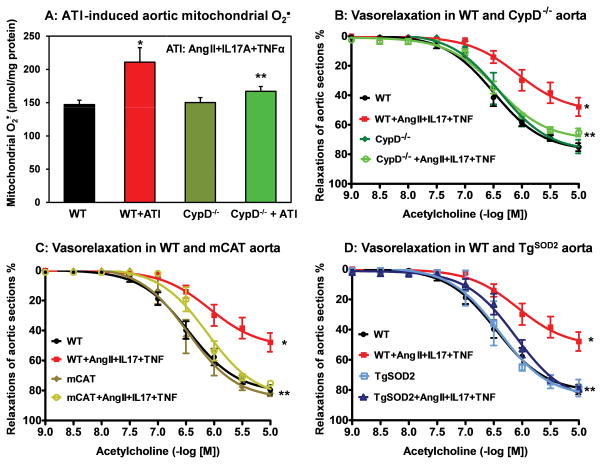
We further examined the functional role of mitochondrial CypD-dependent oxidative stress in response to Ang II, IL17A and TNFα in aortic sections isolated from CypD−/− mice and compared them to wild-type littermates (C57Bl/6J). As we expected, treatment of aortic vessels with Ang II + IL17A + TNFα significantly increased production of mitochondrial O2• and impaired endothelium-dependent relaxation which were prevented by CypD depletion (Figure 7A and 7B).
Figure 7.
Role of CypD and mitochondrial ROS in impaired relaxation in vessels treated with angiotensin II, IL17A and TNFα. Aortas were isolated from wild-type, CypD−/−, mCAT or TgSOD2 mice and were placed in tissue culture (RPMI) for 24 hours. Aortas were supplemented with vehicle or combination of Ang II + TNFα + IL17A (ATI). Mitochondrial O2• (A) and endothelium-dependent relaxation (B, C, D) in vessels treated with combination of Ang II (10 nM), IL17A (10 ng/ml) and TNFα (1 ng/ml) for 24 hours. Mitochondrial O2• was measured by MitoSOX and HPLC.8 Results are mean ± SEM (n=8). *P<0.05 vs WT, **P<0.01 vs WT+ATI.
We have examined the functional role of CypD-dependent oxidative stress in aortic sections isolated from transgenic mice overexpressing the mitochondrial antioxidants SOD2 (TgSOD2) or catalase (mCAT). Our data show that treatment of aortic vessels with Ang II + IL17A + TNFα lead to severe impairment of endothelium-dependent relaxation. Interestingly, SOD2 overexpression or expression of mitochondria-targeted catalase significantly attenuated the impairment of relaxation similar to the protection afforded by CypD deletion (Figure 7B–D).
These data show that the pro-oxidant milieu of Ang II, IL17A and TNFα leads to severe vascular oxidative stress, reduces endothelial NO and impairs vascular relaxation, which is prevented by the scavenging of mitochondrial O2• and H2O2 in vessels from TgSOD2 and mCAT mice. Furthermore, our data confirm an important role of CypD in the regulation of vascular oxidative stress.
Discussion
The present study provides the first evidence that CypD facilitates production of mitochondrial O2• by intact vessels and in cultured human endothelial cells. Our data show that inflammatory cytokines and Ang II co-operatively induce CypD-dependent mitochondrial O2• in HAECs and aortic vessels (Figures 5 and 7). In this work we found that CypD depletion diminished vascular production of mitochondrial O2•, improved relaxation and attenuated the development of hypertension in Ang II infused mice (Figure 1). Furthermore, treatment of hypertensive mice with CypD inhibitor Sanglifehrin A diminished vascular oxidative stress and reduced blood pressure (Figure 2). These data suggest that CypD has a previously unidentified role in hypertension and support the therapeutic potential of targeting CypD in this disease.
CypD mediated overproduction of mitochondrial ROS contributes to impaired vascular relaxation and overexpression of mitochondrial SOD2 and catalase protect endothelium-dependent relaxation (Figure 7). These data support an important role of mitochondrial oxidative stress in impairment of vascular relaxation. We would stress that systemic vascular resistance is increased in virtually all cases of adult hypertension, and thus understanding alterations of vascular function in hypertension is very important. We propose that CypD can also contribute to other vascular conditions associated with oxidative stress such as atherosclerosis.
It should be noted that resistance arteries contribute more significantly to blood pressure changes than large arteries such as aorta; however, hypertension is associated with impaired vascular relaxation both in resistance and conduit arteries. In our study we used aorta since it provides sufficient material from a single mouse to perform several critical measurements: HPLC analysis of O2• specific products 2-OH-Mito-E+ and 2HO-E+;32 specific EPR analysis of endothelial NO; 27 and vascular relaxation. The mechanisms of impaired vasodilatation may differ in resistance and large arteries, therefore, future studies have to confirm that relaxation of resistance vessels can be rescued by CypD inhibition or depletion. Our data showed that CypD inhibition improved endothelium-dependent and endothelium-independent relaxation (Figure 2B) implicating CypD in endothelial and smooth cells dysfunction. The cell specific role of CypD in vascular impairment; however, remain unclear.
We have previously shown that Ang II stimulates the production of mitochondrial O2• in endothelial cells which is blocked by non-specific CypD inhibitor, cyclosporine A, or depletion of NADPH oxidase.9, 11 In this work, we further examined the mechanisms of mitochondrial O2• overproduction and found that stimulation of mitochondrial O2• in mice and isolated aortic vessels is associated with CypD S-glutathionylation and scavenging of mitochondrial H2O2 by mitoEbselen or mitochondria-targeted catalase prevents CypD S-glutathionylation and diminishes CypD dependent production of mitochondrial O2• (Figure 3, 5, 7). These data implicate a redox-sensitive activation of CypD in regulation of vascular mitochondrial O2•.
Inflammation is commonly associated with hypertension and contributes to pathogenesis of this disease.1, 35 TNFα and IL17 are increased in hypertensive subjects by 4-fold 18, 19 and TNFα is an independent risk factor for hypertension.18 Our previous animal studies showed an important role of T cell activation in IL17 and TNFα production in hypertension; 19, 34 however, specific targets of cytokines in hypertension are not clear. It is understood that multiple cytokines interact to promote other established immune and inflammation-based diseases; however, the potential role of cytokine-angiotensin II interplay in hypertension has not been studied. In this work we have shown that Ang II, TNFα and IL17A co-operatively induced CypD-dependent overproduction of mitochondrial ROS which contributes impaired vasodilatation in hypertension.
Previous studies have shown that CypD deficiency and Sanglifehrin A therapy reduced ROS production in leukocytes of Ang II-infused mice.12 It was suggested that ROS overproduction by phagocytic cells contributes to vascular dysfunction and that blockade of CypD diminishes ROS production by leukocytes and reduces oxidative stress. This work adds to the previous studies in showing an important role of this mitochondrial protein in endothelial cells and its role in intact vessels. In this work we have investigated CypD-dependent stimulation of mitochondrial O2• in endothelial cells and intact aortic vessels. We defined a novel role of inflammatory cytokines in redox-dependent CypD activation and directly demonstrated the role of vascular mitochondrial O2• and H2O2 in impaired endothelium-dependent relaxation in response to Ang II, TNFα and IL17A using vessels isolated from transgenic mice overexpressing mitochondrial SOD2 and catalase (Figure 7). This work therefore provides direct evidence for CypD-mediated endothelial dysfunction.
The precise molecular mechanism of CypD-dependent stimulation of mitochondrial O2• in endothelial cells is not clear. It is likely occur at mitochondrial complex I since treatment with complex I inhibitor rotenone significantly inhibited CypD-dependent mitochondrial O2• production (Figure 3A). We have previously shown an important role of reverse electron transport 36 and complex I in mitochondrial O2• overproduction and hypertension 37 and now we found that CypD depletion prevents stimulation of mitochondrial O2• in response to Ang II, TNFα and IL17A.
It is understood that multiple cytokines interact to promote other established immune and inflammation-based diseases; however, the potential role of cytokine-angiotensin II interplay in hypertension has not been studied. Inflammation is commonly associated with hypertension and contributes to the pathogenesis of this disease.1, 35 TNFα and IL17 are increased in hypertensive subjects by 4-fold 18, 19 and TNFα is an independent risk factor for hypertension.18 In this work we have shown that Ang II, TNFα and IL17A co-operatively induced CypD-dependent overproduction of mitochondrial ROS which contributes impaired vasodilatation in hypertension.
Previous studies showed an important role of cytokines in vascular dysfunction and hypertension both in Ang II- and salt-induced hypertension models.20, 33 In this work we show that Ang II alone did not increase O2• or decrease NO in cultured aortic tissue, yet Ang II alone caused a modest blood pressure elevation to the pre-hypertensive level of 130 mm Hg likely due to increased water intake (thirst) and volume retention directly regulated by Ang II.38, 39 The increased shear stress and salt accumulation subsequently causes local inflammation 40 and mitochondrial ROS overproduction 41 leading to end-organ damage such as endothelial dysfunction which drives the development of hypertension.30 Our data showed that CypD inhibition reduced endothelial dysfunction in response to inflammatory cytokines; therefore, therapeutic targeting of CypD can be potentially beneficial in reducing end-organ damage in hypertension.
In addition to hypertension, there are many other common conditions including aging, atherosclerosis, diabetes and degenerative neurological disorders in which mitochondrial oxidative stress seems to play a role. 42, 43 Of note, large clinical trials have failed to show a benefit of often-employed antioxidants such as vitamin E and vitamin C in many of these conditions,44, 45 and have paradoxically shown deleterious effects in some trials.45 There are many potential explanations why these antioxidants have proven ineffective in these studies, but one relates to the fact that agents such as vitamin E and vitamin C are not targeted to sites of ROS generation that are most important in pathological conditions. It is conceivable that CypD inhibitors or mitochondria-targeted antioxidants would be more effective in these conditions. The ability to achieve these effects in relatively low doses might also limit potential untoward effects of antioxidant therapy observed with other agents.
Perspectives
The present studies show that CypD plays an important role in mitochondrial O2• overproduction in endothelial cells and vasculature in response to inflammatory cytokines and Ang II. These studies revise the traditional concept that CypD is mainly acts as Ca2+ sensitizer for mPTP opening leading to mitochondrial swelling and cell death. Our studies demonstrate that Ang II, TNFα and IL17A co-operatively induced CypD-dependent mitochondrial O2• production, implicate CypD in development of vascular oxidative stress, impaired vascular relaxation and hypertension. Our data suggest that redox activation of CypD by S-glutathionylation stimulates O2• production in a feed-forward fashion leading to vascular oxidative stress. Targeting vascular CypD could be used for development of future pharmacological interventions to improve endothelial function, reduce hypertension and attenuate end organ damage associated with hypertension.
Novelty and Significance.
What Is New?
The present study provides the first evidence that CypD facilitates production of mitochondrial O2• by intact vessels and in cultured human endothelial cells.
Stimulation of mitochondrial O2• in mice and isolated aortic vessels is associated with CypD S-glutathionylation and scavenging of mitochondrial H2O2 by mitoEbselen or mitochondria-targeted catalase prevents CypD S-glutathionylation and diminishes CypD dependent production of mitochondrial O2•. These data implicate a redox-sensitive activation of CypD in regulation of vascular mitochondrial O2•.
In this work we found that CypD depletion diminished vascular production of mitochondrial O2•, improved vascular relaxation and attenuated the development of Ang II induced hypertension.
What Is Relevant?
Treatment of hypertensive mice with CypD inhibitor Sanglifehrin A diminished vascular oxidative stress and reduced blood pressure.
Our data suggest that CypD has a previously unidentified role in vascular dysfunction, hypertension and support the therapeutic potential of targeting CypD in this disease.
High blood pressure is associated with ROS overproduction which contributes to end-organ damage such as endothelial dysfunction and drives the development of hypertension. Our data showed that CypD inhibition reduced endothelial dysfunction in response to inflammatory cytokines; therefore, therapeutic targeting of CypD can be potentially beneficial in reducing end-organ damage in hypertension.
We propose that CypD-mediated mitochondrial oxidative stress can contribute not only to hypertension but also to atherosclerosis and other vascular diseases.
Summary
Our data demonstrate a novel role of CypD in regulation of mitochondrial O2• and show that targeting CypD decreases mitochondrial oxidative stress, improves vascular relaxation and reduces hypertension.
Acknowledgments
We thank Dr. Richard Sedrani (Novartis Pharma AG) and Dr. Andreas Daiber (Mainz University Medical Center) for providing CypD inhibitor Sanglifehrin A for our animal studies. We thank AMGEN Inc. for providing TNFα blocker Etanercept for our work.
Sources of Funding: This work was supported by funding from National Institute of Health (R01HL124116-01A1), Vanderbilt University (VR7040 and UL1 RR024975-01) and the American Heart Association (15IRG22730049). Dr. Itani was funded by the National Institute of Health (1F32HL124972-01).
Non-standard Abbreviations and Acronyms
- Ang II
angiotensin II
- ATI
combination of angiotensin II + IL17A + TNFα
- CypD
Cyclophilin D
- CypD−/−
CypD knockout mice
- DHE
dihydroethidium
- ESR
electron spin resonance
- ETN
Etanercept
- HAECs
human aortic endothelial cells
- HPLC
high-performance liquid chromatography
- H2O2
hydrogen Peroxide
- IL17
Interleukin 17
- mCAT
mice expressing mitochondria-targeted catalase
- mitoEbselen
mitochondria-targeted hydrogen peroxide scavenger ebselen
- MitoSOX
mitochondria-targeted analog of dihydroethidium, fluorescent O2• probe
- mPTP
mitochondrial permeability transition pore
- O2•
superoxide radicals
- ROS
reactive oxygen species
- Rot
inhibitor of mitochondrial complex I, rotenone
- SFA
CypD inhibitor Sanglifehrin A
- SNP
sodium nitroprusside
- SOD2
mitochondrial manganese superoxide dismutase
- TgSOD2
transgenic mice overexpressing mitochondrial antioxidants SOD2
- WT
wild-type C57Bl/6J mice
Footnotes
Disclosures: NONE.
References
- 1.Harrison DG, Marvar PJ, Titze JM. Vascular inflammatory cells in hypertension. Front Physiol. 2012;3:128. doi: 10.3389/fphys.2012.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sacco RL, Benjamin EJ, Broderick JP, Dyken M, Easton JD, Feinberg WM, Goldstein LB, Gorelick PB, Howard G, Kittner SJ, Manolio TA, Whisnant JP, Wolf PA. American heart association prevention conference. Iv. Prevention and rehabilitation of stroke. Risk factors. Stroke. 1997;28:1507–1517. doi: 10.1161/01.str.28.7.1507. [DOI] [PubMed] [Google Scholar]
- 3.Fletcher RD, Amdur RL, Kolodner R, McManus C, Jones R, Faselis C, Kokkinos P, Singh S, Papademetriou V. Blood pressure control among us veterans: A large multiyear analysis of blood pressure data from the veterans administration health data repository. Circulation. 2012;125:2462–2468. doi: 10.1161/CIRCULATIONAHA.111.029983. [DOI] [PubMed] [Google Scholar]
- 4.Harrison DG, Gongora MC, Guzik TJ, Widder J. Oxidative stress and hypertension. J Am Soc Hypertens. 2007;1:30–44. doi: 10.1016/j.jash.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Lee MY, Griendling KK. Redox signaling, vascular function, and hypertension. Antioxid Redox Signal. 2008;10:1045–1059. doi: 10.1089/ars.2007.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghiadoni L, Taddei S, Virdis A. Hypertension and endothelial dysfunction: Therapeutic approach. Curr Vasc Pharmacol. 2012;10:42–60. doi: 10.2174/157016112798829823. [DOI] [PubMed] [Google Scholar]
- 7.Rubattu S, Pagliaro B, Pierelli G, Santolamazza C, Castro SD, Mennuni S, Volpe M. Pathogenesis of target organ damage in hypertension: Role of mitochondrial oxidative stress. Int J Mol Sci. 2015;16:823–839. doi: 10.3390/ijms16010823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dikalova AE, Bikineyeva AT, Budzyn K, Nazarewicz RR, McCann L, Lewis W, Harrison DG, Dikalov SI. Therapeutic targeting of mitochondrial superoxide in hypertension. Circ Res. 2010;107:106–116. doi: 10.1161/CIRCRESAHA.109.214601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dikalov SI, Nazarewicz RR, Bikineyeva A, Hilenski L, Lassegue B, Griendling K, Harrison DG, Dikalova A. Nox2-induced production of mitochondrial superoxide in angiotensin II - mediated endothelial oxidative stress and hypertension. Antioxid Redox Signal. 2014;20:281–294. doi: 10.1089/ars.2012.4918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eirin A, Lerman A, Lerman LO. Mitochondria: A pathogenic paradigm in hypertensive renal disease. Hypertension. 2015;65:264–270. doi: 10.1161/HYPERTENSIONAHA.114.04598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doughan AK, Harrison DG, Dikalov SI. Molecular mechanisms of angiotensin II mediated mitochondrial dysfunction. Linking mitochondrial oxidative damage and vascular endothelial dysfunction. Circ Res. 2008;102:488–496. doi: 10.1161/CIRCRESAHA.107.162800. [DOI] [PubMed] [Google Scholar]
- 12.Kroller-Schon S, Steven S, Kossmann S, Scholz A, Daub S, Oelze M, Xia N, Hausding M, Mikhed Y, Zinssius E, Mader M, Stamm P, Treiber N, Scharffetter-Kochanek K, Li H, Schulz E, Wenzel P, Munzel T, Daiber A. Molecular mechanisms of the crosstalk between mitochondria and nadph oxidase through reactive oxygen species-studies in white blood cells and in animal models. Antioxid Redox Signal. 2014;20:247–266. doi: 10.1089/ars.2012.4953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakagawa T, Shimizu S, Watanabe T, Yamaguchi O, Otsu K, Yamagata H, Inohara H, Kubo T, Tsujimoto Y. Cyclophilin D-dependent mitochondrial permeability transition regulates some necrotic but not apoptotic cell death. Nature. 2005;434:652–658. doi: 10.1038/nature03317. [DOI] [PubMed] [Google Scholar]
- 14.Kinnally KW, Peixoto PM, Ryu SY, Dejean LM. Is mptp the gatekeeper for necrosis, apoptosis, or both? Biochim Biophys Acta. 2011;1813:616–622. doi: 10.1016/j.bbamcr.2010.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tavecchio M, Lisanti S, Lam A, Ghosh JC, Martin NM, O’Connell M, Weeraratna AT, Kossenkov AV, Showe LC, Altieri DC. Cyclophilin d extramitochondrial signaling controls cell cycle progression and chemokine-directed cell motility. J Biol Chem. 2013;288:5553–5561. doi: 10.1074/jbc.M112.433045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Lisa F, Carpi A, Giorgio V, Bernardi P. The mitochondrial permeability transition pore and cyclophilin D in cardioprotection. Biochim Biophys Acta. 2011;1813:1316–1322. doi: 10.1016/j.bbamcr.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 17.Ponticelli C, Cucchiari D, Graziani G. Hypertension in kidney transplant recipients. Transpl Int. 2011;24:523–533. doi: 10.1111/j.1432-2277.2011.01242.x. [DOI] [PubMed] [Google Scholar]
- 18.Bautista LE, Vera LM, Arenas IA, Gamarra G. Independent association between inflammatory markers (c-reactive protein, interleukin-6, and tnf-alpha) and essential hypertension. J Hum Hypertens. 2005;19:149–154. doi: 10.1038/sj.jhh.1001785. [DOI] [PubMed] [Google Scholar]
- 19.Madhur MS, Lob HE, McCann LA, Iwakura Y, Blinder Y, Guzik TJ, Harrison DG. Interleukin 17 promotes angiotensin II-induced hypertension and vascular dysfunction. Hypertension. 2010;55:500–507. doi: 10.1161/HYPERTENSIONAHA.109.145094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen H, Chiasson VL, Chatterjee P, Kopriva SE, Young KJ, Mitchell BM. Interleukin-17 causes Rho-kinase-mediated endothelial dysfunction and hypertension. Cardiovasc Res. 2013;97:696–704. doi: 10.1093/cvr/cvs422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clarke SJ, McStay GP, Halestrap AP. Sanglifehrin a acts as a potent inhibitor of the mitochondrial permeability transition and reperfusion injury of the heart by binding to cyclophilin-D at a different site from cyclosporin a. J Biol Chem. 2002;277:34793–34799. doi: 10.1074/jbc.M202191200. [DOI] [PubMed] [Google Scholar]
- 22.Dikalova A, Clempus R, Lassegue B, Cheng G, McCoy J, Dikalov S, San Martin A, Lyle A, Weber DS, Weiss D, Taylor WR, Schmidt HH, Owens GK, Lambeth JD, Griendling KK. Nox1 overexpression potentiates angiotensin II-induced hypertension and vascular smooth muscle hypertrophy in transgenic mice. Circulation. 2005;112:2668–2676. doi: 10.1161/CIRCULATIONAHA.105.538934. [DOI] [PubMed] [Google Scholar]
- 23.Kowluru RA, Kowluru V, Xiong Y, Ho YS. Overexpression of mitochondrial superoxide dismutase in mice protects the retina from diabetes-induced oxidative stress. Free Radic Biol Med. 2006;41:1191–1196. doi: 10.1016/j.freeradbiomed.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 24.Krege JH, Hodgin JB, Hagaman JR, Smithies O. A noninvasive computerized tail-cuff system for measuring blood pressure in mice. Hypertension. 1995;25:1111–1115. doi: 10.1161/01.hyp.25.5.1111. [DOI] [PubMed] [Google Scholar]
- 25.Widder JD, Guzik TJ, Mueller CF, Clempus RE, Schmidt HH, Dikalov SI, Griendling KK, Jones DP, Harrison DG. Role of the multidrug resistance protein-1 in hypertension and vascular dysfunction caused by angiotensin II. Arterioscler Thromb Vasc Biol. 2007;27:762–768. doi: 10.1161/01.ATV.0000259298.11129.a2. [DOI] [PubMed] [Google Scholar]
- 26.Dikalov S, Griendling KK, Harrison DG. Measurement of reactive oxygen species in cardiovascular studies. Hypertension. 2007;49:717–727. doi: 10.1161/01.HYP.0000258594.87211.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dikalov S, Fink B. Esr techniques for the detection of nitric oxide in vivo and in tissues. Methods Enzymol. 2005;396:597–610. doi: 10.1016/S0076-6879(05)96052-7. [DOI] [PubMed] [Google Scholar]
- 28.Linard D, Kandlbinder A, Degand H, Morsomme P, Dietz KJ, Knoops B. Redox characterization of human cyclophilin D: Identification of a new mammalian mitochondrial redox sensor? Arch Biochem Biophys. 2009;491:39–45. doi: 10.1016/j.abb.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Shagdarsuren E, Wellner M, Braesen JH, Park JK, Fiebeler A, Henke N, Dechend R, Gratze P, Luft FC, Muller DN. Complement activation in angiotensin II-induced organ damage. Circ Res. 2005;97:716–724. doi: 10.1161/01.RES.0000182677.89816.38. [DOI] [PubMed] [Google Scholar]
- 30.McMaster WG, Kirabo A, Madhur MS, Harrison DG. Inflammation, immunity, and hypertensive end-organ damage. Circ Res. 2015;116:1022–1033. doi: 10.1161/CIRCRESAHA.116.303697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saleh MA, McMaster WG, Wu J, Norlander AE, Funt SA, Thabet SR, Kirabo A, Xiao L, Chen W, Itani HA, Michell D, Huan T, Zhang Y, Takaki S, Titze J, Levy D, Harrison DG, Madhur MS. Lymphocyte adaptor protein lnk deficiency exacerbates hypertension and end-organ inflammation. J Clin Invest. 2015;125:1189–1202. doi: 10.1172/JCI76327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zielonka J, Kalyanaraman B. Hydroethidine- and mitosox-derived red fluorescence is not a reliable indicator of intracellular superoxide formation: Another inconvenient truth. Free Radic Biol Med. 2010;48:983–1001. doi: 10.1016/j.freeradbiomed.2010.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirabo A, Fontana V, de Faria AP, Loperena R, Galindo CL, Wu J, Bikineyeva AT, Dikalov S, Xiao L, Chen W, Saleh MA, Trott DW, Itani HA, Vinh A, Amarnath V, Amarnath K, Guzik TJ, Bernstein KE, Shen XZ, Shyr Y, Chen SC, Mernaugh RL, Laffer CL, Elijovich F, Davies SS, Moreno H, Madhur MS, Roberts J, 2nd, Harrison DG. DC isoketal-modified proteins activate T cells and promote hypertension. J Clin Invest. 2014;124:4642–4656. doi: 10.1172/JCI74084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guzik TJ, Hoch NE, Brown KA, McCann LA, Rahman A, Dikalov S, Goronzy J, Weyand C, Harrison DG. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. J Exp Med. 2007;204:2449–2460. doi: 10.1084/jem.20070657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boos CJ, Lip GY. Is hypertension an inflammatory process? Curr Pharm Des. 2006;12:1623–1635. doi: 10.2174/138161206776843313. [DOI] [PubMed] [Google Scholar]
- 36.Panov A, Schonfeld P, Dikalov S, Hemendinger R, Bonkovsky HL, Brooks BR. The neuromediator glutamate, through specific substrate interactions, enhances mitochondrial ATP production and reactive oxygen species generation in nonsynaptic brain mitochondria. J Biol Chem. 2009;284:14448–14456. doi: 10.1074/jbc.M900985200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nazarewicz RR, Dikalova AE, Bikineyeva A, Dikalov SI. Nox2 as a potential target of mitochondrial superoxide and its role in endothelial oxidative stress. Am J Physiol Heart Circ Physiol. 2013;305:H1131–1140. doi: 10.1152/ajpheart.00063.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coble JP, Grobe JL, Johnson AK, Sigmund CD. Mechanisms of brain renin angiotensin system-induced drinking and blood pressure: Importance of the subfornical organ. Am J Physiol Regul Integr Comp Physiol. 2015;308:R238–249. doi: 10.1152/ajpregu.00486.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;41:625–633. doi: 10.1161/01.HYP.0000052314.95497.78. [DOI] [PubMed] [Google Scholar]
- 40.Harrison DG, Widder J, Grumbach I, Chen W, Weber M, Searles C. Endothelial mechanotransduction, nitric oxide and vascular inflammation. J Intern Med. 2006;259:351–363. doi: 10.1111/j.1365-2796.2006.01621.x. [DOI] [PubMed] [Google Scholar]
- 41.Dikalov SI, Ungvari Z. Role of mitochondrial oxidative stress in hypertension. Am J Physiol Heart Circ Physiol. 2013;305:H1417–1427. doi: 10.1152/ajpheart.00089.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Cavanagh EM, Inserra F, Ferder M, Ferder L. From mitochondria to disease: Role of the renin-angiotensin system. Am J Nephrol. 2007;27:545–553. doi: 10.1159/000107757. [DOI] [PubMed] [Google Scholar]
- 43.Fridovich I. Mitochondria: Are they the seat of senescence? Aging Cell. 2004;3:13–16. doi: 10.1046/j.1474-9728.2003.00075.x. [DOI] [PubMed] [Google Scholar]
- 44.Song Y, Cook NR, Albert CM, Van Denburgh M, Manson JE. Effects of vitamins C and E and beta-carotene on the risk of type 2 diabetes in women at high risk of cardiovascular disease: A randomized controlled trial. Am J Clin Nutr. 2009;90:429–437. doi: 10.3945/ajcn.2009.27491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sesso HD, Buring JE, Christen WG, Kurth T, Belanger C, MacFadyen J, Bubes V, Manson JE, Glynn RJ, Gaziano JM. Vitamins e and c in the prevention of cardiovascular disease in men: The physicians’ health study II randomized controlled trial. JAMA. 2008;300:2123–2133. doi: 10.1001/jama.2008.600. [DOI] [PMC free article] [PubMed] [Google Scholar]