Abstract
Objective:
This study tested a developmental model in which subtypes of childhood maltreatment were hypothesized to have direct and indirect effects on co-occurring depression, anxiety, and substance misuse in adulthood. Indirect effects involved adolescent alcohol use and depression, which were included as mediators in the tested models.
Method:
This prospective longitudinal study (N = 332; 52.4% male) followed the participants from childhood (18 months to 6 years of age) to adulthood (31–41 years old, M = 36.21). Maltreatment subtypes included parent-reported physical and emotional abuse and child-reported sexual abuse. Adult outcomes included measures of substance misuse and mental health (i.e., depression and anxiety). Latent class analysis and structural equation models were used to identify classes of substance misuse and mental health co-occurrence and to test mediating effects of adolescent alcohol use and depression.
Results:
Three classes were identified: (a) low risk of substance misuse and low mental health symptoms, (b) moderate substance misuse risk and mild depression and anxiety, and (c) moderate substance misuse risk and moderate to high depression and anxiety. Structural models showed that effects of childhood sexual abuse were fully mediated by adolescent alcohol use and depression. Physical abuse increased adolescent depression but did not have direct or indirect effects on adult outcome classes. Emotional abuse had a direct effect on the adult classes.
Conclusions:
Children exposed to severe emotional abuse are at higher risk for comorbid substance misuse, depression, and anxiety into their mid-30s, after taking into account evidence of alcohol use and depression during adolescence. Sexual and physical abuse have more proximal effects on adolescent alcohol use and depression, which then influence the risk of adult problems.
It is well documented that the consequences of childhood maltreatment on problematic substance use and mental health problems extend into adulthood (Gilbert et al., 2009; Herrenkohl et al., 2013; Kim-Cohen et al., 2006). Although it is clear that childhood maltreatment is a risk factor for later mental and behavioral health problems, how this risk is conveyed across developmental time is under-studied. A number of theories have been posited to explain the impact of child maltreatment on later developmental outcomes. For example, Agnew’s strain theory suggests that the experience of being abused leads a child to develop negative emotions (e.g., anger, frustration, shame) that, in turn, lead to depression and/or self-medication in the form of alcohol or other drug use in adolescence (Carson et al., 2008). Cicchetti and colleagues (Cicchetti & Banny, 2014; Cicchetti et al., 2000) describe an ecological-transactional model in which maltreatment is a potent risk factor among many that can influence deviations from normal development. Risks and consequences have been posited to unfold over time— later outcomes are primarily influenced by earlier failure to accomplish the primary tasks of the previous developmental periods. The ecological-transactional model predicts that childhood maltreatment presents a risk for difficulties in meeting the challenges of adolescence, and that the failure to negotiate adolescence successfully then increases the risk of poor adult outcomes.
Adolescence, now considered a distinct and rather extended developmental period, fills the gap between childhood experiences and adult well-being. Previous research shows that child maltreatment, in particular, increases the risk for adolescent drinking (Tonmyr et al., 2010) and depression (Jaffee et al., 2002), and both are risk factors for adult mental health and substance misuse problems (Nikulina et al., 2012). These results suggest a model in which adolescent alcohol use and depressive symptoms mediate the relationship between childhood maltreatment and adult substance misuse and mental health problems. Until now, no strong longitudinal test of this trajectory has been conducted.
Research to date on the link between childhood maltreatment and adult substance misuse and mental health problems raises additional complicating factors. We use the term child maltreatment to represent all subtypes of abuse (sexual, physical, and emotional) and neglect, although it is understood that each is conceptually distinct and important in its own right as a predictor of child, adolescent, and adult functioning. Research on subtypes of abuse has shown that there is considerable overlap in the experiences that characterize the early lives of maltreated children (Wu et al., 2010), although there is also variability in how children are maltreated and in the consequences that follow (McGloin & Widom, 2001). Much of the research on childhood maltreatment, with some important exceptions, has either failed to distinguish between different forms of maltreatment or has focused on a single form of maltreatment without consideration of overlap with other types.
Subtypes of childhood maltreatment have been measured in a variety of ways. Measures depend to a certain extent on the goal of identifying instances of maltreatment and the technique used to make this determination. Self-reports by victims and/or parents (as perpetrators or observers of the child’s experience with all caregivers) and official child welfare and hospital records have been used. As Cicchetti and Toth (2005) point out, each measurement strategy has positive and negative qualities. Comparisons between maltreated and nonmaltreated children based on official records have the advantage of including only substantiated cases of maltreatment in a maltreated group. However, those considered nonmaltreated likely include some children who have been exposed to maltreatment but have not come to the attention of authorities. Reports by victims and parents can fill this gap, suggesting some advantage of using multiple sources to ascertain the most accurate picture of a child’s maltreatment experiences.
In the current study, we examined subtypes of maltreatment in ways that capture both their unique variance and predictive influence on adult substance misuse and mental health problems (Noll et al., 2003; Sugaya et al., 2012). Most of the research on mental health outcomes has focused on a particular problem (e.g., depression) or has examined a range of outcomes (e.g., mood disorder, anxiety, or substance misuse) in separate models as if independent of the others (Wu et al., 2010). Little attention has been paid to the complexity of mental health and the various patterns of comorbidity that are evidenced in the adult population. Although substance misuse, depression, and anxiety can occur in isolation, often they co-occur or overlap (Fergusson et al., 2011). Understanding how childhood maltreatment in its various forms leads to complex adult substance misuse and mental health problems could lead to better prevention and treatment of persistent adult disorders among those who were maltreated during childhood. We account for the complexity of mental health outcomes by using latent class analysis to predict class membership empirically derived from self-reports of symptoms of depression, anxiety, and substance misuse risk. Our primary question is whether adolescent alcohol use behavior and depressive symptoms account for the effects of sexual, physical, and emotional abuse on adult co-occurring substance misuse and mental health problems. To this end, we compare a model of direct effects of childhood maltreatment on adolescent and adult outcomes to a mediational model in which the influence of childhood maltreatment on classifications of comorbid adult substance misuse, depression, and anxiety is conveyed through adolescent alcohol use and depressive symptoms.
Method
Sample
Data are from the Lehigh Longitudinal Study, a prospective study of the causes and consequences of child maltreatment, which began in the 1970s with a sample of 457 children and their families (Herrenkohl et al., 1997). Study procedures were approved by the Office of Research and Sponsored Programs at Lehigh University and the Human Subjects Division at the University of Washington. In the original study design, about half of the families were recruited from child welfare agency abuse and neglect caseloads, and half were selected from childcare settings (i.e., Head Start, day care, and nursery programs) in the same two-county area (to serve as a comparison sample). Measures of child maltreatment were collected from all parents and children (see Measures section). The first “preschool” wave of the study took place in 1976–1977 when children were 18 months to 6 years old. A second “school-age” assessment was conducted in 1980–1982. In 1990–1992, a third “adolescent” assessment was conducted when participants were 18 years old, on average. Data were most recently collected in 2008–2010 from 357 of the original child participants (80% of those living), then in their mid-30s.
The original child sample was gender balanced: 248 (54%) males and 209 females. The racial and ethnic composition was relatively homogeneous but consistent overall with the makeup of the two-county area from which participants were selected: 80.7% (n = 369) White, 5.3% (n = 24) Black or African American, 1.3% (n = 6) American Indian/Alaska Native, 0.2% (n = 1) Native Hawaiian or Other Pacific Islander, and 11.2% (n = 51) more than one race. Some 7.2% (n = 33) self-identified as Hispanic or Latino, and 91.5% (n = 418) self-identified as not Hispanic or Latino. For a small percentage, 1.3% (n = 6), the race/ethnicity of the child was unknown. Eighty-six percent of children were from two-parent households. About 61% were in poverty according to the income-to-needs ratio in 1976 (www.census.gov/hhes/ www/poverty/data/threshld/thresh76.html).
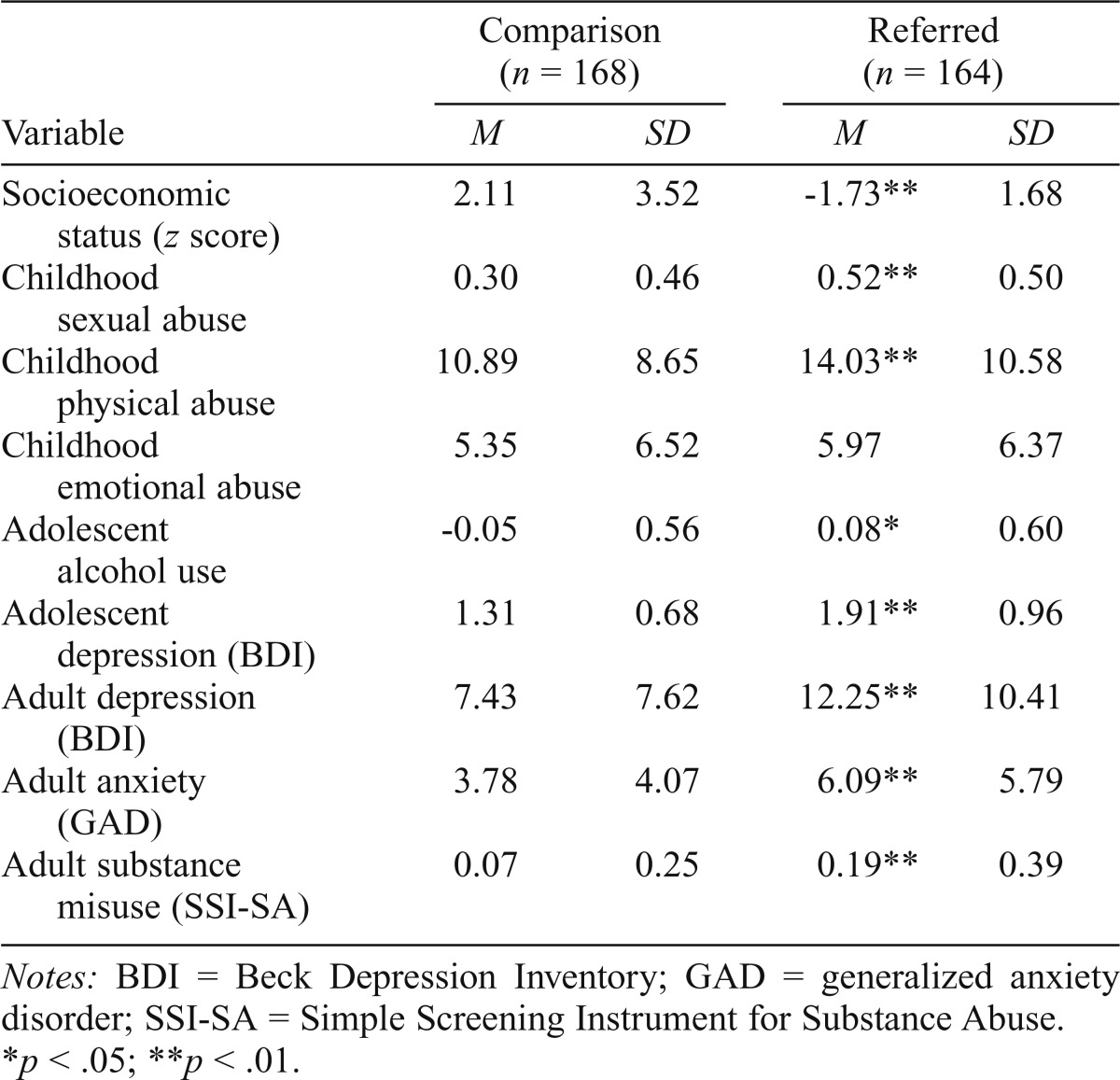
Cases were excluded from the analysis because of missing data on one of the predictors (covariates) included in the analysis. The sample for the mediation analysis (N = 332) remains balanced by gender (52.4% male) and recruitment sources (50% child welfare–referred). An analysis of the retained and full samples indicates no significant between-group differences in gender, age, recruitment, or childhood socioeconomic status. Descriptive information on the analysis sample is provided in Table 1. As expected, participants from the referred group were reported to have higher levels of childhood maltreatment (i.e., sexual and physical abuse); adolescent depression and alcohol use; and adult depression, anxiety, and risk of substance misuse.
Table 1.
Sample description by original recruitment from child welfare agency referral vs. comparison families
| Comparison (n = 168) |
Referred (n = 164) |
|||
| Variable | M | SD | M | SD |
| Socioeconomic status (z score) | 2.11 | 3.52 | -1.73** | 1.68 |
| Childhood sexual abuse | 0.30 | 0.46 | 0.52** | 0.50 |
| Childhood physical abuse | 10.89 | 8.65 | 14.03** | 10.58 |
| Childhood emotional abuse | 5.35 | 6.52 | 5.97 | 6.37 |
| Adolescent alcohol use | -0.05 | 0.56 | 0.08* | 0.60 |
| Adolescent depression (BDI) | 1 .31 | 0.68 | 1 .91** | 0.96 |
| Adult depression (BDI) | 7.43 | 7.62 | 12.25** | 10.41 |
| Adult anxiety (GAD) | 3.78 | 4.07 | 6.09** | 5.79 |
| Adult substance misuse (SSI-SA) | 0.07 | 0.25 | 0.19** | 0.39 |
Notes: BDI = Beck Depression Inventory; GAD = generalized anxiety disorder; SSI-SA = Simple Screening Instrument for Substance Abuse.
p < .05;
p < .01.
Measures
Childhood maltreatment measures: Physical, emotional, and sexual child abuse.
Three types of childhood maltreatment experiences were measured for all study participants regardless of child welfare involvement: physical, emotional, and sexual abuse. These measures are derived from different sources (i.e., prospective parental report and retrospective self-report) and are not mutually exclusive; as such each captures some unique aspect of maltreatment. Some children experienced only one form, whereas others experienced multiple forms.
Questions asked of parents focused on their and other caregivers’ use of physically (12 items) and emotionally (7 items) abusive disciplining strategies. These items are defined as abuse in this study based on severity rating by a group of 41 child welfare workers on a 5-point scale (5 = abusive, 4 = severely punishing, 3 = mildly punishing, 2 = mildly rewarding, 1 = highly rewarding). The abuse items included in this study were all rated as severely punishing to abusive (4 or 5). Examples of physically abusive practices included hit with a stick or paddle; hit with a strap, rope, or belt; slap/spank to bruise; hit/paddle to bruise; and burn. Examples of emotional abuse items included taking away meals, threatening to send child away, isolating in a dark room, and locking out of the house. Abuse data were collected in the preschool and school-age waves of the study with the same items across time. In the preschool wave, parents were asked about their and other caregivers’ physical disciplining practices (a) in the last 3 months and (b) before the last 3 months, whereas emotional disciplining practices were measured for the last 3 months only. At the school-age wave of the study, parents were asked about physical and emotional disciplining over the past year. Scores were computed for each assessment, combining data about mothers, fathers, and other caregivers, and then averaged across assessments.
Questions regarding child sexual abuse were not included in the preschool or school-age assessments. Two relevant questions were asked of youth participants in the adolescent assessment: “How many times has someone pressured or pushed you to do sexual things you didn’t want to do?” and “How many times have you been sexually attacked or raped or an attempt made to do so?” In addition, some adolescents were asked directly whether they had been sexually abused. Unfortunately, only after several of the adolescent interviews had been conducted did it become evident this additional question on sexual abuse was needed. To gather a more complete picture of sexual abuse, the research team used multiple sources to identify the presence of sexual abuse, including interview notes, case records, responses to the physical and emotional abuse and neglect questions where some individuals identified sexual abuse, and adult retrospective reports of childhood sexual abuse. In total, 126 people reported sexual abuse in one or more of these sources. As expected, women were approximately twice as likely as men to report experiencing sexual abuse (55.2% vs. 30.3%, respectively), χ2(1) = 24.99, p < .001.
Adult substance misuse and mental health.
The Simple Screening Instrument for Substance Abuse (SSI-SA; Winters & Zenilman, 1994) was used to assess substance misuse risk. The SSI-SA is composed of 16 items and covers substance consumption, preoccupation and loss of control related to substance use, adverse consequences, problem recognition (making a link between one’s use of substances and the problems that result), and tolerance and withdrawal. Responses are yes/no, with affirmative responses scored 1 and nonaffirmative scored 0. Fourteen items were summed (providing a range of 0–14). Overall, 13% of the sample scored 4 or higher, which is the cutoff for moderate to high risk for substance misuse (Peters et al., 2000); 10% were in the 4–9 range, and 2.8% were in the 10–14 range. The score was dichotomized such that a score of 4 or more was coded 1, indicating moderate to high risk of substance misuse, and all others scored 0. Depression was assessed using the Beck Depression Inventory (BDI; Beck et al., 1988). The BDI is a widely used measure of depression that has been used with various populations (Lopez et al., 2013; Whisman et al., 2013). Standard cutoffs for interpreting results are as follows: 0–13 = minimal depression, 14–19 = mild depression, 20–28 = moderate depression, 29–63 = severe depression. Generalized anxiety disorder (GAD) was assessed using the GAD-7 (Spitzer et al., 2006). The GAD-7 is brief seven-item self-report measure commonly used as a screener, but which recently has been demonstrated to be more accurate as a measure of severity (Beard & Björgvinsson, 2014), with overall good reliability and validity. Scores of 8 and above are considered severe enough to provisionally diagnose GAD.
Adolescent mediators.
The adolescent BDI depression score is the sum of 0 to 3 item responses over 21 items. A high score indicates more depression (Cronbach’s α = .83). This sum was then coded into five categories 0 = 0 (none), 1 = 1–9 (very low), 2 = 10–18 (mild), 3 = 19–29 (moderate), 4 = 30–43 (severe). Adolescent alcohol use behavior is a scale composed of six single items and a severity index of problems attributable to alcohol use from the adolescent interview. Items assessed recent and past frequency of drinking and drunkenness (e.g., “How often have you drunk alcoholic beverages?” “How often did you get drunk in high school?”). Each item was standardized to a mean of 0 and standard deviation of 1 (because of nonequivalence in the scaling of the original items) and averaged (Cronbach’s α = .64).
Covariates
Socioeconomic status is based on mother’s educational level, occupation, total rooms in the family home, and family income at the preschool assessment that was then standardized, resulting in a score with M = 0 and SD = 3.2. Gender is coded 1 = female and 2 = male based on parental report on the preschool interview. Age at the adolescent interview is calculated from date of birth and date of interview administration (M = 18.16 years, SD = 1.80).
Analyses
Analyses were conducted in three phases. In Phase 1, latent class analysis with maximum likelihood estimation and robust standard errors was used to assess empirically based classes of participants based on adult risk of substance misuse and severity of depression and anxiety symptoms. All participants with data from the adult survey were included (n = 356, gender and recruitment status balanced). The models estimating one to four classes were compared on the Bayesian Information Criterion, and a model was selected based on magnitude of improvement in fit with each additional class. Phase 2 introduced measures of childhood maltreatment, adolescent alcohol use, and depression, and control variables as predictors of class membership based on estimated posterior probabilities in structural equation models. In Phase 3, we used structural equation models to estimate mediational paths from childhood maltreatment to adolescent alcohol use and depression to adult comorbid substance misuse and mental health latent classes, controlling for age, gender, race, and childhood family socioeconomic status. In the second and third phases the analysis sample was reduced to 332 because of missing data.
Results
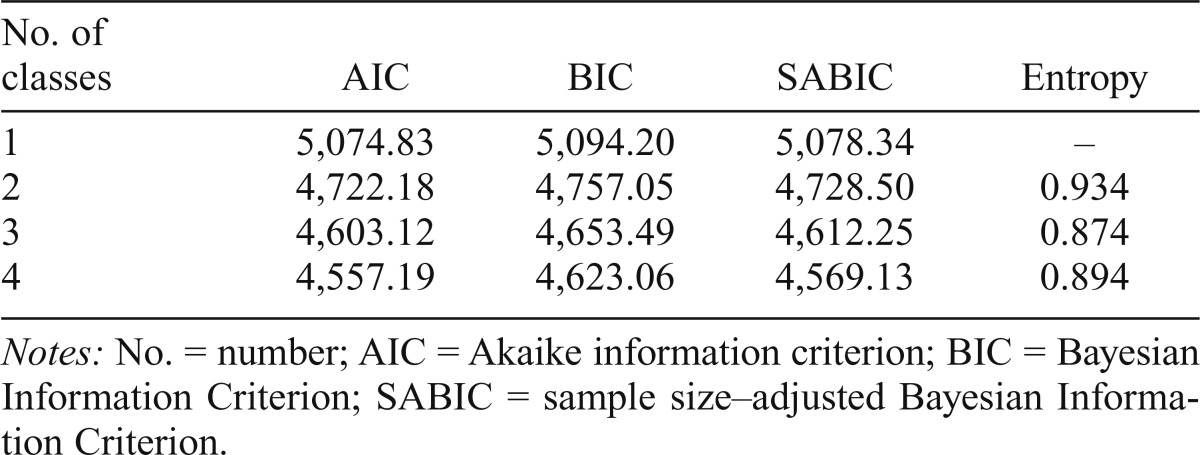
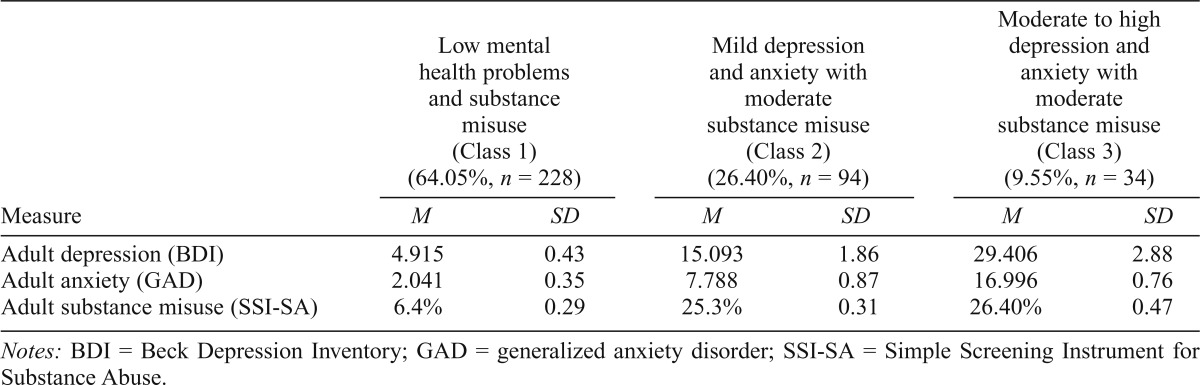
Estimation of a series of latent class models with one to four classes was conducted (n = 356). Although the four-class model showed some indication of improved fit over three classes (Table 2), we selected the three-class model for parsimony and to avoid classes with very small membership (less than 20 cases). Based on the most likely latent class membership, the largest class (Class 1, n = 228) is characterized by a low likelihood of substance misuse and very low depression and anxiety symptoms (Table 3). The second largest class (Class 2, n = 94) is characterized by moderate likelihood of substance misuse and mild depression and anxiety symptoms. The smallest class (Class 3, n = 34) is characterized by a moderate likelihood of substance misuse (similar to Class 2) with moderate to high depression and anxiety symptoms.
Table 2.
Fit statistics for latent class models for one to four classes
| No. of classes | AIC | BIC | SABIC | Entropy |
| 1 | 5,074.83 | 5,094.20 | 5,078.34 | – |
| 2 | 4,722.18 | 4,757.05 | 4,728.50 | 0.934 |
| 3 | 4,603.12 | 4,653.49 | 4,612.25 | 0.874 |
| 4 | 4,557.19 | 4,623.06 | 4,569.13 | 0.894 |
Notes: No. = number; AIC = Akaike information criterion; BIC = Bayesian Information Criterion; SABIC = sample size–adjusted Bayesian Information Criterion.
Table 3.
Estimated means and standard errors by class
| Low mental health problems and substance misuse (Class 1) (64.05%, n = 228) |
Mild depression and anxiety with moderate substance misuse (Class 2) (26.40%, n = 94) |
Moderate to high depression and anxiety with moderate substance misuse (Class 3) (9.55%, n = 34) |
||||
| Measure | M | SD | M | SD | M | SD |
| Adult depression (BDI) | 4.915 | 0.43 | 15.093 | 1.86 | 29.406 | 2.88 |
| Adult anxiety (GAD) | 2.041 | 0.35 | 7.788 | 0.87 | 16.996 | 0.76 |
| Adult substance misuse (SSI-SA) | 6.4% | 0.29 | 25.3% | 0.31 | 26.40% | 0.47 |
Notes: BDI = Beck Depression Inventory; GAD = generalized anxiety disorder; SSI-SA = Simple Screening Instrument for Substance Abuse.
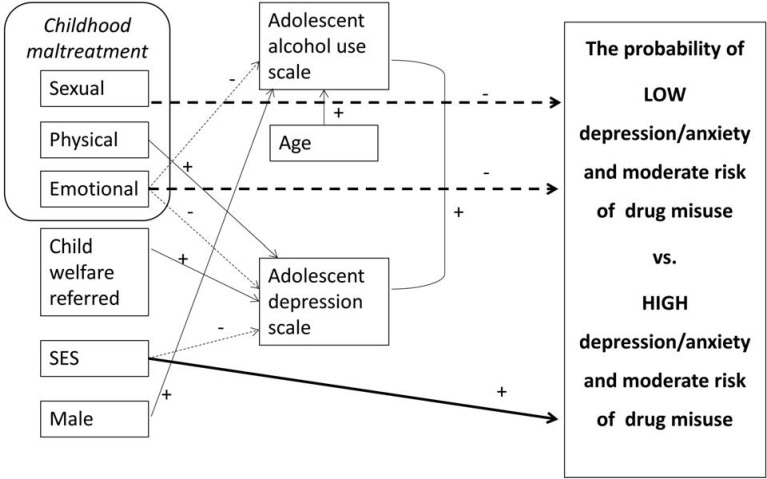
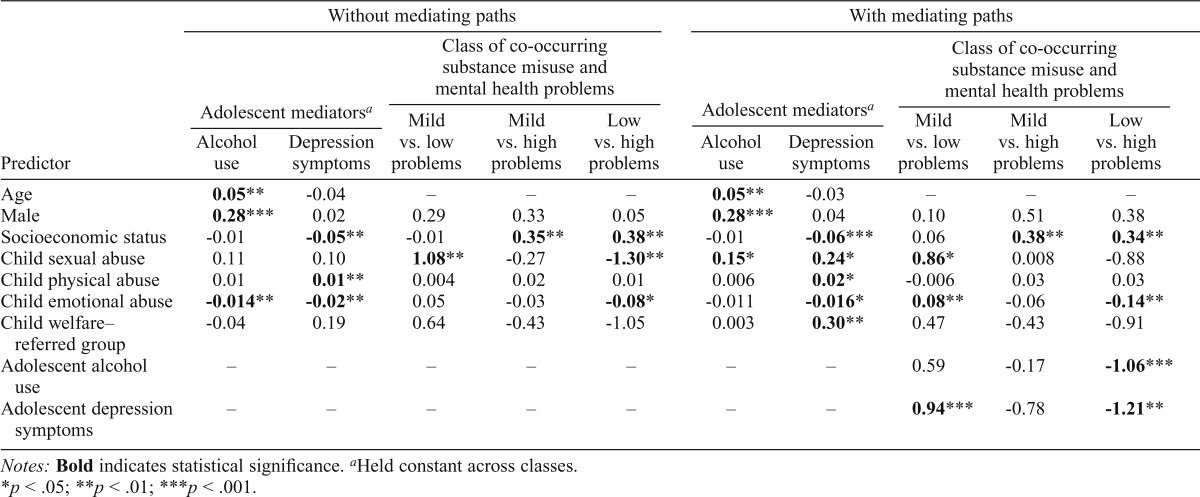
Figure 1 illustrates the direction and significance of direct paths from child maltreatment variables to adolescent and adult outcomes. Parameter estimates are provided in Table 4. As expected, physical abuse relates to higher depression scores in adolescence. However, emotional abuse is associated with lower adolescent depression symptoms and lower adolescent alcohol use scores. Sexual abuse does not significantly predict either adolescent alcohol use or depression symptoms.
Figure 1.
Direct effects of child maltreatment on adolescent and adult outcomes comparing LOW to HIGH problem. Solid arrows indicate positive relationships and dashed arrows indicate negative relationships. SES = socioeconomic status.
Table 4.
Path coefficients for effects of childhood maltreatment on adolescent mediators and adult classification based on latent class analysis without and with mediating paths
| Predictor | Without mediating paths |
With mediating paths |
||||||||
| Adolescent mediatorsa |
Class of co-occurring substance misuse and mental health problems |
Adolescent mediatorsa |
Class of co-occurring substance misuse and mental health problems |
|||||||
| Alcohol use | Depression symptoms | Mild vs. low problems | Mild vs. high problems | Low vs. high problems | Alcohol use | Depression symptoms | Mild vs. low problems | Mild vs. high problems | Low vs. high problems | |
| Age | 0.05** | -0.04 | – | – | – | 0.05** | -0.03 | – | – | – |
| Male | 0.28*** | 0.02 | 0.29 | 0.33 | 0.05 | 0.28*** | 0.04 | 0.10 | 0.51 | 0.38 |
| Socioeconomic status | -0.01 | -0.05** | -0.01 | 0.35** | 0.38** | -0.01 | -0.06*** | 0.06 | 0.38** | 0.34** |
| Child sexual abuse | 0.11 | 0.10 | 1.08** | -0.27 | -1.30** | 0.15* | 0.24* | 0.86* | 0.008 | -0.88 |
| Child physical abuse | 0.01 | 0.01** | 0.004 | 0.02 | 0.01 | 0.006 | 0.02* | -0.006 | 0.03 | 0.03 |
| Child emotional abuse | -0.014** | -0.02** | 0.05 | -0.03 | -0.08* | -0.011 | -0.016* | 0.08** | -0.06 | -0.14** |
| Child welfare–referred group | -0.04 | 0.19 | 0.64 | -0.43 | -1.05 | 0.003 | 0.30** | 0.47 | -0.43 | -0.91 |
| Adolescent alcohol use | – | – | – | – | – | – | – | 0.59 | -0.17 | -1.06*** |
| Adolescent depression symptoms | – | – | – | – | – | – | – | 0.94*** | -0.78 | -1.21** |
Notes: Bold indicates statistical significance.
Held constant across classes.
p < .05;
p < .01;
p < .001.
Two of the three maltreatment measures—sexual and emotional abuse—predict adult substance misuse and mental health class membership. Sexual and emotional abuse, but not physical abuse, are associated with being in the high problem group (i.e., a higher likelihood of being in the high vs. the low problem class; odds ratio [OR] = 3.56 and 1.07, respectively). Sexual abuse also increases the likelihood of mild versus low problem class membership (OR = 2.93). No other associations were found between maltreatment measures and subsequent adult substance misuse and mental health classes in the direct-effects-only model.
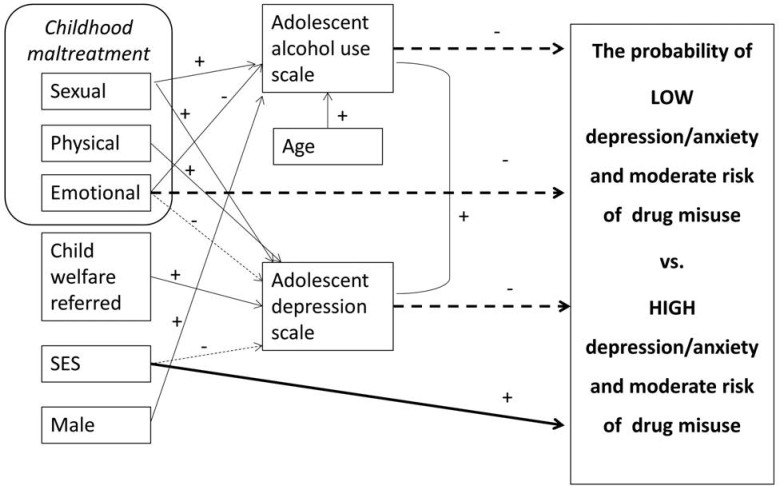
When mediating paths are included (Figure 2), the direct effect of emotional abuse on adult substance misuse and mental health class persists, reducing the likelihood of low versus high substance use and mental health problem class membership (OR = 0.82), as well as increasing the likelihood of mild versus low problem class membership (OR = 1.08). However, the effect of sexual abuse on adult problem class membership appears to be mediated through adolescent alcohol use and depression. Sexual abuse significantly increases adolescent alcohol use and depression (β = 0.15 and 0.24, respectively), which, in turn, reduces the likelihood of being in the low versus the high problem class (OR = 0.30 and 0.35, respectively). Tests of the indirect paths approached significance (sexual abuse to depression to adult classes: β = -.16, p = .07; sexual abuse to adolescent drinking to adult classes: β = -.17, p = .10). Physical abuse significantly increases adolescent depressive symptoms, but neither sexual abuse nor physical abuse significantly predicts adult substance misuse and mental health problem classes directly.
Figure 2.
Mediated effects of child maltreatment through adolescent alcohol use and depression on adult outcomes comparing LOW to HIGH problem groups. Solid arrows indicate positive relationships and dashed arrows indicate negative relationships. SES = socioeconomic status.
Discussion
Several gaps remain in our understanding of how various forms of child maltreatment influence later development over time. We address three issues in this study. First, we use sources of information that are particularly suited to each subtype of maltreatment: parental report of emotional and physical abuse and self-report (victim) of sexual abuse. Second, previous studies of maltreatment and substance misuse have either not addressed other common mental health problems (depression and anxiety) or have examined each outcome separately without considering the likely overlap of these conditions with substance misuse. We used measures of substance misuse risk as well as depression and anxiety symptoms to identify groups of participants with unique patterns across outcomes and discovered that moderate to high risk of substance misuse co-occurs, with some evidence of mild to moderate depression and anxiety being present more often than not. However, the small class of individuals with more severe mental health problems was not more likely to be at elevated risk for substance misuse than those with milder symptoms. Third, very little longitudinal research has been conducted to examine the developmental mediators that link childhood maltreatment to adult substance misuse and mental health outcomes. We tested a model in which adolescent drinking and depressive symptoms temporally and developmentally bridge the gap between child maltreatment and the adult outcomes of interest. We found that both adolescent drinking and depression significantly increased the likelihood of being in the group characterized by moderate substance misuse risk and more severe depression and anxiety compared with the group with low problems. Further, we found that adolescent depression also increased the odds of being in the group with moderate risk for substance misuse and milder symptoms of depression and anxiety compared with the low problem group. None of the predictors of interest distinguish moderate risk for substance misuse with mild depression and anxiety from moderate risk for substance misuse with severe depression and anxiety.
A number of interesting findings emerged related to the subtypes of maltreatment. We found that the impact of emotional abuse reported by parents is not mediated through adolescent alcohol use or depression as hypothesized. It may be that the impact of emotional abuse is mediated through other forms of internalizing or externalizing problems. Anxiety in adolescence, rather than depression, seems a likely candidate because anxiety is part of the pattern of problem outcomes. This would be consistent with our finding that parent-reported childhood emotional abuse was negatively associated with adolescent depression and alcohol use. It is plausible that anxiety-driven hyperdiligence during childhood and adolescence (as a result of emotional abuse) could lead to emotional exhaustion, resulting in depression, anxiety, and self-medicating with substances by the mid-30s.
A second alternative pathway might be through adolescent externalizing behaviors such as aggression or delinquency. Previously published results from this study have found childhood emotional abuse, in particular, to be significantly associated with adolescent externalizing behaviors (Jung et al., 2015). Last, it is possible that the direct effect of emotional abuse on adult co-occurring mental health and substance misuse problems is attributable to continued victimization into adulthood. Early abuse increases the risk of later abuse (Messman & Long, 1996; Messman-Moore & Long, 2000) within the same relationships or in new ones. Those subjected to severe emotional abuse in childhood may be particularly inclined to remain in adult relationships that also include harsh, explosive, or arbitrary emotional conflict (Reyome, 2010; Zurbriggen et al., 2010). If this is the case, the elevated risk of substance misuse and mental health problems in adulthood may be influenced more by recent, concurrent, and ongoing relationship problems than by the original experiences of abuse as a child.
Unlike parental report of emotional abuse, the impact of sexual abuse appears to be at least partially mediated through two distinct paths: adolescent alcohol use and depressive symptoms. By including both in the model, we see that each pathway makes a unique contribution to later comorbid substance misuse and mental health problems. This finding is consistent with the ecological-transactional model (Cicchetti & Banny, 2014) in which later developmental outcomes are heavily influenced by the successful or unsuccessful completion of earlier developmental tasks. These results suggest that successful prevention or treatment of adolescent alcohol use and depressive symptoms could mitigate the impact of sexual abuse on adult substance misuse and mental health problems. However, some caution is called for when interpreting etiological findings in terms of prevention. Our findings support the hypothesis that the observed relationship between sexual abuse and co-occurring adult substance misuse and mental health problems is explained by the measured mediators, but it is possible that if these particular mediators were eliminated, other mechanisms would come into play. In other words, victims of childhood sexual abuse who avoid adolescent alcohol use and depression are not necessarily saved from the negative consequences of sexual abuse on adult substance misuse and mental health.
Childhood physical abuse had no direct effect on co-occurring adult substance misuse and mental health problems. The absence of a direct or total effect on co-occurring adult substance misuse and mental health problems suggests a probabilistic chain of events. Physical abuse seems primarily to lead to more proximal elevated depression symptoms, perhaps as a result of anger, frustration, and shame, as suggested by the general strain model (Carson et al., 2008; Hollist et al., 2009). One possible interpretation is that if teens who have experienced these types of maltreatment manage to navigate adolescence without developing elevated depressive symptoms, the risk to their adult adjustment is minimized.
Despite the many strengths of this study, there are some limitations. Neglect is a form of maltreatment that is difficult to quantify and is not measured separately in our analyses. It is likely that neglect occurred, particularly among the child welfare agency–referred families. It is therefore possible that the significant positive relationship between being a referred case and adolescent depression (after controlling for the other forms of abuse) reflects the effects of neglect. Measuring different forms of childhood maltreatment requires using different sources of data. Although different sources are appropriate, using them also introduces some source-related error. In this study, the measures of physical and emotional abuse are subject to bias introduced by parents reporting on their own and other’s behavior (one parent reporting on the abusive actions of other caregivers), which could result in underreporting of severe discipline practices. There is also bias in the measure of sexual abuse introduced by victim perceptions, which can change over time.
In addition, our measure of sexual abuse is primarily retrospective self-report from the adolescent survey conducted at the same time that the measures of adolescent depression and drinking were collected, and therefore sexual abuse reported then can be assumed to have occurred earlier. Some cases were based on retrospective reports of sexual abuse occurring before age 18 but not reported until the adult survey. It is possible that in a very few of those cases the sexual abuse that occurred before age 18 actually occurred after the adolescent measures were taken. Although the full range of depression and anxiety was represented in the sample, elevated risk of substance misuse was present in only 13% and extreme risk in only 2.8%. This distribution and our decision to dichotomize the SSI-SA measure necessarily influenced the results of the latent class analysis. It will be important to know if qualitatively different classes emerge in larger samples with a more fine-tuned measure of adult substance misuse in conjunction with standard measures of depression and anxiety. The generalizability of these findings is also limited by the homogeneity of the sample with regard to race and family structure.
Conclusions
This study demonstrates already established links between childhood maltreatment and adult substance misuse, depression, and anxiety. In addition, we found that moderate to high risk of substance misuse co-occurred with varying levels of anxiety and depression, but we did not identify a class of participants with only adult substance misuse. As we suspected, the relationships between child maltreatment and adult substance and mental health problems were different for different subtypes of maltreatment, and the mediational paths were also different.
Our findings highlight the importance of prevention for those who have early maltreatment experiences, while at the same time giving consideration to the different types of abuse. For example, for those who were sexually abused, the most effective prevention strategies might be secondary prevention (directed at those with elevated risk for a poor outcome), which focuses on the developmental mediators— depression and alcohol use—during adolescence in particular. However, for those who were emotionally abused, it may be essential to respond with tailored interventions that can reduce the possibility of continued victimization throughout developmental stages from adolescence into adulthood. Teens with a history of emotional abuse may seem to be doing quite well, but the negative impact of their earlier abuse is still to come, and it is likely to be complicated by depression and anxiety that is not yet evident. Further research is needed to understand the development of substance misuse among victims of childhood emotional abuse to find the best strategies for prevention of future substance misuse.
Footnotes
This work was supported by National Institute on Drug Abuse Grant No. R01DA032950 and Grant No. R01HD049767 from the National Institute on Child Health and Human Development and the Office of Behavioral and Social Sciences Research. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
References
- Beard C., Björgvinsson T. Beyond generalized anxiety disorder: Psychometric properties of the GAD-7 in a heterogeneous psychiatric sample. Journal of Anxiety Disorders. 2014;28:547–552. doi: 10.1016/j.janxdis.2014.06.002. doi:10.1016/j.janxdis.2014.06.002. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A., Carbin M. G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. doi:10.1016/0272-7358(88)90050-5. [Google Scholar]
- Carson D. C., Sullivan C. J., Cochran J. K., Lersch K. M. General strain theory and the relationship between early victimization and drug use. Deviant Behavior. 2008;30:54–88. doi:10.1080/01639620802050023. [Google Scholar]
- Cicchetti D., Banny A. A developmental psychopathology perspective on child maltreatment. In: Lewis M., Rudolph K. D., editors. Handbook of developmental psychopathology. New York, NY: Springer Science+Business Media; 2014. pp. 723–741. [Google Scholar]
- Cicchetti D., Toth S. L. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. doi:10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Cicchetti D., Toth S. L., Rogosch F. A. The development of psychological wellness in maltreated children. In: Cicchetti D., Rappaport J., Sandler I., Weissberg R. P., editors. The promotion of wellness in children and adolescents. Washington, DC: Child Welfare League of America; 2000. pp. 395–426. [Google Scholar]
- Fergusson D. M., Boden J. M., Horwood L. J. Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Social Psychiatry and Psychiatric Epidemiology. 2011;46:933–942. doi: 10.1007/s00127-010-0268-1. doi:10.1007/s00127-010-0268-1. [DOI] [PubMed] [Google Scholar]
- Gilbert R., Widom C. S., Browne K., Fergusson D., Webb E., Janson S. Burden and consequences of child maltreatment in high-income countries. The Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. doi:10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Herrenkohl R. C., Egolf B. P., Herrenkohl E. C. Preschool antecedents of adolescent assaultive behavior: A longitudinal study. American Journal of Orthopsychiatry. 1997;67:422–432. doi: 10.1037/h0080244. doi:10.1037/h0080244. [DOI] [PubMed] [Google Scholar]
- Herrenkohl T. I., Hong S., Klika J. B., Herrenkohl R. C., Russo M. J. Developmental impacts of child abuse and neglect related to adult mental health, substance use, and physical health. Journal of Family Violence. 2013;28:191–199. doi: 10.1007/s10896-012-9474-9. doi:10.1007/s10896-012-9474-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollist D. R., Hughes L. A., Schaible L. M. Adolescent maltreatment, negative emotion, and delinquency: An assessment of general strain theory and family-based strain. Journal of Criminal Justice. 2009;37:379–387. doi:10.1016/j.jcrimjus.2009.06.005. [Google Scholar]
- Jaffee S. R., Moffitt T. E., Caspi A., Fombonne E., Poulton R., Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;59:215–222. doi: 10.1001/archpsyc.59.3.215. doi:10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Jung H., Herrenkohl T. I., Lee J. O., Klika J. B., Skinner M. L. Effects of physical and emotional child abuse and its chronicity on crime into adulthood. Violence and Victims. 2015;30:1004–1018. doi: 10.1891/0886-6708.VV-D-14-00071. doi:10.1891/0886-6708.VV-D-14-00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J., Caspi A., Taylor A., Williams B., Newcombe R., Craig I. W., Moffitt T. E. MAOA, maltreatment, and gene-environment interaction predicting children’s mental health: New evidence and a meta-analysis. Molecular Psychiatry. 2006;11:903–913. doi: 10.1038/sj.mp.4001851. doi:10.1038/sj.mp.4001851. [DOI] [PubMed] [Google Scholar]
- Lopez M. N., Pierce R. S., Gardner R. D., Hanson R. W. Standardized Beck Depression Inventory-II scores for male veterans coping with chronic pain. Psychological Services. 2013;10:257–263. doi: 10.1037/a0027920. doi:10.1037/a0027920. [DOI] [PubMed] [Google Scholar]
- McGloin J. M., Widom C. S. Resilience among abused and neglected children grown up. Development and Psychopathology. 2001;13:1021–1038. doi: 10.1017/s095457940100414x. doi:10.1017/S095457940100414X. [DOI] [PubMed] [Google Scholar]
- Messman T. L., Long P. J. Child sexual abuse and its relationship to revictimization in adult women: A review. Clinical Psychology Review. 1996;16:397–420. doi:10.1016/0272-7358(96)00019-0. [Google Scholar]
- Messman-Moore T. L., Long P. J. Child sexual abuse and revictimization in the form of adult sexual abuse, adult physical abuse, and adult psychological maltreatment. Journal of Interpersonal Violence. 2000;15:489–502. doi:10.1177/088626000015005003. [Google Scholar]
- Nikulina V., Widom C. S., Brzustowicz L. M. Child abuse and neglect, MAOA, and mental health outcomes: A prospective examination. Biological Psychiatry. 2012;71:350–357. doi: 10.1016/j.biopsych.2011.09.008. doi:10.1016/j.biopsych.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noll J. G., Horowitz L. A., Bonanno G. A., Trickett P. K., Putnam F. W. Revictimization and self-harm in females who experienced childhood sexual abuse: Results from a prospective study. Journal of Interpersonal Violence. 2003;18:1452–1471. doi: 10.1177/0886260503258035. doi:10.1177/0886260503258035. [DOI] [PubMed] [Google Scholar]
- Peters R. H., Greenbaum P. E., Steinberg M. L., Carter C. R., Ortiz M. M., Fry B. C., Valle S. K. Effectiveness of screening instruments in detecting substance use disorders among prisoners. Journal of Substance Abuse Treatment. 2000;18:349–358. doi: 10.1016/s0740-5472(99)00081-1. doi:10.1016/S0740-5472(99)00081-1. [DOI] [PubMed] [Google Scholar]
- Reyome N. D. Childhood emotional maltreatment and later intimate relationships: Themes from the empirical literature. Journal of Aggression, Maltreatment & Trauma. 2010;19:224–242. doi:10.1080/10926770903539664. [Google Scholar]
- Spitzer R. L., Kroenke K., Williams J. B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. doi:10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sugaya L., Hasin D. S., Olfson M., Lin K.-H., Grant B. F., Blanco C. Child physical abuse and adult mental health: A national study. Journal of Traumatic Stress. 2012;25:384–392. doi: 10.1002/jts.21719. doi:10.1002/jts.21719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonmyr L., Thornton T., Draca J., Wekerle C. A review of childhood maltreatment and adolescent substance use relationship. Current Psychiatry Reviews. 2010;6:223–234. doi:10.2174/157340010791792581. [Google Scholar]
- Whisman M. A., Judd C. M., Whiteford N. T., Gelhorn H. L. Measurement invariance of the Beck Depression Inventory-Second Edition (BDI-II) across gender, race, and ethnicity in college students. Assessment. 2013;20:419–428. doi: 10.1177/1073191112460273. doi:10.1177/1073191112460273. [DOI] [PubMed] [Google Scholar]
- Winters K., Zenilman J. Simple Screening Instrument for Outreach for Alcohol and Other Drug Abuse and Infectious Diseases (Vol. 11, Publication No. (SMA) 02-3683) Rockville, MD: Center for Substance Abuse Treatment: U.S. Department of Health and Human Services (SAMHSA); 1994. [Google Scholar]
- Wu N. S., Schairer L. C., Dellor E., Grella C. Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders. Addictive Behaviors. 2010;35:68–71. doi: 10.1016/j.addbeh.2009.09.003. doi:10.1016/j.addbeh.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurbriggen E. L., Gobin R. L., Freyd J. J. Childhood emotional abuse predicts late adolescent sexual aggression perpetration and victimization. Journal of Aggression, Maltreatment & Trauma. 2010;19:204–223. doi:10.1080/10926770903539631. [Google Scholar]