Abstract
Purpose
Suicide is one of the leading causes of maternal mortality in many countries, but little is known about the epidemiology of suicide and suicidal behavior among pregnant women in the US. We sought to examine trends and provide nationally representative estimates for suicidal behavior (including suicidal ideation, and suicide and self-inflicted injury) among pregnant women from 2006 to 2012 in the US.
Methods
Pregnant women aged 12-55 years were identified through pregnancy- and delivery-related hospitalization records from the National (Nationwide) Inpatient Sample. Suicidal behavior was identified by the International Classification of Diseases, Ninth Revision, Clinical Modification codes. Annual, nationwide estimates and trends were determined using discharge and hospital weights.
Results
The prevalence of suicidal ideation more than doubled from 2006 to 2012 (47.5 to 115.0 per 100,000 pregnancy- and delivery-related hospitalizations), whereas the prevalence of suicide and self-inflicted injury remained stable. Nearly 10% of suicidal behavior occurred in the 12-18-year group, showing the highest prevalence per 100,000 pregnancy- and delivery-related hospitalizations (158.8 in 2006 and 308.7 in 2012) over the study period. For suicidal ideation, blacks had higher prevalence than whites; women in the lowest income quartile had the highest prevalence. Although the prevalence of suicidal behavior was higher among hospitalizations with depression diagnoses, more than 30% of hospitalizations were for suicidal behavior without depression diagnoses.
Conclusions
Our findings highlight the increasing burden and racial differences in suicidal ideation among US pregnant women. Targeted suicide prevention efforts are needed for high-risk pregnant women including teens, blacks, and low-income women.
Keywords: suicidal ideation, suicide and self-inflicted injury, pregnant women, National (Nationwide) Inpatient Sample
Introduction
Prior studies have neglected the issue of suicide and suicidal behavior during pregnancy because pregnancy and childbirth have been historically described as a time of emotional wellbeing, and motherhood, in itself, as protective against suicide and suicidal behavior (Appleby 1991; Gissler et al. 1996; Kendell 1991; Marzuk et al. 1997; Nock et al. 2012). However, several recent studies have suggested that suicide is one of the leading causes of maternal mortality in countries including Australia, Sri Lanka, India, Bangladesh, and the UK (Agampodi et al. 2014; Asad et al. 2010; Austin and Kildea 2007; Chang et al. 2005; Cockburn and Pawson 2007; Fuhr et al. 2014; Gavin et al. 2011a; Lindahl et al. 2005; Oates 2003; Shadigian and Bauer 2005; Yusuf et al. 2007). Little is known about the epidemiology of suicide and suicidal behavior among pregnant women in the US (Gold et al. 2012; Lindahl et al. 2005). Pregnancy is the period when women have frequent interaction with the health care system, presenting a valuable opportunity for healthcare providers to intervene promptly if the epidemiology of suicide was better understood (Gold et al. 2012). Unfortunately, efforts to study suicidal behavior in pregnancy have been hampered by social stigma and methodological constraints including limited data sources capturing pregnancy and delivery status of patients with suicidal behavior (Frautschi et al. 1994; Gissler et al. 1996; Gold et al. 2012; Lindahl et al. 2005; Phillips 2014).
Suicidal ideation significantly predicts suicide attempt, and suicide attempt is the greatest risk factor for completed suicide (Doshi et al. 2005; Kessler et al. 2005; Nock et al. 2012). Therefore, studying suicidal behavior is crucial for identifying women at the highest risk of suicide; and doing so will facilitate the development of tailored interventions (Doshi et al. 2005; Scott et al. 2015). Additionally, the prevention of suicidal ideation and suicide attempt may lead to significant reductions in maternal morbidity and mortality (Doshi et al. 2005). Moreover, studying suicidal behavior among pregnant women is particularly important because the potential for harm will not only threaten the pregnancy but also seriously compromise the future development of infants (Gentile 2011; Huang et al. 2012; Lindahl et al. 2005). Women who have attempted suicide during pregnancy have higher rates of fetal loss, premature labor, and cesarean delivery (Czeizel 2011; Czeizel et al. 1997; Gandhi et al. 2006). Suicidal ideation during pregnancy is associated with inadequate mother-infant interaction (Gavin et al. 2011; Paris et al. 2009); and infants of mothers who have attempted suicide during pregnancy are more likely to experience respiratory distress syndrome (Gandhi et al. 2006).
We sought to examine trends and provide nationally representative estimates for the prevalence of suicidal ideation, and suicide and self-inflicted injury among pregnant women in the US using the largest all-payer inpatient care database, the National (Nationwide) Inpatient Sample (NIS). We examined trends from 2006-2012 for women overall and stratified by age, race, income, and depression.
Methods
Database
As a part of the Healthcare Cost and Utilization Project (HCUP), the NIS is an administrative database of hospital inpatient stays derived from billing data across the US (HCUP 2015a; HCUP 2015b). All HCUP-participating hospitals are included in the sampling frame. Five hospital characteristics — geographic region, ownership, location, teaching status, and bed size — are used for stratification (HCUP 2015a; HCUP 2015b). Prior to 2012, within each stratum, a 20% stratified random sample of hospitals in the sampling frame was drawn (HCUP 2015b). All discharges from sampled hospitals were included. Beginning with 2012, the NIS was redesigned to improve national estimates, and within each stratum, a 20% stratified random sample of discharges from all HCUP-participating hospitals was drawn (HCUP 2015a; HCUP 2015c). Since the data are publicly available and do not contain personal identifiers, this study is exempt from review by institutional review boards.
Study population
We included all pregnancy- and delivery-related hospitalizations identified in the 2006-2012 NIS. Among women aged 12-55 years, the identification of pregnancy- and delivery-related hospitalizations were predicated upon pregnancy- and delivery-related International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes and Diagnosis-Related Group (DRG) codes (Bryant et al. 2012; Hornbrook et al. 2007; Kuklina et al. 2008) (eTable 1).
Variable specification
We included suicidal ideation (thoughts of engaging in behaviors intended to end one’s life) (Nock et al. 2012) and suicide and self-inflicted injury (injuries in suicide, suicide attempt, and self-inflicted injuries specified as intentional) (WHO and PMIC 1998). ICD-9-CM diagnosis codes were used to identify hospitalizations with suicidal ideation (V62.84) and suicide and self-inflicted injury (E950-959). Since diagnosis code for suicidal ideation was first introduced in October 2005, we did not use datasets prior to 2006. As we cannot differentiate between suicidal and non-suicidal self-inflicted injury, the estimates reported included both types of self-inflicted injuries. Suicidal behavior-related hospitalizations were defined as hospitalizations with suicidal ideation or suicide and self-inflicted injury.
Age, race, median household income quartiles for patient zip code, primary payer, length of stay, and total charges were coded in the NIS. Median household income quartiles for patient zip code provided a quartile classification estimating income of residents based on the year of data collection. Depression diagnoses were identified from the same hospitalization record using ICD-9-CM diagnosis codes listed in eTable 2.
Statistical analysis
The unit of analysis was a hospitalization. For trend analysis, to account for the sampling design changes in 2012, we used an alternative set of discharge and hospital weights for the 2006 - 2011 datasets, recalculated on the basis of the 2012 sampling design (HCUP 2015c; HCUP 2015d). This alternative set of weights is recommended to bridge the two different sampling designs (HCUP 2015c; HCUP 2015d). Using weights provided by the datasets, nationally representative estimates for annual numbers of hospitalizations were reported for suicidal behavior, suicidal ideation, and suicide and self-inflicted injury among pregnant women. We calculated the prevalence per 100,000 pregnancy- and delivery-related hospitalizations for suicidal behavior, suicidal ideation, and suicide and self-inflicted injury. To test linear trends across the seven years, we used orthogonal polynomial coefficients calculated recursively (Research Triangle Institute 2014) to generate linear contrasts.
For suicidal behavior-related hospitalizations, we examined the distributions of socio-demographic characteristics, length of stay, total charges, and depression status in each year. Total charges were adjusted for inflation to reflect 2012 dollars (Federal Reserve Bank of Minneapolis 2015). We compared the distributions of aforementioned characteristics between 2006 and 2012 by performing Wald Chi-square and t-tests. We plotted the prevalence of suicidal behavior per 100,000 pregnancy- and delivery-related hospitalizations according to age, race, income, and depression. For plots related to race, we performed direct age standardization using the 2000 standard US population (National Cancer Institute 2015).
All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC, USA) and SAS-callable SUDAAN software (version 11.0.1, RTI International, Research Triangle, NC, USA). Figures were plotted using R 3.1.0 (package “ggplot2”) and Plot.ly. Statistical significance was set at two-sided P<0.05. We used the Odyssey cluster supported by the Research Computing Group, Harvard University.
Results
The prevalence of suicidal ideation more than doubled from 2006 - 2012 (47.5 vs. 115.0 per 100,000 hospitalizations). A significant linear increase was observed for the prevalence of suicidal behavior (P<0.00001), but not for suicide and self-inflicted injury (P=0.57) (Table 1, eFigure 1). The increase in suicidal behavior-related hospitalizations was largely driven by the increase of suicidal ideation-related hospitalizations.
Table 1.
Suicidal behavior-related hospitalizations among pregnant women, United States, 2006-2012
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | P for trend |
|
|---|---|---|---|---|---|---|---|---|
| Total pregnancy- and delivery- related hospitalizations (n) |
4659091 | 4912884 | 4519719 | 4409606 | 4163593 | 4085316 | 4176646 | 0.00002 |
| Numbers of suicidal behavior-related hospitalizations (standard deviation) | ||||||||
| Suicidal behavior | 3609 (267) | 4142 (284) | 4951 (336) | 5214 (379) | 5873 (384) | 5778 (408) | 5940 (246) | <0.00001 |
| Suicidal ideation | 2214 (239) | 2642 (256) | 3426 (287) | 3941 (337) | 4354 (328) | 4602 (367) | 4805 (220) | <0.00001 |
| Suicide and self-inflicted injury | 1484 (102) | 1596 (104) | 1693 (116) | 1471 (118) | 1724 (125) | 1335 (101) | 1365 (89) | 0.42937 |
| Prevalence per 100,000 pregnancy- and delivery-related hospitalizations (standard error) | ||||||||
| Suicidal behavior | 77.5 (5.6) | 84.3 (6.1) | 109.5 (7.7) | 118.3 (8.7) | 141.1 (9.5) | 141.4 (10.6) | 142.2 (6.1) | <0.00001 |
| Suicidal ideation | 47.5 (5.1) | 53.8 (5.3) | 75.8 (6.5) | 89.4 (7.7) | 104.6 (8.1) | 112.7 (9.5) | 115.0 (5.5) | <0.00001 |
| Suicide and self-inflicted injury | 31.8 (2.1) | 32.5 (2.2) | 37.5 (2.7) | 33.4 (2.7) | 41.4 (3.0) | 32.7 (2.5) | 32.7 (2.1) | 0.56822 |
The characteristics of pregnant women with suicidal behavior-related hospitalizations are shown in Table 2. The mean age of women with suicidal behavior was approximately 26 years. More than one-third of suicidal behavior-related hospitalizations occurred in the 19-24-year age group (34.5% in 2006 and 37.6% in 2012); and nearly 10% occurred in the 12-18-year age group (12.7% in 2006 and 9.4% in 2012). Among the six racial groups, an increase in the proportion of whites was seen from 40.6% in 2006 to 45.2% in 2012; the largest proportion increase was seen among blacks (18.0% in 2006; 26.4% in 2012). The proportion of women in the lowest income quartile increased (33.5% in 2006; 39.1% in 2012) while the proportion of women in the highest income quartile decreased (17.3% in 2006; 14.0% in 2012). Medicaid and private insurance were the expected primary payer for nearly 80% of women. Among suicidal behavior-related hospitalizations, the proportion of hospitalizations with depression diagnoses was 69.6% in 2006 and in 2012 declined to 61.4% (P=0.001).
Table 2.
Characteristics of pregnant women with suicidal behavior-related hospitalizations, United States, 2006-2012
| Characteristics | 2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
P valuea | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | ||
| Suicidal behavior-related hospitalizations (n) | 3609 | 4142 | 4951 | 5214 | 5873 | 5778 | 5940 | ||||||||
| Age, mean±SE, year | 25.8±0.3 | 25.5±0.2 | 25.4±0.2 | 26.1±0.2 | 25.7±0.2 | 26.2±0.2 | 25.8±0.2 | 0.96 | |||||||
| Age categories, year | |||||||||||||||
| 12-18 | 458 | 12.7 | 425 | 10.3 | 495 | 10.0 | 465 | 8.9 | 638 | 10.9 | 496 | 8.6 | 560 | 9.4 | 0.04 |
| 19-24 | 1244 | 34.5 | 1619 | 39.1 | 1868 | 37.7 | 1982 | 38.0 | 2354 | 40.1 | 2073 | 35.9 | 2235 | 37.6 | |
| 25-29 | 851 | 23.6 | 1048 | 25.3 | 1364 | 27.6 | 1242 | 23.8 | 1217 | 20.7 | 1524 | 26.4 | 1460 | 24.6 | |
| 30-34 | 653 | 18.1 | 662 | 16.0 | 833 | 16.8 | 892 | 17.1 | 1036 | 17.6 | 1098 | 19.0 | 1205 | 20.3 | |
| 35-39 | 275 | 7.6 | 317 | 7.6 | 311 | 6.3 | 511 | 9.8 | 455 | 7.8 | 390 | 6.8 | 350 | 5.9 | |
| 40-55 | 129 | 3.6 | 72 | 1.7 | 80 | 1.6 | 121 | 2.3 | 173 | 2.9 | 198 | 3.4 | 130 | 2.2 | |
| Race | |||||||||||||||
| White | 1466 | 40.6 | 1660 | 40.1 | 2056 | 41.5 | 1991 | 38.2 | 2466 | 42.0 | 2489 | 43.1 | 2685 | 45.2 | <0.0001 |
| Black | 649 | 18.0 | 638 | 15.4 | 915 | 18.5 | 1088 | 20.9 | 1546 | 26.3 | 1362 | 23.6 | 1570 | 26.4 | |
| Hispanic | 428 | 11.9 | 482 | 11.6 | 450 | 9.1 | 733 | 14.1 | 680 | 11.6 | 651 | 11.3 | 825 | 13.9 | |
| Asian or Pacific Islander | 24 | 0.7 | 66 | 1.6 | 35 | 0.7 | 59 | 1.1 | 131 | 2.2 | 139 | 2.4 | 105 | 1.8 | |
| Native American | 52 | 1.4 | 19 | 0.5 | 38 | 0.8 | 23 | 0.4 | 41 | 0.7 | 59 | 1.0 | 60 | 1.0 | |
| Other | 132 | 3.7 | 173 | 4.2 | 120 | 2.4 | 124 | 2.4 | 203 | 3.5 | 291 | 5.0 | 290 | 4.9 | |
| Missing | 858 | 23.8 | 1104 | 26.7 | 1339 | 27.0 | 1196 | 22.9 | 808 | 13.8 | 786 | 13.6 | 405 | 6.8 | |
| Median household income quartiles for patient zip code | |||||||||||||||
| Quartile 1 (poorest) | 1208 | 33.5 | 1339 | 32.3 | 1711 | 34.6 | 2090 | 40.1 | 2274 | 38.7 | 2199 | 38.1 | 2325 | 39.1 | 0.29 |
| Quartile 2 | 949 | 26.3 | 1108 | 26.7 | 1396 | 28.2 | 1215 | 23.3 | 1558 | 26.5 | 1547 | 26.8 | 1485 | 25.0 | |
| Quartile 3 | 728 | 20.2 | 837 | 20.2 | 972 | 19.6 | 997 | 19.1 | 1110 | 18.9 | 1170 | 20.3 | 1200 | 20.2 | |
| Quartile 4 (wealthiest) | 626 | 17.3 | 757 | 18.3 | 774 | 15.6 | 728 | 14.0 | 755 | 12.9 | 744 | 12.9 | 830 | 14.0 | |
| Missing | 98 | 2.7 | 101 | 2.5 | 98 | 2.0 | 184 | 3.5 | 176 | 3.0 | 118 | 2.0 | 100 | 1.7 | |
| Expected primary payer | |||||||||||||||
| Medicare | 188 | 5.2 | 195 | 4.7 | 160 | 3.2 | 281 | 5.4 | 272 | 4.6 | 404 | 7.0 | 380 | 6.4 | 0.03 |
| Medicaid | 1878 | 52.0 | 2188 | 52.8 | 2715 | 54.8 | 3082 | 59.1 | 3543 | 60.3 | 3360 | 58.2 | 3555 | 59.8 | |
| Private insurance | 928 | 25.7 | 1056 | 25.5 | 1362 | 27.5 | 1167 | 22.4 | 1318 | 22.4 | 1376 | 23.8 | 1365 | 23.0 | |
| Self-pay | 388 | 10.8 | 460 | 11.1 | 415 | 8.4 | 427 | 8.2 | 371 | 6.3 | 353 | 6.1 | 370 | 6.2 | |
| Otherb | 227 | 6.2 | 224 | 5.4 | 281 | 5.7 | 233 | 4.5 | 345 | 5.9 | 271 | 4.7 | 260 | 4.4 | |
| Missing | 0 | 0 | 19 | 0.5 | 17 | 0.4 | 24 | 0.5 | 24 | 0.4 | 14 | 0.2 | 10 | 0.2 | |
| Length of stay, mean±SE, day | 4.0±0.2 | 4.5±0.4 | 3.9±0.1 | 4.0±0.1 | 4.0±0.1 | 4.3±0.2 | 4.5±0.2 | 0.07 | |||||||
| Total chargesc, mean±SE, dollar | 12423±880 | 14052±1091 | 11999±588 | 14434±1154 | 14064±941 | 15522±953 | 16210±1082 | 0.007 | |||||||
| With depression diagnoses | 2513 | 69.6 | 2669 | 64.4 | 3196 | 64.5 | 3207 | 61.5 | 3775 | 64.3 | 3473 | 60.1 | 3650 | 61.4 | 0.001 |
Weighted column percentages may not total 100 because of rounding.
Abbreviations: SE, standard error
Significance test was performed to compare the distributions between 2006 and 2012. P value was calculated using the Wald Chi-square test for categorical variables and the t-test for continuous variables.
Other includes no charges.
Total charges were adjusted for inflation to reflect 2012 dollars.
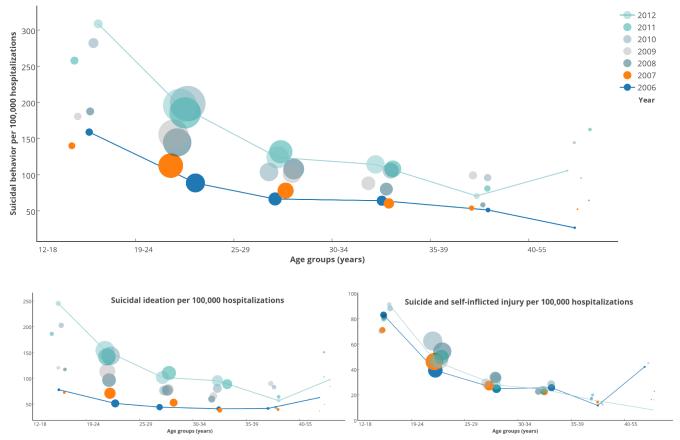
The prevalence of suicidal behavior per 100,000 pregnancy- and delivery-related hospitalizations according to age groups is presented in Figure 1. In general, across the six age groups, the more recent the year, the higher the prevalence for suicidal behavior and suicidal ideation, but not for suicide and self-inflicted injury (Figure 1, eTable 4). The highest prevalence was consistently observed in the 12-18-year age group. The largest numbers of pregnant women with suicidal behavior-related hospitalizations were consistently observed in the 19-24-year age group.
Figure 1.
Suicidal behavior-related hospitalizations per 100,000 hospitalizations according to age groups among pregnant women, United States, 2006-2012
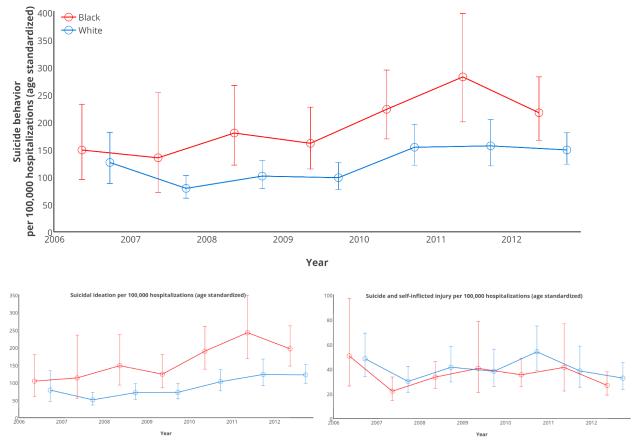
We focused on blacks and whites, the two racial groups with relatively high prevalence and larger populations. Figure 2 shows the prevalence of suicidal behavior per 100,000 pregnancy- and delivery-related hospitalizations (age-standardized). Across the study period, black women had higher prevalence of suicidal behavior, increasing from 148.3 per 100,000 hospitalizations in 2006 to 216.3 in 2012 (eTable 5); the prevalence among white women was 125.6 per 100,000 hospitalizations in 2006 and 148.5 in 2012. A similar pattern was seen for suicidal ideation (Figure 2, eTable 5a). For suicide and self-inflicted injury, no material difference was noted for black and white women (eTable 5b).
Figure 2.
Suicidal behavior-related hospitalizations per 100,000 hospitalizations (age-standardized) according to race among pregnant women, United States, 2006-2012
For suicidal behavior and suicidal ideation, increasing trends in prevalence were generally observed for all income quartiles (eFigure 2). Lower income showed a higher rate of increase in prevalence with the most striking increase seen in the lowest income quartile from 94.3 per 100,000 hospitalizations in 2006 to 193.3 in 2012 (eTable 6). The highest rate of increase was observed during the period of 2007-2008. For suicide and self-inflicted injury, hospitalizations in the lowest income quartile had higher prevalence than those in the highest income quartile.
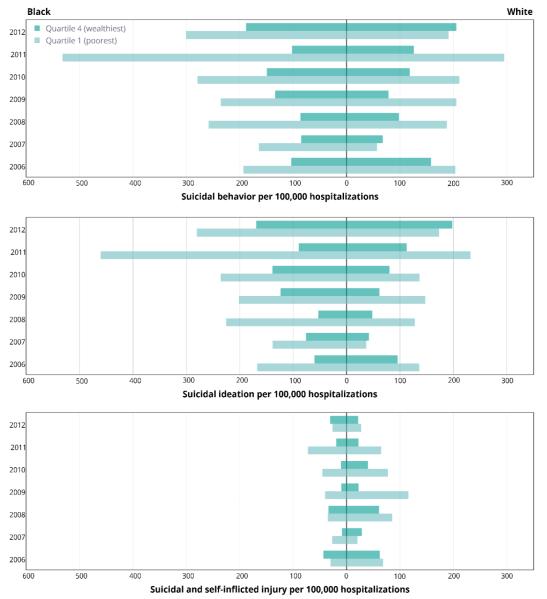
To demonstrate the effects of both race and income on suicidal behavior, we calculated the prevalence (age-standardized) from the lowest and the highest income quartiles for black and white women (Figure 3, eTables 7/7a/7b). Overall, for suicidal behavior, black women had higher prevalence than white women; those in the lowest income quartile had higher prevalence than women in the highest income quartile. Among the four racial-income groups, black women in the lowest income quartile had the highest prevalence of suicidal behavior per 100,000 hospitalizations: 164.3 in 2007, 258.6 in 2008, 235.4 in 2009, 279.2 in 2010, 532.3 in 2011, and 300.6 in 2012 (eTable 7). For suicidal ideation, black women in the lowest income quartile had the highest prevalence across the seven-year study period (eTable 7a). However, for suicide and self-inflicted injury, no consistent pattern was observed.
Figure 3.
Suicidal behavior-related hospitalizations per 100,000 hospitalizations (age-standardized) according to race and median household income quartiles for patient zip code among pregnant women, United States, 2006-2012
We plotted the prevalence of suicidal behavior among three groups: 1) all pregnancy- and delivery-related hospitalizations; 2) hospitalizations with depression diagnoses; and 3) hospitalizations without depression diagnoses (Figure S3). The prevalence of suicidal behavior, suicidal ideation, and suicide and self-inflicted injury was higher among hospitalizations with depression diagnoses (eTables 8, 8a, 8b).
Discussion
The analysis of pregnancy- and delivery-related hospitalizations revealed a substantial increase in the prevalence of suicidal ideation from 2006-2012 while the prevalence for suicide and self-inflicted injury was stable. Women in the 12-18-year age group had the highest prevalence of suicidal ideation and suicide and self-inflicted injury. For suicidal ideation, black women had higher prevalence than white women; women in the lowest income quartile had the highest prevalence and the highest rate of increase; black women in the lowest income quartile had the highest prevalence. The prevalence of suicidal behavior was higher among hospitalizations with depression diagnoses.
During the seven-year study period, the number of suicidal ideation-related hospitalizations more than doubled. However, the increasing usage of the ICD-9-CM diagnosis code V62.84 for suicidal ideation introduced in 2005 may only explain some of increase for suicidal ideation-related hospitalizations since an increasing trend in suicide was also seen in the US over the study period (Centers for Disease Control and Prevention 2015). We speculate that the increase might also be accounted for by more frequent help-seeking behaviors among pregnant women or changing patterns of major risk factors for suicidal ideation such as psychiatric disorders and substance abuse. Nonetheless, it remains unclear if any of these factors are related to the increasing number of suicidal ideation among pregnant women. We did not observe a parallel increase in suicide and self-inflicted injury, highlighting the necessity to understand which factors predict transition from suicidal ideation to attempt (Nock et al. 2012) during pregnancy. More research is needed to investigate whether pregnancy might be associated with better control of impulse and aggression, possibly resulting in fewer suicide attempt (Appleby 1991; Lowry et al. 2014).
Compared with women in other age groups, pregnant teens in the 12-18-year age group consistently showed the highest prevalence of suicidal ideation and suicide and self-inflicted injury. Considering that pregnancy among teens are more likely to be mistimed and/or unwanted (Appleby 1991), pregnant teens may be more prone to stigmatization related to premarital pregnancy, financial difficulties, loss of educational and employment opportunity, and barriers to safe abortion, possibly leading to antepartum suicidal behavior (Appleby 1991; Cockburn and Pawson 2007; Frautschi et al. 1994; Pinheiro et al. 2012). Notably, Silverman suggested that intimate partner violence may play an important role in predisposing teens to suicide and suicidal behavior (Silverman et al. 2001). Programs aimed at reducing teen pregnancy and intimate partner violence may mitigate suicidal behavior in this vulnerable population.
Our findings highlight a racial disparity that warrants further study. We found that blacks had higher prevalence of suicidal ideation than whites across the seven-year study period, although there was no difference between the two groups for suicide and self-inflicted injury. Among non-pregnant populations, investigators have reported inconsistent results regarding racial differences in suicide and suicidal behavior (Doshi et al. 2005; Gibbs 1997; Kessler et al. 1999; Mościcki et al. 1988; Perez-Rodriguez et al. 2008; Rockett et al. 2006; Shaffer et al. 1994; Ting et al. 2012). A study conducted in a US university-affiliated obstetric clinic showed that white women had decreased risks of antepartum suicidal ideation compared with non-whites, although the association was thought to be confounded (Gavin et al. 2011). Other investigators, using nationally representative samples of non-pregnant women and men, have found no racial differences in the risk of suicide ideation (Kessler et al. 2005; Perez-Rodriguez et al. 2008). Among blacks, the higher prevalence of poverty, racism, low education, diagnostic and treatment bias (Nelson et al. 2002) may contribute to observed racial disparity in suicidal behavior. Additionally, black women had higher prevalence of prenatal depression (Orr et al. 2006), but were less likely to initiate treatment and receive follow-up treatment among those who initiate treatment (Kozhimannil et al. 2014). Observed racial differences in suicide and suicidal behavior will have important implications in suicide prevention efforts given that one of the core objective of the Patient Protection and Affordable Care Act is reducing racial disparities. Considering that the racial diversity of the US will continue to increase (Perez-Rodriguez et al. 2008), further studies are needed to understand the distinctive roles that race may play in the etiology and expression of suicide and suicidal behavior, and identify common and specific risk and protective factors among pregnant women across these groups. Culturally-informed prevention programs should be tailored to meet the needs of black pregnant women, especially those among the lowest income quartile.
Growing evidence has documented an association of suicide and suicidal behavior with low income at both the individual and national levels (Economou et al. 2013; Gunnell et al. 1999; Lorant et al. 2005; McMillan et al. 2010; Pagura et al. 2008). We found that women in the highest income quartile had the lowest prevalence of suicidal behavior and women in the lower income quartiles had a higher rate of increase over the study period, suggesting that low income pregnant women were representative of a high-risk population among whom screening for suicidal behavior should be taken into account (Mauri et al. 2012).
Hospitalizations with depression diagnoses had higher prevalence of suicidal behavior. Consequently, identifying women at risk for antenatal depression is vital for detecting women with comorbid suicidal ideation and suicide and self-inflicted injury (Gavin et al. 2011). Women with positive screening results for depression during perinatal visits should be closely monitored for suicidal behavior. Future research should examine whether the treatment of underlying depression reduces suicidal behavior during pregnancy.
Nearly one-third of suicidal behavior-related hospitalizations happened without the presence of depression diagnoses, and this proportion has increased by more than 8% from 2006 to 2012, indicating that the occurrence of suicidal behavior cannot completely be explained by the occurrence of depression. In prenatal care clinics, screening for suicidal behavior is needed for women both with and without depression (Zhong et al. 2014).
Our findings should be considered in the context of several important limitations. First, we identified suicidal behavior through administrative codes (ICD-9-CM and DRG), which suffered from error, and lack of temporal information and clinical content (Bates et al. 2003; Perlis et al. 2012). Psychiatric disorders were often under-coded and suicidal behavior was very likely to be underreported (Fischer et al. 2008; Kessler et al. 2005; Perlis et al. 2012). The effect of these factors combined was to make our estimates more conservative. Future studies using methods that does not rely on administrative codes such as natural language processing (Jha 2011; Murff et al. 2011) are needed to confirm whether the increase in suicidal ideation was an artifact of the recent introduction of the V62.84, and to accurately identify cases. Second, we cannot distinguish between suicidal and non-suicidal self-inflicted injury based on the ICD-9-CM E codes (E950-E959). Hence, potential misclassification may partially account for our inability to observe an increase in suicide and self-inflicted injury. However, according to a study conducted among adolescents treated with antidepressants, the E codes for suicide and self-inflicted injury had a notably positive predictive value of 82.6% for confirmed suicidal behavior (Callahan et al. 2013). Non-suicidal self-inflicted injury may also heighten risk for future suicidal behavior (Scott et al. 2015). Third, we did not present data about methods for suicide and self-inflicted injury used by pregnant women. Understanding the impact of the availability and acceptability of suicide methods on suicide behavior would be helpful to guide the development of prevention strategies.
Conclusions
This study provides the first description of nationally representative estimates for suicidal behavior among pregnant women in the US. Pregnancy is the period when immediate interventions should be indicated for the life and health of both mother and offspring. Our results identify high-risk populations for suicidal behavior that should be recognized, diagnosed, and appropriately intervened. The study highlights the increasing burden and important racial differences in suicidal ideation. Factors that predict the transition from suicidal ideation to suicide attempt during pregnancy should also be explored to understand the disproportional increase in suicidal ideation. Future studies are needed to understand the distinctive roles that race plays in the etiology and expression of suicidal behavior and identify risk factors that may be especially relevant to black pregnant women’s engagement in suicidal behavior. The information gained from such studies can further the efforts to develop tailored, culturally-informed prevention programs for black pregnant women, particularly those with lower income. Our study also illustrates the need for special attention to pregnant teens given the consistently high prevalence of suicidal behavior; programs aimed at reducing teen pregnancy and intimate partner violence may mitigate suicidal behavior. Moreover, it is critical to consider the public health implications of the finding that nearly one-third of suicidal behavior-related hospitalizations happened without depression. While routine screening for antenatal and postpartum depression becomes a standard of care, specific attention should be paid to suicidal behavior during these periods (Lindahl et al. 2005; Zhong et al. 2014).
Supplementary Material
Acknowledgements
This research was supported by awards from the National Institutes of Health (the National Institute on Minority Health and Health Disparities: T37-MD001449; and the National Center for Research Resources (NCRR), the National Center for Advancing Translational Sciences (NCATS): 8UL1TR 000170-05). The authors would like to thank Dr. Miguel-Angel Luque Fernandez and Dr. Wenyuan Li for help with programming. The authors would like to thank Kathy Brenner for help with editing this manuscript. Special thanks are extended to the Research Computing Group at the Faculty of Art and Sciences of Harvard University, for continuous support with computational resources.
Footnotes
Disclosures: The authors declare that there are no conflicts of interest.
References
- Agampodi S, Wickramage K, Agampodi T, Thennakoon U, Jayathilaka N, Karunarathna D, Alagiyawanna S. Maternal mortality revisited: the application of the new ICD-MM classification system in reference to maternal deaths in Sri Lanka. Reprod Health. 2014;11:17. doi: 10.1186/1742-4755-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleby L. Suicide during pregnancy and in the first postnatal year. BMJ. 1991;302:137–140. doi: 10.1136/bmj.302.6769.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asad N, Karmaliani R, Sullaiman N, Bann CM, McClure EM, Pasha O, Wright LL, Goldenberg RL. Prevalence of suicidal thoughts and attempts among pregnant Pakistani women. Acta Obstet Gynecol Scand. 2010;89:1545–1551. doi: 10.3109/00016349.2010.526185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin M-P, Kildea S. Maternal mortality and psychiatric morbidity in the perinatal period: challenges and opportunities for prevention in the Australian setting. Med J Aust. 2007;186:364–367. doi: 10.5694/j.1326-5377.2007.tb00940.x. [DOI] [PubMed] [Google Scholar]
- Bates DW, Evans RS, Murff H, Stetson PD, Pizziferri L, Hripcsak G. Detecting adverse events using information technology. J Am Med Inform Assoc. 2003;10:115–128. doi: 10.1197/jamia.M1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant A, Mhyre JM, Leffert LR, Hoban RA, Yakoob MY, Bateman BT. The association of maternal race and ethnicity and the risk of postpartum hemorrhage. Anesth Analg. 2012;115:1127–1136. doi: 10.1213/ANE.0b013e3182691e62. [DOI] [PubMed] [Google Scholar]
- Callahan ST, Fuchs DC, Shelton RC, Balmer LS, Dudley JA, Gideon PS, DeRanieri MM, Stratton SM, Williams CL, Ray WA. Identifying suicidal behavior among adolescents using administrative claims data. Pharmacoepidemiol Drug Saf. 2013;22:769–775. doi: 10.1002/pds.3421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [Accessed 18 September 2015];Deaths: Final Data for 2013. 2015 http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_02.pdf.
- Chang J, Berg CJ, Saltzman LE, Herndon J. Homicide: A leading cause of injury deaths among pregnant and postpartum women in the United States, 1991-1999. Am J Public Health. 2005;95:471. doi: 10.2105/AJPH.2003.029868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockburn J, Pawson ME. Psychological Challenges in Obstetrics and gynecology. Springer; New York: 2007. [Google Scholar]
- Czeizel AE. Attempted suicide and pregnancy. J Inj Violence. 2011;3:45–54. doi: 10.5249/jivr.v3i1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeizel AE, Tomcsik M, Tímár L. Teratologic evaluation of 178 infants born to mothers who attempted suicide by drugs during pregnancy. Obstet Gynecol. 1997;90:195–201. doi: 10.1016/S0029-7844(97)00216-0. [DOI] [PubMed] [Google Scholar]
- Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo CA. National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997-2001. Ann Emerg Med. 2005;46:369–375. doi: 10.1016/j.annemergmed.2005.04.018. [DOI] [PubMed] [Google Scholar]
- Economou M, Madianos M, Peppou LE, Theleritis C, Patelakis A, Stefanis C. Suicidal ideation and reported suicide attempts in Greece during the economic crisis. World Psychiatry. 2013;12:53–59. doi: 10.1002/wps.20016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Reserve Bank of Minneapolis [Accessed 12 February 2015];Consumer Price Index, 1913 - 2015 https://www.minneapolisfed.org/community/teaching-aids/cpi-calculator-information/consumer-price-index-and-inflation-rates-1913.
- Fischer LR, Rush WA, Kluznik JC, O’Connor PJ, Hanson AM. Abstract C-C1-06: identifying depression among diabetes patients using natural language processing of office notes. Clin Med Res. 2008;6:125–126. [Google Scholar]
- Frautschi S, Cerulli A, Maine D. Suicide during pregnancy and its neglect as a component of maternal mortality. Int J Gynaecol Obstet. 1994;47:275–284. doi: 10.1016/0020-7292(94)90574-6. [DOI] [PubMed] [Google Scholar]
- Fuhr DC, Calvert C, Ronsmans C, Chandra PS, Sikander S, De Silva MJ, Patel V. Contribution of suicide and injuries to pregnancy-related mortality in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2014;1:213–225. doi: 10.1016/S2215-0366(14)70282-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi SG, Gilbert WM, McElvy SS, El Kady D, Danielson B, Xing G, Smith LH. Maternal and neonatal outcomes after attempted suicide. Obstet Gynecol. 2006;107:984–990. doi: 10.1097/01.AOG.0000216000.50202.f6. [DOI] [PubMed] [Google Scholar]
- Gavin AR, Tabb KM, Melville JL, Guo Y, Katon W. Prevalence and correlates of suicidal ideation during pregnancy. Arch Womens Ment Health. 2011;14:239–246. doi: 10.1007/s00737-011-0207-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile S. Suicidal mothers. J Inj Violence research. 2011;3:90–97. doi: 10.5249/jivr.v3i2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs JT. African-American Suicide: A Cultural Paradox. Suicide Life Threat Behav. 1997;27:68–79. [PubMed] [Google Scholar]
- Gissler M, Hemminki E, Lonnqvist J. Suicides after pregnancy in Finland, 1987-1994: register linkage study. BMJ. 1996;313:1431–1434. doi: 10.1136/bmj.313.7070.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold KJ, Singh V, Marcus SM, Palladino CL. Mental health, substance use and intimate partner problems among pregnant and postpartum suicide victims in the National Violent Death Reporting System. Gen Hosp Psychistry. 2012;34:139–145. doi: 10.1016/j.genhosppsych.2011.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D, Lopatatzidis A, Dorling D, Wehner H, Southall H, Frankel S. Suicide and unemployment in young people. Analysis of trends in England and Wales, 1921-1995. Br J Psychiatry. 1999;175:263–270. doi: 10.1192/bjp.175.3.263. [DOI] [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project (HCUP) [Accessed 1 Feburary 2015];Introduction to the HCUP National Inpatient Sample (NIS) 2015a https://www.hcupus.ahrq.gov/db/nation/nis/NISIntroduction2012.pdf.
- Healthcare Cost and Utilization Project (HCUP) [Accessed 1 Feburary 2015];Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2015b https://www.hcup-us.ahrq.gov/db/nation/nis/nisarchive.jsp.
- Healthcare Cost and Utilization Project (HCUP) [Accessed Accessed 1 Feburary 2015];Nationwide Inpatient Sample (NIS) Redesign Report. 2015c http://www.hcupus.ahrq.gov/db/nation/nis/reports/NISRedesignFinalReport040914.pdf.
- Healthcare Cost and Utilization Project (HCUP) [Accessed 1 Feburary 2015];Trend Weights for HCUP NIS Data. 2015d https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp.
- Hornbrook MC, Whitlock EP, Berg CJ, Callaghan WM, Bachman DJ, Gold R, Bruce FC, Dietz PM, Williams SB. Development of an algorithm to identify pregnancy episodes in an integrated health care delivery system. Health Serv Res. 2007;42:908–927. doi: 10.1111/j.1475-6773.2006.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H, Faisal-Cury A, Chan Y-F, Tabb K, Katon W, Menezes PR. Suicidal ideation during pregnancy: prevalence and associated factors among low-income women in São Paulo, Brazil. Arch Womens Ment Health. 2012;15:135–138. doi: 10.1007/s00737-012-0263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK. The promise of electronic records: Around the corner or down the road? JAMA. 2011;306:880–881. doi: 10.1001/jama.2011.1219. [DOI] [PubMed] [Google Scholar]
- Kendell R. Suicide in pregnancy and the puerperium. BMJ. 1991;302:126. doi: 10.1136/bmj.302.6769.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, Adams AS. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2014 doi: 10.1176/appi.ps.62.6.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, Marchbanks PA. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12:469–477. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8:77–87. doi: 10.1007/s00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- Lorant V, Kunst AE, Huisman M, Costa G, Mackenbach J. Socio-economic inequalities in suicide: a European comparative study. Br J Psychiatry. 2005;187:49–54. doi: 10.1192/bjp.187.1.49. [DOI] [PubMed] [Google Scholar]
- Lowry R, Crosby AE, Brener ND, Kann L. Suicidal thoughts and attempts among US high school students: trends and associated health-risk behaviors, 1991–2011. J Adolesc Health. 2014;54:100–108. doi: 10.1016/j.jadohealth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- Marzuk PM, Tardiff K, Leon AC, Hirsch CS, Portera L, Hartwell N, Iqbal MI. Lower risk of suicide during pregnancy. Am J Psychiatry. 1997;154:122–123. doi: 10.1176/ajp.154.1.122. [DOI] [PubMed] [Google Scholar]
- Mauri M, Oppo A, Borri C, Banti S. SUICIDALITY in the perinatal period: comparison of two self-report instruments. Results from PND-ReScU. Arch Womens Ment Health. 2012;15:39–47. doi: 10.1007/s00737-011-0246-y. [DOI] [PubMed] [Google Scholar]
- McMillan KA, Enns MW, Asmundson G, Sareen J. The association between income and distress, mental disorders, and suicidal ideation and attempts: findings from the Collaborative Psychiatric Epidemiology Surveys. J Clin Psychiatry. 2010;71:1168–1175. doi: 10.4088/JCP.08m04986gry. [DOI] [PubMed] [Google Scholar]
- Mościcki E, O'Carroll P, Rae D, Locke B, Roy A, Regier D. Suicide attempts in the Epidemiologic Catchment Area study. Yale J Biol Med. 1988;61:259. [PMC free article] [PubMed] [Google Scholar]
- Murff HJ, FitzHenry F, Matheny ME, Gentry N, Kotter KL, Crimin K, Dittus RS, Rosen AK, Elkin PL, Brown SH. Automated identification of postoperative complications within an electronic medical record using natural language processing. JAMA. 2011;306:848–855. doi: 10.1001/jama.2011.1204. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute [Accessed 1 February 2015];Standard Populations - Single Ages. 2015 http://seer.cancer.gov/stdpopulations/stdpop.singleages.html.
- Nelson AR, Smedley BD, Stith AY. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; Washington: 2002. [PubMed] [Google Scholar]
- Nock M, Nock MK, Borges G, Ono Y. Suicide: global perspectives from the WHO world mental health surveys. Cambridge University Press; New York: 2012. [Google Scholar]
- Oates M. Suicide: the leading cause of maternal death. Br J Psychiatry. 2003;183:279–281. doi: 10.1192/bjp.183.4.279. [DOI] [PubMed] [Google Scholar]
- Orr ST, Blazer DG, James SA. Racial disparities in elevated prenatal depressive symptoms among black and white women in eastern North Carolina. Ann Epidemiol. 2006;16:463–468. doi: 10.1016/j.annepidem.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Pagura J, Cox BJ, Sareen J, Enns MW. Factors associated with multiple versus single episode suicide attempts in the 1990–1992 and 2001–2003 United States national comorbidity surveys. J Nerv Ment Dis. 2008;196:806–813. doi: 10.1097/NMD.0b013e31818b6a77. [DOI] [PubMed] [Google Scholar]
- Paris R, Bolton RE, Weinberg MK. Postpartum depression, suicidality, and mother-infant interactions. Arch Womens Ment Health. 2009;12:309–321. doi: 10.1007/s00737-009-0105-2. [DOI] [PubMed] [Google Scholar]
- Perez-Rodriguez MM, Baca-Garcia E, Oquendo MA, Blanco C. Ethnic differences in suicidal ideation and attempts. Prim psychiatry. 2008;15:44. [PMC free article] [PubMed] [Google Scholar]
- Perlis R, Iosifescu D, Castro V, Murphy S, Gainer V, Minnier J, Cai T, Goryachev S, Zeng Q, Gallagher P. Using electronic medical records to enable large-scale studies in psychiatry: treatment resistant depression as a model. Psychol Med. 2012;42:41–50. doi: 10.1017/S0033291711000997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips MR. Pregnancy and suicide: towards a coherent narrative. Lancet Psychiatry. 2014;1:168–170. doi: 10.1016/S2215-0366(14)70303-7. [DOI] [PubMed] [Google Scholar]
- Pinheiro RT, da Cunha Coelho FM, da Silva RA, de Ávila Quevedo L, de Mattos Souza LD, Castelli RD, de Matos MB, Pinheiro KAT. Suicidal behavior in pregnant teenagers in southern Brazil: Social, obstetric and psychiatric correlates. J Affect Disord. 2012;136:520–525. doi: 10.1016/j.jad.2011.10.037. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute . SUDAAN example manual. Research Triangle Park, NC: 2014. [Google Scholar]
- Rockett IR, Samora JB, Coben JH. The black–white suicide paradox: Possible effects of misclassification. Soc Sci Med. 2006;63:2165–2175. doi: 10.1016/j.socscimed.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Scott LN, Pilkonis PA, Hipwell AE, Keenan K, Stepp SD. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: A multi-wave prospective study. Compr Psychiatry. 2015;58:1–10. doi: 10.1016/j.comppsych.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadigian EM, Bauer ST. Pregnancy-associated death: a qualitative systematic review of homicide and suicide. Obstet Gynecol Surv. 2005;60:183–190. doi: 10.1097/01.ogx.0000155967.72418.6b. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould M, Hicks RC. Worsening suicide rate in black teenagers. Am J Psychiatry. 1994;151:1810–1812. doi: 10.1176/ajp.151.12.1810. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Raj A, Mucci LA, Hathaway JE. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. JAMA. 2001;286:572–579. doi: 10.1001/jama.286.5.572. [DOI] [PubMed] [Google Scholar]
- Ting SA, Sullivan AF, Boudreaux ED, Miller I, Camargo CA. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993–2008. Gen Hosp Psychistry. 2012;34:557–565. doi: 10.1016/j.genhosppsych.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Practice Management Information Corporation . ICD-9-CM: International Classification of Diseases, 9th Revision: Clinical Modification vol 1. PMIC. Practice Management Information Corporation; Los Angeles: 1998. [Google Scholar]
- Yusuf HR, Akhter HH, Chowdhury ME, Rochat RW. Causes of death among women aged 10–50 years in Bangladesh, 1996–1997. J Health Popul Nutr. 2007;25:302. [PMC free article] [PubMed] [Google Scholar]
- Zhong QY, Gelaye B, Rondon MB, Sánchez SE, Simon GE, Henderson DC, Barrios YV, Sánchez PM, Williams MA. Using the Patient Health Questionnaire (PHQ-9) and the Edinburgh Postnatal Depression Scale (EPDS) to assess suicidal ideation among pregnant women in Lima, Peru. Arch Womens Ment Health. 2014:1–10. doi: 10.1007/s00737-014-0481-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.