Abstract
Medically underserved populations in the US continue to experience higher cancer burdens of incidence, mortality and other cancer-related outcomes. It is imperative to understand how health inequities experienced by diverse population groups may contribute to our increasing unequal cancer burdens and disparate outcomes. The National Cancer Institute convened a diverse group of scientists to discuss research challenges and opportunities for cancer epidemiology in medically underserved and understudied populations. This report summarizes salient issues and discuss five recommendations from the group, including the next steps required to better examine and address cancer burden in US among our rapidly increasing diverse and understudied populations.
Keywords: Cancer, Epidemiologic Research, Understudied Populations
Introduction
Despite declining overall cancer incidence and mortality rates in the US, medically underserved populations continue to experience higher cancer burdens of incidence, mortality and other disparate cancer-related outcomes (e.g. more aggressive disease, delayed diagnostic and therapeutic care, patient-reported outcomes). Sobering statistics of disproportionate cancer burden are observed for racial/ethnic sub-populations, such as African-Americans (AA), American Indian/Alaskan Natives (AI/AN), Hispanic/Latino Americans (HL), and Asian-Americans (AsA)(1–5). Beyond race and ethnicity, there is increasing evidence of unequal cancer burden and/or higher prevalence of cancer-associated risk factors (e.g. hepatitis B/C, Helicobacter pylori, smoking, alcohol, obesity, poverty) for diverse and often understudied subpopulations defined by one or more factors such as low socioeconomic status (SES), non-metropolitan/rural populations, sexual and gender minorities (SGM), refugees or asylum seekers, incarcerated, and the elderly. The causes of cancer disparities likely reflect the interplay of biological and environmental determinants as well as a plethora of socio-ecological factors that can assert critical influences on cancer etiology and outcomes at different junction across the cancer continuum (6, 7).
The authors define Understudied Populations as a specific group, who may or may not be medically underserved or socially disadvantaged but whose epidemiologic data on cancer health risks and outcomes are currently limited. There is a lack of sufficient epidemiologic data on this diverse group to informed evidence-based cancer control, prevention and intervention. The dearth of research and information for these groups underscores the urgency to improve our available data and knowledge regarding cancer risks and outcomes within these understudied populations.
The implications for cancer, public health and health-related policies are significant given the impending demographic and socio-cultural shift as the US transitions into a minority-majority nation (8, 9). The reshaping of the US racial and ethnic composition is, in part, due to the arrival of nearly 59 million immigrants in the US over the last 50 years; which has increased the percentage of foreign-born to almost 14% of the US population (10).
In 2013, National Cancer Institute’s (NCI) Office of Science Planning and Assessment conducted an analysis of the Division of Cancer Control and Population Sciences (DCCPS) research portfolio. This assessment revealed that cancer epidemiologic research in understudied populations focused primarily on race/ethnicity, with limited focus of geography and SES, and no focus on other population groups such as refugees or asylum seekers, incarcerated, sexual and gender minority groups (SGM) and the elderly. Therefore, the think tank Understudied Populations in Cancer Epidemiologic Research: Implications for Future Needs (11) was convened by the Epidemiology and Genomics Research Program (EGRP) of the DCCPS, NCI to engage researchers and discuss the challenges, gaps and opportunities for cancer epidemiology research in understudied populations. The immediate goals of the Think Tank were to (1) identify opportunities and resources to expand efforts to bridge the scientific gaps and (2) set research priorities in cancer epidemiology for understudied populations. The long-term goal is to promote epidemiologic studies of understudied populations to generate data and knowledge to inform evidence-based cancer prevention and control guidelines and policies.
Here we highlight discussions of key challenges and opportunities for cancer epidemiologic research within multiple understudied groups, In concert with provocative questions (PQ) submitted prior to the meeting, they informed the five recommendations. The PQs serve as an initial process to stimulate conversations with the broader research community about where research should go and provide a platform of future considerations (Table 1).
Table 1.
Provocative Questions for Cancer Epidemiologic Research in Understudied Populations
|
Discussion
Issues and Challenges
Under-representation of race/ethnic populations within cancer epidemiologic cohorts
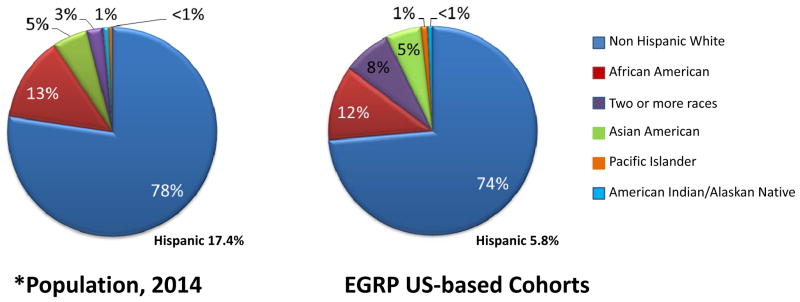
Cancer Epidemiology Cohort (CEC) studies are among the key approaches for advancing understanding of the complex etiology of cancer and provide fundamental insights into environmental, lifestyle, and genetic risk factors responsible for cancer burden. The cohort prospective design enables evaluation of multiple outcomes, on risks of other chronic diseases as well and provides the infrastructure to assess lifestyle, environmental, sociocultural, genetic and biologic factors and their interplay that may contribute to disease onset and may influence disparities. Currently, EGRP funds a sizable number of cohorts with large minority populations, including the Southern Community Cohort Study (SCCS), Black Women’s Health Study (BWHS), Multiethnic Cohort Study (MEC) and the Adventist Health Study (AHS). They collectively they are following a demographically represented proportion of AAs to assess determinants of cancer incidence and outcome (12–17). Nevertheless, a substantial large proportion of other racial and ethnic sub-populations are underrepresented including individuals of Hispanic/Latino (HL) and American Indian and Alaska Native (AI/AN) ancestry (Figure 1), as well as populations of other minority social statuses - often precluding precise estimation of risks and testing of ethnic-specific hypotheses and not enabling comparisons within these groups.
Figure 1.
Distribution of race/ethnic populations in EGRP-supported consortia vs. US populations, 2014
*US Census 2014 data – downloaded 10/26/2015
Heterogeneity within racial/ethnic groups
Currently, it is common practice in research to group racial/ethnic populations into broad monolithic categories that are generally consistent with the race categories mandated by the Office of Management and Budget (OMB) 1997 standards. These types of analyses have been useful to show dramatic differences in cancer burden by race/ethnic background. However, the practice of aggregating diverse ethnic groups together can mask disparities occurring among distinct sub-groups. For example, aggregated data in AI/AN depict lower prostate and breast cancer incidence and mortality and little difference in cervical and colon cancer incidence and mortality when compared to Non-Hispanic Whites (NHW) (18). However, disaggregated data by geographic location shows substantial and/or statistically significant cancer disparities between AI/AN and NHW living in the same region, particularly for breast, cervix, colon and prostate cancers (3, 19–23). In the 48 contiguous states, Northern and Southern Plains AIs have significantly elevated cancer incidence and/or mortality rates. Death rates for AI men were elevated compared to NHW men for lung, colorectal, prostate, and larynx cancers while AI women had significantly higher rates of lung, colorectal, and cervical cancers. There are many other examples of research in which disaggregate data highlight differences across and within ethnic groups in risk factors and cancer related outcomes in other populations including Asian Americans (AsA), Native Hawaiians and Other Pacific Islanders (NH/PI) and US-based populations of African descent (4, 24–26). Furthermore, the challenges for studying cancer in diverse racial/ethnic minority populations (e.g., substantial heterogeneity in language, culture, migration trends, degree of acculturation, SES, and lifestyle) (27–29) are multifold and somewhat unique to each group. For example, unlike for some HL in which there is some shared common language across subpopulations, the heterogeneity in language and culture for AsA is wide-ranging. Therefore, careful consideration will be needed to determine whether to investigate race/ethnic populations as an aggregated or disaggregated variable and will depend upon the research question.
One cross-cutting and central challenge, and perhaps most important in epidemiologic research among specific subpopulations, is the methodological issue of small sample size (30). Many of the current statistical methods only provide correct estimates for large sample sizes and may not be applicable to smaller sample sizes (31). Development of novel methods to address these challenges is needed in conjunction to alternative statistical techniques and factors previously recommended by others (32–39).
Data disparities in special populations
At the very basis of any efforts to address inequities in cancer burden is the availability of epidemiological data that can characterize a population’s sociodemographic features and be used to investigate potential health needs. When fundamental epidemiologic data are not collected and thus unavailable for descriptive analyses, surveillance and scientific inquiries, understudied and special subpopulations become invisible in the larger narrative – perhaps sporadically discussed but anecdotally at best. For example, cancer epidemiologic research for subpopulations such as SGM communities, refugee and asylum seekers, and the elderly are limited or nonexistent; and thus their specific burden of cancer is unknown.
Where such populations are marginalized or experience marked social inequalities, we can anticipate that cancer prevention, screening, treatment, and survivorship may be adversely affected. Studies suggested that the SGM community (3.4 percent of the US population) may carry a disproportionate burden of some types cancer (40–44) and higher prevalence of risk factors (e.g., smoking rates, alcohol consumption) (45–48).. Refugees/asylum seekers represent another example of a subpopulation for whom epidemiologic data are lacking, but are sorely needed considering their unique vulnerabilities such as chronic co-morbidities, chronic stress, poor nutrition, and health care access. There is a paucity of data on refugee/asylum seekers from low and middle income countries (49–54); no epidemiological studies of cancer in many countries affected by humanitarian emergencies (55); and no epidemiological studies of cancer among the newly arrived refugees, perhaps the most vulnerable group of refugees, in the US. More than 3 million refugees have come to the United States in the last 35 years; and nearly 70,000 entered the US in 2014 with projected increases of 75, 000 and 100, 000 new arrivals in 2015 and 2016, respectively (56). The research gaps regarding refugee health and cancer risk/outcomes are substantial as data on refugee status are not collected routinely.
The US elderly population (age 65 and older) is rapidly increasing and is projected to more than double from 40.3 million in 2010 to 83.7 million in 2050(57) and has become more racially and ethnically diverse (58). This will likely lead to increases in cancer incidence given that cancer is a disease associated with aging. Therefore, issues of cancer screening and appropriate care have become more relevant for this population.
Broadening examination of cancer disparities beyond race/ethnicity
Disparities studies have tended to focus on investigating differences by race/ethnicity with few studies considering additional factors such as geographic location or SES, which likely contribute to the differential burden of cancer. Geographic location provides information about the lived conditions and permits opportunities to examine a meta-view of contextual factors (e.g., the physical and social environment) that may be important to identify known and unknown cancer risk factors or determinants of disparities in screening, treatment, and survivorship (59–61). Examples are seen in rural American populations or populations located in “ecological niches” such as populations along the US-Mexico border. These populations tend to be less educated and have lower income than the overall population. Their reduced access to health care – particularly specialty care – results in significant health disparities which include a higher incidence of disease, disability and/or chronic illnesses, increased mortality rates and lower life expectancies.
Comprehensive understanding of causes of disparities may require the incorporation of neighborhood measures, such as area-level demographic factors obtained from Census data and neighborhood conditions using Google Earth and Street View. The immediate challenges will be developing the infrastructure needed to integrate, manage, and determine the best way to analyze the massive amount of data collected.
Measurements of socioeconomic status (SES) are often complex, with no best indicator suitable for all studies. Indicators used to collect information on SES include education; housing tenure, housing conditions and neighborhood; household amenities; income; occupation based measures; and wealth. Each one of these indicators presents strengths and limitations in their use (62, 63). Typically, household income has been used in many studies, but income is affected by many factors, including the number of people living in a household, frequency of employment (full-time, part-time or seasonable), indebtedness, care provided for extended family members, and other factors. These factors may be dynamic and varied throughout the life course. Reported income does not necessarily indicate disposable income, especially in understudied populations and thus collecting data on income is problematic in general with issues such as high non-response rates, and may be more problematic in some populations (64). In these situations, the measure of wealth, which combines total assets and income may serve as a better indicator (62). The choice of SES measurements, whether it is the exposure or confounder, should be informed by the research question and the framework by which SES will be linked to health outcome. Although standardized measures of SES at both individual and contextual levels are ideal for comparing across studies and across populations, additional measures particular to understudied populations should also be considered. English language proficiency and acculturation are also important to consider in immigrant populations as these factors are confounded with SES. Health insurance status and source of health care, also often strongly correlated with SES, might also be measures to consider in many underserved and disadvantaged populations.
Importance of establishing trusting community-scientist collaborations and partnerships
Gaining and sustaining trust from research populations is particularly essential when the communities are underserved/understudied minority groups where it is important to recognize that issues of trust can often be unique to each subpopulation. This may come into play when collecting geographic/spatial data from communities that have experienced discrimination and/or are undocumented. Undocumented individuals, who have been in the US for several years, are more cautious in sharing information whereas new arrivals are less cautious. The lack of trust in the medical system by many American Indians/Alaska Natives and resistance to taking part in research studies is well documented (6, 65–67). In Appalachian communities, there is a general distrust of outsiders. A unique challenge with regards to rural communities is that they may be more motivated to participate in research that offers the opportunity to solve (not simply study) a problem of importance to them and the opportunities to improve local capacity; hence building confidence and trust among this population that the research will lead to improvements is needed. To establish and sustain trust it is important to get the communities input and buy in of the research plans including honest discussions about what can be realistically accomplished and not, and how the research results could be shared or communicated with individuals and communities.
Community-based participatory research (CBPR) has emerged within the last few decades and uses a collaborative approach to understand and protect public health through the involvement of all partners in the research process (68). However, in epidemiological studies the process that has been used more effectively is community engagement (CE) where the community’s input is sought in identifying critical areas for research, for recruitment and retention and in sharing data periodically over the course of the study. The intent of using CE is to bridge the gap between science and practice to increase health equity (69–74). Evidence from these studies can be used to design new interventions and maintain community engagement and build a more robust CBPR process in the conception, design, conduct, analysis and communication of results.
Use of trans-disciplinary research
Utilization of transdisciplinary (TD) research methods can accelerate progress towards a comprehensive view of the multi-factorial causes and complexity of health disparities. TD research occurs when investigators from different disciplines work jointly to create a new conceptual, theoretical, methodological and translational framework that will integrate and move beyond discipline-specific approaches to address a problem. Effective and efficient TD research teams enable scientists to transcend the boundaries of their respective disciplines to address the multilevel complexities of the unequal burden of health in understudied populations. There are examples of TD research in cancer including the Centers for Population Health and Health Disparities (CPHHD) program and the Transdisciplinary Research on Energetics and Cancer (TREC) centers. The research in each of the centers spans from cells to society (75, 76). As TD research continues to evolve, appropriate engagement with multiple sectors including public health researchers, policymakers, community base organizations, clinicians, and patients/survivors will be necessary.
Meeting Recommendations
Based on the above issues and challenges, the following recommendations for cancer epidemiologic research in understudied populations emerged and also included possibilities for infrastructure support. These recommendations are outlined in Table 2 and are addressed below:
Table 2.
Summary of recommendations and proposed actions
| Meeting Recommendations | Proposed Actions |
|---|---|
| 1. Increase representation of race/ethnic populations in Cancer Epidemiology Cohort Studies | Create cohorts for American Indians/Alaska Natives; Hispanic/Latino; and Asian Americans, Native Hawaiians, Pacific Islanders. Maximize potential by focusing on multiple disease/outcomes Develop less expensive ways to support cohorts |
| 2. Inclusion of special populations in cancer epidemiologic research | Include subpopulations such as SGM refugees/asylum seekers, elderly in cancer epidemiology studies Include questions about sexual orientation and gender identity on national health surveys and questionnaires Increase research on non-communicable diseases, including cancer among refugee populations and asylum seekers As cancer cohorts age, evaluate risk factors and outcomes among the elderly populations |
| 3. Examine cancer epidemiology in populations within the context of other factors such as geographic location and/or SES. | Increase research that will improve the knowledge for ways SES combines with race/ethnicity to affect cancer risks and outcomes Propose epidemiologic research that will examine cancer within geographic regions or ecological niches Examine exposures through its biological, psycho-social, environmental, and community context Integrate new technologies into epidemiologic research |
| 4. Optimize available infrastructure to support cancer epidemiologic research among understudied populations | Perform data harmonization across cohorts Link health databases to SEER registries Link non-cancer minority cohorts to cancer related databases for the creation of new cancer cohorts Developing central or universal databases for the coordination of data |
| 5. Support transdisciplinary research and training next generation | Link cancer researchers to other disciplines e.g. linking cancer epidemiologist to geographers, health economics Develop funding opportunities that will encourage and support transdisciplinary research |
| Develop and continue to support training opportunities that will continue to create the next generation of researchers |
Recommendation 1: Increase the representation of race, ethnic and other subpopulations in Cancer Epidemiology Cohort studies
Since there are relatively few cancer epidemiology studies focused on AI/AN, HL, AsA and NHPI groups, they are typically are not targeted for cancer interventions. Given differential cancer burden by factors like race/ethnicity (18) and geographic locations (3, 5, 19–22) as well as considerable variations within ethnic group by nativity and immigration status (24), the recommendation was for increased representation of these populations in cancer epidemiology studies, through the creation of cohorts specific to these populations for studying the independent and joint effects of risk factors for cancer incidence and outcomes at multiple levels over a life-course. Ideally, these cohorts should collect information on multiple health and disease outcomes. It may also be possible to combine data from various sources to create and adequate sample size of subgroups that could provide some preliminary research insights. However, the ability to create large cohorts is challenging given the current fiscal climate and will require the efforts of several funding sources for sustainability. Therefore, there is a need for innovation and development of cost-efficient cohorts that are well representative.
Recommendation 2: Inclusion of special populations in cancer epidemiologic research
Studies on cancer risks and outcomes for other populations, such as SGM, refugees and elderly, will have to account for the intersectionality of factors (gender, race/ethnicity, geographic area, discrimination, etc.) that likely exert multiplicative effects on cancer health outcomes. Measuring the combined effects of these factors can make research particularly challenging for these groups. A first step towards addressing SGM disparities is to include questions about sexual orientation and gender identity on all national health surveys as the National Health Interview Survey, and questionnaires used in cancer epidemiology studies, particularly large cohort studies. For the elderly population, research focus should be as much on quality of care as quality of life. It is also important to consider other co-morbidities within this population, especially since these may have an impact on tolerance for cancer therapy (77, 78). Issues related to palliative care and symptom management will be critical considerations and programs in these are areas are not available to many underserved elderly communities. As populations covered by existing cancer cohorts age, there may be increasing opportunities for new research within these cohorts to evaluate risk factors.
Studies on cancer risks and outcomes for refugee populations will differ from those of immigrants. In the US, a significant disparity exists in healthcare access and health knowledge among refugee populations compared to the wider US population. Recent qualitative formative research identified several barriers associated with healthcare access for new arrivals including inability to comprehend and/or navigate the health system, low awareness of available medical resources, limited English proficiency and low economic opportunities. Prior to the passage of the Affordable Care Act, refugees were provided an initial eight months of refugee medical assistance; and once this service expired, there was no system in place to track the health status of refugees over time. Recent changes to the national medical coverage with the Affordable Care Act provide opportunities for the continuity of services for refugees. Therefore, a collaboration among investigators with US government entities (e.g. Department of State, CDC) will be useful for addressing and understanding the burden of cancer and associated risks affecting newly arrived refugees and asylum seekers.
Recommendation 3: Examine population group differences in cancers within the context of other factors such as geographic location and/or SES
Disparities in cancer burden exist across geography/place of residence, occupation, social class, SES, and numerous other dimensions which are often overlooked in cancer epidemiology research. The study of SES and health disparities is often complex with methodological and analytical issues (64) and SES-related research is on-going (64, 79). A clear priority is understanding the complex interaction between SES with race/ethnicity and its effect on cancer risks and outcomes. Other areas of interest include using Medicaid expansion data to examine effects of race/ethnicity in the this population, examining reasons for geographic segregation of racial/ethnic groups and the effects of living in specific locations (e.g. high income people in poor areas); conducting studies of individuals with high levels of education from minority cohorts, and employing and combining theoretical frameworks from other disciplines. Because of the potential for misattribution of causality, thoughtful consideration should be given to appropriate measurement, analysis, and interpretation of all social determinants.
To date, most studies that examined residential neighborhood characteristics are limited by 1) a focus on current residence only when in fact most people spend one third of their time elsewhere; 2) failure to consider cumulative exposures over time (e.g., residential history); 3) use of arbitrary administrative units (county, census tract, or zip code); and failure to consider adjacent areas; and 4) failure to consider household or individual characteristics. Future research thus should consider geographic heterogeneity of populations to provide etiologic clues for cancer and the causes of cancer disparities across racial/ethnic groups. Novel technologies and methods, such as geographic information system (GIS) or linkage to area-based data on the physical and social environment, geographic location could enrich our understanding about the contexts in which people live and the immediate availability of cancer prevention, screening, and treatment resources in their areas. Towards this goal, to study the geographical connection with cancer disparities, studies should routinely geocode participant addresses and efforts should be devoted to develop rich contextual datasets of geographically linked data.
One new paradigm to assess how a lifetime of exposure to environmental- and community-level factors affects the risk of cancer may be ecogeographic genetic epidemiology that integrates spatial, environmental, and genetic data into models of geographic disease etiology (80).
Additionally, novel analytical and statistical approaches appropriate to the geospatial and multilevel nature of the data should be developed, such as improving traditional structural equation models to help identify mediators and moderators of associations
New technology to measure neighborhood conditions is rapidly becoming available, but evidence about their validity and reliability is often lacking. Google Street View, for example, is a rapidly developing technology that can provide certain types of neighborhood characteristics (81) while the utility of other emerging technologies (e.g. Twitter, Instgram, and Foursquare) remain to be investigated (82, 83).
Recommendation 4: Optimize available infrastructure to support cancer epidemiologic research among understudied populations
The current fiscal environment necessitates the need to optimize existing infrastructure to continue health disparities research. Some strategies include: (1) developing and/or maximizing research infrastructure and resources for understudied populations through partnership and collaborations with other funding agencies (Indian Health Services or Centers for Disease Control and Prevention); (2) leveraging infrastructure created by ongoing initiatives (such as Precision Medicine Initiative); ((3) developing and improving methods for effective mining of existing large-scale data; (4) encouraging and enhancing data sharing to enable new studies and scientific progress; (5) creating a centralized repository identifying harmonized data variables from NCI or NIH funded cohorts; (6) providing opportunities for investigators to add neglected populations (e.g. SGM, refugee or asylum seekers) to existing cohorts or for secondary analysis of existing data for new health disparities research questions.
Creative strategies may also include the creation of new tools (like Health Disparities Calculator, http://seer.cancer.gov/hdcalc/) linking minority populations from non-cancer minority cohorts (such as those from National Heart, Lung and Blood Institute) to the SEER or state cancer registries. Developing central or universal databases for the coordination of data, such as a database allowing the query of population numbers by various social determinants of health (race, ethnicity, SES, SGM) could be pursued as part of the agenda of the Epidemiology and Genomics Research Program’s Cancer Epidemiology Consortia. Linkage of SEER to Medicaid, Blue Cross/Blue Shield, Cancer Research Networks and HMO Research Networks will also be useful, but will require addressing privacy concerns, perhaps through the application of technological advances. These activities will serve to increase collaborative partnerships needed for multi- and trans-disciplinary cancer epidemiologic research focused on understudied populations.
Recommendation 5: Support trans-disciplinary research and training the next generation
Establishing a balance between the time it takes to build and maintain a TD research team with tenure-track clock within an academic environment could present a challenge to researchers, therefore changes in the research and academic environments will be necessary for the sustainability of TD research. The development of funding mechanisms that will support TD research and the substantial dedicated time for engaging in TD research was identified as a priority. In addition, funding mechanisms that support training of junior principal investigators and senior postdoctoral research on TD research approaches will aid future development of this research area. The creation of these funding mechanisms will require new criteria for effective evaluation of TD research applications. These actions should play a role in the creation of a scientific environment supportive of TD research. Given the increasing use of TD research methods, offering training that integrates core curriculum from many disciplines along with high-quality mentoring and opportunities for career-development will be helpful. Suggestions include (1) training for health disparities research at multiple levels of career development; (2) funding grants to support training of junior principal investigators and senior postdoctoral researchers on TD approaches for research in understudied populations (these training grants might support short-term work by researchers in disciplines other than their own); (3) training researchers and other key stakeholders (e.g. community partners) to conduct appropriate research in communities; and (4) supporting training in implementation science research.
This summary captures the salient issues highlighted by the “Think Tank on Understudied Populations in Cancer Epidemiologic Research: Implications for Future Needs”. The purpose of the multidisciplinary Think Tank was to initiate an on-going discussion with investigators interested in research in understudied populations. The issues, challenges, recommendations and provocative questions discussed here will provide information for future discussions, working groups, workshops, and developing funding opportunities. In concert, they provide the next steps in the process as EGRP further collaborates with the wider, multidisciplinary scientific community and the public to better examine and address the unequal burden of cancer across diverse populations.
Acknowledgments
The authors would like to thank Elizabeth Gillanders and Kathy Helzlsouer for their comments and edits to the manuscript; and Scott Rogers and Marina Dathe for the provision of data in preparation of the figure on EGRP supported cohorts.
Footnotes
No Financial Conflicts of Interests
References
- 1.American Cancer Society. Cancer Facts and Figures. Atlanta: 2015. [Google Scholar]
- 2.Siegel RL, Fedewa SA, Miller KD, Goding-Sauer A, Pinheiro PS, Martinez-Tyson D, et al. Cancer statistics for Hispanics/Latinos, 2015. CA Cancer J Clin. 2015;65(6):457–80. doi: 10.3322/caac.21314. [DOI] [PubMed] [Google Scholar]
- 3.Espey DK, Jim MA, Cobb N, Bartholomew M, Becker T, Haverkamp D, et al. Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health. 2014;104(Suppl 3):S303–11. doi: 10.2105/AJPH.2013.301798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomez SL, Noone AM, Lichtensztajn DY, Scoppa S, Gibson JT, Liu T, et al. Cancer incidence trends among Asian American populations in the United States, 1990–2008. Journal of the Nationall Cancer Institute. 2013;105:1096–110. doi: 10.1093/jnci/djt157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS. Disparities in cancer mortality and incidence among American Indians and Alaksa Natives in the United States. Am J Public Health. 2014;104(Supple 3):S377–87. doi: 10.2105/AJPH.2013.301673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hiatt RA, Breen N. The social determinants of cancer: a challenge for transdisciplinary science. Am J Prev Med. 2008;35(2 Suppl):S141–50. doi: 10.1016/j.amepre.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng XL, et al. Considering context, place and culture: the National Latino and Asian American Study. Int J Methods Psychiatr Res. 2004;13(4):208–20. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Census Bureau. As the nation ages, seven states become younger. Census Bureau Reports. 2014 Available from: http://www.census.gov/newsroom/press-releases/2014/cb14-118.html.
- 9.Pew Research Center. Future immigration will change the face of America by 2065. Washington, DC: Pew Research Center; 2015. updated October 5, 2015; cited 2015 November 5. Available from: http://www.pewresearch.org/fact-tank/2015/future-immigration-will-change-the-face-of-america-by-2065/ [Google Scholar]
- 10.Washington, DC: Pew Research Center; 2015. Modern immigration wave brings 59 million to U.S., driving population growth and change through 1965. cited 2015 November 5. Available from: http://www.pewhispanic.org/2015/09/28/modern-immigration-wave-brings-59-million-to-u-s-driving-population-growth-and-change-through-2065. [Google Scholar]
- 11.Think Tank on Understudied Populations in Cancer Epidemiologic Research: Implications for Future Needs. Epidemiology and Genomics Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute; 2015. [December 16, 2015]. Available from: http://epi.grants.cancer.gov/events/understudied-pops/ [Google Scholar]
- 12.Loma Linda University Medical Center. Adventist Health Study. cited 2015 November 6. Available from: http://publichealth.llu.edu/adventist-health-studies.
- 13.Boston University Sloan Epidemiology Center. Black Women’s Health Study. cited 2015 November 6. Available from: www.bu.edu/bwhs/
- 14.University of Hawaii Cancer Center. The Multiethnic Cohort Study. 2015 cited 2105 November 6. Available from: http://www.uhcancercenter.org/research/the-multiethnic-cohort-study-mec.
- 15.Rosenberg L, Adams-Campbell L, Palmer JR. The Black Women’s Health Study: a follow-up study for causes and preventions of illness. J Am Med Womens Assoc. 1995;50(2):56–8. [PubMed] [Google Scholar]
- 16.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010;21(1 Suppl):26–37. doi: 10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Signorello LB, Hargreaves MK, Steinwandel MD, Zheng W, Cai Q, Schlundt DG, et al. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97(7):972–9. [PMC free article] [PubMed] [Google Scholar]
- 18.American Cancer Society. Cancer Facts and Figures for Hispanic/Latinos 2015–2017. Atlanta: American Cancer Society; 2015. [Google Scholar]
- 19.Perdue DG, Haverkamp D, Perkins C, Daley CM, Provost E. Geographic variation in colorectal cancer incidence and mortality: age of onset and stage of diagnosis among American Indian and Alaska Native People, 1990–2009. Am J Public Health. 2014;104(Suppl 3):S404–14. doi: 10.2105/AJPH.2013.301654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plescia M, Henley SJ, Pate A, Underwood JM, Rhodes K. Lung cancer deaths among American Indians and Alaska Natives: 1999–2009. Am J Public Health. 2014;104(Suppl 3):S388–95. doi: 10.2105/AJPH.2013.301609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watson M, Bernard V, Thomas C, Brayboy A, Paisano R, Becker T. Cervical cancer incidence and mortality among American Indian and Alaska Native Women, 1999–2009. Am J Public Health. 2014;104(Supple 3):S415–22. doi: 10.2105/AJPH.2013.301681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White A, Richardson LC, Li C, Ekwuene DU, Kaur JS. Breast cancer morality among American Indian and Alaska Native Women, 1990–2009. Am J Public Health. 2014;104(Suppl 3):S432–8. doi: 10.2105/AJPH.2013.301720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Espey D, Paisano R, Cob N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990–2001. Cancer. 2005;103:1045–53. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 24.Asian Pacific American Legal Center of Southern California Asian Law Caucus, National Asian Pacific American Legal Consortium. Asian and Pacific Islander Demographic Profile. Los Angeles, CA: 2005. The diverse face of Asian and Pacific Islanders in California. [Google Scholar]
- 25.Consedine N, Tuck N, Ragin C, Spencer B. Beyond the black box: A systematic review of breast, prostate, colorectal, and cervical screening among native and immigrant African-descent Caribbean populations. Journal of Immigrant Minority Health. 2015;17:905–24. doi: 10.1007/s10903-014-9991-0. [DOI] [PubMed] [Google Scholar]
- 26.Haile RWJE, Levine AJ, et al. A review of cancer in US Hispanic populations. Can Prev Res (Phila) 2012;5:150–63. doi: 10.1158/1940-6207.CAPR-11-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.UCLA Center for Health Policy Research. CHIS 2007 Adult Public Use File. Los Angeles, CA: 2012. California Health Interview Survey. Available from: http://healthpolicy.ucla.edu/chis/Pages/default.aspx. [Google Scholar]
- 28.Tseng W, McDonnell DD, Ho W. Prepared for the California Program on Access to Care (CPAC) UC Berkeley School of Public Health; 2010. Aug, Ethnic Health Assessment for Asian Americans, Native Hawaiians and Pacific Islanders in California. Report No. [Google Scholar]
- 29.Messias DK, Rubio M. Immigration and health. Annu Rev Nurs Res. 2004;22:101–34. [PubMed] [Google Scholar]
- 30.Srinivasa S, Moser R, Willis G, Riley W, Alexander M, Berrigan D, et al. Small is essential: importance of subpopulation research in cancer control. Am J Public Health. 2015;105(Supple 3):S371–3. doi: 10.2105/AJPH.2014.302267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fok CCT, Henry D, Allen J. Maybe small is too small a term: introduction to advancing small sample prevention science. Prevention Sciece. 2015;16:943–9. doi: 10.1007/s11121-015-0584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Henry D, Dymnicki AB, Mohatt N, Allen J, Kelly JG. Clustering Methods with Qualitative Data: a Mixed-Methods Approach for Prevention Research with Small Samples. Prev Sci. 2015;16(7):1007–16. doi: 10.1007/s11121-015-0561-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hopkin CR, Hoyle RH, Gottfredson NC. Maximizing the Yield of Small Samples in Prevention Research: A Review of General Strategies and Best Practices. Prev Sci. 2015;16(7):950–5. doi: 10.1007/s11121-014-0542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoyle RH, Gottfredson NC. Sample Size Considerations in Prevention Research Applications of Multilevel Modeling and Structural Equation Modeling. Prev Sci. 2015;16(7):987–96. doi: 10.1007/s11121-014-0489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kadane JB. Bayesian Methods for Prevention Research. Prev Sci. 2015;16(7):1017–25. doi: 10.1007/s11121-014-0531-x. [DOI] [PubMed] [Google Scholar]
- 36.CCTF. Henry D, Allen J. Research designs for intervention research with small samples II: Stepped wedge adn interrupted time-series design. Prevention Science. 2015;16:765–77. doi: 10.1007/s11121-015-0569-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fok CCT, Henry D. Increasing the sensitivity of measures to change. Prevention Science. 2015;16:978–86. doi: 10.1007/s11121-015-0545-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hedeker D. Methods for multi-level ordinal data in prevention research. Prevention Science. 2015;16:997–1006. doi: 10.1007/s11121-014-0495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wyman PA, Henry D, Knoblauch S, Brown CH. Designs for testing group-based interventions with limited number of social units: The dynamic wait-listed and regression point displacement designs. Prevention Science. 2015;16:956–66. doi: 10.1007/s11121-014-0535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boehmer U, Ozonoff A, Miao X. An ecological analysis of colorectal cancer incidence and mortality: differences by sexual orientation. BMC Cancer. 2011;11:400. doi: 10.1186/1471-2407-11-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boehmer U, Ozonoff A, Timm A. County-level association of sexual minority density with breast cancer incidence: results from an ecological study. Sex Res Soc Policy. 2011;8:139–45. [Google Scholar]
- 42.Buchting F, Margolies L, Bare M, Bruessow D, Díaz-Toro E, Kamen C, et al. LGBT Best and Promising Practices Throughout the Cancer Continuum. Fort Lauderdale, Florida: LGBT HealthLink; 2015. [Google Scholar]
- 43.Blosnich J, Farmer G, Lee J, Silenzio V, Bowen D. Health inequalities among sexual minority adults: evidence from ten U.S. states, 2010. American Journal of Preventive Medicine. 2014;46:337–49. doi: 10.1016/j.amepre.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boehmer U, Ozonff A, Miao X. An ecological approach to examine lung cancer disparities due to sexual orientation. Public Health. 2012;126:605–12. doi: 10.1016/j.puhe.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Easton A, Jackson K, Mowery P, Comeau D, Sell R. Adolescent same-sex and both-sex romantic attractions and relationships: implications for smoking. Am J Public Health. 2008;98(3):462–7. doi: 10.2105/AJPH.2006.097980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosario M, Corliss HL, Everett BG, Reisner SL, Austin SB, Buchting FO, et al. Sexual orientation disparities in cancer-related risk behaviors of tobacco, alcohol, sexual behaviors, and diet and physical activity: pooled Youth Risk Behavior Surveys. Am J Public Health. 2014;104(2):245–54. doi: 10.2105/AJPH.2013.301506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blosnich J, Jarrett T, Horn K. Disparities in Smoking and Acute Respiratory Illnesses Among Sexual Minority Young Adults. Lung. 2010;188:401–7. doi: 10.1007/s00408-010-9244-5. [DOI] [PubMed] [Google Scholar]
- 48.Tang H, Greenwood GL, Cowling DW, Lloyd JC, Roeseler AG, Bal DG. Cigarette Smoking among lesbians, gays, and bisexuals: how serious a problem? Cancer Causes and Control. 2004;15:797–803. doi: 10.1023/B:CACO.0000043430.32410.69. [DOI] [PubMed] [Google Scholar]
- 49.Khan SM, Gillani J, Nasreen S, Zai S. Pediatric tumors in north west Pakistan and Afghan refugees. Pediatr Hematol Oncol. 1997;14(3):267–72. doi: 10.3109/08880019709009496. [DOI] [PubMed] [Google Scholar]
- 50.Khan SM, Gillani J, Nasreen S, Zai S. Cancer in north west Pakistan and Afghan refugees. J Pak Med Assoc. 1997;47(4):122–4. [PubMed] [Google Scholar]
- 51.Bhatia S, Dranyi T, Rowley D. A social and demographic study of Tibetian refugees in India. Social Science and Medicine. 2002;54:411–22. doi: 10.1016/s0277-9536(01)00040-5. [DOI] [PubMed] [Google Scholar]
- 52.Doocy S, Sirois A, Tileva M, Storey J, Burnham G. Chronic disease and disability among Iraqi populations displaced in Jordan and Syria. International Journal Health Planning Management. 2013;28:e1–12. doi: 10.1002/hpm.2119. [DOI] [PubMed] [Google Scholar]
- 53.Mateen FJ, Carone M, Al-Saedy H, Nyce S, Mutuerandu T, Ghosn J. Cancer diagnosis in Iraqi refugees. Acta Oncol. 2012;51:950–1. doi: 10.3109/0284186X.2012.667148. [DOI] [PubMed] [Google Scholar]
- 54.Otoukesh S, Mojtahedzadeh M, Sherzai D, Behazin A, Bazargan-Hejai S, Bazargan M. A retrospective study of demographic parameters and major health referrals among Afgan refugees in Iran. Int J Equity Health. 2012;11:82. doi: 10.1186/1475-9276-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spiegel P, Khalia A, Mateen FJ. Cancer in refugees in Jordan and Syria between 2009 and 2012: challenges and the way forward in humanitarian emergencies. Lancet Oncol. 2014;15:e290–7. doi: 10.1016/S1470-2045(14)70067-1. [DOI] [PubMed] [Google Scholar]
- 56.Refugee Processing Center. Admission and Arrivals. Interactive Reporting. 2015 cited 2015 November 17. Available from: http://www.wrapsnet.org/Reports/InteractiveReporting/tabid/393/Default.aspx.
- 57.West LA, Cole S, Goodkind D, He W. 65+ in the United States: 2010. 2014. Contract No.: P23–212. [Google Scholar]
- 58.West LACS, Goodkind D, He W. 65+ in the United States: 2010. 2014. Contract No.: P23–212. [Google Scholar]
- 59.Rural Assistance Center. Rural Health Disparities. 2015 cited 2015 November 6. Available from: https://www.raconline.org/topics/rural-health-disparities.
- 60.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. J Urban Health. 2014;91(2):272–92. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soden DL. At the cross roads: US/Mexico border counties in transition. 2006. [Google Scholar]
- 62.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Smith GD. Indicators of socioeconomic position (part 1) J Epidemiol Community Health. 2006;60:7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Smith GD. Indicators of socioeconomic position (part 2) J Epidemiol Community Health. 2006;60:95–101. doi: 10.1136/jech.2004.028092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shavers VL. Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association. 2007;99(9):1013–23. [PMC free article] [PubMed] [Google Scholar]
- 65.Watanabe-Galloway S, Burhansstipanov L, Krebs L. Partnering for success through community based participatory research in Indian Country. Journal of Cancer Education. 2014;29(3):588–95. doi: 10.1007/s13187-014-0683-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Braun KL, Kagawa-Singer M, Holden AE, Burhansstipanov L, Tran JH, Seals BF, et al. Cancer patient navigator tasks across the cancer care continuum. Journal of health care for the poor and underserved. 2012;23(1):398–413. doi: 10.1353/hpu.2012.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Krebs LU, Burhansstipanov L, Watanabe-Galloway S, Pingatore NL, Petereit DG, Isham D. Navigation as an intervention to eliminate disparities in American Indian communities. Seminars in Oncology Nursing. 2013;29:118–27. doi: 10.1016/j.soncn.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 69.Burhansstipano L, Dignan M, Schumacher A, Krebs L, Alfonsi G, Apodaca C. Breast screening navigator programs within three settings that assist underserved women. Journal of Cancer Education. 2010;25:247–52. doi: 10.1007/s13187-010-0071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Burhansstipanov L. Native American community-based cancer projects: theory vs. reality. Cancer Control: Journal of the Moffitt Cancer Center. 1999;6:620–6. doi: 10.1177/107327489900600618. [DOI] [PubMed] [Google Scholar]
- 71.Burhansstipanov L, Christopher S, Schumacher A. Lessons learned from community-based participatory research in Indian Country. Journal of the Moffit Cancer Center. 2005;12(Suppl 2):70–6. doi: 10.1177/1073274805012004s10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Christopher S, Burhansstipanov L, McCormick K, Simmonds A, Watts V. Using a community based participatory research approach to implement a survey within an American Indian community. San Francisco, CA: Jossey-Bass, John Wiley and Sons; 2013. [Google Scholar]
- 73.Krishnan S, Petereit DG, Kanekar S, Burhansstipanov L, Esmond S, Miner R, et al. Community based participatory development, implementatin and evaluatin of a cancer screening educational intervention among American Indian in the Northern Plains. Journal of Cancer Education. 2011;26:530–9. doi: 10.1007/s13187-011-0211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl 1):S40–6. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, et al. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98(9):1608–15. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Patterson RE, Colditz GA, Hu FB, Schmitz KH, Ahima RS, Brownson RC, et al. The 2011–2016 Transdisciplinary Research on Energetics and Cancer (TREC) initiative: rationale and design. Cancer Causes Control. 2013;24(4):695–704. doi: 10.1007/s10552-013-0150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kumar S, Katheria V, Hurria A. Evaluating the older patient with cancer: understanding frality and the geriatric assessment. CA: A Cancer Journal for Clinicians. 2010;60:120–32. doi: 10.3322/caac.20059. [DOI] [PubMed] [Google Scholar]
- 78.Pal SK, Katheria V, Hurria A. Evaluating the older patient with cancer: understanding frailty and the geriatric assessment. CA: A Cancer Journal for Clinicians. 2010;60:120–32. doi: 10.3322/caac.20059. [DOI] [PubMed] [Google Scholar]
- 79.Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs. 2012;31:1803–13. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- 80.Rappaport SM, Smith MT. Epidemiology. Environment and disease risks. Science. 2010;330(6003):460–1. doi: 10.1126/science.1192603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bader MD, Mooney SJ, Lee YJ, Sheehan D, Neckerman KM, Rundle AG, et al. Development and deployment of the Computer Assisted Neighborhood Visual Assessment System (CANVAS) to measure health-related neighborhood conditions. Health Place. 2015;31:163–72. doi: 10.1016/j.healthplace.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Quercia D, Schifanella R, Aiello LM, McLean K. Smelly maps: The digital life of urban smellscapes. Proceedings of the Ninth International AAAI Conference on Web and Social Media. 2015 [Google Scholar]
- 83.Vaca C, Quercia D, Bonchi F, Fraternali P. Taxonomy-based discovery and annotation of functional areas in the city. Proceedings of the Ninth International AAAI Conference on Web and Social Media. 2015:445–53. [Google Scholar]