Abstract
Background
As adults live longer, multiple chronic conditions have become more prevalent over the past several decades. We describe the prevalence of, and patient characteristics associated with, cardiac and non-cardiac-related multimorbidities in patients discharged from the hospital after an acute coronary syndrome.
Methods
We studied 2,174 patients discharged from the hospital after an acute coronary syndrome at 6 medical centers in Massachusetts and Georgia between April, 2011 and May, 2013. Hospital medical records yielded clinical information including presence of 8 cardiac-related and 8 non-cardiac-related morbidities on admission. We assessed multiple psychosocial characteristics during the index hospitalization using standardized in-person instruments.
Results
The mean age of the study sample was 61 years, 67% were men, and 81% were non-Hispanic whites. The most common cardiac-related morbidities were hypertension, hyperlipidemia, and diabetes (76%, 69%, and 31%, respectively). Arthritis, chronic pulmonary disease, and depression (20%, 18%, and 13%, respectively) were the most common non-cardiac morbidities. Patients with ≥4 morbidities (37% of the population) were slightly older and more frequently female than those with 0–1 morbidity; they were also heavier and more likely to be cognitively impaired (26% vs. 12%), have symptoms of moderate/severe depression (31% vs. 15%), high perceived stress (48% vs. 32%), a limited social network (22% vs. 15%), low health literacy (42% vs. 31%), and low health numeracy (54% vs. 42%).
Conclusions
Multimorbidity, highly prevalent in patients hospitalized with an acute coronary syndrome, is strongly associated with indices of psychosocial deprivation. This emphasizes the challenge of caring for these patients, which extends well beyond acute coronary syndrome management.
Keywords: multimorbidities, acute coronary syndrome
Introduction
Multimorbidity, the presence of two or more chronic diseases in an individual, has become increasingly common over the past decade with prevalence estimates of at least 25 percent in the American adult population.1,2 Patients with multimorbidity are at substantial risk for disability, death, and poor quality of life, and account for a disproportionate share of U.S. health expenditures.2,4 This emerging “epidemic” creates substantial challenges for health care providers as well as family members caring for these complex patients.1
The acute coronary syndromes account for most coronary heart disease-related hospitalizations in American adults, with about 2.2 million hospitalizations for an acute coronary syndrome occurring annually.4–8 In patients with an acute coronary syndrome, a high burden of multimorbidities may complicate therapeutic decision-making and acute and long-term clinical management.9–12 Moreover, even though the prevalence of multimorbidities has been increasing in American adults over time, few recent studies have examined the magnitude of various socio-demographic, and particularly psychosocial, factors in patients hospitalized with an acute coronary syndrome and multiple morbidities.7–9
The objectives of this study were to describe and compare the magnitude of, and socio-demographic and psychosocial characteristics associated with, various cardiac and non-cardiac chronic conditions in three groups of patients: those presenting with 0–1 morbidity, any 2 or 3 multimorbidities, and those who had any 4 or more previously diagnosed multimorbidities among a contemporary cohort of patients hospitalized with an acute coronary syndrome in the Transitions, Risks, and Actions in Coronary Events Center for Outcomes Research and Education (TRACE-CORE)13study, one of 3 centers for Cardiovascular Outcomes Research funded by the National Heart, Lung and Blood Institute.14
Methods and Materials
Details of the study design, patient recruitment, and data collection activities for this longitudinal study have been described previously.13 In brief, TRACE-CORE used a multi-site prospective cohort design to recruit and follow a cohort of 2,174 eligible and consenting adults hospitalized with an acute coronary syndrome at 3 medical centers in Worcester, MA,1 in Macon, GA and 2 in Atlanta, GA.13
Participating study sites served a heterogeneous patient population and were purposely selected to provide a study population with socio-demographic and socioeconomic diversity. Eligible and consenting adults discharged alive from the 6 participating hospitals after an acute coronary syndrome were enrolled between April, 2011 and May, 2013.
Trained study staff abstracted an extensive amount of socio-demographic, clinical, and treatment related data from the medical records of patients hospitalized with an independently validated acute coronary syndrome. Diagnoses of ST-segment elevation myocardial infarction, non- ST-segment elevation myocardial infarction, and unstable angina were made using standardized criteria.15
We included in our analysis the most common multimorbidities previously diagnosed in this patient population, defined as those with a frequency equal or greater to 3%.12,16 Information about the most prevalent, cardiac-related and non-cardiac related chronic conditions was ascertained through the review of hospital medical records. The 8 most prevalent cardiac-related conditions we studied included a prior history of hypertension, hyperlipidemia, type II diabetes, peripheral vascular disease, heart failure, atrial fibrillation, stroke, and valvular heart disease. The 8 most prevalent non-cardiac-related conditions we examined included chronic obstructive pulmonary disease, arthritis, depression, anxiety, cancer, chronic kidney disease, cirrhosis, and anemia. For all multimorbidities, their presence was indicated by documentation in the medical record for the index hospitalization.
Data were gathered about a patient’s general quality of life17 using standardized instruments for the completion of a baseline interview at the time of the patient’s index hospitalization for an acute coronary syndrome at participating medical centers. We also collected information during this extensive baseline interview about a variety of psychosocial factors including cognition,18 depression,19 anxiety,20 measures of perceived stress and social support,21,22 and health literacy and numeracy.23,24 Details of the standardized instruments and questionnaire surveys used to collect information about these factors have been described previously.13
Data Analysis
We categorized patients into having none or any 1, 2, 3, or 4 or more of these chronic conditions. We estimated the overall prevalence of individual morbidities and multiple cardiac-related and non-cardiac related morbidities in this patient population. We calculated a tetrachoric correlation, a type of correlation applicable when both observed variables are dichotomous,25 to determine the more prevalent dyads of morbidities among all the possible combinations of the different multimorbidities studied. Differences in patient demographic and clinical characteristics, psychosocial factors, and hospital length of stay (LOS) according to number of combined multimorbid cardiac and non-cardiac related conditions present were examined using analysis of variance for continuous variables and the chi-square test for categorical variables.
Results
The average age of our study population (n=2,174) was 61.3 years, 67% were men, 81% were white, and 25% had completed college.
Frequency of cardiac and non-cardiac related chronic conditions
In this population, 12.5% of patients had none of the cardiac-related multimorbidities examined, 17.7% had a single such morbidity, 31.5% had exactly two, 23.8% had exactly three, and 14.5% had four or more of the 8 cardiac-related multimorbidities examined. In terms of the 8 non-cardiac multimorbidities, 47.4% of patients had none, 30.3% had any one, 15.5% had two, 5.1% had three, and 1.7% had four or more of the non-cardiac conditions examined. Overall, 800 patients (36.8%) had four or more cardiac/non-cardiac related chronic conditions previously diagnosed.
Several individual cardiac-related chronic conditions were highly prevalent in patients discharged from our 6 participating hospitals after an acute coronary syndrome. Hypertension, hyperlipidemia, and type II diabetes (76%, 69%, and 31%, respectively) were the most commonly identified cardiac-related morbidities (Table 1). Arthritis, chronic pulmonary disease, and depression (20%, 18%, and 13%, respectively) were the most common non-cardiac morbidities.
Table 1.
Frequency of chronic conditions in patients with an acute coronary syndrome: TRACE-CORE
| Cardiac-related morbidities | n (%) |
|---|---|
| Hypertension | 1,652 (76.0) |
| Hyperlipidemia | 1,494 (68.7) |
| Diabetes | 683 (31.4) |
| Heart Failure | 305 (14.0) |
| Peripheral Vascular Disease | 209 (9.6) |
| Atrial Fibrillation | 176 (8.1) |
| Stroke | 116 (5.3) |
| Valvular Heart Disease | 61 (2.8) |
| Non-cardiac morbidities | |
| Arthritis | 433 (19.9) |
| Chronic Obstructive Pulmonary Disease | 389 (17.9) |
| Depression | 275 (12.7) |
| Cancer | 254 (11.7) |
| Chronic Kidney Disease | 236 (10.9) |
| Anxiety | 193 (8.9) |
| Anemia | 107 (4.9) |
| Liver Cirrhosis | 59 (2.7) |
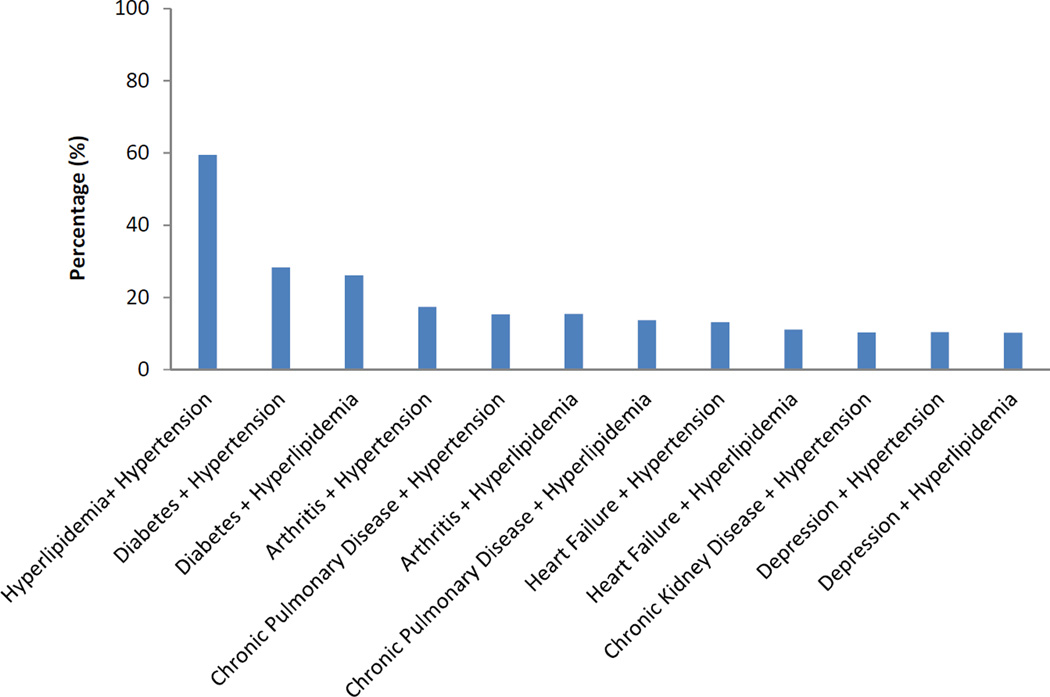
The most common cardiac related dyads present at the time of the underlying acute coronary syndrome were hyperlipidemia and hypertension, diabetes and hypertension, and diabetes and hyperlipidemia (60%, 28%, and 26% of patients presented with these possible chronic conditions, respectively) (Figure 1). Arthritis and chronic pulmonary disease, anxiety and depression, and arthritis and chronic kidney disease (5%, 5%, and 3%, respectively) were the most common non-cardiac-related dyads found. Baseline Socio-Demographic and Clinical Characteristics and Multiple Chronic Conditions
Figure 1.
Dyads of Cardiac and Non-cardiac Related Morbidities in Patients Hospitalized with an Acute Coronary Syndrome by Decreasing Prevalence: TRACE-CORE
Based on our sample distribution, we stratified patients hospitalized with an acute coronary syndrome into three different groups: those presenting with 0–1 morbidity (cardiac-related or non –cardiac condition), any 2 or 3 chronic conditions, and those who had any 4 or more previously diagnosed chronic conditions. Patients with 4 or more cardiac-related or non-cardiac morbidities were slightly older, more likely to be women, and were less likely to be married and currently working as compared to those with 0–1 morbidity (Table 2). Patients who had 4 or more multimorbidites were also heavier and were hospitalized for a longer period of time during their index hospitalization as compared to those with 0–1 morbidity (Table 2).
Table 2.
Socio-demographic and clinical characteristics of patients hospitalized with an acute coronary syndrome according to number of chronic conditions: TRACE-CORE
| Characteristic | 0–1 morbidity (n=472) |
2–3 morbidities (n=902) |
≥4 morbidities (n=800) |
P value (*across 3 categories) |
|---|---|---|---|---|
| Age (years, mean, SD) | 56.2 (11.0) | 61.4 (10.8) | 64.3 (10.9) | 0.98 |
| Male (%) | 350 (74.2) | 612 (67.9) | 484 (60.5) | <0.01 |
| Non-Hispanic white (%) | 399 (84.9) | 728 (81.1) | 627 (78.8)l | 0.15 |
| Married (%) | 285 (60.4) | 551 (61.1) | 433 (54.1) | <0.001 |
| Education (%) | ||||
| High school or less | 205 (43.4) | 396 (43.9) | 409 (51.2) | <0.001 |
| Some college | 125 (26.5) | 261 (28.9) | 240 (30.1) | |
| College graduate | 142 (30.1) | 245 (27.2) | 150 (18.8) | |
| Currently working (%) | 299 (63.4) | 413 (45.8) | 180 (22.5) | <0.001 |
| Body mass index (Kg/m2, mean, SD) | 31.8 (23.0) | 30.9 (12.8) | 33.3 (23.7) | <0.001 |
| Hospital length of stay (days, mean, SD) | 3.8 (3.8) | 6.9 (5.9) | 4.9 (5.1) | <0.001 |
Baseline Psychosocial and Lifestyle Characteristics and Multiple Chronic Conditions
Patients with any 4 or more cardiac-related or non-cardiac related multimorbidities had a higher prevalence of perceived stress, depression, and anxiety, and were more likely to have impaired cognition, a limited social network, and low health literacy and numeracy than those with fewer morbidities at the time of hospitalization for an acute coronary syndrome (Table 3). Patients with 4 or more morbidities were significantly more likely to report a lower quality of life, mental component, as measured by the SF-36 (Table 3).
Table 3.
Psychosocial characteristics of patients hospitalized with an acute coronary syndrome according to number of chronic conditions: TRACE-CORE
| Psychosocial Factors | 0–1 morbidity (n=472) |
2–3 morbidities (n=902) |
≥4 morbidities (n=800) |
P value (*across 3 categories) |
|---|---|---|---|---|
| Alcohol consumption* (%) | ||||
| Moderate | 63 (13.4) | 126 (14.0) | 66 (8.3) | <0.001 |
| Heavy | 68 (14.4) | 89 (9.9) | 51 (6.4) | <0.001 |
| Anxiety (GAD-7)** (%) | ||||
| Mild | 112 (23.7) | 243 (26.9) | 194 (24.2) | 0.20 |
| Moderate/severe | 81 (17.2) | 204 (22.6) | 236 (29.5) | <0.001 |
| Cognitively impaired + (%) | 57 (12.1) | 168 (18.6) | 210 (26.3) | <0.001 |
| Depression (PHQ-9)++ (%) | ||||
| Mild | 94 (20.2) | 253 (28.8) | 219 (28.2) | <0.001 |
| Moderate/severe | 71 (15.1) | 170 (18.9) | 247 (30.9) | <0.001 |
| Low health literacy @ (%), | 147 (31.1) | 306 (34.0) | 331 (41.7) | <0.001 |
| Low health numeracy @@(%) | 198 (42.0) | 422 (46.8) | 433 (54.1) | 0.001 |
| SF-36 mental component, mean (SD) | 50.2 (11.2) | 47.8 (12.3) | 45.4 (13.6) | 0.001 |
| SF-36 physical component, mean (SD) | 46.5 (9.7) | 42.6 (10.2) | 36.4 (10.4) | 0.18 |
| Smoking, current (%) | 151 (32.0) | 190 (21.1) | 166 (20.8) | <0.001 |
| Social Network, Limited &(%) | 72 (15.4) | 127 (14.3) | 170 (21.6) | 0.002 |
| High perceived stress&& (%) | 149 (31.9) | 335 (37.8) | 372 (47.7) | <0.001 |
Moderate alcohol consumption was defined as up to 1 drink per day for women and up to 2 drinks per day for men. Heavy alcohol consumption was defined as drinking 5 or more drinks on the same occasion on each of 5 or more days in the past 30 days.
Anxiety assessed by GAD-7 scoring: 5–9 mild, 10–14 moderate, and ≥15 severe anxiety
Cognitive capacity assessed by the TICS scoring : ≤28 impaired
Depression assessed by the PHQ-9 scoring: 5–9 mild,10–14 moderate, 15–19 moderately severe, and ≥ 20 severe depression
Low Health Literacy was determined by confidence in filling out medical forms answered as “somewhat/a little bit/ not at all”.
Low Health Numeracy was determined by ability to answer both questions on health numeracy correctly.
Social network assessed by the Lubben scale scoring : <=25 limited network
High perceived stress assessed by Perceived Stress Scale scoring: ≥20 high stress
Discussion
In this multi-site observational study approximately 2 out of every 5 patients discharged alive after a hospitalization for an acute coronary syndrome had four or more previously diagnosed morbidities. Patients presenting with multiple chronic conditions were more likely to report stress, depression, and anxiety; these multimorbid patients had a lower quality of life, low health literacy and numeracy, and were more likely to be cognitively impaired than patients with no or just one morbidity.
In terms of the prevalence of chronic conditions, the present results are similar to findings observed in the population-based Worcester Heart Attack Study in which the frequency of multiple cardiovascular morbidities among patients hospitalized with an acute myocardial infarction in all 11 central Massachusetts medical centers between 2003 and 2007 was examined.2,26 Hypertension (75%) and diabetes (35%) were the two most prevalent chronic conditions in this patient population. Our findings in a slightly younger cohort of patients discharged from the hospital after an acute coronary syndrome, about a decade later, are also consistent with the findings from other investigations that have studied patients hospitalized with coronary heart disease, including PROSPER (elderly with established vascular disease, mean age = 75 years), in which 61% of the study sample had hypertension, 11% had diabetes, and 28% were current smokers.27 In the National Registry of Myocardial Infarction, which enrolled almost 2 million patients with an acute myocardial infarction from more than 2,000 U.S. hospitals between 1990 and 2006, dramatic increases in the prevalence of diabetes, hypertension, heart failure, stroke, and hyperlipidemia were observed over the years studied.28
Since the burden of multimorbid diseases is associated with an increased risk of adverse outcomes in patients hospitalized with acute coronary disease, including high in-hospital, 30-day, and 1 year death rates, polypharmacy, and a prolonged hospital stay,1,2,26 it is important to recognize the frequency and importance of these common multimorbidities and take them into consideration when examining differences in hospital and more long-term treatment practices and outcomes in these patients.
Demographic, Clinical, and Psychosocial Correlates of Multimorbidity
In a prior analysis of data from the Worcester Heart Attack Study, older individuals, women, non-married patients, and those developing serious clinical complications of an acute myocardial infarction, including heart failure and atrial fibrillation, were more likely to have presented with multiple cardiovascular and non-cardiovascular chronic conditions than respective comparison groups.2,26 Similarly, researchers at the Cardiovascular Research Network found that older individuals, women, and those with preserved left ventricular ejection fraction findings were more likely to have presented with multiple morbidities than those with a reduced ejection fraction among patients with heart failure.3
Few recent studies have examined the magnitude of, and factors associated with, various psychosocial factors in patients hospitalized with an acute coronary syndrome and multiple chronic conditions.29–31 We found that patients with 4 or more morbidities in our study presented with a higher prevalence of symptoms of moderate/severe depression, anxiety, and a limited social network as compared to those with fewer chronic conditions. Similarly, a cross-sectional study in Australia (n=7,600, mean age=51 years, 66% women) found that the prevalence of depression increased markedly with the number of chronic physical conditions present.29 An observational study of more than 1,400 patients diagnosed with heart failure and multiple chronic medical conditions examined the impact of psychological morbidities on the health care utilization practices of this high risk population.30 Patients presenting with multiple chronic conditions who had a high prevalence of several psychological morbidities, including depression, dementia, and substance abuse, had a significantly higher use of the health care system than those without psychological morbidities. Similarly, in a study of more than 18,000 patients from over 40 general practices in Scotland (mean age=50 years; 49% men), potentially preventable and unplanned admissions to the hospital were highly associated with increasing combinations of various physical and psychosocial conditions.31
Another important finding of our multi-site observational study is that patients with 4 or more multimorbidities had a higher prevalence of low health literacy and numeracy as compared to those with fewer multimorbidities. Other investigators have emphasized the importance of low health literacy and numeracy and their association with poor health outcomes32,33. In a study of more than 300 patients with heart failure (mean age 63 years; 67% women, mean number of morbidities= 3), patients who presented with a higher number of previously diagnosed morbidities, and who had low literacy and numeracy, had greater difficulty in following medication instructions and compliance with medications as compared to those with fewer chronic conditions.32
These findings highlight the importance of screening patients with multiple chronic conditions for various psychosocial factors and suggest the need to tailor behavioral interventions toward the specific clinical and psychosocial characteristics of multimorbid patients who develop an acute coronary syndrome. Indeed, the American College of Cardiology has recently emphasized the consideration of psychosocial factors in practicing patient-centered care with these complex patients.34 Moreover, prior studies suggest a complicated etiological relationship between the development of acute coronary events, multimorbidity, and psychosocial challenges. Many chronic diseases that are independent risk factors for an acute coronary syndrome may also cause stress, depression, anxiety, and functional decline.29–31 Alternatively, the presence of psychosocial difficulties may also precipitate the onset of an acute coronary syndrome.35
Study Strengths and Limitations
The strengths of the present study include its multi-site sample of patients discharged from the hospital after an acute coronary syndrome, its contemporary perspective in examining a number of important cardiac-related and non-cardiac chronic conditions, use of standardized data collection instruments to ascertain various psychosocial, clinical, and other patient characteristics, and rigorous quality control measures. Several limitations need to be acknowledged, however. Since 81% of our study participants were white, and were hospitalized in a limited number of geographic settings in Massachusetts and Georgia, the generalizability of our findings to other race/ethnic groups and geographic settings may be limited. Still, we included a substantial proportion of under-represented minorities, and examined teaching and nonteaching hospitals in very different regions. The presence of the various multimorbidities examined was based on the review of data contained in hospital medical records and there could be some degree of misclassification and underestimation of some of the information recorded. Also, information was unavailable on the duration or severity of each of the chronic conditions examined. Of note, we used the PHQ-9 and GAD-7 scales collected during in-person interviews to identify symptoms of depression and anxiety, covering the 2 weeks prior to hospitalization, as established by the PHQ-9 and GAD-7 scales. We did not, however, use these scales to identify depression or anxiety as pre-existing morbidities, which were ascertained by medical record review. We perceive a chronic diagnosis of depression or of anxiety as a different construct from current symptoms of depression or anxiety at a given time, with possibly transient symptoms perhaps being more likely at the time of an acute event. Thus, we analyzed chronic conditions as entities that are distinct from current symptoms.
Conclusions
In this study of nearly 2,200 patients discharged from the hospital after an acute coronary syndrome in 6 medical centers in central Massachusetts and Georgia, we observed a high prevalence of multiple cardiac-related and non-cardiac chronic conditions. Multimorbidity was strongly associated with measures of psychosocial impairment and worse quality of life. Given the aging U.S. population, the multimorbidity burden in patients with an acute coronary syndrome will likely continue to increase during coming years. Our results emphasize the challenge and complex nature of caring for these patients, which extends well beyond the optimal management of their underlying coronary heart disease.
Multimorbidities are highly prevalent in patients hospitalized with an ACS
Hospitalized ACS patients with multimorbidities presented psychosocial deprivation
Future interventions focusing on psychosocial factors may benefit these patients
Acknowledgement
We are indebted to the trained study staff at each of our participating study sites in Worcester, MA, Macon, GA, and Atlanta, GA.
Funding Source
TRACE-CORE was supported by NIH grant U01HL105268.
Dr. Tisminetzky is funded by the National Heart, Lung, and Blood Institute Diversity Supplement R01 HL35434-29 and by the 1R24AG045050 from the National Institute on Aging, Advancing Geriatrics Infrastructure & Network Growth (AGING).
Dr. McManus is supported by NIH award 1R15HL121761 and KL2RR031981.
Dr. Saczynski is supported by award number K01AG033643 from the National Institute of Aging.
Dr. Gurwitz is supported by award number 1R24AG045050 from the National Institute on Aging, Advancing Geriatrics Infrastructure & Network Growth (AGING).
Dr. Waring is supported by NIH grant KL2TR000160.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
There are no conflicts of interest with any of the authors to report.
All authors had access to the data and had a role in writing this manuscript.
References
- 1.Ward BW, Schiller JS. Prevalence of Multiple Chronic Conditions Among US Adults: Estimates From the National Health Interview Survey, 2010. Preventing chronic disease. 2013;10:E65. doi: 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McManus DD, Nguyen HL, Saczynski JS, Tisminetzky M, Bourell P, Goldberg RJ. Multiple cardiovascular comorbidities and acute myocardial infarction: temporal trends (1990–2007) and impact on death rates at 30 days and 1 year. Clin Epidemiol. 2012;4:115–123. doi: 10.2147/CLEP.S30883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saczynski JS, Go AS, Magid DJ, et al. Patterns of comorbidity in older adults with heart failure: the Cardiovascular Research Network PRESERVE study. J Am Geriatr Soc. 2013;61(1):26–33. doi: 10.1111/jgs.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johns Hopkins School of Public Health. Chronic Conditions: Making the Case for Ongoing Care 2010. Available at: www.rwjf.org/pr/product.jsp?id=50968. [Google Scholar]
- 4.Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303:1303–1304. doi: 10.1001/jama.2010.381. [DOI] [PubMed] [Google Scholar]
- 5.Van den Akker M, Buntinx F, Roos S, Knottnerus JA. Problems in determining occurrence rates of multimorbidity. J Clin Epidemiol. 2001;54:675–679. doi: 10.1016/s0895-4356(00)00358-9. [DOI] [PubMed] [Google Scholar]
- 6.FASTSTATS. [Page last reviewed: January 9, 2015]; Heart Disease: http://www.cdc.gov/nchs/fastats/heart.htm.
- 7.Maeder MT. Comorbidities in patients with acute coronary syndrome: rare and negligible in trials but common and crucial in the real world. Heart. 2014;100(4):268–270. doi: 10.1136/heartjnl-2013-305104. [DOI] [PubMed] [Google Scholar]
- 8.Uijen A, Lisdonk E. Multimorbidity in primary care: prevalence and trend over the last: 20 years. Eur J Gen Pract. 2008;1:28–32. doi: 10.1080/13814780802436093. [DOI] [PubMed] [Google Scholar]
- 9.Salisbury C, Johnson C, Purdy S, Valderas JM, Montgomery A. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;582:e12. doi: 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lugtenberg M, Burgers JS, Clancy C, Westert GP, Schneider EC. Current guidelines have limited applicability to patients with comorbid conditions: a systematic analysis of evidence-based guidelines. PLoS One. 2011;6(10):e2598. doi: 10.1371/journal.pone.0025987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boyd CM, Leff B, Wolff JL, et al. Informing clinical practice guideline development and implementation: prevalence of coexisting conditions among adults with coronary heart disease. J Am Geriatr Soc. 2011;59(5):797–805. doi: 10.1111/j.1532-5415.2011.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marengoni A, Winblad B, Karp A, et al. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. 2008;98:1198–1200. doi: 10.2105/AJPH.2007.121137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waring ME, McManus RH, Saczynski JS, et al. TRACE-CORE Investigators. Transitions, Risks, and Actions in Coronary Events Center for Outcomes Research and Education (TRACE-CORE): design and rationale. Circ Cardiovasc Qual Outcomes. 2012;5(5):e44–e50. doi: 10.1161/CIRCOUTCOMES.112.965418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cook NL, Bonds DE, Kiefe CI, et al. National Heart, Lung, and Blood Institute Centers for Cardiovascular Research (CCOR) Writing Group. Circ Cardiovasc Qual Outcomes. 2013;6:223–228. [Google Scholar]
- 15.Thygesen K, Alpert JS, Jaffe AS, et al. Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 16.Marengoni A, Rizzuto D, Wang H-X, et al. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57:225–230. doi: 10.1111/j.1532-5415.2008.02109.x. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 18.Brandt J, Spencer M, Folstein M. The telephone interview for cognitive status. Neuropsychiatry Neuropsychol. Behav. Neurol. 1988;1:111–117. [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 21.Cohen S, Williamson GM. Chapter 3: perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- 22.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46:503–513. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- 23.Powers BJ, Trinh JV, Bosworth HB. Can this patient read and understand written health information? JAMA. 2010;304:76–84. doi: 10.1001/jama.2010.896. [DOI] [PubMed] [Google Scholar]
- 24.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 25.Kessler R, Chiu W, Demler O, Walters E. Prevalence, Severity, and Comorbidity of Twelve-month DSM-IV Disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen H-Y, Saczynski JS, McManus DD, et al. The impact of cardiac and noncardiac comorbidities on the short-term outcomes of patients hospitalized with acute myocardial infarction: a population-based perspective. Clinical Epidemiology. 2013;5:439–448. doi: 10.2147/CLEP.S49485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): A randomised controlled trial. Lancet. 2002;360(9346):1623–1630. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 28.Rogers WJ, Frederick PD, Stoehr E, et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156(6):1026–1034. doi: 10.1016/j.ahj.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 29.Gunn JM, Ayton DR, Densley K, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):175–184. doi: 10.1007/s00127-010-0330-z. [DOI] [PubMed] [Google Scholar]
- 30.Chamberlain AM, St Sauver JL, Gerber Y, et al. Multimorbidity in heart failure: a community perspective. Am J Med. 2015;128(1):38–45. doi: 10.1016/j.amjmed.2014.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Payne RA, Abel GA, Guthrie B, Mercer SW. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ. 2013;185(5):E221–E228. doi: 10.1503/cmaj.121349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morrow D, Clark D, Tu W, Wu J, Weiner M, Steinley D, Murray MD. Correlates of health literacy in patients with chronic heart failure. Gerontologist. 2006 Oct;46(5):669–676. doi: 10.1093/geront/46.5.669. [DOI] [PubMed] [Google Scholar]
- 33.Schillinger D, Grumbach K, Piette J, et al. Association of Health Literacy With Diabetes Outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 34.Walsh M, Bove AA, Cross RR, et al. ACCF 2012 Health Policy Statement on Patient-Centered Care in Cardiovascular Medicine A Report of the American College of Cardiology Foundation Clinical Quality Committee. Journal of the American College of Cardiology. 2012;59:2125–2143. doi: 10.1016/j.jacc.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460–1467. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]