Abstract
Background: There is evidence that body mass index (BMI) is closely related to hyperlipidemia. This study aimed to estimate the cross-sectional relationship between Body Mass Index (BMI) and hyperlipidemia. Methods: We recruited 21,435 subjects (aged 18–79 years and residing in Jilin province, China) using the multistage stratified cluster random sampling method. Subjects were interviewed with a standardized questionnaire and physically examined. We analyzed the cross-sectional relationship between BMI and hyperlipidemia. Results: The prevalence of hyperlipidemia was 51.09% (52.04% in male and 50.21% in female). The prevalence of overweight and obesity was 31.89% and 6.23%, respectively. Our study showed that underweight (OR = 0.499, 95% CI: 0.426–0.585), overweight (OR = 2.587, 95% CI: 2.428–2.756), and obesity (OR = 3.614, 95% CI: 3.183–4.104) were significantly associated with hyperlipidemia (p < 0.001) in the age- and sex-adjusted logistic regression. After further adjusting for age, gender, region, district, ethnicity, education, marital status, main occupation, monthly family income per capita, smoking, drinking, exercise, central obesity, waist and hip, underweight (OR = 0.729, 95% CI: 0.616–0.864), overweight (OR = 1.651, 95% CI: 1.520–1.793), and obesity (OR = 1.714, 95% CI: 1.457–2.017) were independently associated with hyperlipidemia (p < 0.001). The restricted cubic spline model illustrated a nonlinear dose-response relationship between levels of BMI and the prevalence of hyperlipidemia (Pnonlinearity < 0.001). Conclusion: Our study demonstrated that the continuous variance of BMI was significantly associated with the prevalence of hyperlipidemia.
Keywords: hyperlipidemia, BMI, relationship
1. Introduction
Hyperlipidemia, a major systemic disorder, is an important modifiable risk factor for coronary heart disease and extra-coronary atherosclerosis [1,2] and associated with a higher risk of cardiovascular disease (CVD), which is a leading contributor to mortality worldwide, particularly in China [3]. Estimates from the World Health Organization (WHO) suggested that CVDs contributed to approximately 17.5 million individuals deaths in 2012 [4].
Moreover, hyperlipidemia is commonly associated with obesity which is known as a risk factor for CVD [5,6]. Converging lines of evidence suggests that hyperlipidemia is associated with a high BMI [7,8]. Around 3.4 million adults deaths, 3.9% of years of life lost and 3.8% of disability-adjusted life-years (DALYs) each year worldwide, were attributed to overweight or obese [9]. BMI is currently the most widely used anthropometric measurement to predict health risk related to weight status, and a large number of studies have reported a significant relationship between BMI and hyperlipidemia [10]. However, previous studies converted BMI into categorical variables when performing the multivariate analysis.
In the present study, we examined the nonlinear dose-response relationship between the continuous variance of BMI and the prevalence of hyperlipidemia. As an intuitive method for presenting data, the restricted cubic spline has been widely used in the field of meta-analysis and other researches [11,12,13].
2. Experimental Section
2.1. Study Population
Our study was conducted in the framework of the Project on Present Situation and Change Forecast of Disease Spectrum in Jilin Province, China. It was supported by the Bureau of Public Health of Jilin Province, China. A total of 21,435 participants (community-dwelling residents aged 18 to 79 years) were enrolled from June 2012 to August 2012 and completed the survey. Subjects with incomplete blood lipid information were excluded. Our study adopted a multistage stratified cluster random sampling method, with the sample selected from all nine administrative regions in Jilin Province. The details of the sampling process were published elsewhere [14].
We stuck to the bioethics principles of the Declaration of Helsinki, and our study was authorized by the Ethics Committee of Jilin University School of Public Health (Reference Number: 2012-R-011) and the Bureau of Public Health of Jilin Province(Reference Number: 2012-10). All participants voluntarily joined this study with informed consents.
2.2. Data Collection and Measurements
Our study adopted a structured pre-coded personal health survey questionnaire compiled by the Bureau of Public Health of Jilin Province united with the School of Public Health of Jilin University and the Jilin Disease Prevention and Control Information Platform. Participants were interviewed in a face-to-face manner by specially trained researchers. The collected information included demographic characteristics (region, age, gender, level of education and main occupation), lifestyles (smoking, drinking and exercise), history of hyperlipidemia in the past one year, and current treatment of hyperlipidemia.
In the light of the standard protocols and techniques, the participants went through anthropometric examinations including height, weight, waist, and hip circumference measurements by a trained certified research practitioner. Participants with light-colored clothing were measured for their weight as well as waist and hip circumference early in the morning after the food-intake. They were measured for heights after taking shoes off. Each physical measurement was completed by two research assistants.
Fasting venous blood samples of each participant were extracted by venipuncture for measuring the levels of blood lipids, including total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG). Blood lipids were measured using the MODULE P800 automated biochemistry analyzer (ROCHE Diagnostics Ltd., Indianapoils, IN, USA) in a core laboratory with a standard protocol.
2.3. Definitions
In terms of the Chinese guidelines on the prevention and treatment of dyslipidemia in adults (2007) [15], hyperlipidemia was defined as total cholesterol (TC ≥ 5.18 mmol/L), and/or low-density lipoprotein cholesterol (LDL-C ≥ 3.37 mmol/L), and/or high-density lipoprotein cholesterol (HDL-C < 1.04 mmol/L), and/or triglycerides (TG ≥ 1.70 mmol/L), and/or with history of hyperlipidemia diseases in the past one year. BMI was defined as a person’s weight in kilograms divided by the square of his/her height in meters (kg/m2). Our study categorized adults as: Underweight with BMI < 18.5 kg/m2,normal weight with 18.5 ≤ BMI < 24 kg/m2, overweight with 24 ≤ BMI < 30 kg/m2,and obese with BMI ≥ 30 kg/m2 [16]. Central obesity was defined as the waist circumference ≥85 cm for man or ≥80 cm for woman [17]. The smoking status was categorized into current smoker (smoking at least 100 cigarettes in their lifetime and smoking daily or during the time of the survey), former smoker (smoking at least 100 cigarettes in their lifetime but not smoking at the time of the survey),and non-smoking (never smoked or smoked less than 100 cigarettes in their lifetime) [18]. A drinker was defined as a person who consumed more than one alcoholic drink weekly on average, either spirits, beer, wine, or other forms of alcohol. Participants who exercised one or two times a week were classified as “sometimes exercise”; those who exercised more than three times a week were classified as “often exercise”; and those who do not or seldom exercise were classified as “never or rarely exercise”. Psychological distress was evaluated using the 12-item general health questionnaire (GHQ-12) which has been widely used in China [19]. All participants were sorted into two groups with a cut-point of 4 on a 0–12 point with those scoring 4 or more being deemed as being in psychological distress [20].
2.4. Statistical Analysis
For database management and statistical analysis, we used the Epidata software (version 3.1, Odense, Denmark) and the SPSS software (version 21.0, IBM SPSS, IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test was used to analyze for normality. The distributions of demographic characteristics between participants with and without hyperlipidemia were calculated by Chi-square tests for categorical variables or computed by the Wilcoxon signed-rank test for continuous variables if not following normal distributions. We used the adjusted logistic regression model to individually analyze the correlations of BMI and hyperlipidemia and the restricted cubic spline method was evaluated a potential non-linear relationship between BMI and hyperlipidemia [21,22,23]. Restricted cubic spline was implemented by the Stata software (version 12.0, Stata Press, College Station, TX, USA).Variables that were statistically significant at p < 0.05 level were entered into multivariate logistic regression analyses. All statistical tests were two-tailed and p < 0.05 was considered statistically significant.
3. Results
The prevalence of hyperlipidemia among residents on Jilin Province was 51.09% (10,951/21,435), with 52.04% in males and 50.21% in females. The prevalences of overweight and obesity were respectively 31.89% and 6.23%, with a slightly higher prevalence of both overweight and obesity in women than men (overweight:16.10% vs. 15.78%; obesity:3.28% vs. 2.95%).
Table 1 shows demographic characteristics of participants. Hyperlipidemia was significantly correlated with gender (p = 0.007), region (p < 0.001), district (p < 0.001), ethnicity (p = 0.047), education (p < 0.001), marital status (p < 0.001), main occupation (p < 0.001), monthly family income per capita (p < 0.001), smoking (p < 0.001), drinking (p < 0.001), exercise (p < 0.001), and central obesity (p < 0.001). However, subjects with or without hyperlipidemia did not show significant differences in family history of hyperlipidemia and GHQ-12 (p > 0.05). Table 2 presents that the age, BMI, and waist and hip circumferences of participants with hyperlipidemia were significant higher than those without hyperlipidemia (all p < 0.001).
Table 1.
Demographic characteristics of adult samples (n = 21,435).
| Variable | n | Hyperlipidemia | Non-Hyperlipidemia | χ2 | p | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Gender | 7.166 | 0.007 | |||||
| Female | 11,098 | 5572 | 50.9 | 5526 | 52.7 | ||
| Male | 10,337 | 5379 | 49.1 | 4958 | 47.3 | ||
| Region | 18.788 | <0.001 | |||||
| Urban | 11,152 | 5539 | 50.6 | 5613 | 53.5 | ||
| Rural | 10,283 | 5412 | 49.4 | 4871 | 46.5 | ||
| District | 136.344 | <0.001 | |||||
| Middle | 13,322 | 6433 | 58.7 | 6889 | 65.7 | ||
| East | 4104 | 2171 | 19.8 | 1933 | 18.4 | ||
| West | 4009 | 2347 | 21.4 | 1662 | 15.9 | ||
| Ethnicity | 3.950 | 0.047 | |||||
| Han | 19,865 | 10,111 | 92.3 | 9754 | 93.0 | ||
| Other | 1570 | 840 | 7.7 | 730 | 7.0 | ||
| Education | 134.481 | <0.001 | |||||
| Primary school or below | 6236 | 3440 | 31.4 | 2796 | 26.7 | ||
| Junior high school | 6125 | 3069 | 28.0 | 3056 | 29.1 | ||
| Senior high school | 5559 | 2921 | 26.7 | 2638 | 25.2 | ||
| College and above | 3515 | 1521 | 13.9 | 1994 | 19.0 | ||
| Marital status | 455.081 | <0.001 | |||||
| Married or cohabit | 18,316 | 9613 | 87.8 | 8703 | 83.0 | ||
| Never married | 1693 | 470 | 4.3 | 1223 | 11.7 | ||
| Divorced | 388 | 201 | 1.8 | 187 | 1.8 | ||
| Widowed | 1038 | 667 | 6.1 | 371 | 3.5 | ||
| Main occupation | 425.563 | <0.001 | |||||
| Unemployed | 2653 | 1482 | 13.5 | 1171 | 11.2 | ||
| Mental workers | 4369 | 1973 | 18.0 | 2396 | 22.9 | ||
| Manual workers | 12,046 | 5858 | 53.5 | 6188 | 59.0 | ||
| Retired | 2367 | 1638 | 15.0 | 729 | 7.0 | ||
| Average monthly earnings a | 59.992 | <0.001 | |||||
| <500 | 4304 | 2350 | 21.5 | 1954 | 18.6 | ||
| 500~ | 3959 | 2059 | 18.8 | 1900 | 18.1 | ||
| 1000~ | 7049 | 3628 | 33.1 | 3421 | 32.6 | ||
| 2000~ | 3983 | 1945 | 17.8 | 2038 | 19.4 | ||
| 3000~ | 2140 | 969 | 8.8 | 1171 | 11.2 | ||
| Smoking | 99.722 | <0.001 | |||||
| Never smoked | 12,992 | 6307 | 57.6 | 6685 | 63.8 | ||
| Former smoker | 6723 | 3628 | 33.1 | 3095 | 29.5 | ||
| Current smoker | 1720 | 1016 | 9.3 | 704 | 6.7 | ||
| Drinking | 15.127 | <0.001 | |||||
| No | 14,607 | 7330 | 66.9 | 7277 | 69.4 | ||
| Yes | 6828 | 3621 | 33.1 | 3207 | 30.6 | ||
| Exercise | 165.482 | <0.001 | |||||
| Often | 6386 | 3689 | 33.7 | 2697 | 25.7 | ||
| Sometimes | 5220 | 2467 | 22.5 | 2753 | 26.3 | ||
| Never or rarely | 9829 | 4795 | 43.8 | 5034 | 48.0 | ||
| Central obesity | 1730.612 | <0.001 | |||||
| No | 10,766 | 3978 | 36.3 | 6788 | 64.7 | ||
| Yes | 10,669 | 6973 | 63.7 | 3696 | 35.3 | ||
| Family history b | 2.202 | 0.138 | |||||
| No | 20,494 | 10,448 | 95.4 | 10,046 | 95.8 | ||
| Yes | 941 | 503 | 4.6 | 438 | 4.2 | ||
| GHQ-12 | 0.586 | 0.444 | |||||
| No distress | 16,356 | 8380 | 76.5 | 7976 | 76.1 | ||
| Distress | 5079 | 2571 | 23.5 | 2508 | 23.9 | ||
| Diabetes | |||||||
| No | 19,479 | 9480 | 86.6 | 9999 | 95.4 | 500.924 | <0.001 |
| Yes | 1956 | 1471 | 13.4 | 485 | 4.6 | ||
| Hypertension | |||||||
| No | 13,924 | 5936 | 54.2 | 7988 | 76.2 | 1137.581 | <0.001 |
| Yes | 7511 | 5015 | 45.8 | 2496 | 23.8 | ||
a means monthly family income per capita; b means family history of hyperlipidemia.
Table 2.
Distribution of age, BMI, waist and hip circumferences between participants with and without hyperlipidemia ((n = 21,435), M (Q1–Q3)).
| Variable | Hyperlipidemia (n = 10,951) | Non-Hyperlipidemia (n = 10,484) | Z | p |
|---|---|---|---|---|
| Age (years) | 51 (42–59) | 43 (33–53) | −37.421 | <0.001 |
| BMI (kg/m2) | 25.029 (22.823–27.3995) | 22.977 (20.727–25.044) | −42.684 | <0.001 |
| Waist (cm) | 85.300 (79.000–92.000) | 79.000 (72.000–85.000) | −46.686 | <0.001 |
| Hip (cm) | 96.000 (92.000–101.000) | 94.000 (89.000–97.475) | −29.716 | <0.001 |
As shown in Table 3, BMI levels were significantly associated with hyperlipidemia via unadjusted logistic regression (p < 0.001). In the age- and gender-adjusted logistic regression, our survey observed that there was a significant correlation between different BMI ranges and hyperlipidemia (p < 0.001). Underweight (OR = 0.729, 95% CI: 0.616–0.864) was associated with a lower prevalence of hyperlipidemia and overweight (OR = 1.651, 95% CI: 1.520–1.793), and obesity (OR = 1.714, 95% CI: 1.457–2.017) were independently associated with increased risks of hyperlipidemia (p < 0.001) after adjustment for age, gender, region, district, ethnicity, education, marital status, main occupation, monthly family income per capita, smoking, drinking, exercise, central obesity, and waist and hip circumferences. In further analyses, we found a significant trend between BMI and the presence of hyperlipidemia in the univariate model, model I (adjusted age and gender), and model II (adjusted age, gender, region, district, ethnicity, education, marital status, main occupation, monthly family income per capita, smoking, drinking, exercise, central obesity, and waist and hip circumferences) (all p < 0.001).
Table 3.
Logistic regression analyses of the influence of BMI on hyperlipidemia prevalence.
| Model | BMI | B c | S.E. d | Wald | p | OR (95% CI) |
|---|---|---|---|---|---|---|
| Univariate | <18.5 | −0.792 | 0.078 | 104.196 | <0.001 | 0.453 (0.389–0.527) |
| 18.5~ | 1.000 | |||||
| 24.0~ | 1.008 | 0.031 | 1025.644 | <0.001 | 2.741 (2.577–2.916) | |
| 30.0~ | 1.233 | 0.063 | 379.395 | <0.001 | 3.430 (3.030–3.883) | |
| p value for trend p < 0.001 | ||||||
| Model I a | <18.5 | −0.695 | 0.081 | 73.860 | <0.001 | 0.499 (0.426–0.585) |
| 18.5~ | 1.000 | |||||
| 24.0~ | 0.951 | 0.032 | 865.523 | <0.001 | 2.587 (2.428–2.756) | |
| 30.0~ | 1.285 | 0.065 | 393.025 | <0.001 | 3.614 (3.183–4.104) | |
| p value for trend p < 0.001 | ||||||
| Model II b | <18.5 | −0.316 | 0.086 | 13.337 | <0.001 | 0.729 (0.616–0.864) |
| 18.5~ | 1.000 | |||||
| 24.0~ | 0.501 | 0.042 | 142.217 | <0.001 | 1.651 (1.520–1.793) | |
| 30.0~ | 0.539 | 0.083 | 42.235 | <0.001 | 1.714 (1.457–2.017) | |
| p value for trend p < 0.001 | ||||||
a Adjusted age and gender; b Adjusted age, gender, region, district, ethnicity, education, marital status, main occupation, monthly family income per capita, smoking, drinking, exercise, central obesity, waist, hip; c B represents the logistics regression coefficient; d S.E. represents the standard error.
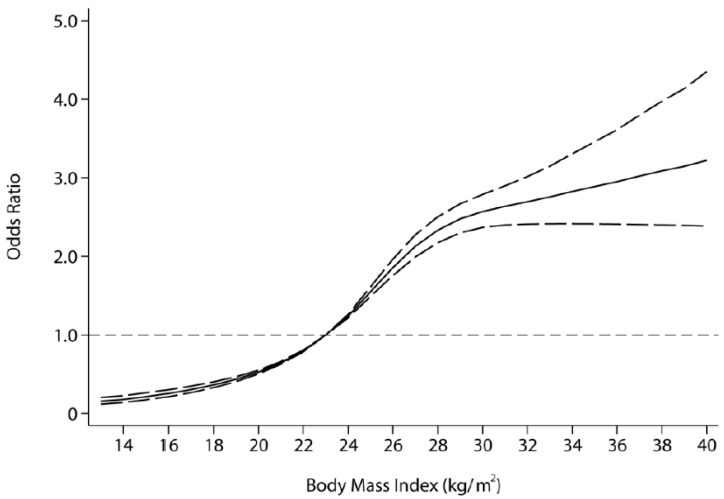
The fitted dose-response relationship is depicted in Figure 1. Overall, we found a significant nonlinear dose-response association between BMI and risk of hyperlipidemia (p value for nonlinearity <0.001) with a significantly increased trend of odds ratio as per 1 kg/m2 increase in BMI, adjusted for age, waist and hip circumferences, gender, ethnicity, education, smoking, drinking. When compared with the reference (median level of the normal BMI range, approximately BMI = 23 kg/m2), the ORs (95% CI) for hyperlipidemia risks were 0.36 (0.33–0.40) for BMI at 18 kg/m2, 1.55 (1.49–1.61) for BMI at 25 kg/m2, and 2.57 (2.37–2.79) for BMI at 30 kg/m2, indicating a significant and progressive risk of hyperlipidemia along with BMI increases.
Figure 1.
The dose-response relationship of BMI and hyperlipidemia based on the restricted cubic spline model (BMI was coded using an RCS function with four knots located at the 17.71 kg/m2, 22.50 kg/m2, 26.83 kg/m2 and 31.52 kg/m2, which respectively correspond to four sections of the median BMI. Lines with long dashes represent the pointwise 95% confidence intervals, comparing for solid lines representing the fitted nonlinear trend).
4. Discussion
Our study showed that there was a significant correlation between different BMI ranges and hyperlipidemia (p < 0.001). Overweight (OR = 1.651, 95% CI: 1.520–1.793), and obesity (OR = 1.714, 95% CI: 1.457–2.017) were independently associated with increased risks of hyperlipidemia (p < 0.001) after adjustment for confounding factors. Furthermore, the dose–response analysis indicated a significant nonlinear association between BMI and the risk of hyperlipidemia, with a significantly increased trend of odds ratio as per 1 kg/m2 increase in BMI. The ORs (95% CI) for hyperlipidemia risks were 0.36 (0.33–0.40) for BMI at 18 kg/m2, 1.55 (1.49–1.61) for BMI at 25 kg/m2, and 2.57 (2.37–2.79) for BMI at 30 kg/m2, indicating a significant and progressive risk of hyperlipidemia along with BMI increases.
To our knowledge, this is the first report concerning the prevalence of hyperlipidemia in Jilin Province, northeast China. The prevalence of hyperlipidemia estimated by our study (total: 51.09%; females: 50.21%; males: 52.04%) was comparable to figures reported in published studies [24]. A previous study using data from administrative officers, who took part in annual regular physical examination from 1 September to 30 November in 1999, reported that the prevalence of hyperlipidemia in Shanghai among participants was 28.9% [25]. Considering that Shanghai is the biggest economic center of China, and one of the richest regions in China, the results of the study conducted with subjects from Shanghai may not be consistent with those from other studies. Compared to studies that examined the prevalence of hyperlipidemia among subjects from the Southwestern China, our results were similar with that reported by Deng et al. [26] (the prevalence of hyperlipidemia: 49.3%), but contradicted with the result of the study conducted by Yin et al. [27], who reported that the prevalence of hyperlipidemia was 35.91% in the Guangxi Zhuang Autonomous Region. Due to the inequality of development and large differences in lifestyles among subjects from different regions of China, the prevalence of hyperlipidemia may have contradictory results. Given that the diet of Chinese people in northeast China, with high salt and high fat content, is different from other parts of the Chinese population, our findings will be meaningful, and enable us to provide a theoretical basis when the government departments make relevant policies.
As we know, modification of excessive body weight (BMI of 27 or higher) is associated with a decreased risk of hyperlipidemia [28]. However, it is unclear whether the relationship between BMI and hyperlipidemia presented in a nonlinear trend, such as a U shaped pattern which was recognized between sleep duration and the risk of type 2 diabetes [29]. The present study demonstrated a nonlinear dose-response relationship between BMI and hyperlipidemia. The dose-response relationship has been reported in many studies [30]. For example, Friedrich et al. [31] reporteda U-shaped relationship between serum ferritin levels and the risk of CVD as well as IHD in women. Weiner et al. [32] also reported such a relationship between each of the non-traditional risk factor and outcomes using restricted cubic splines with four knots generated using S-Plus.
With the rapid economic development and urbanization process in China, the Chinese people have been experiencing tremendous nutritional transition and a big change in lifestyles [33]. Meanwhile, serum total cholesterol (TC) and low-density lipoprotein (LDL) levels of the Chinese peoplehave gradually increased in the past 10 years [34]. Therefore, our findings may have public health implications. Since obesity (BMI is 30 or higher) is an independent risk factor of hyperlipidemia, the intervention for obesity is very necessary for the Chinese people. It is well-known that healthy diets and physical activities are key to controlling the occurrence of obesity and hyperlipidemia. Therefore, we should adopt necessary measures such as replacing trans fats with unsaturated fats, implementing public awareness programs on diet and physical activity, and increasing the consumption of fruits and vegetables, to reduce trends in BMI and serum cholesterol. Furthermore, the Chinese government should pay attention to lipid-related diseases, increase investment for obesity and hyperlipidemia research, strengthen the primary health care system, inform the harm of the lipid-related disease and perform hyperlipidemia prevention and treatment [35].
Our study was subject to the following potential limitations. First, the cross-sectional nature of our study design may not allow us draw definite conclusions about a cause-and-effect relationship. However, since lifestyle behaviors and demographic characteristics for our respondents were relatively stable, our results should be considered to be reliable for policy-making. Second, due to the fact that our study did not take into account the study’s complex sampling design, our samples were not representative of adults (aged 18 to 79 years) of Jilin Province in 2012. Therefore, our results merely reflected the relationship between BMI and hyperlipidemia. Finally, our study design adapted the WHO standard of BMI classification rather than the Chinese standard, which enables us to compare with the results of other studies.
5. Conclusions
The results from the present study suggest that the continuous variance of BMI is significantly associated with the prevalence of hyperlipidemia. Particularly, our study indicates a dose-response nonlinear relationship between BMI and hyperlipidemia, with a significantly increased trend of odds ratio as per 1 kg/m2 increase in BMI. Our findings may guide the government in developing approaches to prevent hyperlipidemia and improving the healthy lifestyles of people.
Acknowledgments
The authors would like to thank Yuepingshen in the Department of Epidemiology and Biostatistics, School of Public Health, Suzhou University and Wenbin Hu in the center for Disease Prevention and control of Kunshan, Suzhou for their guidance in drawing restricted cubic spline. Special thanks go to Huiping Zhang from Yale University for their critical reading of this paper. The authors’ study was financed by the Scientific Research Foundation of the Health Bureau of Jilin Province, China (Grant Number: 2011Z116) and the Norman Bethune Program of Jilin University (Grant Number: 2015227).
Author Contributions
Wenwang Rao, Yingying Su, Yaqin Yu, and Qiong Yu designed the study. Wenwang Rao, Guang Yang, Yue Ma, Shibin Wang, Rui Liu, Shangchao Zhang, and Yingli Fu performed the study. Wenwang Rao analyzed the data and drafted the manuscript, Changgui Kou, Yaqin Yu, and Qiong Yu participated in revising the manuscript. All authors approved the final manuscript.
Conflict of Interest
The authors declare no conflict of interests.
References
- 1.Fischer S., Schatz U., Julius U. Practical recommendations for the management of hyperlipidemia. Atheroscler. Suppl. 2015;18:194–198. doi: 10.1016/j.atherosclerosissup.2015.02.029. [DOI] [PubMed] [Google Scholar]
- 2.Upadhyay U.D., Waddell E.N., Young S., Kerker B.D., Berger M., Matte T., Angell S.Y. Prevalence, awareness, treatment, and control of high LDL cholesterol in New York city, 2004. Prev. Chronic Dis. 2010;7:A61. [PMC free article] [PubMed] [Google Scholar]
- 3.Murray C.J., Lopez A.D. Mortality by cause for eight regions of the world: Global burden of disease study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Cardiovascular Diseases (CVDs) WHO; Geneva, Switzerland: 2015. Fact Sheet No.317. [Google Scholar]
- 5.Ito H., Nakasuga K., Ohshima A., Sakai Y., Maruyama T., Kaji Y., Harada M., Jingu S., Sakamoto M. Excess accumulation of body fat is related to dyslipidemia in normal-weight subjects. Int. J. Obes. 2004;28:242–247. doi: 10.1038/sj.ijo.0802528. [DOI] [PubMed] [Google Scholar]
- 6.McGee D.L., Collaboration D.P. Body mass index and mortality: A meta-analysis based on person-level data from twenty-six observational studies. Ann. Epidemiol. 2005;15:87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Brown C.D., Higgins M., Donato K.A., Rohde F.C., Garrison R., Obarzanek E., Ernst N.D., Horan M. Body mass index and the prevalence of hypertension and dyslipidemia. Obes. Res. 2000;8:605–619. doi: 10.1038/oby.2000.79. [DOI] [PubMed] [Google Scholar]
- 8.Kawada T. Body mass index is a good predictor of hypertension and hyperlipidemia in a rural Japanese population. Int. J. Obes. Relat. Metab. Disord. 2002;26:725–729. doi: 10.1038/sj.ijo.0801984. [DOI] [PubMed] [Google Scholar]
- 9.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C., Abera S.F. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song X., Jousilahti P., Stehouwer C., Söderberg S., Onat A., Laatikainen T., Yudkin J., Dankner R., Morris R., Tuomilehto J. Comparison of various surrogate obesity indicators as predictors of cardiovascular mortality in four European populations. Eur. J. Clin. Nutr. 2013;67:1298–1302. doi: 10.1038/ejcn.2013.203. [DOI] [PubMed] [Google Scholar]
- 11.Bhaskaran K., Douglas I., Forbes H., dos-Santos-Silva I., Leon D.A., Smeeth L. Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5.24 million UK adults. Lancet. 2014;384:755–765. doi: 10.1016/S0140-6736(14)60892-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jianfeng L., Huan J., Baoyue L. The application of restricted cubic spline in nonlinear regression. Chin. J. Health Stat. 2010;3:001. [Google Scholar]
- 13.Orsini N., Bellocco R., Greenland S. Generalized least squares for trend estimation of summarized dose-response data. Stata J. 2006;6:40. [Google Scholar]
- 14.Wang S.B., D’Arcy C., Yu Y.Q., Li B., Liu Y.W., Tao Y.C., Wu Y.H., Zhang Q.Q., Xu Z.Q., Fu Y.L., et al. Prevalence and patterns of multimorbidity in northeastern China: A cross-sectional study. Public Health. 2015;129:1539–1546. doi: 10.1016/j.puhe.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 15.China Adult Dyslipidemia Prevention Committee . China Adult Dyslipidemia Prevention Guide. People’s Health Publishing House; Beijing, China: 2007. [Google Scholar]
- 16.Global Database on Body Mass Index: BMI Classification. 2006. [(accessed on 27 July 2012)]. Available online: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 17.Zhou B.F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—Study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 18.Schoenborn C., Adams P. Health behaviors of adults: United States, 2005–2007. Vital Health Stat. Ser. 2010;245:1–132. [PubMed] [Google Scholar]
- 19.Yang T., Huang L., Wu Z. Study on the appropriateness of the Chinese version of the general health questionnaire as a screening instrument for psychological disorders in mainland China. Chin. J. Epidemiol. 2003;24:769–773. [Google Scholar]
- 20.Phillips M.R., Zhang J., Shi Q., Song Z., Ding Z., Pang S., Li X., Zhang Y., Wang Z. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–2005: An epidemiological survey. Lancet. 2009;373:2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- 21.Desquilbet L., Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat. Med. 2010;29:1037–1057. doi: 10.1002/sim.3841. [DOI] [PubMed] [Google Scholar]
- 22.Heim N., Snijder M.B., Heymans M.W., Deeg D.J., Seidell J.C., Visser M. Optimal cutoff values for high-risk waist circumference in older adults based on related health outcomes. Am. J. Epidemiol. 2011;174:479–489. doi: 10.1093/aje/kwr093. [DOI] [PubMed] [Google Scholar]
- 23.Orsini N., Li R., Wolk A., Khudyakov P., Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: Examples, an evaluation of approximations, and software. Am. J. Epidemiol. 2012;175:66–73. doi: 10.1093/aje/kwr265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruixing Y., Dezhai Y., Shuquan L., Yuming C., Hanjun Y., Qiming F., Shangling P., Weixiong L., Jing T., Yiyang L. Hyperlipidaemia and its risk factors in the Guangxi Bai Ku Yao and Han populations. Public Health Nutr. 2009;12:816–824. doi: 10.1017/S1368980008003273. [DOI] [PubMed] [Google Scholar]
- 25.Shen L., Fan J.-G., Shao Y., Zeng M.-D., Wang J.-R., Luo G.-H., Li J.-Q., Chen S.-Y. Prevalence of nonalcoholic fatty liver among administrative officers in Shanghai: An epidemiological survey. World J. Gastroenterol. 2003;9:1106–1110. doi: 10.3748/wjg.v9.i5.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deng B., Luo T., Huang Y., Shen T., Ma J. Prevalence and determinants of hyperlipidemia in moderate altitude areas of the Yunnan-Kweichow plateau in Southwestern China. High Alt. Med. Biol. 2012;13:13–21. doi: 10.1089/ham.2011.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yin R., Chen Y., Pan S., He F., Liu T., Yang D., Wu J., Yao L., Lin W., Li R., et al. Comparison of lipid levels, hyperlipidemia prevalence and its risk factors between Guangxi Hei Yi Zhuang and Han populations. Arch. Med. Res. 2006;37:787–793. doi: 10.1016/j.arcmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Neaton J.D., Grimm R.H., Prineas R.J., Stamler J., Grandits G.A., Elmer P.J., Cutler J.A., Flack J.M., Schoenberger J.A., McDonald R. Treatment of mild hypertension study: Final results. JAMA. 1993;270:713–724. doi: 10.1001/jama.1993.03510060059034. [DOI] [PubMed] [Google Scholar]
- 29.Shan Z., Ma H., Xie M., Yan P., Guo Y., Bao W., Rong Y., Jackson C.L., Hu F.B., Liu L. Sleep duration and risk of type 2 diabetes: A meta-analysis of prospective studies. Diabetes Care. 2015;38:529–537. doi: 10.2337/dc14-2073. [DOI] [PubMed] [Google Scholar]
- 30.Sorensen M., Andersen Z.J., Nordsborg R.B., Becker T., Tjonneland A., Overvad K., Raaschou-Nielsen O. Long-term exposure to road traffic noise and incident diabetes: A cohort study. Environ. Health Perspect. 2013;121:217–222. doi: 10.1289/ehp.1205503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedrich N., Milman N., Völzke H., Linneberg A., Jørgensen T. Is serum ferritin within the reference range a risk predictor of cardiovascular disease? A population-based, long-term study comprising 2874 subjects. Br. J. Nutr. 2009;102:594–600. doi: 10.1017/S000711450922085X. [DOI] [PubMed] [Google Scholar]
- 32.Weiner D.E., Tighiouart H., Elsayed E.F., Griffith J.L., Salem D.N., Levey A.S., Sarnak M.J. The relationship between nontraditional risk factors and outcomes in individuals with stage 3 to 4 CKD. Am. J. Kidney Dis. 2008;51:212–223. doi: 10.1053/j.ajkd.2007.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhai F., Wang H., Du S., He Y., Wang Z., Ge K., Popkin B.M. Prospective study on nutrition transition in China. Nutr. Rev. 2009;67:S56–S61. doi: 10.1111/j.1753-4887.2009.00160.x. [DOI] [PubMed] [Google Scholar]
- 34.Yang W., Xiao J., Yang Z., Ji L., Jia W., Weng J., Lu J., Shan Z., Liu J., Tian H. Serum lipids and lipoproteins in Chinese men and women. Circulation. 2012;125:2212–2221. doi: 10.1161/CIRCULATIONAHA.111.065904. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization (WHO) Global Status Report on Noncommunicable Diseases 2014. WHO; Geneva, Switzerland: 2015. [Google Scholar]