Abstract
Background
Use of secure messaging through patient portals has risen substantially in recent years due to provider incentives and consumer demand. Secure messaging may increase patient satisfaction and improve outcomes, but also adds to physician workload. Most prior studies of secure messaging focused on primary care and medical specialties. We examined surgeons’ use of secure messaging and the contribution of messaging to outpatient interactions in a broadly-deployed patient portal.
Methods
We determined the number of clinic visits and secure messages for surgical providers in the first three years (2008–10) after patient portal deployment at an academic medical center. We calculated the proportion of outpatient interaction conducted through messaging for each specialty. Logistic regression models compared the likelihood of message-based versus clinic outpatient interaction across surgical specialties.
Results
Over the study period, surgical providers delivered care in 648,200 clinic visits and received 83,912 messages, with more than 200% growth in monthly message volume. Surgical specialties receiving the most messages were orthopedics/podiatry (25.1%), otolaryngology (20.1%), urology (10.8%), and general surgery (9.6%); vascular surgery (0.8%) and pediatric general surgery (0.2%) received the fewest. The proportion of outpatient interactions conducted through secure messaging increased significantly from 5.4% in 2008 to 15.3% in 2010 (p<0.001) with all specialties experiencing growth. Heart/lung transplantation (74.9%), liver/kidney/pancreas transplantation (69.5%), and general surgery (48.7%) had the highest proportion of message-based outpatient interaction by the end of the study.
Conclusions
This study demonstrates rapid adoption of online secure messaging across surgical specialties with significant growth in its use for outpatient interaction. Some specialties, particularly those with long-term follow-up, interacted with patients more through secure messaging than in person. As surgeons devote more time to secure messaging, additional research will be needed to understand the care delivered through online interactions and to develop models for reimbursement.
Keywords: Patient Portal, Secure Messaging, Patient Engagement, Consumer Health Informatics, Patient-Provider Communication, Surgery
INTRODUCTION
Recent years have shown a trend toward increasing online communications between healthcare organizations and the patients they serve. Many institutions have adopted patient portals to facilitate such interactions. Patient portals are secure websites that provide patients access to a variety of clinical data and administrative functions: most portals offer viewing of portions of the electronic health record, the ability to communicate with providers, and appointment scheduling. Secure patient-provider messaging is one of the features of portals most widely used by patients [1–3], yet adoption among providers has been slow [4, 5]. In recent surveys, a majority of patients desired to send messages to their providers [6–8], and many patients preferentially select providers who make secure messaging available [9]. Studies at multiple institutions also reported high patient satisfaction scores with secure messaging [10–13], including equivalent or higher satisfaction as compared to in-office visits or telephone calls [11].
Secure messaging directly addresses the patient-provider communication core focus identified by the Institute of Medicine for improving care quality and patient outcomes [14]. It may also be considered an evolving form of outpatient care—during secure message exchanges, patients reported new problems and providers arranged further evaluation and treatment [15–17]. Secure messaging can deliver clinical care that is complementary to traditional outpatient encounters [11, 17, 18], increase frequency of communication between patients and providers [19], and enable providers to better know their patients [19]. Patients may also feel empowered and safe to discuss questions or concerns through messaging that they would not bring up during an office visit [12, 17]. Studies within primary care or medicine specialty practices demonstrated the potential for secure messaging to improve health outcomes [20] while reducing healthcare system costs and resource utilization [21, 22].
Motivated by a mix of incentives including the Affordable Care Act and Meaningful Use criteria, physicians are slowly adding secure messaging to their practices [23, 24], but few studies have examined the use of secure messaging by surgical providers. Overall, messaging volumes have risen concomitantly with increased availability of secure messaging [25]. Primary care physicians and medical specialists use secure messaging at rates approaching ten times that of their surgical colleagues [24, 25], with surgeons as a group ranked last in total usage among the specialties considered in one recent study [25]. Notably, these studies did not examine usage across surgical subspecialties, where variations in practice patterns (e.g., duration of post-procedure follow-up, elective versus emergent procedures) may alter the likelihood of using secure messaging.
In this study we examined surgeons’ use of secure messaging in the first three years after deployment of a patient portal at a large academic health center. We compared secure messaging use across surgical subspecialties and determined how secure messaging contributes to the overall volume of surgical outpatient interactions.
DATA AND METHODS
Setting
This study was conducted at Vanderbilt University Medical Center (VUMC), a private, non-profit, academic institution in Nashville, Tennessee, that provides primary and regional referral care to adults and children. VUMC launched the My Health At Vanderbilt (MHAV) patient portal in 2005, with implementation across the clinical enterprise completed in 2007. All patients who receive medical care at VUMC may enroll online for access to MHAV, which supports secure messaging with healthcare providers with whom the patient has an established relationship, access to selected portions of the medical record, account and bill management, and personalized health information [2].
MHAV was rolled out incrementally across individual clinical specialties, with physician champions introducing the tool to providers and flyers posted in outpatient clinics promoting MHAV to patients. Individual providers also became advocates, urging their patients to use MHAV. Technical support personnel were available to patients, physicians, and staff as the portal was introduced. Additional details regarding the policies and procedures used to enhance patient and provider adoption have been previously published elsewhere [2]. MHAV currently has over 280,000 registered users with over 200,000 logins per month.
Members of the healthcare team are able to participate in secure messaging through StarPanel, the electronic medical record used at VUMC. Patient-initiated messages from MHAV are directed to provider or specialty-based message baskets, most of which are managed by clinical care teams. The teams may include physicians, nurses, administrative assistants, and allied health professionals within the same division, department, or other clinical unit. All messages become part of the patients’ permanent medical records. When patients initiate a message, the MHAV website cautions users that the average response time is 1–2 business days, that medical emergencies should be handled by calling 911, and that all communication is added to the patient’s medical record. The policies and procedures of the messaging triage system and permanent record storage are described elsewhere [2].
Study Population
We determined the number of surgical clinic visits and patient-initiated MHAV message threads sent to surgical providers between January 1, 2008 and December 31, 2010. This time period was selected to examine the adoption of messaging after full deployment of MHAV to adult and pediatric specialties. A message thread is a collection of related messages exchanged between a MHAV user and their healthcare providers (i.e., an initial message and all replies). MHAV users consist of three groups: (1) patients who have registered for MHAV, termed patients; (2) individuals whom a patient designates to access MHAV on their behalf, termed delegates; and, (3) parents or guardians who have access to their children’s health information through MHAV, called surrogates. Message threads pertaining to multidisciplinary and administrative VUMC message baskets that could not be assigned to a single specialty were excluded. Outpatient clinic visits were excluded if they occurred in a multispecialty practice.
Data Collection and Analysis
We recorded the number of message threads sent to surgical providers during the study period. For each message thread, we determined the message date, role of the message sender (i.e., patient, delegate, or surrogate), surgical specialty of the receiving provider, and patient demographics, including age at the time of thread initiation, gender, and race. To understand the volumes of secure messaging relative to practice volumes, we also collected information about VUMC surgical outpatient clinic visits during the same time period. For each clinic visit, we recorded the encounter date; the age, gender, and race of the patient; and the specialty of the surgical clinic in which the encounter took place. Each clinic was assigned to one of 15 surgical specialties that reflected the departmental organization at VUMC (Table 1). We defined an outpatient interaction as either an outpatient clinic visit or a MHAV message thread, and we calculated the proportion of outpatient interaction conducted through messaging.
Table 1.
Patient Demographics and Specialty Distribution of Outpatient Interactions, 2008–10.
| Outpatient Clinic Visits (N=648,200) |
Message Threads (N=83,912) |
P Value* | |
|---|---|---|---|
| Gender | < 0.001 | ||
|
| |||
| Male | 323098 (49.8%) | 34678 (41.3%) | |
| Female | 325102 (50.2%) | 49234 (58.7%) | |
|
| |||
| Race | < 0.001 | ||
|
| |||
| African American | 72718 (11.2%) | 4499 (5.4%) | |
| American Indian/Eskimo | 1138 (0.2%) | 60 (<0.1%) | |
| Asian/Pac. Islander | 8334 (1.3%) | 338 (0.4%) | |
| Caucasian | 463181 (71.5%) | 72521 (86.4%) | |
| Hispanic/Latino | 16388 (2.5%) | 586 (0.7%) | |
| Unknown | 86441 (13.3%) | 5908 (6.1%) | |
|
| |||
| Age | < 0.001 | ||
|
| |||
| 47 (20, 62) | 52 (41, 60) | ||
|
| |||
| Specialty | < 0.001 | ||
|
| |||
| Cardiac Surgery | 64859 (10.0%) | 853 (1.0%) | |
| Colorectal Surgery | 11133 (1.7%) | 1260 (1.5%) | |
| General Surgery | 17228 (2.7%) | 8080 (9.6%) | |
| Heart/Lung Transplant | 2867 (0.4%) | 4904 (5.8%) | |
| Liver/Kidney/Pancreas Transplant | 5225 (0.8%) | 8057 (9.6%) | |
| Neurosurgery | 35293 (5.4%) | 5057 (6.0%) | |
| Oncologic Surgery | 12949 (2.0%) | 2601 (3.1%) | |
| Orthopedic Surgery/Podiatry | 183255 (28.3%) | 21099 (25.1%) | |
| Otolaryngology | 81537 (12.6%) | 16877 (20.1%) | |
| Pediatric General Surgery | 13634 (2.1%) | 179 (0.2%) | |
| Plastic Surgery | 103518 (16.0%) | 3006 (3.6%) | |
| Thoracic Surgery | 6509 (1.0%) | 756 (0.9%) | |
| Trauma | 10738 (1.7%) | 1426 (1.7%) | |
| Urology | 79507 (12.3%) | 9075 (10.8%) | |
| Vascular Surgery | 19948 (3.1%) | 680 (0.8%) | |
Significance testing was performed using chi-squared test for gender, race and specialty, and by Wilcoxon rank-sum test for age.
We generated summary statistics of specialty assignment and patient demographics for all outpatient interactions, overall and by type of interaction. Continuous variables were summarized with medians and inter-quartile ranges and compared using Wilcoxon rank sum test. Categorical variables were summarized as counts and frequencies and compared using chi-squared test. For each month of the study period we determined the number of recipient message baskets, message threads, unique patients using messaging, and outpatient clinic visits. Wilcoxon rank sum test was used to compare usage rates (i.e., messages per month, active users per month, messages per message basket per month) in 2008 and 2010. An active user was defined as a unique user who initiated at least one message in a given month. The trend over time for messages per 100 active users per month was evaluated using two-tailed Spearman’s rank-order correlation.
We also developed models of the differences in messaging use by specialty, controlling for age, gender, race and time the initial message was sent. The time was calculated as the number of months since the beginning of the study period. We used logistic regression, and interacted month and specialty to allow assessment of changes in messaging use over time. Continuous age was flexibly fit using a restricted cubic spline with four knots. Analyses were conducted in GraphPad Prism 5 or R version 3.0.1. Models were fit in R using lrm from the rms package [26].
This study was approved by the Vanderbilt University Institutional Review Board.
RESULTS
In the three years after full portal deployment, 20,484 unique MHAV patient portal users (96% patients; 3% surrogates; 1% delegates) initiated 83,912 secure message threads to surgical providers. Messages to surgical providers were initiated by 23.7% of all unique MHAV users sending messages and represented 8.7% of all secure message threads exchanged during the study period across the institution. The surgical message threads were distributed across 412 unique provider message baskets. Patients participated in 648,200 outpatient surgical clinic encounters (24.4% of all outpatient clinic encounters) in 119 distinct VUMC clinics. We excluded 1,536 message threads (1.8%) and 5,708 (0.9%) clinic visits that involved multi-specialty practices.
Patients across all surgical outpatient interactions (i.e., secure messages or clinic encounters) were mostly female (51%) and Caucasian (73%), with an average age of 43.6 years. Demographics were significantly different between patients cared for through secure messaging versus clinic encounters (p<0.001 for gender, race and age; Table 1).
In aggregate, surgical specialties experienced near linear growth in the number of message threads on a monthly and annualized basis, while the number of clinic encounters remained relatively constant (Figure 1). The number of message threads per month more than tripled over the study period, from 1001 (standard deviation (SD): 176) threads per month in 2008 to 3370 (SD: 315) per month in 2010 (p<0.001). This increase was paralleled by the number of MHAV users initiating messages, growing from 668 (SD: 123) active users per month in 2008 to 2144 (SD: 178) per month in 2010 (p<0.001). As a result, the average number of message threads per hundred active users per month increased only slightly during this period (p<0.001; Table 2).
Figure 1. Surgical Specialty Use of Secure Messaging and Encounter Volume.
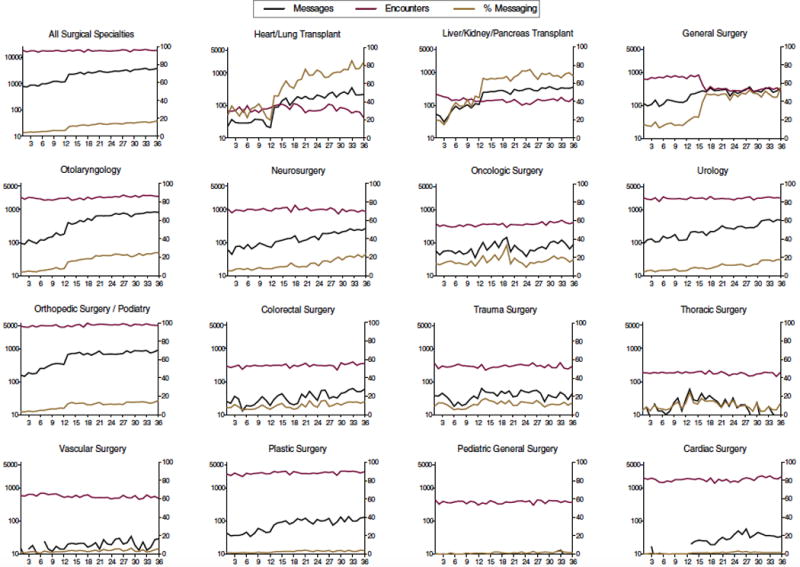
Message volume per month (black solid line) and outpatient clinic encounter volume (gray solid line) are plotted on the left y-axis at logarithmic scale. The percentage of all outpatient interactions accounted for by secure messaging (black dotted line) is plotted on the right y-axis at linear scale. Months are along the x-axis. The specialties are ordered left-to-right, top-to-bottom, by highest percentage of outpatient interactions conducted by secure messaging at the end of the study period. (Note: Monthly message volumes below 10 per month are represented by a break in the plotted line.)
Table 2.
Monthly Messaging Volume per Hundred Active Users by Specialty, 2008–10.
| 2008 n (SD) |
2009 n (SD) |
2010 n (SD) |
Spearman’s rho (95% CI) |
P Value* | |
|---|---|---|---|---|---|
| All Specialties | 148 (3.6) | 156 (2.9) | 157 (2.9) | 0.73 (0.52–0.86) | < 0.001 |
| Cardiac Surgery | 132 (61) | 139 (13) | 163 (15) | 0.50 (0.19–0.71) | 0.002 |
| Colorectal Surgery | 145 (20) | 146 (27) | 144 (11) | 0.02 (−0.32–0.35) | 0.91 |
| General Surgery | 147 (10) | 164 (7.6) | 167 (12) | 0.58 (0.30–0.77) | < 0.001 |
| Heart/Lung Transplant | 168 (35) | 225 (26) | 218 (22) | 0.49 (0.18–0.71) | 0.003 |
| Liver/Kidney/Pancreas Transplant | 186 (23) | 218 (19) | 216 (17) | 0.50 (0.20–0.72) | 0.002 |
| Neurosurgery | 154 (9.7) | 165 (17) | 175 (7.1) | 0.46 (0.14–0.69) | 0.005 |
| Oncologic Surgery | 162 (15) | 149 (18) | 155 (14) | −0.14 (−0.45–0.21) | 0.43 |
| Orthopedic Surgery/Podiatry | 138 (4.4) | 148 (5.0) | 149 (3.3) | 0.68 (0.44–0.82) | < 0.001 |
| Otolaryngology | 138 (9.6) | 137 (5.3) | 141 (1.8) | 0.20 (−0.15–0.50) | 0.26 |
| Pediatric General Surgery | 101 (118) | 118 (31) | 137 (58) | 0.26 (−0.08–0.55) | 0.12 |
| Plastic Surgery | 148 (26) | 137 (12) | 134 (8.3) | −0.25 (−0.54–0.10) | 0.14 |
| Thoracic Surgery | 150 (29) | 177 (31) | 137 (25) | −0.20 (−0.50–0.15) | 0.25 |
| Trauma | 145 (24) | 155 (19) | 143 (16) | −0.17 (−0.48–0.18) | 0.32 |
| Urology | 148 (14) | 145 (6.4) | 153 (9.5) | 0.25 (−0.10–0.54) | 0.14 |
| Vascular Surgery | 125 (27) | 137 (20) | 145 (39) | 0.24 (−0.10–0.54) | 0.16 |
Significance testing was performed using two-tailed Spearman’s rank correlation coefficient.
The number of messages received was highly variable across surgical specialties (Table 1; Figure 1, black lines). Orthopedic surgery/podiatry received the greatest number of messages per month in each of the three years (2008: 251 per month; 2009: 706 per month; 2010: 801 per month). Otolaryngology had the second highest volumes in each year, but increased rapidly in annual volume such that it was no longer significantly different from orthopedics/podiatry in 2010 (p=0.17). Pediatric general surgery was consistently the specialty with the lowest utilization. Analysis of growth in message threads per 100 active users per month revealed significant growth for six of 15 specialties (40%; Table 2), including cardiac surgery, general surgery, heart/lung transplant surgery, liver/kidney/pancreas transplant surgery, neurosurgery, and orthopedic surgery/podiatry.
Secure messages accounted for 11.5% of all outpatient interactions during the study period and had significant yearly growth from 5.4% (SD: 0.8%) in 2008 to 15.3% (SD: 0.9%) in 2010 (p<0.001). All specialties experienced an increase in their proportion of message-based interactions by the end of the study period (Figure 1). Liver/kidney/pancreas transplantation was the specialty with the highest proportion of message-based interactions in 2008 (32.0%, SD: 10.3) and 2009 (67.0%, SD: 3.4), but was surpassed by heart and lung transplantation on a monthly basis at month 20 (August 2009) and on an annualized basis in 2010 with 69.5% (SD: 2.7) and 74.9% (SD: 5.3), respectively. These two transplantation groups and general surgery each received greater numbers of messages than had outpatient clinic visits (i.e., proportion of messages exceeded 50%) during one or more months by the end of the study. Cardiac surgery and pediatric general surgery conducted the smallest percentage of outpatient interactions through messaging in all years.
In our regression modeling adjusted for age, gender, race and message date, the estimated proportion of outpatient interactions accounted for by secure messaging for each specialty (Figure 2) revealed heart/lung transplantation was the most likely to use messaging by the end of the study period (82%), followed by liver/kidney/pancreas transplantation (75%), general surgery (53%), and otolaryngology (34%); plastic surgery had the lowest probability of using messaging (4.5%).
Figure 2. Likelihood of Messaging Use across Surgical Specialties by Month.
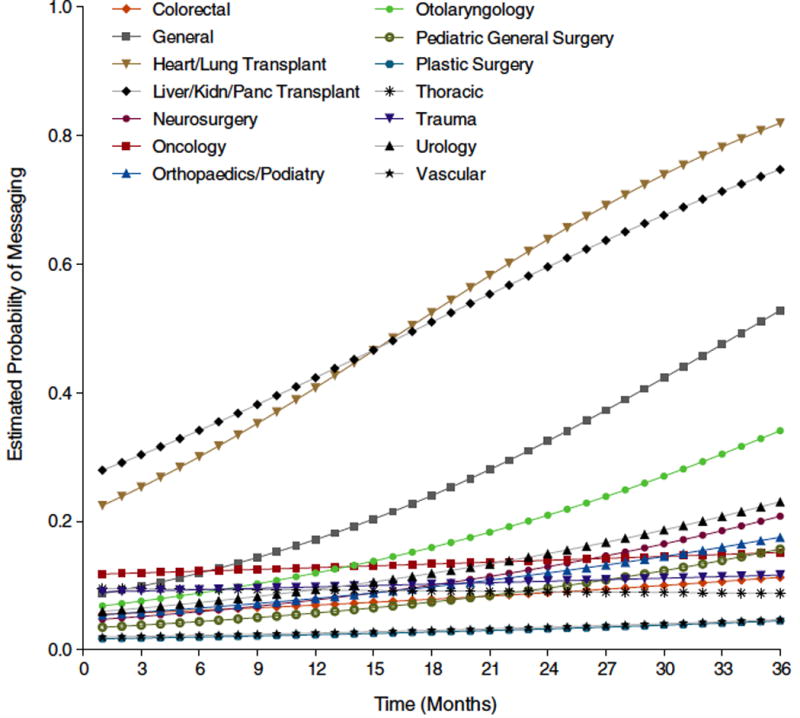
Probability estimates were calculated from logistic regression models controlling for age, gender, race, and time of initial message.
DISCUSSION
Patient portal research and studies of secure messaging to date have focused on use within the context of primary care or medical specialties. In this study, we demonstrate widespread adoption of secure messaging through a patient portal by a diverse set of surgical providers and their patients. Annual messaging volumes for surgical providers more than tripled during our study period to over 40,000 message threads in 2010. This increase was paralleled by similar gains in the number of patient users initiating messages, while the number of outpatient clinic encounters remained relatively stable. A near three-fold increase in rates was also observed for use of messaging as a form of outpatient interaction, growing from 5.4% of outpatient interactions in 2008 to 15.3% in 2010 (p<0.001). Notably, message threads per hundred active users grew slowly over three years, increasing only 4.6% to an average of 157 threads per month in 2010. These findings suggest that the principal driver of increased message volume over time was recruitment of higher numbers of patient users, rather than existing users sending more messages, validating similar trends reported previously for non-surgical disciplines [25, 41].
Our analysis of messaging volumes of individual surgical specialties, which to our knowledge has not been studied previously, identified wide variation across specialties. All specialties except thoracic surgery experienced growth in message volumes over the study period, yet rates of growth were highly variable. Similar variability across specialties has been demonstrated previously for medical specialties at our institution and others [25, 41]. Many factors likely influence the number of messages received by a specialty, including outpatient clinic encounter volume, provider comfort with technology and clinic workflow [10, 27–29], encouragement or discouragement of providers [3, 30], promotion of messaging to patients [3, 12, 30], the duration and frequency of follow-up perioperatively, patients’ clinical needs, and patient demographics and sociotechnical factors [31, 32]. The unique message triage process at our institution, including the ability for each department to set its own workflow and staffing practices, may also have contributed to the differences observed.
Overall growth in messaging volume was driven both by growth in the number of users as well as increased messages per user. The number of users messaging increased by over a factor of three during the study period. The number of messages per user grew significantly for six of 15 specialties – in some cases by as much as 29.8% (i.e., heart/lung transplant) – but overall usage remained at approximately one to two messages per user per month. Thus the greatest contributor to overall messaging growth was the increased number of users. The reasons for growth in both the user population and the number of messages per user are likely multifactorial. Provider support of secure messaging is a critical factor for sustained patient use [42], so specialties with greater increases may have had larger numbers of physician advocates. Other factors may include departmental policies or procedures that aimed to increase use among existing patients and reinforcement after positive experiences using secure messaging.
Growth in messaging volume lead to significant gains in the percentage of outpatient care delivered through messaging across surgical specialties (Figure 1). In 2008, all surgical specialists were more likely to conduct outpatient interactions through traditional clinic encounters than to use secure messaging. By the end of the study period, however, providers in three specialties (heart/lung transplantation, liver/kidney/pancreas transplantation, and general surgery) were more likely to interact with their patients through secure messaging than clinic encounters. The high usage of messaging by these three specialties may reflect the need for long-term follow-up as well as complexity of care for these patients, who often have multiple medical and surgical comorbidities. Additionally, studies of kidney transplant patients indicate this patient population is highly open to using digital technologies in the management of their health [33], and this may contribute to the messaging use patterns we observed among the transplant specialties.
The marked rise in use of online secure messaging as a form of outpatient interaction highlights changing preferences for patient-physician communication. Some studies suggest patients use secure messaging in place of outpatient office visits, telephone calls or emails [10, 18, 34], while other studies report the frequency of using these other forms of communication was unaffected by the adoption of secure messaging [11, 35]. Our study cannot rule out a rapid shift from using telephone calls to secure messaging, as calls are not systematically recorded at our institution and cannot be evaluated for comparison. It is more likely, however, that patients and providers have identified messaging as a preferred communication medium for questions and concerns that might otherwise wait until the next office visit [8]. The asynchronicity of secure messaging may also alleviate patient anxiety over “bothering” their provider and allow patients to communicate at their convenience, even outside of normal office hours [11, 15].
As regulatory and reimbursement policies combine with consumer demand to drive availability and use of secure messaging systems, there is concern that providers will become overwhelmed by the additional volume of messages [22, 27, 29]. Our study suggests that while number of messages per active messaging user may not substantially increase over time, surgical providers can still experience a substantial increase in the volume of messages as increasingly more patients adopt messaging as a means of communication. Whether this will have significant impact on providers’ workload and attitudes is an area warranting further study.
Surgeons, who are often reimbursed in bundled payments for the surgery and all perioperative care [36, 37], may particularly benefit from increasing patient use of secure messaging for preoperative counseling and postoperative follow-up. Opportunities to improve outcomes, reduce costs, and optimize surgeons’ practice efficiency may come about, for example, by increasing revenue-generating consultations in place of postoperative appointments conducted online [5] or by improving patient adherence to pre- and post-operative care instructions through online reminders [38]. In addition, with proposals to compensate providers for online care having already been developed [39] and billing codes announced [40], payers may soon reimburse providers for their use of secure messaging and other online care delivery platforms.
This study has limitations. Our data comes from a single medical center with a locally-developed patient portal, which has its own unique features, policies and procedures [2]. These conditions may limit the generalizability of our findings, although our portal shares many features and policies with some widely-deployed commercial portals, which are being increasingly adopted to meet Meaningful Use criteria. In addition, although MHAV was in operation for several years prior to the study period, accounts for children and their surrogates became available only one year prior to the study period. The messaging utilization patterns observed for pediatric providers may thus reflect early adopter behavior, and the timing of pediatric MHAV deployment may account for the low rates of message-based encounters for pediatric general surgery.
We only included message threads in our analysis that were initiated by patients or their surrogates or delegates. Messages initiated by providers and semi-automated messages, such as prescription refill reminders were excluded. Additionally, when assigning message threads to a surgical specialty, we included only the initial specialty contacted by the patient and did not account for transfer of messages to other specialties. The assigned specialty was assumed to be actively involved in the patient interaction, even if only to make a referral. As a result of these exclusions, our study likely underestimates the total messaging activity that occurred in the portal.
Our outpatient encounter data set did not contain patient identifiers, and thus, in regression analysis, we were unable to cluster message threads or outpatient encounters involving the same patient. The estimated standard errors in the model are likely affected by patient-level correlation. Our findings are likely minimally affected by this limitation given the high level of significance in the observed p-values.
We were also unable to incorporate outpatient interactions involving telephone calls and email messages during the study period. At VUMC, telephone calls and email messages are not systematically recorded across specialties, preventing accurate accounting of their numbers. Email communication was not expected to contribute significantly to outpatient interaction volumes given institutional policies that discourage or prohibit email interactions. With the increasing number of communication modalities available, it will be important for future studies to address the entire spectrum of communication options and characterize what features and circumstances influence patient selection of communication modality.
CONCLUSIONS
To our knowledge, this study is the first to focus on surgeons’ use of secure messaging through a patient portal. We have demonstrated that surgical providers and their patients rapidly adopt secure messaging after portal deployment and that messaging use contributes significantly to the total number of outpatient interactions. Notably, in only three years after broad portal availability, the volume of secure messaging exceeded outpatient clinic encounters for some surgical specialties at our institution. Surgical providers in aggregate did substantially less messaging than primary care and medical specialty providers, and wide variation in rates of messaging use were identified across surgical specialties, likely reflecting differences in practice patterns.
As more surgical practices adopt this technology under the pressures of Meaningful Use incentives, national regulations, and consumer demand, it will be imperative to determine the workload implications of messaging growth and identify opportunities to maximize process efficiency. Delineation of the types of care delivered through secure messaging is also needed to guide reimbursement models that appropriately compensate surgeons for their time and clinical effort.
Acknowledgments
Funding: Robert Cronin and Sharon Davis were supported by the 5T15LM007450-12 training grant from the National Library of Medicine.
Dr. Jackson receives salary support from funding given to Vanderbilt University Medical Center by West Health for a research project involving automated telephone call technologies.
Footnotes
Disclosures: Mr. Shenson, Dr. Cronin, Ms. Davis, and Dr. Chen have no conflicts of interest or financial ties to disclose.
References
- 1.Weingart S, Rind D, Tofias Z, Sands D. Who Uses the Patient Internet Portal? The PatientSite Experience. J Am Med Inform Assoc. 2006;13(1):91–95. doi: 10.1197/jamia.M1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osborn CY, Rosenbloom ST, Stenner SP, Anders S, Muse S, Johnson KB, Jirjis J, Jackson GP. MyHealthAtVanderbilt: policies and procedures governing patient portal functionality. J Am Med Inform Assoc. 2011;18(Suppl 1):i18–23. doi: 10.1136/amiajnl-2011-000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haun JN, Lind JD, Shimada SL, Martin TL, Gosline RM, Antinori N, Stewart M, Simon SR. Evaluating user experiences of the secure messaging tool on the Veterans Affairs’ patient portal system. J Med Internet Res. 2014;16(3):e75. doi: 10.2196/jmir.2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zickmund SL, Hess R, Bryce CL, McTigue K, Olshansky E, Fitzgerald K, Fischer GS. Interest in the use of computerized patient portals: role of the provider-patient relationship. J Gen Int Med. 2008;23(Suppl 1):20–6. doi: 10.1007/s11606-007-0273-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bishop TF, Press MJ, Mendelsohn JL, Casalino LP. Electronic communication improves access, but barriers to its widespread adoption remain. Health Aff. 2013;32(8):1361–7. doi: 10.1377/hlthaff.2012.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kleiner KD, Akers R, Burke BL, Werner EJ. Parent and Physician Attitudes Regarding Electronic Communication in Pediatric Practices. Pediatrics. 2002;109(5):740–744. doi: 10.1542/peds.109.5.740. [DOI] [PubMed] [Google Scholar]
- 7.Liederman E, Morefield C. Web Messaging: A New Tool for Patient-Physician Communication. J Am Med Inform Assoc. 2003;10(3):260–271. doi: 10.1197/jamia.M1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye J, Rust G, Fry-Johnson Y, Strothers H. E-mail in patient-provider communication: A systematic review. Patient Educ Couns. 2010;80(2):266–273. doi: 10.1016/j.pec.2009.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anand SG, Feldman MJ, Geller DS, Bisbee A, Bauchner H. A content analysis of e-mail communication between primary care providers and parents. Pediatrics. 2005;115(5):1283–8. doi: 10.1542/peds.2004-1297. [DOI] [PubMed] [Google Scholar]
- 10.Liederman EM, Lee JC, Baquero VH, Seites PG. Patient-physician web messaging. The impact on message volume and satisfaction. J Gen Intern Med. 2005;20(1):52–7. doi: 10.1111/j.1525-1497.2005.40009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin C-T, Wittevrongel L, Moore L, Beaty BL, Ross SE. An Internet-based patient-provider communication system: randomized controlled trial. J Med Internet Res. 2005;7(4):e47. doi: 10.2196/jmir.7.4.e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stalberg P, Yeh M, Ketteridge G, Delbridge H, Delbridge L. E-mail Access and Improved Communication Between Patient and Surgeon. Arch Surg. 2008;143(2):164–168. doi: 10.1001/archsurg.2007.31. [DOI] [PubMed] [Google Scholar]
- 13.Baer D. Patient-Physician E-Mail Communication: The Kaiser Permanente Experience. J Oncol Pract. 2011;7(4):230–232. doi: 10.1200/JOP.2011.000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Institute of Medicine. National Academy Press; Washington, D.C: 2001. [Google Scholar]
- 15.White C, Moyer C, Stern D, Katz S. A Content Analysis of E-mail Communication between Patients and Their Providers: Patients Get the Message. J Am Med Inform Assoc. 2004;11(4):260–267. doi: 10.1197/jamia.M1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stiles R, Deppen S, Figaro M, Gregg W. Behind-the-scenes of patient-centered care: Content analysis of electronic messaging among primary care clinic providers and staff. Med Care. 2007;45(12):1205–1209. doi: 10.1097/MLR.0b013e318148490c. [DOI] [PubMed] [Google Scholar]
- 17.Wallwiener M, Wallwiener CW, Kansy JK, Seeger H, Rajab TK. Impact of electronic messaging on the patient-physician interaction. J Telemed Telecare. 2009;15(5):243–50. doi: 10.1258/jtt.2009.090111. [DOI] [PubMed] [Google Scholar]
- 18.Roter DL, Larson S, Sands DZ, Ford DE, Houston T. Can e-mail messages between patients and physicians be patient-centered? Health Commun. 2008;23(1):80–6. doi: 10.1080/10410230701807295. [DOI] [PubMed] [Google Scholar]
- 19.Nazi KM. The Personal Health Record Paradox: Health Care Professionals’ Perspectives and the Information Ecology of Personal Health Record Systems in Organizational and Clinical Settings. J Med Internet Res. 2013;15(4):e70. doi: 10.2196/jmir.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff. 2010;29(7):1370–5. doi: 10.1377/hlthaff.2010.0048. [DOI] [PubMed] [Google Scholar]
- 21.Biermann JS, Golladay GJ, Peterson RN. Using the Internet to Enhance Physician-Patient Communication. J Am Acad Orthop Surg. 2006;14(3):136–144. doi: 10.5435/00124635-200603000-00004. [DOI] [PubMed] [Google Scholar]
- 22.McGeady D, Kujala J, Ilvonen K. The impact of patient-physician web messaging on healthcare service provision. Int J Med Inform. 2008;77(1):17–23. doi: 10.1016/j.ijmedinf.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Blumenthal D, Tavenner M. The “Meaningful Use” Regulation for Electronic Health Records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 24.Neuner J, Fedders M, Caravella M, Bradford L, Schapira M. Meaningful Use and the Patient Portal: Patient Enrollment, Use, and Satisfaction With Patient Portals at a Later-Adopting Center. Am J Med Qual. 2014 doi: 10.1177/1062860614523488. February 21, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crotty BH, Tamrat Y, Mostaghimi A, Safran C, Landon BE. Patient-To-Physician Messaging: Volume Nearly Tripled As More Patients Joined System, But Per Capita Rate Plateaued. Health Aff. 2014;33(10):1817–22. doi: 10.1377/hlthaff.2013.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrell FJ, Dupont M, Hmsic D. The design package. 2007 Available at: http://ftp.uni-bayreuth.de/math/statlib/R/CRAN/doc/packages/Design.pdf. Accessed 10 December 2014.
- 27.Byrne JM, Elliott S, Firek A. Initial experience with patient-clinician secure messaging at a VA medical center. J Am Med Inform Assoc. 2009;16(2):267–70. doi: 10.1197/jamia.M2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaster B, Knight C, DeWitt D, Sheffield J, Assefi N, Buchwald D. Physicians’ Use of and Attitudes Toward Electronic Mail for Patient Communication. J Gen Intern Med. 2003;18(5):385–389. doi: 10.1046/j.1525-1497.2003.20627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wakefield DS, Mehr D, Keplinger L, Canfield S, Gopidi R, Wakefield BJ, Koopman RJ, Belden JL, Kruse R, Kochendorfer KM. Issues and questions to consider in implementing secure electronic patient-provider web portal communications systems. Int J Med Inform. 2010;79(7):469–77. doi: 10.1016/j.ijmedinf.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 30.Wade-Vuturo AE, Mayberry LS, Osborn CY. Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc. 2013;20(3):519–25. doi: 10.1136/amiajnl-2012-001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Couchman GR, Forjuoh SN, Rascoe TG, Reis MD, Koehler B, Van Walsum KL. E-mail communications in primary care: what are patients’ expectations for specific test results? Int J Med Inform. 2005;74(1):21–30. doi: 10.1016/j.ijmedinf.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Houston TK, Sands DZ, Jenckes MW, Ford DE. Experiences of patients who were early adopters of electronic communication with their physician: satisfaction, benefits, and concerns. Am J Manag Care. 2004;10(9):601–8. [PubMed] [Google Scholar]
- 33.McGillicuddy JW, Weiland AK, Frenzel RM, Mueller M, Brunner-Jackson BM, Taber DJ, Baliga PK, Treiber FA. Patient attitudes toward mobile phone-based health monitoring: questionnaire study among kidney transplant recipients. J Med Internet Res. 2013;15(1):e6. doi: 10.2196/jmir.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou YY, Garrido T, Chin HL, Wiesenthal AM, Liang LL. Patient access to an electronic health record with secure messaging: impact on primary care utilization. Am J Manag Care. 2007;13(7):418–24. [PubMed] [Google Scholar]
- 35.Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient-provider communication: will it offset office visits and telephone consultations in primary care? Int J Med Inform. 2005;74(9):705–10. doi: 10.1016/j.ijmedinf.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 36.Lee J. Bundled payments give surgeons new incentives to cut costs. Mod Healthcare. 2014 Available at: http://www.modernhealthcare.com/article/20140301/MAGAZINE/303019981. Accessed 10 December 2014. [PubMed]
- 37.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff. 2011;30(11):2107–15. doi: 10.1377/hlthaff.2011.0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Edmiston CEJ, Krepel CJ, Edmiston SE, Spencer M, Lee C, Brown KR, Lewis BD, Rossi PJ, Malinowski M, Seabrook G. Empowering the Surgical Patient: A Randomized, Prospective Analysis of an Innovative Strategy for Improving Patient Compliance with Preadmission Showering Protocol. J Am Coll Surg. 2014;219(2):256–264. doi: 10.1016/j.jamcollsurg.2014.01.061. [DOI] [PubMed] [Google Scholar]
- 39.Tang PC, Black W, Young CY. Proposed criteria for reimbursing eVisits: content analysis of secure patient messages in a personal health record system. AMIA Annu Symp Proc. 2006;2006:764–8. [PMC free article] [PubMed] [Google Scholar]
- 40.Summary of the 2015 Final Medicare Physician Fee Schedule. Am Acad Fam Physicians. 2014 Available at: http://www.aafp.org/dam/AAFP/documents/advocacy/payment/medicare/feesched/ES-2015MPFS-110514.pdf. Accessed 10 December 2014.
- 41.Cronin RM, Davis SE, Shenson JA, Chen Q, Rosenbloom ST, Jackson GP. Growth of Secure Messaging Through a Patient Portal as a Form of Outpatient Interaction across Clinical Specialties. Appl Clin Inf. 2015;6(2):288–304. doi: 10.4338/ACI-2014-12-RA-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wade-Vuturo AE, Mayberry LS, Osborn CY. Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc. 2013;20(3):519–525. doi: 10.1136/amiajnl-2012-001253. [DOI] [PMC free article] [PubMed] [Google Scholar]


