Abstract
Rationale
Recommendations from healthcare providers are one of the most consistent correlates of adolescent vaccination, but few studies have investigated other elements of patient-provider communication and their relevance to uptake.
Objective
We examined competing hypotheses about the relationship of patient-versus provider-driven communication styles with vaccination.
Methods
We gathered information about vaccine uptake from healthcare provider-verified data in the 2010 National Immunization Survey-Teen for tetanus, diphtheria, and pertussis (Tdap) booster, meningococcal vaccine, and human papillomavirus (HPV) vaccine (initiation among females) for adolescents ages 13–17. We categorized communication style in parents’ conversations with healthcare providers about vaccines, based on parents’ reports (of whether a provider recommended a vaccine and, if so, if conversations were informed, shared, or efficient) (N = 9,021).
Results
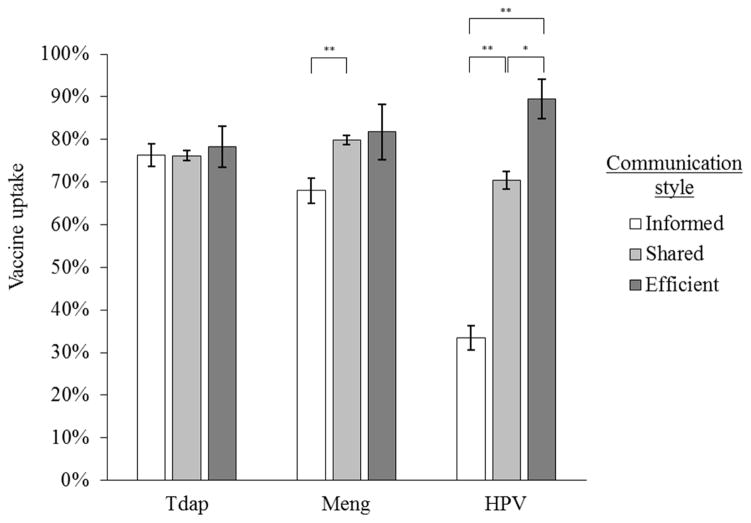
Most parents reported either no provider recommendation (Tdap booster: 35%; meningococcal vaccine: 46%; and HPV vaccine: 31%) or reported a provider recommendation and shared patient-provider communication (43%, 38%, and 49%, respectively). Provider recommendations were associated with increased odds of vaccination (all ps < .001). In addition, more provider-driven communication styles were associated with higher rates of uptake for meningococcal vaccine (efficient style: 82% vs. shared style: 77% vs. informed style: 68%; p < .001 for shared vs. informed) and HPV vaccine (efficient style: 90% vs. shared style: 70% vs. informed style: 33%; p < .05 for all comparisons).
Conclusion
Efficient communication styles were used rarely (≤ 2% across vaccines) but were highly effective for encouraging meningococcal and HPV vaccination. Intervention studies are needed to confirm that efficient communication approaches increase HPV vaccination among adolescents.
Keywords: Patient-provider communication; adolescents; providers; tetanus, diphtheria and pertussis (Tdap) booster; meningococcal vaccine; human papillomavirus (HPV) vaccine
National guidelines recommend that adolescents routinely receive three vaccines: tetanus, diphtheria, and pertussis (Tdap) booster, meningococcal vaccine, and human papillomavirus (HPV) vaccine (Centers for Disease Control and Prevention (CDC), 2015b). Healthy People 2020 (Department of Health and Human Services, 2015) set the goal of 80% coverage for each of these vaccines among 13- to 15-year-old adolescents. As of 2014, vaccination coverage among all adolescents (ages 13 to 17) surpassed this benchmark for Tdap booster (88%), fell somewhat short for meningococcal vaccine (79%), and was far from desired targets for HPV vaccine (40% for 3-dose completion among females) (Reagan-Steiner et al., 2015). Primary healthcare providers are central to efforts to increase adolescent vaccination.
1.1. Patient-provider communication and vaccination
Healthcare exists in a social context, and previous research has highlighted the potent influence of primary care providers’ recommendations on uptake of vaccines (Dorell, Yankey, Kennedy, & Stokley, 2013; Small, Sampselle, Martyn, & Dempsey, 2013). Healthcare is characterized by steep power imbalances between providers and patients. In such settings, patients often look to providers for expert advice and care. Providers’ recommendations act as a cue to action (Hochbaum, 1958; Skinner, Tiro, & Champion, 2015), a potent, timely intervention, since vaccines are available on the spot in many healthcare providers’ offices and practices. Few studies have gone beyond examining provider recommendations to assess the potential impact of how providers and patients talk about vaccines. In the context of adolescent vaccines, when patients are generally aged 17 or younger, parents also are part of the conversation; thus, when we refer to “patients,” we include adolescents and their parents or other caregivers.
A useful framework for understanding these patient-provider interactions is the collaborative communication continuum proposed by Charles, Gafni, and colleagues (1997; 1999; 2006). Generally, this continuum captures different modes of communication according to how patient- or provider-driven the conversation is across three dimensions: information exchange, deliberation, and deciding on which treatment to implement. A patient-driven conversation, called “informed,” involves one-way information flow from provider to patient (theoretically giving the patient all the information needed to make an informed decision independently), but deliberating and deciding on a treatment option is completely the patient’s responsibility. The opposite extreme on this continuum is a provider-driven conversation, called “paternalistic,” which involves one-way information flow from provider to patient (perhaps only the minimum amount required for a patient to be able to give consent), but deliberating and deciding on a treatment option is completely the provider’s responsibility. Finally, a mid-point on the continuum is collaboration between patient and provider, called “shared,” which involves two-way exchange of information and joint efforts to deliberate and decide on a treatment option (Charles et al., 1999).
Researchers in public health and healthcare have examined the acceptability of some of these communication styles, primarily regarding shared and paternalistic styles. Shared patient-provider communication, which has become more accepted in the last few decades, honors patients’ decision-making autonomy (Levinson, Lesser, & Epstein, 2010; Lidz, Appelbaum, & Meisel, 1988; Quill & Brody, 1996; Vermeersch, 1999; Whitney, McGuire, & McCullough, 2004), especially when healthcare options are complex and/or lack professional consensus (Braddock, Fihn, Levinson, Jonsen, & Pearlman, 1997; Braddock, Edwards, Hasenberg, Laidley, & Levinson, 1999; Elwyn, Edwards, Gwyn, & Grol, 1999; Tzeng et al., 2010). In the context of routine vaccinations, bidirectional or two-way information exchange and joint deliberation and decision making can be particularly useful. Parents often report needing more information before consenting to their children receiving vaccines (Bartlett & Peterson, 2011; Gust et al., 2005). Shared communication allows providers to give information in a way that addresses patients’ values (Bartlett & Peterson, 2011; Charles et al., 1999). Use of a shared communication style has been associated with improved clinical outcomes, such as better medication adherence (Coletti et al., 2012; Francis, Korsch, & Morris, 1969) and diabetes self-management (Rathert, Wyrwich, & Boren, 2013).
In contrast, paternalistic communication maps on to a traditional model for patient-provider interactions. This technique is time-efficient (Lidz et al., 1988; Tenrreiro, 2005) and highly acceptable to (and even preferred by) many patients (Arora & McHorney, 2000). Ethicists and medical scholars have suggested that a paternalistic communication approach is acceptable when providers and patients consider healthcare options that are minimally invasive, highly efficacious, and marked by professional consensus (Braddock et al., 1999; Whitney, 2003; Whitney et al., 2004), such as routine vaccinations. A paternalistic communication style may lead to fewer parents opting out of vaccination for their children (Hughes, Jones, Feemster, & Fiks, 2011; Opel et al., 2013). For example, Opel and colleagues (2013) found that 74% of parents accepted flu vaccinations for their infants if providers used paternalistic (or “directive”) communication styles versus 4% of parents whose providers used patient-driven collaborative styles. However, it is unclear whether these results generalize to adolescent vaccinations.
1.2. Hypotheses
Drawing upon research discussed in the previous section, we formulated three hypotheses about the relationships between patient-provider communication and uptake of adolescent vaccines.
First, provider recommendations for vaccination would be positively associated with uptake (Hypothesis 1). Physicians have specialized and extensive training, may have ongoing relationships with adolescent patients and their families, and are well trusted. Thus, adolescents and their parents may be likely to follow the advice of their providers when making vaccination decisions. Across the adolescent vaccination literature, provider recommendation is one of the strongest and most consistent correlates of uptake, likely because it is a behavioral cue (Hochbaum, 1958; Skinner et al., 2015) and the means for action (opportunity, capability, and motivation) (Michie, van Stralen, & West, 2011) are all present. Thus, we expected to find a similar relationship in our study.
Next, we proposed two competing hypotheses regarding the direction of the association between communication style and vaccination. It is unclear what communication style (informed versus shared versus paternalistic) is the best way for providers to communicate with parents in order to achieve high vaccine acceptance. All three approaches are characterized by unique strengths and weaknesses, and previous empirical studies have found evidence of relationships between shared and paternalistic styles and improved healthcare outcomes.
We hypothesized that more patient-driven patient-provider communication styles would be associated with higher adolescent vaccination than other types of communication (Hypothesis 2). Patient-driven communication offers parents and adolescents adequate time to process information about vaccination and gives providers the opportunity to persuade vaccine-hesitant parents. This style of communication also respects the decision-making authority of adolescent patients and their parents, and it could increase their trust and satisfaction with healthcare providers. These processes could lead to higher vaccination compared to a more provider-driven communication style.
Finally, to compete with Hypothesis 2, we hypothesized that more patient-driven patient-provider communication styles would be associated with lower adolescent vaccination than other types of communication (Hypothesis 3), a relationship demonstrated in the context of infant vaccination (Opel et al., 2013). In patient-driven communication, deliberating and deciding on a treatment option is partly or completely the responsibility of adolescents and their parents. This approach affords parents and adolescents more opportunities to object and opt out of vaccination. Patient-driven communication may also suggest professional ambivalence about vaccination or that vaccination is not routine, and as a result, problematize and discourage vaccination. These processes could lead to lower vaccination compared to a more provider-driven communication style.
Methods
2.1. Procedures
Data came from the 2010 National Immunization Survey (NIS)-Teen, implemented by the CDC (2015a). NIS-Teen included phone interviews with a national sample of caretakers of 13- to 17-year-old adolescents (hereafter called “parents”), during which parents reported the vaccination history of a randomly-selected adolescent in the household. At the end of the interview, NIS-Teen staff asked for consent to contact adolescents’ primary healthcare providers to verify vaccination history with written surveys. Among 39,811 eligible parents that NIS-Teen staff contacted, 32,429 (82% of those contacted) completed interviews. Of these, 23,738 (73% of those interviewed) consented to provider verification, and NIS-Teen staff mailed surveys to the healthcare practices of all identified providers. Practices returned written surveys on the vaccination history of 19,257 adolescents (81% of those who consented). NIS-Teen staff developed sampling weights for each participant in the sample with provider-verified vaccination history to account for non-equal probability of selection.
During the final two quarters of the 2010 survey year, 11,860 participants from the 50 states and the District of Columbia completed the Parental Attitudes Module, a supplementary set of items measuring parents’ attitudes, beliefs, and experiences regarding adolescent vaccines, including patient-provider communication (Centers for Disease Control and Prevention (CDC), 2015a). Among these participants, 9,194 (77.5%) had provider verification of vaccination history. We used data from this sample in the current study. We excluded participants who had missing data for all communication items (n = 173), for a final analytic sample of 9,021.
The National Center for Health Statistics (NCHS) Research Ethics Review Board approved data collection for NIS-Teen. Analysis of de-identified data from the survey is exempt from federal regulations for the protection of human research participants. Analysis of restricted data through the NCHS Research Data Center is also approved by the NCHS ERB. The Institutional Review Board at the University of North Carolina exempted this study from review.
2.2. Measures
2.2.1. Patient-provider communication
Parents answered one item about provider recommendation for each vaccine (three items in total). These items read: “Has a doctor or other healthcare professional ever recommended that [teen name] receive [vaccine]?” (Centers for Disease Control and Prevention (CDC), 2015a). For each adolescent vaccine, we coded participants as 1 if they received a provider’s recommendation and 0 for all other responses.
In addition, parents answered three items about conversations with their adolescents’ healthcare providers for each vaccine (Tdap booster, meningococcal vaccine, and HPV vaccine; nine items in total). These items mapped on to three components of patient-provider communication described by Charles and Gafni (1997; 1999; 2006): information exchange, deliberation, and decision. Items began with “At visits made for [teen name]’s vaccinations, did [his/her] healthcare provider…” and ended with “…talk to you about [vaccine]?” (information exchange); “…give you enough time to discuss [vaccine]?” (deliberation); and “…play a role in your decision to get [teen name] vaccinated or not to get [teen name] vaccinated with [vaccine]?” (decision) (Centers for Disease Control and Prevention (CDC), 2015a).
Separately for each vaccine, we classified patient-provider communication into one of three categories: informed, shared, or paternalistic. According to Charles and Gafni (1997; 1999; 2006), an informed communication style involves information exchange and deliberation, but not decision. Therefore, we categorized conversations as involving an informed style if parents responded “yes” to the information exchange and deliberation items, but did not respond “yes” to the decision item. A shared communication style involves all three components; we categorized conversations as shared if parents responded “yes” to the information exchange, deliberation, and decision items. Finally, a paternalistic style involves information exchange and decision, but not deliberation; we categorized conversations as paternalistic if parents responded “yes” to the information exchange and decision items, but not the deliberation item. We hereafter refer to the paternalistic category as “efficient” because of the negative connotations some ascribe to the term “paternalistic.” We defined communication styles using these categories, as well as a final, “other” category for participants who reported different combinations of the communication components.
Because of collinearity between provider recommendation for vaccines and communication style (e.g., 90% of parents reporting a shared communication style also reported provider recommendations), we created a five-level variable to incorporate both constructs into a single predictor variable. The reference group was no provider recommendation. If parents did not report that a provider recommended a particular vaccine to them, we put them in this category. The remaining levels for this variable are provider recommendation plus informed, shared, efficient, or other communication style, as defined above.
2.2.2. Vaccination status
NIS-Teen measured parental reports of receipt of Tdap booster, meningococcal vaccine, and HPV vaccine and verified these reports with providers’ records. We classified adolescents as having received each vaccine if their healthcare providers verified administration in the written survey. For HPV vaccine, we measured initiation (i.e., receipt of at least one dose) of the three-dose series among females only, following the operationalization in previous studies (Gilkey, Moss, McRee, & Brewer, 2012; Moss, Gilkey, Reiter, & Brewer, 2012; Reiter et al., 2013) and in the CDC’s publications using NIS-Teen data (Centers for Disease Control and Prevention (CDC), 2011). Analyses involving HPV vaccination excluded male adolescents because of the low vaccine coverage among males (1.4%) in 2010 (Centers for Disease Control and Prevention (CDC), 2011). National guidelines in 2008 gave a permissive recommendation for HPV vaccination of males, and in 2011, the guidelines expanded to recommend routine administration (Centers for Disease Control and Prevention (CDC), 2015b).
2.2.3. Control variables
In addition to the primary study variables, we examined characteristics of adolescents, parents, and their households (Table 1). Adolescent characteristics were sex, age at the time of interview, race/ethnicity, and whether they had private health insurance, had a preventive check-up in the last year, and had a well-child check-up at age 11 or 12. Parent characteristics were relationship of the respondent to the index adolescent, mother’s age, and mother’s education level. Household characteristics were census region, urbanicity, annual income, and number of children in the household. Parents reported all of these variables in the NIS-Teen phone interviews.
Table 1.
Characteristics of participants and their children, Parental Attitudes Module, National Immunization Survey (NIS)-Teen, 2010.
| Total | Total Sample | Male | Female | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
|
| ||||||
| 9,021 | 4,709 | 51.8 | 4,312 | 48.2 | ||
|
Adolescent characteristics
| ||||||
| Age | ||||||
| 13 | 1,824 | 19.1 | 961 | 19.4 | 863 | 18.8 |
| 14 | 1,859 | 19.4 | 933 | 19.2 | 926 | 19.7 |
| 15 | 1,836 | 20.9 | 969 | 20.4 | 867 | 21.5 |
| 16 | 1,877 | 21.7 | 997 | 22.9 | 880 | 20.4 |
| 17 | 1,625 | 18.9 | 849 | 18.1 | 776 | 19.7 |
| Race/ethnicity | ||||||
| Hispanic | 1,152 | 18.2 | 596 | 19.5 | 556 | 16.7 |
| Non-Hispanic white | 6,196 | 59.5 | 3,240 | 58.5 | 2,956 | 60.6 |
| Non-Hispanic black | 928 | 14.8 | 481 | 14.6 | 447 | 15.1 |
| Other | 745 | 7.5 | 392 | 7.4 | 353 | 7.6 |
| Private health insurance | ||||||
| No | 2,921 | 39.0 | 1,519 | 39.9 | 1,402 | 38.0 |
| Yes | 6,100 | 61.0 | 3,190 | 60.1 | 2,910 | 62.0 |
| Preventive check-up in last year | ||||||
| No | 1,284 | 15.0 | 696 | 16.5 | 588 | 13.4 |
| Yes | 7,737 | 85.0 | 4,013 | 83.5 | 3,724 | 86.6 |
| Well child check-up at age 11–12 | ||||||
| No | 861 | 11.2 | 462 | 12.0 | 399 | 10.3 |
| Yes | 6,755 | 88.8 | 3,518 | 88.0 | 3,237 | 89.7 |
|
| ||||||
|
Parent characteristics
| ||||||
| Relationship of respondent to adolescent | ||||||
| Mother/female guardian | 7,200 | 76.8 | 3,699 | 74.0 | 3,501 | 79.7 |
| Father/male guardian | 1,413 | 16.7 | 795 | 19.0 | 618 | 14.2 |
| Other | 408 | 6.5 | 215 | 7.0 | 193 | 6.0 |
| Mother’s age | ||||||
| ≤ 34 years | 646 | 7.7 | 339 | 7.8 | 307 | 7.7 |
| 35–44 years | 3,655 | 44.3 | 1,931 | 44.6 | 1,724 | 43.9 |
| ≥ 45 years | 4,720 | 48.0 | 2,439 | 47.6 | 2,281 | 48.4 |
| Mother’s education level | ||||||
| Less than 12 years | 781 | 12.0 | 404 | 12.9 | 377 | 11.0 |
| 12 years | 1,856 | 26.3 | 984 | 26.4 | 872 | 26.1 |
| More than 12 years, non-college grad | 2,623 | 26.1 | 1,341 | 25.1 | 1,282 | 27.2 |
| College graduate | 3,761 | 35.6 | 1,980 | 35.6 | 1,781 | 35.7 |
|
| ||||||
|
Household characteristics
| ||||||
| Census region | ||||||
| Northeast | 1,850 | 18.2 | 959 | 18.1 | 891 | 18.4 |
| Midwest | 1,953 | 21.3 | 990 | 20.5 | 963 | 22.1 |
| South | 3,285 | 36.7 | 1,749 | 37.3 | 1,536 | 36.0 |
| West | 1,933 | 23.8 | 1,011 | 24.1 | 922 | 23.5 |
| Urbanicity | ||||||
| Metro | 6,971 | 84.2 | 3,661 | 83.6 | 3,310 | 84.9 |
| Non-metro | 2,050 | 15.8 | 1,048 | 16.4 | 1,002 | 15.1 |
| Annual income | ||||||
| Below poverty level | 1,296 | 18.4 | 675 | 18.9 | 621 | 18.0 |
| Above poverty level, ≤$75,000 | 3,493 | 38.5 | 1,839 | 39.2 | 1,654 | 37.8 |
| Above poverty level, >$75,000 | 3,872 | 37.4 | 2,012 | 35.9 | 1,860 | 39.0 |
| Unknown | 360 | 5.7 | 183 | 6.1 | 177 | 5.3 |
| Number of children in household | ||||||
| 1 | 3,567 | 31.6 | 1,886 | 31.7 | 1,681 | 31.5 |
| 2–3 | 4,612 | 55.7 | 2,404 | 55.0 | 2,208 | 56.5 |
| 4 or more | 842 | 12.7 | 419 | 13.3 | 423 | 12.0 |
2.3. Statistical analysis
We used chi-square tests to examine the bivariate associations of vaccine uptake with each of the control variables (data not shown). We included all the control variables that demonstrated statistically-significant associations with vaccination (adolescent age, sex, and insurance status) in the multivariable models (Elam-Evans et al., 2014; Moss et al., 2012; Zimet et al., 2005). Because analysis of HPV vaccination was limited to female adolescents, that model did not control for adolescent sex.
To test our hypotheses, we used multivariable logistic regression models to examine the associations of communication style (predictor) with uptake of each adolescent vaccination (outcome), including the control variables. Logistic regression analyses used listwise deletion to exclude participants with missing data on any of the variables in that model (Tdap booster: 188/9,021 excluded, or 2.1%; meningococcal vaccine: 309/9,021 excluded, or 3.4%; and HPV vaccine: 191/4,312 excluded, or 4.4%). To test Hypothesis 1, we examined the difference in vaccine uptake of patients reporting no provider recommendation for vaccination versus patients reporting provider recommendations (combining the informed, shared, efficient, and other groups). To test Hypotheses 2 and 3, we used models comparing uptake across communication styles compared to the no provider recommendation group, using post-hoc tests to compare vaccine uptake among patients who reported the three communication styles described by Charles and Gafni (1997; 1999; 2006) and the “other” communication style.
Analyses were conducted in SAS version 9.2 (Cary, NC). Statistical tests used a two-tailed critical p value of .05. Analyses controlled for clustering of observations within states and incorporated survey weights provided by NIS-Teen to account for non-equal probability of selection. We report unweighted frequencies and weighted proportions.
Results
Adolescents were nearly evenly split between male (52%) and female (48%) (Table 1). Most adolescents were non-Hispanic white (60%), and 61% had private health insurance. Vaccination among this sample was similar to rates of uptake for the entire population in 2010 (Centers for Disease Control and Prevention (CDC), 2011): 73% of adolescents had received Tdap boosters, 66% had received meningococcal vaccines, and 49% of female adolescents had initiated HPV vaccination.
For Tdap boosters, 35% of parents reported that they had not received a provider recommendation for the vaccine (Table 2). Overall, 12% of parents reported provider recommendations and an informed communication style, 43% reported recommendations and a shared style, and 2% reported recommendations and an efficient style. Compared to adolescents whose parents reported no provider recommendation, Tdap booster uptake was higher among adolescents whose parents reported provider recommendations (76% vs. 67%, p < .001). In multivariable analyses, three communication styles were associated with increased odds of Tdap booster uptake compared to no provider recommendation: informed (uptake = 76%; odds ratio [OR] = 1.61, 95% confidence interval [CI] = 1.16, 2.22); shared (uptake = 76%; OR = 1.53, 95% CI = 1.26, 1.86); and efficient (uptake = 78%; OR = 1.77, 95% CI = 1.01, 3.09) (Table 3). The three theoretically-defined communication styles (informed, shared, and efficient) did not differ in their associations with vaccine coverage (all ps > .05) (Figure 1).
Table 2.
Prevalence of patient-provider communication styles in conversations about adolescent vaccines, based on parental report.
| Tdap (N=8,833) | Meng (N=8,712) | HPV1 (N=4,121) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
|
| ||||||
| No recommendation | 2,884 | 34.6 | 3,970 | 46.3 | 1,202 | 30.5 |
| Recommendation and informed communication | 972 | 11.8 | 762 | 9.1 | 704 | 16.0 |
| Recommendation and shared communication | 3,988 | 43.0 | 3,418 | 38.1 | 2,049 | 48.5 |
| Recommendation and efficient communication | 200 | 2.4 | 90 | 1.3 | 40 | 1.5 |
| Recommendation and other communication | 789 | 8.1 | 472 | 5.3 | 126 | 3.4 |
Note. Tdap=tetanus, diphtheria, and pertussis booster; Meng=meningococcal vaccine; HPV=human papillomavirus vaccine.
First dose among female adolescents only.
Table 3.
Associations of communication style and adolescent vaccine uptake.
| Tdap | Meng | HPV1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n vacc’d/N | % | OR | 95% CI | n vacc’d/N | % | OR | 95% CI | n vacc’d/N | % | OR | 95% CI | |
|
| ||||||||||||
| No recommendation | 1,847/2,884 | 67.0 | (ref) | 2,061/3,970 | 54.3 | (ref) | 285/1,202 | 22.3 | (ref) | |||
| Recommendation and informed communication | 753/972 | 76.3 | 1.61 | (1.16, 2.22)* | 542/762 | 68.0 | 1.78 | (1.33, 2.39)** | 246/704 | 33.4 | 1.81 | (1.27, 2.58)** |
| Recommendation and shared communication | 3,093/3,988 | 76.2 | 1.53 | (1.26, 1.86)** | 2,710/3,418 | 76.8 | 3.29 | (2.74, 3.94)** | 1,473/2,049 | 70.4 | 8.61 | (6.25, 11.86)** |
| Recommendation and efficient communication | 149/200 | 78.3 | 1.77 | (1.01, 3.09)* | 69/90 | 81.8 | 3.84 | (1.63, 9.04)* | 25/40 | 89.5 | 31.45 | (10.60, 93.34)** |
| Recommendation and other communication | 578/789 | 72.1 | 1.27 | (0.96, 1.69) | 319/472 | 67.9 | 1.77 | (1.28, 2.45)** | 65/126 | 50.2 | 3.28 | (1.40, 7.69)** |
Note. Analyses controlled for adolescent age and insurance status; Tdap and Meng models also controlled for adolescent sex. Tdap=tetanus, diphtheria, and pertussis booster; Meng=meningococcal vaccine; HPV=human papillomavirus vaccine; vacc’d=vaccinated.
First dose among female adolescents only.
p<.05;
p<.001.
Figure 1.
Association of communication style with vaccine uptake, among adolescents who received recommendations for vaccination. Error bars show standard errors. Tdap=tetanus, diphtheria, and pertussis booster; Meng=meningococcal vaccine; HPV=human papillomavirus vaccine (first dose among female adolescents only). *p<.05; **p<.001.
For meningococcal vaccines, 46% of parents reported that they had not received a provider recommendation for the vaccine (Table 2). Overall, 9% of parents reported provider recommendations and an informed communication style, 38% reported recommendations and a shared style, and 1% reported recommendations and an efficient style. Compared to adolescents whose parents reported no provider recommendation, meningococcal vaccine uptake was higher among adolescents whose parents reported provider recommendations (77% vs. 54%, p < .001). In multivariable analyses, all four communication styles were associated with increased odds of meningococcal vaccine uptake compared to no provider recommendation: informed (uptake = 68%; OR = 1.78, 95% CI = 1.33, 2.39); shared (uptake = 77%; OR = 3.29, 95% CI = 2.74, 3.94); efficient (uptake = 82%; OR = 3.84, 95% CI = 1.63, 9.04); and other (uptake = 68%; OR = 1.77, 95% CI = 1.28, 2.45) (Table 3). Among the three theoretically-defined communication styles, parental report of a shared communication style was associated with higher meningococcal vaccine uptake than for an informed style (p < .001), but no other differences emerged (Figure 1).
Finally, for HPV vaccines, 31% of parents of female adolescents reported that they had not received a provider recommendation for the vaccine (Table 2). Overall, 16% of parents reported provider recommendations and an informed communication style, 49% reported recommendations and a shared style, and 2% reported recommendations and an efficient style. Compared to adolescents whose parents reported no provider recommendation, HPV vaccine uptake was higher among adolescents whose parents reported provider recommendations (61% vs. 22%, p < .001). In multivariable analyses, all four communication styles were associated with increased odds of HPV vaccine uptake compared to no provider recommendation: informed (uptake = 33%; OR = 1.81, 95% CI = 1.27, 2.58); shared (uptake = 70%; OR = 8.61, 95% CI = 6.25, 11.86); efficient (uptake = 90%; OR = 31.45, 95% CI = 10.60, 93.34); and other (uptake = 50%; OR = 3.28, 95% CI = 1.40, 7.69) (Table 3). Among the three theoretically-defined communication styles, HPV vaccine uptake was lowest for an informed style, higher for a shared style, and higher still for an efficient style (p < .05 for each comparison) (Figure 1).
Discussion
Dimensions of communication between providers and patients, including recommendation and style, are important for achieving high levels of adolescent vaccine coverage. In a nationally-representative sample of U.S. adolescents, we found evidence of consistent positive associations between provider recommendations and vaccine uptake, and, for meningococcal and HPV vaccines, between more provider-driven communication styles and vaccine uptake. Indeed, the highest rates of vaccine uptake emerged in the group of adolescents whose parents reported provider recommendations and an efficient (provider-driven) communication style. These findings have important implications for adolescent preventive healthcare and public health.
In support of Hypothesis 1, we found that providers’ recommendations for vaccination were associated with higher rates of uptake for Tdap booster, meningococcal vaccine, and HPV vaccine. Specifically, a provider recommendation was associated with a 9% absolute increase in uptake for Tdap booster, 23% for meningococcal vaccine, and 39% for HPV vaccine. This finding builds upon previous studies, including studies using NIS-Teen data, that have identified the importance of providers’ recommendations (Dorell et al., 2013; Small et al., 2013).
In addition, provider recommendation was associated with increased vaccination regardless of the communication style that providers used. Many previous studies have suggested that additional training is needed for primary care providers regarding how to engage parents and patients in conversations about vaccines (Dorell, Yankey, & Strasser, 2011; Dorell et al., 2013; Hughes et al., 2011; Omer, Salmon, Orenstein, deHart, & Halsey, 2009), and our results underscore the importance of providers’ recommendations regardless of their communication styles. In addition, our findings offer support for Hypothesis 3 but not Hypothesis 2: Adolescent vaccination was higher when parents who received a provider recommendation reported more provider-driven communication styles. Notably, though, this relationship only emerged for meningococcal vaccine (for shared versus informed communication) and HPV vaccine (for efficient versus shared versus informed communication). Uptake of Tdap booster did not vary by communication style. However, although the efficient style was quite rare (1 – 2% of parents reported this style), descriptively, it was associated with the highest rates of coverage for all three vaccines. The association was particularly strong for HPV vaccination: uptake reached 90% for female adolescents whose parents reported a recommendation and an efficient style (Figure 1). This latter figure is particularly striking, given that national HPV vaccination coverage (one or more dose) among female adolescents at the time of data collection was only 49% (Centers for Disease Control and Prevention (CDC), 2011). Efficient patient-provider communication may also improve completion of the three-dose HPV vaccine series. Future studies should examine this possibility.
These findings build on conceptual work by Charles and Gafni (1997; 1999; 2006) in that we observed a graded difference in vaccination behaviors across the collaborative communication continuum (for HPV vaccine and partially for meningococcal vaccine). In addition, these findings build on the empirical work by Opel (2013; 2015) and others (Hughes et al., 2011) in that more provider-driven (“paternalistic,” “efficient,” “presumptive,” or “directive”) communication was associated with higher rates of vaccination. We could not evaluate the reasons why this pattern emerged, but the contrast between the informed style versus the shared and efficient styles suggests the importance of provider involvement in decision making. We observed that, when providers made decisions about routine adolescent vaccination, either alone or in conjunction with adolescents’ parents, vaccine uptake was higher. Such an interaction style could reassure parents about the safety and effectiveness of adolescent vaccines and imply a behavioral standard or expectation in favor of vaccination. This explanation could also contribute to the striking association between communication and HPV vaccination, a behavior marked by significant negative press (Zimet, Rosberger, Fisher, Perez, & Stupiansky, 2013). To the extent that adolescent vaccination is a medical intervention marked by considerable professional consensus (American Academy of Pediatrics & Bright Futures, ; Centers for Disease Control and Prevention (CDC), 2015b; Department of Health and Human Services, 2015; Hammer et al., 2010), provider-driven communication is appropriate for discussions about adolescent vaccination (Braddock et al., 1997; Braddock et al., 1999; Whitney, 2003; Whitney et al., 2004). The lack of a statistically significant association between communication style and uptake of Tdap booster could be attributable to ceiling effects, since national coverage for Tdap booster in 2010 was 74%, 10 percentage points higher than coverage for meningococcal vaccine and 35 percentage points higher than coverage for HPV vaccine (Centers for Disease Control and Prevention (CDC), 2011). The difference also could be due to Tdap booster being required for school entry in many states in 2010 (Immunization Action Coalition, 2015); these requirements would reasonably be expected to attenuate most other influences. Future research should use experimental designs to establish causal associations between communication style and vaccination, along with qualitative data collection about patients’, parents’, and providers’ perspectives on how this relationship emerges.
4.1 Strengths and limitations
Study strengths include a large, nationally-representative sample, allowing us to evaluate relationships between study variables in a diverse population. In addition, provider-verified adolescent vaccination records give us confidence in the validity of our dependent variable. Limitations include the cross-sectional nature of analysis, which precluded our ability to draw causal inferences about the proposed relationships. Another limitation is that the data come from the 2010 NIS-Teen questionnaire. In the intervening years, vaccination coverage increased, and the CDC began recommending routine administration of HPV vaccine to both female and male adolescents (Centers for Disease Control and Prevention (CDC), 2015b). As a result, the context in which vaccination takes place now is different than in 2010. However, we have no reason to believe the relationships described in this study have changed. Additionally, the informed and, especially, the efficient communication groups were quite small, which reduced our power to detect differences among communication styles.
Measures of patient-provider communication only captured parents’ perceptions, and not the providers’ (or the adolescents’). To the extent that these perceptions diverge, the relationship between communication style and vaccination may vary. Items began with a stem stating “At visits for made for [teen’s name]’s vaccinations…” and parents may have interpreted that to exclude conversations during healthcare visits that did not exclusively focus on vaccination (e.g., sick visits). A related point about respondents’ interpretations of questionnaire items is that parents may not have reflected on the same provider or the same healthcare encounter when answering items assessing communication style and recommendation for a given vaccine, a phenomenon that likely introduced noise into the measurement of our predictor variables. Given that our findings are based on secondary data analysis, the survey items were an approximate but not precise fit to the Charles and Gafni conceptualization. Future studies should attempt to better understand different communication styles and their unique effects on vaccination. This focus is important since it appears that not only whether healthcare providers recommend vaccination but how they recommend vaccination is important.
4.2 Conclusions
In conclusion, uptake of adolescent vaccines was higher when parents reported that providers recommended the vaccines and, for meningococcal and HPV vaccines, that they used provider-driven communication styles (i.e., shared and efficient communication). Both dimensions of patient-provider communication were associated with high levels of vaccination that approached or surpassed Healthy People 2020 goals for Tdap booster and meningococcal vaccination (Department of Health and Human Services, 2015). These findings highlight the need for experimental studies that examine the causal effects of patient-provider communication on adolescent vaccination.
Highlights.
Some adolescent vaccination rates do not meet national guidelines.
Leveraging patient-provider communication could increase vaccination.
Vaccination was higher when parents reported receiving providers’ recommendations.
Vaccination was higher when parents reported more provider-driven communication.
Efficient communication was rare but effective at increasing uptake.
Acknowledgments
Funding source: This study was supported by an NIH grant (F31 CA189411; PI: Moss). The funder had no role in study design; in the collection, analysis, and interpretation of data; in writing the manuscript; or in the decision to submit it for publication.
We thank Dr. Melissa Gilkey for her help in conceptualizing the paper. This study was supported by an NIH grant (F31 CA189411; PI: Moss). The research in this article was conducted while JLM was a Special Sworn Status researcher of the U.S. Census Bureau at the Center for Economic Studies. All results have been reviewed by the National Center for Health Statistics to ensure that no confidential information is disclosed. Research results and conclusions expressed are those of the authors and do not necessarily reflect the views of the National Cancer Institute or the National Center for Health Statistics.
Footnotes
Conflicts of interest: JLM and BKR have no conflicts of interest to disclose. PLR has received a research grant from Merck Sharp & Dohme Corp. PLR has also received a research grant from Cervical Cancer-Free America, via an unrestricted educational grant from GlaxoSmithKline. NTB has served on paid advisory boards or received research grants from Merck, GSK, CDC, and FDA, and now serves as chair of the CDC-funded National HPV Vaccination Roundtable. These entities had no role in the study design, data analysis, or reporting of the results.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Academy of Pediatrics, & Bright Futures. Recommendations for preventive pediatric health care. Retrieved from http://brightfutures.aap.org/pdfs/AAP%20Bright%20Futures%20Periodicity%20Sched%20101107.pdf.
- Arora NK, McHorney CA. Patient preferences for medical decision making: Who really wants to participate? Medical Care. 2000;38(3):335–341. doi: 10.1097/00005650-200003000-00010. [DOI] [PubMed] [Google Scholar]
- Bartlett JA, Peterson JA. The uptake of human papillomavirus (HPV) vaccine among adolescent females in the United States: A review of the literature. The Journal of School Nursing: The Official Publication of the National Association of School Nurses. 2011;27(6):434–446. doi: 10.1177/1059840511415861. [DOI] [PubMed] [Google Scholar]
- Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: Time to get back to basics. JAMA. 1999;282(24):2313–2320. doi: 10.1001/jama.282.24.2313. joc91394. [DOI] [PubMed] [Google Scholar]
- Braddock CH, 3rd, Fihn SD, Levinson W, Jonsen AR, Pearlman RA. How doctors and patients discuss routine clinical decisions. Informed decision making in the outpatient setting. Journal of General Internal Medicine. 1997;12(6):339–345. doi: 10.1046/j.1525-1497.1997.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) National and state vaccination coverage among adolescents aged 13 through 17 years--United States, 2010. MMWR Morbidity and Mortality Weekly Report. 2011;60(33):1117–1123. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) National Immunization Survey: Datasets for the National Immunization Survey-Teen. 2015a Retrieved from http://www.cdc.gov/nchs/nis/data_files_teen.htm.
- Centers for Disease Control and Prevention (CDC) Recommendations and guidelines: Advisory Committee on Immunization Practices. 2015b Retrieved from http://www.cdc.gov/vaccines/acip/index.html.
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (Or it takes at least two to tango) Social Science & Medicine (1982) 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: Revisiting the shared treatment decision-making model. Social Science & Medicine (1982) 1999;49(5):651–661. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- Coletti DJ, Pappadopulos E, Katsiotas NJ, Berest A, Jensen PS, Kafantaris V. Parent perspectives on the decision to initiate medication treatment of attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 2012;22(3):226–237. doi: 10.1089/cap.2011.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services. Immunization and infectious diseases. 2015 Retrieved from http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- Dorell C, Yankey D, Kennedy A, Stokley S. Factors that influence parental vaccination decisions for adolescents, 13 to 17 years old: National Immunization Survey-Teen, 2010. Clinical Pediatrics. 2013;52(2):162–170. doi: 10.1177/0009922812468208. [DOI] [PubMed] [Google Scholar]
- Dorell C, Yankey D, Strasser S. Parent-reported reasons for nonreceipt of recommended adolescent vaccinations, National Immunization Survey: Teen, 2009. Clinical Pediatrics. 2011;50(12):1116–1124. doi: 10.1177/0009922811415104. [DOI] [PubMed] [Google Scholar]
- Elam-Evans LD, Yankey D, Jeyarajah J, Singleton JA, Curtis RC, MacNeil J … Immunization Services Division, National Center for Immunization and Respiratory Diseases. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years - United States, 2013. MMWR Morbidity and Mortality Weekly Report. 2014;63(29):625–633. mm6329a4. [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, Edwards A, Gwyn R, Grol R. Towards a feasible model for shared decision making: Focus group study with general practice registrars. BMJ (Clinical Research Ed) 1999;319(7212):753–756. doi: 10.1136/bmj.319.7212.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication. Patients’ response to medical advice. The New England Journal of Medicine. 1969;280(10):535–540. doi: 10.1056/NEJM196903062801004. [DOI] [PubMed] [Google Scholar]
- Gilkey MB, Moss JL, McRee AL, Brewer NT. Do correlates of HPV vaccine initiation differ between adolescent boys and girls? Vaccine. 2012;30(41):5928–5934. doi: 10.1016/j.vaccine.2012.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers the role of information. American Journal of Preventive Medicine. 2005;29(2):105–112. doi: 10.1016/j.amepre.2005.04.010. [DOI] [PubMed] [Google Scholar]
- Hammer LD, Curry ES, Harlor AD, Laughlin JJ, Leeds AJ, Lessin HR … Council on Community Pediatrics. Increasing immunization coverage. Pediatrics. 2010;125(6):1295–1304. doi: 10.1542/peds.2010-0743. [DOI] [PubMed] [Google Scholar]
- Hochbaum GM. Public participation in medical screening programs: A socio-psychological study. US Department of Health, Education, and Welfare, Public Health Service, Bureau of State Services, Division of Special Health Services, Tuberculosis Program; 1958. [Google Scholar]
- Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: A semi-structured interview study. BMC Pediatrics. 2011;11:74. doi: 10.1186/1471-2431-11-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immunization Action Coalition. State information: State mandates on immunization and vaccine-preventable diseases. 2015 Retrieved from http://www.immunize.org/laws/
- Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Affairs (Project Hope) 2010;29(7):1310–1318. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- Lidz CW, Appelbaum PS, Meisel A. Two models of implementing informed consent. Archives of Internal Medicine. 1988;148(6):1385–1389. [PubMed] [Google Scholar]
- Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science : IS. 2011;6 doi: 10.1186/1748-5908-6-42. 42-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss JL, Gilkey MB, Reiter PL, Brewer NT. Trends in HPV vaccine initiation among adolescent females in North Carolina, 2008–2010. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology. 2012;21(11):1913–1922. doi: 10.1158/1055-9965.EPI-12-0509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E, Charles C, Gafni A. Shared decision-making in primary care: Tailoring the Charles et al. model to fit the context of general practice. Patient Education and Counseling. 2006;62(2):205–211. doi: 10.1016/j.pec.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. The New England Journal of Medicine. 2009;360(19):1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- Opel DJ, Heritage J, Taylor JA, Mangione-Smith R, Salas HS, Devere V, … Robinson JD. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037–1046. doi: 10.1542/peds.2013-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel DJ, Mangione-Smith R, Robinson JD, Heritage J, DeVere V, Salas HS, … Taylor JA. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. American Journal of Public Health. 2015:e1–e7. doi: 10.2105/AJPH.2014.302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quill TE, Brody H. Physician recommendations and patient autonomy: Finding a balance between physician power and patient choice. Annals of Internal Medicine. 1996;125(9):763–769. doi: 10.7326/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: A systematic review of the literature. Medical Care Research and Review : MCRR. 2013;70(4):351–379. doi: 10.1177/1077558712465774. [DOI] [PubMed] [Google Scholar]
- Reagan-Steiner S, Yankey D, Jeyarajah J, Elam-Evans LD, Singleton JA, Curtis CR, … Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 Years–United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(29):784–792. doi: 10.15585/mmwr.mm6429a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter PL, McRee AL, Pepper JK, Gilkey MB, Galbraith KV, Brewer NT. Longitudinal predictors of human papillomavirus vaccination among a national sample of adolescent males. American Journal of Public Health. 2013;103(8):1419–1427. doi: 10.2105/AJPH.2012.301189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner CS, Tiro JA, Champion VL. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior: Theory, research and practice. 5. CA: Wiley; 2015. [Google Scholar]
- Small SL, Sampselle CM, Martyn KK, Dempsey AF. Journal of the American Association of Nurse Practitioners. 2013. Modifiable influences on female HPV vaccine uptake at the clinic encounter level: A literature review. [DOI] [PubMed] [Google Scholar]
- Tenrreiro KN. Time-efficient strategies to ensure vaccine risk/benefit communication. Journal of Pediatric Nursing. 2005;20(6):469–476. doi: 10.1016/j.pedn.2005.06.012. S0882-5963(05)00238-1. [DOI] [PubMed] [Google Scholar]
- Tzeng JP, Mayer D, Richman AR, Lipkus I, Han PK, Valle CG, … Brewer NT. Women’s experiences with genomic testing for breast cancer recurrence risk. Cancer. 2010;116(8):1992–2000. doi: 10.1002/cncr.24990. [DOI] [PubMed] [Google Scholar]
- Vermeersch E. Individual rights versus societal duties. Vaccine. 1999;17(Suppl 3):S14–7. [PubMed] [Google Scholar]
- Whitney SN. A new model of medical decisions: Exploring the limits of shared decision making. Medical Decision Making: An International Journal of the Society for Medical Decision Making. 2003;23(4):275–280. doi: 10.1177/0272989X03256006. [DOI] [PubMed] [Google Scholar]
- Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Annals of Internal Medicine. 2004;140(1):54–59. doi: 10.7326/0003-4819-140-1-200401060-00012. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Perkins SM, Sturm LA, Bair RM, Juliar BE, Mays RM. Predictors of STI vaccine acceptability among parents and their adolescent children. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2005;37(3):179–186. doi: 10.1016/j.jadohealth.2005.06.004. S1054-139X(05)00280-6. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Preventive Medicine. 2013 doi: 10.1016/j.ypmed.2013.05.013. [DOI] [PubMed] [Google Scholar]