Abstract
The provision of sufficient amounts of dietary proteins is central to muscle health as it ensures the supply of essential amino acids and stimulates protein synthesis. Older persons, in particular, are at high risk of insufficient protein ingestion. Furthermore, the current recommended dietary allowance for protein (0.8 g/kg/day) might be inadequate for maintaining muscle health in older adults, probably as a consequence of “anabolic resistance” in aged muscle. Older individuals therefore need to ingest a greater quantity of protein to maintain muscle function. The quality of protein ingested is also essential to promoting muscle health. Given the role of leucine as the master dietary regulator of muscle protein turnover, the ingestion of protein sources enriched with this essential amino acid, or its metabolite β-hydroxy β-methylbutyrate, is thought to offer the greatest benefit in terms of preservation of muscle mass and function in old age.
Keywords: sarcopenia, frailty, malnutrition, leucine, anorexia, supplementation, amino acid
1. Introduction
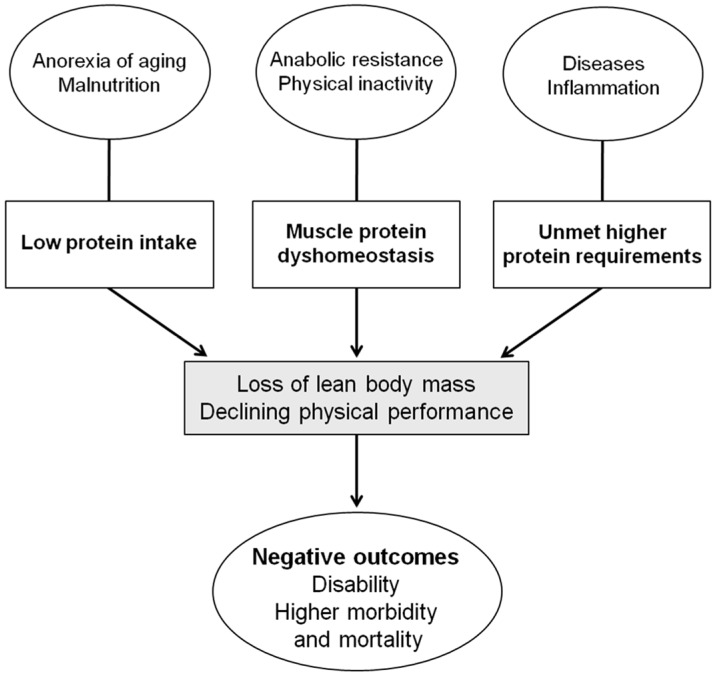
An adequate intake of dietary proteins is vital to maintaining muscle mass as it ensures the provision of essential amino acids and stimulates protein synthesis. Older individuals are at high risk for insufficient protein intake. Furthermore, the current recommended dietary allowance (RDA) for protein (0.8 g/kg/day) might not be sufficient for preserving muscle mass and quality in old age [1]. This, along with the fact that high protein ingestion decreases the risk of perioperative complications [2,3], increases bone mineral density [4,5], and reduces rehabilitation time after an acute disease [6], highlights the importance of optimal protein ingestion in later life. However, it is debated whether the current RDA for protein intake is truly sufficient to avoid major adverse events in older persons, especially in frail, critically ill patients [7]. Given the fact that protein–energy malnutrition is a major risk factor for the development of sarcopenia [8,9,10], a suboptimal nutritional status may mediate the association between sarcopenia and negative clinical outcomes in older and frail individuals (Figure 1).
Figure 1.
Alterations in protein homeostasis during aging and related clinical outcomes.
For example, in the Health, Aging, and Body Composition (Health ABC) Study, older participants in the highest quintile of protein intake lost nearly 40% less appendicular lean mass than did those in the lowest quintile over three years of follow-up, after adjusting for potential confounders [11]. In this respect, it is important to highlight that protein supplementation per se may be sufficient to increase muscle mass in malnourished older inpatients [12]. This effect may clarify, at least partially, the improvement in clinical outcomes observed in older hospitalized persons undergoing specific protein supplementation regimens [7,13]. This evidence emphasizes the central role of nutrition and in particular, the correct level of protein consumption in the management of sarcopenia.
One crucial aspect to consider is that a greater dietary protein intake may be necessary for the promotion of muscle health in older individuals compared with younger persons [7]. Yet, a number of issues related to protein intake and eventually protein supplementation in old age must still be addressed.
2. Putative Mechanisms of Protein Action on Muscle Cells
Skeletal muscle mass is controlled by the complex interaction of many factors; nevertheless, it is indisputable that the balance between protein synthesis and breakdown has an integral role in the process [14]. Significant losses or improvements in muscle mass are therefore primarily the result of persistent changes in muscle protein synthesis rates, breakdown rates, or a combination of both mechanisms. On the other hand, muscle protein metabolism is greatly dependent upon ingesting an adequate amount of proteins and amino acids [15,16].
Muscle protein synthesis rates are controlled predominantly by responsiveness to anabolic stimuli, such as physical activity and food consumption [17]. Dietary protein and/or specific amino acid ingestion largely increases muscle protein synthesis rates and inhibits protein breakdown, thus favoring net muscle protein deposition. In particular, aging does not seem to influence skeletal muscle protein breakdown, autophagy, or the ubiquitin proteasome system, for example following an acute bout of resistance exercise [18]. Therefore, targeting the muscle protein synthesis response may hold more promise in the prevention sarcopenia during the aging process.
The amino acid content of dietary proteins has a significant impact on their anabolic power [19]. In fact, essential amino acids (EAAs) are the main nutritional stimulus for protein synthesis. Leucine is considered the principal dietary regulator of muscle protein anabolism [20], due to its capability to activate the mammalian target of rapamycin (mTOR) pathway and inhibit the proteasome [8]. Even though during the aging process muscle shows a decreased anabolic response to low doses (e.g., 7 g) of EAAs [8], higher doses (e.g., 10–15 g, with at least 3 g of leucine) are able to overcome these anabolic resistances and stimulate a protein synthetic response similar to that mounted by younger adults [8]. Consequently, older individuals should be advised to consume protein sources containing high proportions of EAAs (i.e., high-quality proteins), such as lean meat and dairy-based products, and other leucine-rich foods (e.g., soybeans, peanuts, cowpea, lentils). It is important to highlight that plant-based sources are likely to result in a lower muscle anabolic response upon ingestion when compared with animal-based proteins [21]. In particular, the ingestion of soy protein results in a reduced muscle anabolic response in older individuals relative to the ingestion of whey [22] or beef [23], most likely due to a lower leucine content and/or a lack in specific EEAs, such as methionine and/or lysine.
Anabolic resistance reflects the inability of skeletal muscle to maintain protein mass through the appropriate stimulation of protein synthesis. Recently it has been demonstrated that fast-digesting soluble milk protein improves postprandial muscle protein synthesis especially within the mitochondrial compartment and the myosin fractional synthesis rate, in older persons [24]. At the same time, it should be emphasized that decreased levels of physical activity play a major role in determining muscle anabolic resistance [25]. Indeed, physical inactivity and muscle disuse lead to the rapid development of anabolic resistance in both young and older individuals [26,27,28]. Reduced physical activity is also expected to lower basal muscle protein synthesis rates. Finally, several other lifestyle and biological factors, such as smoking, alcohol abuse, hormonal status, various disease conditions, and chronic inflammation may strongly influence muscle protein metabolism [29,30,31].
Insulin plays a particularly important role in protein metabolism [32]. Amino acids and insulin have a synergistic effect on stimulating muscle protein anabolism [33]. In physiological conditions, maximum protein anabolism occurs throughout the fed state, during which concentrations of insulin and amino acids are higher. In particular, the postprandial increase in insulin to stimulate protein synthesis and to inhibit breakdown is permissive rather than modulatory [34]. The postprandial rise in amino acid concentrations dictates the muscle anabolic response.
3. Dietary Protein Requirements: How Much Protein Is Enough for Older Adults?
A dietary protein requirement is defined as the amount of protein or its constituent amino acids, or both, that must be supplied in one’s diet in order to satisfy metabolic demand and achieve nitrogen equilibrium. For more vulnerable people, like pregnant or lactating women, older and diseased persons, newborns and children, the provision of adequate dietary protein intake is crucial for growth and/or the preservation of muscular homeostasis.
Skeletal muscle mass and functional capacity are controlled by the dynamic interaction of numerous factors, also encompassing diet and nutrition. An adverse yet typical consequence of the aging process is the progressive loss of muscle mass and physical function, named sarcopenia. Although the onset and progression of sarcopenia can be influenced by many factors, a compromised capacity to maintain the anabolic response after dietary protein intake [35] has become a key target for researchers.
Independent of the type of protein and its source, it is important to underline that meals should include an appropriate amount of high-quality protein. In recent years, consensus statements and opinion articles have asserted that protein intake above 0.8 g/kg/day may confer muscle health benefits greater than those conferred by the current RDA [36,37,38,39].
As such, a protein intake of 1.0–1.2 g/kg/day has been recommended for the preservation of healthy aging muscles, while 1.2–1.5 g/kg/day of protein may be necessary in older patients with acute or chronic diseases [7,14,33]. Elderly people with severe illness or malnutrition may need as much as 2.0 g/kg/day of protein [7].
Epidemiological studies have suggested that low protein intake is correlated with the onset and progression of sarcopenia. Recently, it has been demonstrated that a low intake of calories, protein, and leucine is associated with reduced muscle mass in hip-fractured elderly [40]. Given the relevance of sarcopenia as a risk factor for adverse outcomes in frail older persons [41,42], these findings emphasize the importance of a comprehensive dietary assessment for the detection of nutritional deficits that predispose to or aggravate muscle atrophy.
Tieland and colleagues [43,44] reported the findings of two trials on the effect of protein supplementation on muscle mass and physical performance in frail older participants. They determined that a 24-week supplementation of a beverage containing 15 g milk protein concentrate administered twice-daily improved muscle strength and physical performance, but did not increase muscle mass. A similar supplementation regimen increased muscle mass when combined with resistance exercise training. Interestingly, in both trials, after including the dietary supplements, the daily protein intake in the intervention group increased up to 1.4 g/kg/day. However, it is important to highlight that it is likely that the older persons who had greater protein intakes and displayed greater strength and muscle size also had higher intakes of other nutrients, which may also explain their improved status. Nevertheless, protein metabolism is dynamic in nature and can become more efficient under specific conditions such as exercise training and a well-balanced diet.
4. Protein Quality: Which Is the Best Protein Source?
Besides quantity, the quality of consumed protein has a critical role in the context of muscle health [8,45,46]. Amino acids have been traditionally categorized as indispensable (essential), conditionally indispensable, or dispensable (nonessential), based on the capacity of the body to synthesize the amino acid from other carbon sources. Dietary protein sources are often assorted in their amino acid content; however, differences in EAA profile, digestibility, and bioavailability determine the anabolic properties (or quality) of specific protein sources [47]. Ingesting EAAs, which cannot be synthesized de novo and have primary role in the regulation of muscle protein synthesis, can potentially mitgate the loss of muscle protein during the aging process. At the same time, the ingestion of EAAs provides a more efficient nutritional approach (i.e., greater stimulation of protein synthesis relative to the amount of amino acids ingested) to enhance muscle protein synthesis compared with the ingestion of intact protein.
4.1. Fast versus Slow Proteins
The absorption kinetics and the amino acid composition of dietary proteins are important factors that must be considered. The rapidity of absorption of dietary amino acids by the gut influences the postprandial protein synthesis rate, breakdown, and, finally, protein deposition [48]. This observation has contributed to the development of the fast versus slow protein model [48], which may have significant implications for the prevention and treatment of sarcopenia. In young individuals, slowly digested proteins (e.g., casein) may produce greater protein retention than those that are more quickly digested (e.g., whey). An opposite pattern has been documented in older individuals [49]. Accordingly, some authors have demonstrated that the intake of whey protein stimulates postprandial muscle protein deposition in older men more efficiently than casein or casein hydrolysate [50]. Consequently, the concept of “fast” versus “slow” protein may need to be considered when developing specific nutritional recommendations as well as the prescription of specific supplements.
4.2. Animal- versus Plant-Derived Proteins
No definitive evidence is available regarding the possibly differing effects of animal-derived and plant-based proteins on muscle health in old age. Few studies have compared the capacity of animal- versus plant-derived proteins to influence muscle mass or function [51]. Plant-based proteins generally contain smaller quantities of EAAs and are less digestible than animal-derived proteins. This is predominantly due to lower amounts of lysine, methionine, and/or leucine in plant-based proteins. Hence, it is expected that the ingestion of greater amounts of plant-based proteins per meal may be necessary to achieve the same anabolic response evoked by smaller quantities of animal-derived proteins [21]. However, recent findings in elderly men indicate that the consumption of large amounts of plant-based proteins, as a strategy to ameliorate muscle protein synthesis, may not be as effective as expected [22]. Indeed, the authors showed that amino acids derived from soy protein were directed more toward oxidation than used for de novo muscle protein synthesis compared with whey protein-derived amino acids.
Meat is an excellent source of high quality proteins, which are essential for optimal muscle and bone development. Meat contains a large quantity of EAAs and it is important to highlight that the intake of EAAs from meat, for the same weight, is higher than all other foods. The correct intake of biologically active compounds contained in meat, such as creatine, carnitine, and other nutrients such as iron and cobalamin, have a significant impact upon human protein metabolism and so likely have beneficial effects on the prevention of sarcopenia [52]. In this respect, within a varied and balanced diet aimed at preventing sarcopenia, consuming meat 4–5 times a week (i.e., white meat two times per week, lean red meat less than two times per week, and processed meat less than two time per week) should be recommended.
4.3. Physical Properties of Protein Sources
The formulation of protein sources has an important effect on protein digestion, absorption, as well as whole-body and muscle anabolism. The ingestion of amino acids in liquid form produces a greater postprandial amino acid concentration compared with the same amino acids consumed in solid form [51]. However, some studies demonstrated that, even though minced beef was more rapidly digested and absorbed than whole steak, the difference did not translate into greater postprandial muscle protein synthesis rates [53]. Further studies are necessary to assess the significance of not only the “biological” quality but also the “physical” quality of protein sources and the specific milieu in which the protein is eaten.
5. Protein Ingestion Timing: When Is It Best to Consume Protein?
The timing of protein ingestion and the synergistic effect of protein intake with physical activity are relevant factors to consider in enhancing muscle health.
5.1. Protein Feeding Patterns
The most significant issue regarding the timing of protein intake is the pattern of ingestion. Arnal and colleagues [54] documented that, in older persons, a two-week protein pulse-feeding pattern in which 80% of daily protein intake was delivered in one meal was more effective in enhancing whole-body protein retention than the same amount of protein distributed uniformly across four meals. However, ingesting large quantities of proteins in a single meal may be difficult to maintain over the long term, particularly in old age. Moreover, most researchers agree proteins should be introduced uniformly throughout the day in order to guarantee a more sustained 24-h anabolic response [35,39]. Hence, older persons should be encouraged to eat between 1.0 and 1.2 g/kg of body weight per day of protein through the consumption of an adequate serving (e.g., 25–35 g) of high-quality protein sources at every meal [35,39]. The resulting spread-feeding pattern, in which a similar quantity of proteins is consumed at every meal, would ensure a 24-h stimulus of protein synthesis [54].
The protein meal threshold theory has been addressed by recent findings on the differential effects of 10, 20, and 35 g of whey protein during a primed continuous intravenous infusion of phenylalanine and tyrosine (l-[ring-2H5]phenylalanine and l-[ring-2H2]tyrosine) in healthy older men [55]. The authors demonstrated that amino acid absorption and the consequent stimulation of muscle protein synthesis were suboptimal after the intake of 10 g of protein, slightly improved after a 20-g protein meal and were greatest and statistically significant only after the ingestion of 35 g [55]. Other recent studies have shown the possible importance of meal distribution patterns for optimal, repeated stimulation of muscle protein synthesis throughout the day [56,57]. On the other hand, other investigations examining the eating patterns of older adults support the idea that daily protein ingestion should be focused on individual meals or specific eating opportunities, with breakfast offering the best chance to more equally allocate protein throughout the day [57]. Considering the uncertainty of the current evidence, studies designed to specifically assess the effects of different patterns of protein ingestion are needed to develop nutritional interventions for the management of sarcopenia.
5.2. Protein Intake and Physical Exercise
A harmonized prescription of dietary protein and physical exercise may be important for middle-aged and older adults suffering from catabolic stressors such as illness, inflammation, or injury, or experiencing prolonged physical inactivity. The combination of physical exercise and protein intake has a positive and synergistic effect on skeletal muscle protein synthesis [58]. Some data suggest that resistance and aerobic exercise offers the greatest benefit to aged muscle when combined with a dietary protein intake that exceeds the current RDA [59]. Still, one of the major issues regarding protein intake is identifying when to ingest protein relative to physical exercise. The consumption of branched-chain amino acids combined with exercise training produces an anabolic environment [60]. Protein intake following physical exercise has positive effects on the balance between protein synthesis and breakdown, stimulating muscle protein anabolism [14].
Optimizing the timing of protein intake and exercise training is a “biologically plausible” approach to increase the potential for muscle protein anabolism. Some studies suggest that resistance exercise training momentarily constrains protein synthesis via increased AMP-activated protein kinase (AMPK) activation and decreased phosphorylation of eukaryotic translation initiation factor 4E-binding protein 1 (4E-BP1) and other specific key regulators of translation initiation [54]. However, 60 min after exercising, maximal muscle protein synthesis is restored and theoretically amplified via the activation of protein kinase B (Akt), mTOR, ribosomal protein S6 kinase beta-1 (S6K1), and eukaryotic elongation factor 2 (eEF2) [61,62]. Consequently, the highest level of muscle protein synthesis is observed around 60 min after the end of exercise training. Accordingly, improving the availability of amino acids throughout this period could offer the largest anabolic advantage [14]. However, even though protein synthesis in the first hour after exercise is maximized, the sensitivity of the muscle to protein feeding is enhanced for up to 24 h after exercise [63]. In this respect, it should be highlighted that repeated protein feeding in the post exercise period is important to optimally facilitate the muscle adaptive response.
For older persons, eating a moderate amount of protein (i.e., 20–30 g/kg/day) at breakfast, lunch, and dinner could offer the required amino acid precursors and flexibility required to permit at least some protein–exercise anabolic synergy, regardless of when the exercise session or physical activities are performed.
6. Protein Supplementation: New Evidence
Robust evidence indicates that anorexia of aging is a major reason for overall and selective malnutrition [64]. Anorexia is associated with a higher risk of quantitative malnutrition (for example, protein-energy malnutrition) due to inadequate overall nutritional intake. However, in the early stages, anorexia increases the risk of qualitative malnutrition, due to the suboptimal intake of specific nutrients, like proteins and vitamins [65]. Studies have demonstrated that selective malnutrition is also related to the development of sarcopenia and several other negative health outcomes, including morbidity and mortality [10,66].
Nutritional supplementation does not directly treat anorexia of aging, only its consequences, such as weight loss and protein-energy malnutrition. A small number of studies have demonstrated positive effects from energy supplementation in malnourished older adults. Nevertheless, the heterogeneity of the supplementation protocols implemented impedes their applicability to standard patient care. As it stands, the only conclusive evidence is presently limited to protein supplementation. Recently, it has been demonstrated that β-hydroxy β-methylbutyrate (HMB)—an amino acid metabolite of leucine—is able to stimulate protein synthesis and improve muscle strength and body composition in older adults [67].
6.1. Nutritional Supplementation with Leucine
Given the role of leucine as the principal dietary regulator of muscle protein anabolism, supplementation with protein sources enriched with this EAA should provide substantial benefits in the preservation of muscle mass and function [35,68]. This view is in line with recent findings that both total protein ingestion and leucine intake are positively associated with muscle mass in hip-fractured elderly patients [40]. However, the effects of leucine supplementation in clinical studies have not been consistent. Differences in the results might be attributable to dissimilar study protocols, with some programs administering a large bolus of leucine over a short period of time and others serving a continuous infusion of leucine. Generally, the findings suggest that leucine supplementation has potential positive effects on muscle metabolism in older people and that there is a minimal dosage that produces these effects [40]. For example, one study assessed the effects of a single dose of branched-chain amino acids (6.7 g) with different amounts of leucine (2.8 versus 1.7 g) on postprandial protein synthesis in older persons, demonstrating that those supplemented with a higher dosage had a significant increase in protein synthesis compared with participants supplemented with a smaller dose of leucine [69]. More recently, the PROVIDE study demonstrated that a oral nutritional supplement containing vitamin D- and leucine-enriched whey protein improved in muscle mass and lower extremity function in sarcopenic older adults [70]. The active group achieved a higher total protein intake (1.5 g/kg/day) during the study period, which is in line with the recent PROT-AGE recommendations for older populations [7]. Finally, leucine supplementation has been shown to enhance the muscle anabolic response when suboptimal amounts of protein are consumed [71,72,73].
6.2. Nutritional Supplementation with HMB
HMB is an active leucine metabolite which activates the mTOR signaling pathway in muscle. Following its absorption, dietary leucine is converted into α-ketoisocaproate (KIC), which is further metabolized into either isovaleryl-CoA or HMB. Under normal conditions, the majority of KIC is converted into isovaleryl-CoA, while only approximately 5% of leucine is metabolized to HMB. This implies that, in order to reach pharmacological levels of HMB, this compound needs to be administered directly, rather than via increasing leucine dosage. It has recently been suggested that HMB may be used to protect or restore muscle mass in older persons with reduced lean body mass [74].
HMB exerts its effects through protective, anticatabolic mechanisms and directly influences protein synthesis. HMB has also been shown to stabilize the muscle cell membrane, to modulate protein degradation and to up-regulate protein synthesis [68]. The daily administration of a nutritional mixture including HMB (2 g), arginine (5 g), and lysine (1.5 g) for 12 weeks was shown to improve physical performance, muscle strength, fat-free mass and protein synthesis in sedentary older women [74]. More recently, Deutz and colleagues [13]—in a multicenter, randomized, placebo-controlled, double-blind trial—demonstrated that the early administration (within 72 h of hospitalization) of a nutrient-dense oral nutritional supplement containing high concentrations of protein and HMB was associated with decreased post-discharge mortality and improved nutritional status in malnourished older adults [13].
Similar to leucine, HMB holds promise when suboptimal amounts of protein are consumed. In short, HMB has emerged as a promising candidate for nutritional interventions against sarcopenia, but more extensive studies are needed to establish the optimal dosage and possible side effects resulting from chronic supplementation.
7. Conclusions
The recognition of sarcopenia as a major risk factor for adverse outcomes in frail older populations indicates that skeletal muscle may represent a critical target for interventions. The association between low energy and protein intake and reduced muscle mass in older adults, revealed by several studies [40,64,75], highlights the importance of a comprehensive dietary assessment for the early detection of nutritional deficits, which may promote muscle loss. The suboptimal consumption of protein is often the case for older individuals. When nutritional supplements are suggested as a strategy to improve muscle health, providing protein (containing a variety of amino acids) may be preferred over the ingestion of a single amino acid (such as leucine, let alone its metabolite HMB). Given the heterogeneity of the older population, it is likely that, as opposed to standardized nutritional regimens, the greatest health benefits may be achieved through the provision of personalized dietary recommendations [76]. Finally, in older persons engaged in physical activity, nutritional interventions should be structured to take advantage of the anabolic window “opened” by physical exercise.
Acknowledgments
The study was partly supported by grants from the Innovative Medicines Initiative—Joint Undertaking (IMI-JU #115621), intramural research grants from the Catholic University of the Sacred Heart (D3.2 2013 and D3.2 2015), and the “Centro Studi Achille e Linda Lorenzon”.
Author Contributions
All of the authors participated in the conceiving, design and writing of the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
Emanuele Marzetti, Francesco Landi, Matteo Tosato, and Riccardo Calvani are partners of the SPRINTT Consortium, which is partly funded by the European Federation of Pharmaceutical Industries and Associations (EFPIA). Anna Maria Martone, Alex Sisto, Emanuela D’Angelo, Elena Ortolani, and Giulia Savera declare no conflict of interest.
References
- 1.Wolfe R.R., Miller S.L. The recommended dietary allowance of protein: A misunderstood concept. JAMA. 2008;299:2891–2893. doi: 10.1001/jama.299.24.2891. [DOI] [PubMed] [Google Scholar]
- 2.Milne A.C., Potter J., Vivanti A., Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst. Rev. 2009 doi: 10.1002/14651858.CD003288.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Botella-Carretero J.I., Iglesias B., Balsa J.A., Arrieta F., Zamarrón I., Vázquez C. Perioperative oral nutritional supplements in normally or mildly undernourished geriatric patients submitted to surgery for hip fracture: A randomized clinical trial. Clin. Nutr. 2010;29:574–579. doi: 10.1016/j.clnu.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Schürch M.A., Rizzoli R., Slosman D., Vadas L., Vergnaud P., Bonjour J.P. Protein supplements increase serum insulin-like growth factor-I levels and attenuate proximal femur bone loss in patients with recent hip fracture. A randomized, double-blind, placebo-controlled trial. Ann. Intern. Med. 1998;128:801–819. doi: 10.7326/0003-4819-128-10-199805150-00002. [DOI] [PubMed] [Google Scholar]
- 5.Tengstrand B., Cederholm T., Söderqvist A., Tidermark J. Effects of protein-rich supplementation and nandrolone on bone tissue after a hip fracture. Clin. Nutr. 2007;26:460–465. doi: 10.1016/j.clnu.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Avenell A., Handoll H.H.G. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst. Rev. 2005 doi: 10.1002/14651858.CD001880.pub5. [DOI] [PubMed] [Google Scholar]
- 7.Bauer J., Biolo G., Cederholm T., Cesari M., Cruz-Jentoft A.J., Morley J.E., Phillips S., Sieber C., Stehle P., Teta D., et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the PROT-AGE Study Group. J. Am. Med. Dir. Assoc. 2013;14:542–559. doi: 10.1016/j.jamda.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Calvani R., Miccheli A., Landi F., Bossola M., Cesari M., Leeuwenburgh C., Sieber C.C., Bernabei R., Marzetti E. Current nutritional recommendations and novel dietary strategies to manage sarcopenia. J. Frailty Aging. 2013;2:38–53. [PMC free article] [PubMed] [Google Scholar]
- 9.Landi F., Liperoti R., Russo A., Giovannini S., Tosato M., Barillaro C., Capoluongo E., Bernabei R., Onder G. Association of anorexia with sarcopenia in a community-dwelling elderly population: Results from the ilSIRENTE study. Eur. J. Nutr. 2013;52:1261–1268. doi: 10.1007/s00394-012-0437-y. [DOI] [PubMed] [Google Scholar]
- 10.Martone A.M., Onder G., Vetrano D.L., Ortolani E., Tosato M., Marzetti E., Landi F. Anorexia of aging: A modifiable risk factor for frailty. Nutrients. 2013;5:4126–4133. doi: 10.3390/nu5104126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Houston D.K., Nicklas B.J., Ding J., Harris T.B., Tylavsky F.A., Newman A.B., Lee J.S., Sahyoun N.R., Visser M., Kritchevsky S.B. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: The Health, Aging, and Body Composition (Health ABC) Study. Am. J. Clin. Nutr. 2008;87:150–155. doi: 10.1093/ajcn/87.1.150. [DOI] [PubMed] [Google Scholar]
- 12.Bos C., Benamouzig R., Bruhat A., Roux C., Valensi P., Ferrière F., Tomé D. Nutritional status after short-term dietary supplementation in hospitalized malnourished geriatric patients. Clin. Nutr. 2001;20:225–233. doi: 10.1054/clnu.2000.0387. [DOI] [PubMed] [Google Scholar]
- 13.Deutz N.E., Matheson E.M., Matarese L.E., Luo M., Baggs G.E., Nelson J.L., Hegazi R.A., Tappenden K.A., Ziegler T.R. Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: A randomized clinical trial. Clin. Nutr. 2016;35:18–26. doi: 10.1016/j.clnu.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 14.Paddon-Jones D., Short K.R., Campbell W.W., Volpi E., Wolfe R.R. Role of dietary protein in the sarcopenia of aging. Am. J. Clin. Nutr. 2008;87:1562S–1566S. doi: 10.1093/ajcn/87.5.1562S. [DOI] [PubMed] [Google Scholar]
- 15.Wolfe R.R. Regulation of muscle protein by amino acids. J. Nutr. 2002;132:3219S–3224S. doi: 10.1093/jn/131.10.3219S. [DOI] [PubMed] [Google Scholar]
- 16.Phillips S.M., Glover E.I., Rennie M.J. Alterations of protein turnover underlying disuse atrophy in human skeletal muscle. J. Appl. Physiol. 2009;107:645–654. doi: 10.1152/japplphysiol.00452.2009. [DOI] [PubMed] [Google Scholar]
- 17.Wall B.T., Gorissen S.H., Pennings B., Koopman R., Groen B.B.L., Verdijk L.B., van Loon L.J.C. Aging Is Accompanied by a Blunted Muscle Protein Synthetic Response to Protein Ingestion. PLoS ONE. 2015;10:295. doi: 10.1371/journal.pone.0140903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fry C.S., Drummond M.J., Glynn E.L., Dickinson J.M., Gundermann D.M., Timmerman K.L., Walker D.K., Volpi E., Rasmussen B.B. Skeletal muscle autophagy and protein breakdown following resistance exercise are similar in younger and older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013;68:599–607. doi: 10.1093/gerona/gls209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang J.E., Phillips S.M. Maximizing muscle protein anabolism: The role of protein quality. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:66–71. doi: 10.1097/MCO.0b013e32831cef75. [DOI] [PubMed] [Google Scholar]
- 20.Anthony J.C., Anthony T.G., Kimball S.R., Jefferson L.S. Signaling pathways involved in translational control of protein synthesis in skeletal muscle by leucine. J. Nutr. 2001;131:856S–860S. doi: 10.1093/jn/131.3.856S. [DOI] [PubMed] [Google Scholar]
- 21.Van Vliet S., Burd N.A., van Loon L.J.C. The skeletal muscle anabolic response to plant- versus animal-based protein consumption. J. Nutr. 2015;145:1981–1991. doi: 10.3945/jn.114.204305. [DOI] [PubMed] [Google Scholar]
- 22.Yang Y., Churchward-Venne T.A., Burd N.A., Breen L., Tarnopolsky M.A., Phillips S.M. Myofibrillar protein synthesis following ingestion of soy protein isolate at rest and after resistance exercise in elderly men. Nutr. Metab. (Lond.) 2012;9:57. doi: 10.1186/1743-7075-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phillips S.M. Nutrient-rich meat proteins in offsetting age-related muscle loss. Meat Sci. 2012;92:174–178. doi: 10.1016/j.meatsci.2012.04.027. [DOI] [PubMed] [Google Scholar]
- 24.Walrand S., Gryson C., Salles J., Giraudet C., Migné C., Bonhomme C., le Ruyet P., Boirie Y. Fast-digestive protein supplement for ten days overcomes muscle anabolic resistance in healthy elderly men. Clin. Nutr. 2016;35:660–668. doi: 10.1016/j.clnu.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 25.Burd N.A., Gorissen S.H., van Loon L.J.C. Anabolic resistance of muscle protein synthesis with aging. Exerc. Sport Sci. Rev. 2013;41:169–173. doi: 10.1097/JES.0b013e318292f3d5. [DOI] [PubMed] [Google Scholar]
- 26.Wall B.T., Snijders T., Senden J.M.G., Ottenbros C.L.P., Gijsen A.P., Verdijk L.B., van Loon L.J.C. Disuse impairs the muscle protein synthetic response to protein ingestion in healthy men. J. Clin. Endocrinol. Metab. 2013;98:4872–4881. doi: 10.1210/jc.2013-2098. [DOI] [PubMed] [Google Scholar]
- 27.Glover E.I., Phillips S.M., Oates B.R., Tang J.E., Tarnopolsky M.A., Selby A., Smith K., Rennie M.J. Immobilization induces anabolic resistance in human myofibrillar protein synthesis with low and high dose amino acid infusion. J. Physiol. 2008;586:6049–6061. doi: 10.1113/jphysiol.2008.160333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breen L., Stokes K.A., Churchward-Venne T.A., Moore D.R., Baker S.K., Smith K., Atherton P.J., Phillips S.M. Two weeks of reduced activity decreases leg lean mass and induces “anabolic resistance” of myofibrillar protein synthesis in healthy elderly. J. Clin. Endocrinol. Metab. 2013;98:2604–2612. doi: 10.1210/jc.2013-1502. [DOI] [PubMed] [Google Scholar]
- 29.Parr E.B., Camera D.M., Areta J.L., Burke L.M., Phillips S.M., Hawley J.A., Coffey V.G. Alcohol ingestion impairs maximal post-exercise rates of myofibrillar protein synthesis following a single bout of concurrent training. PLoS ONE. 2014;9:295. doi: 10.1371/journal.pone.0088384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guillet C., Masgrau A., Walrand S., Boirie Y. Impaired protein metabolism: Interlinks between obesity, insulin resistance and inflammation. Obes. Rev. 2012;13(Suppl. S2):51–57. doi: 10.1111/j.1467-789X.2012.01037.x. [DOI] [PubMed] [Google Scholar]
- 31.Landi F., Onder G., Bernabei R. Sarcopenia and diabetes: Two sides of the same coin. J. Am. Med. Dir. Assoc. 2013;14:540–541. doi: 10.1016/j.jamda.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 32.Wolfe R.R. Effects of insulin on muscle tissue. Curr. Opin. Clin. Nutr. Metab. Care. 2000;3:67–71. doi: 10.1097/00075197-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Bassil M.S., Gougeon R. Muscle protein anabolism in type 2 diabetes. Curr. Opin. Clin. Nutr. Metab. Care. 2013;16:83–88. doi: 10.1097/MCO.0b013e32835a88ee. [DOI] [PubMed] [Google Scholar]
- 34.Cuthbertson D., Smith K., Babraj J., Leese G., Waddell T., Atherton P., Wackerhage H., Taylor P.M., Rennie M.J. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J. 2005;19:422–424. doi: 10.1096/fj.04-2640fje. [DOI] [PubMed] [Google Scholar]
- 35.Paddon-Jones D., Rasmussen B.B. Dietary protein recommendations and the prevention of sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:86–90. doi: 10.1097/MCO.0b013e32831cef8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paddon-Jones D. Interplay of stress and physical inactivity on muscle loss: Nutritional countermeasures. J. Nutr. 2006;136:2123–2126. doi: 10.1093/jn/136.8.2123. [DOI] [PubMed] [Google Scholar]
- 37.Fielding R.A., Vellas B., Evans W.J., Bhasin S., Morley J.E., Newman A.B., van Kan G.A., Andrieu S., Bauer J., Breuille D., et al. Sarcopenia: An undiagnosed condition in older adults. Current consensus definition: Prevalence, etiology, and consequences. International working group on sarcopenia. J. Am. Med. Dir. Assoc. 2011;12:249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Volpi E., Campbell W.W., Dwyer J.T., Johnson M.A., Jensen G.L., Morley J.E., Wolfe R.R. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013;68:677–681. doi: 10.1093/gerona/gls229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morley J.E., Argiles J.M., Evans W.J., Bhasin S., Cella D., Deutz N.E.P., Doehner W., Fearon K.C.H., Ferrucci L., Hellerstein M.K., et al. Nutritional recommendations for the management of sarcopenia. J. Am. Med. Dir. Assoc. 2010;11:391–396. doi: 10.1016/j.jamda.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Calvani R., Martone A.M., Marzetti E., Onder G., Savera G., Lorenzi M., Serafini E., Bernabei R., Landi F. Pre-hospital dietary intake correlates with muscle mass at the time of fracture in older hip-fractured patients. Front. Aging Neurosci. 2014;6:269. doi: 10.3389/fnagi.2014.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Landi F., Liperoti R., Russo A., Giovannini S., Tosato M., Capoluongo E., Bernabei R., Onder G. Sarcopenia as a risk factor for falls in elderly individuals: Results from the ilSIRENTE study. Clin. Nutr. 2012;31:652–658. doi: 10.1016/j.clnu.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 42.Landi F., Cruz-Jentoft A.J., Liperoti R., Russo A., Giovannini S., Tosato M., Capoluongo E., Bernabei R., Onder G. Sarcopenia and mortality risk in frail older persons aged 80 years and older: Results from ilSIRENTE study. Age Ageing. 2013;42:203–209. doi: 10.1093/ageing/afs194. [DOI] [PubMed] [Google Scholar]
- 43.Tieland M., van de Rest O., Dirks M.L., van der Zwaluw N., Mensink M., van Loon L.J.C., de Groot L.C.P.G.M. Protein supplementation improves physical performance in frail elderly people: A randomized, double-blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2012;13:720–726. doi: 10.1016/j.jamda.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 44.Tieland M., Dirks M.L., van der Zwaluw N., Verdijk L.B., van de Rest O., de Groot L.C.P.G.M., van Loon L.J.C. Protein supplementation increases muscle mass gain during prolonged resistance-type exercise training in frail elderly people: A randomized, double-blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2012;13:713–719. doi: 10.1016/j.jamda.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 45.Landi F., Marzetti E., Bernabei R. Perspective: Protein: What kind, how much, when? J. Am. Med. Dir. Assoc. 2013;14:66–67. doi: 10.1016/j.jamda.2012.09.020. [DOI] [PubMed] [Google Scholar]
- 46.Reeds P., Schaafsma G., Tomé D., Young V. Criteria and significance of dietary protein sources in humans. Summary of the workshop with recommendations. J. Nutr. 2000;130:1874S–1876S. doi: 10.1093/jn/130.7.1874S. [DOI] [PubMed] [Google Scholar]
- 47.Elango R., Ball R.O., Pencharz P.B. Amino acid requirements in humans: With a special emphasis on the metabolic availability of amino acids. Amino Acids. 2009;37:19–27. doi: 10.1007/s00726-009-0234-y. [DOI] [PubMed] [Google Scholar]
- 48.Boirie Y., Dangin M., Gachon P., Vasson M.P., Maubois J.L., Beaufrère B. Slow and fast dietary proteins differently modulate postprandial protein accretion. Proc. Natl. Acad. Sci. USA. 1997;94:14930–14935. doi: 10.1073/pnas.94.26.14930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dangin M., Guillet C., Garcia-Rodenas C., Gachon P., Bouteloup-Demange C., Reiffers-Magnani K., Fauquant J., Ballèvre O., Beaufrère B. The rate of protein digestion affects protein gain differently during aging in humans. J. Physiol. 2003;549:635–644. doi: 10.1113/jphysiol.2002.036897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pennings B., Boirie Y., Senden J.M.G., Gijsen A.P., Kuipers H., van Loon L.J.C. Whey protein stimulates postprandial muscle protein accretion more effectively than do casein and casein hydrolysate in older men. Am. J. Clin. Nutr. 2011;93:997–1005. doi: 10.3945/ajcn.110.008102. [DOI] [PubMed] [Google Scholar]
- 51.Paddon-Jones D., Campbell W.W., Jacques P.F., Kritchevsky S.B., Moore L.L., Rodriguez N.R., van Loon L.J. Protein and healthy aging. Am. J. Clin. Nutr. 2015;101:1339S–1345S. doi: 10.3945/ajcn.114.084061. [DOI] [PubMed] [Google Scholar]
- 52.Rondanelli M., Perna S., Faliva M.A., Peroni G., Infantino V., Pozzi R. Novel insights on intake of meat and prevention of sarcopenia: All reasons for an adequate consumption. Nutr. Hosp. 2015;32:2136–2143. doi: 10.3305/nh.2015.32.5.9638. [DOI] [PubMed] [Google Scholar]
- 53.Pennings B., Groen B.B.L., van Dijk J.W., de Lange A., Kiskini A., Kuklinski M., Senden J.M.G., van Loon L.J.C. Minced beef is more rapidly digested and absorbed than beef steak, resulting in greater postprandial protein retention in older men. Am. J. Clin. Nutr. 2013;98:121–128. doi: 10.3945/ajcn.112.051201. [DOI] [PubMed] [Google Scholar]
- 54.Arnal M.A., Mosoni L., Boirie Y., Houlier M.L., Morin L., Verdier E., Ritz P., Antoine J.M., Prugnaud J., Beaufrère B., Mirand P.P. Protein pulse feeding improves protein retention in elderly women. Am. J. Clin. Nutr. 1999;69:1202–1208. doi: 10.1093/ajcn/69.6.1202. [DOI] [PubMed] [Google Scholar]
- 55.Pennings B., Groen B., de Lange A., Gijsen A.P., Zorenc A.H., Senden J.M.G., van Loon L.J.C. Amino acid absorption and subsequent muscle protein accretion following graded intakes of whey protein in elderly men. Am. J. Physiol. Endocrinol. Metab. 2012;302:E992–E999. doi: 10.1152/ajpendo.00517.2011. [DOI] [PubMed] [Google Scholar]
- 56.Areta J.L., Burke L.M., Ross M.L., Camera D.M., West D.W.D., Broad E.M., Jeacocke N.A., Moore D.R., Stellingwerff T., Phillips S.M., et al. Timing and distribution of protein ingestion during prolonged recovery from resistance exercise alters myofibrillar protein synthesis. J. Physiol. 2013;591:2319–2331. doi: 10.1113/jphysiol.2012.244897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mamerow M.M., Mettler J.A., English K.L., Casperson S.L., Arentson-Lantz E., Sheffield-Moore M., Layman D.K., Paddon-Jones D. Dietary protein distribution positively influences 24-h muscle protein synthesis in healthy adults. J. Nutr. 2014;144:876–880. doi: 10.3945/jn.113.185280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Witard O., Wardle S., Macnaughton L., Hodgson A., Tipton K. Protein considerations for optimising skeletal muscle mass in healthy young and older adults. Nutrients. 2016;8:181. doi: 10.3390/nu8040181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Morris M.S., Jacques P.F. Total protein, animal protein and physical activity in relation to muscle mass in middle-aged and older Americans. Br. J. Nutr. 2013;109:1294–1303. doi: 10.1017/S0007114512003133. [DOI] [PubMed] [Google Scholar]
- 60.Sharp C.P.M., Pearson D.R. Amino acid supplements and recovery from high-intensity resistance training. J. Strength Cond. Res. 2010;24:1125–1130. doi: 10.1519/JSC.0b013e3181c7c655. [DOI] [PubMed] [Google Scholar]
- 61.MacLaren D. Nutrition and Sport. 1st ed. Churchill Livingstone; London, UK: 2007. [Google Scholar]
- 62.Dickinson J.M., Volpi E., Rasmussen B.B. Exercise and nutrition to target protein synthesis impairments in aging skeletal muscle. Exerc. Sport Sci. Rev. 2013;41:216–223. doi: 10.1097/JES.0b013e3182a4e699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Burd N.A., West D.W.D., Moore D.R., Atherton P.J., Staples A.W., Prior T., Tang J.E., Rennie M.J., Baker S.K., Phillips S.M. Enhanced amino acid sensitivity of myofibrillar protein synthesis persists for up to 24 h after resistance exercise in young men. J. Nutr. 2011;141:568–573. doi: 10.3945/jn.110.135038. [DOI] [PubMed] [Google Scholar]
- 64.Landi F., Calvani R., Tosato M., Martone A., Ortolani E., Savera G., Sisto A., Marzetti E. Anorexia of aging: Risk factors, consequences, and potential treatments. Nutrients. 2016;8:69. doi: 10.3390/nu8020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Landi F., Laviano A., Cruz-Jentoft A.J. The anorexia of aging: Is it a geriatric syndrome? J. Am. Med. Dir. Assoc. 2010;11:153–156. doi: 10.1016/j.jamda.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 66.Landi F., Russo A., Liperoti R., Tosato M., Barillaro C., Pahor M., Bernabei R., Onder G. Anorexia, physical function, and incident disability among the frail elderly population: Results from the ilSIRENTE study. J. Am. Med. Dir. Assoc. 2010;11:268–274. doi: 10.1016/j.jamda.2009.12.088. [DOI] [PubMed] [Google Scholar]
- 67.Cruz-Jentoft A.J., Landi F., Schneider S.M., Zúñiga C., Arai H., Boirie Y., Chen L.K., Fielding R.A., Martin F.C., Michel J.P., et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS) Age Ageing. 2014;43:748–759. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barillaro C., Liperoti R., Martone A.M., Onder G., Landi F. The new metabolic treatments for sarcopenia. Aging Clin. Exp. Res. 2013;25:119–127. doi: 10.1007/s40520-013-0030-0. [DOI] [PubMed] [Google Scholar]
- 69.Katsanos C.S. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. AJP Endocrinol. Metab. 2006;291:E381–E387. doi: 10.1152/ajpendo.00488.2005. [DOI] [PubMed] [Google Scholar]
- 70.Bauer J.M., Verlaan S., Bautmans I., Brandt K., Donini L.M., Maggio M., McMurdo M.E.T., Mets T., Seal C., Wijers S.L., et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: A randomized, double-blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2015;16:740–747. doi: 10.1016/j.jamda.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 71.Churchward-Venne T.A., Burd N.A., Mitchell C.J., West D.W.D., Philp A., Marcotte G.R., Baker S.K., Baar K., Phillips S.M. Supplementation of a suboptimal protein dose with leucine or essential amino acids: Effects on myofibrillar protein synthesis at rest and following resistance exercise in men. J. Physiol. 2012;590:2751–2765. doi: 10.1113/jphysiol.2012.228833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Casperson S.L., Sheffield-Moore M., Hewlings S.J., Paddon-Jones D. Leucine supplementation chronically improves muscle protein synthesis in older adults consuming the RDA for protein. Clin. Nutr. 2012;31:512–519. doi: 10.1016/j.clnu.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rieu I., Balage M., Sornet C., Giraudet C., Pujos E., Grizard J., Mosoni L., Dardevet D. Leucine supplementation improves muscle protein synthesis in elderly men independently of hyperaminoacidaemia. J. Physiol. 2006;575:305–315. doi: 10.1113/jphysiol.2006.110742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Flakoll P., Sharp R., Baier S., Levenhagen D., Carr C., Nissen S. Effect of beta-hydroxy-beta-methylbutyrate, arginine, and lysine supplementation on strength, functionality, body composition, and protein metabolism in elderly women. Nutrition. 2004;20:445–451. doi: 10.1016/j.nut.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 75.Landi F., Calvani R., Cesari M., Tosato M., Martone A.M., Bernabei R., Onder G., Marzetti E. Sarcopenia as the biological substrate of physical frailty. Clin. Geriatr. Med. 2015;31:367–374. doi: 10.1016/j.cger.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 76.Marzetti E., Calvani R., Landi F., Hoogendijk E.O., Fougère B., Vellas B., Pahor M., Bernabei R., Cesari M. Innovative medicines initiative: The SPRINTT project. J. Frailty Aging. 2015;4:207–208. [PMC free article] [PubMed] [Google Scholar]