ABSTRACT
Purpose
To determine if the use of pigments or adding polyvinyl pyrrolidone during the fabrication of 1-DAY ACUVUE DEFINE (AD) brand contact lenses impacts open-eye corneal swelling compared with no lens wear (NLW).
Methods
A partial double-masked, randomized, bilateral crossover study was conducted in 24 Asian subjects using AD, 1-DAY ACUVUE DEFINE with Lacreon (ADL), NLW, and a control lens with no tint (1-DAY ACUVUE MOIST [AM]). Central corneal thickness was measured before insertion and immediately after removal after 8 ± 1 h of open-eye wear using an optical pachymeter in one eye. Corneal thickness along a 10-mm cord was measured in the contralateral eye using the Visante optical coherence tomographer (OCT). Corneal swelling was tested for noninferiority using a 5% margin. The endothelial bleb response was measured at baseline and 20 min after lens insertion using specular microscopy. Subjective grading of corneal staining and limbal/bulbar hyperemia were also monitored.
Results
After 8 ± 1 h of open-eye wear, central corneal swelling across the study lenses with either optical pachymeter or OCT methods was negligible. Peripheral corneal swelling least-square mean differences with OCT were −0.03% (95% confidence interval [95% CI], −0.65 to 0.58%) and −0.26% (95% CI, −0.87 to 0.36%) between AD and ADL and the control lens (AM), respectively, and 1.67% (95% CI, 1.06 to 2.29%) and 1.45% (95% CI, 0.84 to 2.06%) between AD and ADL and NLW, respectively. No endothelial blebs were observed. No clinically significant differences were distinguished between the lenses and NLW for corneal staining and limbal/bulbar hyperemia.
Conclusions
After 8 ± 1 h of open-eye wear, central and peripheral corneal swelling along the horizontal meridian with AD, ADL, AM, and NLW were equivalent. These results confirm that the addition of polyvinyl pyrrolidone or pigments to etafilcon A to obtain a limbal ring design have no impact on corneal swelling or limbal/bulbar hyperemia during normal open-eye wear.
Key Words: corneal swelling, limbal hyperemia, oxygen transmissibility, hydrogel lens, daily disposable, limbal ring lens, optical pachymetry, OCT
The avascular cornea is dependent on atmospheric oxygen to maintain normal corneal physiology. When a soft contact lens is placed on the cornea, the amount of oxygen reaching the corneal surface is reduced. If this reduction in oxygen affects corneal metabolism, then corneal swelling may occur because of water retention from increased osmotic pressure in the corneal stroma caused by accumulation of lactic acid from anaerobic metabolism.1 Corneal swelling is often used as a method of determining if the cornea is receiving sufficient oxygen through the contact lens.2–4 In contact lens–induced hypoxic corneal swelling, lactic acid accumulation and excessive carbon dioxide retention will lower the stromal pH.5 The resultant corneal acidosis may result in swelling of localized areas of the corneal endothelium.6 Under high magnification, the swollen corneal endothelial cells appear as nonreflecting dark areas, simulating localized areas of missing endothelial mosaic. This phenomenon is known as the “corneal endothelial bleb response”7 and peaks about 20 min after lens insertion.8 Previous studies have shown that Asian eyes were more susceptible to this phenomenon than non-Asian eyes.9 This response has also been used to determine whether sufficient oxygen transport through the lens is being met.10,11
The amount of oxygen that passes through a soft lens is termed the oxygen transmissibility (Dk/t; unit = [cm ml O2]/[ml s mmHg]) and is the product of lens oxygen permeability (Dk; unit = [cm2/s] [ml O2/ml mmHg]) divided by its local thickness (t). The degree of corneal swelling measured in response to oxygen deprivation by hydrogel contact lens wear is inversely related to this Dk/t.12 More recent work has also shown that this inverse relation holds true for measurable limbal hyperemia and peripheral lens Dk/t.13
Although highly oxygen-permeable lenses made from various siloxane polymers (termed silicone hydrogels) have shown tremendous growth during the past decade,14 hydrogel materials, in which the Dk increases with increasing water content,15,16 continue to be prescribed in large numbers, accounting for 50% of fits in many countries.14 Daily disposable (DD) contact lenses, in which the lenses are inserted, worn during the day, and then removed and discarded, offer many advantages to the wearer, including convenience and a low rate of adverse events.17 Silicone hydrogel DD lenses have only recently been commercialized,18,19 and thus, the majority of DD lenses are only available in hydrogel materials.14
The first DD hydrogel lens to be commercialized globally was the 1-DAY ACUVUE lens, which was introduced in 199520–22 and made from etafilcon A. In 2005, 1-DAY ACUVUE MOIST (AM) was introduced, which is manufactured from the etafilcon A material with polyvinyl pyrrolidone (PVP) added to enhance lens performance.23–25 Johnson & Johnson Vision Care’s 1-DAY ACUVUE DEFINE brand contact lenses are a further variant of the 1-DAY ACUVUE family of etafilcon A DD hydrogel lenses, with an additional enclosed peripheral limbal ring of pigments beneath the front lens surface in the lens matrix.26,27 This limbal ring is about 5 mm wide, extending as a concentric ring from 7 to about 12 mm in diameter in the lens periphery, with the dimensions of the ring differing slightly depending on the variant.28 The purpose of adding this limbal ring is to enhance the cosmetic appearance of the iris, to define a clear edge for the iris at the limbus, and to make the eye look naturally larger.28 1-DAY ACUVUE DEFINE was first introduced by Johnson & Johnson Vision Care to the Asia-Pacific region about a decade ago.29 Recently, a version with the added PVP wetting agent, 1-DAY ACUVUE DEFINE with Lacreon (ADL), was launched globally.
Whereas the ADL and AM lenses have the built-in wetting agent (PVP), the AD lens does not contain PVP. It has been shown, in vitro, that adding PVP to 1-DAY ACUVUE MOIST does not impact the Dk of etafilcon A (Galas S. Oxygen permeability of the pigmented material used in cosmetic daily disposable CLs. Data on file, Johnson and Johnson Vision Care Inc., 2014), and the addition of the pigments used in the fabrication of 1-DAY ACUVUE DEFINE brand contact lenses does not alter the Dk of the core lens material.30 However, to date, the physiological impact of adding these pigments or PVP has not been determined in vivo by assessing any differences in corneal swelling or endothelial bleb response.
The purpose of this study was to evaluate the open-eye corneal swelling and endothelial bleb response of 1-DAY ACUVUE DEFINE, 1-DAY ACUVUE DEFINE with Lacreon, 1-DAY ACUVUE MOIST, and no lens wear (NLW) for an 8-h period.
MATERIALS AND METHODS
This study was performed in compliance with the ethical principles of the Declaration of Helsinki and Good Clinical Practice. The study received ethics clearance through the Office of Research Ethics at the University of Waterloo. Informed consent was obtained from all subjects before enrollment in the study.
Study Design and Masking
A partially double-masked, randomized, 4 by 4 crossover design was used, using three study contact lenses and habitual spectacles (NLW), all of which were used for an 8-h open-eye period. Each subject, in blocks of four, was randomly assigned to one of the four sequences using William’s 4 × 4 Latin squares. Randomly permuted block randomization was used to avoid bias in the assignment of subjects to treatment sequences and to enhance the validity of statistical comparisons across treatment groups. Subjects and investigators were not aware of the identity of the two pigmented lenses (1-DAY ACUVUE DEFINE lenses with and without Lacreon). Masking subjects and investigators was not possible with NLW and the clear control lens (1-DAY ACUVUE MOIST). Only the study research assistants had access to the study randomization code, and they were responsible for the assignment of the study test article for each subject.
Subjects and Sample Size Justification
Assuming a within-subject/eye variation of 5 and an intraclass correlation of 0.5, the sample size of 24 subjects in a 4 by 4 crossover trial had a power of 98% to detect 3% change in corneal swelling difference, with an overall type I error controlled at 5%. The power was only 70% to detect a difference of 2%. The sample size calculation was conducted using an extension of the O’Brien and Lohr (1984) method for linear mixed models, with a type I error rate of 0.025.
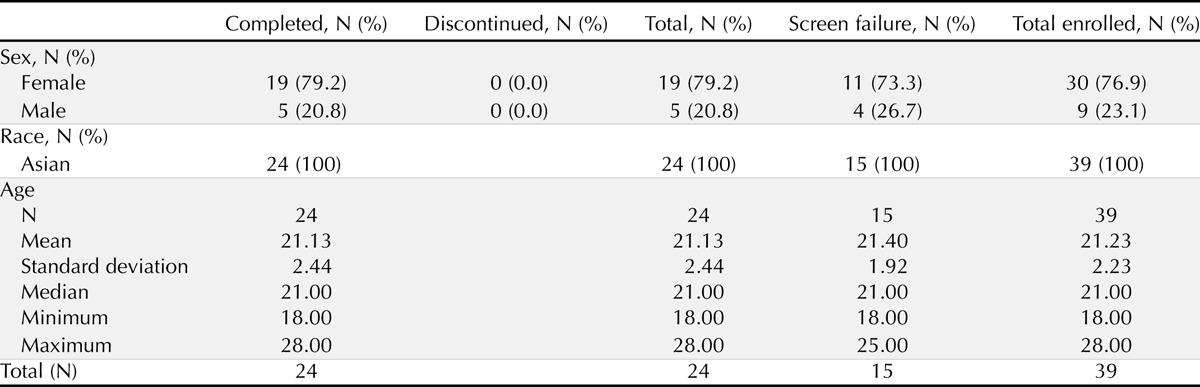
Thirty-nine subjects of self-reported Asian descent were enrolled in this study, from which 15 subjects were ineligible (screen failures who did not meet study inclusion/exclusion criteria). Twenty-four eligible subjects were randomized, and all completed the study. To be eligible, subjects were required to be between the ages of 18 and 45 years and to be current daily contact lens wearers with normal eyes. Demographics of the study participants are listed in Table 1.
TABLE 1.
Subject demographics
Lenses and Solutions
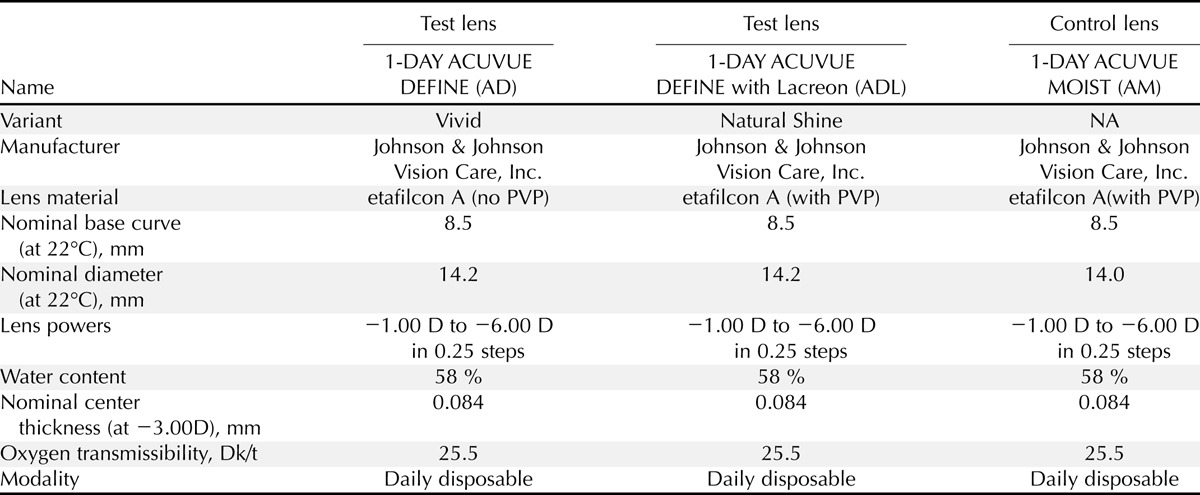
The three study lenses and their parameters are listed in Table 2. On each study day, a research assistant assigned the lens type for each subject according to a randomization table. Subjects wore the lenses for 8 ± 1 h and discarded each pair of the study contact lenses at the end of the respective study day.
TABLE 2.
Lens parameters
There were no contact lens care solutions or any other contact lens care products used in this study. The use of rewetting drops was not permitted in this study to avoid any confounding effects on the study outcome variables.
Procedures
The study included a screening visit and four study phases. In each study phase, one of four randomly assigned study treatments (one of three contact lens types or spectacle wear) was used bilaterally; contact lenses were worn on a daily disposable basis. Subjects were dispensed the study treatment during a baseline visit in the morning (a.m.) and returned to the Centre for Contact Lens Research after 8 ± 1 h of lens wear (p.m.). Prior to attending any of the four study phases, each participant was required to cease contact lens wear for a minimum washout period of 24 hours. In addition, each participant was instructed to wake up at least 3 hours before attending each baseline visit to ensure that any residual corneal swelling from overnight eye closure had dissipated.31–33
Central corneal thickness at baseline (am) and immediately after lens removal (pm) was measured for one eye (determined randomly) with a modified optical pachymeter (OP) on a Zeiss biomicroscope, interfaced to a desktop computer. The pachymetry measurement included seven readings; the computer was programmed by custom software to remove the highest and lowest readings and to calculate the average of the remaining five readings to provide a measure of the central corneal thickness. The OP was calibrated at the beginning of the study using a calibration method described elsewhere34 and its calibration was verified before taking the measurements on each study day throughout the study period. Corneal thickness of the contralateral eye was measured using the Visante optical coherence tomographer (OCT) (Carl Zeiss Meditec, Jena, Germany) pachymetry map for corneal thickness data along the horizontal meridian, within a range from -5 to +5 mm around the center of the cornea (Fig. 1).
FIGURE 1.
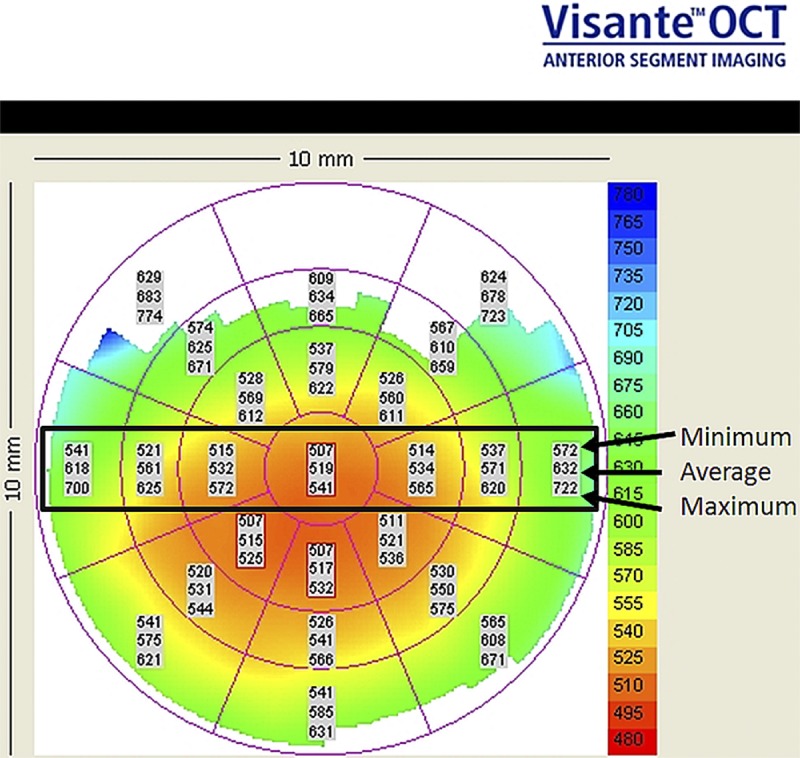
Example of OCT pachymetry map.
These measurements comprised the average data for the central 0- to 2-mm cornea and both temporal and nasal 2- to 5-mm pericentral, 5- to 7-mm transitional/midperipheral and 7- to 10-mm peripheral zones along the horizontal meridian. The mean corneal thickness at each corneal zone (except central) was derived from averaging the temporal and nasal OCT measurements for that zone. The Visante OCT performance was tested and automatically set when the instrument was turned on at the beginning of each study day using the self-verification test tool provided by the OCT manufacturer.
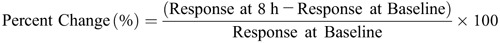
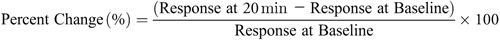
The percentage change of corneal swelling (central for OP and for each zone along the horizontal meridian for OCT) from baseline to 8 ± 1 h follow-up was calculated for each subject/eye and treatment as:
Examination of corneal endothelial cells was conducted using the Topcon SP-3000P Specular Microscope (Topcon Corporation, Tokyo, Japan) and its Cell Count software. Images of the central corneal endothelial specular reflection of approximately 0.25 × 0.5 mm were captured. The instrument features an auto-alignment function that operates over an area of 8 mm2, thereby facilitating repeatable image capture of “good” to “excellent” quality. Immediate inspection of images allowed the observer to grade the image quality and recapture where the quality was considered to be substandard. Images suitable for analysis were obtained before lens insertion and at 20 min after lens wear (repeated accordingly on the day of NLW). No contact with the ocular surface was required. The Topcon SP-3000P has a self-calibrating function that automatically verifies the calibration on turning on the instrument each day. Endothelial cell images were analyzed with ImageNet software (Topcon Corporation, Tokyo, Japan). Although this software determines cell density and coefficient of cell size automatically, endothelial bleb analysis required the bleb areas to be manually identified. A masked observer (who was not one of the clinicians assigned to the study) performed the analysis by subjectively selecting a region in a given image that provided an optimal balance of maximum area and clarity of cell outlines. When blebs are observed with this technique, they are outlined manually, enabling the software to calculate the area of the blebs. This was then compared with the total area of the region selected for analysis to yield the dependent variable of interest, which is the percentage bleb area. Typically, the area of endothelium used to obtain each datum was about 0.03 mm2 and comprised up to 100 cells.
The percentage change in endothelial blebs was calculated from baseline at 20 min after fitting.
In addition to corneal swelling, the ocular physiological impact of the lenses was also assessed by determining the degree of bulbar and limbal hyperemia and corneal staining before lens insertion and after 8 ± 1 h of lens wear. Bulbar and limbal redness was assessed using the Efron grading scales35,36 by quadrant using 0.1 scale increments. Corneal staining by sodium fluorescein was assessed using a combination of severity/degree (type) and area. Severity was assessed using a 0 (none) to 4 (patch) scale,37 and location/area was assessed by recording the area of staining (in 1% increments) for five zones of the cornea.38 Observations were made using a Wratten 12 barrier filter.39
In addition to corneal swelling, the ocular physiological impact of the lenses was also assessed by determining the degree of bulbar and limbal hyperemia and corneal staining before lens insertion and after 8 ± 1 h of lens wear. Bulbar and limbal redness was assessed using the Efron grading scales35,36 by quadrant using 0.1 scale increments. Corneal staining by sodium fluorescein was assessed using a combination of severity/degree (type) and area. Severity was assessed using a 0 (none) to 4 (patch) scale,37 and location/area was assessed by recording the area of staining (in 1% increments) for five zones of the cornea.38 Observations were made using a Wratten 12 barrier filter.39
Data Analysis
All data summaries and statistical analyses were performed using SAS software version 9.2 or higher (SAS Institute, Cary, NC).
For corneal swelling, comparisons between the 1-DAY ACUVUE DEFINE lenses and the 1-DAY ACUVUE MOIST lens or the NLW treatment for the respective location (central, pericentral, midperipheral, peripheral) were conducted using a t-test on least-square means. Adjustment for multiple comparisons was performed using Dunnett’s adjustment method. The corresponding simultaneous confidence intervals (CIs) of least-square means differences (test minus control) were calculated with 95% confidence. A test for noninferiority of a test lens relative to the control lens was carried out by comparing the upper limit CI of the corresponding least-square means difference to the 5% margin. If the upper limit was below 5%, noninferiority was concluded. If the upper limit was below 5% and the lower limit was above −5%, then clinical equivalence was concluded. If noninferiority of both test lenses relative to the control was met, each test lens was compared with when no lenses were worn using a Dunnett’s t-test on least-square means to test for noninferiority.
For endothelial bleb analysis, a mixed-model analysis was planned. However, because of the fact that no blebs were observed for any treatment group at any time point (see Results), no analysis could be conducted.
RESULTS
After 8 ± 1 h of open-eye lens wear, both variants of 1-DAY ACUVUE DEFINE lenses were equivalent or noninferior to NLW and 1-DAY ACUVUE MOIST within ±1%, which was well within the prestated clinical margin of 5% with OP measurement of central corneal swelling (Fig. 2; Table 3).
FIGURE 2.
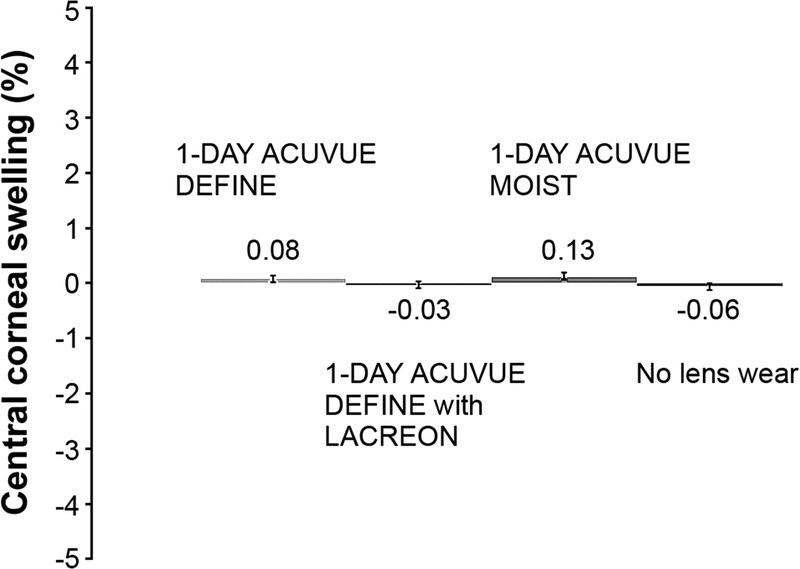
Eight-hour open-eye central corneal swelling (LS mean ± SE) (OP).
TABLE 3.
LS mean difference estimates and 95% CIs of central corneal swelling (in percent) measured with optical pachymetry after 8 ± 1 h of open-eye lens wear
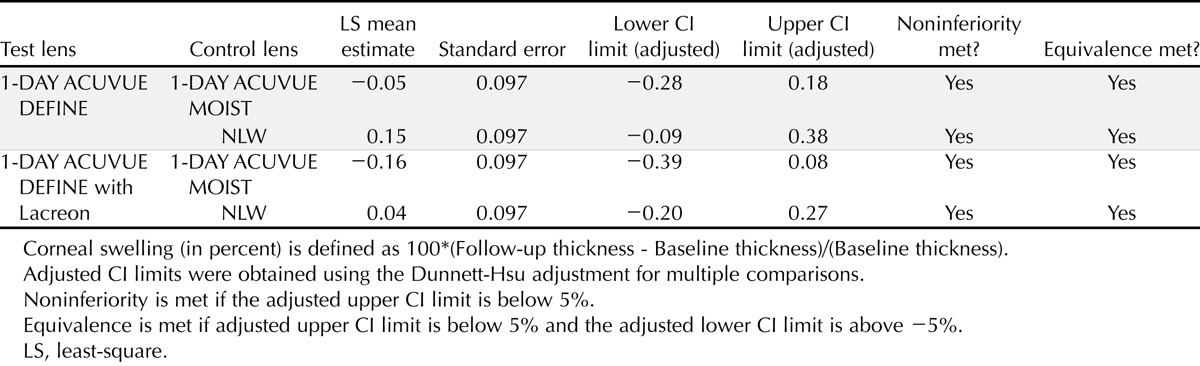
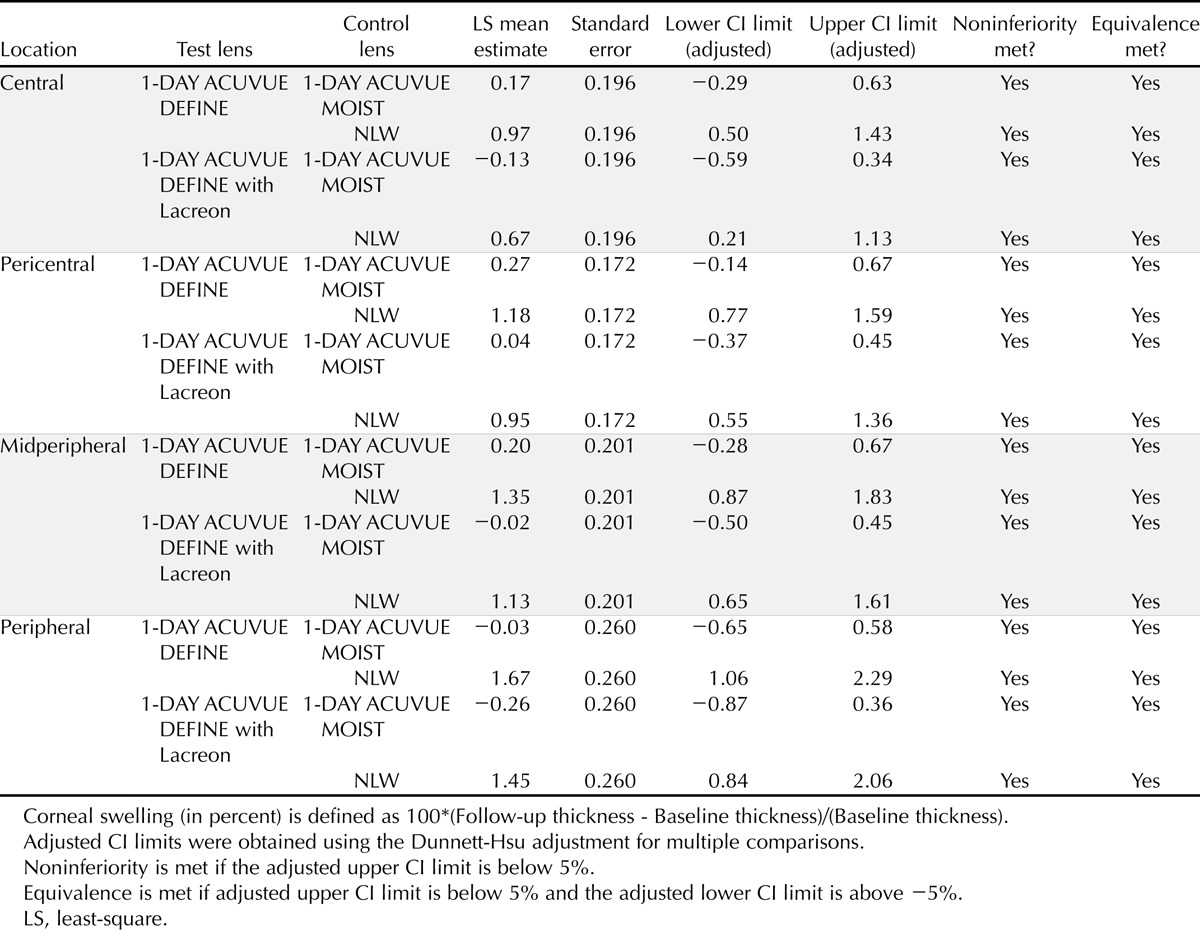
There was also no significant statistical difference within ±3% (which was also well within the prestated clinical margin of ±5%) in OCT measurement of corneal swelling induced with either variant of 1-DAY ACUVUE DEFINE lens compared with either 1-DAY ACUVUE MOIST or NLW treatment in the respective corneal locations along the horizontal meridian (Fig. 3; Table 4).
FIGURE 3.
Eight-hour open-eye corneal swelling (LS mean ± SE) across the cornea (OCT).
TABLE 4.
LS mean difference estimates and 95% CIs of corneal swelling (in percent) along horizontal meridian measured with OCT after 8 ± 1 h of open-eye lens wear
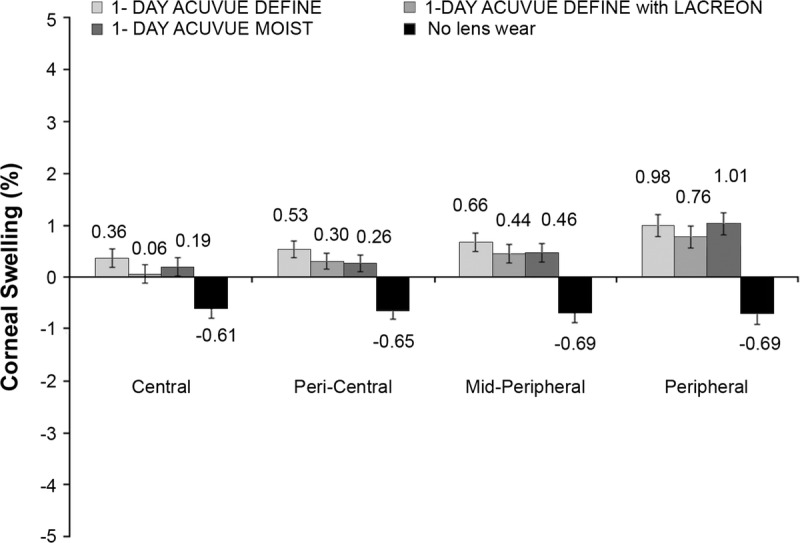
For all subjects on all study days, no endothelial blebs were observed at baseline or after 20 min postfit. Therefore, there was no difference in endothelial bleb response with either 1-DAY ACUVUE DEFINE lens compared with 1-DAY ACUVUE MOIST or NLW.
After 8 ± 1 h of open-eye lens wear, the maximum grade of average limbal hyperemia (on a 0 to 4 scale, 0.1 grade interval) in any quadrant with any study contact lens was not more than 0.16 grade greater than NLW (Fig. 4). At the same time and on the same scale, the maximum grade of average bulbar hyperemia in any quadrant with any study contact lens was not more than 0.20 grade greater than the NLW (Fig. 5).
FIGURE 4.
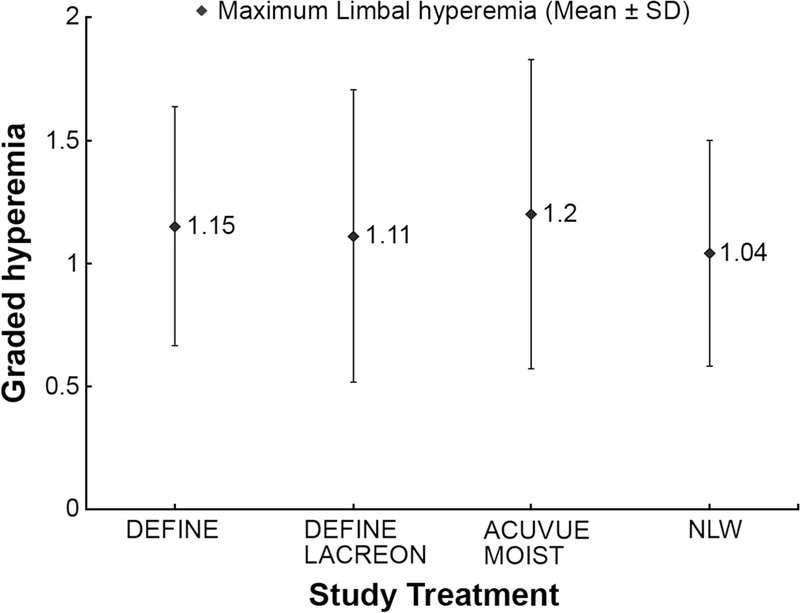
Eight-hour open-eye maximum limbal hyperemia across study treatments.
FIGURE 5.
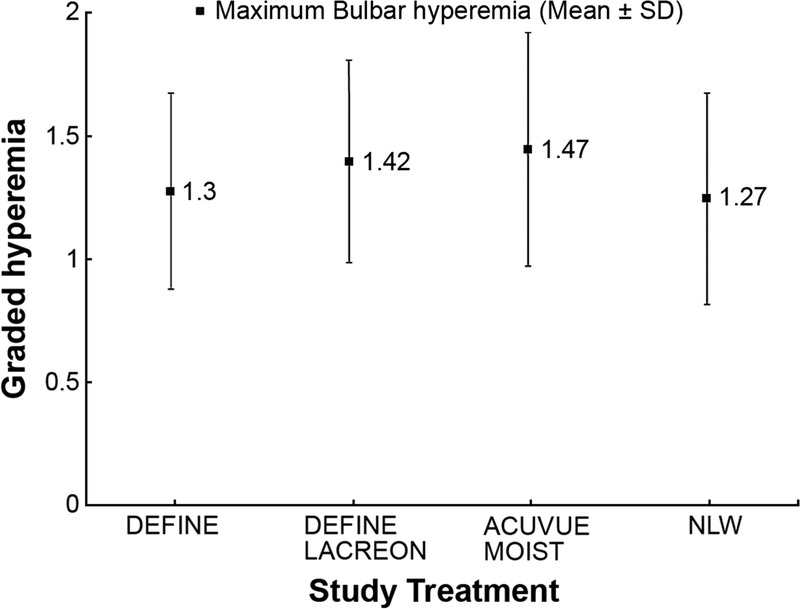
Eight-hour open-eye maximum bulbar hyperemia across study treatments.
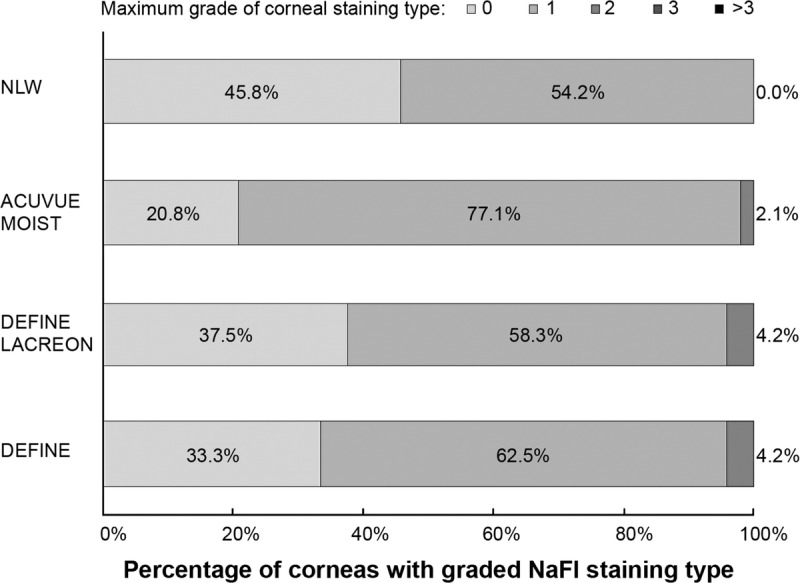
At the end of the wearing period, the maximum grade of average corneal staining type in peripheral corneal quadrants was not more than 1 grade (on 0 to 4 steps) in all eyes (100%) with the NLW treatment compared with 95.8% of eyes with each 1-DAY ACUVUE DEFINE lens and 97.9% eyes with 1-DAY ACUVUE MOIST (Fig. 6). At the same time, the maximum grade of average corneal staining area was not more than 20% of one peripheral corneal quadrant with all study treatments (Fig. 7). No central corneal staining was found with any treatment in this study.
FIGURE 6.
Eight-hour open-eye maximum corneal staining type with study treatments.
FIGURE 7.
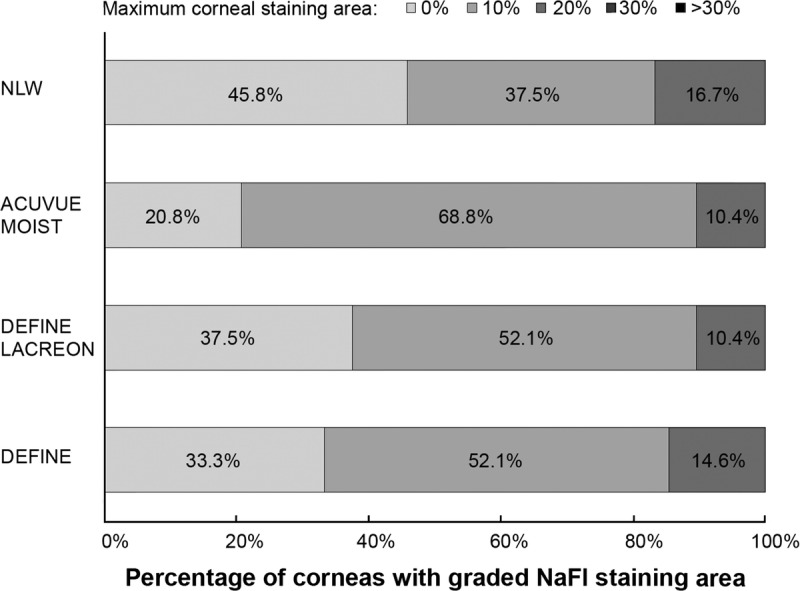
Eight-hour open-eye maximum corneal staining area with study treatments.
DISCUSSION
The primary purpose of this study was to investigate the impact of limbal ring pigments and the incorporation of PVP on the clinical performance of two limbal ring DD contact lenses compared with a clear lens of the same design and NLW. Ocular physiological response to the study treatment was determined by evaluating corneal swelling and endothelial bleb response, in addition to limbal and bulbar hyperemia and corneal staining.
Corneal swelling is regarded as one of the main indices of corneal physiological change as a result of corneal oxygen deficiency by lens wear.40,41 Early studies42,43 for open-eye contact lens wear showed approximately 2% average central corneal swelling with daily wear of conventional hydrogel lenses with low oxygen transmissibility. A more recent study in 2009 by Morgan et al.44 using the Pentacam Scheimpflug imaging system found maximum central swelling of 4.8% and maximum peripheral swelling of 3.3% with open-eye wear of a low oxygen–transmissible hydrogel lens. In this current study, we were unable to detect any clinically significant amount of corneal swelling either centrally or across a horizontal 10-mm diameter (Figs. 2 and 3) with the 1-DAY ACUVUE MOIST lens. This finding is expected because the manufacturer’s published central Dk/t of 25.5 for the study lenses is slightly higher than the Holden and Mertz12 criterion to avoid central corneal swelling in daily wear of 24 Dk/t units. However, the novel finding in this study is that we did not find any statistically or clinically significant differences in central corneal swelling between this clear lens and the two pigmented variants with or without added PVP. This is the first report that the added pigments and PVP have no impact on corneal swelling in vivo.
In a study with soft lens open-eye wear in 2009, Morgan et al.44 suggested a threshold of 32.6 Dk/t for peripheral lens transmissibility compared with 19.8 central lens Dk/t to avoid corneal swelling with daily soft lens wear. They showed a transmissibility range of 6 to 11 Dk/t units in the periphery for −3.00D conventional hydrogel lenses with a central Dk/t in the range of 17 to 30 units, respectively. Therefore, none of the minus-powered conventional hydrogel lenses in their study met the peripheral Dk/t criterion of 32.6 to avoid peripheral corneal swelling. This is in line with findings from Bruce45 who compared local Dk/t measurements of spherical hydrogel and silicone hydrogel lenses of various powers and found a maximum peripheral Dk/t of 16 in only a few hydrogel lenses in low minus powers. In the current study, using a range of minus lens powers from −1.00 to −6.00D, we found an average corneal swelling in the range of 0.76 to 1% approximately 5 mm from the corneal center, which was not statistically or clinically different between the three study contact lenses. Based on the Morgan et al.44 central and peripheral lens transmissibility criteria for conventional hydrogel lenses, we estimate an oxygen transmissibility of about 10.5 peripheral Dk/t for a 1-DAY ACUVUE of −3.00D power. For a 10.5 peripheral Dk/t, using the graph from the same article,44 a peripheral swelling of approximately 1% is estimated, which is consistent with the peripheral corneal swelling findings from this current study (Fig. 3). We found that the cornea in no lens wearing control eyes became thinner by about −0.6% in all locations at the end of the day (Fig. 3). The slight corneal thinning with NLW in this study was expected based on diurnal variation in corneal thickness.46 Also, the same graphs by Morgan et al.44 predict slight amounts of corneal thinning for oxygen transmissibility values in excess of their suggested central and peripheral criterion of 19.8 and 32.6 Dk/t, respectively.
Previous work has shown that the endothelial bleb response can be used as an indicator of oxygen performance.9 Holden et al.6 showed that the endothelial bleb response in open-eye lens wear can be prevented by using a high oxygen–transmissible lens. We were unable to record any endothelial blebs with open-eye contact lens wear of any of the study lenses in this study. This is consistent with a result of another study by Rivera and Polse47 who suggested a minimum Dk/t of 17.2 to minimize or avoid corneal acidosis in soft lens open-eye wear. We used Asian subjects for this study because they were previously shown to develop greater extents of corneal endothelial blebs than non-Asians.9 After 20 min of lens wear and eye closure using soft contact lenses (Dk/t range of 24 to 175 units), Hamano et al.9 found trace amounts of the bleb response in more than one-third of Asian subjects compared with no bleb response in the non-Asian group. In addition, the magnitude of the bleb response in their study was inversely related to the lens oxygen transmissibility in the Asian group. Brennan et al.11 later found a similar association between the endothelial bleb response and soft lens oxygen transmissibility (Dk/t range of 4 to 175 units) in another study on Asian subjects.
Limbal hyperemia is regarded as a sign of peripheral corneal oxygen deprivation with open-eye contact lens wear.48 It was shown that limbal hyperemia can be eliminated by using highly oxygen–transmissible silicone hydrogel lenses.48–50 In a recent study, Brennan and Osborn51 found statistically significantly greater corneal swelling and limbal hyperemia with daily wear of a low Dk hydrogel lens compared with silicone hydrogel lenses. However, the differences were not clinically significant. In a previous study with normal conjunctival hyperemia, Murphy et al.52 concluded that a change of 0.40 grade or higher in bulbar redness may be considered clinically significant. Although they used a different subjective grading system (CCLRU), the grading scale limits (i.e., grading from 0 to 4) were the same as the Efron scale in the present study. We found no clinical difference in either limbal or bulbar hyperemia among the study contact lenses (Figs. 4 and 5). Also, the maximum increase in average graded limbal or bulbar hyperemia for the study lenses compared with NLW was 0.20 grade or less, which we considered clinically insignificant. This closely follows the absence of any reported change in ocular redness by the study subjects during the course of the 8-h wearing period. Finally, the amount of corneal staining recorded (Figs. 6 and 7) were also clinically irrelevant.
In summary, we found minimal impact on corneal physiology with open-eye contact lens wear in this study. This was determined by clinically insignificant levels of corneal swelling, measured by both OCT and OP methods, which could not be statistically differentiated after 8 ± 1 h of lens wear at each corneal location among the study lenses or in comparison with NLW using a 5% difference in swelling as the clinical margin. The minimal impact of the study lenses on corneal physiology is further supported by the complete absence of any endothelial blebs at 20 min after lens wear and the presence of clinically insignificant levels of corneal staining53 and minimal difference in limbal or bulbar hyperemia52,54 between either 1-DAY ACUVUE DEFINE lenses and their clear equivalent lens control or between the three study contact lenses compared with NLW. These study results confirm that the addition of PVP or the limbal ring pigment to etafilcon A lenses has no clinically meaningful effect on the corneal swelling response to open-eye daily wear. All three study lenses can therefore be interchangeably used for open-eye daily disposable wear, with the anticipation of minimal physiological difference from no lens wear.
Amir M. Moezzi
Centre for Contact Lens Research
School of Optometry and Vision Science
University of Waterloo
200 University Ave W
Waterloo Ontario N2L 3G1
Canada
e-mail: ammoezzi@uwaterloo.ca
ACKNOWLEDGMENTS
Supported by Johnson & Johnson Vision Care, Inc.
Kathrine Osborn Lorenz and Danielle Boree are employees of Johnson & Johnson Vision Care, Inc. Lyndon Jones has received lectureship honoraria from Alcon and Johnson & Johnson Vision Care, Inc. Centre for Contact Lens Research employees listed have received funds for conducting research from Advanced Vision Research, Alcon, AlgiPharma, Allergan, CIBA Vision, CooperVision, Essilor, J&J Vision Care, Ocular Dynamics, Oculus, Ocusense, TearScience, and Visioneering Technologies.
Presented in part as a poster at the ARVO annual meeting, May 2014, Orlando, Florida, and as a poster at the British Contact Lens Association meeting, June 2014, Manchester, United Kingdom.
REFERENCES
- 1. Klyce SD. Stromal lactate accumulation can account for corneal oedema osmotically following epithelial hypoxia in the rabbit. J Physiol (Lond) 1981; 321: 49– 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Holden BA. The Glenn A. Fry Award lecture 1988: the ocular response to contact lens wear. Optom Vis Sci 1989; 66: 717– 33. [PubMed] [Google Scholar]
- 3. Liesegang TJ. Physiologic changes of the cornea with contact lens wear. CLAO J 2002; 28: 12– 27. [PubMed] [Google Scholar]
- 4. Sweeney DF. Have silicone hydrogel lenses eliminated hypoxia? Eye Contact Lens 2013; 39: 53– 60. [DOI] [PubMed] [Google Scholar]
- 5. Bonanno JA, Polse KA. Corneal acidosis during contact lens wear: effects of hypoxia and CO2. Invest Ophthalmol Vis Sci 1987; 28: 1514– 20. [PubMed] [Google Scholar]
- 6. Holden BA, Williams L, Zantos SG. The etiology of transient endothelial changes in the human cornea. Invest Ophthalmol Vis Sci 1985; 26: 1354– 9. [PubMed] [Google Scholar]
- 7. Efron N. Endothelial blebs. In: Efron N, ed. Contact Lens Complications, 3rd ed London: Saunders; 2012; 278– 84. [Google Scholar]
- 8. Zantos SG, Holden BA. Transient endothelial changes soon after wearing soft contact lenses. Am J Optom Physiol Opt 1977; 54: 856– 8. [DOI] [PubMed] [Google Scholar]
- 9. Hamano H, Jacob JT, Senft CJ, Hamano T, Hamano T, Mitsunaga S, Kotani S, Kaufman HE. Differences in contact lens-induced responses in the corneas of Asian and non-Asian subjects. CLAO J 2002; 28: 101– 4. [PubMed] [Google Scholar]
- 10. Inagaki Y, Akahori A, Sugimoto K, Kozai A, Mitsunaga S, Hamano H. Comparison of corneal endothelial bleb formation and disappearance processes between rigid gas-permeable and soft contact lenses in three classes of DK/L. Eye Contact Lens 2003; 29: 234– 7. [DOI] [PubMed] [Google Scholar]
- 11. Brennan NA, Coles ML, Connor HR, McIlroy RG, Gavras S, Moody KJ, Henderson T. Short-term corneal endothelial response to wear of silicone-hydrogel contact lenses in East Asian eyes. Eye Contact Lens 2008; 34: 317– 21. [DOI] [PubMed] [Google Scholar]
- 12. Holden BA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci 1984; 25: 1161– 7. [PubMed] [Google Scholar]
- 13. Papas E. On the relationship between soft contact lens oxygen transmissibility and induced limbal hyperaemia. Exp Eye Res 1998; 67: 125– 31. [DOI] [PubMed] [Google Scholar]
- 14. Morgan PB, Woods CA, Tranoudis IG, Helland M, Efron N, Jones L, Davila-Garcia E, Magnelli P, Teufl M, Grupcheva CN, et al. International contact lens prescribing in 2014. Contact Lens Spect 2015; 30(January 2015): 28– 33. [Google Scholar]
- 15. Morgan PB, Efron N. The oxygen performance of contemporary hydrogel contact lenses. Cont Lens Anterior Eye 1998; 21: 3– 6. [DOI] [PubMed] [Google Scholar]
- 16. Tighe BJ. Contact lens materials. In: Phillips AJ, Speedwell A, eds. Contact Lenses. Edinburgh: Butterworth-Heinemann; 2006: 59– 78. [Google Scholar]
- 17. Chalmers RL, Hickson-Curran SB, Keay L, Gleason WJ, Albright R. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci 2015; 56: 654– 63. [DOI] [PubMed] [Google Scholar]
- 18. Varikooty J, Keir N, Richter D, Jones LW, Woods C, Fonn D. Comfort response of three silicone hydrogel daily disposable contact lenses. Optom Vis Sci 2013; 90: 945– 53. [DOI] [PubMed] [Google Scholar]
- 19. Varikooty J, Schulze MM, Dumbleton K, Keir N, Woods CA, Fonn D, Jones LW. Clinical performance of three silicone hydrogel daily disposable lenses. Optom Vis Sci 2015; 92: 301– 11. [DOI] [PubMed] [Google Scholar]
- 20. Jones L. Currently available disposable contact lens systems. Optician 1995; 209: 16– 22. [Google Scholar]
- 21. Jones L, Jones D, Langley C, Houlford M. Subjective responses of 100 consecutive patients to daily disposables. Optician 1996; 211: 28– 32. [Google Scholar]
- 22. Solomon OD, Freeman MI, Boshnick EL, Cannon WM, Dubow BW, Kame RT, Lanier JC, Jr., Lopanik RW, Quinn TG, Rigel LE, et al. A 3-year prospective study of the clinical performance of daily disposable contact lenses compared with frequent replacement and conventional daily wear contact lenses. CLAO J 1996; 22: 250– 7. [PubMed] [Google Scholar]
- 23. Nichols JJ. A look at lubricating agents in daily disposables. Contact Lens Spect 2007; 22(January 2007): 22. [Google Scholar]
- 24. Veys J, Meyler J. Do new daily disposable lenses improve patient comfort? Optician 2006; 231: 34– 6. Available at: http://www.opticianonline.net/do-new-daily-disposable-lenses-improve-patient-comfort/ Accessed October 20, 2015. [Google Scholar]
- 25. Sheardown H, Liu L, Jones L. Chemical characterization of 1-Day Acuvue Moist and 1-Day Acuvue contact lenses. Invest Ophthalmol Vis Sci 2006; 47: E-abstract 2388. [Google Scholar]
- 26. Lorenz K, Tosatti S, Kakkassery J, Aeschlimann R, Boree D. Location of lens pigment with etafilcon A daily disposable limbal ring hydrogel contact lenses and the effect on coefficient of friction. Cont Lens Anterior Eye 2015; 38(Suppl. 1): e23 Available at: http://www.contactlensjournal.com/article/S1367-0484%2814%2900165-9/fulltext Accessed October 21, 2015. [Google Scholar]
- 27. Lorenz KO, Kakkassery J, Boree D, Pinto D. Atomic force microscopy and scanning electron microscopy analysis of daily disposable limbal ring contact lenses. Clin Exp Optom 2014; 97: 411– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mayers M, Jansen M, Lorenz KO. Defining eye enhancement—part 2. Optician 2014; 248: 17– 8. Available at: http://www.opticianonline.net/defining-eye-enhancement-part-2/ Accessed October 20, 2015. [Google Scholar]
- 29. Walsh K. Defining eye enhancement. Optician 2014; 248: 18– 23. Available at: http://www.opticianonline.net/defining-eye-enhancement/. Accessed October 20, 2015. [Google Scholar]
- 30. McCarthy K. Color contact lenses and oxygen permeability. Optom Vis Sci 2006; 83: E-abstract 065274. [Google Scholar]
- 31. Mandell RB, Fatt I. Thinning of the human cornea on awakening. Nature 1965; 208: 292– 3. [DOI] [PubMed] [Google Scholar]
- 32. Mertz GW. Overnight swelling of the living human cornea. J Am Optom Assoc 1980; 51: 211– 4. [PubMed] [Google Scholar]
- 33. O’Neal MR, Polse KA. In vivo assessment of mechanisms controlling corneal hydration. Invest Ophthalmol Vis Sci 1985; 26: 849– 56. [PubMed] [Google Scholar]
- 34. Moezzi AM, Sin S, Simpson TL. Novel pachometry calibration. Optom Vis Sci 2006; 83: 366– 71. [DOI] [PubMed] [Google Scholar]
- 35. Efron N. Grading scales for contact lens complications. Ophthalmic Physiol Opt 1998; 18: 182– 6. [DOI] [PubMed] [Google Scholar]
- 36. Efron N, Morgan PB, Katsara SS. Validation of grading scales for contact lens complications. Ophthalmic Physiol Opt 2001; 21: 17– 29. [PubMed] [Google Scholar]
- 37. Back A. Corneal staining with contact lens wear. J Br Contact Lens Assoc 1988; 11: 16– 8. [Google Scholar]
- 38. Caffery BE, Josephson JE. Corneal staining after sequential instillations of fluorescein over 30 days. Optom Vis Sci 1991; 68: 467– 9. [DOI] [PubMed] [Google Scholar]
- 39. Cox I, Fonn D. Interference filters to eliminate the surface reflex and improve contrast during fluorescein photography. Int Contact Lens Clin 1991; 18: 178– 81. [Google Scholar]
- 40. Bruce AS, Brennan NA. Corneal pathophysiology with contact lens wear. Surv Ophthalmol 1990; 35: 25– 58. [DOI] [PubMed] [Google Scholar]
- 41. Fonn D, Sweeney D, Holden BA, Cavanagh D. Corneal oxygen deficiency. Eye Contact Lens 2005; 31: 23– 7. [DOI] [PubMed] [Google Scholar]
- 42. Weissman BA, Blaze PA, Ingles S, Wheeler N. Open-eye corneal swelling secondary to hydrogel contact lens wear. Am J Optom Physiol Opt 1988; 65: 272– 6. [DOI] [PubMed] [Google Scholar]
- 43. La Hood D. Daytime edema levels with plus powered low and high water content hydrogel contact lenses. Optom Vis Sci 1991; 68: 877– 80. [DOI] [PubMed] [Google Scholar]
- 44. Morgan PB, Brennan NA, Maldonado-Codina C, Quhill W, Rashid K, Efron N. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye soft contact lens wear. J Biomed Mater Res (B) 2010; 92: 361– 5. [DOI] [PubMed] [Google Scholar]
- 45. Bruce A. Local oxygen transmissibility of disposable contact lenses. Cont Lens Anterior Eye 2003; 26: 189– 96. [DOI] [PubMed] [Google Scholar]
- 46. du Toit R, Vega J, Fonn D, Simpson T. Diurnal variation of corneal sensitivity and thickness. Cornea 2003; 22: 205– 9. [DOI] [PubMed] [Google Scholar]
- 47. Rivera RK, Polse KA. Effects of hypoxia and hypercapnia on contact lens-induced corneal acidosis. Optom Vis Sci 1996; 73: 178– 83. [DOI] [PubMed] [Google Scholar]
- 48. Papas EB, Vajdic CM, Austen R, Holden BA. High-oxygen-transmissibility soft contact lenses do not induce limbal hyperaemia. Curr Eye Res 1997; 16: 942– 8. [DOI] [PubMed] [Google Scholar]
- 49. Dumbleton K, Keir N, Moezzi A, Feng Y, Jones L, Fonn D. Objective and subjective responses in patients refitted to daily-wear silicone hydrogel contact lenses. Optom Vis Sci 2006; 83: 758– 68. [DOI] [PubMed] [Google Scholar]
- 50. Dumbleton KKN, Moezzi AM, Jones L, Fonn D. Redness, dryness and comfort following refitting long term low Dk hydrogel wearers with silicone hydrogels. Optom Vis Sci 2004; 81(Suppl.): 31. [Google Scholar]
- 51. Brennan N, Osborn K. Ocular response to narafilcon B. Optom Vis Sci 2010; 87: E-abstract 105281. [Google Scholar]
- 52. Murphy PJ, Lau JS, Sim MM, Woods RL. How red is a white eye? Clinical grading of normal conjunctival hyperaemia. Eye (Lond) 2007; 21: 633– 8. [DOI] [PubMed] [Google Scholar]
- 53. Peterson R, Woods C, Fonn D. Comparing the CCLR grading system for corneal staining to a traditional 0–4 scale. Optom Vis Sci 2008; 85: E-abstract 85324. [Google Scholar]
- 54. Pult H, Murphy PJ, Purslow C, Nyman J, Woods RL. Limbal and bulbar hyperaemia in normal eyes. Ophthalmic Physiol Opt 2008; 28: 13– 20. [DOI] [PubMed] [Google Scholar]


