Child maltreatment presents a substantial public health concern. Estimates using Child Protective Service (CPS) reports from the National Child Abuse and Neglect Data System (NCANDS) suggest that 678,810 youth were subjected to maltreatment in 2012 with 18% of these experiencing physical abuse (U. S. Department of Health and Human Services et al., 2013). Additionally a large proportion of cases are undetected by CPS, suggesting that a greater number of youth is likely subjected to abusive or neglectful behavior (Fallon et al., 2010). Most seriously, maltreatment was responsible for an estimated 1,640 youth fatalities in 2012 (U. S. Department of Health and Human Services et al., 2013).
Childhood victimization has been found to have lasting detrimental effects. Victims of child physical abuse (CPA) are more likely to struggle with internalizing, externalizing, and health problems, and to perpetrate aggressive behavior and intimate partner violence, compared to individuals without abuse histories (Milaniak & Widom, 2015; Springer, Sheridan, Kuo & Carnes, 2007; Sugaya et al., 2012). CPA also appears to be associated with structural and functional brain changes and abnormality in systems involved in emotion, executive control, and stress response (Hart & Rubia, 2012; Leeb, Lewis & Zolotor, 2011; McCrory, De Brito & Viding, 2012). In sum, CPA has a devastating impact on victims and presents an important public health concern. Understanding variables contributing to perpetration of CPA may help decrease the harm done to victims. If emotional and behavioral characteristics associated with caregiver aggression are better understood, effectiveness of intervention and prevention strategies targeting this behavior can be improved.
Current Study
The purpose of the current study is three-fold. First, we wanted to identify characteristics that are thought to distinguish abusive from non-abusive caregivers (as indicated by official records) in a help-seeking sample of high conflict families. Second, because a large proportion of maltreatment is not identified by CPS (Fallon et al., 2010), we were interested in identifying if similar characteristics would differentiate caregivers who do vs. do not report any severe child-directed aggression, regardless of whether they had an official record for child physical abuse. Use of both official records and self-report methodology to identify subgroups of aggressive and abusive caregivers provides a means to identify clinical characteristics of each group and explore similarities between them. Third, we wanted to test a proposed model of dysfunction describing relationships between parenting stress, negative affect, positive parenting, and child directed aggression and to assess their associations with other relevant factors.
Understanding characteristics of abusive and aggressive caregivers and the interrelation between these subgroups would inform advances in both case conceptualization and intervention efforts. Identifying clinical variable differences characterizing physically abusive caregivers (vs. those without official records) and caregivers engaging in any severe child directed aggression (vs. not) may help to inform conceptualization of risk and treatment emphasis. Experiencing parenting stress (Black, Heyman & Smith-Slep, 2001; Haskett, Ahern, Ward & Allaire, 2006; McPherson, Lewis, Lynn, Haskett & Behrend, 2008), greater negative affect (Mammen, Kolko & Pilkonis, 2002; Mammen, Pilkonis & Kolko, 2000; Smith, Cross, Winkler, Jovanovic & Bradley, 2014), poorer parenting (Wilson, Rack, Shi & Norris, 2008), and more drug and alcohol use (Friesthler, 2011; Friesthaler & Gruenewald, 2013; Laslett, Room, Dietze & Ferris, 2012; Oral et al., 2011) have been associated with abusive and aggressive caregiving. Child physical abuse commonly occurs with other forms of maltreatment (Stevens, Schneiderman, Negriff, Brinkmann & Trickett, 2015), including child neglect, although this comorbidity has received less attention within the extant literature (Stoltenborg, Bakermans-Kraneburg, Alink & van IJzendoorn, 2014) and merits additional explication.
In addition to characterizing aggressive/abusive caregivers, we sought to test a structural equation model of dysfunction examining the contribution of parenting stress to child directed aggression. Parenting stress has been related to greater abuse risk (Black, Heyman & Smith-Slep, 2001; Haskett et al., 2006; McPherson et al., 2008), however it does not always lead to this behavior. Associated variables may account for some of this relationship: parenting stress has been related to higher negative affect (Haskett et al., 2006) and less positive parenting (Park & Walton-Moss, 2012). Negative affect and dysregulation of negative emotion have been associated with CPA perpetration (Mammen et al., 2002; Mammen et al., 2000; Smith et al., 2014) and positive parent-child interactions appear protective against child abuse (Thornberry et al., 2013; Wilson et al., 2008).
Stressed parents who experience more symptoms of negative affect or have fewer positive parenting interactions may be more likely to engage in child directed aggression. In addition to testing this model, we examine relationships between child directed aggression and drug and alcohol use and the contribution of affective and parenting variables to neglect to see the manner in which these variables could be integrated into a conceptualization of dysfunction. The current examination tests the contribution of negative affect to aggressive caregiving, while placing it in the context of parenting stress and positive parent child interactions. Additionally, applicability of this model to child neglect and the impact of drug and alcohol use is examined. Our project contributes to understanding factors contributing to aggressive and abusive caregiving and tests a model of relationships between affective and parenting components and aggression.
Method
Participants
Participants were 195 caregivers who were seeking services from providers in 10 community agencies. Families were referred to the trial by local mental health agencies due to experience of family conflict or aggression. All had been identified during a study screening interview as having a recent (6 months) history of or being at risk for CPA. Among our families, 83.6% (n = 163) of participants were included due to reported family use of physical force with a child, 82.6% (n = 161) for caregiver and child physical conflict, 94.9% (n = 185) any caregiver harming or injuring a child, and 37.4% (n = 73) for report of physical abuse or child maltreatment. Thus, participants were caregivers within high conflict aggressive families.
Families were generally economically disadvantaged, with household incomes as follows; 42.1% making $14,999 or less, 27.2% $15,000-$29,999, 10.3% 30,000-49,999, 4.1% 50,000-74,999, 2.6% making $75,000 or more, and 13.8% being unable to estimate or declining to respond. Caregivers were 8.7% male and 91.3% female. Ethnic composition was as follows: 1.5% American Indian or Alaskan Native, 0% Asian, 0.5% Native Hawaiian or Pacific Islander, 37.4% Black or African American, 62.1% White, 2.6% not reported, and 4.1% Latino or Hispanic. Mean caregiver age was 37.81 (SD = 8.04). Children of caregivers involved were 46.2% female and 53.8% male with ethnic composition as follows: 2.6% American Indian or Alaskan Native, 0% Asian, 0% Native Hawaiian or Pacific Islander, 50.3% Black or African American, 56.9% White, 3.6% not reported, and 4.1% Latino or Hispanic. Mean child age was 11.49 (SD = 3.14). A fairly substantial proportion of caregivers reported recent difficulties with aggressiveness towards youth: 29.2% (n = 57) reported threatening to use physical force, 13.3% (n = 26) admitted to using physical force, and 1.5% (n = 3) reported injuring a child. Among caregivers 14.7% (n = 28) have been identified as having a CPS report having been filed against them for child physical abuse.
Assessment
Trained research associates completed assessments with caregivers and children over the course of this trial that captured the child, caregiver, and family/environment domains. The current study data reflect baseline assessments during which caregivers completed standardized self-report and interview measures in the domains of emotional response, parenting and associated behaviors, and child directed aggression.
Measures
Brief Symptom Inventory-18 (BSI-18; Derogatis, 2000)
BSI-18 is a measure of psychological distress that highlights affective features. BSI provides scales assessing for symptoms of Depression, Anxiety, and Somatization with a five point Likert type scale. BSI-18 has received psychometric support and higher scores indicated greater difficulties in these areas.
Parenting Stress Index-Short Form (PSI-SF; Abidin, 1995)
PSI-SF is a 36-item measure of stress associated with parenting. PSI-SF provides three subscales: Difficult Child, Parental Distress, and Parent Child Dysfunctional Interaction. Parenting Distress measures negative emotions and perceived limitations associated with caregiver role. Difficult Child assesses the extent to which a caregiver views his or her child as possessing behavioral difficulties. Parent Child Dysfunctional Interaction measures the extent to which the caregiver feels dissatisfied within the relationship. Higher scores on these scales indicate greater difficulties.
Alabama Parenting Questionnaire (APQ; Shelton, Frick, & Wootton, 1996)
APQ is a 42-item psychometrically validated questionnaire assessing a range of parenting practices. APQ provides Parental Involvement, Positive Parenting, Inconsistent Discipline, Corporal Punishment, Poor Parental Monitoring and Supervision, and Other Discipline scales. Higher scores on this measure indicate more engagement in associated parenting behavior.
Mother Child Neglect Scale-Short Form (MCNS-SF; Lounds, Borkowski & Whitman, 2004)
MCNS-SF is an eight-item measure providing an assessment of care for a child's supervision, physical, and emotional needs using a four point Likert type response scale. Higher scores on this measure indicate greater caregiver neglect. Psychometric and validity support for MCNS-SF has been obtained (Lounds et al., 2004). MCNS-SF scores have been correlated with poorer quality of maternal interactions and greater child abuse potential, providing validity support (Lounds et al., 2004). Parent reported MCNS-SF scores were used in this examination.
Short Alcohol and Drug Use Questionnaire (SADUQ; Donovan, 1993)
SADUQ is a brief measure of parental drug and alcohol use adapted from Donovan (1993). This measure assesses how much and how often caregivers drank over the prior six months and how frequently they used a variety of drugs including marijuana, crack cocaine, Quaaludes, heroin, and inhalants. SADUQ provides Alcohol and Drug Use subscales.
Conflict Tactics Scale (CTS; Straus, Hamby, Finkelhor, Moore, & Runyan, 1998)
CTS is a 22-item measure of responses to family conflict. CTS consist of scales measuring use of Non-Aggressive Discipline strategies (such as time out), Psychological Aggression (e.g., shouting at and threatening a child), Minor Assault (e.g., spanking, pinching), Severe Assault (such as throwing a child down or hitting them with a fist), and Very Severe Assault (e.g., burning a child, threatening with a weapon). Caregivers were asked to indicate how frequently they have engaged in each behavior over the past year, with higher scores indicating greater frequency. Endorsement of any items on the Severe Assault and Very Severe Assault scales was used to classify caregivers engaging in any severe child directed aggression (yes/no).
Maltreatment Classification System (MCS; Barnett, Manly, & Cicchetti, 1993)
The MCS was used in conjunction with official CPS record reviews for one year prior to the beginning of the study. The MCS allows for classification of CPS reports according to the type of maltreatment and perpetrator. It has been shown to have strong psychometric properties (see Manly, Cicchetti, & Barnett, 1994). Data were used to classify caregivers with a legal record of CPA.
Results
Preliminary Analyses: Data Preparation
Data were examined for the presence of univariate and multivariate outliers. No multivariate scores were identified and following Kline's (2011) suggestion univariate outlier scores were winsorized prior to analyses. In order to normalize scores on APQ Corporal Punishment a square root transformation was applied. In order to normalize scores on SADUQ Drug, CTS Minor Assault, and CTS Severe Assault a natural log transformation was applied. A reciprocal transformation was applied to reduce skew and kurtosis in CTS Very Severe Assault.
Preliminary Analyses: Demographic Differences
First we were interested in the effect of demographic differences on engagement in child directed aggression and related problematic behaviors. Participants were collapsed across four minority ethnic categories and we examined whether minority status (white/non-Latino compared to Latino and minority ethnicities) was associated with extent of engaging in child directed aggression, neglect, and drug and alcohol use in a multivariate analysis of variance (MANOVA). Minority status was not associated with differences in engagement in these behaviors. There were also no differences in minority status in relation to having a CPS record for child physical abuse in a χ2 analysis. Given the overwhelming female composition of the sample, we did not test for gender differences. Parent age was negatively correlated with Minor Assault (r = −.18, p< .05), Psychological Aggression (r = −.16, p< .05), SADUQ Drug (r = −.19, p<.05), and SADUQ Alcohol (r = −.15, p<.05) scales. Parent age was not significantly related to parenting stress (PSI) or negative affect (BSI) variables or child neglect. Within parenting variables, age was negatively correlated with Inconsistent Disciple (r = −.20, p < .01) and Corporal Punishment (r = −.18, p < .01) and positively correlated with Poor Monitoring (r = .20, p < .01). There was no significant difference in parent age between caregivers with a CPS record of physical abuse compared to those without in an ANOVA.
Overlap Between Self-Reported Severe Aggression & an Official Record of CPA
Given prior research suggesting that physical abuse is not always identified by CPS (Fallon et al., 2010), we were interested in examining the overlap between caregivers who report any severe child directed aggression and those with CPS records. Among our sample 33.5% of caregivers (n = 64) reported engaging in severe child directed aggression and 14.7% (n = 28) had official records of child physical abuse. We explored the overlap between these indicators. We found that, among caregivers without a CPS record, 32.9% (n = 51) of individuals reported engaging in any severe aggression. Additionally, 53.6% of individuals with CPS records (n = 15) denied engaging in any severe aggression. Overall, among participants who had CPS records of physical abuse 15 individuals denied and 13 endorsed engagement in severe aggression. The kappa coefficient between the two metrics was low (.09) and non-significant. Due to lack of congruence between these metrics and small cell sizes we examined differences in severe aggression and CPS physical abuse separately.
Characteristics of Caregivers Engaging in Severe Aggression to Children
A number of caregivers within our clinical sample reported child directed aggression on the CTS: 55.5% endorsed Minor Assault, 31.9% Severe Assault, and 4.6% Very Severe Assault. We examined differences between caregivers who endorsed engaging in any severe aggression (yes vs. no) on parenting behaviors of involvement, positive parenting, poor monitoring, inconsistent discipline, corporal punishment, and use of other discipline strategies, neglect, negative affect variables of anxiety, depression, somatization, parenting stress related to perception of the child as difficult, dysfunctional parent child interactions, and distress in the parental role, and drug and alcohol use. Due to demonstrated relationship between age and parenting behavior and drug and alcohol variables, we ran a MANCOVA analysis to control for the effect of age and examine group differences (Table 1). We found that there was a significant difference between caregivers reporting any severe aggression compared to those who were not on this combination of variables (Wilks’ λ = .65, F (15, 117) = 4.17, p < 0.001, η2p = .35). Caregivers reporting any severe aggression (vs. not) were less involved, used fewer positive parenting strategies, were poorer at monitoring child behavior, used more corporal punishment, were less consistent in applying consequences, used less other discipline strategies, and reported more drug use.
Table 1.
MANCOVA Any (vs. None) Severe Aggression Directed Towards Child (CTS)
| No Severe Aggression | Any Severe Aggression | |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Difficult Child PSI-SF | 40.72 (8.54) | 39.71 (7.94) |
| Parental Distress PSI-SF | 31.90 (10.09) | 34.00 (8.46) |
| Dysfunctional Interaction PSI-SF | 32.15 (8.64) | 32.36 (7.32) |
| Involvement APQ** | 38.35 (6.08) | 34.43 (5.81) |
| Positive Parenting APQ** | 26.07 (3.80) | 23.69 (4.33) |
| Other Discipline APQ* | 22.65 (3.93) | 22.02 (3.73) |
| Poor Monitoring APQ** | 16.97 (5.81) | 19.18 (7.03) |
| Inconsistent Discipline APQ** | 17.08 (4.34) | 19.16 (4.12) |
| Corporal Punishment APQ** | 4.27 (2.10) | 5.80 (1.78) |
| Neglect MCNS-SF | 14.11 (2.71) | 14.73 (2.45) |
| Drug Use SADUQ** | 11.40 (1.43) | 12.11 (2.44) |
| Alcohol Use SADUQ | 6.81 (8.21) | 8.18 (8.63) |
| Depression BSI-18 | 3.98 (4.66) | 5.87 (5.29) |
| Anxiety BSI-18 | 3.54 (4.18) | 4.80 (4.39) |
| Somatization BSI-18 | 2.87 (3.73) | 4.33 (4.50) |
Note:
p ≤ .05
p ≤ .01.
Untransformed values for APQ Corporal Punishment and SADUQ Drug Use are presented to allow for comparison to published literature. PSI-SF = Parenting Stress Index-Short Form, BSI-18 = Brief Symptom Inventory-18, APQ = Alabama Parenting Questionnaire, MCNS-SF = Mother Child Neglect Scale-Short Form, SADUQ = Short Alcohol and Drug Use Questionnaire
Characteristics of Caregivers with CPS Records of Child Physical Abuse
We repeated the above MANCOVA analysis to compare caregivers with (vs. without) a CPS record of child physical abuse using the same variables. We did not find a statistically significant difference between these groups on this combination of variables.
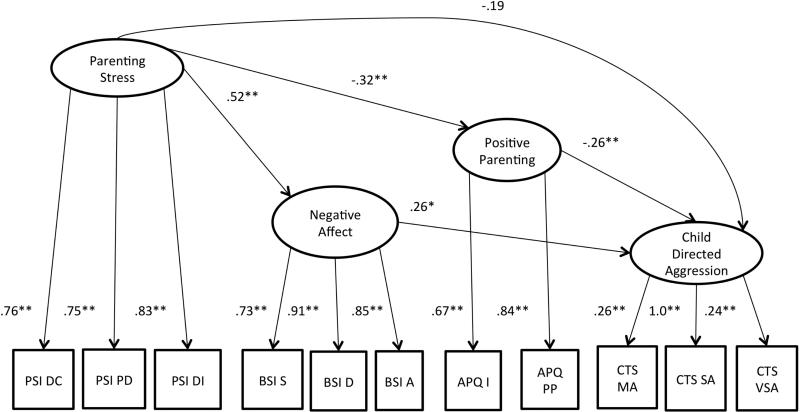
Structural Equation Model Examinations of Dysfunction
We examined the contribution of parenting stress (PSI), negative affect (BSI), and positive parenting behavior (APQ Positive Parenting, APQ Involvement) to engagement in child directed aggression (CTS Minor Assault, Severe Assault, and Very Severe Assault) using structural equation modeling. We expected parents who experienced more parenting stress to have higher negative affect and engage in less positive parenting, with these relationships partially accounting for the influence of parenting stress on child directed aggression. A non-significant negative residual for CTS Severe Assault was fixed to zero to allow the model to run. This model (Figure 1) provided good fit for the data; χ2 = 72.98, df = 40, p =.001, RMSEA = .07, CFI = 0.94, SRMR = .06. As expected, parenting stress predicted higher negative affect and negative affect was related to more child directed aggression. Parenting stress was also associated with less positive parenting and positive parenting was predictive of lower child directed aggression. Parenting stress did not have a direct influence on child directed aggression. However, there were significant indirect effects: parenting stress predicted greater child directed aggression due to its positive influence on negative affect (β= 0.14, p < .05) and due to its negative influence on positive parenting (β = 0.09, p < .05). Mean sample scores for measures used are presented in Table 2.
Figure 1. Structural Regression Model.
Note: * p ≤ .05, ** p ≤ .01. PSI DC = Parenting Stress Index-Short Form Difficult Child, PSI PD = Parenting Stress Index-Short Form Parental Distress, PSI DI = Parenting Stress Index-Short Form Dysfunctional Interaction, BSI S = Brief Symptom Inventory-18 Somatization, BSI D = Brief Symptom Inventory-18 Depression, BSI A = Brief Symptom Inventory-18 Anxiety, APQ I = Alabama Parenting Questionnaire Involvement, APQ PP = Alabama Parenting Questionnaire Positive Parenting, CTS MA = Conflict Tactics Scale Minor Assault, CTS SA = Conflict Tactics Scale Severe Assault, CTS VSA = Conflict Tactics Scale Very Severe Assault.
Table 2.
Mean Scores on Measures Used in Structural Equation Models
| Scale | Mean (SD) |
|---|---|
| Difficult Child PSI-SF | 40.01 (8.37) |
| Parental Distress PSI-SF | 32.76 (9.78) |
| Dysfunctional Interaction PSI-SF | 32.35 (8.10) |
| Involvement APQ | 36.99 (6.43) |
| Positive Parenting APQ | 25.42 (4.12) |
| Neglect MCNS-SF | 14.29 (2.69) |
| Drug Use SADUQ | 11.61 (1.81) |
| Alcohol Use SADUQ | 7.30 (8.14) |
| Depression BSI-18 | 4.61 (4.94) |
| Anxiety BSI-18 | 3.96 (4.28) |
| Somatization BSI-18 | 3.36 (4.05) |
| Minor Assault CTS | 5.02 (9.22) |
| Severe Assault CTS | 1.24 (2.94) |
| Very Severe Assault CTS | .11 (.62) |
Untransformed values for SADUQ Drug, CTS Minor Assault, Severe Assault, and Very Severe Assault scales are presented to facilitate comparison with published literature. PSI-SF = Parenting Stress Index-Short Form, BSI-18 = Brief Symptom Inventory-18, APQ = Alabama Parenting Questionnaire, CTS = Conflict Tactics Scale, MCNS-SF = Mother Child Neglect Scale-Short Form, SADUQ = Short Alcohol and Drug Use Questionnaire
As drug and alcohol use have been related to engagement in child directed aggression, we were interested in determining whether the addition of these variables as predictors of child directed aggression would improve model fit. We added SADUQ Drug and SADUQ Alcohol Use as predictors of child directed aggression to the model described above. Model fit was as follows: χ2 = 111.30, df = 60, p <.001, RMSEA = .07, CFI = 0.92, SRMR = .07. χ2 difference testing was conducted and determined that this model provided significantly poorer fit (χ2diff = 38.32, df = 20, p < 0.05), although drug use was a significant predictor of child directed aggression (β= 0.32, p < .05). However, due to significantly poorer fit, we concluded that the addition of drug and alcohol to the model did not add substantially to the prediction of child directed aggression over and above positive parenting, negative affect, and parenting stress within the current sample.
Structural Regression Model of Contributors to Neglect
As child abuse and neglect frequently co-occur, we wanted to examine whether the model applicable to child directed aggression was similarly applicable to caregiver reported neglect. Firstly we examined the contribution of parenting stress, negative affect, and positive parenting behavior to engagement in neglect using the initial model described above. We found that this model provided good fit for the data: χ2 = 45.62, df = 23, p =.003, RMSEA = .07, CFI = 0.96, SRMR = .05. As in the prior analysis, we found that parenting stress predicted lower positive parenting and higher negative affect. Positive parenting predicted less neglect, although neglect relationships with negative affect and parenting stress were not significant. Additionally, parenting stress did not significantly influence neglect through its effect on positive parenting.
Interested in the potential impact of drug and alcohol use, we added these variables to the model as predictors of neglect. Model fit was as follows: χ2 = 76.02, df = 39, p < .001, RMSEA = .07, CFI = 0.94, SRMR = .07. Drug and alcohol use were not significantly related to neglect within the model. χ2 difference testing was conducted and determined that this model provided significantly poorer fit (χ2diff = 30.40, df = 16, p<0.05). We concluded that the addition of drug and alcohol use did not add to the descriptive power of this model within the current sample.
Discussion
This study examined psychosocial variables contributing to child-directed aggression reported by their caregivers and the characteristics of aggressive and abusive caregivers. We found support for a model of dysfunction in which negative affect and positive parenting account for the influence of parenting distress on child directed aggression. We found that adding drug and alcohol use as predictors resulted in a poorer fitting model. Relationships between the above variables and neglect were examined and only lower positive parenting scores were related to caregiver reported neglect. In addition to testing these structural equation models, we documented differences in parenting and drug use among caregivers engaging in any (vs. none) severe aggression. Implications of these findings for future assessment and intervention efforts are discussed below.
Demographic Associations
We found that demographic characteristics, with the exception of age, did not contribute to child directed aggression. Caucasian and minority (primarily Black or African American) individuals were comparable in their likelihood of engaging in child-directed aggression, reports of drug use, alcohol use, and neglect, and having an official report for child physical abuse. This finding is contrary to those finding a greater incidence of CPA among African Americans (Hawkins et al., 2010). Due to the smaller proportion of our sample with CPS records for child physical abuse, we may not have been able to detect a relationship between minority status and legal record. Still, minority status was unrelated to negative caregiving behaviors in this sample. Perhaps minority status may interact with broader contextual variables to contribute to abuse risk; for example, limited resources or experience of discrimination may contribute to negative affect, which may in turn lead to greater abuse risk.
Age was inversely associated with drug and alcohol use, minor assault, psychological aggression, inconsistent discipline, and corporal punishment and positively related to poor monitoring. Generally younger participants reported more child directed aggression, poorer parenting and drug and alcohol use, which could contribute to perpetration risk and are consistent with others’ findings (U.S. Department of Health and Human Services et al., 2013). The association between age and poor monitoring is somewhat surprising, but may reflect older participants having older children, who require less supervision. Caregiver age was correlated with child age (r = 0.41) supporting this conclusion. Findings suggest the need for stronger emphasis on early intervention and prevention efforts for younger caregivers.
Overlap Between Severe Aggression and CPS Physical Abuse
We found a substantial discrepancy between CPS records of physical abuse and caregiver endorsement of engaging in any severe child directed aggression. This finding suggests that a number of individuals engaging in severely aggressive acts towards children are not necessarily identified by CPS as abusive, and is consistent with Fallon and colleagues (2010) finding that only about a third of abuse cases are investigated by CPS. The discrepancy between caregiver report and official record also suggests that researchers and child service providers might need to probe for severely aggressive behaviors even when legal indicators of maltreatment are absent (see Kolko & Kolko, 2010).
Characteristics of Caregivers Engaging in Severe Aggression
Caregivers who did (vs. did not) report any severe aggression towards children reported poor parenting in general (i.e. less involvement and positive parenting, poorer child monitoring, less consistency in applying consequences, and more corporal punishment) and more drug use, consistent with the literature (Friesthler, 2011; Laslett et al., 2012; Oral et al., 2011; Thornberry et al., 2013; Wilson et al., 2008). Caregivers who use severe physical aggression may have fewer appropriate parenting options for effectively managing their children's behavior and resort to aggression as a means of exerting control. Higher drug use in relation to severe child directed aggression is interesting as a potential contributor from a mechanistic perspective. Given that substance abuse has a negative impact on executive control (Verdejo-Garcia, 2011), substance abusers may find it more difficult to inhibit aggressive behavior and engage in the cognitive strategies needed to regulate negative affect, leading to aggressive caregiving. More extensive examination of these relationships would be beneficial to conceptualizations of dysfunction and treatment.
Contrary to other recent findings (Stevens et al., 2015), we did not find differences in neglectful behavior between caregivers endorsing severe aggression and those who did not, suggesting that these behaviors may only co-occur under certain circumstances. For example, we found that positive parenting was inversely related to both neglect and caregiver aggression. It is possible that both neglectful and aggressive parents lack the skills needed to engage in adaptive parenting; however neglectful parents may avoid child related interactions to deal with this difficulty, whereas aggressive parents may try to exert control through aggression. More research is needed to refine our understanding of dysfunction underlying these harmful behaviors and identifying individuals for whom both difficulties may occur.
Characteristics of Caregivers with CPS Records of Physical Abuse
Unexpectedly, we did not find differences between caregivers with vs. without CPS records of physical abuse on any clinical variable (i.e. parenting, neglect, negative affect, parenting stress, or drug and alcohol use). Several possibilities could be responsible for the lack of association. First, the number of caregivers who had CPS records for child physical abuse within our sample was small (14.7%) and may not have constituted a large enough group to allow us to detect a difference. Second, the sample was recruited due to having some type of child abuse or child directed aggression, so they may have been more comparable clinically than different. Relatedly, we found considerable asynchrony between caregivers who had CPS records of physical abuse and those who reported engagement in severe aggression. While CPS records reflect an official indicator of threat to child safety and need for intervention, they may fail to identify a large number of caregivers who acknowledge severe aggression directed towards their children (Fallon et al., 2010).
Support for a Model of Dysfunction
In addition to examining differences associated with child directed aggression, our study contributes to understanding its underpinnings. Parenting stress, which has been associated with greater abuse risk (Black et al., 2001; Haskett et al., 2006; McPherson et al., 2008), was found to contribute to child directed aggression through negative affect and positive parenting. The inverse relationship between positive parenting and child directed aggression, and the positive relationship between negative affect and child directed aggression are consistent with the literature (Mammen et al., 2002; Mammen et al., 2000; Smith et al., 2014; Thornberry et al., 2013; Wilson et al., 2008). Our findings extend support for the view that caregivers who experience more parenting stress and more internalizing symptoms may be more likely to be physically aggressive or abusive to their children. Parents who experience more stress also tend to have fewer positive parenting interactions, providing another potential pathway contributing to child-directed aggression.
Many of these factors appear to map onto Gross and Thompson's (2007) model of emotion regulation, which has extensive links with affective neuroscience (Ochsner & Gross, 2005; Ochsner, Silvers & Buhle, 2012). Gross and Thompson's (2007) model posits that emotion regulation consists of selection/modification of situations, control of attention, cognitive reappraisal, and modulation of physiological, behavioral, and emotional response. Caregivers may experience more parenting stress due to a failure to adapt to and successfully modify caregiving situations leading to greater negative emotions. These individuals may then fail to modulate behavioral responding due to a more limited positive parenting behavior repertoire resulting in engagement in child directed aggression. Placing caregiver aggression with this framework may have heuristic benefits due to its integration of a wealth of affective neuroscience literature. Other theoretical conceptualizations of negative emotion in caregiver aggression tend to be narrower in their focus (on cognitive processes; Azar, Reitz & Goslin, 2008; Milner, 2003) and less connected to affective neuroscience (e.g. Belsky, 1993), limiting their ability to draw upon its rich literature and gain insight into mechanisms of dysfunction within physical abuse.
Examination of some of these variables informs our conceptualization of dysfunction within child directed aggression and can offer direction for future prevention and intervention efforts. Participants who indicate stress within the caregiver role may need to be assessed for heightened negative affect and positive parenting behavior to provide a measure of cumulative CPA risk. Developing interventions to better address these variables may be important. Alternatively, prophylactically targeting systems supporting adaptive emotion regulation and improved ability to cope with stress may also be beneficial. For example, exercise has been linked to decreased stress reactivity (Klaperski, von Dawans, Heinrichs & Fuchs, 2013) and has shown a beneficial effect on negative affect and stress among individuals with psychopathology (Vancampfort et al., 2011). It is possible that targeting exercise behavior would reduce vulnerability to negative parenting among at risk caregivers by reducing stress and affective dysfunction.
Implications for Future Prevention and Intervention Efforts
Current prevention efforts have focused on at home visitation of new parents, provision of psychoeducation, teaching parenting skills, and social support (Krugman, Lane, & Walsh, 2007; Olds et al., 2002). Empirical examinations have been limited, but offer some support for these approaches (Bugental, Lin, Ellerson, Rainey, & Kokotovic, 2010). Focusing on caregivers who appear at greater risk and present with modifiable risk factors (negative affect, stress, poorer parenting behavior, drug and alcohol use) may offer a means to maximize benefit obtained from limited public health resources through targeted screening and intervention deployment. Additionally, at-risk caregivers may benefit from individualized or targeted interventions that address cognitive, affective, and behavioral contributors child directed aggression, such as Alternatives for Families: A Cognitive Behavioral Treatment (AF-CBT; see Kolko, Simonich, & Loiterstein, 2014). AF-CBT targets several of these factors with both caregivers and children as it addresses both the risks for and clinical consequences of exposure to conflict and coercion in the family. Screening of individual risk factors in health care settings may also identify potential recipients of preventive or intervention services that can target their specific types of dysfunction. Exploration of prophylactic low cost interventions, such as psychoeducation on the potential benefits of exercise for stress and negative affect or bibliotherapy may offer additional avenues for decreasing maladaptive caregiving.
Limitations
Limitations of the current study should be considered when interpreting results. Although we obtained support for our model and contribute to conceptualization of mechanisms of dysfunction within child directed aggression, our study examines cross-sectional data and statements of mediation and causality cannot be as strong as those drawn from longitudinal datasets. However, the current study contributes to understanding child directed aggression and suggests that the cost and resources associated with examining relationships among these variables in a longitudinal examination would be worthwhile. Additionally, we drew upon a sample of clinically referred families who sought intervention for a range of family problems and varied in their level of engagement. This sample presents both a more ecologically valid group of caregivers (as will be seen within a real world clinic setting) and a more heterogeneous population. Readers should consider both the benefits of greater validity and potential for diversity within our group.
Conclusions & Future Directions
The current study contributes to characterizing aggressive caregivers and understanding of mechanisms potentially driving engagement in child directed aggression. We found that negative affect and positive parenting statistically mediated the relationship between parenting stress and child directed aggression. Additionally, we found that caregivers who engaged in any (vs. none) severe child directed aggression displayed poorer parenting behaviors and more drug use. Neglect appears to be underpinned by a distinguishable pathway and would benefit from further examination building a stronger conceptual and intervention framework (Dubowitz, 2007). Future longitudinal examinations of the contribution of parenting stress, negative affect, and positive parenting to child directed aggression would strengthen our understanding of their contribution to abusive behavior. Examinations of these variables and their interactions with other cognitive and affective variables (i.e. biases towards attention and perception of hostility, anger, and other emotion regulation strategies) would also be beneficial. Findings on poorer parenting behavior and drug use as variables characterizing parents who engage in severe child directed aggression suggest that these behaviors should be examined as potential factors identifying at risk caregivers. We hope that these results will inform the development of brief assessment and intervention protocols to address at risk families. For example, brief screenings of at risk caregivers could identify modifiable risk factors presented by those families and these could be targeted with evidence-based modules. Alternatively prophylactic treatments reducing vulnerability to poor caregiving behavior through supporting resilience and emotion regulation and providing psychoeducation on parenting may be beneficial. Intersections between child physical abuse and neglect need to be clarified and caregiver factors characterizing neglect further examined. We hope future researchers will continue to expand upon these areas and enrich understanding and strengthen treatment of this public health concern.
Acknowledgments
NIMH Funding: R01-MH074737-05, T32-MH018951-24
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Olga V. Berkout, University of Pittsburgh
David J. Kolko, University of Pittsburgh
References
- Abidin RR. Parenting stress index: Professional manual. 3rd ed. Psychological Assessment Resource; Odessa, FL: 1995. [Google Scholar]
- Azar ST, Reitz EB, Goslin MC. Mothering: Thinking is part of the job description: Application of cognitive views to understanding maladaptive parenting and doing intervention and prevention work. Journal of Applied Developmental Psychology. 2008;29:295–304. doi:10.1016/j.appdev.2008.04.009. [Google Scholar]
- Barnett D, Manly JT, Cicchetti D. Defining Child Maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, editors. Advances in Applied Developmental Psychology: Child Abuse, Child Development and Social Policy. Chapter 2. Ablex Publishing Corp.; Norwood, NJ: 1993. pp. 7–73. [Google Scholar]
- Belsky J. Etiology of child maltreatment: A developmental€cological analysis. Psychological Bulletin. 1993;114:413–434. doi: 10.1037/0033-2909.114.3.413. doi:10.1037/0033-2909.114.3.413. [DOI] [PubMed] [Google Scholar]
- Black DA, Heyman RE, Smith-Slep AM. Risk factors for child physical abuse. Aggression & Violent Behavior. 2001;6:121–188. doi:10.1016/S1359-1789(00)00021-5. [Google Scholar]
- Bugental DB, Lin EK, Ellerson PC, Rainey B, Kokotovic A. A cognitive approach to child abuse prevention. Psychology of Violence. 2010;1:84–106. doi: 10.1037//0893-3200.16.3.243. doi: 10.1037/2152-0828.1.S.84. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. BSI Brief Symptom Inventory: Administration, Scoring, and Procedure Manual. 4th Ed. National Computer Systems; Minneapolis, MN: 1993. [Google Scholar]
- Donovan JE. Young adult drinking-driving: Behavioral and psychosocial correlates. Journal of Studies on Alcohol. 1993;54:600–613. doi: 10.15288/jsa.1993.54.600. doi:10.15288/jsa.1993.54.600. [DOI] [PubMed] [Google Scholar]
- Dubowitz H. Understanding and addressing the “neglect of neglect:” Digging into the molehill. Child Abuse & Neglect. 2007;31:603–606. doi: 10.1016/j.chiabu.2007.04.002. doi:10.1016/j.chiabu.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Fallon B, Trocme N, Fluke J, MacLaurin B, Tonmyr L, Yuan YY. Methodological challenges in measuring child maltreatment. Child Abuse & Neglect. 2010;34:70–79. doi: 10.1016/j.chiabu.2009.08.008. doi:10.1016/j.chiabu.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Friesthler B. Alcohol use, drinking venue utilization, and child physical abuse: Results from a pilot study. Journal of Family Violence. 2011;26:185–193. doi: 10.1007/s10896-010-9352-2. doi:10.1007/s10896-010-9352-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Gruenewald PJ. Where the individual meets the ecological: A study of parent drinking patterns, alcohol outlets, and child physical abuse. Alcoholism: Clinical and Experimental Research. 2013;37:993–1000. doi: 10.1111/acer.12059. doi:10.1111/acer.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, Thompson RA. Emotion regulation: Conceptual foundations. In: Gross JJ, editor. Handbook of emotion regulation. Guilford Press; New York, NY: 2007. pp. 3–24. [Google Scholar]
- Hart H, Rubia K. Neuroimaging of child abuse: A critical review. Frontiers in Human Neuroscience. 2012;6:52. doi: 10.3389/fnhum.2012.00052. doi:10.3389/fnhum.2012.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the Parenting Stress Index-Short Form. Journal of Clinical Child & Adolescent Psychology. 2006;35:302–312. doi: 10.1207/s15374424jccp3502_14. doi:10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Hawkins AO, Danielson CK, de Arellano MA, Hanson RF, Ruggiero KJ, Smith DW. Ethnic/racial differences in the prevalence of injurious spanking and other child physical abuse in a national survey of adolescents. Child Maltreatment. 2010;15:242–249. doi: 10.1177/1077559510367938. doi:10.1177/1077559510367938. [DOI] [PubMed] [Google Scholar]
- Klaperski S, von Dawans B, Heinrichs M, Fuchs R. Does the level of physical exercise affect physiological and psychological responses to psychosocial stress in women? Psychology of Sport and Exercise. 2013;14:266–274. doi:10.1016/j.psychsport.2012.11.003. [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 3rd ed. Guilford Press; New York, NY: 2011. [Google Scholar]
- Kolko DJ, Kolko RP. Psychological impact and treatment of child physical abuse. In: Jenny C, editor. Child abuse and neglect: Diagnosis, treatment and evidence. Elsevier, Inc.; New York, NY: 2010. pp. 476–489. doi:10.1016/b978-1-4160-6393-3.00050-6. [Google Scholar]
- Kolko DJ, Simonich H, Loiterstein A. Timmer S, Urquiza A, editors. Alternatives for families: A Cognitive Behavioral Therapy: An overview and a case example. Evidence-Based Approaches for the Treatment of Maltreated Children. 2013:187–212. doi:10.1007/978-94-007-7404-9_11. [Google Scholar]
- Krugman SD, Lane WG, Walsh CM. Update on child abuse prevention. Current Opinion in Pediatrics. 2007;19:711–718. doi: 10.1097/MOP.0b013e3282f1c7e1. doi:10.1097/MOP.0b013e3282f1c7e1. [DOI] [PubMed] [Google Scholar]
- Laslett MA, Room R, Dietze P, Ferris J. Alcohol's involvement in recurrent child abuse and neglect cases. Addiction. 2012;107:1786–1793. doi: 10.1111/j.1360-0443.2012.03917.x. doi:10.1111/j.1360-0443.2012.03917.x. [DOI] [PubMed] [Google Scholar]
- Leeb RT, Lewis T, Zolotor AJ. A review of physical and mental health consequences of child abuse and neglect and implications for practice. American Journal of Lifestyle Medicine. 2011;5:454–468. doi:10.1177/1559827611410266. [Google Scholar]
- Lounds JJ, Borkowski JG, Whitman TL. Reliability and validity of the Mother-Child Neglect Scale. Child Maltreatment. 2004;9:371–381. doi: 10.1177/1077559504269536. doi: 10.1177/1077559504269536. [DOI] [PubMed] [Google Scholar]
- Manly JT, Cicchetti D, Barnett D. The impact of subtype, frequency, chronicity, and severity of child maltreatment on social competence and behavior problems. Development & Psychopathology. 1994;6:121–143. doi:10.1017/s0954579400005915. [Google Scholar]
- Mammen O, Pilkonis P, Kolko DJ. Anger and parent-to- child aggression in mood and anxiety disorders. Comprehensive Psychiatry. 2000;41:461–468. doi: 10.1053/comp.2000.16567. doi:10.1053/comp.2000.16567. [DOI] [PubMed] [Google Scholar]
- Mammen OK, Kolko DJ, Pilkonis PA. Negative affect and parental aggression in child physical abuse. Child Abuse & Neglect. 2002;26:407–424. doi: 10.1016/s0145-2134(02)00316-2. doi:10.1016/s0145-2134(02)00316-2. [DOI] [PubMed] [Google Scholar]
- McCrory E, De Brito SA, Viding E. The link between child abuse and psychopathology: A review of neurobiological and genetic research. Journal of the Royal Society of Medicine. 2012;105:151–156. doi: 10.1258/jrsm.2011.110222. doi:10.1258/jrsm.2011.110222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson AV, Lewis KM, Lynn AE, Haskett ME, Behrend TS. Predictors of parenting stress for abusive and nonabusive mothers. Journal of Child and Family Studies. 2008;18:61–69. doi:10.1007/s10826-008-9207-0. [Google Scholar]
- Milaniak I, Widom CS. Does child abuse and neglect increase risk for perpetration of violence inside and outside the home? Psychology of Violence. 2015;5:246–255. doi: 10.1037/a0037956. doi:10.1037/a0037956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner JS. Social information processing in high-risk and physically abusive parents. Child Abuse & Neglect. 2003;27:7–20. doi: 10.1016/s0145-2134(02)00506-9. doi:10.1016/s0145-2134(02)00506-9. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O'Brien R, Luckey DW, Pettitt LM, Henderson CR., Jr. Home visiting by paraprofessionals and by nurses: A randomized controlled trial. Pediatrics. 2002;110:486–496. doi: 10.1542/peds.110.3.486. doi:10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- Ochsner K, Gross J. The cognitive control of emotion. Trends in Cognitive Sciences. 2005;9:242–249. doi: 10.1016/j.tics.2005.03.010. doi:10.1016/j.tics.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences. 2012;1251:E1–E24. doi: 10.1111/j.1749-6632.2012.06751.x. doi:10.1111/j.1749-6632.2012.06751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oral R, Bayman L, Assad A, Wibbenmeyer L, Burhow J, Austin A, Bayman EO. Illicit drug exposure in patients evaluated for alleged child abuse and neglect. Pediatric Emergency Care. 2011;27:490–495. doi: 10.1097/PEC.0b013e31821d860f. doi: 10.1097/pec.0b013e31821d860f. [DOI] [PubMed] [Google Scholar]
- Park H, Walton-Moss B. Parenting style, parenting stress, and children's health-related behaviors. Journal of Developmental & Behavioral Pediatrics. 2012;33:495–503. doi: 10.1097/DBP.0b013e318258bdb8. doi:10.1097/dbp.0b013e318258bdb8. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wooten J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25:317–329. doi:10.1207/s15374424jccp2503_8. [Google Scholar]
- Smith AL, Cross D, Winkler J, Jovanovic T, Bradley B. Emotional dysregulation and negative affect mediate the relationship between maternal history of child maltreatment and maternal child abuse potential. Journal of Family Violence. 2014;29:483–494. doi:10.1007/s10896-014-9606-5. [Google Scholar]
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse & Neglect. 2007;31:517–530. doi: 10.1016/j.chiabu.2007.01.003. doi:10.1016/j.chiabu.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens KI, Schneiderman JU, Negriff S, Brinkmann A, Trickett PK. The whole picture: Child maltreatment experiences of youths who were physically abused. Child Abuse & Neglect. 2015;43:30–41. doi: 10.1016/j.chiabu.2014.12.006. doi:10.1016/j.chiabu.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltenborg M, Bakermans-Kraneburg MJ, Alink LRA, van IJzendoorn MH. The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review, Published online in Wiley Online Library. 2014 ( wileyonlinelibrary.com) doi: 10.1002/car.2353.
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. doi:10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Sugaya L, Hasin DS, Olfson M, Lin KH, Grant BF, Blanco C. Child physical abuse and adult mental health: A national study. Journal of Traumatic Stress. 2012;25:384–392. doi: 10.1002/jts.21719. doi:10.1002/jts.21719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Henry KL, Smith CA, Ireland TO, Greenman SJ, Lee RD. Breaking the cycle of maltreatment: The role of safe, stable, and nurturing relationships. Journal of Adolescent Health. 2013;53:S25–S31. doi: 10.1016/j.jadohealth.2013.04.019. doi:10.1016/j.jadohealth.2013.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children Youth and Families, & Children's Bureau Child Maltreatment 2012. 2013 doi:10.1037/e305872003-008. [Google Scholar]
- Vancampfort D, De Hert M, Knapen J, Wampers M, Demunter H, Deckx S, Probst M. State anxiety, psychological stress and positive well-being responses to yoga and aerobic exercise in people with schizophrenia: a pilot study. Disability and Rehabilitation. 2011;33:684–689. doi: 10.3109/09638288.2010.509458. doi:10.3109/09638288.2010.509458. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A. Novel therapies for cognitive dysfunction secondary to substance abuse. Psychiatric Times. 2011;28:46–48. [Google Scholar]
- Wilson SR, Rack JJ, Shi X, Norris AM. Comparing physically abusive, neglectful, and non-maltreating parents during interactions with their children: A meta-analysis of observational studies. Child Abuse & Neglect. 2008;32:897–911. doi: 10.1016/j.chiabu.2008.01.003. doi:10.1016/j.chiabu.2008.01.003. [DOI] [PubMed] [Google Scholar]