Abstract
Background
Histoplasma capsulatum comprises a worldwide complex of saprobiotic fungi mainly found in nitrogen/phosphate (often bird guano) enriched soils. The microconidia of Histoplasma species may be inhaled by mammalian hosts, and is followed by a rapid conversion to yeast that can persist in host tissues causing histoplasmosis, a deep pulmonary/systemic mycosis. Histoplasma capsulatum sensu lato is a complex of at least eight clades geographically distributed as follows: Australia, Netherlands, Eurasia, North American classes 1 and 2 (NAm 1 and NAm 2), Latin American groups A and B (LAm A and LAm B) and Africa. With the exception of the Eurasian cluster, those clades are considered phylogenetic species.
Methodology/Principal Findings
Increased Histoplasma sampling (n = 234) resulted in the revision of the phylogenetic distribution and population structure using 1,563 aligned nucleotides from four protein-coding regions. The LAm B clade appears to be divided into at least two highly supported clades, which are geographically restricted to either Colombia/Argentina or Brazil respectively. Moreover, a complex population genetic structure was identified within LAm A clade supporting multiple monophylogenetic species, which could be driven by rapid host or environmental adaptation (~0.5 MYA). We found two divergent clades, which include Latin American isolates (newly named as LAm A1 and LAm A2), harboring a cryptic cluster in association with bats.
Conclusions/Significance
At least six new phylogenetic species are proposed in the Histoplasma species complex supported by different phylogenetic and population genetics methods, comprising LAm A1, LAm A2, LAm B1, LAm B2, RJ and BAC-1 phylogenetic species. The genetic isolation of Histoplasma could be a result of differential dispersion potential of naturally infected bats and other mammals. In addition, the present study guides isolate selection for future population genomics and genome wide association studies in this important pathogen complex.
Author Summary
Histoplasmosis is a potentially severe fungal disease of mammals caused by Histoplasma capsulatum. The highest incidence of the disease is reported on the American continent, and approximately 30% of HIV and histoplasmosis co-infections are fatal. Previous studies have suggested at least 7 phylogenetic species within H. capsulatum, however by increasing taxon sampling and using different phylogenetic and population genetic methods, we detect at least 5 additional phylogenetic species within Latin America (LAm A1, LAm A2, LAm B1, LAm B2, RJ and BAC-1). These phylogenetic species are nested in the former LAm A clade. We found evidence that bats may be a cause of speciation in Histoplasma, as well-supported monophyletic clades were found in association with different species of bats. The radiation of the Latin American H. capsulatum species took a place around 5 million years ago, which is consistent with the radiation and diversification of bat species. Previous phylogenetic distribution of Histoplasma is upheld and strong support is indicated for the species delineation and evolution of this important pathogen.
Introduction
Histoplasma capsulatum sensu lato are dimorphic fungal species found in a filamentous form in the environment as saprobiotic-geophilic microorganisms [1]. These species encompass a globally distributed complex of fungi, which are mainly found in nitrogen/phosphate-enriched soils associated with bird and bat guano [2, 3]. In addition, moderate temperatures (18–28°C), constant humidity (>60%), and a low light environment characterize suitable ecological conditions for fungal growth [4, 5]. Histoplasma species in the saprobic mycelial phase at less than 35°C can produce asexual microconidia and macroconidia [6]. Microconidia, macroconidia or fragmented hyphal cells may be inhaled by various vertebrate species, including humans, and upon reaching the alveoli undergo a rapid conversion to yeast cells that can persist in host lungs and may disseminate to other tissues causing histoplasmosis [5]. The pathogenic yeasts are ovoid thick-walled cells that can be cultured in cysteine-enriched blood or brain-heart infusion media (BHI) at 37°C or in infected tissues [5]. In addition, Histoplasma utilize a heterothallic mating system where opposite mating type strains can complete the sexual cycle. Ascocarps are produced by hyphal constriction and coiling of opposite mating type cells thus forming the gymnothecia harboring meiospores [7].
Histoplasmosis was first reported by Samuel Darling in 1905–1906 in a patient from Martinique [8]. The spectrum of histoplasmosis varies from asymptomatic infection or mild illness to deep pulmonary and/or systemic mycosis. Severe clinical manifestations occur in less than 1% of patients [9–11]. Immunocompetent humans may acquire the disease tilling soil, visiting caves, building, cleaning old houses or bird roosting sites or even cutting down trees [12]. Among immuncompromised population with acquired cellular immunity impairment (HIV), the disease is responsible for high rates of morbidity and mortality [13]. In addition, with the increase of immunosuppressive therapy due to transplants and other chronic inflammatory disorders, disseminated histoplasmosis is becoming more frequent and is geographically expanding [14–16]. Autochthonous outbreaks of histoplasmosis have been reported in the latitudes 54° North and 38° South [17]. In patients with an impaired immune system, the disease is mostly fatal without an early diagnosis and proper treatment. For example, in Latin America about 30% of HIV infected people may die from histoplasmosis [4, 18].
Outbreaks are often reported with Histoplasma-contaminated soils, commonly in the presence of bat or bird guano. Birds are infected with H. capsulatum sporadically, however they could play role in its dispersal [19]. In endemic areas of histoplasmosis throughout the Americas, bats are often infected with this fungus [20, 21]. In addition to bats, the fungus has been detected in wild mammals such as non-human primates (e.g., baboons) [22, 23], mustelids (e.g., badgers and northern sea otter) [24–26], procyonids (e.g., raccoons) [27], as well as in domesticated animals such as equines [28, 29], felines [30, 31] and canines [32, 33]. This broad host range and tight association with vertebrates suggests that mammals play an important role in the speciation and dispersal mechanisms of this species complex.
Histoplasma capsulatum is a cosmopolitan fungus, and epidemiological knowledge has been improved by serology, culturing and molecular-based diagnostic methods [13, 34]. The endemicity of histoplasmosis varies from low (Europe and Oceania), to moderate (Africa and South Asia), to high (Americas) prevalence areas. The Midwestern and Southeastern regions of the United States, specifically the Ohio, St Lawrence and Mississippi river regions are considered highly endemic [11]. In Latin America, the high prevalence areas range from Uruguay to Mexico, mostly in countries with a moderate climate and constant humidity [4]. In Africa, two well-delimited areas are considered endemic—southern Africa, which includes South Africa, Tanzania and Zimbabwe, and western/central Africa [35]. In southern Asia, histoplasmosis is found in China, India and Thailand based on very few clinical reports; however, skin test surveys suggest that the fungus also occurs in Malaysia, Indonesia, Myanmar and the Philippines [36, 37]. Epidemiological surveys suggest that under-surveyed areas of the disease can have moderate to high levels of Histoplasma natural infections and the impact of the disease outside of the current known endemic regions should be investigated.
Based on phenotypic characteristics (host, morphology and pathogenicity), the genus Histoplasma was split into three varieties: H. capsulatum var. capsulatum, H. capsulatum var. duboisii and H. capsulatum var. farciminosum. The capsulatum var. is the most broadly dispersed, the lungs are the main compromised organs, and in isolated cases the phagocytic mononuclear system is involved in disseminated forms. The var. H. duboisii is restricted to tropical areas in Africa, causing cutaneous, subcutaneous and bone lesions and the var. farciminosum isolates are known to occur in Europe, Northern Africa, India and Southern Asia, commonly infecting horses and mules [5]. Advances in molecular genotyping methods have led to a closer investigation of H. capsulatum sensu stricto. Techniques such as Restriction Fragment Length Polymorphisms (RFLP), DNA hybridization, Random Amplified Polymorphic DNA (RAPD) and ITS1/2 sequencing all revealed high genetic diversity in Histoplasma, with some indication of geographical association [21]. Population structure based on molecular genotyping suggested different patterns of genetic variation among H. capsulatum populations, and that both recombination and clonal reproduction might occur [38]. Applying the genealogic concordance for phylogenetic species recognition (GCPSR) method [39, 40] for H. capsulatum sensu stricto using four partial coding loci in 137 isolates distributed across 25 countries, Kasuga and colleagues suggested at least 8 clades with 7 phylogenetic species: North America clade 1 (NAm 1), North America clade 2 (NAm 2), Latin America clade A (LAm A), Latin America clade B (LAm B), Australia, Netherlands, Eurasia, and Africa, where the Eurasian clade was not considered as a phylogenetic species by these authors [40]. This study improved our understanding of cryptic speciation and epidemiology for Histoplasma, however because of the ubiquitous worldwide distribution and broad host range, a complete understanding of the phylogenetic relationships of H. capsulatum sensu stricto is lacking. In addition, regional genetic diversity of this pathogen has been assessed, but a meta-analysis of these data has not been completed [41–44].
Therefore, we applied GCPSR and population genetic meta-analysis using four genetic markers across 234 globally-distributed taxa to better understand the phylogenetic structure of H. capsulatum sensu stricto [39]. Our main questions were: (i) What is the phylogenetic species distribution for H. capsulatum sensu stricto? (ii) Do GCPSR and population structure methods reveal similar patterns of species delineation in Histoplasma? (iii) Is there any evidence for host-derived speciation in H. capsulatum? (iv) Does recombination occur between and within populations, and is there evidence for introgression or gene flow between populations?
Methods
Phylogenetic and haplotype network analyses
Sequences of partial protein-coding loci used in this study were ADP-ribosylation factor (arf), H antigen precursor (H-anti), delta-9 fatty acid desaturase (ole1) and alpha-tubulin (tub1) from 234 isolates that were retrieved from GENBANK and TreeBASE and are listed in S1 Table. To increase sample size and phylogenetic signal we collected all Histoplasma isolate genome data that had at least one deposited sequence of the aforementioned studied loci. Recombining sites were removed from each individual gene alignment using RDP4 software, which could cause systematic errors in phylogenetic tree estimation [45]. For the final concatenated data set containing the four loci, missing sequences were treated as missing data for the final matrix totaling 234 taxa. Sequences were aligned using Muscle algorithm within MEGA 6.0 with default options [46]. Nucleotide substitution of best-fit model for each locus were statistically selected using jModelTest 2.0 [47]. Phylogenetic analyses were conducted by Bayesian Inference (BI) and Maximum Likelihood (ML) methods.
ML trees were inferred by fast and effective stochastic algorithm implemented in IQ-TREE v1.3.5 software [48]. Branch support was inferred by 1,000 non-parametric bootstrap pseudoreplicates [49]. BI was used to infer the phylogeny altogether as well divergence dating using BEAST v1.8.2 [50] based on conservative intervals of nucleotide substitutions rates and dates (0.00043–0.00656 subst/site/lineage/My; 0.0–15 mya) that encompass values obtained by Kasuga et al. [40] (0.0086–0.00432 s/s/l/My; 3.2–13.0 Ma). BI branch support was inferred by posterior probabilities [51]. The presence of saturation in the sequences was tested using DAMBE 5 [52] to infer if a strict molecular clock would be reasonable or whether a relaxed clock should be implemented. As this test did not detect saturation, we proceeded with the use of a strict molecular clock, using rate and date priors (parameters clock.rate and treeModel.rootHeight) for the ranges above. The runs were implemented under a coalescent framework, assuming the Extended Bayesian Skyline Plot [53] population model in which the effective population size is allowed to change throughout the tree time frame. Each run was performed twice for 100M generations (or longer in case of lack of convergence). Convergence of all runs (including the ones described below), parameter effective sample sizes (ESSs), burn-in determination, and 95% highest posterior densities (HPDs) of parameters were done in Tracer v1.6 [54]. Consolidation of run results was done in LogCombiner v1.8.2 [50], after removing the burn-in.
Haplotype networks were built using 202 strains through harboring sequences for each one of the four loci analyzed to visualize differences and diversity among Histoplasma worldwide populations. Thirty isolates were excluded from haplotype analysis due missing sequence information for at least one locus to avoid bias [55]. The haplotype distribution and diversity of the four analyzed loci were estimated using DnaSP v5 and used for input in Network 4.6.1.6 (fluxus-engineering.com). Gaps and missing data were excluded from the analysis. Median-joining networks [56] for each locus were obtained and visualized in Network 4.6.1.6.
Population structure in H. capsulatum
Genetic differentiation and neutrality tests between populations of H. capsulatum were calculated using Arlequin v. 3.11 [57]. Input haplotype files containing 202 taxa were generated using DnaSP v5, and ΦST was calculated. The statistical significance of phi-statistic was tested based on 1000 permutations using default settings. The effects of natural selection on molecular polymorphisms among the Histoplasma sequences was assessed using Tajima’s D [58] and Fu’s FS neutrality tests [59]. Population structure within Histoplasma was also assessed by SNP matrix calculated from the four analyzed loci with Bayesian Analysis of Population Structure (BAPS) 6.0 [60]. BAPS uses a Bayesian approach under an admixture model to infer the true number of natural populations in a single run [61, 62]. It differs from STRUCTURE [63] in methodology to address linked markers (as is the case for SNPs closely linked to one another in the same gene). It proceeds in two phases: first, it estimates K (inferred number of natural populations) under a no-admixture model; then, using these a priori populations, it estimates the probability (0.0–1.0) of each individual being from each of these K populations. We assumed a model in which individual SNPs from the same gene are considered linked but the four genes are assumed to be unlinked. Ten runs were performed for each of the two phases (no-admixture and admixture) and results automatically assembled into a single bar graph, where each bar represents an individual and colors represent the probability of it being assigned to a population. An output file is also generated reporting these individual probabilities for each individual.
Inference of the population tree was done in *Beast v1.8.2 assuming a species tree model, therefore assuming that each gene tree evolved within the actual species tree, but possibly having different topologies due to incomplete lineage sorting. Only individuals with P > = 0.95 of pertaining to a single population as inferred by BAPS in the previous step were included (for a total of 193 individuals included), therefore minimizing artifact branches in the species tree due to shared ancestry. The model for each of the genes was the same obtained by jModelTest previously to the ML search (see above). A birth-death model with incomplete sampling was chosen as the prior for the species tree topology, with rates (clock.rate) fixed at a relative rate of one. Two MCMC chains were used. Number of generations, assessment of convergence, and generation of the clade credibility tree followed the same steps previously described.
Results/Discussion
Worldwide distribution of Histoplasma
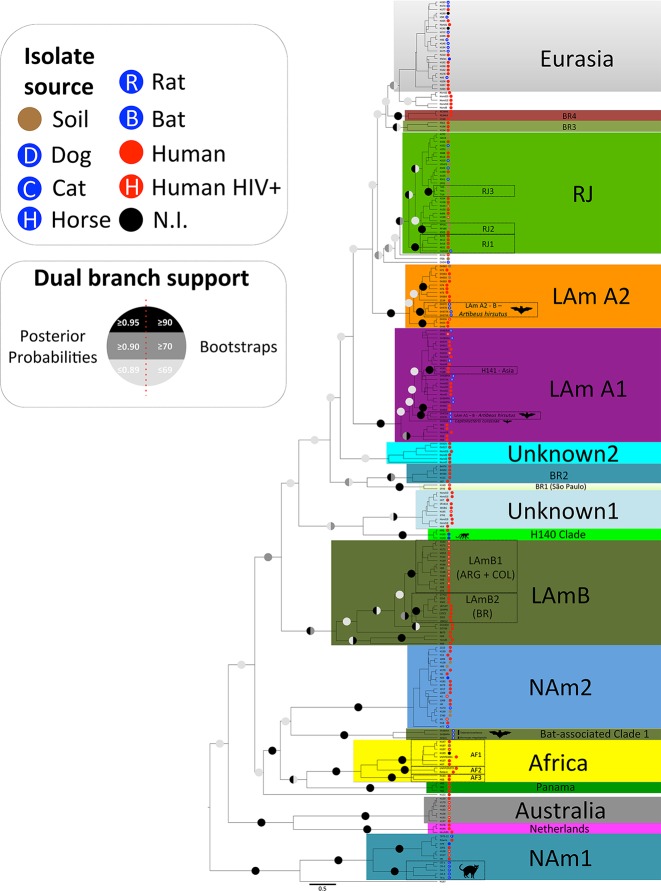
Our phylogenetic analysis of H. capsulatum sensu stricto revealed at least 17 cryptic phylogenetic species supported by bootstrap and posterior probabilities (Fig 1). The majority of novel phylogenetic species identified are nested within LAm A (LAm A1, LAm A2 and RJ) and LAm B (LAm B1 and LAm B2) species as proposed previously [40]. However the basal clades diagnosed by phylogenetic analyses display low bootstrap and posterior probability values, and the four analyzed loci did not resolve those branches (Fig 1). Low supported clades such as Unknown 1 and Unknown 2 harboring Latin American isolates as well the previously described Eurasia clade were also identified. Low-resolution branches could be explained by either rapid diversification of Histoplasma, or accelerated mutation rates in Central-South America. Alternatively, sampling of four loci and the numbers of representatives of each population were insufficient to resolve phylogenies.
Fig 1. Maximum Likelihood (ML) tree of Histoplasma capsulatum generated by IQ-TREE software for 232 taxa through 4 different loci (arf, ole1, tub and anti-H loci) reveals at least monophyletic braches as following: NAm 1, NAm 2, RJ, LAm B, NAm LAm A1, LAm A2, BR1-4, and Cluster 6 containing Netherlands, Panama, Africa, Australia and BAC1.
Dual branch support, inferred by non-parametric bootstrap for ML analysis, combined with posterior probabilities obtained for the BI analysis, was added to the branches. Monophyletic branches that were supported by two methods (Bootstrap≥70/Posterior Probabilities≥0.95) were designated high confidence clades. We also identified possible in-group variation that may be associated with specific niches. Low supported clades such as Eurasia, Unknown 1 and Unknown 2 were detected but do not follow our monophyletic branches supporting criteria.
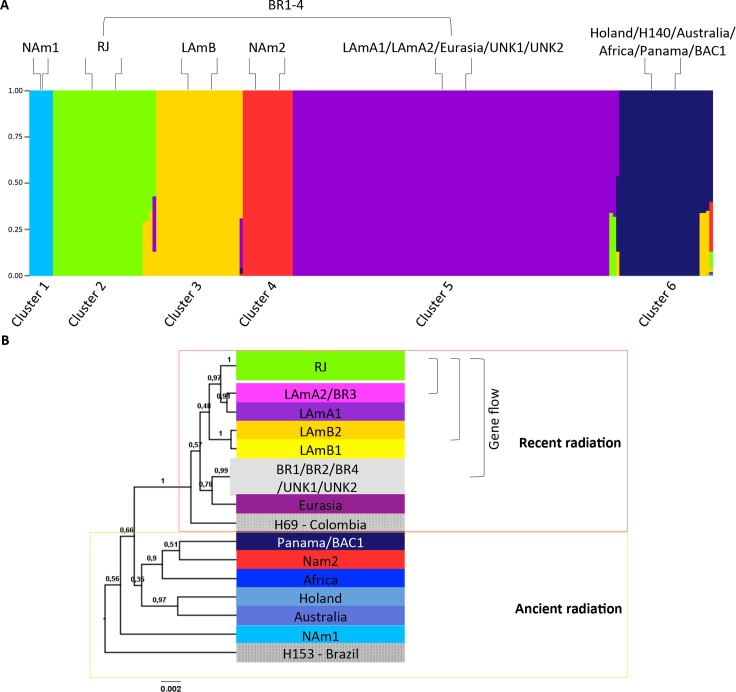
Admixture analysis inferred by Bayesian structuring methods reveals at least six populations as follows: Cluster 1 representing the phylogenetic species NAm 1, Cluster 2 representing the phylogenetic species RJ, Cluster 3 containing LAm B, Cluster 4 constituted by phylogenetic species NAm 2, Cluster 5 constituted by LAm A1, LAm A2, BR1-4, and the paraphyletic low supported clades Eurasia, Unknown 1 and Unknown 2, and Cluster 6 containing Netherlands, Panama, Africa, Australia and BAC1. To further explore the cryptic species of H. capsulatum sensu stricto, monophyletic branches and population structures were investigated individually to reconstruct the biogeographic history of this important pathogen.
North American Histoplasma capsulatum populations
Histoplasma capsulatum is endemic to North America, and mainly found in the central and eastern regions of the United States through Mississippi, St Lawrence and Ohio River valleys. Beyond humans, histoplasmosis is the second most common systemic fungal disease of cats in the USA [33]. About 60% to 90% of people who live in endemic areas in the US positively react to histoplasmin skin tests (HST) [64]. Among the elderly, the disease incidence varies from 3.4 to 6.1 cases per 100,000 individuals with highest rates in the Midwestern USA. Serological data show that the fungus naturally infects people in Canada, however rates are relatively low. The sensitivity reaction to HST ranges from 0 to 68% among tested Canadian populations, with higher prevalence of autochthonous infections in Ontario and Quebec provinces [65]. Recent expansion of autochthonous infections were detected in Montana [66] and an outbreak was reported in the Quebec province of Canada among employees from a demolition company [67]. Several outbreaks have been demonstrated in North America [68] and studies comparing genotypes of infectious strains are encouraged, as this could assist with predicting potential for infection. Despite the high incidence of this mycosis in North America little is known about the genetic background of the causative agents of histoplasmosis, relationships with different hosts, and variation in clinical presentation of the disease.
Based on phylogenetic and population structure analyses, three main species are found in the United States: NAm 1, NAm cat-associated and NAm 2 [40] (Fig 1). Those species are found to be monophyletic and supported by bootstrap and posterior probability values. In addition, those species have unique haplotype structures as revealed by Median-Joining vector analysis for each individual locus (S1 Fig). Interestingly, the NAm 1 and cat-associated species shared a single common ancestor, indicating that speciation could be driven by host-specific interactions. According to population structure using BAPS, both NAm 1 and NAm 2 phylogenetic species are distinct from Clusters 1 and 4, respectively (Fig 2). In addition, no admixture was found between these clusters in agreement with high FST values suggesting no gene flow between populations (S2 Table). The isolate 2134 from Texas and the isolate 2761 from Alabama grouped with the LAm A2 and unknown populations, respectively. This suggests that either those patients were infected in Central-South America, or those species are found in North America. No geographic differentiation between populations was observed, and both NAm 1 and NAm 2 species co-occur in the endemic areas of United States (S2 Fig). According to Tajima’s and Fu’s test of selective neutrality (Tajima’s D = -1.79268; p<0.05, and Fu’s Fs = -6.50886; p<0.02), NAm 2 populations may have expanded after a recent speciation (S3 Table). The haplotype diversity between NAm 1 and NAm 2 also indicates different population dynamics. We observe a complex haplotype network of the arf locus within NAm 2 while the NAm 1 isolates are nested in a single haplotype (S1 Fig). While NAm2 underwent a recent population expansion, NAm 1 may be subject to disruptive selection driven by different hosts (cat and human). Sexual reproduction has been demonstrated with North American strains of Histoplasma [7]. In addition, recombination and genetic exchange has been shown to occur [38]. Sexual reproduction allows fungal populations to adapt to adverse or novel conditions, which results in the emergence of novel and potentially more virulent genotypes that are able to infect to new hosts [69].
Fig 2. Population structure of Histoplasma capsulatum deduced by Bayesian Analysis of Population Structure (BAPS).
A) Structure plots of 205 isolates revealing 6 different major populations (Clusters 1–6). Phylogenetic species were assigned to each of the six deduced populations as follows: Cluster 1 representing the phylogenetic species NAm 1, Cluster 2 representing the phylogenetic species RJ, Cluster 3 containing LAm B, Cluster 4 constituted by phylogenetic species NAm 2, Cluster 5 constituted by LAm A1, LAm A2, BR1-4, and the paraphyletic low supported clades Eurasia, Unknown 1 and Unknown 2 and Cluster 6 containing Netherlands, Panama, Africa, Australia and BAC1. B) Bayesian population tree based on substructures of the 6 initial clusters deduced by BAPS. Gene flow is represented by mixture isolates that are annotated with brackets along the tree.
Latin America Histoplasma capsulatum populations
Histoplasma capsulatum isolates from Latin America contributed to the highest genetic diversity compared with other regions of the globe. In fact, South and Central America contributes to the majority of cases of histoplasmosis in the world [4, 18]. Although histoplasmosis is not a reportable disease, the elevated incidence of this mycosis among the HIV/AIDS population as well the reports of several outbreaks in immunocompetent patients suggests a high prevalence of this disease in Latin America [4, 18, 70, 71].
At least two populations are reported within Latin America: LAm A and LAm B [40]. Several reports have described distinct genetic clusters containing taxa from environmental and clinical samples from Brazil, various bat-associated samples from Mexico and clinical samples from Honduras [41–43]. However the fine-scale evolutionary relationships within and between the LAm A and LAm B have not been addressed. Phylogenetic and evolutionary analyses reveal complex genetic structure within the Latin American populations (Fig 1). The LAm B phylogenetic species comprises a single haplotype complex for ole1, tub1 and H-anti loci (S1 Fig). According to the Bayesian inference of the genetic structure in Histoplasma the LAm B clade comprises Cluster 3 using the admixture model (Fig 2A). However, phylogenetic analysis suggests genetic differentiation within this proposed phylogenetic species (Fig 1). The isolates from Argentina/Colombia (LAm B1) and Brazil (LAm B2 –Rio Grande do Sul and Espírito Santo states) are placed in two different monophyletic clades strongly supported by bootstrap and posterior probability values (Fig 1). Moreover, a refined population structure of Cluster 3 suggests the same split. According to Fig 2B, LAm B1 and LAm B2 are represented by a single population cluster. Admixtures between LAm B clades and within Cluster 5 were also observed (Fig 2B, S4 Table). In addition to those observations, LAm B populations exhibit excess of high-frequency variants, indicating balancing selection (Tajima’s D = -1.51512; p<0.05) suggesting population expansion (LAm B1 and LAm B2) after recent speciation (Fig 1, S3 Table). It is worth mentioning that the majority of LAm B1 isolates were isolated from HIV-infected patients (Fig 1).
The former LAm A clade exhibits greater genetic diversity and several phylogenetic species were revealed after inclusion of other Latin American isolates. The newly analyzed dataset revealed a large number of polytomic branches due to homoplastic characters, which suggests a rapid diversification within the former LAm A clade. We propose splitting the LAm A clade into at least 3 phylogenetic species (RJ, LAm A1 and LAm A2). Clades with low support such as Eurasia and Unknown2 were placed within the former LAm A clade (Fig 1). Two phylogenetic species represented by Central America and Colombia isolates were proposed: LAm A1 and LAm A2 (Fig 1). The phylogenetic species LAm A1 and LAm A2 are composed of isolates obtained in Mexico, Guatemala, Honduras, Panama and Colombia (S1 Table). Haplotype networks also support both phylogenetic species, especially for the tub locus where both are separated in haplotypes clusters (S1 Fig). Within LAm A1 the Colombian strains clustered in a cryptic monophyletic branch (LAm A1) along with a single Honduran strain indicating intraspecific genetic isolation (Fig 1). In addition, a cryptic branch (H141 clade) harboring the isolates H141 (Indonesia) and H188 (Panama) was also inferred. According to Tajima’s and Fu’s test of selective neutrality, LAm A1 (Tajima’s D = -2.18568; p<0.05 and Fu’s Fs = -13.08523; p<0.02) and LAm A2 (Tajima’s D = -1.74401; p<0.05 and Fu’s Fs = -2.13715; p<0.02) populations exhibit excess of high-frequency variants, from a large haplotype (Tajima’s D = -1.79268; p<0.05 and Fu’s Fs = -6.50886; p<0.02) suggesting population expansion after a recent speciation from the basal former LAm A clade (S3 Table). Interestingly, some monophyletic clusters were found among the Latin American phylogenetic species, which supports population expansion (Fig 1).
Within the LAm A clade we detected a single monophyletic lineage of both environmental and clinical isolates collected in Rio de Janeiro and São Paulo state of Brazil, indicating geographic isolation (Fig 1). This cryptic species was designated RJ and is supported by both bootstrap and posterior probability values (Fig 1). In addition, the RJ clade is represented by a single haplotype complex in the H-anti and tub1 loci supporting the proposition of a cryptic species within the H. capsulatum sensu lato (S1 Fig). Moreover, the RJ isolates composed a unique population as revealed by Bayesian analysis and grouped in Cluster 2 (Fig 2B). Interestingly, both soil and clinical isolates cluster together, corroborating soil as the source of infection (Fig 1). A number of supported monophyletic branches within RJ phylogenetic species are in agreement with population diversity under neutrality, since both Tajima’s D and Fu’s Fs test indicated negative values, however not statistically significant, which indicates sequences are evolving randomly (-1.3065; p = 0.076 and -6.51844; p = 0.031 respectively; S3 Table).
Other monophyletic lineages were found within Brazilian isolates. There are four different monophyletic lineages (BR1-4) harboring isolates from Brazil that are supported by both bootstrap and posterior probability values found along the tree and are also supported by single haplotypes (Fig 1, S1 Fig). The BR1 clade is composed by two isolates (SP49 and H149) from São Paulo state in Brazil. The BR2 clade is composed by three isolates from Rio de Janeiro (84476, 84502 and 84564); one from São Paulo state (H151) and one from Ceará state in Brazil (JIEF) represented by single haplotypes in the H-anti and tub1 loci. The BR3 clade is formed by an isolate from Rio de Janeiro (H196), São Paulo (H154) and Espírito Santo (ES62) and is also supported by a single haplotype within the tub1 locus. Finally, the BR4 clade harbors three isolates: two from Pernambuco state (RE5646 and RE9463) and another one from Brazil but without identification (H146) and supported by a single haplotype within the H-anti locus (Fig 1). Because of a small sample size, the neutrality tests did not indicate a significant effect (S3 Table). According to population structure analysis, isolates from the BR1-4 clades are admixtures between Cluster 5 and Cluster 2, suggesting that these groups are freely recombining (Fig 2, S4 Table). However, population structure analysis suggests admixtures between Cluster 5 and Cluster 2, suggesting gene flow within the former LAm A clade (S4 Table). In order to avoid misleading taxonomic classification we do not rank the BR1-4 clades as phylogenetic species due to potential recent hybridization within the well-supported Latin American phylogenetic species (Fig 1, S1 Fig). The Panama clade was also identified to be strongly monophyletic, supported and represented by an unique haplotype in the current analysis (Fig 1, S1 Fig) and no structural genetic differences within this clade were found even with additional Latin American strains [40]. Moreover the isolate EH315 from the BAC1 clade appears to be result of a hybridization event between Cluster 6 and Cluster 4 indicating that introgression may occur within this genus, allowing the emergence of new genotypes (Fig 2, S4 Table).
Non-American Histoplasma capsulatum populations
On the African continent, histoplasmosis was first described in 1952 by Dubois and colleagues [72] and is also known as histoplasmosis duboisii, or African histoplasmosis caused by Histoplasma duboisii. The disease is prevalent in the tropical belt of Africa, more specifically in the western and central areas of the sub-Saharan, as well as Madagascar. About 300 histoplasmosis cases were reported up to 2007, mostly due the increase of the HIV-infected population, as well as antiretroviral therapy [35]. Imported cases of African histoplasmosis have been diagnosed in Europe [73]. Due to inefficiency and inaccuracy of diagnosis of deep mycosis in these areas, those numbers are likely to be an underestimate.
Histoplasmosis is reported frequently in horses throughout the African continent, but associated with H. capsulatum var. farciminosum [28, 29]. However, an analysis of equine cases revealed that the disease could be caused by other varieties of Histoplasma [40]. In addition, the former classification of H. capsulatum var. duboisii based on occurrence in Africa was determined to be obsolete, due to the fact that the H. capsulatum var. duboisii and H. capsulatum var. capsulatum phenotypic variants co-occur within Africa [40].
Previous phylogenetic analysis of African strains (H. capsulatum var. duboisii and H. capsulatum var. capsulatum) with the addition of three new genotyped isolates revealed a different genetic structure than previously demonstrated [40, 74]. Three groups (AF1-3) within Africa species were detected, which contained highly supported branches and single haplotypes (Fig 1, S1 Fig). Structure analysis places the Africa species within the Cluster 6 (Fig 2A). However, a more detailed analysis of Cluster 6 revealed that African isolates are represented by a unique genotype (phylogeny and haplotypes) but no interspecies differentiation was observed in the BAPS analysis (Fig 2B). Neutrality tests suggest that the African population of Histoplasma is under a balancing selection or has undergone a recent bottleneck or effective population size decrease (D>0 and Fs>0), however they are not statically significant (S3 Table). Despite analyzing few sequences, a potential population bottleneck was observed in the African clade. We suggest that the African continent could harbor more Histoplasma species and disease burden than reported.
The Eurasian clade contains isolates from North Africa (Egypt), Europe (England, German and Poland) and Asia (Thailand, China and India). A monophyletic clade was observed with the same isolate compositions previously reported, however with low bootstrap support [40] (Fig 1). Also, the Eurasian clade is represented by a single group within Cluster 5 (Fig 2). Of note is that almost all equine Histoplasma isolates cluster within the Eurasian clade, which may suggest susceptibility of horses to a particular genotype of Histoplasma (Fig 1). The Netherlands and Australia phylogenetic species remain unaltered as no additional isolates were added. Both species are monophyletic and are represented by single haplotypes (Fig 1, S1 Fig). However, an intrapopulation analysis revealed that these two species compose a single cluster, cluster 6 (Fig 2B). Histoplasmosis should be further explored in Europe, Africa and Asia, especially with the increase of HIV cases. Serological surveys and PCR-based methods revealed the prevalence of the fungus in Asia with new potential regions of Histoplasma exposure [75, 76]. Also new cases and emergent genotypes have been recently identified in non-HIV patients from China [77]. Recently, disseminated histoplasmosis was diagnosed in a non-HIV patient from Sweden, which is considered a non-endemic region [78]. Our main conclusion from this limited sampling is that H. capsulatum is more widespread in non-endemic regions than previously thought [34, 37, 79], and thus more effort to understand both the ecology and distribution in these regions is warranted.
Bat/bird flight’s potential role in Histoplasma speciation and global distribution
Beyond the Americas, Histoplasma is endemic to Africa, Asia, Europe and Oceania, however at a lower incidence based on reported cases [34, 35, 37, 80]. Among the Onygenalean mycoses, histoplasmosis caused by H. capsulatum sensu lato is rather unique. This species is found on 5 continents, and exhibits higher genetic variation when compared to Coccidioides, Blastomyces and Paracoccidioides [81]. Histoplasma has a worldwide distribution while Paracoccidioides, Coccidioides, and Blastomyces have limited geographic distribution [81, 82]. Similar to Emmonsia species that also cause systemic infections outside the Americas [83], Histoplasma is found on all continents, and therefore it is reasonable to hypothesize a mechanism of long-range dispersal.
One of the important questions concerning the evolution of Histoplasma species remains unanswered: Why does Histoplasma have a worldwide distribution compared to its close ajellomycetacean relatives? Some ecological features may reveal dispersion mechanisms of this pathogen. First, Histoplasma is found and grows in nitrogen/phosphate (bird and bat guano) enriched soils and environments, which selects against other microorganisms [2, 3]. Second, Histoplasma can naturally infect avian and chiropteran species, and disseminated disease is reported in those organisms [19, 84]. Third, some avian and chiropteran species are long-range migratory reservoirs, aiding in the dispersal of this microorganism [85].
Histoplasma is recurrently isolated from bats in endemic areas of histoplasmosis [42, 86]. The fungus was isolated from internal organs as well as in bat guano-enriched soils [42, 43]. Other closely related human fungal pathogens such as Coccidioides posadasii [87], Blastomyces dermatitidis [88], and Paracoccidioides brasiliensis [89] have been isolated only sporadically from bats. Bats are widely distributed across many continents and ecosystems, being one of the largest groups of mammals, second in number of species after the order Rodentia and first in number of individuals [90]. Bats live in caves, abandoned or occupied buildings, mines, plant crowns, bark, or rocks, which in association with humidity and guano enriched microenvironment favors the development of Histoplasma [86]. Some significant bat-associated clades were reported in our phylogenetic analysis, which reinforces that bats may drive speciation and aid in dispersal. Within the LAm A1 and LAm A2, two supported clades containing bat-derived Histoplasma strains were identified (Fig 1). Because of its guano-growth ability in sheltered habitats, Histoplasma likely may have a focal distribution, with habitats that can be widely separated from each other.
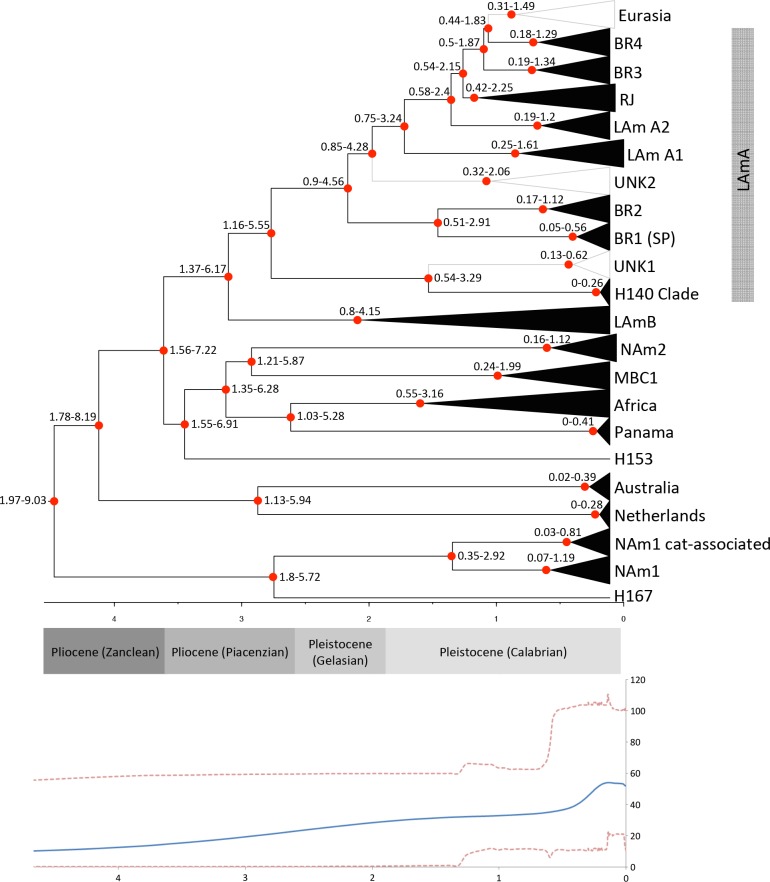
The LAm A1 bat-associated clade is composed of the strains EH375 and EH376 while the LAm A2 bat-associated is harbors the isolates EH372, EH373, EH377 and EH378. Both clades contain isolates recovered from Artibeus hirsutus (i.e., hairy fruit-eating) from Morelos-Mexico, indicating that bats could play an important role in the Histoplasma speciation and dispersion [42]. This is in agreement with population expansion revealed by neutrality tests performed within LAm A1 and LAm A2 populations. In addition, we designate a bat-associated species-specific clade (BAC1) harboring Histoplasma genotypes (EH384I and EH384P isolates) associated with the long-migratory bat species Tadarida brasiliensis as well as with Mormoops megalophylla (EH315 isolate) (Fig 1). This cryptic species harbors the isolates EH315, EH384I and EH384P as previously suggested by Taylor et al. [41, 42] and no human clinical isolates were placed within this clade so far. Recently, the addition of 6 new Histoplasma strains isolated from T. brasiliensis reinforced the proposition of a new phylogenetic species (Vite-Garín submitted). Bats originated in the early Eocene (52–50 Mya) coincident with the global temperature rise [91] and as well with the origin of ancestral Histoplasma [92], however the diversification of the Histoplasma-associated bats species such as the Artibeus genus occurred more recently. The radiation of Artibeus genus is estimated to have initiated around 13.2 Mya (19.9–8.8 Mya) in the Miocene, splitting into Artibeus and Dermadura clades followed by diversification [93]. This is in agreement with the subsequent radiation of the Histoplama capsulatum complex (Fig 3) around 1.97–9.03 Mya. Bats represent an interesting model to understand the dispersal of Histoplasma and its ability to infect humans; however, the mechanisms are still unknown. Interestingly, several studies indicate that bat mitochondrial physiology has evolved to tolerate oxidative stress incurred during high metabolic flights, possibly allowing tolerance to intracellular parasitism [94]. These results strongly suggest that Histoplasma could co-evolve with its most frequently associated host.
Fig 3. Extended Bayesian Skyline Plot (EBSP) of Histoplasma capsulatum sensu lato.
EBSPs represents population size changes over time and divergence dating was inferred using BEAST v1.8.2 based on conservative intervals of nucleotide substitutions rates and dates (0.00043–0.00656 subst/site/lineage/My; 0.0–15 Ma) that encompass values obtained by Kasuga et al. [40]. Y-axes are effective population size divided by generation time. X-axes are in millions of years. Confidence intervals of each dated phylogenetic species were added to the nodes.
Geological history of Histoplasma
The demographic history of Histoplasma was assessed by Extended Bayesian Skyline Plot (EBSP) analyses using relaxed molecular clock models for Bayesian inferences. Convergence of the Beast runs, ESSs, and “burn-ins” were >200 for all parameters. According to EBSP analyses and relaxed molecular clock models for Bayesian inferences, the radiation of H. capsulatum sensu stricto took place between 1.97 to 9.03 Mya during the Neocene period, more specifically from the late Miocene through the Pleistocene epochs (Fig 3). The fact that the highest genetic diversity was found in Latin America, as well as ancestral branches/lineages such as H167 and H153, strongly suggests that the center of dispersion of Histoplasma was in fact South/Central America (Figs 1 and 2, [40]). In addition, the EBSP tree clearly shows that diversification of Histoplasma occurred about 0.5 Mya during the Pleistocene epoch. According to population tree, two main events of radiation took place during Histoplasma evolution. The first radiation event is clearly observed in the “old world” and probably originated from the basal H153 genotype as well as the NAm 1, NAm 2, Africa, Netherlands, Australia and Panama/BAC1 species (Fig 2). It is important to note that this speciation took place between 1.97–9.03 Mya, and these new populations remained stable as revealed by long branch lengths and low diversity (Figs 2 and 3), except for the North American clades which originated more recently and harbor a higher genetic diversity (S3 Table). There are two main possibilities for the long-range Histoplasma colonization: intercontinental macro/microconidia migration via air dispersal or by long-range migratory animals. Histoplasma can survive passage through the digestive tract of bats [94–96] and some avian species [3, 19, 84]. The second radiation of Histoplasma took place more recently (1.37–6.17 Mya). The short branches associated with the new emerging lineages, high genetic diversity, population expansion (deduced by neutrality tests), and high rates of recombination within and between groups are in agreement with the emergence of new Latin American genotypes (Figs 1–3). This recent radiation took place in Latin America and appears to be a constant process that according to the EBSP analysis occurred about 0.5 Mya (Fig 3). Those genotypes could be associated with more virulent/pathogenic variants that could reflect in different disease phenotypes. Recently, studies of host-pathogen interactions using a small set of Histoplasma isolates (NAm1, NAm2, Panama and LAm A species) revealed significant differences in fungal burden, disease kinetics, disease symptoms, and cytokine response [97, 98].
Summarizing, based on the concordance between GCPSR and population structures methods, six new phylogenetic species are proposed: RJ, LAm B1, LAm B2, LAm A1, LAm A2, BAC1 (Figs 1 and 2). The clades Eurasia, BR1-4, Unknown 1 and Unknown 2 were not concordant among the three addressed methods and gene flow was found between these isolates and the RJ, LAm B1, LAm B2, LAm A1 and LAm A2 phylogenetic species. Many processes, such as incomplete lineage sorting, horizontal gene transfer, gene/genome duplication, recombination and hybridization can all create incongruities within closely related organisms [99, 100]. In order to resolve those incongruences, a whole genome sequencing approach to define and evaluate a broader number of SNPs across the Histoplasma population is suggested. Strong evidence of host-derived speciation and radiation in Histoplasma species was found. The radiation of both Histoplasma and its more frequently associated bat host, A. hirsutus, took place in similar geographical areas (Fig 3). Moreover, well-supported clades of bat-associated isolates were detected, reinforcing the hypothesis that bats may play an important role in diversification and dispersion of Histoplasma capsulatum.
Assessing pathogen genotypes will provide the foundation to understand the variable clinical manifestations of this important fungal disease. For example, are there specific Histoplasma genotypes responsible for outbreaks or severe clinical cases in immunocompetent humans? Are there isolates with differential sporulation, expression of virulence factors, or tolerance to extreme nitrogen/phosphate enriched soils? Does speciation affect the sequence or expression of any reported virulence genes in Histoplasma such as hsp60/82, yps3, ryp1/2, cbp1 or ags1 [101, 102]? Further studies to explore the genetic diversity of Histoplasma and correlate genotype with medically important phenotypes via population genomics and genome wide association studies [103] will help provide answers to the above questions.
Supporting Information
Diagrams were inferred through haplotypes from 4 different loci as follows: arf, ole1, tub1 and H-anti. Circles are proportional to haplotype frequency and numbers of haplotype (h) and Haplotype Diversity index are shown. Black dots represent a single mutation and red dots represent median-joining vectors.
(PDF)
Epidemiological map was obtained at the Centers for Disease Control and Prevention (CDC) web site: www.cdc.gov/fungal/diseases/histoplasmosis/causes.html.
(PDF)
(XLSX)
(XLS)
(XLSX)
(XLS)
Acknowledgments
We are thankful to John W. Taylor from the Department of Plant and Microbial Biology, University of California, Berkeley-CA, USA, for his critical suggestion throughout the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by Fundação de Amparo a Pesquisa do Distrito Federal/Conselho Nacional de Desenvolvimento Cientifico (FAP-DF/CNPq/Pronex 193000569/2009) and National Institute of Health/ National Institute of Allergy and Infectious Diseases (NIH/NIAID K22 AI104801). RMZO was supported in part by CNPq [304976/2013-0] and FAPERJ [E-26/103.157/2011]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Menges RW, Furcolow ML, Selby LA, Habermann RT, Smith CD. Ecologic studies of histoplasmosis. American journal of epidemiology. 1967;85(1):108–19. Epub 1967/01/01. . [DOI] [PubMed] [Google Scholar]
- 2.Lockwood GF, Garrison RG. The possibel role of uric acid in the ecology of Histoplasma capsulatum. Mycopathologia et mycologia applicata. 1968;35(3):377–88. Epub 1968/10/14. . [DOI] [PubMed] [Google Scholar]
- 3.Ajello L. Relationship of Histoplasma Capsulatum to Avian Habitats. Public health reports. 1964;79:266–70. Epub 1964/03/01. [PMC free article] [PubMed] [Google Scholar]
- 4.Negroni R. [Histoplasmosis in Latin America]. Biomedica: revista del Instituto Nacional de Salud. 2011;31(3):304 Epub 2012/08/02. . [PubMed] [Google Scholar]
- 5.Kwon-Chung KJ, Bennett JE. Medical Mycology. Philadelphia: Lea & Febiger; 1992. [Google Scholar]
- 6.Maresca B, Kobayashi GS. Dimorphism in Histoplasma capsulatum: a model for the study of cell differentiation in pathogenic fungi. Microbiological reviews. 1989;53(2):186–209. Epub 1989/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwon-Chung KJ. Emmonsiella capsulata: perfect state of Histoplasma capsulatum. Science. 1972;177(4046):368–9. Epub 1972/07/28. . [DOI] [PubMed] [Google Scholar]
- 8.Darling ST. The Morphology of the Parasite (Histoplasma Capsulatum) and the Lesions of Histoplasmosis, a Fatal Disease of Tropical America. The Journal of experimental medicine. 1909;11(4):515–31. Epub 1909/07/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wheat LJ, Kauffman CA. Histoplasmosis. Infectious disease clinics of North America. 2003;17(1):1–19, vii. Epub 2003/05/20. . [DOI] [PubMed] [Google Scholar]
- 10.Goodwin RA, Loyd JE, Des Prez RM. Histoplasmosis in normal hosts. Medicine. 1981;60(4):231–66. Epub 1981/07/01. . [DOI] [PubMed] [Google Scholar]
- 11.Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clinical microbiology reviews. 2007;20(1):115–32. Epub 2007/01/16. 10.1128/CMR.00027-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faiolla RC, Coelho MC, Santana Rde C, Martinez R. Histoplasmosis in immunocompetent individuals living in an endemic area in the Brazilian Southeast. Revista da Sociedade Brasileira de Medicina Tropical. 2013;46(4):461–5. Epub 2013/08/29. 10.1590/0037-8682-0124-2013 . [DOI] [PubMed] [Google Scholar]
- 13.Adenis A, Nacher M, Hanf M, Vantilcke V, Boukhari R, Blachet D, et al. HIV-associated histoplasmosis early mortality and incidence trends: from neglect to priority. PLoS neglected tropical diseases. 2014;8(8):e3100 Epub 2014/08/22. 10.1371/journal.pntd.0003100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nacher M, Adenis A, Mc Donald S, Do Socorro Mendonca Gomes M, Singh S, Lopes Lima I, et al. Disseminated histoplasmosis in HIV-infected patients in South America: a neglected killer continues on its rampage. PLoS neglected tropical diseases. 2013;7(11):e2319 Epub 2013/11/28. 10.1371/journal.pntd.0002319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gugnani HC, Denning DW. Burden of serious fungal infections in the Dominican Republic. Journal of infection and public health. 2015. Epub 2015/06/02. 10.1016/j.jiph.2015.04.026 . [DOI] [PubMed] [Google Scholar]
- 16.Putot A, Perrin S, Jolivet A, Vantilcke V. HIV-associated disseminated histoplasmosis in western French Guiana, 2002–2012. Mycoses. 2015;58(3):160–6. Epub 2015/02/03. 10.1111/myc.12293 . [DOI] [PubMed] [Google Scholar]
- 17.Anderson H, Honish L, Taylor G, Johnson M, Tovstiuk C, Fanning A, et al. Histoplasmosis cluster, golf course, Canada. Emerg Infect Dis. 2006;12(1):163–5. 10.3201/eid1201.051083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez BL. Histoplasmosis: Epidemiology in Latin America. Current fungal infection reports. 2011;5(4):6. [Google Scholar]
- 19.Quist EM, Belcher C, Levine G, Johnson M, Heatley JJ, Kiupel M, et al. Disseminated histoplasmosis with concurrent oral candidiasis in an Eclectus parrot (Eclectus roratus). Avian pathology: journal of the WVPA. 2011;40(2):207–11. Epub 2011/04/19. 10.1080/03079457.2011.554796 . [DOI] [PubMed] [Google Scholar]
- 20.Taylor ML, Chavez-Tapia CB, Vargas-Yanez R, Rodriguez-Arellanes G, Pena-Sandoval GR, Toriello C, et al. Environmental conditions favoring bat infection with Histoplasma capsulatum in Mexican shelters. The American journal of tropical medicine and hygiene. 1999;61(6):914–9. Epub 2000/02/16. . [DOI] [PubMed] [Google Scholar]
- 21.Vite-Garin T, Estrada-Barcenas DA, Cifuentes J, Taylor ML. The importance of molecular analyses for understanding the genetic diversity of Histoplasma capsulatum: an overview. Revista iberoamericana de micologia. 2014;31(1):11–5. Epub 2013/11/21. 10.1016/j.riam.2013.09.013 . [DOI] [PubMed] [Google Scholar]
- 22.Walker J, Spooner ET. Natural infection of the African baboon Papio papio with the large-cell form of Histoplasma. The Journal of pathology and bacteriology. 1960;80:436–8. Epub 1960/10/01. . [PubMed] [Google Scholar]
- 23.Butler TM, Gleiser CA, Bernal JC, Ajello L. Case of disseminated African histoplasmosis in a baboon. Journal of medical primatology. 1988;17(3):153–61. Epub 1988/01/01. . [PubMed] [Google Scholar]
- 24.Burek-Huntington KA, Gill V, Bradway DS. Locally acquired disseminated histoplasmosis in a northern sea otter (Enhydra lutris kenyoni) in Alaska, USA. J Wildl Dis. 2014;50(2):389–92. 10.7589/2013-11-288 . [DOI] [PubMed] [Google Scholar]
- 25.Jensen HE, Bloch B, Henriksen P, Dietz HH, Schonheyder H, Kaufman L. Disseminated histoplasmosis in a badger (Meles meles) in Denmark. APMIS. 1992;100(7):586–92. . [DOI] [PubMed] [Google Scholar]
- 26.Eisenberg T, Seeger H, Kasuga T, Eskens U, Sauerwald C, Kaim U. Detection and characterization of Histoplasma capsulatum in a German badger (Meles meles) by ITS sequencing and multilocus sequencing analysis. Med Mycol. 2013;51(4):337–44. 10.3109/13693786.2012.723831 . [DOI] [PubMed] [Google Scholar]
- 27.Clothier KA, Villanueva M, Torain A, Reinl S, Barr B. Disseminated histoplasmosis in two juvenile raccoons (Procyon lotor) from a nonendemic region of the United States. J Vet Diagn Invest. 2014;26(2):297–301. 10.1177/1040638714521207 . [DOI] [PubMed] [Google Scholar]
- 28.Gabal MA, Hassan FK, Siad AA, Karim KA. Study of equine histoplasmosis farciminosi and characterization of Histoplasma farciminosum. Sabouraudia. 1983;21(2):121–7. Epub 1983/06/01. . [DOI] [PubMed] [Google Scholar]
- 29.Selim SA, Soliman R, Osman K, Padhye AA, Ajello L. Studies on histoplasmosis farciminosi (epizootic lymphangitis) in Egypt. Isolation of Histoplasma farciminosum from cases of histoplasmosis farciminosi in horses and its morphological characteristics. European journal of epidemiology. 1985;1(2):84–9. Epub 1985/06/01. . [DOI] [PubMed] [Google Scholar]
- 30.Fischer NM, Favrot C, Monod M, Grest P, Rech K, Wilhelm S. A case in Europe of feline histoplasmosis apparently limited to the skin. Veterinary dermatology. 2013;24(6):635–8, e158. Epub 2013/10/15. 10.1111/vde.12077 . [DOI] [PubMed] [Google Scholar]
- 31.Arunmozhi Balajee S, Hurst SF, Chang LS, Miles M, Beeler E, Hale C, et al. Multilocus sequence typing of Histoplasma capsulatum in formalin-fixed paraffin-embedded tissues from cats living in non-endemic regions reveals a new phylogenetic clade. Medical mycology: official publication of the International Society for Human and Animal Mycology. 2013;51(4):345–51. Epub 2012/10/18. 10.3109/13693786.2012.733430 . [DOI] [PubMed] [Google Scholar]
- 32.Seibold HR. A case of histoplasmosis in a dog. Journal of the American Veterinary Medical Association. 1946;109:209–11. Epub 1946/09/01. . [PubMed] [Google Scholar]
- 33.Bromel C, Sykes JE. Histoplasmosis in dogs and cats. Clinical techniques in small animal practice. 2005;20(4):227–32. Epub 2005/12/02. 10.1053/j.ctsap.2005.07.003 . [DOI] [PubMed] [Google Scholar]
- 34.Antinori S. Histoplasma capsulatum: more widespread than previously thought. The American journal of tropical medicine and hygiene. 2014;90(6):982–3. Epub 2014/04/30. 10.4269/ajtmh.14-0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loulergue P, Bastides F, Baudouin V, Chandenier J, Mariani-Kurkdjian P, Dupont B, et al. Literature review and case histories of Histoplasma capsulatum var. duboisii infections in HIV-infected patients. Emerging infectious diseases. 2007;13(11):1647–52. Epub 2008/01/26. 10.3201/eid1311.070665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gopalakrishnan R, Nambi PS, Ramasubramanian V, Abdul Ghafur K, Parameswaran A. Histoplasmosis in India: truly uncommon or uncommonly recognised? The Journal of the Association of Physicians of India. 2012;60:25–8. Epub 2013/06/20. . [PubMed] [Google Scholar]
- 37.Pan B, Chen M, Pan W, Liao W. Histoplasmosis: a new endemic fungal infection in China? Review and analysis of cases. Mycoses. 2013;56(3):212–21. Epub 2012/12/12. 10.1111/myc.12029 . [DOI] [PubMed] [Google Scholar]
- 38.Carter DA, Taylor JW, Dechairo B, Burt A, Koenig GL, White TJ. Amplified single-nucleotide polymorphisms and a (GA)(n) microsatellite marker reveal genetic differentiation between populations of Histoplasma capsulatum from the Americas. Fungal genetics and biology: FG & B. 2001;34(1):37–48. Epub 2001/09/25. 10.1006/fgbi.2001.1283 . [DOI] [PubMed] [Google Scholar]
- 39.Taylor JW, Jacobson DJ, Kroken S, Kasuga T, Geiser DM, Hibbett DS, et al. Phylogenetic species recognition and species concepts in fungi. Fungal genetics and biology: FG & B. 2000;31(1):21–32. 10.1006/fgbi.2000.1228 . [DOI] [PubMed] [Google Scholar]
- 40.Kasuga T, White TJ, Koenig G, McEwen J, Restrepo A, Castaneda E, et al. Phylogeography of the fungal pathogen Histoplasma capsulatum. Molecular ecology. 2003;12(12):3383–401. . [DOI] [PubMed] [Google Scholar]
- 41.Taylor ML, Hernandez-Garcia L, Estrada-Barcenas D, Salas-Lizana R, Zancope-Oliveira RM, Garcia de la Cruz S, et al. Genetic diversity of Histoplasma capsulatum isolated from infected bats randomly captured in Mexico, Brazil, and Argentina, using the polymorphism of (GA)(n) microsatellite and its flanking regions. Fungal biology. 2012;116(2):308–17. Epub 2012/02/01. 10.1016/j.funbio.2011.12.004 . [DOI] [PubMed] [Google Scholar]
- 42.Taylor ML, Chavez-Tapia CB, Rojas-Martinez A, del Rocio Reyes-Montes M, del Valle MB, Zuniga G. Geographical distribution of genetic polymorphism of the pathogen Histoplasma capsulatum isolated from infected bats, captured in a central zone of Mexico. FEMS immunology and medical microbiology. 2005;45(3):451–8. Epub 2005/08/03. 10.1016/j.femsim.2005.05.019 . [DOI] [PubMed] [Google Scholar]
- 43.Muniz Mde M, Morais ESTP, Meyer W, Nosanchuk JD, Zancope-Oliveira RM. Comparison of different DNA-based methods for molecular typing of Histoplasma capsulatum. Applied and environmental microbiology. 2010;76(13):4438–47. Epub 2010/05/11. 10.1128/AEM.02004-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Galo C, Sanchez AL, Fontecha GA. Genetic Diversity of Histoplasma Capsulatum Isolates from Honduras. Science Journal of Microbiology. 2013;Article ID sjmb-288,:7. [Google Scholar]
- 45.Martin DP, Murrell B, Golden M, Khoosal A, Muhire B. RDP4: Detection and analysis of recombination patterns in virus genomes. Virus Evolution. 2015;1(1). 10.1093/ve/vev003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Molecular biology and evolution. 2013;30(12):2725–9. Epub 2013/10/18. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Darriba D, Taboada GL, Doallo R, Posada D. jModelTest 2: more models, new heuristics and parallel computing. Nature methods. 2012;9(8):772 Epub 2012/08/01. 10.1038/nmeth.2109 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nguyen LT, Schmidt HA, von Haeseler A, Minh BQ. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol. 2015;32(1):268–74. 10.1093/molbev/msu300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Minh BQ, Nguyen MA, von Haeseler A. Ultrafast approximation for phylogenetic bootstrap. Molecular biology and evolution. 2013;30(5):1188–95. Epub 2013/02/19. 10.1093/molbev/mst024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drummond AJ, Suchard MA, Xie D, Rambaut A. Bayesian phylogenetics with BEAUti and the BEAST 1.7. Molecular biology and evolution. 2012;29(8):1969–73. Epub 2012/03/01. 10.1093/molbev/mss075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rannala B, Yang Z. Probability distribution of molecular evolutionary trees: a new method of phylogenetic inference. Journal of molecular evolution. 1996;43(3):304–11. . [DOI] [PubMed] [Google Scholar]
- 52.Xia X. DAMBE5: a comprehensive software package for data analysis in molecular biology and evolution. Molecular biology and evolution. 2013;30(7):1720–8. Epub 2013/04/09. 10.1093/molbev/mst064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ho SY, Shapiro B. Skyline-plot methods for estimating demographic history from nucleotide sequences. Molecular ecology resources. 2011;11(3):423–34. Epub 2011/04/13. 10.1111/j.1755-0998.2011.02988.x . [DOI] [PubMed] [Google Scholar]
- 54.Rambaut A, Suchard MA, Xie D, Drummond AJ. Tracer v1.6. 2014.
- 55.Joly S, Stevens MI, van Vuuren BJ. Haplotype networks can be misleading in the presence of missing data. Systematic biology. 2007;56(5):857–62. Epub 2007/10/25. 10.1080/10635150701633153 . [DOI] [PubMed] [Google Scholar]
- 56.Bandelt HJ, Forster P, Rohl A. Median-joining networks for inferring intraspecific phylogenies. Molecular biology and evolution. 1999;16(1):37–48. . [DOI] [PubMed] [Google Scholar]
- 57.Excoffier L, Laval G, Schneider S. Arlequin (version 3.0): an integrated software package for population genetics data analysis. Evolutionary bioinformatics online. 2005;1:47–50. [PMC free article] [PubMed] [Google Scholar]
- 58.Tajima F. Statistical method for testing the neutral mutation hypothesis by DNA polymorphism. Genetics. 1989;123(3):585–95. Epub 1989/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fu YX. Statistical tests of neutrality of mutations against population growth, hitchhiking and background selection. Genetics. 1997;147(2):915–25. Epub 1997/10/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hubisz MJ, Falush D, Stephens M, Pritchard JK. Inferring weak population structure with the assistance of sample group information. Mol Ecol Resour. 2009;9(5):1322–32. Epub 2009/09/01. 10.1111/j.1755-0998.2009.02591.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Corander J, Marttinen P. Bayesian identification of admixture events using multilocus molecular markers. Molecular ecology. 2006;15(10):2833–43. Epub 2006/08/17. 10.1111/j.1365-294X.2006.02994.x . [DOI] [PubMed] [Google Scholar]
- 62.Corander J, Marttinen P, Siren J, Tang J. Enhanced Bayesian modelling in BAPS software for learning genetic structures of populations. BMC bioinformatics. 2008;9:539 Epub 2008/12/18. 10.1186/1471-2105-9-539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pritchard JK, Stephens M, Donnelly P. Inference of population structure using multilocus genotype data. Genetics. 2000;155(2):945–59. Epub 2000/06/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Manos NE, Ferebee SH, Kerschbaum WF. Geographic variation in the prevalence of histoplasmin sensitivity. Diseases of the chest. 1956;29(6):649–68. Epub 1956/06/01. . [DOI] [PubMed] [Google Scholar]
- 65.Ajello L. A comparative study of the pulmonary mycoses of Canada and the United States. Public health reports. 1969;84(10):869–77. Epub 1969/10/01. [PMC free article] [PubMed] [Google Scholar]
- 66.Skillman D, Davis B, Harris JR, Nett RJ. Histoplasmosis in a state where it is not known to be endemic—Montana, 2012–2013. MMWR Morbidity and mortality weekly report. 2013;62(42):834–7. Epub 2013/10/25. . [PMC free article] [PubMed] [Google Scholar]
- 67.Allard A, Décarie D, Grenier JL, Lacombe MC, F. L. Histoplasmosis outbreak associated with the renovation of an old house—Quebec, Canada, 2013. MMWR Morbidity and mortality weekly report. 2014;62(51–52):1041–4. Epub 2014/01/02. . [PMC free article] [PubMed] [Google Scholar]
- 68.Retallack DM, Woods JP. Molecular epidemiology, pathogenesis, and genetics of the dimorphic fungus Histoplasma capsulatum. Microbes and infection / Institut Pasteur. 1999;1(10):817–25. Epub 2000/05/18. . [DOI] [PubMed] [Google Scholar]
- 69.Nielsen K, Heitman J. Sex and virulence of human pathogenic fungi. Advances in genetics. 2007;57:143–73. 10.1016/S0065-2660(06)57004-X . [DOI] [PubMed] [Google Scholar]
- 70.Nacher M, Adenis A, Aznar C, Blanchet D, Vantilcke V, Demar M, et al. How many have died from undiagnosed human immunodeficiency virus-associated histoplasmosis, a treatable disease? Time to act. Am J Trop Med Hyg. 2014;90(2):193–4. 10.4269/ajtmh.13-0226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.neglected histoplasmosis in Latin America G. Disseminated histoplasmosis in Central and South America, the invisible elephant: the lethal blind spot of international health organizations. AIDS. 2016;30(2):167–70. 10.1097/QAD.0000000000000961 . [DOI] [PubMed] [Google Scholar]
- 72.Dubois A, Janssens PG, Brutsaert P, Vanbreuseghem R. [A case of African histoplasmosis; with a mycological note on Histoplasma duboisii n.sp]. Annales de la Societe belge de medecine tropicale. 1952;32(6):569–84. Epub 1952/12/31. . [PubMed] [Google Scholar]
- 73.Martin-Iguacel R, Kurtzhals J, Jouvion G, Nielsen SD, Llibre JM. Progressive disseminated histoplasmosis in the HIV population in Europe in the HAART era. Case report and literature review. Infection. 2014;42(4):611–20. Epub 2014/03/15. 10.1007/s15010-014-0611-7 . [DOI] [PubMed] [Google Scholar]
- 74.Pellaton C, Cavassini M, Jaton-Ogay K, Carron PN, Christen-Zaech S, Calandra T, et al. Histoplasma capsulatum var. duboisii infection in a patient with AIDS: rapid diagnosis using polymerase chain reaction-sequencing. Diagn Microbiol Infect Dis. 2009;64(1):85–9. Epub 2009/03/24. 10.1016/j.diagmicrobio.2009.01.001 . [DOI] [PubMed] [Google Scholar]
- 75.Norkaew T, Ohno H, Sriburee P, Tanabe K, Tharavichitkul P, Takarn P, et al. Detection of environmental sources of Histoplasma capsulatum in Chiang Mai, Thailand, by nested PCR. Mycopathologia. 2013;176(5–6):395–402. Epub 2013/09/14. 10.1007/s11046-013-9701-9 . [DOI] [PubMed] [Google Scholar]
- 76.Ohno H, Tanabe K, Umeyama T, Kaneko Y, Yamagoe S, Miyazaki Y. Application of nested PCR for diagnosis of histoplasmosis. Journal of infection and chemotherapy: official journal of the Japan Society of Chemotherapy. 2013;19(5):999–1003. Epub 2013/01/25. 10.1007/s10156-013-0548-2 . [DOI] [PubMed] [Google Scholar]
- 77.Wang Y, Pan B, Wu J, Bi X, Liao W, Pan W, et al. Detection and phylogenetic characterization of a case of Histoplasma capsulatum infection in mainland China. The American journal of tropical medicine and hygiene. 2014;90(6):1180–3. Epub 2014/04/02. 10.4269/ajtmh.14-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mota de Almeida FJ, Kivijarvi K, Roos G, Nylander K. A case of disseminated histoplasmosis diagnosed after oral presentation in an old HIV-negative patient in Sweden. Gerodontology. 2014. Epub 2014/09/12. 10.1111/ger.12150 . [DOI] [PubMed] [Google Scholar]
- 79.De D, Nath UK. Disseminated Histoplasmosis in Immunocompetent Individuals- not a so Rare Entity, in India. Mediterranean journal of hematology and infectious diseases. 2015;7(1):e2015028 Epub 2015/05/12. 10.4084/MJHID.2015.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McLeod DS, Mortimer RH, Perry-Keene DA, Allworth A, Woods ML, Perry-Keene J, et al. Histoplasmosis in Australia: report of 16 cases and literature review. Medicine. 2011;90(1):61–8. Epub 2011/01/05. 10.1097/MD.0b013e318206e499 . [DOI] [PubMed] [Google Scholar]
- 81.Bagagli E, Bosco SM, Theodoro RC, Franco M. Phylogenetic and evolutionary aspects of Paracoccidioides brasiliensis reveal a long coexistence with animal hosts that explain several biological features of the pathogen. Infection, genetics and evolution: journal of molecular epidemiology and evolutionary genetics in infectious diseases. 2006;6(5):344–51. 10.1016/j.meegid.2005.12.002 . [DOI] [PubMed] [Google Scholar]
- 82.Untereiner WA, Scott JA, Naveau FA, Sigler L, Bachewich J, Angus A. The Ajellomycetaceae, a new family of vertebrate-associated Onygenales. Mycologia. 2004;96(4):812–21. . [DOI] [PubMed] [Google Scholar]
- 83.Kenyon C, Bonorchis K, Corcoran C, Meintjes G, Locketz M, Lehloenya R, et al. A dimorphic fungus causing disseminated infection in South Africa. The New England journal of medicine. 2013;369(15):1416–24. Epub 2013/10/11. 10.1056/NEJMoa1215460 . [DOI] [PubMed] [Google Scholar]
- 84.Pollock C. Fungal diseases of columbiformes and anseriformes. The veterinary clinics of North America Exotic animal practice. 2003;6(2):351–61. Epub 2003/06/28. . [DOI] [PubMed] [Google Scholar]
- 85.Constantine DG. Geographic translocation of bats: known and potential problems. Emerging infectious diseases. 2003;9(1):17–21. Epub 2003/01/21. 10.3201/eid0901.020104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hoff GL, Bigler WJ. The role of bats in the propagation and spread of histoplasmosis: a review. Journal of wildlife diseases. 1981;17(2):191–6. Epub 1981/04/01. . [DOI] [PubMed] [Google Scholar]
- 87.Cordeiro Rde A, e Silva KR, Brilhante RS, Moura FB, Duarte NF, Marques FJ, et al. Coccidioides posadasii infection in bats, Brazil. Emerging infectious diseases. 2012;18(4):668–70. Epub 2012/04/04. 10.3201/eid1804.111641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Randhawa HS, Chaturvedi VP, Kini S, Khan ZU. Blastomyces dermatitidis in bats: first report of its isolation from the liver of Rhinopoma hardwickei hardwickei Gray. Sabouraudia. 1985;23(1):69–76. Epub 1985/02/01. . [PubMed] [Google Scholar]
- 89.Greer DL, McMurray DN. Pathogenesis and immune response to Paracoccidioides brasiliensis in the fructivorous bat, Artibeus lituratus. Sabouraudia. 1981;19(3):165–78. Epub 1981/09/01. . [PubMed] [Google Scholar]
- 90.Nowak RM. Walker's mammals of the world Baltimore, MD: The John Hopkins University Press; 1999. [Google Scholar]
- 91.Teeling EC, Springer MS, Madsen O, Bates P, O'brien SJ, Murphy WJ. A molecular phylogeny for bats illuminates biogeography and the fossil record. Science. 2005;307(5709):5. [DOI] [PubMed] [Google Scholar]
- 92.Sharpton TJ, Stajich JE, Rounsley SD, Gardner MJ, Wortman JR, Jordar VS, et al. Comparative genomic analyses of the human fungal pathogens Coccidioides and their relatives. Genome research. 2009;19(10):1722–31. Epub 2009/09/01. 10.1101/gr.087551.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Redondo RA, Brina LP, Silva RF, Ditchfield AD, Santos FR. Molecular systematics of the genus Artibeus (Chiroptera: Phyllostomidae). Molecular phylogenetics and evolution. 2008;49(1):44–58. Epub 2008/07/30. 10.1016/j.ympev.2008.07.001 . [DOI] [PubMed] [Google Scholar]
- 94.Brook CE, Dobson AP. Bats as 'special' reservoirs for emerging zoonotic pathogens. Trends in microbiology. 2015;23(3):172–80. Epub 2015/01/13. 10.1016/j.tim.2014.12.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Greer DL, McMurray DN. Pathogenesis of experimental histoplasmosis in the bat, Artibeus lituratus. The American journal of tropical medicine and hygiene. 1981;30(3):653–9. Epub 1981/05/01. . [DOI] [PubMed] [Google Scholar]
- 96.Gugnani HC, Muotoe-Okafor FA, Kaufman L, Dupont B. A natural focus of Histoplasma capsulatum var. duboisii is a bat cave. Mycopathologia. 1994;127(3):151–7. Epub 1994/09/01. . [DOI] [PubMed] [Google Scholar]
- 97.Sahaza JH, Suarez-Alvarez R, Estrada-Barcenas DA, Perez-Torres A, Taylor ML. Profile of cytokines in the lungs of BALB/c mice after intra-nasal infection with Histoplasma capsulatum mycelial propagules. Comp Immunol Microbiol Infect Dis. 2015;41:1–9. 10.1016/j.cimid.2015.05.003 . [DOI] [PubMed] [Google Scholar]
- 98.Sepulveda VE, Williams CL, Goldman WE. Comparison of phylogenetically distinct Histoplasma strains reveals evolutionarily divergent virulence strategies. MBio. 2014;5(4):e01376–14. 10.1128/mBio.01376-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mirarab S, Bayzid MS, Warnow T. Evaluating Summary Methods for Multilocus Species Tree Estimation in the Presence of Incomplete Lineage Sorting. Syst Biol. 2014. 10.1093/sysbio/syu063 . [DOI] [PubMed] [Google Scholar]
- 100.Davidson R, Vachaspati P, Mirarab S, Warnow T. Phylogenomic species tree estimation in the presence of incomplete lineage sorting and horizontal gene transfer. BMC Genomics. 2015;16 Suppl 10:S1 10.1186/1471-2164-16-S10-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mihu MR, Nosanchuk JD. Histoplasma virulence and host responses. International journal of microbiology. 2012;2012:268123 Epub 2011/10/19. 10.1155/2012/268123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nguyen VQ, Sil A. Temperature-induced switch to the pathogenic yeast form of Histoplasma capsulatum requires Ryp1, a conserved transcriptional regulator. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(12):4880–5. Epub 2008/03/15. 10.1073/pnas.0710448105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Grad YH, Lipsitch M. Epidemiologic data and pathogen genome sequences: a powerful synergy for public health. Genome biology. 2014;15(11):538 Epub 2014/11/25. 10.1186/s13059-014-0538-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagrams were inferred through haplotypes from 4 different loci as follows: arf, ole1, tub1 and H-anti. Circles are proportional to haplotype frequency and numbers of haplotype (h) and Haplotype Diversity index are shown. Black dots represent a single mutation and red dots represent median-joining vectors.
(PDF)
Epidemiological map was obtained at the Centers for Disease Control and Prevention (CDC) web site: www.cdc.gov/fungal/diseases/histoplasmosis/causes.html.
(PDF)
(XLSX)
(XLS)
(XLSX)
(XLS)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.