Abstract
Purpose
To determine which patient and injury factors are associated with the detection of high-grade laxity at examination under anesthesia prior to anterior cruciate ligament (ACL) reconstruction.
Methods
2318 patients who underwent primary ACL reconstruction without associated ligament injuries were identified. Demographic data and information regarding meniscal tears were collected. Patients with high-grade Lachman (>10mm difference from contralateral), pivot-shift (IKDC grade 3), or anterior drawer (>10mm difference from contralateral) were identified by physical examination under anesthesia prior to ACL reconstruction. Logistic regression modeling was used to evaluate whether chronicity of the ACL injury, patient age, sex, body mass index, generalized ligamentous laxity, and presence of meniscal tears were associated with increased odds of high-grade laxity, controlling for examining surgeon.
Results
Patients with chronic tears (>6 months from injury) had greater than twice the odds of having a high-grade Lachman, pivot-shift, and anterior drawer (all p<0.001) relative to patients with acute tears (<3 months from injury). Generalized ligamentous laxity (OR=2.33, p<0.001) and the presence of medial (OR=1.63, p<0.001) or lateral (OR=1.41, p=0.013) meniscus tears were associated with increased odds of a high-grade Lachman. Age less than 20 years (OR=1.34, p=0.023), female sex (OR=1.49, p=0.001), generalized ligamentous laxity (OR=3.46, p<0001), and the presence of a medial (OR=1.53, p <0.001) or lateral (OR=1.27, p=0.041) meniscus tear were associated with increased odds of a high-grade pivot-shift. Generalized ligamentous laxity (OR=2.27, p<0.001) and the presence of a medial (OR=1.73, p=0.001) or lateral (OR=1.50, p = 0.010) meniscus tear were associated with increased odds of a high-grade anterior drawer.
Conclusion
Chronic ACL tears, generalized ligamentous laxity, and meniscus tears are associated with increased odds of high-grade laxity with all three tests. Female patients and age under 20 is associated with increased odds of a high-grade pivot33 shift.
Level of Evidence
Level 2 - lesser quality prospective study
Introduction
The anterior cruciate ligament (ACL) is frequently injured in athletic populations. Knee laxity in the setting of an ACL injury is often assessed through physical examination using the Lachman,(1) pivot-shift,(2, 3) and anterior drawer tests.(4) The degree of laxity noted on these examinations, along with the patient’s history and imaging findings, informs the physician’s diagnosis and may influence treatment decisions and prognosis.(5)
In addition to injury to the ACL, numerous other factors may influence the degree of laxity detected with these physical examination tests. Previous work has demonstrated an increased incidence of a positive Lachman, anterior drawer, and pivot-shift in the setting of more chronic ACL injuries.(6–10) Previous studies have demonstrated a higher prevalence of lateral meniscus tears in patients with a high49 grade pivot-shift (11, 12) and in those with a positive anterior drawer test.(13) The influence of patient demographic factors on the findings of these pre-operative physical examination tests has not been explored in detail, although females have been noted to have increased anterior laxity in some series following ACL reconstruction.(14) All previous studies on the subject have involved relatively small patient numbers, limiting the number of potential factors that could be evaluated.
The purpose of this study is to determine which patient and injury factors are associated with the detection of high-grade laxity at examination under anesthesia prior to ACL reconstruction. We hypothesized that younger age, female sex, lower body mass index (BMI), generalized ligamentous laxity, concomitant meniscus injuries, and increased time from ACL injury to reconstruction are associated with high-grade laxity prior to ACL reconstruction.
Methods
Patients
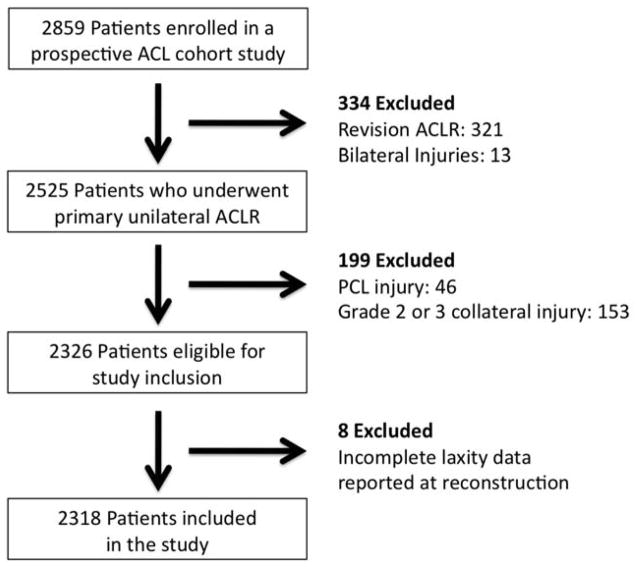
From an ongoing IRB approved prospective comparative study, 2859 patients were identified who underwent ACL reconstruction between 2002 and 2008. No patients with associated fractures were included in the cohort. Following exclusion of patients undergoing revision surgery and those with bilateral injuries, 2525 patients remained who underwent unilateral primary ACL reconstruction. Following exclusion of 199 patients with associated grade 2 or 3 collateral ligament injuries or posterior cruciate ligament injuries according the magnetic resonance imaging and examination at the time of reconstruction, 2326 patients were eligible for inclusion in the current study. Complete data regarding laxity at the time of ACL reconstruction was available for 2318 patients (99.6%) that form the study population (Figure 1).
Figure 1.
Flowchart demonstrating the selection of patients for study inclusion as well as loss to follow-up.
Data Extraction
Demographic data (age, sex, BMI), physical examination findings under anesthesia prior to ACL reconstruction, the presence of concomitant meniscus injury, the surgeon performing the examination, and the time from ACL injury to reconstruction were collected. Patients reported by the operating surgeon as having a Lachman or anterior drawer examination greater than 10 mm difference from the contralateral side were classified as having a high-grade Lachman or anterior drawer respectively (based on the IKDC classification system). Studies is awake patients have demonstrated variables degrees agreement among investigators when classifying anterior translation using this system.(15–18) Patients reported by the operating surgeon as having an IKDC 3+ pivot-shift were classified as having a high88 grade pivot-shift. The pivot-shift examination has also been shown to have moderate inter-rater reliability.(18) Generalized ligamentous laxity was classified according to the IKDC system as “tight,” “normal,” or “lax.” For analysis, these were collapsed into two categories based on whether they were classified as “lax” or not. Meniscus tears were classified as absent or present in both the medial and lateral compartments. The time from ACL injury to surgery was classified as acute (less than 3 months), intermediate (3 to 6 months), or chronic (greater than 6 months). Due to insufficient certainty of accurate patient reporting of time from injury, chronic injuries were compared to acute injuries when evaluating the effect of injury chronicity on pre-operative laxity.
Statistics
Multiple logistic regression modeling was used to evaluate whether patient age, sex, BMI, generalized ligamentous laxity, meniscal tears, and chronicity of the ACL injury were associated with increased odds of a high-grade pre-reconstruction Lachman, pivot-shift, or anterior drawer, controlling for examiner. Because age and BMI were determined not to be linear in the logit, both were dichotomized for analysis. Age was dichotomized at 20 years and BMI was dichotomized at 25 kg/m2. Dichotomization at a BMI of 25 was selected because patients with a BMI over 25 are classified as overweight.(19) The presence of interactions between chronicity of injury, age, sex, BMI, generalized ligamentous laxity, and meniscus status were evaluated and no significant interactions were identified. Based on the 24 degrees of freedom required to model these potential predictor variables while controlling for examiner (17 surgeons), it was calculated that approximately 240 “events” (patients with high-grade pre-operative laxity) were needed for each laxity assessment. With a minimum of 10% of the 2318 patients exhibiting high-grade laxity, the sample size was adequate for this analysis.
Results
The 2318 patient study group consisted of 1299 males (56.0%) and 1019 females (44.0%). Mean patient age was 26.7 ± 11.1 years (range: 10–68 years), including 868 patients under age 20 (mean: 16.3 ± 1.8 years) and 1450 patients age 20 and older (mean: 32.9 ± 9.6 years). Mean BMI was 25.5 ± 4.9 kg/m2, including 1182 patients with a BMI less than 25 kg/m2 (mean: 22.1 ± 1.8 kg/m2) and 1113 patients with a BMI of 25 kg/m2 or greater (mean: 29.2 ± 4.4 kg/m2). BMI was unknown in 23 patients (0.1%). One hundred ninety-eight patients (8.5%) were characterized as having generalized ligamentous laxity. There were 1428 patients with acute tears who underwent ACL reconstruction within 3 months of injury (61.8%), 331 patients with intermediate tears who underwent ACL reconstruction between 3 and 6 months after ACL injury (14.3%), 552 patients with chronic tears who underwent reconstruction greater than 6 months after ACL injury (23.8%), and 7 patients in whom the date of injury was unknown (0.3%). At reconstruction, medial meniscus tears were noted in 931 patients (40.2%) and lateral meniscus tears were noted in 1098 patients (47.4%).
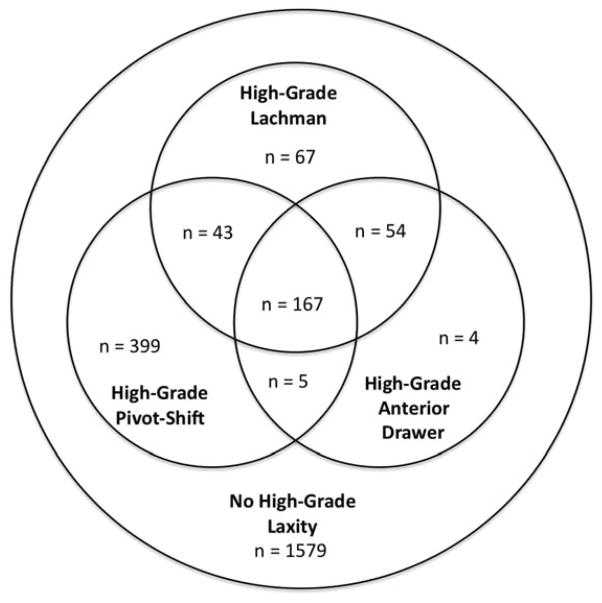
At total of 739 of 2318 patients (31.9%) demonstrated high-grade laxity on at least one physical examination test, including 167 patients (7.2%) who exhibited increased laxity on all three tests (Figure 2). The proportion of patients noted by each surgeon as having high-grade laxity varied greatly, ranging from 2.4% to 73.5% A high-grade pre-reconstruction Lachman (side-to-side difference of greater than 10 mm) was noted in 331 patients (14.3%), a high-grade pre-reconstruction pivot-shift (IKDC 3+) was noted in 614 patients of (26.5%), and a high-grade pre139 reconstruction anterior drawer (side-to-side difference of greater than 10 mm) was noted in 230 patients (9.9%).
Figure 2.
Venn diagram demonstrating the distribution of patients with high-grade laxity by physical examination test.
Multiple logistic regression demonstrated a high-grade Lachman to be associated with generalized ligamentous laxity, the presence of medial or lateral meniscus tears, and chronic relative to acute ACL injury (Table 1). Similarly, a high grade pivot-shift was associated with age less than 20 years, female sex, generalized ligamentous laxity, the presence of a medial or lateral meniscus tear, and chronic relative to acute ACL injury (Table 2). Finally, a high-grade anterior drawer was associated with generalized ligamentous laxity, the presence of a medial or lateral meniscus tear, and chronic relative to acute ACL injury (Table 3). No correlation was noted between BMI and high-grade Lachman, pivot-shift, or anterior drawer.
Table 1.
Factors Associated with High-Grade (>10 mm) Lachman Prior to ACL Reconstruction in a Multiple Logistic Regression Model Controlling for Surgeon
| Risk Factor | Odds Ratio (95% CI) | Significance |
|---|---|---|
| Age less than 20 years | 1.16 (0.86–1.56) | p = 0.33 |
| Female Sex | 1.14 (0.87 – 1.50) | p = 0.34 |
| Body Mass Index over 25 kg/m2 | 0.99 (0.72 – 1.31) | p = 0.93 |
| Generalized Ligamentous Laxity | 2.33 (1.59 – 3.42) | p < 0.001 |
| Medial Meniscus Tear | 1.63 (1.25 – 2.13) | p < 0.001 |
| Lateral Meniscus Tear | 1.41 (1.07 – 1.84) | p = 0.013 |
| Chronic (>6 months) Relative to Acute (<3 months) ACL Injuries | 2.99 (2.20 – 4.07) | p < 0.001 |
Table 2.
Factors Associated with High-Grade (3+) Pivot-Shift Prior to ACL Reconstruction in a Multiple Logistic Regression Model Controlling for Surgeon
| Risk Factor | Odds Ratio (95% CI) | Significance |
|---|---|---|
| Age less than 20 years | 1.34 (1.04 – 1.72) | p = 0.023 |
| Female Sex | 1.49 (1.18 – 1.88) | p = 0.001 |
| Body Mass Index over 25 kg/m2 | 0.89 (0.69 – 1.13) | p = 0.33 |
| Generalized Ligamentous Laxity | 3.46 (2.38 – 5.05) | p < 0.001 |
| Medial Meniscus Tear | 1.53 (1.21 – 1.94) | p < 0.001 |
| Lateral Meniscus Tear | 1.27 (1.01 – 1.61) | p = 0.041 |
| Chronic (>6 months) Relative to Acute (<3 months) ACL Injuries | 2.71 (2.04 – 3.61) | p < 0.001 |
Table 3.
Factors Associated with High-Grade (>10 mm) Anterior Drawer Prior to ACL Reconstruction in a Multiple Logistic Regression Model Controlling for Surgeon
| Risk Factor | Odds Ratio (95% CI) | Significance |
|---|---|---|
| Age less than 20 years | 1.15 (0.82 – 1.61) | p = 0.43 |
| Female Sex | 1.31 (0.96 – 1.79) | p = 0.10 |
| Body Mass Index over 25 kg/m2 | 0.98 (0.71 – 1.36) | p = 0.92 |
| Generalized Ligamentous Laxity | 2.27 (1.50 – 3.42) | p < 0.001 |
| Medial Meniscus Tear | 1.73 (1.27 – 2.35) | p = 0.001 |
| Lateral Meniscus Tear | 1.50 (1.10 – 2.04) | p = 0.010 |
| Chronic (>6 months) Relative to Acute (<3 months) ACL Injuries | 3.31 (2.33 – 4.71) | p < 0.001 |
Discussion
The key findings of this study are that patient age, sex, generalized ligamentous laxity, and presence of meniscal pathology significantly influence the odds of detection of high-grade ligamentous laxity in the setting of an ACL injury. Additionally, previous reports that more chronic ACL injuries are more likely to demonstrate increased laxity were confirmed.
Previously published work has demonstrated that lateral meniscus loss is associated with a larger pivot-shift prior to ACL reconstruction,(11) while demonstrating other factors such as femoral condylar anatomy that can also influence this risk.(12, 20) The current study confirmed the influence of lateral meniscus injury of pivot-shift magnitude, but also noted a relationship between pivot-shift magnitude and medial meniscus pathology that was not noted in prior work. These conflicting data may reflect differences between instrumented pivot164 shift assessment as done by Musahl et al(11) and the manual assessment performed by surgeons in the current study. There has been very little prior work evaluating the impact of patient demographic factors on pre-reconstruction knee laxity. Pre167 operative rotational knee laxity has been shown to strongly correlate with post168 operative rotational laxity,(21) and increased post-reconstruction laxity has been demonstrated to correlate with lower patient satisfaction(22) and Lysholm scores.(23) It is therefore important to understand factors associated with high171 grade laxity that may allow identification of populations at higher risk for poorer outcomes.
There is little known regarding factors that influence anterior knee laxity as determined with the Lachman test beyond ACL injury and the time from injury to reconstruction. This study identifies patient characteristics and meniscal pathology factors that are strongly associated with a high-grade Lachman. As with the pivot177 shift, such knowledge is important as increased anterior knee laxity at 20 degrees of flexion has been associated by some authors with poorer patient-reported outcomes following ACL reconstruction.(5)
Previous work evaluating the sensitivity of the anterior drawer test have demonstrated the test to be less sensitive than the Lachman examination,(24) with a higher odds of a positive result reported in the setting of an ACL tear with associated meniscal tears than in the setting of an isolated ACL tear.(13) The current study confirms this finding, which likely reflects the key role of the medial meniscus as a restraint to anterior tibial translation in the ACL deficient knee.
The high-grade laxity patient population may represent a group at increased risk of poor results following ACL reconstruction. Some authors have suggested that additional augmentation procedures in such patients to control high-grade laxity may improve outcomes.(25) Further work is required to determine the best management for such patients, but an understanding of the factors related to such laxity is critical.
The strengths of this study include a large sample size, which allowed for robust logistic regression analysis, and prospective data collection that which resulted in a very complete dataset. The data were collected by 17 surgeons at multiple institutions, making them broadly generalizable. In addition, separate reporting of medial and lateral meniscus tears is considered a strength of the study.
Limitations
This study does have several limitations. No specialized instruments were used to assess pre-reconstruction knee laxity and no assessment of intra- or inter201 rater reliability was performed. Previous studies have demonstrated inconsistent inter-rater reliability for assessment of laxity in ACL deficient knees, (17, 18) with guarding noted as a contributing factor.(20) Although the examinations in the current study were all performed under anesthesia, the laxity measures remain subjective and examiner-dependent. While limited, these assessments do represent the laxity data most frequently obtained and used by surgeons in making treatment decisions, making the data highly relevant for surgeons. Due to the variability laxity assessment among examiners, the logistic regression model did include and control for the examining surgeon, mitigating the influence of any examiner effects on the findings of the study. A further limitation is the lack of imaging data that would allow for assessment of other factors that may influence laxity, including condylar morphology and the presence of osteoarthritis.(12) Details of the depth of anesthesia and patient paralysis would have also been useful to control for in the model; however, these data are not available. Further, while patients were generally not reconstructed until the knee was calm, post-injury stiffness could potentially influence laxity assessments in patients reconstructed acutely; however, findings that laxity is increased in more chronic cases case been confirmed by prior work.(6–10) A more detailed assessment of the degree of generalized ligamentous laxity demonstrated by each patients (such as a Beighton score)(26) would also have been interesting to assess,; the collected data included on ly the IKDC classification of “tight”, “normal”, or “lax.”A final limitation of this study is the lack of specific details regarding the type of meniscus tears that were noted in each patient. Larger or more peripheral tears, as well as those located in the posterior horn of the menisci (particularly medially) may have a larger influence on the presence of high-grade knee laxity. Although some of this information was obtained at the time of surgery, this study was not appropriately powered to analyze this question.
Conclusion
Chronic ACL tears, generalized ligamentous laxity, and meniscus tears are associated with increased odds of high-grade laxity with all three tests. Female patients and age under 20 is associated with increased odds of a high-grade pivot232 shift.
Footnotes
- Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work was performed by all authors in this multicenter study.
- Drafting the work or revising it critically for important intellectual content: All authors
- Final approval of the version to be published: All authors
- All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 2.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980:45–50. [PubMed] [Google Scholar]
- 3.Larson RL. Physical examination in the diagnosis of rotatory instability. Clin Orthop Relat Res. 1983:38–44. [PubMed] [Google Scholar]
- 4.Malanga GA, Andrus S, Nadler SF, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003;84:592–603. doi: 10.1053/apmr.2003.50026. [DOI] [PubMed] [Google Scholar]
- 5.Heijne A, Ang BO, Werner S. Predictive factors for 12-month outcome after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2009;19:842–849. doi: 10.1111/j.1600-0838.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 6.Dahlstedt LJ, Dalen N. Knee laxity in cruciate ligament injury. Value of examination under anesthesia. Acta Orthop Scand. 1989;60:181–184. doi: 10.3109/17453678909149249. [DOI] [PubMed] [Google Scholar]
- 7.Jonsson T, Althoff B, Peterson L, Renstrom P. Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparative study of the Lachman test and the anterior drawer sign. Am J Sports Med. 1982;10:100–102. doi: 10.1177/036354658201000207. [DOI] [PubMed] [Google Scholar]
- 8.Mitsou A, Vallianatos P. Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparison between the Lachman test and the anterior drawer sign. Injury. 1988;19:427–428. doi: 10.1016/0020-1383(88)90139-8. [DOI] [PubMed] [Google Scholar]
- 9.Katz JW, Fingeroth RJ. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am J Sports Med. 1986;14:88–91. doi: 10.1177/036354658601400115. [DOI] [PubMed] [Google Scholar]
- 10.Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36:267–288. doi: 10.2519/jospt.2006.2011. [DOI] [PubMed] [Google Scholar]
- 11.Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 12.Musahl V, Ayeni OR, Citak M, Irrgang JJ, Pearle AD, Wickiewicz TL. The influence of bony morphology on the magnitude of the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2010;18:1232–1238. doi: 10.1007/s00167-010-1129-x. [DOI] [PubMed] [Google Scholar]
- 13.Donaldson WF, 3rd, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations. Initial versus examination under anesthesia. Am J Sports Med. 1985;13:5–10. doi: 10.1177/036354658501300102. [DOI] [PubMed] [Google Scholar]
- 14.Ryan J, Magnussen RA, Cox CL, Hurbanek JG, Flanigan DC, Kaeding CC. ACL reconstruction: do outcomes differ by sex? A systematic review. J Bone Joint Surg Am. 2014;96:507–512. doi: 10.2106/JBJS.M.00299. [DOI] [PubMed] [Google Scholar]
- 15.Johnson DS, Ryan WG, Smith RB. Does the Lachman testing method affect the reliability of the International Knee Documentation Committee (IKDC) Form? Knee Surg Sports Traumatol Arthrosc. 2004;12:225–228. doi: 10.1007/s00167-003-0475-3. [DOI] [PubMed] [Google Scholar]
- 16.Lange T, Freiberg A, Droge P, Lutzner J, Schmitt J, Kopkow C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture--A systematic review. Man Ther. 2015;20:402–411. doi: 10.1016/j.math.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Wiertsema SH, van Hooff HJ, Migchelsen LA, Steultjens MP. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee. 2008;15:107–110. doi: 10.1016/j.knee.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Peeler J, Leiter J, MacDonald P. Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sport Med. 2010;20:80–85. doi: 10.1097/JSM.0b013e3181ceca45. [DOI] [PubMed] [Google Scholar]
- 19.WHO. WHO Trachincal Report Series 854. World Health Organization; 1995. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. [PubMed] [Google Scholar]
- 20.Tanaka M, Vyas D, Moloney G, Bedi A, Pearle AD, Musahl V. What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc. 2012;20:737–742. doi: 10.1007/s00167-011-1866-5. [DOI] [PubMed] [Google Scholar]
- 21.Signorelli C, Bonanzinga T, Lopomo N, et al. Do pre-operative knee laxity values influence post-operative ones after anterior cruciate ligament reconstruction? Scand J Med Sci Sports. 2013;23:e219–224. doi: 10.1111/sms.12059. [DOI] [PubMed] [Google Scholar]
- 22.Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84-A:1560–1572. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 24.Kim SJ, Kim HK. Reliability of the anterior drawer test, the pivot shift test, and the Lachman test. Clin Orthop Relat Res. 1995:237–242. [PubMed] [Google Scholar]
- 25.Lerat JL, Mandrino A, Besse JL, Moyen B, Brunet-Guedj E. Effect of external extra-articular ligament plasty on the results of anterior cruciate ligament reconstruction with patellar tendon, a 4 years follow-up. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:591–601. [PubMed] [Google Scholar]
- 26.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]