Highlights
-
•
The extent of colon affected by MP varied a good deal between the cases.
-
•
Computed tomography was useful to determine the extent of affected colon.
-
•
MP caused by herbal medicine was often localized in the right colon.
-
•
Limited colonic resection is usually indicated.
Keywords: Herbal medicine, Mesenteric phlebosclerosis, Surgical procedures, Case report
Abstract
Introduction
Mesenteric phlebosclerosis is a rare ischemic disease affecting the colon. Systemic disease and herbal medicine have been pointed out as possible causes, and the disease is characterized by calcifications involved the mesocolic veins. Patients who do not respond to conservative therapy require surgical treatment. In surgical intervention, an adequate extent of colonic resection is important.
Presentation of case
We present a case of an 87-year-old woman with mesenteric phlebosclerosis who had consumed herbal medicine for 40 years. She suffered from ileus caused by mesenteric phlebosclerosis, and the symptoms did not improve with conservative therapy. Right hemicolectomy was performed since the disease was localized in the right colon. Long-term use of herbal medicine was considered the potential cause of mesenteric phlebosclerosis. The postoperative course was mostly uneventful. The patient stopped using herbal medicine and had no signs of recurrence 2 years after surgery.
Discussion and conclusion
The greatest concern in surgery for mesenteric phleboscrerosis is to detect the affected area, which should be removed. Characteristic findings in computed tomography and intraoperative findings can help to determine the optimal extent of colonic resection. Mesenteric phlebosclerosis caused by herbal medicines occurs as localized disease in the right colon compared with mesenteric phlebosclerosis caused by other pathogenesis. Limited colonic resection is usually indicated for mesenteric phlebosclerosis caused by herbal medicine.
1. Introduction
Mesenteric phlebosclerosis (MP) is a rare ischemic disease affecting the colon. Less than 100 cases have been reported thus far [1], [2], and most of these have been reported from Asian countries. This disease shows non-specific symptoms, such as nausea, vomiting, and abdominal pain and distension; therefore, it is often diagnosed in an advanced stage [1]. The pathogenesis of MP remains unclear, but conditions that cause portal vein hypertension [3], [4] or the administration of toxic agents such as certain herbal medicines [5] have been suggested to contribute to the onset of MP. The progress of this disease is chronic but irreversible [6]. Further, among patients with symptoms such as intestinal obstruction that are refractory to conservative therapy, surgical intervention is needed [1], [2]. However, the appropriate extent of colonic resection in these patients remains unclear.
We present a case of MP that required surgical intervention after long-term use of herbal medicines. We also review previously reported cases focusing on surgical interventions for MP.
2. Presentation of case
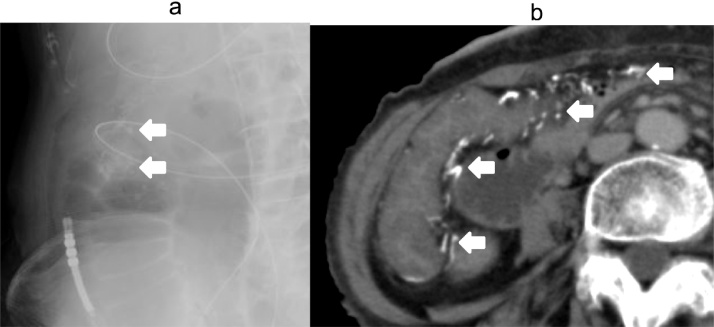
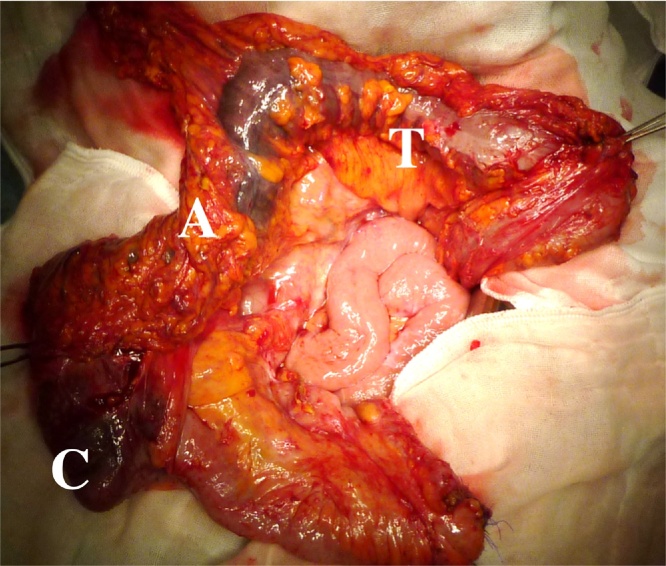
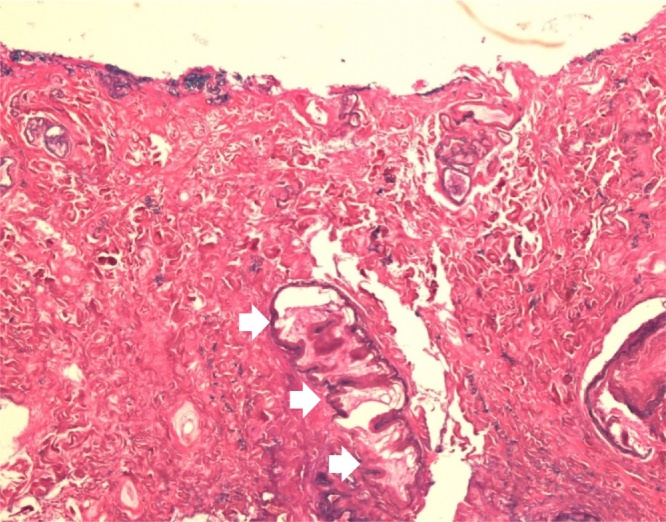
The patient was an 87-year-old woman who had worked at a pharmacy that dispensed herbal medicines. She often used several herbal medicines, such as Orengedokuto, for 40 years. Her past medical history included appendectomy, bronchiectasis, and mild chronic renal failure. In April 2013, she visited a hospital for abdominal pain and distension, where she was diagnosed with ileus and was admitted. She received conservative therapy using a nasogastric decompression tube or ileus tube, but the symptoms did not improve and she was transferred to our hospital. Physical examination revealed a distended abdomen and diffuse abdominal tenderness. Laboratory data showed mild inflammation (C-reactive protein 4.0 mg/dL), anemia (hemoglobin 9.7 g/dL), malnutrition (albumin 2.6 g/dL), and mild renal dysfunction (creatinine 1.53 g/dL). Other findings were normal. Abdominal radiography revealed threadlike calcifications in the right abdomen (Fig. 1a). Computed tomography (CT) revealed a dilated small intestine, thickened colonic wall, luminal stenosis of the ascending colon, and serpentine calcifications alongside the colonic and mesenteric veins, extending from the ileocolic to the middle colic vein (Fig. 1b). These findings suggested that she had MP, and her drug history suggested long-term use of herbal medicine as a possible cause. Given the patient’s advanced age and poor general condition, performing wide colonic resection was not feasible. Therefore, emergency ileostomy was performed to decompress the dilated small intestine after identifying the existence of arterial blood flow in the affected mesenteric region. The postoperative course was uneventful, and she was temporarily discharged from our hospital. In June 2013, she was re-admitted for a planned second surgery. Intraoperatively, we observed that the intestinal wall between the ascending and mid-transverse colon was dark purple. In particular, the cecum and proximal ascending colon were strongly affected and they were hard (Fig. 2). We performed a right hemicolectomy with ileo-colonic anastomosis (Fig. 3). Pathological examination of the resected portion revealed shedding mucosa, increased submucosal collagen fibers, intimal thickening, calcifications of the mesenteric veins, normal arteries, and no malignancy, which was consistent with the typical pathological findings of MP (Fig. 4). The postoperative course was uneventful except for temporary arrhythmia, and the patient was discharged 20 days after the second operation. She stopped using the herbal medicine and had no sign of recurrence at 2 years after the second operation.
Fig. 1.
Preoperative images. (A) Plain abdominal radiography shows thread-like calcifications in the right-sided colon area (arrows). (B) Non-contrast abdominal computed tomography reveals diffuse thickening of the ascending colon wall along with calcifications in the ascending colon and mesenteric veins (arrows).
Fig. 2.
Intraoperative findings. Dark purple-colored intestine was seen between the cecum and transverse colon (A: Ascending colon; C: cecum; T: transverse colon).
Fig. 3.
Resected specimen. The resected specimen shows a dark-purple thickened colon and luminal stenosis at the ascending colon (arrows).
Fig. 4.
Microscopic findings. Histological examination (hematoxylin-eosin staining, ×40) demonstrates shedding mucosa, increased submucosal collagen fibers, intimal thickening, the normal arteries and calcifications of the veins (arrows).
3. Discussion
MP was first reported by Koyama et al [7] in 1991. Yao et al. [4] termed it phlebosclerotic colitis, while Iwashita et al [8] called it idiopathic MP because of the unknown pathogenesis and the lack of pathological inflammation. Of the approximately 100 reported cases, most reports have described patients from Asian countries, especially Japan [2].
The symptoms of MP are non-specific, so it is difficult to diagnose it in its early stages [1]. There are no distinct diagnostic criteria for MP, but a few specific imaging findings have been reported, including dark-purple mucosa seen in colonoscopy, thread-like calcifications in abdominal radiographs, serpentine calcifications on abdominal CT, narrowing of the colon in barium enema, and decreased venous flow on angiography [2], [4], [6]. The pathogenesis of this disease remains unclear; however, circulatory disturbances caused by mesenteric venous occlusion (e.g., due to liver cirrhosis) have been suspected as a possible cause [4]. Recently, Hiramatsu et al5 summarized 25 cases with MP associated with the long-term usage of herbal medicines. They suspected that geniposide contained in herbal medicines might be a causative agent of MP. Orengedokuto, the herbal agent used in this case, contains geniposide.
MP progresses chronically, and the symptoms of this disease often improve by stopping the herbal intake1. However, intractable cases require surgical intervention. In the English literature, we identified 22 cases that required surgical treatment [1], [2], [3], [4], [5], [8], [9], [10], [11], [12], [13], [14], [15], including 9 cases [1], [2], [5], [12] with a history of using herbal medicines (Table 1). Of these, 10 cases were preoperatively diagnosed as MP, and 3 cases were misdiagnosed as Crohn’s disease and appendicitis. CT (11 cases) and/or colonoscopy (10 cases) were frequently used as the diagnostic modalities. Especially, CT was used in the last 7 cases. Also, angiography and/or barium enema were used in some former cases [2], [4], [6], [8], [10], [11]. The reasons for performing surgery in these cases were persistent abdominal pain (7 cases), intestinal stenosis (5 cases), intestinal perforation (2 cases), intestinal gangrene (1 case), intra-abdominal abscess and intestinal stenosis (1 case), and unknown (6 cases). Total colectomy was performed in 3 cases; subtotal colectomy, in 12 cases; and right hemicolectomy in 7 cases. With regard to the relationship between the extent of colonic resection and the pathogenesis of MP, limited colonic resection appeared to be performed in the cases of MP caused by herbal medicine. As described previously, geniposide in herbal medicines has been reported to be a causative agent of MP [5]. Geniposide is usually absorbed in the ascending colon, and MP often occurs first in the ascending colon [5]. Therefore, MP caused by herbal medicines occurs as localized disease in the right colon in contrast with MP caused by other pathogenesis, including liver cirrhosis and right heart failure, which could cause high blood pressure in the mesenteric veins and affect the entire colon [3], [4]. Additionally, genipin, which is derived from geniposide via the action of enteric bacteria, has been reported to dye the intestinal wall blue [5]; this can help in identifying the affected region intraoperatively, as in our case. Therefore, we consider that when surgical intervention is needed for patients with MP, it is very important to confirm whether the MP has been caused by herbal medicines in order to determine the extent of intestinal resection and enable minimal resection. There have been no reports referring the relation between the cause of MP and the extent of surgery. However, in some cases, it might be difficult to detect the cause. The diagnostic value of CT scan in MP should also be noted. The characteristic distribution of perivenous calcifications as detected on CT scans is useful for determining the colonic areas affected by MP.
Table 1.
Review of previously reported surgical cases and our case.
| Year | Author | Age | Sex | Herbal medicine | Affected region |
Preoperative diagnosis | Operative indication | Surgical method | ||
|---|---|---|---|---|---|---|---|---|---|---|
| CT | Colonoscopy | Intraoperative | ||||||||
| 1997 | Maruyama | 78 | F | ND | − | I-D | I-D | − | Stenosis | Subtototal colectomy |
| 1999 | Kitamura | 56 | F | ND | − | − | A-T | − | Perforation | Subtototal colectomy |
| 2000 | Yao | 36 | M | − | A-T | − | − | Ileus | Abdominal pain | Subtototal colectomy |
| 57 | M | ND | A-T | − | C-D | Crohn's disease | Abdominal pain | Subtototal colectomy | ||
| 2003 | Iwashita | 57 | M | − | − | I-D | − | − | Abdominal pain | Subtototal colectomy |
| 53 | F | − | − | C-S | − | − | Stenosis | Subtototal colectomy | ||
| 73 | F | − | − | I-T | − | − | Abdominal pain | Right hemicolectomy | ||
| 61 | F | − | − | I-D | − | − | Stenosis | Subtototal colectomy | ||
| 2003 | Kimura | 74 | F | ND | C-A | C-A | C-D | MP | − | Total colectomy |
| 2005 | Markos | 53 | M | − | C-T | − | C-T | − | − | Right hemicolectomy |
| 2007 | Chang | 46 | F | + | − | − | C-S | Crohn's disease | Perforation | Subtototal colectomy |
| 33 | M | + | − | − | C-T | Appendicitis | − | Subtototal colectomy | ||
| 53 | M | + | − | − | − | MP | − | Subtototal colectomy | ||
| 52 | F | + | − | − | − | MP | − | Subtototal colectomy | ||
| 2010 | Kato | 68 | M | − | − | − | − | MP | Abscess/Stenosis | Total colectomy |
| 2012 | Hiramatsu | 55 | F | + | C-T | A-T | − | MP | Abdominal pain | Right hemicolectomy |
| 59 | F | + | A-T | A-T | − | MP | Abdominal pain | Right hemicolectomy | ||
| 2014 | Chang | 56 | F | ND | C-T | − | − | Ileus | Stenosis | Right hemicolectomy |
| 2014 | Guo | 63 | M | + | C-D | C-S | − | MP/Crohn's disease | Abdominal pain | Total colectomy |
| 2014 | Shibata | 70 | F | ND | C-A | I-T | I-T | MP | − | Right hemicolectomy |
| 2014 | Fang | 56 | M | + | I-D | − | C-S | MP | Gangrene | Subtototal colectomy |
| 2015 | Our case | 87 | F | + | C-T | − | C-T | MP | Stenosis | Right hemicolectomy |
A, ascending colon; C, cecum; CT, computed tomography; D, descending colon; I, terminal ileum;MP: mesenteric phlebosclerosis; ND, not documented; S, sigmoid colon; T, transverse colon.
In summary, when surgical intervention is needed for MP, preoperative assessment should determine whether MP is caused by herbal medicines; further, CT should be performed in order to assess the extent of the affected region accurately. In the present case, the long-term use of herbal medicine was suspected to be the cause of the disease, and we performed right hemicolectomy because the calcifications on CT were localized in the right colon.
4. Conclusion
We have reported a case of MP potentially caused by long-term use of herbal medicine. Limited colonic resection is usually indicated for MP caused by herbal medicine. Characteristic findings in CT and intraoperative findings can help to determine the optimal extent of intestinal resection in patients with MP that does not respond to conservative management.
Conflicts of interest
None.
Funding
None.
Ethical approval
This is not a research study, and ethical approval is not required.
Consent
Written informed consent was obtained from the patients for publication of this Case Report and any accompanying images.
Author contributions
Koya Hida performed the surgery. Nobuaki Hoshino wrote the draft. Suguru Hasegawa and Kenji Kawada revised it critically. Yoshiharu Sakai approved it to be published.
Guarantor
Nobuaki Hoshino.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.ijscr.2016.05.051.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Guo F., Zhou Y.F., Zhang F., Yuan F., Yuan Y.Z., Yao W.Y. Idiopathic mesenteric phlebosclerosis associated with long-term use of medical liquor: two case reports and literature review. World J. Gastroenterol. 2014;20:5561–5566. doi: 10.3748/wjg.v20.i18.5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fang Y.L., Hsu H.C., Chou Y.H., Wu C.C., Chou Y.Y. Phlebosclerotic colitis: a case report and review of the literature. Exp. Ther. Med. 2014;7:583–586. doi: 10.3892/etm.2014.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitamura T., Kubo M., Nakanishi T., Fushimi H., Yoshikawa K., Taenaka N. Phlebosclerosis of the colon with positive anti-centromere antibody. Intern. Med. 1999;38:416–421. doi: 10.2169/internalmedicine.38.416. [DOI] [PubMed] [Google Scholar]
- 4.Yao T., Iwashita A., Hoashi T., Matsui T., Sakurai T., Arima S. Phlebosclerotic colitis: value of radiography in diagnosis—report of three cases. Radiology. 2000;214:188–192. doi: 10.1148/radiology.214.1.r00ja01188. [DOI] [PubMed] [Google Scholar]
- 5.Hiramatsu K., Sakata H., Horita Y., Orita N., Kida A., Mizukami A. Mesenteric phlebosclerosis associated with long-term oral intake of geniposide, an ingredient of herbal medicine. Aliment. Pharmacol. Ther. 2012;36:575–586. doi: 10.1111/j.1365-2036.2012.05221.x. [DOI] [PubMed] [Google Scholar]
- 6.Kusanagi M., Matsui O., Kawashima H., Gabata T., Ida M., Abo H. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am. J. Roentgenol. 2005;185:441–447. doi: 10.2214/ajr.185.2.01850441. [DOI] [PubMed] [Google Scholar]
- 7.Koyama N., Koyama H., Hanajima T., Matsubara N., Fujisaki J., Shimoda T. Chronic ischemic colitis causing stenosis: report of a case. Stomach Intest. 1991;26:455–456. (in Japanese, English abstract) [Google Scholar]
- 8.Iwashita A., Yao T., Schlemper R.J., Kuwano Y., Iida M., Matsumoto T. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis. Colon Rectum. 2003;46:209–220. doi: 10.1097/01.DCR.0000044720.43258.6E. [DOI] [PubMed] [Google Scholar]
- 9.Maruyama Y., Watanabe F., Kanaoka S., Kanamaru H., Yoshino G., Koda K. A case of phlebosclerotic ischemic colitis: a distinct entity. Endoscopy. 1997;29:334. doi: 10.1055/s-2007-1004207. [DOI] [PubMed] [Google Scholar]
- 10.Kimura Y., Kashima K., Daa T., Tou Y., Hanzawa K., nakayama I. Phlebosclerotic colitis coincident with carcinoma in adenoma. Pathol. Int. 2003;53:721–725. doi: 10.1046/j.1440-1827.2003.01539.x. [DOI] [PubMed] [Google Scholar]
- 11.Markos V., Kelly S., Yee W.C., Davis J.E., Cheifetz R.E., Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am. J. Roentgenol. 2005;184:1584–1586. doi: 10.2214/ajr.184.5.01841584. [DOI] [PubMed] [Google Scholar]
- 12.Chang K.M. New histologic findings in idiopathic mesenteric phlebosclerosis: clues to its pathogenesis and etiology—probably ingested toxic agent-related. J. Chin. Med. Assoc. 2007;70:227–235. doi: 10.1016/S1726-4901(09)70364-8. [DOI] [PubMed] [Google Scholar]
- 13.Kato T., Miyazaki K., Nakamura T., Tan K.Y., Chiba T., Konishi F. Perforated phlebosclerotic colitis—description of a case and review of this condition. Colorectal Dis. 2010;12:149–151. doi: 10.1111/j.1463-1318.2008.01726.x. [DOI] [PubMed] [Google Scholar]
- 14.Chang Y.Y., Lin H.H., Lin C.C. Phlebosclerotic colitis presenting as intestinal obstruction. Clin. Gastroenterol. Hepatol. 2014;12:e81–2. doi: 10.1016/j.cgh.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 15.Shibata H., Nishikawa J., Sakaida I. Dark purple-colored colon: sign of idiopathic mesenteric phlebosclerosis. Dig. Endosc. 2014;26:604–605. doi: 10.1111/den.12299. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.