Abstract
With one fifth of the world’s total population, China’s prevention and control of cardiovascular disease (CVD) may affect the success of worldwide efforts to achieve sustainable CVD reduction. To understand China’s current cardiovascular epidemic, requires awareness of the economic development in the past decades. The rapid economic transformations (industrialization, marketization, urbanization, globalization, and informationalization) contributed to the aging demography, unhealthy lifestyles, and environmental changes. The later have predisposed to increasing cardiovascular risk factors and the CVD pandemic. Rising CVD rates have had a major economic impact, which has challenged the health care system and the whole society. With recognition of the importance of health, initial political steps and national actions have been taken to address the CVD epidemic. Looking to the future, we recommend that four priorities should be taken: pursue multi-sectorial government and non-government strategies targeting the underlying causes of CVD (the “whole-of-government and whole-of-society” policy); give priority to prevention; reform the health care system to fit the nature of noncommunicable diseases; and conduct research for evidence-based, low-cost, simple, sustainable, and scalable interventions. By pursuing the four priorities, the pandemic of CVD and other major NCDs in China will be reversed and the global sustainable development goal achieved.
Keywords: Cardiovascular disease, risk factors, socioeconomic changes, China, prevention
China is the most populous country in the world; the total population was over 1.36 billion in 2014.1, 2 The status in prevention and control of cardiovascular disease (CVD) in this large and aging country with about 1/5 of the world total population bears a huge potential impact on global health. It may also affect the global success in achieving the Sustainable Development Goal of a one-third reduction in premature deaths from noncommunicable diseases by 2030.3 To better understand China’s status in prevention and control of CVD, we will start from China’s evolving socioeconomic context to introduce the accompanying environmental and lifestyle changes, the consequent changes in major risk factors and burden of CVD, the resulting challenges to the economy, healthcare system and whole society. We also identify China’s opportunities and responses to the challenge. Priorities are recommended at the end of the article as the critical steps to curb increasing CVD in China, which should help achieve the global sustainable development goals.
Socioeconomic Context, Demography and General Health Status
The rapid economic expansion started in 1978 when China implemented the open-door policy. With the policy, China started to reform its planned economy and encouraged outside investment from other countries.4 The reform movement has resulted in rapid changes that have driven economic growth: industrialization, marketization, urbanization, globalization, and informationalization. The key economic and health sequelae of the economic transformations are listed in Table 1. Meanwhile, China has gradually switched from a planned economy to a socialist market economy. As the result, the average annual rate of increase in GDP has been about 9% from 1983 to 2011.2 From 2000 to 2010, China’s total gross domestic product (GDP) grew from 1.5 to 6.5 trillion USD per year, while GDP per capita increased from around $1,000 to $4500, overall a 3–4 fold increase in both over just 10 years. In 2011, China became the world’s second largest economy.1
Table 1.
Transformations driving China’s economy in the past decades, and the link between health hazards and major non-communicable diseases
| Rapid Transformations | Major indications of the transformations* | Intermediate health hazard factors driven by the transformations | Cardiovascular risk factors | Major non-communicable diseases |
|---|---|---|---|---|
| Industrialization |
|
↑Air, water, and soil pollution ↑Processed foods ↓Physical activity |
|
|
| Marketization |
|
↑Privatization ↑Competition ↑Mental stress ↑Health inequity |
||
| Urbanization |
|
↓ Physical activity ↑Unhealthy diet ↑ Air & water pollution ↑Mental stress ↑Sedentary lifestyle |
||
| Globalization |
|
↑Fast food ↑High salt snack foods ↑High sugar soft drinks & foods |
||
| Informationalization |
|
↓Physical activity ↓Face-to-face social interactions |
Data from China national statistics annual reports1.
During the same period there have been dramatic changes in health as well. Life expectancy increased from 67.9 years in 1981 to 74.8 in 2010.5 In 2013, life expectancy at birth in China was reported 73.5 years for males and 80.0 years for females.6 Infant mortality declined from 50.2 per 1000 live births in 1991 to 9.5 per 1000 live births in 2013, the same trend was observed for children under 5 years and maternal mortality.7 And the deaths from communicable diseases remained at or below 1 per 100,000.7
As a consequence of rapid economic and health changes, the proportion of the Chinese older population is increasing exponentially. Today, 10% of the population is 65 years or older.1 By 2030, 17% (240 million) of the population will be over 65 years of age.8 In the next 30-year period, from 2010 to 2040, China will be the fastest aging country in the world.9
With the social and economic transformation, the standard of living is greatly improved. However, unhealthy eating patterns and sedentary lifestyle have increased and the environment has become heavily polluted.10, 11 The aging of the population, the changes in lifestyle and environment are contributing to marked increases in CVD and other NCDs.
Changes in Lifestyle
Physical activity and sedentary lifestyle
The changes in China’s industrial productivity reflected the dramatic and unhealthy lifestyle changes chosen by most people living in China. Figure 1 shows the changes in number of major industrial products that were closely related to people’s daily life from 1990 to 2010. Annually the production of cars increased from only 35 thousand to 18.3 million, computers from 82 thousand to 246 million and televisions from 10.3 million to 118.3 million. However, annual bicycle production declined from 41.2 million in 1990 to 23.1 million in 1998. Production rose steadily to 68.2 million in 2010, the rebound reflecting exports after 2000. Local sales of bicycles have continued to fall.1 In fact, bicycles were ubiquitous in China 20–30 years ago. From 1992 to 2007 the number of households possessing at least one bicycle decreased from 97% to 49% in China, exhibiting the most dramatic variation among the 150 participating countries in the study.12 Declining bicycle use and shifting to motorized vehicle use has contributed to weight gain in China.13
Figure 1.
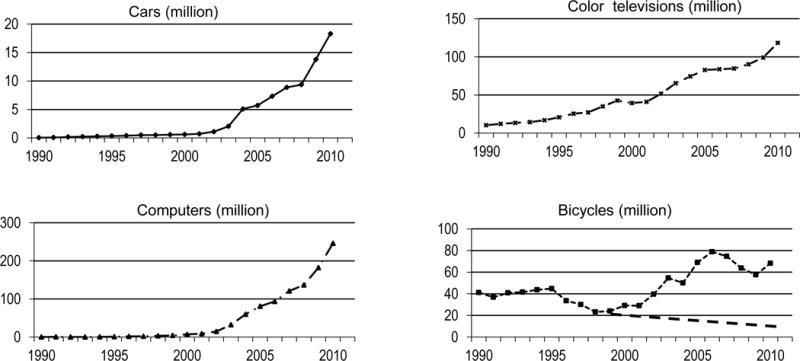
Number of annual production of cars, computers, televisions and bicycles in China from 1990 to 2010. Data source: National Bureau of Statistics of China.1
Multiple studies have reported declining physical activity levels in China. For example, nearly half of the United States-People’s Republic of China Joint Study of Cardiovascular and Cardiopulmonary Epidemiology (US-PRC Joint Study) participants from Beijing and Guangzhou, urban and rural, reported that their physical activity reduced significantly from 1988 to 1998.14 Data from samples in 9 provinces in the China Health and Nutrition Survey (CHNS) showed that total physical activity fell by 31% among adult men, from 382 MET hours per week in 1991 to 264 MET hours per week in 2011, and fell by 42% among adult women, from 420 MET hours per week in 1991 to 243 MET hours per week in 2011.15 In the 2002 Chinese National Nutrition and Health Survey (CNNHS), only 34% of adults in large cities and 45% in medium and small cities reported adequate physical activity.16 In 2012, only 18.7% of Chinese adults reported getting regular exercise.17 In China, occupational physical activities (77.6% and 59.8%, respectively, in men and women) accounted for most of the daily activities, while leisure time physical activities accounted for the least (3.1% in both men and women).18 Occupational physical activity dropped in Chinese men and women and in both urban and rural areas.15 Conversely, Chinese individuals are spending more time watching television. CHNS showed that urbanization factors predicted more than four-fifths of the decline in occupational physical activity over the 1991–2006 period for men and nearly two-thirds of the decline for women.19
Sedentary lifestyle has serious health and economic consequences.11, 20 CHNS reported that physical inactivity contributes to 12% to 19% of the risks associated with the five major NCDs in China, including coronary heart disease, stroke, hypertension, cancer, and type 2 diabetes. Physical inactivity is estimated to be responsible for more than 15% of the medical and non-medical yearly costs of the main NCDs in the country.21
Diet
The economic reform brought economic prosperity, a growing openness to international markets, and domestic policy changes to enhance agricultural productivity and end food rationing. Compared with data in early 1980s, the National Nutrition Surveys showed that Chinese are eating much more meat, dairy products, eggs, and edible oils, and eating much less grains and vegetables (see Table 2 for details).22 Dramatic changes in food patterns also have been confirmed in other studies.23–26 Studies in other countries and recent Chinese data support beneficial effect of diets with more fish, more vegetables and fruits, more coarse grains, and less fat and animal foods.27–29 China Kadoorie Biobank Study28 recently reported that as compared with participants who never or rarely consumed fresh fruit, those who ate fresh fruit daily had lower systolic blood pressure (by 4.0 mm Hg) and blood glucose levels (by 0.5 mmol/L). The adjusted hazard ratios for daily consumption versus nonconsumption were 0.60 (95% CI, 0.54 to 0.67) for cardiovascular death, and 0.66 (95% CI, 0.58 to 0.75), 0.75 (95% CI, 0.72 to 0.79), and 0.64 (95% CI, 0.56 to 0.74), respectively, for incident major coronary events, ischemic stroke, and hemorrhagic stroke. They also reported that the habitual consumption of spicy foods was inversely associated with total and certain cause specific mortality, independent of other risk factors of death.29 However, there are still lacking data from China on the relationship of foods or food patterns with CVD.
Table 2.
The changes of food pattern in China in the past decades, data from the National Nutrition Surveys in China, the average amount of each food group is given in grams per reference man per day
| Food groups | 1982 | 1992 | 2002 |
|---|---|---|---|
| Grains | 509.7 | 439.9 | 401.7 |
| Potato & tubers | 179.9 | 86.6 | 49.5 |
| Vegetables | 316.1 | 310.3 | 275.2 |
| Meat | 34.2 | 58.9 | 79.5 |
| Dairy | 8.1 | 14.9 | 26.3 |
| Eggs | 7.3 | 16.0 | 23.6 |
| Fish & sea foods | 11.1 | 27.5 | 30.1 |
| Edible oil | 18.2 | 29.5 | 41.1 |
| Salt | 12.7 | 13.9 | 12.0 |
| Soy sauce | 14.2 | 12.6 | 9.0 |
Data source: Chinese Journal of Cardiovascular Review 2004, 2(12):919–921.22
According to the China Industry Information report, beverage production in China increased from 26.2 million tons in 2004 to 167.05 million tons in 2014,30 and many of these products were sugar-sweetened. CHNS data from 9 provinces showed that the proportion of adults exposed to sugar-sweetened beverages increased from 15.1% to 29.3%. The average energy from added sugar and sugar-sweetened beverages also increased to 10.7% of the total energy intake, which exceeded the World Health Organization (WHO) and Food and Agriculture Organization recommendations.31 A recent meta-analysis on data from 32 678 children and 183 629 adults in 19 studies across the world showed that sugar-sweetened beverages significantly increase the risk of obesity (pooled OR:1.41, 95%CI: 1.12–1.76 for children; and 1.39, 95%CI: 1.07–1.80 for adults), indicating that increasing sugar-sweetened beverage consumption may contribute to poorer Chinese health.32
Another marked Chinese temporal trend is the increase of processed foods. First introduced by global food companies, the processed food sector has grown rapidly in China to meet the huge demand for better food quality, safety, and convenience. Using data from 14,976 participants at least two years of age in 2011, CHNS showed that 74.5% of participants consumed processed foods, excluding edible oils and other condiments, and 28.5% of participants’ total daily energy intake was from processed foods.33 The percentage of processed foods was 40.2% for children and teenagers in megacities. People who lived in megacities or highly urbanized neighborhoods with higher incomes and educational achievement consumed more processed foods.33 Further, the processed food purchases are growing at the rate of 50% per year.33 The high salt, high fat, high sugar, and other potential hazards often contained in processed foods, have concerning implications for the future.
Salt (sodium) intake
China has a long history of using salt to preserve and flavor foods, and the average salt intake is among the highest of all countries.34, 35 The most recent data announced by the National Health and Family Planning Commission indicated that the current average salt intake is about 10 grams per day, which is lower than what had been reported in previous national nutrition surveys (see Table 2), but still 2 fold the amount recommended by the WHO.36 Although the relations between salt and health can be traced back thousands of years to traditional Chinese medicine, the studies on the relationship between salt and hypertension took place in China mostly after 1980. The nutritional salt studies included single center and multi-center cross-sectional studies, cohort reexamination studies, and randomized trials in human subjects.37–59
Many of the salt studies were part of international collaborations examining the relations between sodium intake and blood pressure, including INTERSALT,35 CARDIAC,42 US-PRC Joint Study,40 INTERMAP,46, 47 and more recently CHNS.51, 52 The results were generally in agreement that dietary high sodium and low potassium intake were associated with high blood pressure. In contrast, the reduction of salt intake or replacing regular salt with salt substitute significantly reduced blood pressure among patients with hypertension or high cardiovascular risk.54–59 For example, the multivariable-adjusted data from three Chinese populations in the INTERMAP study showed that about 66% of the Chinese north-south difference in systolic blood pressure could be explained by differences in sodium and potassium intake between the regions.47 And about one third of the north-south difference in systolic blood pressure could be explained by the difference in sodium intake alone.47
Recently, a cluster randomized controlled trial found that an innovative school-based salt reduction education program reduced systolic blood pressure by 1.9 mmHg on average in parents.56 The China Salt Substitute Study demonstrated, among 608 individuals with high cardiovascular risk from rural northern China, after 12 months of intervention with salt substitute, systolic blood pressure was significantly reduced by 5.4 mm Hg (P=0.001) on average in comparison with the regular salt group.57 The blood pressure lowering effect of salt substitute has been reconfirmed in trials in patients with hypertension in other Chinese populations.58, 59 Based on data from the China Salt Substitute Study, using a salt substitute only among those with hypertension would reduce the number of cardiovascular events by 300,000 annually, and would save hundreds millions of medical costs.57 The evidence strongly argues for population salt reduction to be a national strategy for prevention and control of hypertension and CVD.
Alcohol intake
Alcohol drinking has a special role in Chinese life, being used as a tool for socializing.60 It is often an indispensable part of a meal or banquet in celebrating traditional festivals, weddings, birth of babies, moving into new houses, promotions, etc. Alcohol is also commonly used, particularly by men, as part of business meetings or social networking to maintain good relationships between partners and colleagues. As the economy developed, alcohol drinking increased dramatically in China.61 The average annual consumption of alcohol among Chinese people 15 years of age or older has increased progressively, from 0.4 litres of pure alcohol in 1952 to 2.5 litres in 1978 at the beginning of the economic reform, to 4.9 litres in 2009.62 A recent national survey revealed that 55.6% of the men and 15.0% of the women were current drinkers.63 Among respondents who endorsed alcohol consumption, 62.7% of the men and 51.0% of the women reported excessive drinking, and 57.3% and 26.6%, respectively, reported binge drinking.63
Cardiovascular health harms of alcohol drinking have been studied in China. Similar to other populations, moderate alcohol drinking was associated with a lower risk of CVD.64 However, excessive drinking alcohol was found significantly associated with a higher risk of stroke. Compared with non-drinkers, the relative risks of incident ischemic stroke for those who drank alcohol less than 5 g/d, 15 to 30 g/d, 30 to 60 g/d and above 60 g/d were 0.86 (95% confidence interval 0.57–1.27), 1.20 (0.87–1.65), 1.26 (0.86–1.84) and 1.96 (1.30–2.93), respectively.65
The great challenge now is how to get the Chinese people, particularly the poor, to adopt healthy lifestyles. A countervailing force is the allure of the unhealthy Western lifestyle, which has been an aspiration for many years because of very recent experiences of poverty.
Smoking
Smoking remains one of the most prevalent unhealthy behavioral risk factors in China. The total number of smokers in China are estimated over 300 million.66 In 2010, 52.9% of Chinese men but only about 2.4% of women smoked. Although first hand women smokers are uncommon, 3/4 women in rural and 1/2 women in urban regions were exposed to second hand smoking.67 It is estimated that 556 million individuals in China are exposed to second hand smoking.67 There have been multiple cohort, case-control, and meta-analytical studies showing that second hand smoke increases the risk of coronary heart disease by 25–30%.68, 69 It is interesting to observe the very low rate of smoking among Chinese women, and the expected rise in smoking in women after opening doors to western countries never materialized. Chinese culture discourages women from smoking.
The Chinese government has been gradually strengthening the policies against tobacco use, and the smoking rates are slowly but continuously declining.17, 70, 71 Recently, local laws to ban smoking in public places have been established in Beijing72 and other cities. Monitoring data show that second hand smoking has started to drop.73 The Chinese government raised tobacco taxes in 2015, from 49% to 56% of the retail price.74 However, the percentage is still relatively low compared to the WHO-recommended benchmark, which is about 70% of the retail price. Therefore, ample room remains for the Chinese government to further increase cigarette taxes.75,76
Changes in Environment
Industrialization has polluted water, air, and soil to a great extent. According to the China Environment Status Report 2012,11 underground water in 57.3% of cities had poor (cannot directly be used for drinking) or very poor quality (not usable as drinking water) according to the national quality standard for ground water.77 Of the 113 core cities 88.5% met the old but only 23.9% met the new standard of air quality.78 The new national ambient air quality standards set limits for PM2.5 at average 75μg/m3 in 24 hours, which is much higher than the WHO standards (25μg/m3)79 and those of the US (35μg/m3)80 Few Chinese cities can meet the international standards. It was estimated that 1 of 10 farmlands had been either polluted or destroyed by sewage or solid waste in 2006 and about 1200 tons of grains were polluted annually by heavy metals.81
There have been numerous epidemiological studies on air pollution and cardiovascular mortality in China, using time-series, case-crossover, or cross-sectional designs.82–87 The increased cardiovascular mortality risks observed in the Chinese population are similar in magnitude, per amount of pollution, to the risks found in other parts of the world.82 Recently, a randomized, double-blind crossover trial among 35 healthy college students in Shanghai found that air purification reduced mean systolic and diastolic BP significantly by 2.7% and 4.8% respectively in addition to decreases in several circulating inflammatory and thrombogenic biomarkers.88
As well as deteriorating cardiovascular health, ambient air pollution causes lung cancer, respiratory illness and symptoms, infant mortality as well as total mortality.89–92 In China, ambient air pollution was estimated to cause about 300 000 premature deaths in the year 2000 and more than 1.2 million in the year 2010.93 The economic cost of ambient air pollution-related disease burden is substantial, ranging from 8% to 16% of the city’s gross domestic product for a typical Chinese city.94
In China, chronic exposure to high concentrations of arsenic in drinking water was associated with peripheral vascular disease and hypertension, as well as non-vascular diseases.95
Increasing of Conventional CVD Risk Factors
Hypertension
As a consequence of the changes in lifestyle and environment, and population aging, major CVD risk factors have started to increase. The recent official prevalence of hypertension in China in 2012 was 25.2% among adults aged 20 years and above, about 5 fold of that in 1959.17 Figure 2 shows the remarkable increasing trend in both crude and age-standardized prevalence of hypertension in China over the past decades. The age-standardized national hypertension prevalence rate, according to the national standard population of 1964, increased from 7.5% in 1979–80 to 9.4% in 1991,96 then further to 12.4% in 2002 for population aged 15 years and above.97 These data clearly demonstrated that even if the rapid aging of the Chinese population did not happen Chinese people would be still at significant increased risk of developing hypertension. The increased risk mainly can be attributed to lifestyle changes, including increases in overweight and obesity, alcohol drinking, high salt intake, and mental stress.47, 96, 98–100 There are large disparities in hypertension prevalence between regions (Figure 3), generally higher in the north and lower in the south. The map of regional differences in prevalence of hypertension mirrors the regional differences in salt intake,43 overweight/obesity,17 and binge drinking63 as well as the regional differences in cardiovascular mortality.101
Figure 2.
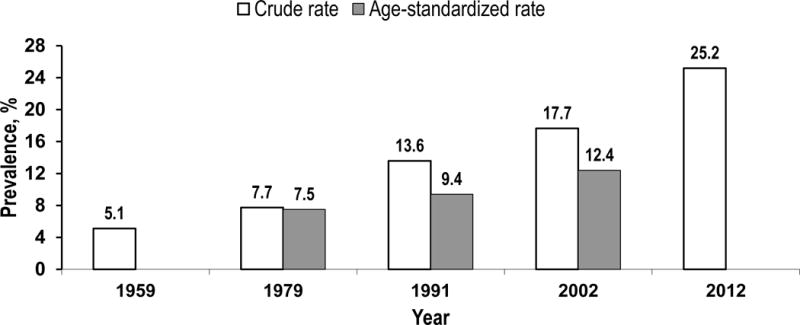
The increasing trend in prevalence of hypertension in China in the past decades, crude and age-standardized rate based on data from national hypertension surveys. Criteria of diagnosis: Not documented for the survey in 1959; SBP≥141mmHg and/or DBP≥91mmHg for the survey in 1979;96 SBP≥140 and/or DBP≥90 or medication use in 2 wks for the surveys in 199196 and 2002.97 Age of participants: Participants aged 15 years and above except for the survey in 2012, which was among adults age 20 and above.17 Age-standardized rate with the national census data in 1964 as reference. Same criteria as of 1979 survey was used.
Figure 3.

Map showing provincial differences in age-adjusted prevalence of hypertension in China in 199196
Dyslipidemia
With the rising standard of living, malnutrition has been greatly diminished, but over-nutrition has emerged as a new health problem and caused dramatic increases in obesity, diabetes, and dyslipidemia.17 The first nationally representative sample on serum lipids was from the China National Nutrition and Health Survey (CNNHS) organized by the Ministry of Health and implemented by China CDC in 2002, which showed that 2.9% of Chinese age 18 years and above had total cholesterol over 240 mg/dL.102 In 2007–08, a national survey conducted by the Chinese Society of Diabetes reported that 9.0% of Chinese adults age 20 years and older had total cholesterol over 240 mg/dL.103 Due to the differences in methodology, population demography and quality control measures, it is hard to judge the amount of the increase over the past decades. The only available comparable data on the secular trends of blood lipids among Chinese populations was from the Study on Trends of CVDs and Preventive Strategy, which was conducted as a series of cross-sectional surveys of population samples in 1982–84, 1992–94 and 1998 in the same 9 geographical locations and at the same age of 35 to 59 years. The result showed that the age-standardized rate (according to the world standard population) of high cholesterol (defined as total cholesterol ≥ 200 mg/dL) was 17.6% in early 1980s, 24.0% in early 1990s and 33.1% in the late 1990s (Figure 4).104
Figure 4.
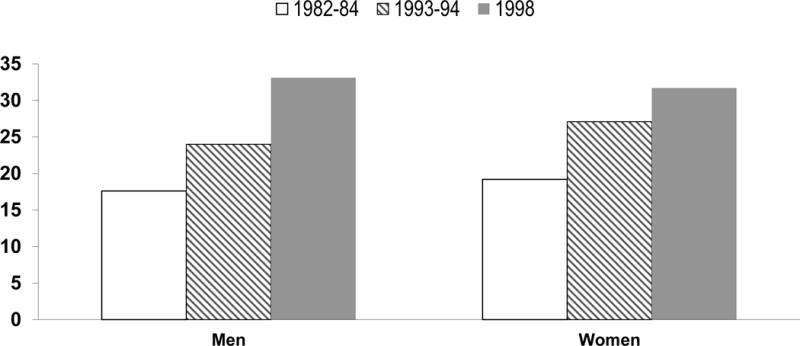
The increasing trend in high cholesterol (total cholesterol ≥ 200 mg/dL) in China in the past decades, age-standardized rate on pooling data from 9 populations at 35 to 59 years and with urban-rural and geographic diversity. Data source: Chinese Journal of Cardiology. 2001;29:74–79.104
Diabetes
There also have been large increases in the prevalence of type 2 diabetes. The first national diabetes survey conducted in 300,000 individuals from 14 provinces in 1980 reported a prevalence of 0.67%.105 The subsequent national surveys reported the prevalence of diabetes was 2.5% in 1994 and 5.5% in 2000–2001.106, 107 The CNNHS reported a prevalence of 2.6% in 2002.102 The Chinese Society of Diabetes national survey reported that the prevalence of diabetes was 9.7% in 2007,108 and the most recent national survey done in 2010 reported that the prevalence of diabetes was 11.6%, and the prevalence of prediabetes was 50.1% among Chinese adults. The prevalence rates translate into an estimated 113.9 million Chinese adults with diabetes and 493.4 million with prediabetes.109 It should be noted that sampling methods, screening procedures, diagnostic criteria as well as statistical methods varied considerably between surveys, which explains the large fluctuations over the period. The studies are not sufficiently comparable for a quantitative estimation of increasing temporal trends. However, the increase of type 2 diabetes in China is definitely evident.
Overweight and obesity
An alarming increase in overweight and obesity has been seen over the past decades, in both children and adults.110, 111 Using the Chinese criteria of overweight (BMI: 24.0–27.9 kg/m2) and obesity (BMI: ≥28 kg/m2),112 CNNHS reported that 22.8% of adults were overweight and 7.1% obese in 2002.102 In 2012, the corresponding rates increased to 30% and 12%, respectively. The prevalence of overweight and obesity were 9.6% and 6.4% in 2012 in children age 6–17 years old, an absolute increase of 5.1% and 4.3% respectively in comparison with that in 2002.17
More recently a global study used a spatial temporal regression model and Gaussian process regression to synthesize the time series cross-sectional data from multiple sources and years in China and reported the prevalence of overweight (BMI: 25.0–29.9 Kg/m2) and obesity (BMI: ≥30 Kg/m2) according to the WHO criteria.113 The results showed that from 1980 to 2013, overweight and obesity prevalence more than doubled in adults and more than tripled in youngsters (Figure 5).114 As the ratio of overweight to obesity was high, about 3 to 1, it is anticipated that many of these overweight persons may become obese in the near future. As a result of the rising prevalence of overweight and obesity the number of patients with hypertension, diabetes, and dyslipidemia is also projected to increase.
Figure 5.
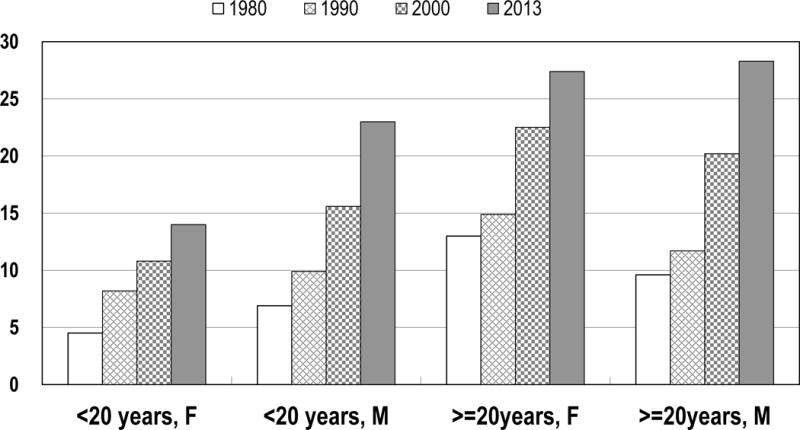
The increasing trend of overweight and obesity in China in the past decades, age-standardized rate (BMI>=25Kg/m2). Data source: Lancet 2014; 384(9945): 766–781.114
Increasing Pandemic of CVD
The increase in classical CVD risk factors has been followed by a major rise in the incidence and mortality of CVD. CVD has been the leading cause of death in both urban and rural areas since late 1980s. Further, the proportion of deaths due to cardiovascular causes has continued to increase. (Table 3) The increase in rural populations has been particularly large – and now CVD accounts for 40% of all deaths in both urban and rural populations, with more than 80% due to NCDs.7
Table 3.
Changing causes of death (%) in China: 1957–2012.
| Disease | 1957 | Urban | Rural | ||
|---|---|---|---|---|---|
| 1988 | 2012 | 1988 | 2012 | ||
| Infectious diseases | 7.9 | 1.5 | 0.7 | 2.3 | 0.9 |
| Tuberculosis | 7.5 | 1.5 | 0.3 | 3.0 | 0.3 |
| Heart disease | 6.6 | 15.1 | 21.5 | 11.4 | 18.1 |
| Stroke | 5.5 | 20.9 | 19.6 | 16.1 | 20.6 |
Data source: China annual health statistics reports7
Compared with the selected high-income and upper middle income countries, China now has similar rates of heart disease deaths, but much higher rates of death from stroke, of which 62% are ischemic, 30% hemorrhagic, and 8% unknown.115 The overall rate of cardiovascular death in China now far exceeds those of the upper income countries and is higher than those of the upper middle income countries as well. In particular, the rate of total cardiovascular death is almost three times higher than that of its neighbor Japan.116 (Figure 6)
Figure 6.
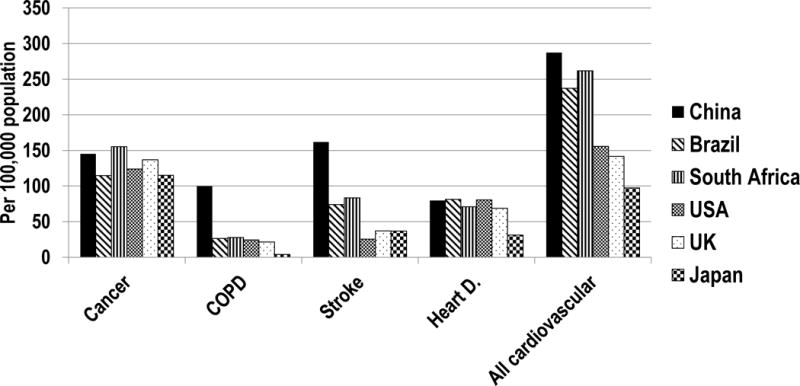
Age-standardized Mortality Rates from Major NCDs in China and Selected Upper and Upper Middle Income Countries. Data source: World Health Organization, Disease and injury country estimates
While maternal and infant mortality rates continue to decline, the recent increase in CVD death rates have actually caused a slight increase in total mortality recently after many decades of decline. It is anticipated that rising CVD death rates may also slow down the increase in life expectancy (Figure 7).1, 7 Looking to the future, the World Bank has projected that the prevalence of major NCDs in China will double or even triple over the next two decades, risking the possibility of a reversal in life expectancy if nothing changes.117
Figure 7.
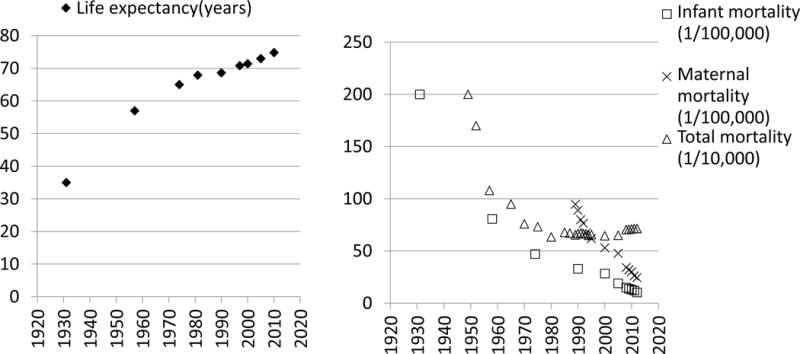
Changes in infant, maternal and total mortality and life expectancy in China from 1930 to 2012. Data source: National Bureau of Statistics1 and National Health and Family Planning Commission7
The Economic Impact
The economic consequences of the increasing disease burden from cardiovascular and other NCDs are likely to be substantial. The economic burden is particularly notable as China’s economy moves into a new stage and GDP growth rate has dropped from the rapid increase in the past decades. Even if the rapid increase of the economy remains at 9%, it is far below the increase in health costs. From 1987 to 2003, the overall health costs have increased annually by 12% on average118 and the cost of CVD care is increasing by around 18.6% per year.119 The National Bureau of Statistics data showed that the recent increase of health costs after 2003 was even faster, at 16.6% on average from 2004 to 2013, with the peak on 25% in 2008.120 Further expansion of the CVD epidemic is likely to have important adverse effects on economic development through increasing the direct and indirect health costs and loss of productive workers.
The precipitous increase in health costs is not only a problem for society as a whole but it is also a major problem for the individuals personally affected. Government healthcare spending has been increasing over 20% annually in the past decade. At the same time, private expenditures on health care accounts for more than a third of total costs and has been increasing at around 10% per year.121
The high personal expenditures on healthcare effects communities heterogeneously. For example, the average cost of a hospital admission of acute myocardial infarction in cardiology would cost about 77% of disposable annual per capita income in urban areas in 2011. By contrast, in the rural areas, the cost is 240% of annual per capita net income – i.e. 27 months of wages.7 Because healthcare costs are high relative to income in China, families face considerable economic hardship after developing CVD. Among 4739 3-month survivors of stroke in 62 hospitals across the country, 71% of patients had experienced catastrophic out-of-pocket expenditures.122
While China’s total economy is the second largest in the world, the per capita GDP ranks only 79,123 it is still home to vast numbers of people living in poverty. According to Chinese authorities, China still has over 70 million people living under the local poverty line (defined as 2300 Ren Min Bi (RMB) annual per capita net income in rural in 2010, equivalent to about 1 US Dollar per day),124 and the number would be over 250 and 800 million if the standard of poverty were raised to less than 2 and 5 US dollars a day, respectively according to the World Bank.125 The burden of CVD is the largest among individuals living in poverty.
Studies showed that cardiovascular risk factors were positively associated with socioeconomic status in early 1980s.126, 127 The relationship quickly became an inverse one in 1990s in urban cities,128 and recently studies generally have reported more prominent cardiovascular risk factors among participants with low socioeconomic status, such as less educated and rural residents.129, 130 These people often have no or inadequate health insurance. Without sufficient health insurance, the risk of experiencing catastrophic payments after major NCDs in China is very high. For example, for patients with acute stroke those without insurance incur 7 times the cost.122 With inadequate health insurance, poor patients used less outpatient services than richer ones.131 Socioeconomic inequality is contributing to health inequity. Therefore one major challenge is to provide acute care that is affordable for both society and individuals.
Challenges for the Healthcare System
The increasing pandemic of CVD and other major chronic diseases poses a number of major challenges for the healthcare system in various areas.
Primary care
The primary health care system cannot cope well with the CVD pandemic. For example, the majority of patients with hypertension, dyslipidemia, or type 2 diabetes are not aware of their condition, fewer are on treatment, and those well-controlled are rare;96, 97, 109, 132, 133 and there has been little improvement over time. The most updated data from a national survey in 2007–8 showed that among hypertensive patients, 45.0% were aware of their condition, 36.2% were treated, and 11.1% were adequately controlled.132 A recent meta-analysis with a total of 387,825 Chinese adults showed that the prevalence, awareness, treatment, and control rates of dyslipidemia were 41.9%, 24.4%, 8.8%, and 4.3%, respectively.133 The most recent national diabetes survey showed that only 25.8% of individuals with diabetes received treatment for the condition, and only 10.2% had adequate glycemic control.109 In contrast in the US, the awareness, treatment and control of hypertension were 80%, 73% and 50% in 2007–08,134 and 85.6% of diabetes patients were on treatment in 2012.135
Data from the Prospective Urban Rural Epidemiology (PURE) study136 showed that China was among the worst performing countries in the world in terms of secondary prevention. Among patients living in the communities participating in the PURE study,. less than 20% of people with coronary disease were taking an antiplatelet agent, and much smaller proportions were taking any of the other core components of standard secondary prevention care.
The poor performance of primary care system is largely due to the poor resources. In 2012, there were less than 0.7 million primary care providers in China. In contrast, 1.3 million doctors practiced in hospitals. Furthermore, 63.8% of physicians in hospitals had an undergraduate or graduate medical degree in 2012, but it was only 33.2% and 10% in primary care, respectively for urban and rural.7 The low capacity of primary care providers contributes to patients’ distrust and further prevents their access to primary care. For example, aware of the poorer quality of their health care, residents often bypass primary care facilities to seek care in the tertiary hospitals, leading to underuse of the former and overuse of the later.137 Both increase health costs. The overuse of hospital, particularly tertiary hospital services increases direct medical costs. The underuse of primary care leads providers to try multiple strategies to over use or misuse their services in order to maintain their earnings. It was estimated that one third of drugs dispensed in rural areas are counterfeit, enabling their vendors to earn huge markups.138 So, the challenge faced by China is how to strengthen the primary care system to improve both primary and secondary prevention of CVD.
Hospital care
Hospital care also poses a major challenge for China. Early data from WHO Multinational MONItoring of trends and determinants in CArdiovascular disease (MONICA) Project showed that the case fatality rate for coronary events were among the highest in the world. More than 60% of men and more than 80% of women died following an acute coronary event in early 1990s in Beijing, which has the most advanced and most ample health and medical care resources in China.139
In 2004 to 2005 the Clinical Pathways in Acute Coronary Syndrome in China (CPACS) Phase-1 study, a prospective registry established in 51 hospitals across the China, investigated the quality of hospital care provided to patients admitted with acute coronary syndromes. The results revealed that 2/3 of ST elevation myocardial infarction patients in China received no reperfusion therapy and fewer than half (48%) of patients were discharged on 4-drug combination therapy (antiplatelet, β-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, and statin), even though the participating hospitals were mainly large tertiary care centres.140, 141 The Bridging the Gap on CHD Secondary Prevention in China study confirmed the findings and reported a much worse situation among secondary hospitals.142
Additionally, 52% of acute coronary syndrome patients were discharged without appropriate secondary prevention.140, 141 A major contributor to the lack of secondary prevention was the frequent view (21% to 30%) of cardiologists that drugs such as statins, angiotensin-converting enzyme inhibitors and β-blockers were not indicated.141 It is therefore not surprising that surveys of hospitalized patients showed that very few patients meet national targets for cholesterol control.143
However, in contrast to the lack of secondary prevention, the number of percutaneous coronary intervention (PCI) has climbed steeply and continuously at an annual rate of 30% to 60% for the past decade, reaching more than half a million in 2012.143 The factors driving the increase includes the increasing incidence of myocardial infarction, the marketing of stent companies, and the competition among the hospitals due to inadequate funding from government, the pay-for-service policy, and higher profit margin for advanced technologies such as stents.144
But in the absence of adequate primary and secondary prevention, there are serious questions as to whether the proliferation of revascularization is appropriate. Despite an increase in the use of primary PCI among 12,264 acute ST elevation myocardial infarction patients in the recent China Patient-Centered Evaluative Assessment of Cardiac Events study,145 there was no significant change in the proportion of patients who failed to receive reperfusion and adjusted in-hospital mortality between 2001 and 2011. CPACS-1 has shown that patients at low risk were much more likely to receive PCI (25.1% in non-tertiary hospitals and 47.5% in tertiary hospitals) than those at high risk (9.7% in non-tertiary hospitals and 35.5% in tertiary hospitals).140 The inverse relation between disease severity and likelihood of revascularization may help to explain the dilemma regarding why the number of PCIs increased but mortality did not change. The government and society of cardiology should take actions to better regulate PCI practice in order to ensure maximizing the benefits to be gained from these expensive technologies.
Beyond the healthcare system
The challenges are far beyond the healthcare system. If population health is not included in other societal sectors’ agendas, the healthcare system will not completely succeed. For example, it is hard to ask people to exercise outdoor in polluted air. It is clearly beyond the ability of healthcare system to improve health through improving environment protection. But individuals need an unpolluted environment to have a healthy lifestyle. The greatest challenge is how to leverage the central leadership for coordinated whole government policies/actions.
China’s Opportunity and Responses
The challenges in China also create opportunities. One important opportunity that has arisen is the political realization that there are conflicts between various aspects of economic growth that has been achieved and sustainable development, social equity, and community harmony that are aspirations of the Chinese people. For example, China’s industrialization consumes tremendous natural resources, and pollutes the environment heavily. Ongoing pollution causes enormous disease burden and thus is being criticized widely by the public. The urbanization of economic development leaves families in rural settings having only children and elderly adults at home. Urbanization has created many social problems such as disparities in childhood education and elderly care, as well as more urban but unhealthy lifestyles and health inequities.146 The long-term economy-focused national development policy has led to uneven development of society and under-resourced healthcare system, resulting in common patients’ dissatisfaction and doctors injuries, as just one of many examples of disharmony.147 The realization of the conflicts has led to a political transition from the politics of GDP to the politics of people’s livelihood.148, 149 The new politics has already stimulated healthcare reforms designed to improve health care for the most disadvantaged groups in Chinese society.
Examples of new political approaches include the rapid development of the community health services system in urban China,150 the introduction of the new rural cooperative medical scheme (NRCMS),151 and the establishment of Basic Public Health Services Package152 and the National Essential Drugs List.153
In 1997, the central government decided to develop China’s community health services to optimize its healthcare system in order to meet the unmet needs by hospital services.150 The main required functions of the community health services centers include: disease prevention, basic medical services, health management, rehabilitation, health education, and family planning services. By 2013, there were 33,965 community health centers and clinics in urban area and another 221,065 health stations and 648,619 health clinics in rural area.7
By 2015, more than 95% of China’s population has some sort of basic medical insurance while the number was only 15% in 2000. The improved insurance rates are largely due to the introduction of the NRCMS, which was initiated in 2003 and covered 802 million (98.7% of its target population) in 2013.7 While there is still a lot of out of pocket expenditure on health care, with basic insurance coverage for all there is the potential for the benefits to grow. The growth is clearly indicated by the large increase in per capita compensation from the government for NRCMS. NRCMS started with about 8 USD (50 RMB) per capita in 2003 and quickly increased to about 60 USD (370 RMB) per capita in 2013.7
In 2009, China initiated a national program named Basic Public Health Services (BPHS) to provide community residents free basic public health services under 10 categories with an initial total budget of 15 RMB per capita.152 The services included establishing health records for all residents, community health education, elderly health management, chronic disease (hypertension and diabetes) management, etc. By 2014, the budget for BPHS had increased to 35 RMB per capita7, 50 and over 85 million patients with hypertension have been regularly managed through the program [informal communications with National Health and Family Planning Commission]. Studies found that patients with hypertension and diabetes had equal and high accessibility to BPHS with more than 90% of them receiving BPHS across socioeconomic status.154, 155 Individuals willing to receive services had the most positive results on effective management and control in blood pressure and blood glucose. But unsatisfactory quality of BPHS still exists; just 44% of individuals receiving BPHS had their blood pressure and glucose under control.155 A case from Rushan county in eastern China showed that among nearly 100 thousand patients with high blood pressure, 73% were managed through BPHS and 31% had blood pressure under control, which is far better than the national average control rate of 11%.132
The national basic drug list was initiated, as part of the new health care reform in 2009, to ensure the supply and safety of basic drugs and control of health care costs.156 The current version of the list includes 205 western medicines and 102 traditional Chinese medicines.153 The common generic antihypertensive medicines are included. The policy significantly increased the use of basic drugs at the beginning. For example, the use of basic drugs in 15 community health facilities in Zhongshan, China increased by 54%.157 However, whether the basic drug list enhanced the supply and safety of drugs while reducing healthcare expenditures remains unclear. A study based on a sample of primary health care facilities in 83 counties or cities nationwide showed variable and small reductions in inappropriate drug prescriptions and expenditure in facilities with an essential medicine program, but most of the changes were not statistically significant.158 A study reported that mean availability of essential medicines was low and further decreased from 2010 to 2012, particularly in primary hospitals (from 27·4% to 22·3% for lowest priced generics; p<0·0001).159 There are also reports of adverse events from using the essential medicines and shortage or delayed supply of the essential medicines due to corruption or inappropriate bidding for low prices.160–162 The problems indicate the need for better management of the national basic drug system.
In addition, National Action on Healthy Lifestyle for All was initiated in 2007 with the aim to promote healthy lifestyle across the country.163 Up to the end of 2014, the program was initiated in 2401 county/districts (77% of all) and created 32,989 health supporting environments including health schools, communities, canteens/restaurants, institutions, parks/gardens, streets, etc.164
The establishment of exercise facilities in communities across the country was initiated by the General Administration of Sports in 2000 as part of its National Plan on Public Exercise: Healthy Body for All.165
A few months after the UN High Level Meeting in 2011,166 China issued its first country level (not ministry level) national work plan in NCDs prevention and control.167 The plan was an important milestone in history, because it was the first time 15 ministries signed onto one document agreeing to work together on NCDs. The “whole-of-government and whole-of-society” policy adopted by the UN High Level Meeting166 has been well recognized and endorsed by Chinese government and was reflected in the plan.
As the effects of environment pollution have become increasingly apparent to the public, China also has become more serious about environment protection. In 2013, China initiated the Air Pollution Control Action Plan with the aim to reduce the inhaled particulate matter more than 10% in all cities across the country.168 On the first day of January 2015, the new Environment Protection Law was implemented.169 Also in 2015, the Plan for Water Pollution Prevention and Control in Key River Basin was implemented.170 The surface water with very poor quality dropped from 15.6% in 2010 to 8.8% in 2015, nationwide.170 Monitoring ambient air quality was established in 2015 in all 338 cities across the country with the capacity to monitor PM2.5 and other 5 major pollutants.170 In the 74 cities that implemented the new ambient air quality monitoring since 2012, the average concentration of PM2.5 decreased by 14.1% in 2015 in comparison with the previous year.170
Future Directions
Looking into the future, there are 4 policy priorities that should be further developed and implemented in China in order to prevent and control CVD as well as other NCDs and to improve the health of all Chinese (Table 4).
Table 4.
The four policy priorities that should be further developed and implemented in China
| 1. | The “whole-of-government and whole-of-society” policy should be the highest priority. Health cannot be limited to the health system alone |
| 2. | “Give priority to prevention” should be reinforced and implemented as an essential policy to guide all other policies and actions against NCDs |
| 3. | The health care system needs to be reformed to fit the nature of NCDs. The new health care system should be able to provide continuous life-long services rather than the current discontinuous and fragmented services. Priority should be given to primary care rather than hospital care, and the interventions should be more focused on communities rather than individuals |
| 4. | Research needs to be strengthened to develop evidence-based, low-cost, simple, sustainable and scalable interventions |
First, the “whole-of-government and whole-of-society” policy adopted by the UN High Level Meeting166 should be the number one priority. China faces challenges from increasing unhealthy lifestyles, environment pollution, disabled healthcare system, and backward policies that fundamentally drive the increased burden from CVD and other NCDs. To address the multiple challenges will require the strong leadership of the government and other nongovernmental entities. The responsibility for improved health care can no longer be left to the health system alone.
Second, “Give priority to prevention”, an old policy issued by Mao to fight against infectious diseases epidemic since the 1950s, should be implemented as an essential policy to guide all other policies and actions against NCDs. Under the original prevention policy, the incidence of acute infectious diseases significantly dropped from 20% in early 1950s to 203/100,000 in 1998,171 and life expectancy increased from about 35 years to nearly 70 years at the same time.172 China achieved these gains with very low average income during that time period; the available data showed that average per capita GDP increased from only 62 USD in 1978 to 1102 USD in 1998.173 The marked improvements were realized because infectious population prevention measures such as vaccination and environmental hygiene were much less expensive but more effective than treatment of individual patients.
With the new pandemic of CVD and other chronic diseases, the costly treatments with medicines and advanced technologies such as PCI are effective but not the optimal solution. Any policy that relies on costly treatments will either not be scalable or will increase health inequities, risking doing more harm than benefit. The WHO “best buys” for population-wide interventions that address risk factors are both effective and affordable, fitting well with Chinese “give priority to prevention’ policy, and should be reinforced for prevention and control of NCDs.174
Third, the healthcare system needs to be reformed to fit the nature of NCDs. NCDs have multiple social determinants, unfold chronically over the life course, and remain silent until acute life-threatening conditions emerge. NCDs often are not curable but are mostly controllable. The new health system should be able to provide continuous life-long services rather than the current discontinuous and fragmented services. Priority should be given to primary care rather than hospital care, and the interventions should be more focused on communities rather than individuals. Fortunately, strengthening primary care and reinforcing the public health system are included among the core components of the new healthcare reform.175 Increased access to essential public health services, essential drugs and healthcare services will be highly beneficial for the prevention and control of CVD.
Last, research needs to be strengthened to develop evidence-based, low-cost, simple, sustainable, and scalable interventions. Only interventions that meet these criteria are likely to result in substantive changes in the burden of CVD in China. The interventions that are most likely to meet these criteria include tobacco control and population salt reduction. Both interventions were listed as ‘best buys’ for the world by WHO for their effectiveness and low cost.176
In 1992, the Victoria Declaration177 stated “we have the scientific knowledge to create a world in which most heart disease and stroke could be eliminated”. In the present era we have much greater knowledge, but heart disease and stroke have yet to be eliminated. In China we have yet to fully implement population wide prevention. As was acknowledged when the declaration was signed, “The prescription is simple. To implement it is much more difficult.” In truth we do not have the knowledge to implement the prescription. We believe that research has a critical role to play in generating this knowledge. Unfortunately, many people including researchers themselves hold a belief that finding a way to implement knowledge is NOT research. We must shift the research agenda to focus on effective implementation of prevention at the population level.
The examples of implementation research in prevention and control of CVD in China include the Simplified Cardiovascular Management Study (SimCard),178 school based education programme to reduce salt intake in children and their families (School EduSalt),56 China Rural Health Initiative (CRHI)179, 180, CPACS,181, 182 China Da Qing Diabetes Prevention Study,183 etc.184 For example, the recently completed SimCard trial demonstrated that a simplified cardiovascular management program, only two drugs (anti-hypertensive and aspirin) and two lifestyle recommendations (smoking cessation and salt reduction), delivered by community health workers with the aid of a smartphone-based electronic decision support system, was effective178. The SimCard intervention significantly increased antihypertensive medication use by 25.5% and aspirin use by 17.1%, and reduced systolic blood pressure by –2.7 mm Hg for individuals at high cardiovascular risk in rural Tibet, China, and Haryana, India, both places with very scarce health care resources, in comparison with the control group.178 The School EduSalt trial demonstrated that a school-based health education program effectively reduced salt intake by about 25% in both children and adult family members and significantly reduced systolic blood pressure by 2.3 mmHg in adults in one school term. As the first successful randomized controlled trial on salt reduction by health education in the community, showed the great value of non-healthcare social sectors (here is the education system) and ‘health in all policies’ in prevention and control of CVD.56 Findings from these studies have generated much knowledge that is guiding policy making and clinical practice in China and other low-resource settings.
In summary, after several decades of rapid economic development China faces a huge and expanding pandemic of CVD, which poses challenges for both prevention and treatment. The challenges are not limited to the healthcare system but to the whole society, particularly in terms of healthy lifestyle and environment protection. Fortunately, realization of the challenges has been made. China has embarked on important initiatives such as primary care prioritized health reform, and multi-sector endorsed national NCDs work plan. China needs to pursue research that will expand knowledge necessary to implement innovative, practical, low cost, scalable interventions for both the prevention and treatment of CVD. China needs to implement these evidence-based interventions through the new healthcare reform program, under the direction of the whole government and whole society policy, giving priority to prevention. With these strategies we anticipate a reduction of cardiovascular mortality and morbidity in the coming decade.
Acknowledgments
We are very grateful to Prof. Keqin Rao for his creative ideas and suggestions that helped us to form the link between socioeconomic development and the increasing NCDs in China. We would like to thank Dr Wuxiang Xie, Ms Aoming Jin and Ms Amy Tu for their assisting in preparation of the manuscript.
Funding Sources: Dr. Wu is supported by 1R01MH100332; 1S07TW008833; and Dr. Benjamin is supported by 1R01HL128914; 2R01HL092577; 1P50HL120163.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.National Bureau of Statistics of People’s Republic of China. statistical bulletin of national economic and social development. 2014 Available at: http://www.stats.gov.cn/tjsj/tjgb/ndtjgb/index.html. Accessed July 20, 2015.
- 2.China’s GDP in 1949–2011. Available at: http://www.360doc.com/content/12/1112/18/4375009_247444369.shtml. Accessed July 20, 2015.
- 3.United Nations. Goal3: Ensure healthy lives and promote well-being for all at all ages. Available at: https://sustainabledevelopment.un.org/sdg3. Accessed December 22, 2015.
- 4.Bulletin of the Third Plenary Session of the Eleventh Central Committee of the Communist Party of China. Beijing. 1978 Dec 22; [Google Scholar]
- 5.National Bureau of Statistics of People’s Republic of China. China life expectancy. Available at: http://data.stats.gov.cn/easyquery.htm?cn=C01&zb=A0304&sj=2014. July 20, 2015.
- 6.Institute of Health Metrics and Evaluation. Life expectancy globally and in China. :1990–2013. Available at: http://www.healthdata.org/china. Accessed January 20, 2015.
- 7.National Health and Family Planning Commission of People’s Republic of China. Statistical bulletin on the development of health and family planning in 2013. Available at: http://www.nhfpc.gov.cn/guihuaxxs/s10742/201405/886f82dafa344c3097f1d16581a1bea2.shtml. Accessed July 20, 2015.
- 8.China population 2015. Available at: http://worldpopulationreview.com/countries/china-population. Accessed July 20, 2015.
- 9.United Nations, Department of economic and social affairs, population division. World Population Ageing 2013. ST/ESA/SER.A/348. Available at: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf. Accessed April 20, 2016.
- 10.Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, Remais JV. Urbanisation and health in china. Lancet. 2012;379:843–852. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ministry of Environmental Protection of the People’s Republic of China. The China Environment Status Report 2012. Available at: http://www.zhb.gov.cn/gkml/hbb/qt/201306/t20130604_253201.htm. Accessed July 20, 2015.
- 12.Oke O, Bhallac K, Loved DC, Siddiquia S. Tracking global bicycle ownership patterns. Journal of Transport & Health. 2015;2:490–501. [Google Scholar]
- 13.Bell AC, Ge K, Popkin BM. The road to obesity or the path to prevention: motorized transportation and obesity in China. Obes Res. 2002;10:277–283. doi: 10.1038/oby.2002.38. [DOI] [PubMed] [Google Scholar]
- 14.Xie G, Mai J, Zhao L, Liu X, Zhou B, Li Y, Wu Y. Physical activity status of working time and its change over a ten-year period in Beijing and Guangzhou populations. Journal of hygiene research. 2008;37:33–36. [PubMed] [Google Scholar]
- 15.Ng SW, Howard AG, Wang H, Su C, Zhang B. The physical activity transition among adults in China: 1991–2011. Obes Rev. 2014;15:27–36. doi: 10.1111/obr.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Center for Cardiovascular Diseases. Report on cardiovascular diseases in China. Encyclopedia of China Publishing House; 2007. [Google Scholar]
- 17.National Health and Family Planning Commission of People’s Republic of China. Report on status of nutrition and chronic diseases in China. 2015 Available at: http://www.nhfpc.gov.cn/xcs/s3574/201506/6b4c0f873c174ace9f57f11fd4f6f8d9.shtml. Accessed July 20, 2015.
- 18.Fan M, Lyu J, Guo Y, Bian Z, Yu C, Du H, Zhou H, Tan Y, Chen J, Chen Z, Li L. Regional differences on patterns of physical activity and leisure sedentary time: findings from the China Kadoorie Biobank study, including a million people from 10 regions. Zhonghua Liu Xing Bing Xue Za Zhi. 2015;36:779–785. [PubMed] [Google Scholar]
- 19.Ng SW, Norton EC, Popkin BM. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc Sci Med. 2009;68:1305–1314. doi: 10.1016/j.socscimed.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang X, Xie G, Zhang L, Li X, Zhao L, Li Y, Zhou B, Wu Y. Study on the baseline physical activity and the risk of ischemic cardiovascular disease. Chinese J Epidemiology. 2006;27:930–933. [PubMed] [Google Scholar]
- 21.Zhang J, Chaaban J. The economic cost of physical inactivity in China. Prev Med. 2013;56:75–78. doi: 10.1016/j.ypmed.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 22.Ministry of Health, Ministry of Science and Technoloy and National Bureau of Statistics of People’s Republic of China. The nutrition and health status of Chinese residents. Chinese Journal of Cardiovascular Review. 2004;2(12):919–921. [Google Scholar]
- 23.Dong F, Fuller F. Changing Diets in China’s Cities: Empirical Fact or Urban Legend? Center for Agricultural and Rural Development Iowa State University; Ames, Iowa: 2007. (Working Paper 06-WP 437). Available at: http://www.card.iastate.edu/iowa_ag_review/winter_07/article2.aspx. Accessed January 18, 2016. [Google Scholar]
- 24.Zhai F, Du S, Wang Z, Zhang J, Du W, Popkin BM. Dynamics of the Chinese diet and the role of urbanicity, 1991 to 2011. Obes Rev. 2014;15(Supplement S1):16–26. doi: 10.1111/obr.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao L, Hu J, Zheng R, Tian X, Ren F, Wu Y. The trend of dietary cholesterol intake and its food sources among workers and farmers in Beijing. Acta Nutrimenta Sinica. 2009;31:556–559. [Google Scholar]
- 26.Dennis B, Zhou B, Liu X, Yang J, Mai J, Cao T, Ni G, Zhao L. Trends in food, nutrient and energy intake in People’s Republic of China samples of urban and rural north and south adults surveyed in 1983–84 and resurveyed in 1987–88. Asia Pacific Journal Clinical Nutrition. 1997;6:277–286. [PubMed] [Google Scholar]
- 27.Anand SS, Hawkes C, Souza RJ, Mente A, Dehghan M, Nugent R, Zulyniak MA, Weis T, Bernstein AM, Krauss RM, Kromhout D, Jenkins DJ, Malik V, Martinez-Gonzalez MA, Mozaffarian D, Yusuf S, Willett WC, Popkin BM. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system. A report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015;66:1590–614. doi: 10.1016/j.jacc.2015.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Du H, Li L, Bennett D, Guo Y, Key TJ, Bian Z, Sherliker P, Gao H, Chen Y, Yang L, Chen J, Wang S, Du R, Su H, Collins R, Peto R, Chen Z, for the China Kadoorie Biobank Study Fresh Fruit Consumption and Major Cardiovascular Disease in China. N Engl J Med. 2016;374:1332–1343. doi: 10.1056/NEJMoa1501451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lv J, Qi L, Yu C, Yang L, Guo Y, Chen Y, Bian Z, Sun D, Du J, Ge P, Tang Z, Hou W, Li Y, Chen J, Chen Z, Li L, on behalf of the China Kadoorie Biobank collaborative group Consumption of spicy foods and total and cause specific mortality: population based cohort study. BMJ. 2015;351:h3942. doi: 10.1136/bmj.h3942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.China Industry Information. Beverage production in China in 2014. Available at: http://www.chyxx.com/industry/201508/333270.html. Accessed January 18, 2016.
- 31.Li D. Current status and trend in food and beverages containing added sugar in adults from 9 provinces in China from 1997 to 2009. China Center for Disease Control and Prevention; Beijing: 2014. p. R151.41. [Google Scholar]
- 32.Ding C, Guo H, Song C, Liu A. A meta-analysis of relationship between consumption of sugar-contained beverages and obesity and body weight change. Zhong Guo Man Xing Bing Yu Fang Yu Kong Zhi Za Zhi. 2015;7:506–511. [Google Scholar]
- 33.Zhou Y, Du S, Su C, Zhang B, Wang H, Popkin B. The food retail revolution in China and its association with diet and health. Food Policy. 2015;55:92–100. doi: 10.1016/j.foodpol.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988;297:319–328. doi: 10.1136/bmj.297.6644.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stamler R, Liu L, Nichols R, Huang D, Long Z, Xie J, Elliott P. Blood pressure and life style in the People’s Republic of China:three samples in the INTERSALT Study. J Hum Hyperten. 1993;7:429–435. [PubMed] [Google Scholar]
- 36.World Health Organization. Reducing salt intake in populations:report of a WHO forum and technical meeting; 5–7 October 2006; Paris, France. Available at: www.who.int/dietphysicalactivity/SaltReport-VC-April07. Accessed January 18, 2016. [Google Scholar]
- 37.Yan L, Li N, Wu Y. Salt Restriction and Challenges in China for Hypertension Control. Curr Cardiovasc Risk Rep. 2011;5:180–186. [Google Scholar]
- 38.Yan L, Li Y, Wu Y. Reducing salt intake for hypertension control: related evidence and recommendation on strategies in China. Chinese Journal of Epidemiology. 2011;32:1188–1192. [PubMed] [Google Scholar]
- 39.Liu L, Tao S, Lai S. Relationship between salt excretion and blood pressure in various regions of China. Bull WHO. 1984;62:255–260. [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou B, Wu X, Tao S, Yang J, Cao T, Zheng R, Tian X, Lu C, Miao H, Ye F, Zhu L, Zhu C, Jiang J, He H, Ma F, Du F, Wang B, for Collaborative Study Group for Cardiovascular Diseases and Their Risk Factors Dietary patterns in 10 groups and the relationship with blood pressure. Chin Med J (Engl) 1989;102:257–261. [PubMed] [Google Scholar]
- 41.Zhao L, Zhou B, Yang J, Zhang H, Wu Y. Association of food intake with blood pressure among different population. Chin J Prev Contr Chron Non-eommun Dis. 1996;4:155–159. [Google Scholar]
- 42.Liu L, Liu L, Ding Y, Huang Z, He B, Sun S, Zhao G, Zhang H, Miki T, Mizushima S, Ikeda K, Nara Y, Yamori Y. Ethnic and environmental differences in various markers of dietary intake and blood pressure among Chinese Han and three other minority peoples of China: results from the WHO Cardiovascular Diseases and Alimentary Comparison (CARDIAC) Study. Hyperten Res. 2001;24:315–322. doi: 10.1291/hypres.24.315. [DOI] [PubMed] [Google Scholar]
- 43.Xie J, Hao J, Liu L. Relationship between Urinary Electrolytes and blood pressure in 16 Regions of China. Chin J Hyperten. 2002;10:172–175. [Google Scholar]
- 44.Zhou B, Zhang X, Zhu A, Zhao L, Zhu S, Ruan L, Zhu L, Liang S. The relationship of dietary animal protein and electrolytes to blood pressure:a study on three Chinese populations. Int J Epidemiol. 1994;23:716–722. doi: 10.1093/ije/23.4.716. [DOI] [PubMed] [Google Scholar]
- 45.Tian H, Nan Y, Shao R, Dong Q, Hu G, Pietinen P, Nissinen A. Associations between blood pressure and dietary intake and urinary excretion of electrolytes in a Chinese population. J Hyperten. 1995;13:49–56. [PubMed] [Google Scholar]
- 46.Zhou B, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, Zhao L, Chan Q, Elliott P, for INTERMAP Research Group Nutrient intakes of middle-aged men and women in China,Japan,United Kingdom,and United States in the late 1990s:the INTERMAP Study. J Hum Hyperten. 2003;17:623–630. doi: 10.1038/sj.jhh.1001605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao L, Stamler J, Yan L, Zhou B, Wu Y, Liu K, Daviglus ML, Dennis BH, Elliott P, Ueshima H, Yang J, Zhu L, Guo D, for INTERMAP Research Group Blood pressure differences between northern and southern Chinese:role of dietary factors the international study on macronutrients and blood pressure. Hypertension. 2004;43:1332–1337. doi: 10.1161/01.HYP.0000128243.06502.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ma G, Zhou Q, Hu X. Relationship between salt consumption and hypertension in Chinese people. Chin J Prev Contr Chron Non-commun Dis. 2008;16:441–444. [Google Scholar]
- 49.Klag MJ, He J, Coresh J, Whelton P, Chen J, Mo J, Qian M, Mo P, He G. The contribution of urinary cations to the blood pressure differences associated with migration. Am J Epidemiol. 1995;142:295–303. doi: 10.1093/oxfordjournals.aje.a117635. [DOI] [PubMed] [Google Scholar]
- 50.Wu Y, Cai R, Zhou B, Xu X. Effects of genetic factors and dietary electrolytes on blood pressure of rural secondary school students in Hanzhong. Chin Med Sci J. 1991;6:148–152. [PubMed] [Google Scholar]
- 51.Batis C, Gordon-Larsen P, Cole SR, Du S, Zhang B, Popkin B. Sodium Intake and Incident Hypertension among Chinese Adults: Estimated Effects Across Three Different Exposure Periods. Epidemiology. 2013;24:410–418. doi: 10.1097/EDE.0b013e318289e047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Du S, Neiman A, Batis C, Wang H, Zhang B, Zhang J, Popkin B. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;99:334–343. doi: 10.3945/ajcn.113.059121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yan L, Bi Z, Tang J, Wang L, Yang Q, Guo X, Cogswell M, Zhang X, Hong Y, Engelgau M, Zhang J, Elliott P, Angell S, Ma J. Relationships Between Blood Pressure and 24-Hour Urinary Excretion of Sodium and Potassium by Body Mass Index Status in Chinese Adults. The Journal of Clinical Hypertension. 2015;17:916–25. doi: 10.1111/jch.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu Y, Wu X, Zhou B. Salt reduction in 16 farmer families and its effect on blood pressure. Chin Circulation J. 1994;9:347–349. [Google Scholar]
- 55.Wu X, Cao T, Zhu Y. Effects of dletary pattern modification on blood pressure over in a work site intervention program. Chin J Cardiol. 1999;27:22–25. [Google Scholar]
- 56.He F, Wu Y, Feng X, Ma J, Ma Y, Wang H, Zhang J, Yuan J, Lin CP, Nowson C, MacGregor G. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ. 2015;350:h770. doi: 10.1136/bmj.h770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.China Salt Substitute Study Collaborative Group. Salt substitution:a low-cost strategy for blood pressure control among rural Chinese. A randomized,controlled trial. J Hyperten. 2007;25:2011–2018. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 58.Zhao X, Yin X, Li X, Yan L, Lam C, Li S, He F, Xie W, Sang B, Luobu G, Ke L, Wu Y. Using a Low-Sodium, High-Potassium Salt Substitute to Reduce Blood Pressure among Tibetans with High Blood Pressure: A Patient-Blinded Randomized Controlled Trial. PLoS ONE. 2014;9:e110131. doi: 10.1371/journal.pone.0110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou B, Wang H, Wang W, Wu X, Fu L, Shi J. Long-term effects of salt substitution on blood pressure in a rural North Chinese population. Journal of Human Hypertension. 2013;27:427–433. doi: 10.1038/jhh.2012.63. [DOI] [PubMed] [Google Scholar]
- 60.Cochrane J, Chen H, Conigrave K, Hao W. Alcohol use in China. Alcohol Alcohol. 2003;38:537–542. doi: 10.1093/alcalc/agg111. [DOI] [PubMed] [Google Scholar]
- 61.Tang Y, Xiang X, Wang X, Cubells J, Babor T, Hao W. Alcohol and alcohol-related harm in China: policy changes needed. Bulletin of the World Health Organization. 2013;91:270–276. doi: 10.2471/BLT.12.107318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hao W, Chen H, Su Z. China: alcohol today. Addiction. 2005;100:737–741. doi: 10.1111/j.1360-0443.2005.01036.x. [DOI] [PubMed] [Google Scholar]
- 63.Li Y, Jiang Y, Zhang M, Yin P, Wu F, Zhao W. Drinking behaviour among men and women in China: the 2007 China Chronic Disease and Risk Factor Surveillance. Addiction. 2011;106:1946–1956. doi: 10.1111/j.1360-0443.2011.03514.x. [DOI] [PubMed] [Google Scholar]
- 64.Bazzano L, Gu D, Reynolds K, Chen J, Wu X, Chen C, Duan X, Chen J, He J. Alcohol consumption and risk of coronary heart disease among Chinese men. Int J Cardiol. 2009;135:78–85. doi: 10.1016/j.ijcard.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang L, Zhao L, Zhou B, Yang J, Li Y, Wu Y. Alcohol consumption and incidence of ischemic stroke in male Chinese. Chin J Epidemiol. 2004;25:954–957. [PubMed] [Google Scholar]
- 66.Li Q, Hsia J, Yang G. Prevalence of Smoking in China in 2010. N Engl J Med. 2011;364:2469–2470. doi: 10.1056/NEJMc1102459. [DOI] [PubMed] [Google Scholar]
- 67.Xiao L, Yang Y, Li Q, Wang C, Yang G. Population-based survey of secondhand smoke exposure in China. Biomed Environ Sci. 2010;23:430–436. doi: 10.1016/S0895-3988(11)60003-2. [DOI] [PubMed] [Google Scholar]
- 68.Dunbar A, Gotsis W, Frishman W. Second-Hand Tobacco Smoke and Cardiovascular Disease Risk An Epidemiological Review. Cardiology in Review. 2012;21:94–100. doi: 10.1097/CRD.0b013e31827362e4. [DOI] [PubMed] [Google Scholar]
- 69.He Y, Lam T, Jiang B, Wang J, Sai X, Fan L, Li X, Qin Y, Hu F. Passive Smoking and Risk of Peripheral Arterial Disease and Ischemic Stroke in Chinese Women Who Never Smoked. Circulation. 2008;118:1535–1540. doi: 10.1161/CIRCULATIONAHA.108.784801. [DOI] [PubMed] [Google Scholar]
- 70.The CPC Central Committee and the general office of the State Council. The circular on the leading cadres to take the lead in public places to ban smoking in public places. Beijing: Dec 2013, [Google Scholar]
- 71.China News. China intends to legislate all indoor public places no smoking. 2014 Nov 24; Available at: http://www.chinanews.com/gn/2014/11–24/6809399.shtml. Accessed January 18, 2016.
- 72.The Standing Committee of the fourteenth Beijing Municipal People’s Congress. The Beijing municipal control smoking regulation. Adopted on November 28, 2014 by and officially implemented in June 1, 2015. [Google Scholar]
- 73.China Center for Disease Control and Prevention. 2015 China Adult Tobacco Survey Report. Beijing: Dec 28, 2015. [Google Scholar]
- 74.Hu TW, Zhang X, Zheng R. China has raised the tax on cigarettes: what’s next? Tob Control. 2015;0:1–3. doi: 10.1136/tobaccocontrol-2015-052534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Meyers D, Neuberger J, He J. Cardiovascular Effect of Bans on Smoking in Public Places: A Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2009;54:1249–1255. doi: 10.1016/j.jacc.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 76.Gulland A. Countries should raise taxes on tobacco, says WHO. BMJ. 2015;351:h3691. doi: 10.1136/bmj.h3691. [DOI] [PubMed] [Google Scholar]
- 77.National Technical Supervision Bureau. People’s Republic of China Groundwater Quality Standard(GB/T 14848-93) Issued on December 30, 1993 and implemented on October 1, 1994. [Google Scholar]
- 78.Ministry of Environment Protection and National Technical Supervision Bureau. People’s Republic of China Ambient air quality standards(GB 3095-2012) Issued on Feburary 29, 2012 and implemented on January 1, 2016. [Google Scholar]
- 79.World Health Organization. Air quality guidelines. Global update 2005. Particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Available at: http://www.euro.who.int/en/health-topics/environment-and-health/Housing-and-health/publications/pre-2009/air-quality-guidelines.-global-update-2005-particulate-matter,-ozone,-nitrogen-dioxide-and-sulfur-dioxide. Accessed January 18, 2016. [PubMed]
- 80.US EPA. National Ambient Air Quality Standards (NAAQS) Available at: http://www3.epa.gov/ttn/naaqs/. Accessed January 18, 2016.
- 81.Ministry of Environmental Protection of the People’s Republic of China. Soil pollution in China. Available at: http://sts.mep.gov.cn/trhjbh/qgtrxzdc/200607/t20060720_91677.htm. Accessed July 20, 2015.
- 82.Kan H, Huang W, Chen B, Zhao N. Impact of outdoor air pollution on cardiovascular health in Mainland China. CVD Prevention and Control. 2009;4:71–78. [Google Scholar]
- 83.Xu M, Guo Y, Zhang Y, Westerdahl D, Mo Y, Liang F, Pan X. Spatiotemporal analysis of particulate air pollution and ischemic heart disease mortality in Beijing, China. Environmental Health. 2014;13:109. doi: 10.1186/1476-069X-13-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li G, Zhou M, Zhang Y, Cai Y, Pan X. Seasonal effects of PM10 concentrations on mortality in Tianjin, China: a time-series analysis. J Public Health. 2013;21:135–144. [Google Scholar]
- 85.Chen R, Samoli E, Wong CM, Huang W, Wang Z, Chen B, Kan H. Associations between short-term exposure to nitrogen dioxide and mortality in 17 Chinese cities: the China Air Pollution and Health Effects Study (CAPES) Environ Int. 2012;45:32–38. doi: 10.1016/j.envint.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 86.Zhang A, Qi Q, Jiang L, Zhou F, Wang J. Population exposure to PM2.5 in the urban area of Beijing. PLoS One. 2013;8:e63486. doi: 10.1371/journal.pone.0063486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xie W, Li G, Zhao D, Xie X, Wei Z, Wang W, Wang M, Li G, Liu W, Sun J, Jia Z, Zhang Q, Liu J. Relationship between fine particulate air pollution and ischaemic heart disease morbidity and mortality. Heart. 2015;101:257–263. doi: 10.1136/heartjnl-2014-306165. [DOI] [PubMed] [Google Scholar]
- 88.National Research Council (US) Subcommittee on Arsenic in Drinking Water. Arsenic in Drinking Water. Washington (DC): National Academies Press (US); 1999. [PubMed] [Google Scholar]
- 89.Chen R, Zhao A, Chen H, Zhao Z, Cai J, Wang C, Yang C, Li H, Xu X, Ha S, Li T, Kan H. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: a randomized, double-blind crossover trial of air purifiers. J Am Coll Cardiol. 2015;65:2279–2287. doi: 10.1016/j.jacc.2015.03.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pope C, III, Dockery D. Health Effects of Fine Particulate Air Pollution: Lines that Connect. Air & Waste Manage Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 91.Huang C, Yu H, Koplan J. Can China diminish its burden of non-communicable diseases and injuries by promoting health in its policies, practices, and incentives? Lancet. 2014;384:783–792. doi: 10.1016/S0140-6736(14)61214-9. [DOI] [PubMed] [Google Scholar]
- 92.Saikawa E, Naik V, Horowitz L, Liu J, Mauzerall D. Present and potential future contributions of sulfate, black and organic carbon aerosols from China to global air quality, premature mortality and, radiative forcing. Atmospheric Environment. 2009;43:2814–2822. [Google Scholar]
- 93.Zhang J, Mauzerall D, Zhu T, Liang S, Ezzati M, Remais JV. Environmental health in China: challenges to achieving clean air and safe water. Lancet. 2010;375:1110–1119. doi: 10.1016/S0140-6736(10)60062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cohen A, Ross A, Ostro B, Pandey K, Krzyzanowski M, Kunzli N, Gutschmidt K, Arden Pope, Romieu I, Samet J, Smith K. The global burden of disease due to outdoor air pollution. J Toxicol Environ Health A. 2005;68:1301–1307. doi: 10.1080/15287390590936166. [DOI] [PubMed] [Google Scholar]
- 95.Wang X, Mauzerall D. Evaluating Impacts of Air Pollution in China on Public Health: Implications for Future Air Pollution and Energy Policies. Atmospheric Environment. 2006;40:1706–1721. [Google Scholar]
- 96.National Blood Pressure Survey Cooperative Group. Prevalence and developemt of hypertension in China. Chinese Journal of Hypertension. 1995;3(suppl):7–13. [Google Scholar]
- 97.Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, Woodward M, Li X, Chalmers J, Gao R, Kong L, Yang X. Prevalence, awareness, treatment, and control of hypertension in China: Data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 98.Wu X, Wu Y, Zhou B, Tao S, Shen L, Wang S, Zhu S, Xu X, Yang R, Du F, Wang Y, He H, Xia S, Ruan L. The incidence of hypertension and associated factors in 10 population groups of China. Natl Med J China. 1996;76:24–29. [PubMed] [Google Scholar]
- 99.Hu B, Liu X, Yin S, Fan H, Feng F, Yuan J. Effects of Psychological Stress on Hypertension in Middle-Aged Chinese: A Cross-Sectional Study. PLoS ONE. 2015;10:e0129163. doi: 10.1371/journal.pone.0129163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Greenstadt L, Yang L, Shapiro D. Caffeine, mental stress, and risk for hypertension: a cross-cultural replication. Psychosom Med. 1988;50:15–22. doi: 10.1097/00006842-198801000-00003. [DOI] [PubMed] [Google Scholar]
- 101.Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, Li Y, Wang L, Liu Y, Yin P, Liu J, Yu S, Tan F, Barber RM, Coates MM, Dicker D, Fraser M, Gonzalez-Medina D, Hamavid H, Hao Y, Hu G, Jiang G, Kan H, Lopez AD, Phillips MR, She J, Vos T, Wan X, Xu G, Yan LL, Yu C, Zhao Y, Zheng Y, Zou X, Naghavi M, Wang Y, Murray CJ, Yang G, Liang X. Cause-specific mortality for 240 causes in china during 1990–2013: A systematic subnational analysis for the global burden of disease study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 102.Wong LD, editor. The 2002 China National Nutrition and Health Survey (1): General Report. People Health Publishing House; Beijing: 2005. [Google Scholar]
- 103.Yang W, Xiao J, Yang Z, Ji L, Jia W, Weng J, Lu J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. China National Diabetes and Metabolic Disorders Study Investigators. Serum lipids and lipoproteins in Chinese men and women. Circulation. 2012;125:2212–2221. doi: 10.1161/CIRCULATIONAHA.111.065904. [DOI] [PubMed] [Google Scholar]
- 104.The Collaborative Study Group on Trends of Cardiovascular Disease in China and Preventive Strategy. Current status of major cardiovascular risk factors in Chinese populations and their trends in the past two decades. Chinese Journal of Cardiology. 2001;29:74–79. [Google Scholar]
- 105.National Diabetes Research Group. A mass survey of diabetes mellitus in a population of 300,000 in 14 provinces and municipalities in China. Zhonghua Nei Ke Za Zhi. 1981;20:678–683. [PubMed] [Google Scholar]
- 106.Pan X, Yang W, Li G, Liu J. Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care. 1997;20:1664–1669. doi: 10.2337/diacare.20.11.1664. [DOI] [PubMed] [Google Scholar]
- 107.Gu D, Reynolds K, Duan X, Xin X, Wu X, Mo J, Whelton P, He J. Prevalence of diabetes and impaired fasting glucose in the Chinese adult population. Diabetologia. 2003;46:1190–1198. doi: 10.1007/s00125-003-1167-8. [DOI] [PubMed] [Google Scholar]
- 108.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 109.Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, Xu M, Li Y, Hu N, Li J, Mi S, Chen CS, Li G, Mu Y, Zhao J, Kong L, Chen J, Lai S, Wang W, Zhao W, Ning G. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 110.Wu Y. Overweight and obesity in China. BMJ. 2006;333:362–363. doi: 10.1136/bmj.333.7564.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Obesity: A growing threat to health in china. Lancet. 2014;384:716. doi: 10.1016/S0140-6736(14)61421-5. [DOI] [PubMed] [Google Scholar]
- 112.Department of Disease Control Ministry of Health, PR China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36. [PubMed] [Google Scholar]
- 113.World Health Organization. Obesity and overweight. Available at: http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed January 18, 2016.
- 114.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhang L, Yang J, Hong Z, Yuan G, Zhou B, Zhao L, Huang Y, Chen J, Wu Y, for the Collaborative Group of China Multicenter Study of Cardiovascular Epidemiology Proportion of Different Subtypes of Stroke in China. Stroke. 2003;34:2091–2096. doi: 10.1161/01.STR.0000087149.42294.8C. [DOI] [PubMed] [Google Scholar]
- 116.WHO Department of Measurement and Health Information. Disease and injury country estimates. Available at: http://www.who.int/healthinfo/global_burden_disease/estimates_country/en. Accessed July 20, 2015.
- 117.World Bank. (World Bank Report Number 62318-cn).Toward a healthy and harmonious life in China: Stemming the rising tide of non-communicable diseases. Available at: http://documents.worldbank.org/curated/en/2011/07/14639951/toward-healthy-harmonious-life-china-stemming-rising-tide-non-communicable-diseases. Accessed July 20, 2015.
- 118.Yu D. Analysis on health costs in China. Chinese Health Economics Magazine. 2005;24:5–7. [Google Scholar]
- 119.Hu D. Thinking on the prevention, treatment and patient rehabilitation of cardiovascular disease in China. Chinese Journal of Practical Internal Medicine. 2013;33:253–255. [Google Scholar]
- 120.National Bureau of Statistics of People’s Republic of China. Health cost in China. Available at: http://data.stats.gov.cn/easyquery.htm?cn=C01&zb=A0O0K&sj=2014. Accessed July 20, 2015.
- 121.National Bureau of Statistics of People’s Republic of China. Private expenditure on health care. Available at: http://data.stats.gov.cn/adv.htm?m=advquery&cn=C01. Accessed July 20, 2015.
- 122.Heeley E, Anderson C, Huang Y, Jan S, Li Y, Liu M, Sun J, Xu E, Wu Y, Yang Q, Zhang J, Zhang S, Wang J, for the ChinaQUEST Investigators Role of Health Insurance in Averting Economic Hardship in Families After Acute Stroke in China. Stroke. 2009;40:2149–2156. doi: 10.1161/STROKEAHA.108.540054. [DOI] [PubMed] [Google Scholar]
- 123.World Bank. GDP per capita (current US$) Available at: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD?display=default. Accessed July 20, 2015.
- 124.Baidu baike. China’s standard of poverty. Available at: http://baike.baidu.com/link?url=gYWmIr9wjvy7pd3Gxmq548m9FQhMa-Br50U9chDhL3FsOulfmAoYynTlCAR4Wv6jG2-YpM5piIC4Kz52SoLMHK. Accessed January 18, 2016.
- 125.World Bank. Poverty & Equity. Available at: http://povertydata.worldbank.org/poverty/country/CHN. Accessed July 20, 2015.
- 126.Molarius A, Seidell J, Sans S, Tuomilehto J, Kuulasmaa K, for the WHO MONICA Project Educational Level, Relative Body Weight, and Changes in Their Association Over 10 Years: An International Perspective From the WHO MONICA Project. American Journal of Public Health. 2000;90:1260–1268. doi: 10.2105/ajph.90.8.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yu Z, Nissinen A, Vartiainen E, Song G, Guo Z, Tian H. Changes in cardiovascular risk factors in different socioeconomic groups: seven year trends in a Chinese urban population. J Epidemiol Community Health. 2000;54:692–696. doi: 10.1136/jech.54.9.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yu Z, Nissinen A, Vartiainen E, Song G, Guo Z, Zheng G, Tuomilehto J, Tian H. Associations between socioeconomic status and cardiovascular risk factors in an urban population in China. Bulletin of the World Health Organization. 2000;78:1296–1305. [PMC free article] [PubMed] [Google Scholar]
- 129.Gao B, Zhang L, Wang H, on behalf of the China National Survey of Chronic Kidney Disease Working Group Clustering of Major Cardiovascular Risk Factors and the Association with Unhealthy Lifestyles in the Chinese Adult Population. PLoS ONE. 2013;8:e66780. doi: 10.1371/journal.pone.0066780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhan Y, Yu J, Chen R, Gao J, Ding R, Fu Y, Zhang L, Hu D. Socioeconomic status and metabolic syndrome in the general population of China: a cross-sectional study. BMC Public Health. 2012;12:921. doi: 10.1186/1471-2458-12-921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dou L, Liu X, Zhang T, Wu Y. Health care utilization in older people with cardiovascular disease in China. International Journal for Equity in Health. 2015;14:59. doi: 10.1186/s12939-015-0190-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gao Y, Chen G, Tian H, Lin L, Lu J, Weng J, Jia W, Ji L, Xiao J, Zhou Z, Ran X, Ren Y, Chen T, Yang W. Prevalence of hypertension in China: A cross-sectional study. PLoS ONE. 2013;8:e65938. doi: 10.1371/journal.pone.0065938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Population Health Metrics. 2014;12:28. doi: 10.1186/s12963-014-0028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 135.The US CDC. National Diabetes Statistics Report, 2014. Available at: http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed April 20, 2016.
- 136.Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, Gupta R, Kelishadi R, Iqbal R, Avezum A, Kruger A, Kutty R, Lanas F, Lisheng L, Wei L, Lopez-Jaramillo P, Oguz A, Rahman O, Swidan H, Yusoff K, Zatonski W, Rosengren A, Teo KK, Prospective Urban Rural Epidemiology Study I Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): A prospective epidemiological survey. Lancet. 2011;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 137.Blumenthal D, Hsiao WC. Privatization and Its Discontents — The Evolving Chinese Health Care System. N Engl J Med. 2005;353:1165–1170. doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 138.Hsiao WC. Disparity in health: the underbelly of China’s economic development. Harv China Rev. 2004;5:64–70. [Google Scholar]
- 139.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 140.Gao R, Patel A, Gao W, Hu D, Huang D, Kong L, Qi W, Wu Y, Yang Y, Harris P, Algert C, Groenestein P, Turnbull F, Investigators C Prospective observational study of acute coronary syndromes in China: Practice patterns and outcomes. Heart. 2008;94:554–560. doi: 10.1136/hrt.2007.119750. [DOI] [PubMed] [Google Scholar]
- 141.Bi Y, Gao R, Patel A, Su S, Gao W, Hu D, Huang D, Kong L, Qi W, Wu Y, Yang Y, Turnbull F, Investigators C Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: Results from the Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study. Am Heart J. 2009;157:509–516. doi: 10.1016/j.ahj.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 142.Guo L, Wang J, Zhao D, Liu J, Liu J, Zhang H, Xing L, Sun J, Wang M. Current clinical practice and guideline application in therapies of ST segment elevation ACS inpatient in a multi-provincial study in China: results of BRIG project. Heart. 2010;96(Suppl 3):A81–A82. [Google Scholar]
- 143.The collaborative research group for the second multi-center survey of clinical management of dyslipidemia in China. The second multi-center survey of dyslipidemia management in China: goal attainment rate and related factors. Chinese Journal of Cardiology. 2007;35:420–427. [PubMed] [Google Scholar]
- 144.The coronry stent market in China. Available at: http://news.39.net/mtpl/2012222/1978515.html. Accessed July 20, 2015.
- 145.Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi F, Spertus J, Krumholz H, Jiang L. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2015;385:441–451. doi: 10.1016/S0140-6736(14)60921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li M, Wu Y, editors. Urbanization and health in China. New Jersey: Imperial College Press; 2015. [Google Scholar]
- 147.The Lancet. Violence against doctors: Why China? Why now? What next? Lancet. 2014;383(9922):1013. doi: 10.1016/S0140-6736(14)60501-8. [DOI] [PubMed] [Google Scholar]
- 148.“Livelihood” become “major political issues” of National People’s Congress and Chinese People’s Political Consultative Conference, Chinese people’s livelihood political speed up. Available at: http://www.chinanews.com/gn/2011/03-10/2897757.shtml. Accessed July 20, 2015.
- 149.People’s livelihood is the biggest politics. Available at: http://news.gmw.cn/2014-03/07/content_10603378.htm. Accessed July 20, 2015.
- 150.CPC Central Committee and the State Council. Decision on health reform and development. 1997 Jan 15; Available at: http://www.moh.gov.cn/wsb/pM30115/200804/18540.shtml. Accessed July 20, 2015.
- 151.CPC Central Committee and the State Council. Decision on further strengthening the work of rural health. 2002 Oct 19; Available at: http://www.gov.cn/gongbao/content/2002/content_61818.htm. Accessed July 20, 2015.
- 152.National Health and Family Planning Commission of People’s Republic of China. Notice on the work of the national basic public health service project in 2014. Available at: http://www.nhfpc.gov.cn/jws/s3577/201409/acaeab089ac44d7a87d38393ccec4a78.shtml. Accessed July 20, 2015.
- 153.China Food and Drug Administration. Notice on printing and distribution of The Implementation Guidance on the Establishment of the National Essential Drug List System. Available at: http://www.sda.gov.cn/WS01/CL0056/40753.html. Accessed July 20, 2015.
- 154.Zhou D, Feng Z, He S, Sun X, Ma C, Lv B, Zou X. Equity of the essential public health service in rural China: Evidence from a nationwide survey of hypertensive patients. Pak J Med Sci. 2013;29:1012–1017. doi: 10.12669/pjms.294.3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tian M, Wang H, Tong X, Zhu K, Zhang X, Chen X. Essential Public Health Services’ Accessibility and its Determinants among Adults with Chronic Diseases in China. PLoS ONE. 2015;10:e0125262. doi: 10.1371/journal.pone.0125262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Barber S, Huang B, Santoso B, Laing R, Paris V, Wu C. The reform of the essential medicines system in China: a comprehensive approach to universal coverage. Viewpoints. 2013;3:1–9. doi: 10.7189/jogh.03.010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yu Q, Liu Y, Li X, Deng B. The effects of implementing National Essential Drugs System in primary care facilities in Zhongshan. China Pharmaceuticals. 2011;12:2–3. [Google Scholar]
- 158.Yip W, Hsiao W, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379:833–842. doi: 10.1016/S0140-6736(11)61880-1. [DOI] [PubMed] [Google Scholar]
- 159.Fang Y, Wagner AK, Yang S, Jiang M, Zhang F, Ross-Degnan D. Access to affordable medicines after health reform: evidence from two cross-sectional surveys in Shaanxi province, western China. Lancet Glob Health. 2013;1:e227–e237. doi: 10.1016/S2214-109X(13)70072-X. [DOI] [PubMed] [Google Scholar]
- 160.Yao Q, Luo F, He L, Chen S, Yao L, Liu Z. Effectiveness Evaluation of National Essential Medicine System in China from the Perspective of Drug Access. Chinese Hospital Management. 2014;34(3):60–62. [Google Scholar]
- 161.Chen Y, Xin Y. Effect of essential drug distribution on the security of drug supply in China. Shanghai Medical & Pharmaceutical Journal. 2015;35(15):66–72. [Google Scholar]
- 162.Liang N, Chen Z, Zeng L, Liang Z, Wu H. Adverse Drug Reactions/Adverse Drug Events Induced by National Essential Drugs: Analysis of 12 198 Cases. Evaluation and analysis of drug-use in hospitals of China. 2013;13(1):64–66. [Google Scholar]
- 163.The Ministry of Health General Office. Circular on the conduct of the National Action on Healthy Lifestyle for All (Document No: [2007]189) Available at: http://www.nhfpc.gov.cn/mohbgt/pw10801/200804/19287.shtml. Accessed July 20, 2015.
- 164.The summary of the work in National Action on Healthy Lifestyle for All in 2014. Available at: http://www.docin.com/p-1217956143.html. Accessed July 20, 2015.
- 165.The State Council. National Plan on Public Exercise: Healthy Body for All. Available at: http://www.china.com.cn/chinese/zhuanti/tyzcfg/885961.htm. Accessed July 20, 2015.
- 166.Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases (A/RES/66/2) Geneve: Jan 24, 2012. United Nations General Assembly Sixty-sixth Session. [Google Scholar]
- 167.Ministry of Health and other 14 ministries. Notice of the issuance of the work plan for the prevention and control of chronic diseases in China. 2012–2015. (Document No.: 2012). [Google Scholar]
- 168.State Council. Air pollution control action plan. Released on September 10, 2013. [Google Scholar]
- 169.People’s Republic of China Environment Protection Law (implemented since January 1, 2015), issued on April 25, 2014.
- 170.Cheney J. Speech at the 2016 National Conference on Environment Protection. 2016 Jan 11; Available at: http://www.mep.gov.cn/gkml/hbb/qt/201601/t20160114_326153.htm. Accessed January 18, 2016.
- 171.Policy of prevention in the first place and integrating prevention with control. Available at: http://www.people.com.cn/electric/hh50/9/9_3_2.html. Accessed July 20, 2015.
- 172.National Health and Family Planning Commission of People’s Republic of China. Age-specific expected life years. Available at: http://www.moh.gov.cn/open/2007tjts/P65.htm. Accessed July 20, 2015.
- 173.National Bureau of Statistics of People’s Republic of China. China average per capita GDP. Available at: http://data.stats.gov.cn/easyquery.htm?cn=C01&zb=A0A03&sj=2014. Accessed July 20, 2015.
- 174.World Health Organization, World Economic Forum. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. Geneva: Sep 18, 2011. [Google Scholar]
- 175.CPC Central Committee and the State Council. Opinions on deepening the reform of the medical and health system. Issued on March 17, 2009. Available at: http://www.gov.cn/test/2009-04/08/content_1280069.htm. Accessed July 20, 2015.
- 176.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, Cecchini M, Colagiuri R, Colagiuri S, Collins T, Ebrahim S, Engelgau M, Galea G, Gaziano T, Geneau R, Haines A, Hospedales J, Jha P, Keeling A, Leeder S, Lincoln P, McKee M, Mackay J, Magnusson R, Moodie R, Mwatsama M, Nishtar S, Norrving B, Patterson D, Piot P, Ralston J, Rani M, Reddy KS, Sassi F, Sheron N, Stuckler D, Suh I, Torode J, Varghese C, Watt J, Lancet NCDAG, Alliance NCD Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 177.Advisory board of the international heart health conference. Victoria declaration on heart health. CMAJ. 1992;147:1794–1797.172. [Google Scholar]
- 178.Tian M, Ajay VS, Dunzhu D, Hameed SS, Li X, Liu Z, Li C, Chen H, Cho KW, Li R, Zhao X, Jindal D, Rawal I, Ali MK, Peterson ED, Ji J, Amarchand R, Krishnan A, Tandon N, Xu L, Wu Y, Prabhakaran D, Yan LL. A Cluster-Randomized, Controlled Trial of a Simplified Multifaceted Management Program for Individuals at High Cardiovascular Risk (SimCard Trial) in Rural Tibet, China, and Haryana, India. Circulation. 2015;132:815–824. doi: 10.1161/CIRCULATIONAHA.115.015373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yan LL, Fang W, Delong E, Neal B, Peterson ED, Huang Y, Sun N, Yao C, Li X, MacMahon S, Wu Y. Population impact of a high cardiovascular risk management program delivered by village doctors in rural China: design and rationale of a large, cluster-randomized controlled trial. BMC Public Health. 2014;14:345. doi: 10.1186/1471-2458-14-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Li N, Yan LL, Niu W, Labarthe D, Feng X, Shi J, Zhang J, Zhang R, Zhang Y, Chu H, Neiman A, Engelgau M, Elliott P, Wu Y, Neal B. A Large-scale cluster randomized trial to determin the effects of community-based dietary sodium reduction – The China Rural Health Initiative sodium reduction study. Am Heart J. 2013;166:815–822. doi: 10.1016/j.ahj.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Du X, Gao R, Turnbull F, Wu Y, Rong Y, Lo S, Billot L, Hao Z, Ranasinghe I, Iedema R, Kong L, Hu D, Lin S, Shen W, Huang D, Yang Y, Ge J, Han Y, Lv S, Ma A, Gao W, Patel A. Hospital Quality Improvement Initiative for Patients With Acute Coronary Syndromes in China: A Cluster Randomized, Controlled Trial. Circulation: Cardiovascular Quality and Outcomes. 2014;7:217–226. doi: 10.1161/CIRCOUTCOMES.113.000526. [DOI] [PubMed] [Google Scholar]
- 182.Li S, Wu Y, Du X, Li X, Patel A, Peterson ED, Turnbull F, Lo S, Billot L, Laba T, Gao R, on behalf of the CPACS-3 investigators Rational and design of a stepped-wedge cluster randomized trial evaluating quality improvement initiative for reducing cardiovascular events among patients with acute coronary syndromes in resource-constrained hospitals in China. Am Heart J. 2015;169:349–355. doi: 10.1016/j.ahj.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 183.Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y, Shuai Y, Zhang B, Zhang J, Thompson TJ, Gerzoff RB, Roglic G, Hu Y, Bennett PH. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008;371:1783–1789. doi: 10.1016/S0140-6736(08)60766-7. [DOI] [PubMed] [Google Scholar]
- 184.Yu R, Yan LL, Wang H, Ke L, Yang Z, Gong E, Guo H, Liu J, Gu Y, Wu Y. Effectiveness of a community-based individualized lifestyle intervention among older adults with diabetes and hypertension, Tianjin, China, 2008–2009. Prev Chronic Dis. 2014;11:120333. doi: 10.5888/pcd11.120333. [DOI] [PMC free article] [PubMed] [Google Scholar]


