Abstract
As the role of genomics in healthcare grows, patients increasingly require adequate genetic literacy to fully engage in their care. This study investigated a model for delivering consumer-friendly genetic information to improve understanding of precision medicine using health literacy and learning style principles. My Cancer Genome (MCG), a freely available cancer decision support tool, was used as a test-bed. MCG content on a melanoma tumor mutation, BRAF V600E, was translated to a sixth grade reading level, incorporating multiple learning modalities. Ninety patients and caregivers were recruited from a melanoma clinic at an academic medical center and randomized to three groups. Group A (control) received an exact copy of text from MCG. Group B was given the same content with hyperlinks to videos explaining key genetic concepts, identified and labeled by the team as “knowledge pearls.” Group C received the translated content with the knowledge pearls embedded. Changes in knowledge were measured through pre- and post- questionnaires. Group C showed the greatest improvement in knowledge. The study results demonstrate that providing information based on health literacy and learning style principles can improve patient understanding of genetic concepts, thus increasing their likelihood of taking an active role in any decision-making concerning their health.
Genetically informed medicine is rapidly becoming the new standard of care and offers promise for treating complex diseases and medical conditions (Green, Guyer, & National Human Genome Research Institute, 2011). This has given hope to cancer patients but has also generated many questions for clinicians and patients alike. Previous investigators have highlighted an urgent need for research to examine how limited health literacy may affect understanding of complex genetic information (Lea, Kaphingst, Bowen, Lipkus, & Hadley, 2011; Syurina, Brankovic, Probst-Hensch, & Brand, 2011). Nearly half of the United States population, or 90 million adults, have difficulty understanding and acting upon health information, thus seriously diminishing their ability to make appropriate health decisions (Nielson-Bohlman, Panzer, Hamlin, & Kindig, 2004).
In addition to a high prevalence of limited health literacy, policy and healthcare stakeholders have also identified substantial genetic literacy deficits in the public as a whole (Center for Public Health and Community Genomics, 2011; Christensen, Jayaratne, Roberts, Kardia, & Petty, 2010; Condit, 2010; Klitzman, 2010; Lanie et al., 2004). Genetic literacy refers to “the ability of an individual to understand concepts important to the use of personal genetic information” (Erby, Roter, Larson, & Cho, 2008) and includes the concept of active application of genetic knowledge for informed decision-making (Bowling et al., 2008). Inadequate genetic literacy is a critical barrier that impedes the acceptance and utilization of genetically informed healthcare (Lea et al., 2011).
With the advent of genetically informed medicine, there is a growing need for educational intervention research to help patients understand their test results and treatment options (Dougherty, Lontok, Donigan, & McInerney, 2014; Hurle et al., 2013; Secretary’s Advisory Committee on Genetics, Health and Society, 2011). Educational materials in print and web-based formats are heavily used by patients, yet are often written at a reading level that may be too advanced for individuals with low health literacy (D’Alessandro, Kingsley, & Johnson-West, 2001; Helitzer, Hollis, Cotner, & Oestreicher, 2009; Sabharwal, Badarudeen, & Unes Kunju, 2008; Vargas, Chuang, Ganor, & Lee, 2014; Vargas, Koolen, Chuang, Ganor, & Lee, 2014). According to the National Adult Literacy survey, on average, adults read at the eighth to ninth grade level, and one in five adults read at a fifth grade level or below (Kirsch, Jungeblut, Jenkins, & Kolstad, 1993). Thus, unfortunately, much of the educational materials available to consumers are ill-suited to their needs.
Multiple studies indicate that individuals learn best when materials are presented in a manner addressing health literacy needs (Inott & Kennedy, 2011; Kandula et al., 2009). Additionally, adequate health literacy levels equip patients and caregivers with the ability to effectively understand and interact with health information (Mancuso & Rincon, 2006; McCray, 2005). Our study team has also previously demonstrated that adaptation of information to health literacy level and learning style preferences facilitates learning of complex health topics, including information about hypertension and diabetes (N.B. Giuse, Koonce, Storrow, Kusnoor, & Ye, 2012; Koonce et al., 2013; Koonce, Giuse, & Storrow, 2011). In these studies, participants were provided with tailored educational materials based on their health literacy level and preferences for learning via visual, aural, read/write, and kinesthetic sensory modalities.
Building on our previous research, the goal of this study was to create a scalable model for delivering consumer-friendly genetic information incorporating health literacy and learning style principles to improve understanding of precision cancer medicine. Central to this effort was the use of My Cancer Genome (MCG, http://www.mycancergenome.org) as a test-bed for content development and evaluation. My Cancer Genome, launched by the Vanderbilt-Ingram Cancer Center (VICC) in January 2011, was the first freely available personalized cancer decision support tool designed to provide clinicians with state-of-the-art relevant information on treatment options currently available for cancers associated with specific tumor mutations (Eisenberg, 2013; Levy, Lovly, & Pao, 2012; Parmar, 2012; Health Data Consortium, 2013; Stuart, 2011). Internally-collected Google Analytics data indicates that My Cancer Genome currently receives more than 8,000 site visits weekly from countries all around the world. While originally designed for researchers and clinicians, MCG has the potential to benefit patients and their families, who are regular visitors to the publicly available site according to MCG-conducted focus groups and patient anecdotal data.
Building upon an “information prescription” model validated through previous research (N.B. Giuse et al., 2012; Koonce et al., 2013, 2011), we developed a complementary consumer-friendly version of the content currently available in MCG regarding the BRAF V600E mutation in melanoma. The mutation was selected because it accounts for 80–90% of V600 BRAF mutations in melanoma (Lovly CM et al., 2012; Rubinstein JC et al., 2010) and because knowing whether a patient has this tumor mutation is important for therapy selection. Terms that could not be easily translated through a simple English literacy effort were hyperlinked to short explanatory videos, referred to as “knowledge pearls,” that were developed in-house by our study team and designed to incorporate multiple learning styles through the use of images, text, audio, and animation. We then evaluated the effectiveness of the information through a randomized controlled trial with melanoma patients and caregivers. We hypothesized that participants who received the consumer-level materials, embedded with hyperlinks to the knowledge pearls, would show greater improvements in performance on a knowledge questionnaire about the materials than individuals who were given the health professional-level content with or without hyperlinks to the knowledge pearls. The research was predicated on the understanding that patients informed about precision medicine are more likely to take a proactive, participatory role and engage with their healthcare team.
Method
The Vanderbilt University Medical Center Institutional Review Board (IRB # 141323) and the Vanderbilt-Ingram Cancer Center Scientific Review Committee approved this study protocol.
Study Design
The primary objective of this study was to compare knowledge gained among participants receiving information about the BRAF V600E mutation in melanoma via three different mechanisms. The study contained three groups. Group A, the control group, received professional-level information as it appears on the My Cancer Genome website. Group B participants received information as it appears on the My Cancer Genome website, however, the MCG information included embedded hyperlinks to relevant knowledge pearls. Group C participants, instead of receiving information directly from the My Cancer Genome website, received a consumer-level version of the MCG information created by the team to be more accessible for lay audiences; the consumer-level version included hyperlinks to the knowledge pearls. We included Group B to determine whether adding hyperlinks to the knowledge pearls in the MCG healthcare professional version would be sufficient for enhancing understanding of the material, since adding links to videos alone, without the need to translate the content into a consumer-friendly version, would allow for greater scalability.
Prior to randomization, participants completed several assessments. Participants were asked to fill out a demographics form and to indicate their understanding of several genetic terms. To better understand the impact of health literacy and learning style on study results, the study team also determined participants’ health literacy levels using the three-question assessment described by Chew, Bradley, and Boyko (2004) and asked participants to identify their learning style preferences. Changes in knowledge were measured using a pre- and post- knowledge questionnaire developed by the study team. Appendix A (available in the supplemental online appendix) includes the demographic form and assessments participants completed during the study. Figure 1 provides a schematic of the overall study design and structure. The time required of subjects for participation in the study was approximately 30 minutes.
Fig. 1.
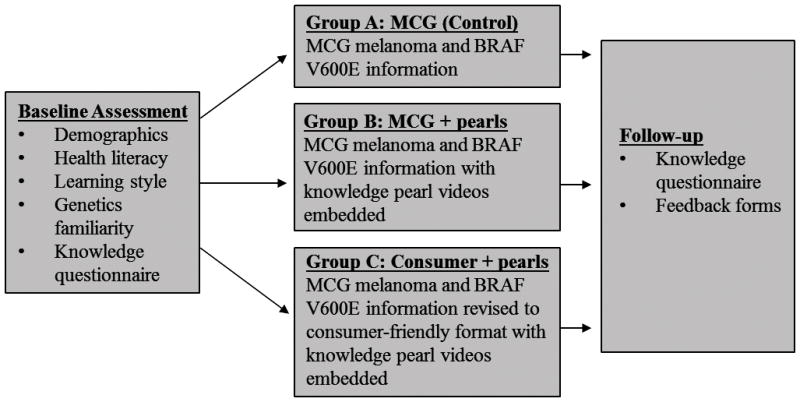
Study design schematic.
Setting
Patients and caregivers were recruited for the study from the Melanoma Clinic at the Vanderbilt-Ingram Cancer Center (VICC). VICC is one of 41 centers designated by the National Cancer Institute as a Comprehensive Cancer Center and provides care to more than 6,252 new cancer patients each year Vanderbilt-Ingram Cancer Center, n.d.).
Participants
From September 19–November 4, 2014, we recruited participants from the VICC Melanoma Clinic. To participate in the study, participants had to be 18 or older, have the ability to read and speak English, and have melanoma or be the caregiver for a melanoma patient who had agreed to participate in the study. Individuals who were cognitively impaired (as determined by clinical judgment of the melanoma provider) or imprisoned were excluded from the study. Our team collected baseline data from each participant on age, race, gender, education level, income level, occupation status, and participant status (melanoma patient or caregiver). The time since diagnosis was also determined via medical record review in StarPanel, Vanderbilt University Medical Center’s electronic medical record system (D. A. Giuse, 2003). Additionally, cancer stage and date of tumor profiling were determined from review of the medical record for demographic and data analysis purposes.
Participants who satisfied all inclusion criteria were randomized equally to three groups based on the educational information they received (Figure 1). Randomization was carried out using stratified permuted-block randomization with stratification factors “time since melanoma diagnosis” (within 12 months, 13 to 24 months, or over 24 months) and “type of study participant” (melanoma patient or caregiver of melanoma patient) with a block size of 3. After exclusions, 90 participants were randomized in an approximately 1:1:1 ratio to one of the three intervention groups (Figure 2).
Fig. 2.
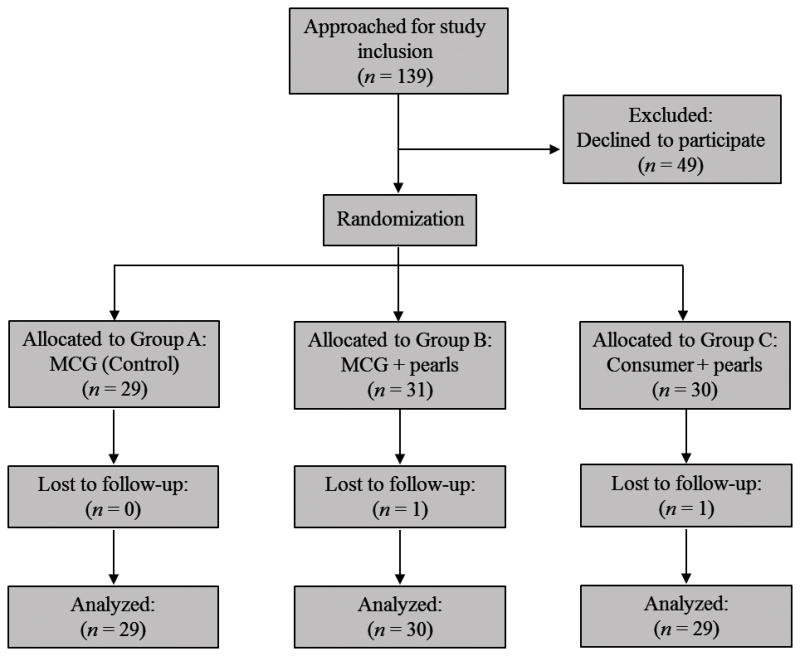
Participant flowchart.
Measures
Participants were given the subjective health literacy assessment developed by Chew et al. to determine health literacy level (Chew et al., 2004). The measure consists of three questions assessing confidence filling out medical forms, frequency with which help is needed reading hospital materials, and how often participants had problems learning about medical conditions. Our study team previously confirmed other researchers’ findings that asking individuals to answer these three questions matched the effectiveness of the Short Test of Functional Health Literacy (S-TOFHLA) in identifying individuals with low health literacy levels (Chew et al., 2008; N. B. Giuse et al., 2012; McNaughton, Wallston, Rothman, Marcovitz, & Storrow, 2011).
To determine learning style preferences, participants were asked to indicate whether they would recall how to do something a year from now if they learned it by reading, listening, watching, or doing. Our previous research revealed that asking patients to subjectively indicate their learning style preferences produced results that corresponded closely with those of formal learning style measures (N. B. Giuse et al., 2012).
Few tools for assessing genetic literacy have been developed (Daack-Hirsch, Driessnack, Perkhounkova, Furukawa, Ramirez, 2012; Rodriguez, Roter, Castillo-Salgado, Hooker, Erby, 2015; Hooker et al., 2014). One of the most commonly used assessments for genetic literacy is the rapid estimate of adult literacy in genetics (REAL-G), a test that assesses a person’s ability to read and pronounce a list of 121 genetic words (Erby et al, 2008). One limitation of the REAL-G is that it does not measure comprehension (Erby et al., 2008, Rodriguez et al., 2015). Therefore, we chose to assess the participants’ baseline familiarity of terminology regarding genetics and melanoma therapy by asking them to rate their level of understanding of the terms gene, DNA, mutation, BRAF, and targeted therapy on a 1–5 scale, with 1 corresponding to fully understanding and 5 to having never heard the term. The questions were modeled after those used by Falcone and colleagues (Falcone, Wood, Xie, Siderowf, & Van Deerlin, 2011). Participants were also asked to complete a knowledge questionnaire before and after viewing the educational materials to assess the effectiveness of the intervention. The questionnaire was developed internally by our study team and consisted of 10 items, including multiple choice and true/false questions about genetics, melanoma, and BRAF (see Appendix A in the supplemental online appendix).
Intervention
Content within My Cancer Genome was initially reviewed to identify terms regarding genetics or cancer medicine that may be difficult for patients to understand and that could not easily be translated through an English literacy effort (Kusnoor et al., 2015). These terms were chosen to be knowledge pearls. Selection of which terms to include was informed by discussions with librarians, information scientists, and clinicians on our team. We originally referred to these pearls as “genetic pearls”; however, in an effort to more widely include basic concepts, procedures, and conditions that are related to genetics but may not be specifically genetic, we later chose to refer to them as “knowledge pearls.” This term more accurately reflects the pearls’ content and allows for broader scalability for multiple uses. The knowledge pearls were developed in-house using the software program Sparkol VideoScribe, and the approximate length of the pearls was one to two minutes. The script for the knowledge pearls was aimed at the sixth grade level.
As studies have shown that many people learn best through multimodal learning (Kusnoor et al., 2015; Mainemelis, Boyatzis, & Kolb, 2002; Pashler, McDaniel, Rohrer, & Bjork, 2009; Truluck & Courtenay, 1999), the knowledge pearls were developed using a multimedia format to allow for the incorporation of several learning style modalities, including preferences for text (read/write), images (visual), audio (aural), and some animation (kinesthetic). By incorporating multiple learning styles, the knowledge pearls were developed to be applicable for learners with varying learning preferences.
We used feedback from focus groups to guide the creation of the knowledge pearls (Kusnoor et al., 2015). Basic and advanced versions of three of the knowledge pearls were initially prepared and presented to cancer patients, caregivers, and family members in a series of five focus groups, which were conducted in April 2014 and included a total of 30 participants. Based on this feedback, we refined the pearls into one version, combining some elements of the basic and advanced videos. We also developed a style guide based on general themes from the focus group comments, which we used for creating the additional pearls (Kusnoor et al., 2015).
Working in collaboration with the My Cancer Genome team, a group of physicians and scientists with expertise in cancer genetics and bioinformatics, our team of librarians and information scientists then developed a consumer-friendly version of information regarding the BRAF V600E mutation in melanoma. Through extensive process refinement, we developed a workflow for content development to allow the team to reach consensus and ensure that the expertise of the varied members of the study team was utilized. The workflow was used to create the version of the BRAF V600E mutation information shown to participants in Group C.
We revised the original text from MCG on the BRAF V600E mutation, which was written at the twelfth grade level as assessed by the SMOG (McLaughlin, 1969), to the sixth grade level in the consumer translation. The consumer translation used a question and answer format to make the information more engaging for patients and help break up important concepts. We used bulleted lists to improve readability in the consumer version and added images where appropriate. Additional explanation of the types of melanoma treatments was added to the consumer version since some patients may be unfamiliar with this terminology. We aimed to reduce the use of jargon in the consumer version and to focus primarily on need-to-know information. The description of what the BRAF V600E mutation does and how it works was greatly simplified from the MCG version, and images were added to facilitate comprehension of the information. The consumer version also addressed some of the additional concerns our partnering oncologists communicated that patients may have, such as whether the mutation could be passed to their children and the implications of having a different BRAF mutation other than V600E or having no mutations in BRAF.
Participants were randomized to receive one of three types of information (Figure 1). Group A, the control group, received information taken directly from the My Cancer Genome website on the BRAF V600E mutation in melanoma (Appendix B in the supplemental online appendix). Group B was given the same information from MCG with hyperlinks to the knowledge pearl videos embedded next to the words they defined. Finally, Group C received a consumer-level version of the MCG information with knowledge pearls embedded (Appendix C in the supplemental online appendix). The knowledge pearls were simply referred to as “videos” when interacting with the patients. The text viewed by Group B included 13 knowledge pearls, while the consumer version contained hyperlinks to 5 knowledge pearls.
Follow-up Assessment
Immediately after reviewing the educational information, participants again took the knowledge questionnaire about genetics and personalized cancer therapy. Participants were also asked to rate their level of agreement on a 1 to 5 Likert scale, with 5 corresponding to strongly agree, with statements about whether the information they received was easy to understand, if it was confusing, if they were satisfied with the information, and if the information taught them something new. Using the same scale, they were also asked to indicate their level of agreement with statements about whether the knowledge pearl videos helped them understand the information they received, if the videos were easy to understand, and if the videos were confusing. Those completing the study received a $25 gift card.
Statistical Analysis
The primary objective of the study was to evaluate the educational effectiveness of consumer-level information about BRAF and melanoma, which was assessed by comparing pre- and post-knowledge test scores among the three intervention groups. With a total sample size of 90 (n = 30 per group), the study provided at least 80% power to detect a 0.86x standard deviation difference at a two-sided overall significance level of 5%. This sample size calculation was based on the assumption that the effect size is equal to the mean difference between groups divided by the standard deviation.
Multivariable linear regression was used to estimate the intervention effect on post-knowledge test score, adjusted for pre-knowledge test score (baseline assessment), as well as other covariates (age and health literacy). We omitted item 4 of the knowledge questionnaire from the primary analysis because this question could only be answered by a knowledge pearl video available to Group B and C participants. Residual analysis was used to check the linear regression assumptions of homogeneity for variance, normality and linearity. The final model was decided based on likelihood ratio tests for nested models as well as adjusted R2. All tests were significant at the two-sided 5% level. Analyses were performed in R 3.1.0, and the study statisticians were blinded to the group assignment.
Ad-hoc Fisher’s exact tests were conducted to evaluate differences among the three groups in participant ratings of whether the information they viewed was easy to understand, if it was confusing, if they were satisfied with the information, and if the information taught them something new. Ad-hoc Fisher’s exact tests were also used to evaluate differences among groups in responses to whether the knowledge pearl videos helped them understand the information they received, if the videos were easy to understand, and if the videos were confusing. All study data were entered into Research Electronic Data Capture (REDCap), a secure, web-based research data management software program (Harris et al., 2009).
Results
Study Participants
Ninety participants were enrolled. Two individuals withdrew, resulting in a total of eighty-eight participants at study completion (Figure 2 and Table 1). Groups A and C both had 29 participants, and Group B had 30 participants. There were approximately twice as many patients as caregivers in each group. Participants were similarly distributed by gender and race. Nearly twice as many participants in Group B reported a household income greater than $75,000 when compared to Groups A and C. Most patients had been diagnosed with melanoma for more than 24 months, and over half the participants in each group reported stage IV melanoma. Most of the participants had previously had tumor sequencing conducted.
Table 1.
Participant characteristics
| Characteristic | Group A (n = 29) | Group B (n = 30) | Group C (n = 29) |
|---|---|---|---|
| Participant type, n (%) | |||
| Melanoma patient | 20 (69) | 20 (67) | 20 (69) |
| Caregiver | 9 (31) | 10 (33) | 9 (31) |
| Time since diagnosis, n (%) | |||
| Within 12 months | 3 (10) | 3 (10) | 3 (10) |
| 13–24 months | 3 (10) | 5 (17) | 4 (14) |
| Over 24 months | 23 (79) | 22 (73) | 22 (76) |
| Cancer stage, n (%) | |||
| Stage II | 0 (0) | 0 (0) | 2 (6.9) |
| Stage III | 7 (24) | 5 (17) | 6 (21) |
| Stage IV | 22 (76) | 20 (67) | 17 (59) |
| Not available | 0 (0) | 5 (17) | 3 (10) |
| Other | 0 (0) | 0 (0) | 1 (3.5) |
| Tumor sequencing conducted, n (%) | |||
| Yes | 19 (66) | 24 (80) | 19 (66) |
| No/data was not available | 10 (34) | 6 (20) | 10 (34) |
| Age in years, mean (SD) | 52.8 (12) | 62.0 (13) | 56.4 (17) |
| Gender, n (%) | |||
| Male | 13 (45) | 15 (50) | 13 (45) |
| Female | 16 (55) | 13 (43) | 16 (55) |
| Left blank | 0 (0) | 2 (6.7) | 0 (0) |
| Race, n (%) | |||
| White | 28 (97) | 28 (93) | 29 (100) |
| Black or African American | 1 (3.5) | 0 (0) | 0 (0) |
| Left blank | 0 (0) | 2 (6.7) | 0 (0) |
| Education, n (%) | |||
| High school graduate, GED or equivalent | 7 (24) | 4 (13) | 3 (10) |
| Some college - no degree | 2 (6.9) | 6 (20) | 8 (28) |
| Vocational/technical degree | 6 (21) | 3 (10) | 4 (14) |
| Bachelor’s degree | 8 (28) | 8 (27) | 7 (24) |
| Master’s degree | 6 (21) | 7 (23) | 5 (17) |
| Professional school degree | 0 (0) | 1 (3.3) | 2 (6.9) |
| Doctoral degree | 0 (0) | 1 (3.3) | 0 (0) |
| Household income, n (%) | |||
| Prefer not to say | 8 (28) | 5 (17) | 6 (21) |
| $10,000 or less | 0 (0) | 0 (0) | 1 (3.5) |
| $10,001 – $20,000 | 1 (3.5) | 0 (0) | 1 (3.5) |
| $20,001 – $35,000 | 3 (10) | 1 (3.3) | 2 (6.9) |
| $35,001 – $55,000 | 2 (6.9) | 6 (20) | 5 (17) |
| $55,001 – $75,000 | 7 (24) | 1 (3.3) | 7 (24) |
| more than $75,000 | 7 (24) | 15 (50) | 6 (21) |
| Left blank | 1 (3.5) | 2 (6.7) | 1 (3.5) |
| Health literacy level, n (%) | |||
| Adequate | 22 (76) | 26 (87) | 27 (93) |
| Marginal | 4 (14) | 3 (10) | 1 (3.5) |
| Inadequate | 3 (10) | 1 (3.3) | 1 (3.5) |
| Learning style, n (%) | |||
| Reading | 1 (3.5) | 4 (13) | 1 (3.5) |
| Listening | 3 (10.3) | 1 (3.3) | 2 (6.9) |
| Watching | 2 (6.9) | 0 (0) | 0 (0) |
| Doing | 11 (38) | 10 (33) | 8 (28) |
| Multimodala | 12 (41) | 15 (50) | 18 (62) |
Note. Percentages may not equal 100% due to rounding.
Participants who selected more than one learning style were classified as multimodal learners.
All participants had completed at least a high school education. Eighty-five percent (75/88) of the participants in the study had adequate health literacy while 9% (8/88) had marginal health literacy and 6% (5/88) had inadequate health literacy. Approximately half the participants (45/88, 51%) indicated that they preferred learning via multiple modalities.
In the baseline assessment of understanding of genetic terms, participants’ mean response was between fully and somewhat understanding the terms gene, DNA, mutation, and targeted therapy; they were less familiar with BRAF (Figure 3).
Fig. 3.
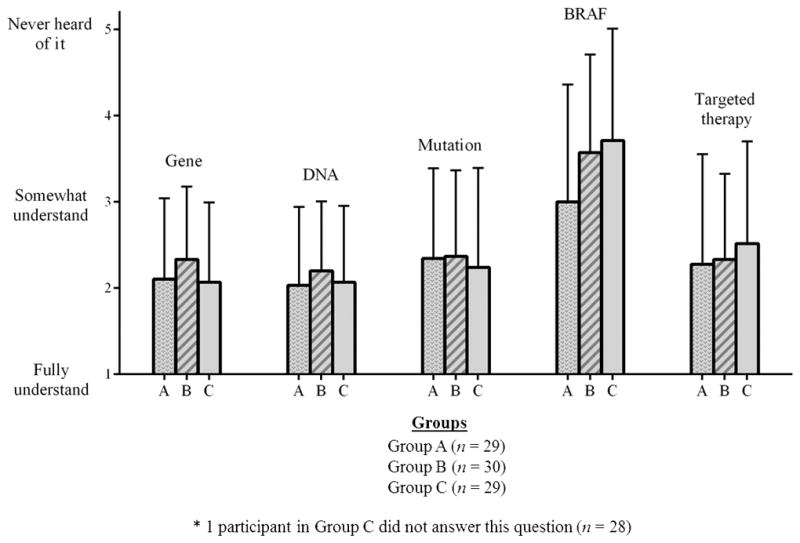
Baseline self-assessment of understanding of terms. *One participant in Group C did not answer this question (n = 28).
Knowledge Questionnaire Differences
On the pre-test, less than 22% of participants correctly answered items 2 and 8, regarding where melanomas can appear and what is BRAF, respectively (Table 2). Less than half the participants correctly answered the question on the pre-test about mutations (item #5). By contrast, over 70% of the participants in each group correctly answered pre-test item #3, which asked participants to identify ways to treat melanoma. A high percentage of participants (70–97%) also correctly answered pre-test item #6, which addressed whether knowing about mutations in melanoma can guide treatment options.
Table 2.
Percentage of participants responding correctly to individual items on the knowledge test
| Item | Pretest | Posttest | Change in Percentage | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Group A (n = 29) | Group B (n = 30) | Group C (n = 29) | Group A (n = 29) | Group B (n = 30) | Group C (n = 29) | Group A (n = 29) | Group B (n = 30) | Group C (n = 29) | |
| 1. Which of these statements is true about melanoma? | 83 | 80 | 76 | 76 | 70 | 79 | −7 | −10 | 3 |
| 2. Besides skin, where else might melanoma appear? | 3.5 | 6.7 | 3.5 | 3.5 | 0 | 6.9 | 0 | −6.7 | 3.4 |
| 3. Melanoma can be treated by:a | 76 | 80 | 72 | 90 | 93 | 93 | 14 | 13 | 21 |
| 4. Which of these statements about genes is correct?b | 79 | 67 | 76 | 86 | 83 | 83 | 7 | 16 | 7 |
| 5. A mutation can:a | 45 | 47 | 41 | 55 | 67 | 72 | 10 | 20 | 31 |
| 6. Knowing about mutations in melanoma can help guide treatment options. | 97 | 70 | 86 | 97 | 93 | 100 | 0 | 23 | 14 |
| 7. Which of these statements is true about targeted therapies? | 79 | 87 | 62 | 90 | 80 | 97 | 11 | −7 | 35 |
| 8. What is BRAF? | 21 | 17 | 21 | 38 | 50 | 59 | 17 | 33 | 38 |
| 9. How common is the BRAF mutation in melanoma? | 41 | 43 | 34 | 83 | 77 | 72 | 42 | 34 | 38 |
| 10. Dabrafenib and vemurafenib are types of: | 55 | 43 | 45 | 83 | 77 | 93 | 28 | 34 | 48 |
See Appendix A (supplemental online appendix) for the full question.
Item 4 was not fully addressed in the information given to Group A.
Participants in Group C showed improvements in performance on the post-test for all items (Table 2). By contrast, Groups A and B showed an increase in the percentage of participants with correct responses for 6 of the 9 questions (excluding question 4). The change in percentage of participants in Group C who correctly answered individual items on the knowledge questionnaire ranged from 3–48%.
Mean scores for participants in all three groups were higher on the post-assessment than the pre-assessment (Table 3 and Figure 4). Multivariable linear regression revealed that Group C showed a significantly greater improvement compared to the control, Group A (p =0.0267; Table 4). On average, Group C had a 0.8 point higher follow-up test score compared to Group A, after adjustment for baseline score, age, and health literacy. There were no significant differences detected between Group B and Group A. The multivariable analysis also identified age as a significant predictor of post-test scores (p = 0.0025; Table 4). For each increase in age of one year, the follow-up test score decreased 0.03 points on average after adjustment for baseline pre-knowledge test score, study group, and health literacy. Bonferroni’s correction was applied to control for inflated type I error rate due to multiple testing
Table 3.
Mean scores on the knowledge assessment questionnaire
| Group A (n = 29) | Group B (n = 30) | Group C (n = 29) | |
|---|---|---|---|
| Knowledge test score, mean number of correct answers, (SD) | |||
| Pre-assessment score | 5.00 (2.04) | 4.73 (1.95) | 4.41 (2.10) |
| Post-assessment score | 6.17 (1.56) | 6.17 (1.68) | 6.72 (1.60) |
| Change in test score | 1.17 (1.47) | 1.43 (1.76) | 2.31 (1.95) |
Fig. 4.
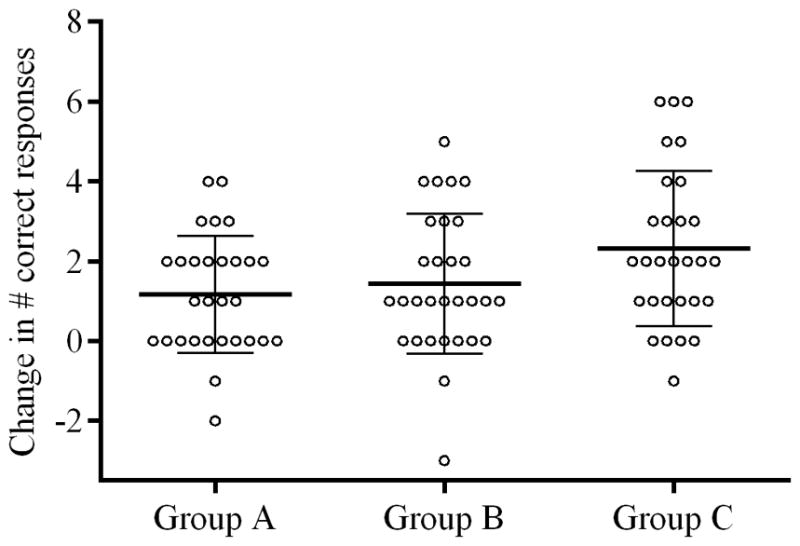
Change in scores from preassessment to postassessment.
Table 4.
Multivariate linear regression
| Variable | Posttest score (N = 88)
|
|||
|---|---|---|---|---|
| B | (SE) | t | p (two-tailed) | |
| Intercept | 6.22 | (0.780) | 7.97 | < .0001 |
| Pretest score | 0.35 | (0.075) | 4.68 | < .0001 |
| Group B | 0.28 | (0.467) | 0.81 | .4176 |
| Group C | 0.8 | (0.340) | 2.36 | .0207 |
| Age | −0.03 | (0.010) | −2.85 | .0055 |
| Health Literacy* | −0.12 | (0.066) | −1.83 | .0714 |
Health literacy is scored on an inverse scale.
Web Analytics
To assess the intervention fidelity, we collected web analytics to determine whether participants viewed the knowledge pearls. Ninety percent of participants in Group B and 82.8% of participants in Group C viewed at least one of the knowledge pearls. The knowledge pearls viewed by at least 50% of participants in Group B were mutation, oncogene, and somatic. In Group C, the pearls viewed by at least 50% of participants were protein and gene (Table 5).
Table 5.
Web analytics data
| Group A (n = 29) | Group B (n = 30) | Group C (n = 29) | |
|---|---|---|---|
| Duration viewing content in minutes, mean (SD)a | 8.67 (4.42) | 16.7 (11.0) | 11.0 (12.9) |
| Viewed pearls, n (%) | |||
| None | N/A | 3 (10) | 5 (17.2) |
| One or more | N/A | 27 (90) | 24 (82.8) |
| One | N/A | 3 (10) | 5 (17.2) |
| Two | N/A | 4 (13.3) | 6 (20.7) |
| Three | N/A | 4 (13.3) | 9 (31.0) |
| Four | N/A | 4 (13.3) | 4 (13.8) |
| Five | N/A | 3 (10) | 0 (0) |
| Six or more | N/A | 9 (30) | N/A |
| All | N/A | 1 (3.33) | 0 (0) |
Data were not available for three participants in Group A and one participant in Group C.
Participant Feedback
We asked participants in each of the three groups to indicate their agreement or disagreement with statements about whether the materials were easy to understand, if they were satisfied with the information they received, and if they learned something from the information they received (Figure 5). When compared to Groups A and B, a higher percentage of Group C participants responded that they either agreed or strongly agreed with statements that the materials were easy to understand, that they were satisfied with the information, and that they learned something new. The differences observed in the proportion of responses for understandability and satisfaction were statistically significant (p=0.0018 and 0.0006 respectively). A lower percentage of Group C participants reported that they thought some of the information was confusing; however, overall differences in responses to the question were not statistically significant (p=0.278).
Fig. 5.
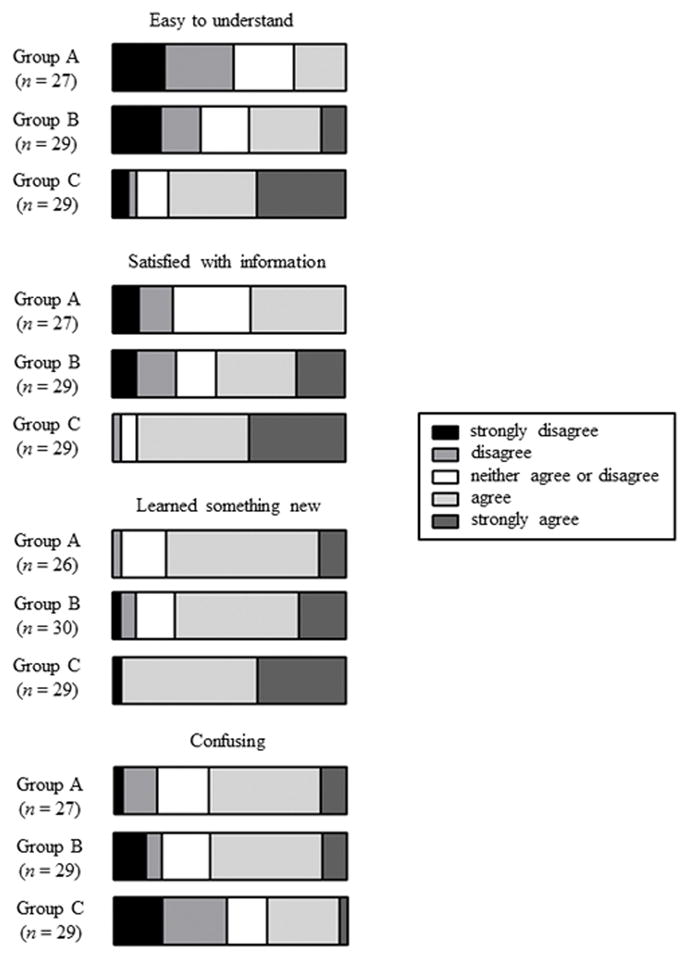
Likert scale responses for the four questions about information.
The assessment also asked participants to indicate their satisfaction with the videos (Figure 6). A high percentage in both groups viewing videos (Groups B and C) agreed or strongly agreed with statements that the videos were useful. Most participants also indicated that the videos were easy to understand and not confusing. There were no statistically significant differences in responses of Group B and C participants regarding whether the videos were useful and easy to understand, while there were marginally significant differences between groups in responses to whether the videos were confusing (p=0.054).
Fig. 6.
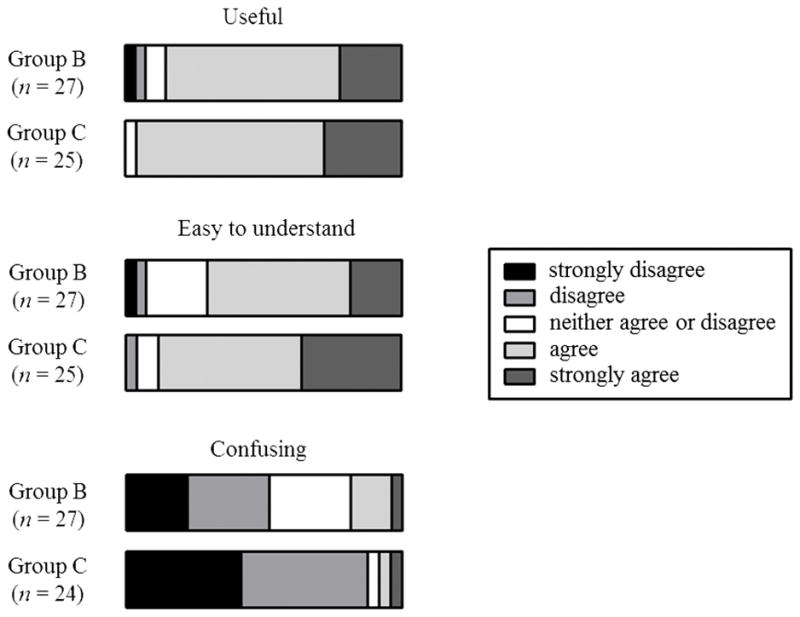
Likert scale responses for the three questions about videos.
Discussion
This study demonstrates the utility of adapting materials based on health literacy and learning styles to facilitate learning about genetically informed melanoma treatments. Consistent with our hypothesis, the group that received the consumer-level version of the information with hyperlinks to the knowledge pearls (Group C) showed the greatest improvements in performance on the knowledge questionnaire. Interestingly, the mean scores for the group receiving information in the professional version with the knowledge pearls embedded (Group B) were between those of the control group (Group A) and those receiving the consumer-level version (Group C), suggesting that the knowledge pearls by themselves may facilitate learning of the professional-level information.
In addition to greater knowledge, participants also demonstrated greater satisfaction with the consumerr-level materials with knowledge pearls embedded than with the original My Cancer Genome content. Participants’ feedback about the knowledge pearls was also very positive. The improved satisfaction resulting from addition of knowledge pearls is an important finding, as engaged patients are more likely to share decision-making responsibilities that, in turn, often translate into improved health outcomes (Scalise, 2006; Stevenson, Kerr, Murray, & Nazareth, 2007; Wald, Dube, & Anthony, 2007).
The multivariate analysis indicated that age was a significant predictor of post-test score. Ashida and colleagues previously found that older adults had lower health literacy and genetic knowledge levels than younger age groups (Ashida et al., 2011). As older adults may be more likely to encounter genetic information as a component of their healthcare, there is a potential need for future interventions to further investigate the impact of age on genetic knowledge outcomes.
We chose to provide information about the BRAF V600E mutation because it is the most prevalent BRAF mutation in melanoma. The majority of patients in our study had tumor sequencing conducted. We did not record the specific mutations patients had, but only whether tumor sequencing had been conducted. Some of the patients for whom tumor sequencing was conducted may have had mutations in genes other than BRAF or no mutations. It is helpful to understand whether patients had previously had their tumor sequenced since they may have previously received education on this topic. Patients who had already had their tumor sequenced are still a relevant population for our educational information, since they may directly benefit from the knowledge provided about targeted therapies for melanoma.
The model we have provided improves upon work of previous initiatives by providing content written at the average consumer’s health literacy level and accounting for the impact of learning style on understanding. Several initiatives, including the National Library of Medicine’s Genetics Home Reference resource and the University of Utah’s Genetic Science Learning Center, have previously developed consumer-friendly information to elucidate the connection between health and genetics for the public (Spatz, 2004; University of Utah Genetic Science Learning Center, n.d.). In 2013, the Massachusetts General Hospital Cancer Center launched its Targeted Cancer Care website, which offers consumer-level information about personalized cancer care (Fuseideas, 2013; Massachusetts General Cancer Center, n.d.). Although useful, these resources may still be difficult for consumers to understand as the material is often written at a high school reading level or higher (Crumb, 2013; Spatz, 2004).
Limitations
This study has some limitations. The majority of the participants had adequate health literacy and had completed at least a high school education. Nearly all the participants were white. Also, the study evaluated the effectiveness of information regarding one mutation in one condition, and changes in knowledge were assessed immediately after participants viewed the information. In future studies it will be important to assess the effectiveness of our approach in a population with more diversity and with higher rates of low health literacy. It will also be necessary to test both the applicability and reproducibility of our approach to genetic patient education for other conditions and to determine whether the changes in knowledge are long-lasting.
Another limitation of the study is that we did not ask the participants how long they had been patients at Vanderbilt or collect information about metastases. This may have impacted the likelihood that they previously received information about targeted therapies, BRAF and melanoma. We plan to collect this data in future studies with cancer patients.
A total of eighty-eight participants completed the study. While the number of participants provided adequate power to detect the observed differences in knowledge outcomes between Groups A and C, a larger study population may have provided additional power to detect potentially significant differences between Groups A and B.
Additionally, in this study, participants completed a subjective health literacy measure (Chew et al., 2004) and a subjective assessment of their baseline familiarity of terminology regarding genetics and melanoma therapy (i.e., gene, DNA, mutation, BRAF, and targeted therapy). Given the self-reported nature of these assessments, it is possible that the high rates of adequate health literacy and familiarity with genetic/melanoma therapy terminology observed in our population could be subject to social desirability bias. As in our previous research (N. B. Giuse et al., 2012; Koonce et al., 2013), the team chose to use the brief health literacy assessment by Chew, Bradley, and Boyko (2004) to minimize participant burden and overall time required for study participation as we interacted with patients and caregivers during their busy clinic visits. Future work may be needed to investigate how to best incorporate objective health literacy assessments (Baker, Williams, Parker, Gazmararian, & Nurss, 1999; Weiss et al., 2005) into the clinical workflow. It is important to note that because of the limitations of relying on a subjective assessment of genetic/melanoma treatment concepts, to better gauge participant baseline knowledge of the information we provided, the team also used the objective assessment described in the methods section.
Finally, our study population included both patients and caregivers. There may be differences between the two groups that differentially affect their comprehension of the educational information. Future studies are needed to assess how factors, such as pain, fatigue, ability to concentrate, and stress influence the effectiveness of the intervention.
Conclusion
Oncologists have been early adopters in embracing knowledge of genetic variation to inform therapy selection (Ciardiello et al., 2014). As decisions about cancer treatment options increasingly rely on knowledge of an individual’s tumor genetic makeup, patients need to be able to understand the significance of tumor testing and the implications of their results. It will be critical for patients and caregivers to have access to information about precision medicine they can easily understand. The need for the public to rapidly comprehend such information will also likely grow with increased funding for precision medicine research (Collins & Varmus, 2015; White House, Office of the Press Secretary, 2015).
Our study shows the effectiveness of a paradigm for developing consumer-friendly information using health literacy and learning style principles to enhance understanding of a tumor mutation and its impact on cancer therapy. It is important to note that although our population included a high percentage of participants with adequate health literacy, the results from the study are still applicable for this population, as individuals with adequate health literacy may still have a limited understanding of genetics. This model builds on our previous investigations of health literacy and learning style for patient education (N. B. Giuse et al., 2012; Koonce et al., 2013, 2011) and adds additional features for scalability. One of the innovative features was the use of the knowledge pearl videos, which enabled us to simultaneously incorporate multiple learning modalities to help explain the complicated terminology pertaining to genetics and personalized cancer therapy. This helped streamline the content development process, which is ultimately necessary for scalability as it allows for content reuse.
The approach described in this study can be used to facilitate lifelong learning for patients and caregivers. In the era of precision medicine and ongoing genetic discoveries, enhancing participatory care by promoting genetic health literacy may provide the necessary impetus to drive individual behavior modifications required for improving health outcomes overall (Green et al., 2011; Olsen, Saunders, & McGinnis, 2011; Syurina et al., 2011).
Supplementary Material
Acknowledgments
Funding
This study was funded by a grant from the Institute of Museum and Library Services (IMLS LG-06-13-0180-13). The melanoma disease area on My Cancer Genome was supported by the Joyce Family Foundation, the Robert J. Kleberg, Jr., and Helen C. Kleberg Foundation, the T. J. Martell Foundation, an anonymous foundation, and a corporate gift from Bristol-Myers Squibb. Support for the REDCap database, used in this study for data entry and data collection, was provided by CTSA award UL1TR000445 from the National Center for Advancing Translational Sciences.
References
- Ashida S, Goodman M, Pandya C, Koehly LM, Lachance C, Stafford J, Kaphingst KA. Age differences in genetic knowledge, health literacy and causal beliefs for health conditions. Public Health Genomics. 2011;14(4–5):307–316. doi: 10.1159/000316234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Education and Counseling. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- Bowling BV, Acra EE, Wang L, Myers MF, Dean GE, Markle GC, … Huether CA. Development and evaluation of a genetics literacy assessment instrument for undergraduates. Genetics. 2008;178(1):15–22. doi: 10.1534/genetics.107.079533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Public Health and Community Genomics. Priorities for public health genomics 2012–2017. 2011 Retrieved from http://genomicsforum.org/files/geno_report_WEB_w_RFI_1122rev.pdf.
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;36(8):588–594. [PubMed] [Google Scholar]
- Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, … VanRyn M. Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of General Internal Medicine. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen KD, Jayaratne TE, Roberts JS, Kardia SLR, Petty EM. Understandings of basic genetics in the United States: Results from a national survey of black and white men and women. Public Health Genomics. 2010;13(7–8):467–476. doi: 10.1159/000293287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciardiello F, Arnold D, Casali PG, Cervantes A, Douillard JY, Eggermont A, … Stahel R. Delivering precision medicine in oncology today and in future-The promise and challenges of personalised cancer medicine: A position paper by the European Society for Medical Oncology (ESMO) Annals of Oncology. 2014;25(9):1673–1678. doi: 10.1093/annonc/mdu217. [DOI] [PubMed] [Google Scholar]
- Collins FS, Varmus H. A new initiative on precision medicine. The New England Journal of Medicine. 2015 doi: 10.1056/NEJMp1500523. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condit CM. Public understandings of genetics and health. Clinical Genetics. 2010;77(1):1–9. doi: 10.1111/j.1399-0004.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- Crumb SI. An evaluation framework to assess educational genetic websites: Are they meeting public needs? Master’s thesis. 2013 Retrieved from https://digital.lib.washington.edu/researchworks/bitstream/handle/1773/25159/Crumb_washington_0250O_12604.pdf?sequence=1.
- Daack-Hirsch S, Driessnack M, Perkhounkova Y, Furukawa R, Ramirez A. A practical first step to integrating genetics into the curriculum. The Journal of Nursing Education. 2012;51(5):294–298. doi: 10.3928/01484834-20120309-02. [DOI] [PubMed] [Google Scholar]
- D’Alessandro DM, Kingsley P, Johnson-West J. The readability of pediatric patient education materials on the World Wide Web. Archives of Pediatrics & Adolescent Medicine. 2001;155(7):807–812. doi: 10.1001/archpedi.155.7.807. [DOI] [PubMed] [Google Scholar]
- Dougherty MJ, Lontok KS, Donigan K, McInerney JD. The critical challenge of educating the public about genetics. Current Genetic Medicine Reports. 2014;2(2):48–55. doi: 10.1007/s40142-014-0037-7. [DOI] [Google Scholar]
- Eisenberg A. In cancer treatment, new DNA tools. The New York Times. 2013 Apr 27; Retrieved from http://www.nytimes.com/2013/04/28/business/in-cancer-treatment-new-dna-tools.html.
- Erby LH, Roter D, Larson S, Cho J. The Rapid Estimate of Adult Literacy in Genetics (REAL-G): A means to assess literacy deficits in the context of genetics. American Journal of Medical Genetics. Part A. 2008;146A(2):174–181. doi: 10.1002/ajmg.a.32068. [DOI] [PubMed] [Google Scholar]
- Falcone DC, Wood EM, Xie SX, Siderowf A, Van Deerlin VM. Genetic testing and Parkinson disease: Assessment of patient knowledge, attitudes, and interest. Journal of Genetic Counseling. 2011;20(4):384–395. doi: 10.1007/s10897-011-9362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuseideas. Fuseideas launches MGH Targeted Cancer Care website. 2013 Aug 22; Retrieved October 7, 2015, from http://fuseideas.com/news/fuseideas-launches-mgh-targeted-cancer-care-website.
- Giuse DA. Supporting communication in an integrated patient record system. AMIA ... Annual Symposium Proceedings / AMIA Symposium. AMIA Symposium; 2003. p. 1065. [PMC free article] [PubMed] [Google Scholar]
- Giuse NB, Koonce TY, Storrow AB, Kusnoor SV, Ye F. Using health literacy and learning style preferences to optimize the delivery of health information. Journal of Health Communication. 2012;17(sup3):122–140. doi: 10.1080/10810730.2012.712610. [DOI] [PubMed] [Google Scholar]
- Green ED, Guyer MS National Human Genome Research Institute. Charting a course for genomic medicine from base pairs to bedside. Nature. 2011;470(7333):204–213. doi: 10.1038/nature09764. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Data Consortium. Health Data Stories: My Cancer Genome. 2013 Mar 13; Retrieved from http://www.healthdataconsortium.org/blog_home.asp?display=40.
- Helitzer D, Hollis C, Cotner J, Oestreicher N. Health literacy demands of written health information materials: An assessment of cervical cancer prevention materials. Cancer Control: Journal of the Moffitt Cancer Center. 2009;16(1):70–78. doi: 10.1177/107327480901600111. [DOI] [PubMed] [Google Scholar]
- Hooker GW, Peay H, Erby L, Bayless T, Biesecker BB, Roter DL. Genetic literacy and patient perceptions of IBD testing utility and disease control: a randomized vignette study of genetic testing. Inflammatory Bowel Diseases. 2014;20(5):901–908. doi: 10.1097/MIB.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurle B, Citrin T, Jenkins JF, Kaphingst KA, Lamb N, Roseman JE, Bonham VL. What does it mean to be genomically literate? National Human Genome Research Institute meeting report. Genetics in Medicine. 2013;15(8):658–663. doi: 10.1038/gim.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inott T, Kennedy BB. Assessing learning styles: Practical tips for patient education. The Nursing Clinics of North America. 2011;46(3):313–320. vi. doi: 10.1016/j.cnur.2011.05.006. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Nsiah-Kumi PA, Makoul G, Sager J, Zei CP, Glass S, … Baker DW. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Education and Counseling. 2009;75(3):321–327. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: A first look at the results of the National Adult Literacy Survey. 3. Washington, D.C: Office of Educational Research and Improvement, U.S. Department of Education; 1993. Retrieved from http://nces.ed.gov/pubs93/93275.pdf. [Google Scholar]
- Klitzman RL. Misunderstandings concerning genetics among patients confronting genetic disease. Journal of Genetic Counseling. 2010;19(5):430–446. doi: 10.1007/s10897-010-9307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koonce TY, Giuse NB, Choemprayong S, Hurley S, Martin SL, Epelbaum M, Kusnoor SV. Using personalized education delivery to improve community clinic patients’ knowledge of hypertension. Presented at the Special Libraries Association Annual Meeting; San Diego, California. 2013. Retrieved from http://dbiosla.org/events/past_sla_conference/San%20Diego/Personalized%20Education%20Delivery_Final%20Paper_2013.pdf. [Google Scholar]
- Koonce TY, Giuse NB, Storrow AB. A pilot study to evaluate learning style-tailored information prescriptions for hypertensive emergency department patients. Journal of the Medical Library Association: JMLA. 2011;99(4):280–289. doi: 10.3163/1536-5050.99.4.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusnoor SV, Justiss K, Stamm M, Naylor HM, Karabel BE, Lee P, … Giuse NB. Using health literacy and learning styles to improve patient understanding of genetics and personalized medicine. Presented at the Medical Library Association Annual Meeting; Austin, Texas. 2015. Retrieved from https://mla.socious.com/d/do/1923. [Google Scholar]
- Lanie AD, Jayaratne TE, Sheldon JP, Kardia SLR, Anderson ES, Feldbaum M, Petty EM. Exploring the public understanding of basic genetic concepts. Journal of Genetic Counseling. 2004;13(4):305–320. doi: 10.1023/b:jogc.0000035524.66944.6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW. Communicating genetic and genomic information: Health literacy and numeracy considerations. Public Health Genomics. 2011;14(4–5):279–289. doi: 10.1159/000294191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy MA, Lovly CM, Pao W. Translating genomic information into clinical medicine: Lung cancer as a paradigm. Genome Research. 2012;22(11):2101–2108. doi: 10.1101/gr.131128.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovly CM, Dahlman KB, Fohn LE, Su Z, Dias-Santagata D, Hicks DJ, … Pao W. Routine multiplex mutational profiling of melanomas enables enrollment in genotype-driven therapeutic trials. PloS One. 2012;7(4):e35309. doi: 10.1371/journal.pone.0035309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mainemelis C, Boyatzis RE, Kolb DA. Learning styles and adaptive flexibility: Testing experiential learning theory. Management Learning. 2002;33(1):5–33. [Google Scholar]
- Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. Journal of General Internal Medicine. 2006;21(8):813–817. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massachusetts General Cancer Center. Targeted Cancer Care: About. n.d Retrieved January 22, 2015, from https://targetedcancercare.massgeneral.org/About.aspx.
- McCray AT. Promoting health literacy. Journal of the American Medical Informatics Association: JAMIA. 2005;12(2):152–163. doi: 10.1197/jamia.M1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin GH. SMOG Grading - a new readability formula. Journal of Reading. 1969;12(8):639–646. [Google Scholar]
- McNaughton C, Wallston KA, Rothman RL, Marcovitz DE, Storrow AB. Short, subjective measures of numeracy and general health literacy in an adult emergency department. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine. 2011;18(11):1148–1155. doi: 10.1111/j.1553-2712.2011.01210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielson-Bohlman L, Panzer AM, Hamlin B, Kindig DA. Health literacy: A prescription to end confusion. Institute of Medicine of the National Academies; 2004. Retrieved from http://www.iom.edu/Reports/2004/Health-Literacy-A-Prescription-to-End-Confusion.aspx. [PubMed] [Google Scholar]
- Olsen L, Saunders RS, McGinnis JM. Patients charting the course: Citizen engagement in the learning health system: Workshop summary. Washington, D.C: National Academies Press; 2011. Retrieved from http://www.nap.edu/catalog/12848/patients-charting-the-course-citizen-engagement-in-the-learning-health. [PubMed] [Google Scholar]
- Parmar A. 7 consumer, big data healthcare apps you should know about. MedCity News. 2012 Jun 5; Retrieved from http://medcitynews.com/2012/06/seven-consumer-big-data-healthcare-apps-that-you-should-know-about/
- Pashler H, McDaniel M, Rohrer D, Bjork R. Learning styles: Concepts and evidence. Psychological Science in the Public Interest. 2009;9(3):105–119. doi: 10.1111/j.1539-6053.2009.01038.x. [DOI] [PubMed] [Google Scholar]
- Rodríguez SA, Roter DL, Castillo-Salgado C, Hooker GW, Erby LH. Translation and validation of a Spanish-language genetic health literacy screening tool. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2015;34(2):120–129. doi: 10.1037/hea0000162. [DOI] [PubMed] [Google Scholar]
- Rubinstein JC, Sznol M, Pavlick AC, Ariyan S, Cheng E, Bacchiocchi A, … Halaban R. Incidence of the V600K mutation among melanoma patients with BRAF mutations, and potential therapeutic response to the specific BRAF inhibitor PLX4032. Journal of Translational Medicine. 2010;8:67. doi: 10.1186/1479-5876-8-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabharwal S, Badarudeen S, Unes Kunju S. Readability of online patient education materials from the AAOS web site. Clinical Orthopaedics and Related Research. 2008;466(5):1245–1250. doi: 10.1007/s11999-008-0193-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalise D. Patient satisfaction and the new consumer. Hospitals & Health Networks / AHA. 2006;80(12):57, 59–62. [PubMed] [Google Scholar]
- Secretary’s Advisory Committee on Genetics, Health and Society. Genetics education and training. Bethesda, MD: Department of Health and Human Services; 2011. Retrieved from http://www.genome.gov/Pages/Careers/HealthProfessionalEducation/SACGHS-EducationReport2011.pdf. [Google Scholar]
- Spatz MA. Genetics Home Reference. Journal of the Medical Library Association. 2004;92(2):282–283. [Google Scholar]
- Stevenson FA, Kerr C, Murray E, Nazareth I. Information from the Internet and the doctor-patient relationship: The patient perspective--A qualitative study. BMC Family Practice. 2007;8:47. doi: 10.1186/1471-2296-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart D. Vanderbilt Medical Center Reporter. Nashville, TN: 2011. Mar 3, Vanderbilt-Ingram Cancer Center launches online genetic research tool. Retrieved from http://news.vanderbilt.edu/2011/03/vicc-online-genetic-research-tool/ [Google Scholar]
- Syurina EV, Brankovic I, Probst-Hensch N, Brand A. Genome-based health literacy: A new challenge for public health genomics. Public Health Genomics. 2011;14(4–5):201–210. doi: 10.1159/000324238. [DOI] [PubMed] [Google Scholar]
- Truluck JE, Courtenay BC. Learning style preferences among older adults. Educational Gerontology. 1999;25(3):221–236. doi: 10.1080/036012799267846. [DOI] [Google Scholar]
- University of Utah Genetic Science Learning Center. Learn.Genetics: Genetic Science Learning Center. n.d Retrieved January 22, 2015, from http://learn.genetics.utah.edu/
- Vanderbilt-Ingram Cancer Center. Fast facts. n.d Retrieved January 16, 2015, from http://www.vicc.org/about/facts.php.
- Vargas CR, Chuang DJ, Ganor O, Lee BT. Readability of online patient resources for the operative treatment of breast cancer. Surgery. 2014;156(2):311–318. doi: 10.1016/j.surg.2014.03.004. [DOI] [PubMed] [Google Scholar]
- Vargas CR, Koolen PGL, Chuang DJ, Ganor O, Lee BT. Online patient resources for breast reconstruction: An analysis of readability. Plastic and Reconstructive Surgery. 2014;134(3):406–413. doi: 10.1097/PRS.0000000000000472. [DOI] [PubMed] [Google Scholar]
- Wald HS, Dube CE, Anthony DC. Untangling the Web--The impact of Internet use on health care and the physician-patient relationship. Patient Education and Counseling. 2007;68(3):218–224. doi: 10.1016/j.pec.2007.05.016. [DOI] [PubMed] [Google Scholar]
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, … Hale FA. Quick assessment of literacy in primary care: the newest vital sign. Annals of Family Medicine. 2005;3(6):514–522. doi: 10.1370/afm.405. http://doi.org/10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White House, Office of the Press Secretary. FACT SHEET: President Obama’s Precision Medicine Initiative. 2015 Jan 30; Retrieved from http://www.whitehouse.gov/the-press-office/2015/01/30/fact-sheet-president-obama-s-precision-medicine-initiative.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


