Abstract
High-mobility group box 1 protein (HMGB1) is a highly conserved, non-histone and ubiquitous chromosomal protein found enriched in active chromatin forming part of the high mobility group family of proteins and is encoded by the HMGB1 gene (13q12) in human beings. It has various intranuclear and extracellular functions. It plays an important role in the pathogenesis of many diseases including cancer. In 2012, there was approximately 1.67 million new breast cancer cases diagnosed which makes it the second most frequent cancer in the world after lung cancer (25% of all cancers) and the commonest cancer among women. Both pre-clinical and clinical studies have suggested that HMGB1 might be a useful target in the management of breast cancer. This review summarises the structure and functions of HMGB1 and its dual role in carcinogenesis both as a pro-tumorigenic and anti-tumorigenic factor. It also sums up evidence from in vitro and in vivo studies using breast cancer cell lines and samples which demonstrate its influence in radiotherapy, chemotherapy and hormonal therapy in breast cancer. It may have particular importance in HER2 positive and metastatic breast cancer. It might pave the way for new breast cancer treatments through development of novel drugs, use of microRNAs (miRNAs), targeting breast cancer stem cells (CSCs) and breast cancer immunotherapy. It may also play a role in determining breast cancer prognosis. Thus HMGB1 may open up novel avenues in breast cancer management.
Keywords: Breast cancer, high-mobility group box 1 protein (HMGB1), amphoterin
Introduction
High-mobility group box 1 protein (HMGB1) [high-mobility group 1 protein (HMG1), amphoterin] which is a small (25 kDa), highly conserved, non-histone and ubiquitous chromosomal protein found enriched in active chromatin, forms part of the high mobility group family of proteins and is encoded by the HMGB1 gene (13q12) in human beings (1). HMGB1 is named after its high mobility in polyacrylamide gel. It is abundantly expressed in all tissues except neurons with highest levels present in thymus, liver and pancreas. Although the weight HMGB1 in the nucleus is very small as compared to histones or DNA content (only 3%) it is sufficient to carry out its function of gene derepression for which only few molecules per structural gene are required (2). It is present in almost all metazoans and plants. It is highly conserved because HMGB1 in rodents and human molecules have more than 99% amino acid identity. HMGB1 plays a role in the pathogenesis of many disease conditions including sepsis (3), ischemia-reperfusion (4), arthritis (5), meningitis (6), neurodegeneration (7), aging (8), and cancer. It is a pathogenic mediator in the inflammatory disease sepsis and is targeted to treat sepsis and rheumatoid arthritis (9).
In 2012, there was approximately 1.67 million new breast cancer cases diagnosed which makes it the second most frequent cancer in the world after lung cancer (25% of all cancers) and the commonest cancer among women. It is the most common cancer in women irrespective of the level of development of the region, with slightly more cases in less developed (883,000 cases) than in more developed (794,000 cases) regions. There is approximately a four-fold variation of incidence rate across the globe, with rates ranging from 27 per 100,000 in Middle Africa and Eastern Asia to 96 in Western Europe (10). In our hospitals the management of breast cancer is multi-disciplinary, involving surgery, radiotherapy, chemotherapy, hormonal therapy and use of immunotherapeutic agents with the treatment decision depending on the stage of the cancer. Although many options are available in the management of this disease, breast cancer has a high mortality rate. Patient management is affected by many hurdles. Indeed in initially 90% of primary breast cancers and 50% of metastases the drug regimen is effective but unfortunately treatment is stopped due to drug toxicity and drug resistance by many mechanisms including interruption of the apoptotic signalling pathway (11). In addition cancer treatment is expensive, notably immunotherapeutic agents, so that not every patient can afford the ideal treatment regimen, especially in developing countries. Thus the need for effective, safe and cost-effective alternatives is necessary.
This review summarises the structure and actions of HMGB1 as well as the pre-clinical and clinical evidence of how it can be directly and indirectly useful in breast cancer management.
Structure of HMGB1
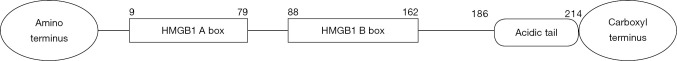
Figure 1 is a schematic diagram representing HMGB1.
Figure 1.
Schematic representation of HMGB1. HMGB1, high-mobility group box 1 protein.
HMGB1 belongs to high mobility group and has the HMG-box domain. It is a 214 amino acid long molecule and has two homologous DNA-binding domains termed A box and B box with A box spanning amino acids 9 to 79, B box spanning amino acids 88 to 162. The A and B box domains are responsible for binding to and bending of DNA. It has an acidic tail spanning amino acids 186–214. The acidic carboxyl region consists of a continuous stretch of glutamate and aspartate residues and is believed to interact with and protect the A box and B box during emigration from the nucleus (2,12,13). Following translation they are extensively glycosylated, acetylated, methylated, oxidized, and phosphorylated to perform specific functions (12,14,15). These modifications have specific importance like formation of a specific complex with homologous DNA polymerase-α to stimulate its activity (acetylation), translocation of HMGB1 from the nucleus to the cytoplasm (acetylation and phosphorylation) and cytoplasmic localization in neutrophils (methylation). HMGB1 release depends on a calcium or reactive oxygen species (ROS)-dependent mechanism (16,17). The expression of HMGB1 is regulated by transcription factors such as p53 (18), c-Myc (19), and Kruppel-like factor (KLF)-4 (20) in various cell types.
Functions of HMGB1
HMGB1 exerts various nuclear and extracellular functions. HMGB1 is located mainly in the nucleus where it helps the cell perform essential life functions so as to maintain a constant internal environment. Its absence in HMGB1 knockout mice causes their death within 24 hours of birth from hypoglycemia (21). It has a relatively high non-specific affinity for DNA and participates in DNA replication, transcription and modification The nuclear functions result from the A and B box domains allowing HMGB1 to bind DNA in a structure-specific fashion modifying transcriptional regulation and chromatin structure (22). Hence they are known as architectural transcription factors. HMGB1 also binds preferentially to damage DNA thus playing a role in DNA repair. Moreover the interaction between HMGB1 and transcription factors increases the activities of the latter. Thus enhanced activity of pro-carcinogenic transcription factors like p53, p73, the retinoblastoma (RB) protein, members of the Rel/NF-κB family and nuclear hormone receptors including the estrogen receptor (ER) stimulates carcinogenesis.
Almost all body tissues express HMGB1 in large amounts. Hence it is readily available to be translocated out of the nucleus into the cytosol from where it can be either actively or passively secreted. The extracellular functions are achieved when necrotic cells passively release HMGBI while activated macrophages actively secrete HMGBI which is hence known as a damage-associated molecular pattern molecule (DAMP). Release of HMGB1 in the tumor microenvironment has also resulted from cytolysis of human melanoma cells by immune effectors (both activated NK and T cells) (23). Cell death following necrosis, caspase-dependent apoptosis and hypermembrane permeability all lead to HMGB1 release. However cells undergoing apoptosis release HMGB1 slowly and the process occurs late during aponeurosis when phagocytic cells are not available. As a result HMGB1 binds with high affinity to several DAMP receptors including the receptor for advanced glycation end products (RAGE), Toll-like receptors (TLR)-2, TLR-4, TLR-9, and CD24. HMGB1 is the only member of the high mobility group of proteins that has been shown to activate RAGE while small interfering RNA (siRNA) suppresses TLR4 and subsequently diminishes tumor growth in various mouse models (24).
Role of HMGB1 in carcinogenesis
HMGB1 has a complex role in carcinogenesis because it has both pro- and anti-tumorigenic bioactivities. HMGB1 upregulation or down-regulation varies with the type of cancer. Even in a particular cancer it may show a spectrum of expression as evidenced by a significant intertumoral variation of HMGB1 expression which has been reported in different breast cancers (25). Another reason for their complex interaction is that cancer cells killed by chemotherapy, virotherapy or radiotherapy release HMGB1 in a pulsatile fashion and it may complex with soluble moieties in tumors (e.g., nucleic acids, microbial products, and cytokines) to exert its inflammatory properties (26-28). However when a tumour grows it secretes HMGB1 chronically so that it does not form complexes or it may need to be specifically modified post-translationally (e.g., oxidation) to be able to promote tumor invasion, metastasis or immune tolerance (29-31).
HMGB1 suppresses tumorigenesis by interacting with tumor suppressor genes like p53, p73 (the first identified homologue of p53) and RB. It bends and binds DNA providing the optimal structure for p53 binding (32). It physically interacts with the two splicing variants of p73 (p73α and p73β), and enhances binding of p73 to specific cognate DNA sites. It associates with RB via an LXCXE motif-dependent interaction mechanism (33). It enhances the ability of RB to repress both E2F and cyclin-A transcription (34,35).
Moreover HMGB1 has mixed effects on the hallmarks of cancer namely unlimited replicative potential, ability to develop blood vessels (angiogenesis), evasion of programmed cell death (apoptosis), self-sufficiency in growth signals, insensitivity to inhibitors of growth, and tissue invasion and metastasis with the seventh feature suggested to be inflammation (36-38). Up-regulation of HMGB1 is associated with decreased apoptosis and hence pro-carcinogenic effect. For example overexpression of HMGB1 in K562 leukemia cells sustains Bcl-2 protein expression and inhibits adriamycin (ADM)-induced activation of caspase-3 and -9 (39). On the other hand suppression of HMGB1 by siRNA in K562/A02 leukemia cells reverses the resistance to ADM, and significantly promotes ADM-induced Smac/DIABLO release from the mitochondria to the cytoplasm, increasing the activation of caspase-3 (40). Paradoxically HMGB1 overexpression has been associated with increased apoptosis when breast cancer cell lines have been treated with anti-cancer drugs and radiation thereby sensitizing them (33,41,42). HMGB1 promotes angiogenesis by binding to its receptor RAGE, activating NF-κB upregulating leukocyte adhesion molecules and the production of proinflammatory cytokines and angiogenic factors in both hematopoietic and endothelial cells (43). Antibody targeting HMGB1 inhibits angiogenesis in vitro and in vivo (44). HMGB1 plays a role in unlimited replication of cancer cells by dissociating from chromosomes during mitosis and participating in telomere maintenance (45). When present in the extracellular matrix, it binds to the RAGE-products mediating tumor growth, invasion and metastasis (29,46-49). HMGB1 interacts with RAGE activating p44/p42, p38 and SAP/JNK MAP kinases which is linked to tumor proliferation, invasion and expression of matrix metalloproteinases (MMPs) (49). If we block the RAGE-HMGB1 axis by using soluble RAGE, anti-RAGE and/or anti-HMGB1 Ab, this will inhibit tumor growth and metastases, leading to therapeutic potential. Antigrowth signals inhibit proliferation by forcing cells out of the active proliferative cycle into the quiescent (G0) state from which they exit later when extracellular signals permit or inducing them to enter into postmitotic states, usually associated with acquisition of specific differentiation-associated traits. HMGB-1 overexpression alone does not change the MCF-7 cell cycle progression, but the addition of estrogen to the HMGB1 overexpressing MCF-7 cells appears to accelerate the cell cycle progression (50). HMGB1 activates signaling pathways involving protein kinase B (AKT), mitogen-activated protein kinases (MAPKs), and NF-κB, which play important role in tumor growth. In tumor cells, mutations in genes encoding the NF-κB transcription factors or in genes that control NF-κB activity (such as IκB genes) or by tumor secreted factors activate NF-κB. Drosophila protein DSP1, an HMG-1/2-like protein, binds DNA highly cooperatively with three members of the Rel family of transcriptional regulators (NF-kappaB, the p50 subunit of NF-kappaB, and the Rel domain of Dorsal) (51), thus promoting tumor activity. When estrogen binds to the ER, it causes mammary cells to proliferate, with the resulting increase in cell division and DNA replication, leading to mutations. ER is a ligand-inducible nuclear receptors and it binds to cis-acting DNA elements in the regulatory region of target genes. HMGB1 enhances the action of oestrogen by interacting with ER and promoting estrogen response element (ERE) binding in a concentration- and time-dependent manner (52,53) and facilitating strong ER binding to ERE consensus half-sites (54).
HMGB1 plays an important immunogenic role which again can be both pro-tumorigenic and anti-tumorigenic. Tumor cells can act as antigens and elicit an immune response (55). In murine models extracellular HMGB1 activates dendritic cells and induces protective immune response against poorly immunogenic apoptotic lymphoma cells (56). In addition chemotherapeutic agents like alkylating agents and taxanes are more effective than others like oxaliplatin because they are more effective in causing translocation of HMGB1 out of the nucleus to be then released extracellularly where it exerts its immunogenic function (57,58). Also factors which prevent the binding of HMGB1 to dendritic cells leads to failure of immunogenic function of HMGB1. For example DCs derived from individuals bearing the variant TLR4 allele poorly cross presented the MART-1 tumor antigen from dying melanoma cells to specific T cells (26).
However, HMGB1 released by tumour cells into the tumor microenvironment could promote immune escape by inhibiting conventional T cells, Tcon and activating regulatory T cells, Tregs (formerly known as suppressor T cells) thus causing tumors to grow. Tregs is a subpopulation of T cells which modulate the immune system, maintain tolerance to self-antigens, and abrogate autoimmune disease. These cells generally suppress or downregulate induction and proliferation of effector T cells. HMGB1 may also promote carcinogenesis through its interaction as a ligand with TLR4 and RAGE expressed on Treg thus modulating its function. By causing Treg to release IL-10, HMGB1 promotes Treg survival and enhances their immune inhibitory functions in a RAGE dependent manner and limits the number and activity of Tcon in the setting of chronic inflammatory states such as cancer (59). HMGB1 released by cancer cells causes Tregs to produce IL-10 which not only enhances the immunosuppressant action of Tregs but also suppresses antitumor immunity action of CD8 T cells (60). Thus HMGB1 knock-down will prevent tumor growth in vivo by boosting body immunity and changing tumor phenotype so that cancer cells are more susceptible to be killed by cytotoxic T lymphocytes which operate in an unopposed manner following Treg deactivation. HMGB1, released from dying tumor cells following chemotherapy, virotherapy or radiotherapy, stimulates mature dendritic cells (mDC) to process tumor antigen through its interaction with TLR-2/4 or activates innate immunity, leading to an antitumor immune response therefore acting as a ‘danger’ molecule (26-28). For these reasons HMGB1 knockdown may be beneficial and HMGB1 mAb (neutralizing HMGB1 signaling), siRNA HMGB1 (to cause HMGB1 KD) or using glycyrrhizin (a specific inhibitor of extracellular HMGB1) may enhance the anti-tumour action of CD8 T cells.
Potential applications of HMGB1 in breast cancer
Radiation therapy
Radiation therapy is an essential component in the multimodality treatment of breast cancer. It is indicated in early stage cancer following lumpectomy, in localized breast cancer following breast conserving surgery, in locally advanced breast cancer following breast conserving surgery or modified radical mastectomy and in metastatic breast cancer as palliative therapy. Pre-clinical studies have shown conflicting roles of HMGB1 as far as radiosensitization is concerned.
Apetoh et al. (61) found that HMGB1 sensitized breast cancer cells to radiation by its immunogenic action. When the mammary adenocarcinoma cell line TS/A was injected in mice, it produced tumors which were sensitive to radiation in immunocompetent mice but not in nu/nu mice. They suggested that the cells exposed to radiation can elicit cognate immune response which contributes to sensitize the tumor cells to radiation. They showed that ionizing radiation which killed the cells promoted HMGB1 release from the dying tumor cells. HMGB1 release increases the immunogenicity of cell death because HMGB1 binds to TLR4 which is expressed by dendritic cells preventing other ligands released by agonizing tumor cells from binding to antigen-presenting cells. During radiotherapy dendritic cells require signaling through TLR4 and its adaptor MyD88 to efficiently process and cross-present antigens from dying tumour cells. Breast cancer patients with a loss of function TLR4 allele relapse more quickly after radiotherapy than those patients carrying the normal TLR4 allele (26).
Jiao et al. (33) confirmed the role of HMGB1 as a radiosensitizer in breast cancer and also investigated its potential association with RB-binding LXCXE motif. They found that HMGB1 enhanced the radiosensitivity of both MCF-7 cells (containing the wild-type Rb gene) and BT-549 cells (containing the Rb gene deletion). HMGB1-RB interaction is not needed for radiosensitization but is important for its tumor suppressor role (transcriptional repression, cell growth inhibition, G1 cell cycle arrest, apoptosis induction). When HMGB1 expression is increased, it suppresses E2F and cyclin A transcriptional activation which is mediated by RB. However HMGB1 on its own does not affect E2F and cyclin A transcriptional activity. When RB binds to the LXCXE motif of the HMGB1 sequence, it acts as a bridge to cause simultaneous contact between HMGB1 and E2F1.
On the other hand, Ke et al. (62) showed that HMGB1 decreases radiosensitivity, interferes with telomere homeostasis, and prevents radiation-induced DNA damage repair in human breast cancer cells, thus confirming the role of HMGB1 in cancer cells in replenishing telomeric DNA and maintaining cell immortality. When ShRNA silenced HMGB1 expression in MCF-7 cells, they became more radio-sensitive and caused the amount of hTERT (human telomerase reverse transcriptase) and cyclin D1 to decrease. Moreover, knockdown of HMGB1 in MCF-7 cells inhibited telomerase activity and cell proliferation but increased apoptosis. When HMGB1 is downregulated it alters the level of telomere-binding proteins, such as TPP1 (PTOP), TRF1 and TRF2 while simultaneously inhibiting the ATM and ATR signaling pathways. Thus the authors suggested HMGB1knockdown as a potential therapeutic manoeuvre in radiotherapy.
Chemotherapy
Chemotherapy is another component in the multi-modality management of breast cancer. It includes neoadjuvant chemotherapy which refers to drugs given before the main treatment like before surgery, adjuvant chemotherapy in which drugs are given after the main treatment like after surgery and palliative chemotherapy. It is indicated in stages 1 to 4 in breast cancer. First generation regimens include CMF (cyclophosphamide, methotrexate, 5-FU), second generation regimens include CEF (cyclophosphamide, epirubicin, 5-FU), FAC (5-FU, ADM, cyclophosphamide) while third generation regimens include TAC (docetaxel, ADM, cyclophosphamide) and FEC-D/T (5-FU, epirubicin, cyclophosphamide, docetaxel or paclitaxel). Interestingly it is now recognized that conventional chemotherapeutic agents not only kill cancer cells by apoptosis but also induce nonapoptotic death like necrosis and autophagy (63). Since HMGB1 plays a role in apoptosis, autophagy and necrosis it can lead to development of novel combination therapies with traditional anti-cancer agents.
One the problems associated with chemotherapy is failure leading to patient relapse. One study showed that the presence of HMGB1 along with cytoplasmic MAP1LC3B/LC3B (microtubule-associated protein 1 light chain 3B)-positive puncta is associated with longer survival in breast cancer patients after adjuvant chemotherapy (64). The authors compared the immunohistochemistry in the surgical breast cancer specimens in the validation cohort comprising of 1,646 localized breast cancer patients who received adjuvant anthracycline-based chemotherapy compared to the 152 patients in the test cohort. They found that the proteins alone could not be used as an independent prognostic factor for metastasis-free survival (MFS). However the combination constituted an independent prognostic factor significantly increasing MFS (hazard ratio: 0.49, 95% confidence interval, 0.26–0.89; P=0.02), and improving breast cancer specific survival (hazard ratio: 0.21, 95% confidence interval, 0.05–0.85; P=0.029). When subgroups were analysed it was found that within patients with poor-prognosis breast cancer, HMGB1(+) LC3B(+) double-positive tumors had a better prognosis than those breast cancers lacking one or both of these markers. So analysis of breast cancer specimens for MAP1LC3B/LC3B and HMGB1 can direct the choice of the chemotherapy regimen.
Tumor-associated stromal cells cause acquired drug resistance by preventing cancer cells from dying and protecting them from cytotoxic effect of anti-cancer agents (65,66). Another study showed that stromal fibroblast-induced HMGB1 production was partly responsible for resistance to doxorubicin in breast cancer cells (67). The authors basically isolated breast cancer-associated fibroblasts (BCFs) and non-tumor-associated fibroblasts (NTFs), measured HMGB1 level intracellularly and extracellularly in MDA-MB-231 cells, compared the cells response to doxorubicin following pre-treatment with BCF and NTF and investigated the effect of an HMGB1 neutralizing antibody on doxorubicin resistance. They found that pretreatment with BCF increased the migratory potential of cancer cells, increased both intracellular and extracellular HMGB1 levels of doxorubicin-treated cells and induced chemoresistance which correlated with the level of secreted HMGB1. Recombinant HMGB1 induced autophagy leading to chemoresistance while anti-HMGB1 neutralizing antibody reversed the chemoresistance. Thus targeting extracellular HMGB1 which is responsible for chemoresistance may be beneficial while targeting the more genetically stable cancer-associated fibroblasts is another approach in cancer therapy.
Neoadjuvant chemotherapy in breast cancer aims to reduce the tumor size before surgery to improve the outcome of surgery and prognosis. However not all patients respond positively to this treatment modality and so it is necessary to predict the responders to be able to adapt the treatment and prevent the use of less effective agents thereby minimizing the associated side-effects. Stoetzer et al. (68) showed that HMGB1 could be used to predict neoadjuvant therapy response in locally confined breast cancer. Kinetics of HMGB1 during therapy correlated with efficacy of the treatment (P=0.053). Their opinion was confirmed by Arnold et al. (69) who showed that HCC1143 breast cancer cells treated with epirubicin/docetaxel significantly released HMGB-1 in vitro while in vivo out of 41 patients who were treated with the drug combination 22 responders showing pathological complete response or partial remission also showed a significant increase in HMGB1 level while the remaining 19 did not respond and also did not show any significant change in plasma HMGB1 level. Breast cancer patients receiving epirubicin/docetaxel-based neoadjuvant therapy can have their plasma HMGB1 measured using a commercially available ELISA kit and can easily participate in neoadjuvant trials in breast cancer to confirm HMGB-1 as an early response marker to neoadjuvant chemotherapy.
The level HMGB1 released by dying tumor cells can be used to determine the immunogenicity and effectiveness of chemotherapeutic regimens. HMGB1 binds to TLR4 receptors on dendritic cells which selectively cross-prime anti-tumor T lymphocytes in vivo. A TLR4 polymorphism that affects the binding of HMGB1 to TLR4 predicts early relapse after anthracycline-based chemotherapy in breast cancer patients (61). During chemotherapy dendritic cells require signaling through TLR4 and its adaptor MyD88 to efficiently process and cross-present antigens from dying tumour cells. Breast cancer patients with a loss of function TLR4 allele relapse more quickly after chemotherapy than those patients carrying the normal TLR4 allele (26). Breast cancer patients harboring the loss-of-function Asp299Gly polymorphism of TLR4 relapsed earlier after receiving anthracycline-based chemotherapy (70). The latter is the result of a retrospective cohort of 280 breast cancer patients who presented with metastatic lymph node disease and treated with local radiotherapy and anthracycline-based adjuvant chemotherapy. The frequency of monoallelic expression of the Asp299Gly polymorphisms in this cohort was 17.1%. There was no significant association between TLR4 allele mutation and classic prognostic factors like age, pathologic tumor size, lymph node involvement, tumor grade, hormone receptors, and median follow up. However when normal and cancer patients were compared, MFS was significantly decreased in women carrying the variant allele of TLR4 (50% of relapse in mutated versus 37.4% in nonmutated patients at 10 years; Log-rank test, P=0.03). Thus TLR4 mutation can independently predict the success of anthracycline-based adjuvant regimen.
HMGB1 experiments have led us to rethink about current practice in cancer treatment. Cancer cause immunosuppression and the success of chemotherapy also depends on the efficacy of the drugs to boost the immune system. High dose glucocorticoids are administered along with chemotherapy to reduce side effects like vomiting. However steroids are potent immunosupressants (71) which decrease the immunoadjuvant effect of anti-cancer drugs. Also the advantage of neoadjuvant therapy over adjuvant therapy is increased delivery of tumor antigens like HMGB1 and hence a better immune response.
Interaction between HMGB1 and hormones in breast cancer
Many breast carcinomas express high levels of ER, progesterone receptor (PR) or both (72). While high estrogen level is considered a risk factor for breast cancer ER status is an important determinant of adjuvant therapy. Breast cancer patients who are ER positive are given anti-estrogen therapy in the form of tamoxifen (in premenopausal and postmenopausal women) and aromatase inhibitors like anastrozole and letrozole (in postmenopausal women).
17β-estradiol (E2), along with estrone and estriol, is one of the three major oestrogens in women and exerts genomic and non-genomic effects in a variety of cell types, such as breast cancer cells. E2 regulates cell growth by mediating autophagy and apoptosis in breast cancer cells. In one study the authors found that HMGB1 is involved in E2-mediated pro-autophagy and anti-apoptotic processes by the caveolin-1/HMGB1 pathway (73). They showed that E2 promoted the expression of not only both caveolin-1 and HMGB1 but also autophagy-related proteins (LC3-II, Beclin-1 and Atg12/5). When HMGB1 was down-regulated it caused a decrease in the expression of Beclin-1 and LC3-II thus attenuating autophgosome formation and promoting apoptosis. Furthermore, caveolin-1 or HMGB1 knockdown significantly suppressed E2-induced cell growth. Thus the researchers suggested that caveolin-1/HMGB1 axis positively regulates E2-induced cell growth by promoting autophagy and inhibiting apoptosis in BT474 cells.
In another study (41), the authors found that treating breast cancer MCF-7 cells with estrogen and/or progesterone according to the receptor positivity sensitize them to cisplatin and carboplatin by inducing HMGB1 over expression. Hence we can use lower doses of the drug reducing the side effects of nephrotoxicity, myelosuppression, neurotoxicity and emesis (74). In breast cancer oestrogen causes proliferation, so progesterone may be preferred. The researchers suggested that endogenous HMGB1 proteins are already involved in complexes with chromatin and transcription factors and HMGB1 transiently expressed as a scaffold to facilitate ER or PR-mediated transcription could more readily bind to cisplatin-DNA intrastrand crosslinks. A 2-fold increase in cisplatin sensitization was associated with a 2-fold increase in HMGB1 protein levels which may be very useful clinically. HMGB1 facilitates the binding of PR by inducing a structural change in the target DNA (75). HMGB1 and TAF(II)30 act in sequence, the former acting to promote ER-ERE binding followed by the latter to stimulate transcription initiation (53). The 2- to 3-fold increase in HMGB1expression observed in proliferating cells or breast cancer cells stimulated by estrogen may probably result from the action of the enhancer elements in intron 1 (76). Another study showed that estrogen induces overexpression of HMGB1 which shields cisplatin-DNA adducts from nucleotide excision repair (NER) (77).
HMGB1 in HER2-positive breast cancers
HER2 receptor positivity is a prognostic factor for breast cancer. HER2 gene amplification or over-expression occurs in about 15–30% of breast cancers (78). It strongly correlates with increased disease recurrence and a poor prognosis (79). The monoclonal antibody trastuzumab (Herceptin) is indicated in those cancers over-expressing HER2.
Tumor infiltrating lymphocytes (TILs) are present in tumors and are involved in cancer cell killing and so their presence is associated with better clinical outcome. Lee et al. (80) investigated whether there was an association between TILs and the immunohistochemical expression of HMGB1 and HMGN1 in 447 HER2-positive breast cancer tissues. They found that high levels of cytoplasmic HMGB1 and HMGN1 protein expression correlated with high levels of TILs in HER2-positive breast cancers and suggested targeting HMGB1 and HMGN1 as an immunotherapeutic approach to promote TIL influx into a tumor thus enhancing antitumor immunity. High levels of HMGB1 or HMGN1 in the cytoplasm of tumor cells were significantly associated with increased TILs, peritumoral lymphocytic infiltration, and tertiary lymphoid structures (TLSs). Immunogenic cell death (ICD) in HER2-positive breast cancer may potentially be achieved by evaluating the status of HMGB1 expression and manipulating HMGB1 expression and location.
Development of novel anti-cancer drugs against breast cancer
The therapeutic potential of quercetin as an anti-cancer agent, a flavonol found in many fruits, vegetables, leaves and grains, is still at an early stage. Dhumale et al. (81) found that it induced apoptosis in MCF-7 cells and also protect them from necrotic insult. The mechanism involved is inhibition of the expression of RAGE and HMGB1 leading to failure of activation of NF-κB, reduced synthesis of several proinflammatory cytokines and hence elevated apoptosis. Quercetin inhibits the expression of RAGE and HMGB1 at transcriptional and post-transcriptional levels. It inhibits the nuclear translocation of p65 from cytosol to hinder NF-κB activation. It protects against necrotic cell death by inhibiting the release of LDH (an indicator of cytotoxic or necrotic cell death) and HMGB1 in the presence of necrotic inducer.
Drug resistance in cancer therapy is a major problem which needs to be circumvented. For example in the case of cisplatin which is a widely used anticancer drug, one of the solutions is the synthesis of estrogen-tethered platinum(IV) complexes, the mechanism of action of which involves HMGB1 which might prove valuable as novel anticancer drug candidates (42). The proposed mechanism of action for estrogen-tethered platinum(IV) complexes involves the reduction of platinum(IV) to platinum(II) by the reducing environment of the cell leading to release of cisplatin and two equivalents of a modified estrogen. Upregulation of HMGB1 will shield cisplatin-DNA crosslinks from repair and enhance cell death. HMG-domain proteins specifically inhibit the repair of the major DNA adduct of cisplatin by human excision nuclease (77). The authors synthesized several novel estrogen-tethered platinum(IV) complexes and evaluated their ability to upregulate HMGB1, as well as screened them for cytotoxicity against breast cancer cell lines. All BEPn complexes (bis-estrogen-cis-diamminedichloroplatinum(IV), BEPn (where n=1–5 methylene groups between Pt and estrogen), induced the overexpression of HMGB1 in ER(+) MCF-7 cells. BEP3 was nearly 2-fold more cytotoxic in ER(+) MCF-7 cells than in ER(−) HCC-1937 cells. Thus these compounds can be used to specifically target ER(+) malignancies, such breast and ovarian cancers. Synthesis of the BEPn compounds is not only a novel method to develop new platinum-containing anticancer agents but also the chemistry involved can be used to attach other moieties to direct platinum complexes more effectively to cancer cells.
Side-effects of cytotoxic drugs need to be minimized in different ways like giving adjuvant non-chemotherapeutic drugs. HMGB1 release is one mechanism of such drug, apicidin. In one study (82), the authors used epigenetic modulator apicidin combined with low dose cytotoxic agent docetaxel in tumor breast cell lines having different grades of invasiveness. They found that the combination induce signals of immunogenic apoptosis such as cell surface expression of calreticulin and release of significant amounts of HMGB1, thus causing the cell death to induce an antitumor immune response along with increased apoptosis.
Role of HMGB1 in breast cancer metastasis
In advanced cases of breast cancer tumor cells usually metastasize to bone (commonest site), liver and lung. Bone complications include pathological fractures and spinal cord compression. The ability of cancer to invade local tissues and subsequently metastasize to distant organs is responsible for the associated mortality and morbidity. Metastasis is a multi-step process which includes cell detachment from primary tumor, entry in circulation, extravasation at distant site and proliferation in distant organ parenchyma. Each step involves different proteins, proteases, adhesion molecules, motility factors, and angiogenic factors and since HMGB1 affects the gene transcription of these proteins of the metastatic cascade it has therapeutic potential.
HMGB1 and microRNAs (miRNAs)
A miRNA is a small, non-coding RNA molecule (containing about 22 nucleotides) found in plants, animals, and some viruses, which plays a role in RNA silencing and post-transcriptional regulation of gene expression. Several miRNAs have been linked to HMGB1. One of them is miR-200c which was previously shown to regulate epithelial-mesenchymal transition (EMT) by inhibiting ZEB1 and ZEB2 expression in breast cancer cells (83). In their study the authors found that miR-200c also regulated HMGB1 gene expression. When MDA-MB-231 cells were transfected with the miR-200c mimic or inhibitor, the HMGB1 levels decreased and increased respectively. When the HMGB1 expression was silenced, the invasive and migratory capacities of the cells were impaired. The ability of miR-200c to suppress the invasion and migration of breast cancer cells by down-regulating the expression of HMGB1 implies that both of them may become useful biomarkers for progression of breast cancer and targets of gene therapy.
According to one study breast cancer cells which were radio-resistant strongly induced autophagy post irradiation which protected them against the effects of radiation (84). Luo et al. (85) showed that the miR-129-5p/HMGB1 axis is involved in the regulation of irradiation-induced autophagy and radiosensitivity of breast cancer cells. In breast cancer cells miR-129-5p directly targets the functions of HMGB1 and increases radiosensitivity. The researchers found that miR-129-5p made MDA-MD-231 cells more susceptible to radiation, miR-129-5p knockdown made MCF-7 cells less sensitive to radiation while miR-129-5p overexpression inhibited irradiation-induced autophagy.
Breast cancer stem cells (CSCs)
CSCs are slow dividing cancer-initiating cells endowed with stem cell properties, such as the capacity to self-renew and to reestablish tumor heterogeneity. They constitute only a small fraction of the tumor mass but are chemo- and radioresistant and possess immune-evasive features. Treatment fails to eliminate them and so they cause the tumor to grow again resulting in tumor progression, metastasis, resistance to therapy, and tumor recurrence (86,87). Conti et al. (88) showed that murine and human mammary CSCs express TLR2 and its ligand HMGB1. TLR2 signaling inhibition impaired in mammosphere generation in both murine and human mammary cell lines in different proportions including triple-negative breast cancer (TNBC) lines. TNBC is one of the most aggressive forms of human breast cancer, characterized by a unique molecular profile, aggressive behavior, and a distinctive metastasis pattern in both human and mouse breast cancer. The axis HMGB1/TLR2 determines NF-κB activation, IL-6 and TGF-β production, and STAT3 and Smad3 activation. IL-6 activates STAT3 and expands breast CSC population. TGF-β signaling has been implicated in the maintenance and survival of CSC populations, resulting in enhanced metastatic ability. TLR2 acts as an intrinsic mechanism for CSC proliferation and tumorigenic ability in vivo, regardless of its immune-related effects. Since box A, the competitive antagonist of HMGB1, inhibited mammosphere generation the authors suggested that HMGB1 inhibitors could be applied in cancer therapy.
HMGB1 and breast cancer prognosis
Kostova et al. (89) suggested that HMGB1 and RAGE expression and their exact location in the cell, and the state of tumor differentiation can be used as a prognosis in cancer including breast cancer. They investigated tissue samples from several cancers (colorectal, hepatocellular, testicular) including 72 cases of ductal breast carcinoma (38 cases of cribriform type). During immunohistochemical analysis of breast cancer samples they found that HMGB1 in malignant tissue sections showed stronger immunoreactivity than in normal tissue. In contrast to moderately differentiated ductal breast carcinomas in which HMGB1 had a perinuclear location, invasive cribriform carcinomas showed a strong immune reaction in the whole nucleus of the cells which form a duct like pattern consisting of cellular bridges but perinuclear localization of HMGB1 was absent. In addition the RAGE level varied according to the tumor type. In all cribriform carcinoma specimens, a positive cytoplasmic diffuse signal was seen in the duct like structure while the weak immunoreactivity in case of the moderately differentiated ductal carcinoma samples meant that only a few cells with granular positive immune reaction could be seen. No normal tissue samples showed the presence of RAGE.
HMGB1, immunotherapy and breast cancer
Whole-cell vaccines provide target antigens. The whole tumor cell is the source of immunogens which induce an antitumor immune response. The advantage of using whole tumor cell vaccine, also known as polyvalent vaccine, include minimal immune escape with presentation of wide variety of tumor-associated antigens (TAAs) and no HLA restrictions as whole proteins are present. However, live pathogens are not safe. Killing the cancer cells but maintaining immunogenicity via γ-irradiation may be beneficial. Also many cancers may be weakly immunogenic.
Yan et al. (90) lethally irradiated, 4T1 cells which are a weakly immunogenic and highly metastatic murine mammary cancer model, infected them with AdVEGFR2 which is a recombinant adenovirus carrying the VEGFR2 gene and used them to vaccinate mice. In vaccinated mice tumor growth and pulmonary metastasis were inhibited as compared to non-vaccinated mice. Also vaccination inhibited angiogenesis and increased number of CD8+ T lymphocytes within the tumors. Antitumor activity was also caused by the adoptive transfer of isolated spleen lymphocytes. Activation of tumor antigen-specific T-cell immunity involves secretion or surface exposure of the HMGB1 alarmin protein and HSP70 by dying tumor cells. HMGB1 and HSP70 were upregulated in the irradiated AdVEGFR2-infected 4T1 cells. In vitro, the AdVEGFR2 infected 4T1 cells showed increased expression of HMGB1 and HSP70 which activated tumor antigen-specific T-cell immunity. Hence this vaccine may be useful in the treatment of breast cancer.
Conclusions
HMGB1 is a protein with multiple functions and thus is implicated in a variety of diseases. Increasing evidence shows its implication in carcinogenesis including breast cancer. In this review, the implication of HMGB1 in breast cancer has been summarised. Addition of HMGB1 targets in the multi-modality treatment of breast cancer may open new therapeutic avenues in breast cancer management. Nevertheless its paradoxical dual effect on tumors warrants further studies which will be essential to understand specificity of interactions, under which conditions to target HMGB1 so as to cause anti-tumor activity, and the possibility of providing selective anti-tumour action without affecting normal host defense mechanisms.
Acknowledgements
Funding: This work was supported by grants from the National Natural Science Foundation of China (No. 81101677).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Ferrari S, Finelli P, Rocchi M, et al. The active gene that encodes human high mobility group 1 protein (HMG1) contains introns and maps to chromosome 13. Genomics 1996;35:367-71. 10.1006/geno.1996.0369 [DOI] [PubMed] [Google Scholar]
- 2.Goodwin GH, Johns EW. The isolation and purification of the high mobility group (HMG) nonhistone chromosomal proteins. Methods Cell Biol 1977;16:257-67. 10.1016/S0091-679X(08)60104-1 [DOI] [PubMed] [Google Scholar]
- 3.Wang H, Yang H, Tracey KJ. Extracellular role of HMGB1 in inflammation and sepsis. J Intern Med 2004;255:320-31. 10.1111/j.1365-2796.2003.01302.x [DOI] [PubMed] [Google Scholar]
- 4.Tsung A, Sahai R, Tanaka H, et al. The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion. J Exp Med 2005;201:1135-43. 10.1084/jem.20042614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersson U, Tracey KJ. HMGB1 as a mediator of necrosis-induced inflammation and a therapeutic target in arthritis. Rheum Dis Clin North Am 2004;30:627-37, xi. 10.1016/j.rdc.2004.04.007 [DOI] [PubMed] [Google Scholar]
- 6.Tang D, Kang R, Cao L, et al. A pilot study to detect high mobility group box 1 and heat shock protein 72 in cerebrospinal fluid of pediatric patients with meningitis. Crit Care Med 2008;36:291-5. 10.1097/01.CCM.0000295316.86942.CE [DOI] [PubMed] [Google Scholar]
- 7.Qi ML, Tagawa K, Enokido Y, et al. Proteome analysis of soluble nuclear proteins reveals that HMGB1/2 suppress genotoxic stress in polyglutamine diseases. Nat Cell Biol 2007;9:402-14. 10.1038/ncb1553 [DOI] [PubMed] [Google Scholar]
- 8.Enokido Y, Yoshitake A, Ito H, et al. Age-dependent change of HMGB1 and DNA double-strand break accumulation in mouse brain. Biochem Biophys Res Commun 2008;376:128-33. 10.1016/j.bbrc.2008.08.108 [DOI] [PubMed] [Google Scholar]
- 9.Ulloa L, Messmer D. High-mobility group box 1 (HMGB1) protein: friend and foe. Cytokine Growth Factor Rev 2006;17:189-201. 10.1016/j.cytogfr.2006.01.003 [DOI] [PubMed] [Google Scholar]
- 10.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer. Available online: http://globocan.iarc.fr. Accessed on 22/04/2015.
- 11.Guchelaar HJ, Vermes A, Vermes I, et al. Apoptosis: molecular mechanisms and implications for cancer chemotherapy. Pharm World Sci 1997;19:119-25. 10.1023/A:1008654316572 [DOI] [PubMed] [Google Scholar]
- 12.Lotze MT, Tracey KJ. High-mobility group box 1 protein (HMGB1): nuclear weapon in the immune arsenal. Nat Rev Immunol 2005;5:331-42. 10.1038/nri1594 [DOI] [PubMed] [Google Scholar]
- 13.Bustin M, Lehn DA, Landsman D. Structural features of the HMG chromosomal proteins and their genes. Biochim Biophys Acta 1990;1049:231-43. 10.1016/0167-4781(90)90092-G [DOI] [PubMed] [Google Scholar]
- 14.Müller S, Scaffidi P, Degryse B, et al. New EMBO members' review: the double life of HMGB1 chromatin protein: architectural factor and extracellular signal. EMBO J 2001;20:4337-40. 10.1093/emboj/20.16.4337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexandrova EA, Beltchev BG. Differences between HMG1 proteins isolated from normal and tumour cells. Biochim Biophys Acta 1987;915:399-405. 10.1016/0167-4838(87)90026-4 [DOI] [PubMed] [Google Scholar]
- 16.Oh YJ, Youn JH, Ji Y, et al. HMGB1 is phosphorylated by classical protein kinase C and is secreted by a calcium-dependent mechanism. J Immunol 2009;182:5800-9. 10.4049/jimmunol.0801873 [DOI] [PubMed] [Google Scholar]
- 17.Tang D, Shi Y, Kang R, et al. Hydrogen peroxide stimulates macrophages and monocytes to actively release HMGB1. J Leukoc Biol 2007;81:741-7. 10.1189/jlb.0806540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uramoto H, Izumi H, Nagatani G, et al. Physical interaction of tumour suppressor p53/p73 with CCAAT-binding transcription factor 2 (CTF2) and differential regulation of human high-mobility group 1 (HMG1) gene expression. Biochem J 2003;371:301-10. 10.1042/bj20021646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rothermund K, Rogulski K, Fernandes E, et al. C-Myc-independent restoration of multiple phenotypes by two C-Myc target genes with overlapping functions. Cancer Res 2005;65:2097-107. 10.1158/0008-5472.CAN-04-2928 [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Liu Y, Zhang H, et al. KLF4 promotes the expression, translocation, and releas eof HMGB1 in RAW264.7 macrophages in response to LPS. Shock 2008;30:260-6. [DOI] [PubMed] [Google Scholar]
- 21.Calogero S, Grassi F, Aguzzi A, et al. The lack of chromosomal protein Hmg1 does not disrupt cell growth but causes lethal hypoglycaemia in newborn mice. Nat Genet 1999;22:276-80. 10.1038/10338 [DOI] [PubMed] [Google Scholar]
- 22.Grosschedl R, Giese K, Pagel J. HMG domain proteins: architectural elements in the assembly of nucleoprotein structures. Trends Genet 1994;10:94-100. 10.1016/0168-9525(94)90232-1 [DOI] [PubMed] [Google Scholar]
- 23.Ito N, DeMarco RA, Mailliard RB, et al. Cytolytic cells induce HMGB1 release from melanoma cell lines. J Leukoc Biol 2007;81:75-83. 10.1189/jlb.0306169 [DOI] [PubMed] [Google Scholar]
- 24.Huang B, Zhao J, Li H, et al. Toll-like receptors on tumor cells facilitate evasion of immune surveillance. Cancer Res 2005;65:5009-14. 10.1158/0008-5472.CAN-05-0784 [DOI] [PubMed] [Google Scholar]
- 25.Flohr AM, Rogalla P, Meiboom M, et al. Variation of HMGB1 expression in breast cancer. Anticancer Res 2001;21:3881-5. [PubMed] [Google Scholar]
- 26.Apetoh L, Ghiringhelli F, Tesniere A, et al. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med 2007;13:1050-9. 10.1038/nm1622 [DOI] [PubMed] [Google Scholar]
- 27.Curtin JF, Liu N, Candolfi M, et al. HMGB1 mediates endogenous TLR2 activation and brain tumor regression. PLoS Med 2009;6:e10. 10.1371/journal.pmed.1000010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guerriero JL, Ditsworth D, Catanzaro JM, et al. DNA alkylating therapy induces tumor regression through an HMGB1-mediated activation of innate immunity. J Immunol 2011;186:3517-26. 10.4049/jimmunol.1003267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ellerman JE, Brown CK, de Vera M, et al. Masquerader: high mobility group box-1 and cancer. Clin Cancer Res 2007;13:2836-48. 10.1158/1078-0432.CCR-06-1953 [DOI] [PubMed] [Google Scholar]
- 30.Campana L, Bosurgi L, Rovere-Querini P. HMGB1: a two-headed signal regulating tumor progression and immunity. Curr Opin Immunol 2008;20:518-23. 10.1016/j.coi.2008.04.012 [DOI] [PubMed] [Google Scholar]
- 31.Srikrishna G, Freeze HH. Endogenous damage-associated molecular pattern molecules at the crossroads of inflammation and cancer. Neoplasia 2009;11:615-28. 10.1593/neo.09284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKinney K, Prives C. Efficient specific DNA binding by p53 requires both its central and C-terminal domains as revealed by studies with high-mobility group 1 protein. Mol Cell Biol 2002;22:6797-808. 10.1128/MCB.22.19.6797-6808.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiao Y, Wang HC, Fan SJ. Growth suppression and radiosensitivity increase by HMGB1 in breast cancer. Acta Pharmacol Sin 2007;28:1957-67. 10.1111/j.1745-7254.2007.00669.x [DOI] [PubMed] [Google Scholar]
- 34.Giavara S, Kosmidou E, Hande MP, et al. Yeast Nhp6A/B and mammalian Hmgb1 facilitate the maintenance of genome stability. Curr Biol 2005;15:68-72. 10.1016/j.cub.2004.12.065 [DOI] [PubMed] [Google Scholar]
- 35.Celona B, Weiner A, Di Felice F, et al. Substantial histone reduction modulates genomewide nucleosomal occupancy and global transcriptional output. PLoS Biol 2011;9:e1001086. 10.1371/journal.pbio.1001086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mantovani A. Cancer: Inflaming metastasis. Nature 2009;457:36-7. 10.1038/457036b [DOI] [PubMed] [Google Scholar]
- 37.Mantovani A, Allavena P, Sica A, et al. Cancer-related inflammation. Nature 2008;454:436-44. 10.1038/nature07205 [DOI] [PubMed] [Google Scholar]
- 38.Vakkila J, Lotze MT. Inflammation and necrosis promote tumour growth. Nat Rev Immunol 2004;4:641-8. 10.1038/nri1415 [DOI] [PubMed] [Google Scholar]
- 39.Yu Y, Xie M, He YL, et al. Role of high mobility group box 1 in adriamycin-induced apoptosis in leukemia K562 cells. Ai Zheng 2008;27:929-33. [PubMed] [Google Scholar]
- 40.Xie M, Kang R, Yu Y, et al. Enhancive effect of HMGB1 gene silence on adriamycin-induced apoptosis in K562/A02 drug resistance leukemia cells. Zhonghua Xue Ye Xue Za Zhi 2008;29:549-52. [PubMed] [Google Scholar]
- 41.He Q, Liang CH, Lippard SJ. Steroid hormones induce HMG1 overexpression and sensitize breast cancer cells to cisplatin and carboplatin. Proc Natl Acad Sci U S A 2000;97:5768-72. 10.1073/pnas.100108697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barnes KR, Kutikov A, Lippard SJ. Synthesis, characterization, and cytotoxicity of a series of estrogen-tethered platinum(IV) complexes. Chem Biol 2004;11:557-64. 10.1016/j.chembiol.2004.03.024 [DOI] [PubMed] [Google Scholar]
- 43.van Beijnum JR, Buurman WA, Griffioen AW. Convergence and amplification of toll-like receptor (TLR) and receptor for advanced glycation end products (RAGE) signaling pathways via high mobility group B1 (HMGB1). Angiogenesis 2008;11:91-9. 10.1007/s10456-008-9093-5 [DOI] [PubMed] [Google Scholar]
- 44.van Beijnum JR, Dings RP, van der Linden E, et al. Gene expression of tumor angiogenesis dissected: specific targeting of colon cancer angiogenic vasculature. Blood 2006;108:2339-48. 10.1182/blood-2006-02-004291 [DOI] [PubMed] [Google Scholar]
- 45.Pallier C, Scaffidi P, Chopineau-Proust S, et al. Association of chromatin proteins high mobility group box (HMGB) 1 and HMGB2 with mitotic chromosomes. Mol Biol Cell 2003;14:3414-26. 10.1091/mbc.E02-09-0581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huttunen HJ, Fages C, Kuja-Panula J, et al. Receptor for advanced glycation end products-binding COOH-terminal motif of amphoterin inhibits invasive migration and metastasis. Cancer Res 2002;62:4805-11. [PubMed] [Google Scholar]
- 47.van Beijnum JR, Nowak-Sliwinska P, van den Boezem E, et al. Tumor angiogenesis is enforced by autocrine regulation of high-mobility group box 1. Oncogene 2013;32:363-74. 10.1038/onc.2012.49 [DOI] [PubMed] [Google Scholar]
- 48.Sasahira T, Kirita T, Bhawal UK, et al. The expression of receptor for advanced glycation end products is associated with angiogenesis in human oral squamous cell carcinoma. Virchows Arch 2007;450:287-95. 10.1007/s00428-006-0359-2 [DOI] [PubMed] [Google Scholar]
- 49.Taguchi A, Blood DC, del Toro G, et al. Blockade of RAGE-amphoterin signalling suppresses tumour growth and metastases. Nature 2000;405:354-60. 10.1038/35012626 [DOI] [PubMed] [Google Scholar]
- 50.Yoon S, Lee JY, Yoon BK, et al. Effects of HMGB-1 overexpression on cell-cycle progression in MCF-7 cells. J Korean Med Sci 2004;19:321-6. 10.3346/jkms.2004.19.3.321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brickman JM, Adam M, Ptashne M. Interactions between an HMG-1 protein and members of the Rel family. Proc Natl Acad Sci U S A 1999;96:10679-83. 10.1073/pnas.96.19.10679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang CC, Krieg S, Shapiro DJ. HMG-1 stimulates estrogen response element binding by estrogen receptor from stably transfected HeLa cells. Mol Endocrinol 1999;13:632-43. 10.1210/mend.13.4.0264 [DOI] [PubMed] [Google Scholar]
- 53.Verrier CS, Roodi N, Yee CJ, et al. High-mobility group (HMG) protein HMG-1 and TATA-binding protein-associated factor TAF(II)30 affect estrogen receptor-mediated transcriptional activation. Mol Endocrinol 1997;11:1009-19. 10.1210/mend.11.8.9962 [DOI] [PubMed] [Google Scholar]
- 54.Das D, Peterson RC, Scovell WM. High mobility group B proteins facilitate strong estrogen receptor binding to classical and half-site estrogen response elements and relax binding selectivity. Mol Endocrinol 2004;18:2616-32. 10.1210/me.2004-0125 [DOI] [PubMed] [Google Scholar]
- 55.Boon T, Coulie PG, Van den Eynde BJ, et al. Human T cell responses against melanoma. Annu Rev Immunol 2006;24:175-208. 10.1146/annurev.immunol.24.021605.090733 [DOI] [PubMed] [Google Scholar]
- 56.Rovere-Querini P, Capobianco A, Scaffidi P, et al. HMGB1 is an endogenous immune adjuvant released by necrotic cells. EMBO Rep 2004;5:825-30. 10.1038/sj.embor.7400205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dong Xda E, Ito N, Lotze MT, et al. High mobility group box I (HMGB1) release from tumor cells after treatment: implications for development of targeted chemoimmunotherapy. J Immunother 2007;30:596-606. 10.1097/CJI.0b013e31804efc76 [DOI] [PubMed] [Google Scholar]
- 58.Formenti SC, Demaria S. Effects of chemoradiation on tumor-host interactions: the immunologic side. J Clin Oncol 2008;26:1562-3; author reply 1563. 10.1200/JCO.2007.15.5499 [DOI] [PubMed] [Google Scholar]
- 59.Wild CA, Bergmann C, Fritz G, et al. HMGB1 conveys immunosuppressive characteristics on regulatory and conventional T cells. Int Immunol 2012;24:485-94. 10.1093/intimm/dxs051 [DOI] [PubMed] [Google Scholar]
- 60.Liu Z, Falo LD, Jr, You Z. Knockdown of HMGB1 in tumor cells attenuates their ability to induce regulatory T cells and uncovers naturally acquired CD8 T cell-dependent antitumor immunity. J Immunol 2011;187:118-25. 10.4049/jimmunol.1003378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Apetoh L, Ghiringhelli F, Tesniere A, et al. The interaction between HMGB1 and TLR4 dictates the outcome of anticancer chemotherapy and radiotherapy. Immunol Rev 2007;220:47-59. 10.1111/j.1600-065X.2007.00573.x [DOI] [PubMed] [Google Scholar]
- 62.Ke S, Zhou F, Yang H, et al. Downregulation of high mobility group box 1 modulates telomere homeostasis and increases the radiosensitivity of human breast cancer cells. Int J Oncol 2015;46:1051-8. [DOI] [PubMed] [Google Scholar]
- 63.Ricci MS, Zong WX. Chemotherapeutic approaches for targeting cell death pathways. Oncologist 2006;11:342-57. 10.1634/theoncologist.11-4-342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ladoire S, Penault-Llorca F, Senovilla L, et al. Combined evaluation of LC3B puncta and HMGB1 expression predicts residual risk of relapse after adjuvant chemotherapy in breast cancer. Autophagy 2015;11:1878-90. 10.1080/15548627.2015.1082022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Castells M, Thibault B, Delord JP, et al. Implication of tumor microenvironment in chemoresistance: tumor-associated stromal cells protect tumor cells from cell death. Int J Mol Sci 2012;13:9545-71. 10.3390/ijms13089545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tiago M, de Oliveira EM, Brohem CA, et al. Fibroblasts protect melanoma cells from the cytotoxic effects of doxorubicin. Tissue Eng Part A 2014;20:2412-21. 10.1089/ten.tea.2013.0473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Amornsupak K, Insawang T, Thuwajit P, et al. Cancer-associated fibroblasts induce high mobility group box 1 and contribute to resistance to doxorubicin in breast cancer cells. BMC Cancer 2014;14:955. 10.1186/1471-2407-14-955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stoetzer OJ, Fersching DM, Salat C, et al. Circulating immunogenic cell death biomarkers HMGB1 and RAGE in breast cancer patients during neoadjuvant chemotherapy. Tumour Biol 2013;34:81-90. 10.1007/s13277-012-0513-1 [DOI] [PubMed] [Google Scholar]
- 69.Arnold T, Michlmayr A, Baumann S, et al. Plasma HMGB-1 after the initial dose of epirubicin/docetaxel in cancer. Eur J Clin Invest 2013;43:286-91. 10.1111/eci.12043 [DOI] [PubMed] [Google Scholar]
- 70.Apetoh L, Tesniere A, Ghiringhelli F, et al. Molecular interactions between dying tumor cells and the innate immune system determine the efficacy of conventional anticancer therapies. Cancer Res 2008;68:4026-30. 10.1158/0008-5472.CAN-08-0427 [DOI] [PubMed] [Google Scholar]
- 71.Zitvogel L, Apetoh L, Ghiringhelli F, et al. Immunological aspects of cancer chemotherapy. Nat Rev Immunol 2008;8:59-73. 10.1038/nri2216 [DOI] [PubMed] [Google Scholar]
- 72.Fernö M, Borg A, Johansson U, et al. Estrogen and progesterone receptor analyses in more than 4,000 human breast cancer samples. A study with special reference to age at diagnosis and stability of analyses. Southern Swedish Breast Cancer Study Group. Acta Oncol 1990;29:129-35. [DOI] [PubMed] [Google Scholar]
- 73.Wang R, He W, Li Z, et al. Caveolin-1 functions as a key regulator of 17β-estradiol-mediated autophagy and apoptosis in BT474 breast cancer cells. Int J Mol Med 2014;34:822-7. [DOI] [PubMed] [Google Scholar]
- 74.Von Hoff DD, Schilsky R, Reichert CM, et al. Toxic effects of cis-dichlorodiammineplatinum(II) in man. Cancer Treat Rep 1979;63:1527-31. [PubMed] [Google Scholar]
- 75.Oñate SA, Prendergast P, Wagner JP, et al. The DNA-bending protein HMG-1 enhances progesterone receptor binding to its target DNA sequences. Mol Cell Biol 1994;14:3376-91. 10.1128/MCB.14.5.3376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lum HK, Lee KL. The human HMGB1 promoter is modulated by a silencer and an enhancer-containing intron. Biochim Biophys Acta 2001;1520:79-84. 10.1016/S0167-4781(01)00243-3 [DOI] [PubMed] [Google Scholar]
- 77.Huang JC, Zamble DB, Reardon JT, et al. HMG-domain proteins specifically inhibit the repair of the major DNA adduct of the anticancer drug cisplatin by human excision nuclease. Proc Natl Acad Sci U S A 1994;91:10394-8. 10.1073/pnas.91.22.10394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Burstein HJ. The distinctive nature of HER2-positive breast cancers. N Engl J Med 2005;353:1652-4. 10.1056/NEJMp058197 [DOI] [PubMed] [Google Scholar]
- 79.Tan M, Yu D. Molecular Mechanisms of ErbB2-Mediated Breast Cancer Chemoresistance. In: Yu D, Hung MC, editors. Breast Cancer Chemosensitivity. New York: Springer, 2007:119-29. [DOI] [PubMed] [Google Scholar]
- 80.Lee HJ, Kim JY, Song IH, et al. High mobility group B1 and N1 (HMGB1 and HMGN1) are associated with tumor-infiltrating lymphocytes in HER2-positive breast cancers. Virchows Arch 2015;467:701-9. 10.1007/s00428-015-1861-1 [DOI] [PubMed] [Google Scholar]
- 81.Dhumale SS, Waghela BN, Pathak C. Quercetin protects necrotic insult and promotes apoptosis by attenuating the expression of RAGE and its ligand HMGB1 in human breast adenocarcinoma cells. IUBMB Life 2015;67:361-73. 10.1002/iub.1379 [DOI] [PubMed] [Google Scholar]
- 82.Buoncervello M, Borghi P, Romagnoli G, et al. Apicidin and docetaxel combination treatment drives CTCFL expression and HMGB1 release acting as potential antitumor immune response inducers in metastatic breast cancer cells. Neoplasia 2012;14:855-67. 10.1593/neo.121020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chang BP, Wang DS, Xing JW, et al. miR-200c inhibits metastasis of breast cancer cells by targeting HMGB1. J Huazhong Univ Sci Technolog Med Sci 2014;34:201-6. 10.1007/s11596-014-1259-3 [DOI] [PubMed] [Google Scholar]
- 84.Chaachouay H, Ohneseit P, Toulany M, et al. Autophagy contributes to resistance of tumor cells to ionizing radiation. Radiother Oncol 2011;99:287-92. 10.1016/j.radonc.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 85.Luo J, Chen J, He L. mir-129-5p Attenuates Irradiation-Induced Autophagy and Decreases Radioresistance of Breast Cancer Cells by Targeting HMGB1. Med Sci Monit 2015;21:4122-9. 10.12659/MSM.896661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wicha MS, Liu S, Dontu G. Cancer stem cells: an old idea--a paradigm shift. Cancer Res 2006;66:1883-90; discussion 1895-6. [DOI] [PubMed]
- 87.Frank NY, Schatton T, Frank MH. The therapeutic promise of the cancer stem cell concept. J Clin Invest 2010;120:41-50. 10.1172/JCI41004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Conti L, Lanzardo S, Arigoni M, et al. The noninflammatory role of high mobility group box 1/Toll-like receptor 2 axis in the self-renewal of mammary cancer stem cells. FASEB J 2013;27:4731-44. 10.1096/fj.13-230201 [DOI] [PubMed] [Google Scholar]
- 89.Kostova N, Zlateva S, Ugrinova I, et al. The expression of HMGB1 protein and its receptor RAGE in human malignant tumors. Mol Cell Biochem 2010;337:251-8. 10.1007/s11010-009-0305-0 [DOI] [PubMed] [Google Scholar]
- 90.Yan HX, Cheng P, Wei HY, et al. Active immunotherapy for mouse breast cancer with irradiated whole-cellvaccine expressing VEGFR2. Oncol Rep 2013;29:1510-6. [DOI] [PubMed] [Google Scholar]