Abstract

Community-led total sanitation (CLTS) is a participatory approach to addressing open defecation that has demonstrated success in previous studies, yet there is no research on how implementation arrangements and context change effectiveness. We used a quasi-experimental study design to compare two interventions in Ethiopia: conventional CLTS in which health workers and local leaders provided facilitation and an alternative approach in which teachers provided facilitation. In 2012, Plan International Ethiopia trained teachers from 111 villages and health workers and leaders from 54 villages in CLTS facilitation. The trained facilitators then implemented CLTS in their respective villages for a year. Latrine ownership, use, and quality were measured with household surveys. Differences between interventions were explored using surveys and interviews. The decrease in open defecation associated with teacher-facilitated CLTS was 8.2 percentage points smaller than for conventional CLTS (p = 0.048). Teachers had competing responsibilities and initially lacked support from local leaders, which may have lessened their success. Teachers may be more appropriate for a supporting rather than leading role in sanitation promotion because they did demonstrate ability and engagement. Open defecation decreased by 15.3 percentage points overall but did not change where baseline open defecation was below 30%. Ownership of a latrine with stable flooring increased by 8.7 percentage points overall. Improved latrine ownership did not change during the intervention. CLTS is most appropriate where open defecation is high because there were no significant changes in sanitation practices or latrine upgrades where baseline open defecation was low.
Introduction
Although sanitation has improved dramatically in the past decade, globally 2.4 billion people lack access to improved sanitation. An estimated 946 million lack access to any sanitation facility and practice open defecation,1 although the actual number is probably much higher.2,3 Fecal contamination of the environment from poor sanitation together with poor handwashing are responsible for an estimated 577 000 deaths annually.4 Additionally, there is growing evidence that, through environmental enteropathy, open defecation contributes to more malnutrition than previously thought5,6 and could be responsible for approximately half of child stunting.7−9 There are also rationales for sanitation beyond health. Many households construct latrines for improved social status and dignity;10,11 there are also potential gender-equity benefits,12 the benefit of increased school attendance for girls,13 and economic benefits including time savings and increased productivity.14
Community-led total sanitation (CLTS) emerged in the year 2000 as a participatory approach to address open defecation. CLTS aims to generate emotional reactions to open defecation during a community meeting such as shame and disgust and to elicit collective action on sanitation. The CLTS Handbook provides a thorough explanation of the approach.15 CLTS is now a well-established approach that has been implemented in over 50 countries.16 Many, such as Ethiopia, include it in national policy.17 Much of CLTS literature is “gray” or unpublished. The Water Institute at the University of North Carolina at Chapel Hill (UNC) and Plan International (Plan) conducted a systematic review of journal-published and gray literature. The review found few published studies on CLTS or related approaches, which tended to focus on impacts.18 The gray literature was more extensive and focused on project settings and processes rather than impacts. Gray literature included a preponderance of low-quality study designs and data-collection methods.
A randomized controlled trial of CLTS in Mali reported a 23 percentage point reduction in open defecation among adults, and a 30 percentage point increase in latrine ownership.19 It also reported beneficial health impacts in the form of increased height-for-age and decreased stunting among children despite there being no impact on diarrheal incidence. A case study in Zimbabwe reported that latrine ownership and use was higher where CLTS had been implemented than in other villages.20 A total of five evaluations of India’s Total Sanitation Campaign (TSC), which includes some CLTS features with the addition of hardware subsidies, have shown positive impacts on latrine access,21−25 although only two demonstrated health impacts.22,25 Water-, sanitation-, and hygiene- (WaSH) related health outcomes are difficult to measure and to attribute to WaSH interventions, and a failure to demonstrate health impact does not necessarily indicate the absence of health benefits.26
Our study is designed as operational research and has the aim of generating findings with immediate implications for policy and practice. To address a gap in the evidence, we investigated how context and process (or implementation arrangements) influence CLTS effectiveness. We applied collaborative design by an implementation organization (Plan) and a research institute (UNC),27 focused on an existing public health program,28 compared different institutional arrangements for public service delivery,29 and here report on context and the intervention process in addition to outcomes.30
Health extension workers (HEWs) are tasked with facilitating CLTS in Ethiopia, where there have been dramatic reductions in open defecation since CLTS was introduced.17,31 A kebele is the lowest administrative unit in Ethiopia and is composed of 20–30 villages and approximately 5000 people. Every kebele in Ethiopia has one health post staffed by one to three HEWs who typically are from that geographic area, speak the local language, and share cultural background with residents. HEWs are responsible for 15 separate tasks in addition to CLTS.32 Plan has explored training teachers as CLTS facilitators to alleviate the burden on HEWs and enable increased follow-up activities with some signs of success.33
Teachers have demonstrated aptitude for promoting healthy WaSH behaviors previously for household water treatment and handwashing in Kenya,34 for student handwashing in China,35 and for schistosomiasis prevention in Tanzania.36,37 However, to date, there are no studies published on teachers leading sanitation promotion at the community level. We compared two interventions in different regions of Ethiopia: conventional CLTS, in which health workers and local leaders provided facilitation, and an alternative intervention, in which teachers provided facilitation.
Materials and Methods
Program Description
CLTS implementation in Ethiopia consists of the standard three stages from the CLTS Handbook:15 pretriggering, triggering, and follow-up. Pretriggering includes community entry and acceptance by leaders. Triggering consists of a community meeting in which outside facilitators use tools (such as sanitation mapping) designed to “trigger” an emotional response and a collective desire to improve the situation. Typically, each individual village within a kebele is triggered separately. All of the villages are under the authority of the kebele leaders, who must approve any development activities within villages and often coordinate them. In the follow-up, facilitators visit villages to monitor progress and guide them in eliminating open defecation. In Ethiopia, the follow-up includes emphasis on handwashing with soap or ash at key times.38 When ready, a kebele can request certification of open-defecation-free (ODF) status by the government.39
This study compares CLTS as facilitated by two different groups of local actors. The first group of actors (“conventional CLTS”) is composed of HEWs who lead facilitation and kebele leaders who support them. The second (“teacher-facilitated CLTS”) is composed of teachers facilitating CLTS. In October 2012, Plan initiated the interventions by training the two groups of facilitators, who then facilitated CLTS for the following year. The same CLTS tools and activities were used by both groups of facilitators; the only difference was in who facilitated. Plan provided monthly guidance to both groups of facilitators and occasionally observed their facilitation in communities.
In the two kebeles that received conventional CLTS, Plan trained one to three HEWs and eight leaders per kebele (Table 1). In the four teacher-facilitated CLTS kebeles, Plan trained 10 to 28 teachers and two leaders per kebele. HEWs and teachers led CLTS facilitation. Kebele leaders were trained as they must approve development activities within their kebeles. All trained HEWs and teachers attended each village triggering within their kebele. A timeline of implementation activities for both interventions is in the Supporting Information, and the teacher training manual and report on detailed implementation activities written by Plan are available online.40,41
Table 1. Implementation Details: Facilitators Trained and Leadership Attendance at Triggerings.
| kebele
leaders |
|||||||
|---|---|---|---|---|---|---|---|
| intervention | kebele | villages | teachers trained | HEWs trained | days per month on CLTSb | trained | at triggeringsc |
| conventional | kebele 1 | 24 | 0 | 1 | 0.00 | 8 | 1.6 |
| kebele 2 | 30 | 0 | 3 | 4.67 | 8 | 1.5 | |
| teacher-facilitated | kebele 3 | 32 | 12 | 0 | 2.44 | 2 | 0.3 |
| kebele 4 | 22 | 18 | 0 | 1.92 | 2 | 0.0 | |
| kebele 5 | 31 | 10 | 0 | 1.30 | 2 | 0.3 | |
| kebele 6 | 26 | 28 | 0 | 3.16 | 2 | 0.3 | |
The HEW trained from kebele 1 in Oromia left their job in May 2013 (7 months into implementation); a replacement HEW had not been hired by the follow-up survey. The eight kebele leaders from kebele 1 continued facilitating CLTS for the duration of the intervention.
Teachers and HEWs were surveyed at follow-up on their activity level during the CLTS interventions.
Kebele leaders’ attendance was recorded by Plan. Kebele leaders were not surveyed; their activity level outside of triggerings is not known.
The implementation in this project was enabled by existing enabling factors. Plan had prior experience implementing CLTS, training facilitators, and collaborating with the government on sanitation and hygiene. The Government of Ethiopia had included CLTS in national policy and had institutional support mechanisms in place, such as a Memorandum of Understanding between three ministries for coordination on water, sanitation, and hygiene.42 The catchment areas for schools and health posts are the same in Ethiopia, the kebele, which enables teachers to facilitate CLTS. Teachers are known by community members (the intended beneficiaries of CLTS) and speak the local language. Development activities are typically coordinated at the kebele level, and teachers are familiar with all of the villages within their kebele.
Study Design
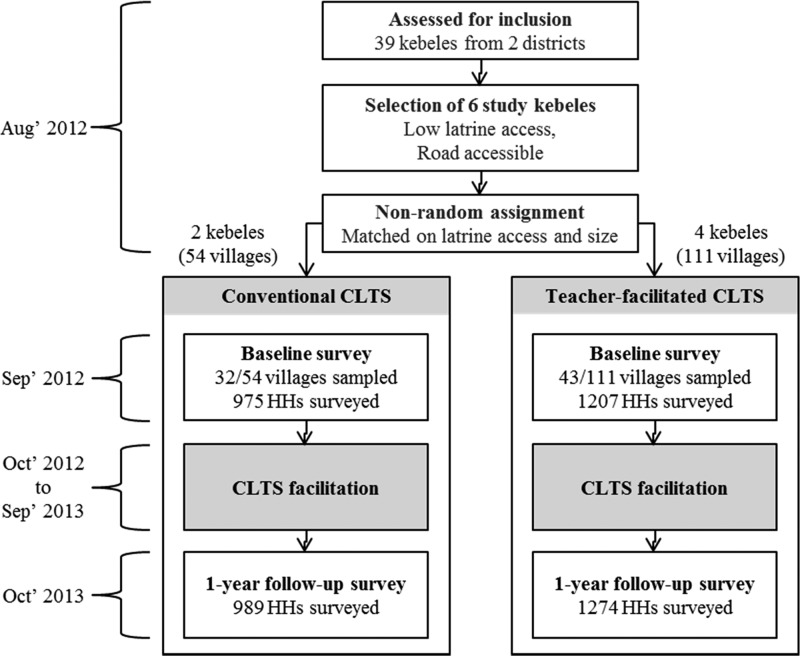
This is a mixed-methods study that uses quantitative data from a quasi-experimental design and qualitative data from interviews. We selected six kebeles from two regions, prematched them within each region on latrine access and kebele size (number of households) using 2011 census data collected from district government, and then manually assigned them to receive conventional or teacher-facilitated CLTS (Figure 1). We chose prematching because with six study sites, it was more likely than random assignment to result in similar comparison groups. Prematching is established as a valuable tool for evaluating community-demand-driven sanitation policies.43,44 We used a difference-in-difference estimator to test for a difference in the effectiveness of the two interventions in changing sanitation practices because it removes baseline differences in the outcome and accounts for time-invariant differences between comparison groups.23,43 We used a multivariable regression, incorporating robust covariate indicators, to further account for baseline differences between comparison groups. Because this study was designed to compare two interventions, no do-nothing control group was included.
Figure 1.
Timeline and sequence of the quasi-experimental study design and execution.
While we used prematching, a difference-in-difference estimator, and a multivariable regression to address any baseline differences between comparison groups; outcomes cannot be attributed solely to the different interventions because this study involves nonrandom assignment. Interviews with NGO employees, facilitators, and government and supplemental data collected from household surveys were used to understand the implementation process and to explore possible explanations for the differences in outcomes between interventions.
Sampling
A pair of regions where Plan had prior CLTS experience and government collaboration were selected: Oromia and the Southern Nations, Nationalities, and Peoples’ (SNNP) regions. One district with no prior CLTS was selected from each region (Deksis and Dara districts, respectively). A total of three road-accessible kebeles with no major towns and low reported latrine access in the 2011 census were selected from each district.
The sample size (number of households) was set to detect a difference between a 30 and 40 percentage point (pp) reduction in open defecation (i.e., a 10 pp difference-in-difference, β = 0.8, α = 0.05). We used a conservative intracluster correlation (ICC) of 0.2.23,45 On the basis of the average village size, we randomly sampled 75 villages. All 2444 households within sampled villages were approached for surveying. At the baseline, 2182 households were surveyed. At the follow-up, 2263 households were surveyed (Figure 1; sampling details in the Supporting Information).
Data Collection
Household surveys, latrine and handwashing station observations, and health extension worker and teacher surveys were completed at the baseline (September 2012) and the follow-up (October 2013). Household surveys covered demographics, sanitation, hygiene, interactions, and recall of CLTS events. Indicators were selected from review of prior WaSH research15,23,46,47 and input from UNC and Plan. Sanitation outcomes were assessed by asking heads-of-households where they primarily defecated and their handwashing practices. Those reporting using a latrine were asked a series of questions to determine if it was private, shared, or communal. Latrine and handwashing station quality and maintenance were assessed by observation. HEW and teacher surveys covered CLTS-related knowledge, attitudes, and practices. All surveying was completed by an independent contractor with extensive experience in Ethiopia, one team lead per region, and experienced local surveyors. Household surveys were translated into the local languages (Oromo and Sidama); HEW and teacher surveys were translated into Amharic by the contractor and translations checked by an independent WaSH specialist and rechecked by Plan. Printed survey tools were pretested during training, piloted in nonproject kebeles, and revised in consultation with UNC. The follow-up survey tool is available in the Supporting Information. Survey team leaders reviewed surveys each evening, and Plan staff were available to help locate missed households. Surveyors were audited by Plan resurveying one randomly selected village per kebele (23–40 households per audited village) with 11 questions from the full survey.
The CLTS process was monitored with checklists filled out by the Plan coauthors and interviews with Plan staff (including coauthors) and district government. Interviews with Plan staff used open-ended questions on the relative successes and challenges of the two interventions and two regions included in the study and lasted 1–2 h. Interviews occurred 2, 6, and 12 months into implementation and 3 months after implementation ended. Interviews with district government used semistructured questions on the sanitation-related roles, activities, and experiences of different district government offices and lasted 0.5–1 h. Plan staff and government officers spoke English and were interviewed by the primary author. ODF certification dates were collected from district officials. ODF certification by district government is part of implementation and was not validated by the researchers.39
Analysis
Descriptive statistics from household surveys and observations were used to assess differences between the comparison groups at baseline. The primary outcome was change in levels of open defecation, with the household as the unit of analysis. Secondary outcomes assessed were use of a communal, shared, or private latrine, latrine quality, and access to handwashing materials. Self-reported latrine use was validated by observing latrines. Latrines that surveyors observed to be full, collapsed, or had unstable flooring were categorized as open defecation.
A difference-in-difference (or treatment-time) estimator was used to account for baseline differences in outcome variables. Sanitation practice was modeled using logistic regression as a function of treatment, survey time point (time), and treatment time, and four covariates were included to address baseline differences between comparison groups. The four covariates (roofing material, household size, water collection time, and discussing sanitation or hygiene with a neighbor in the past two months) showed statistically significant differences at baseline and no multicollinearity (the highest variance inflation factor was 1.01) and could logically associate with household sanitation practices (Table 2). To avoid issues with potential endogeneity, we used only baseline values of covariates. Analysis was completed in STATA 12/13/SE. The sampling design including village clustering of outcomes, unequal selection probabilities, and nonresponse rates was accounted for using the “svyset” command.
Table 2. Household and Respondent Characteristics at Baseline by Comparison Group.
| comparison
group |
|||
|---|---|---|---|
| household and respondent characteristics | conventional | teacher-facilitated | p value |
| female respondent | 73.2% | 77.0% | 0.087 |
| years of education of respondents (regardless of gender)b | 2.03 | 1.72 | 0.089 |
| household size (people)b | 6.05 | 5.66 | 0.001 |
| number of children per householdb | 0.94 | 0.94 | 0.981 |
| with diarrhea in past 2 weeksb | 0.18 | 0.19 | 0.787 |
| metal roof | 28.2% | 18.6% | 0.001 |
| own radio | 25.9% | 26.6% | 0.809 |
| own television | 1.2% | 0.7% | 0.367 |
| dirty household compound | 33.0% | 29.7% | 0.238 |
| use improved water supplyc | 51.3% | 51.0% | 0.966 |
| water collection time (minutes)b | 50.4 | 40.06 | <0.001 |
| attended village meeting in past 2 monthsb | 51.7% | 38.1% | <0.001 |
| visited health post in past 2 monthsb | 32.6% | 36.8% | 0.117 |
| discussed sanitation or hygiene with a neighbor in past 2 monthsb | 51.2% | 35.8% | <0.001 |
| open defecationb | 37.7% | 47.9% | <0.001 |
| own a latrine | 84.0% | 76.2% | 0.001 |
| with accessible handwashing materials | 19.0% | 11.4% | 0.007 |
| owns an improved latrinec | 22.7% | 20.2% | 0.120 |
| primarily uses a shared latrineb | 6.3% | 5.4% | 0.477 |
| primarily uses a communal/public latrineb | 1.9% | 2.6% | 0.423 |
| want to own a latrineb | 14.8% | 23.4% | <0.001 |
| plan to build a latrine in next yearb | 14.2% | 22.5% | <0.001 |
Respondents were heads-of-households, and females were preferred if available. A t test was used to check for significant differences. All values account for unequal selection probability, nonresponse rates, and village clustering.
Self-reported by respondent. Remaining variables are surveyor observed.
Interviews with government and Plan staff were either transcribed in real-time or audio-recorded and then transcribed. Transcripts were analyzed by the primary author for statements regarding kebele leaders, HEWs, teachers, their interactions, and challenges they faced in facilitating CLTS.
This study was reviewed and approved by the UNC Office of Human Research Ethics (study no. #12-1851). Study approval was obtained from zonal and district health offices within Ethiopia. Informed consent was received from all respondents.
Results
Baseline Statistics
For most variables, the baseline differences between the comparison groups were insignificant (Table 2). In conventional CLTS kebeles, average household size was larger, water collection time longer, and metal roofing more common, as was participation in village meetings and discussions regarding sanitation and hygiene with neighbors. Household ownership of a latrine and handwashing station was also higher in conventional CLTS kebeles, and fewer practiced open defecation. Prematching did not fully eliminate baseline sanitation differences, likely because it was based on government census data from 2011, which occurred one year before our baseline household surveys and likely used the improved latrine definition, which does appear to be well-balanced in our baseline.
Sanitation Outcomes
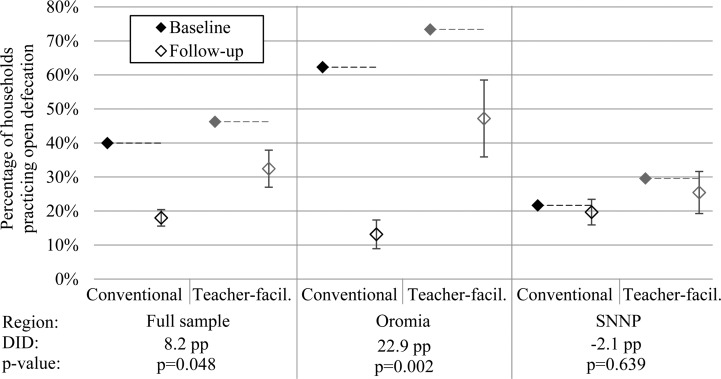
From baseline to follow-up, the proportion of households practicing open defecation decreased in both the teacher-facilitated and conventional CLTS groups (Figure 2). Conventional CLTS was associated with an 8.2 percentage point greater decrease in open defecation than was teacher-facilitated CLTS in the full sample (p = 0.048). The difference-in-difference in open defecation was associated with minimal change in use of communal or shared latrines, and a 9.0 percentage point greater increase in use of private latrines was associated with conventional CLTS (details and figure in the Supporting Information). Outcomes varied dramatically between regions (Figure 2 and Table 4). In Oromia, conventional CLTS was associated with a 22.9 percentage point greater decrease in open defecation than was teacher-facilitated CLTS (p = 0.002). In the SNNP region, there were no significant changes in open defecation associated with either intervention.
Figure 2.
Open defecation before and after conventional and teacher-facilitated CLTS interventions in Ethiopia. Conventional includes two kebeles (54 villages). Teacher-facilitated includes four kebeles (111 villages). Kebeles are split evenly between the Oromia and SNNP regions. Horizontal lines are baseline means. Bars are 95% confidence intervals. The confidence interval is largest for teacher-facilitated CLTS in Oromia because standard error for binary variables is largest at 50%. Open defecation is modeled from logistic regression parameters with covariates set to their means (full regressions in the Supporting Information). Open defecation results are based on survey responses and latrine observations. All analysis accounts for unequal selection probabilities, nonresponse rates, and village clustering. ICC = 0.278 for open defecation at the village level. “DID” = difference-in-difference.
Table 4. Baseline and Follow-Up Open Defecation Levels and ODF Certification Dates by Kebelea.
| region | kebele | baseline (Sept 2012) | follow-up (Oct 2013) | change | ODF certification dateb |
|---|---|---|---|---|---|
| Oromia | kebele 1 (conventional) | 62.0% | 13.6% | –48.4% | May 31, 2013 |
| kebele 3 (teacher-facilitated) | 77.1% | 56.6% | –20.5% | June 5, 2014 | |
| kebele 4 (teacher-facilitated) | 66.9% | 32.0% | –34.9% | June 5, 2014 | |
| SNNP | kebele 2 (conventional) | 21.4% | 19.6% | –1.7% | April 19, 2013 |
| kebele 5 (teacher-facilitated) | 29.9% | 26.6% | –3.3% | June 17, 2013 | |
| kebele 6 (teacher-facilitated) | 30.0% | 24.9% | –5.1% | May 30, 2013 |
Proportions account for unequal selection probability and nonresponse rates.
ODF certification was conducted by district governments. The research team did not observe or validate ODF status.
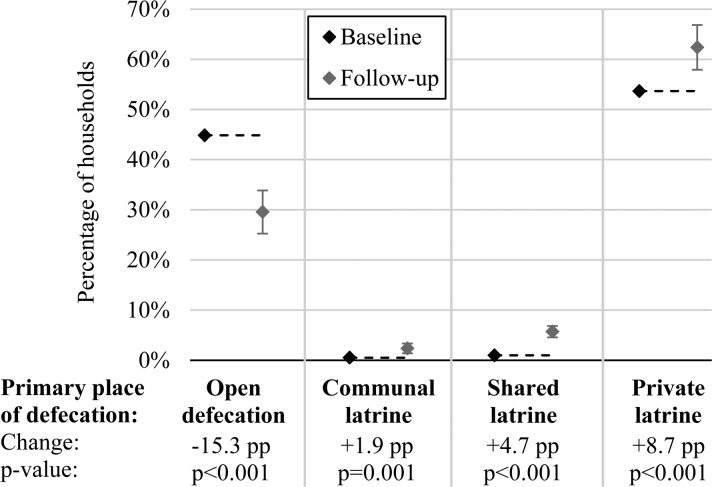
Across both interventions, open defecation decreased by 15.3 percentage point through an increase in use of communal latrines (+ 1.9 pp), shared latrines (+4.7 pp), and private latrines (+8.7 pp) (Figure 3). At baseline, 33.2% of households with a metal roof (an indicator of economic status) were practicing open defecation, and 48% of households without a metal roof were practicing open defection. During the CLTS interventions, 10.6% of households with a metal roof and 8.9% of households without a metal roof adopted use of a private latrine (data in the Supporting Information).
Figure 3.
Sanitation practices before and after CLTS interventions in Ethiopia. Percentages represent six kebeles (165 villages). Kebeles are split evenly between the Oromia and SNNP regions. Horizontal lines are extensions of baseline means. Bars are 95% confidence intervals. Percentages are simple proportions. A t test was used to check for significant differences between baseline and follow-up. Households reporting the use of latrines not shown to surveyors or latrines with unstable flooring were classified as open-defecation. All analysis accounts for unequal selection probability, nonresponse rates, and village clustering.
Across both interventions, household ownership of any observed latrine did not change significantly during the CLTS interventions, nor did ownership of an improved latrine (a pit latrine with stable flooring made of a durable material) (Table 3). However, ownership of latrines with stable, safe flooring and an intact superstructure increased. Ownership of latrines with indicators of cleaning and with available handwashing materials also increased. Changes in latrine characteristics came about through upgrades of existing latrines and through some old latrines collapsing and new latrines being built (data not presented).
Table 3. Household Ownership of a Private Latrine and Latrine Characteristics Before and After CLTS Interventions in Ethiopia.
| latrine
ownership |
|||||
|---|---|---|---|---|---|
| variable | baseline | follow-up | change | p value | |
| infrastructure | any observed latrine | 79% | 77% | –1.1% | 0.476 |
| durable flooring materialb | 21% | 17% | –3.3% | 0.139 | |
| stable and safe flooringc | 54% | 62% | 8.7% | <0.001 | |
| fully intact walls | 4% | 6% | 2.3% | 0.044 | |
| intact door | 5% | 9% | 3.5% | 0.005 | |
| protective roof | 3% | 8% | 4.3% | <0.001 | |
| complete privacy | 4% | 6% | 2.5% | 0.037 | |
| improvedd | 17% | 16% | –1.4% | 0.460 | |
| upkeep | hole covered | 2% | 8% | 6.5% | <0.001 |
| clean (no feces on floor) | 48% | 53% | 5.0% | 0.046 | |
| less than ∼10 flies | 56% | 61% | 5.1% | 0.048 | |
| handwashing station with water or cleansing material | 14% | 18% | 4.5% | 0.044 | |
This analysis covers the 1684 of 1692 privately owned latrines that were observed at baseline and 1779 of 1803 at follow-up. Variables are based on surveyor observations, who had descriptions so that latrine categorization was consistent. Percentages are simple proportions. A t test was used to check for significant differences. Percentages and p values account for unequal selection probability, nonresponse rates, and village clustering. ICC = 0.317 for household ownership of any observed latrine at the village level.
Concrete or wood.
Based on surveyors’ observations and judgment.
A total of four kebeles were certified as ODF by district government during the evaluation (Table 4). The two remaining kebeles in the teacher-facilitated CLTS group were certified ODF in 2014 after the follow-up survey.
Local-Actor and Community-Member Experiences and Participation
In-depth interviews and monitoring of the CLTS process were used to explore possible explanations for the differences in outcomes between interventions. There were some challenges specific to teachers. Kebele leader attendance at teacher-facilitated village triggerings was lower than in conventional CLTS kebeles (Table 1), possibly because kebele leaders do not typically work with teachers, and fewer kebele leaders were trained in these kebeles. A Plan employee noted that “HEWs are seen using the kebele structure more effectively because they spend most of their time in the kebele and have got an already established relationship. Unlike that, teachers seem less effective in using kebele structure, though they are using it...” Individual teachers were less active than HEWs in CLTS (an average of 2.4 versus 4.7 days per month). However, the more numerous teachers collectively spent more time on CLTS than HEWs. According to a Plan employee, “...teachers actually take a shorter time for triggering...” however, “...due to vacations and exams in schools, teachers have some less time to conduct follow ups than HEWs.” Government and Plan interviewees further explained that teachers typically report directly to the district education office and do not have an official relationship with kebele leaders. Additionally, kebele leaders were noted as the most influential: “political leaders can have a higher role (in sanitation) even though it’s not their responsibility.”
Households had differing levels of engagement in CLTS depending on who facilitated. At the follow-up, households in the conventional CLTS kebeles reported higher attendance at triggering meetings and could recall more activities from the triggering, such as the mapping exercise (Table 5). This could be partly due to baseline differences; at baseline, households in the conventional CLTS kebeles reported being more active in village meetings. However, this does not affect the effect estimates presented above, as baseline activity was included as a covariate in outcome regressions.
Table 5. Household Interactions and Activities for Conventional and Teacher-Facilitated CLTS Kebeles at Baseline and Follow-Up.
| comparison
group |
||||
|---|---|---|---|---|
| variable | conventional | teacher-facilitated | p value | |
| baseline | attendedb a village meeting in past 2 months | 52% | 38% | <0.001 |
| attended a meeting in past 2 months: | ||||
| in which sanitation was discussed | 48% | 35% | <0.001 | |
| in which hygiene was discussed | 45% | 33% | <0.001 | |
| follow-upc | attended the CLTS triggering meeting | 45% | 38% | 0.066 |
| remember specific activities or events from triggering | 36% | 27% | 0.032 | |
| average number of activities or events remembered from triggering | 2.3 | 1.9 | 0.012 | |
A t test was used to check for significant differences between comparison groups.
All attendance variables in this table are self-reported by the attendee.
Baseline and follow-up surveys were administered in September 2012 and 2013.
A few challenges were common to all kebeles. All facilitators had competing responsibilities. A Plan employee observed that “...teachers have their own assignments, and they are also expected to do CLTS. The same is true for kebele administration and HEWs.” In January 2013, facilitation stalled for one month in all kebeles while development activities were restricted to a natural resource conservation campaign. According to district officials, households faced challenges in latrine construction: the closest place to buy latrine slabs, cement, or PVC was approximately 2 h of travel from project kebeles.
Discussion
We found that teachers were willing and active facilitators of sanitation promotion at a community level in Ethiopia. There have been no prior assessments of teachers leading sanitation promotion at the community level. Our findings are consistent with previous studies that identified teachers as effective in promoting sanitation and hygiene within schools.34−37 Open defecation decreased by 13.8 percentage points during teacher-facilitated CLTS, but the conventional facilitation approach in Ethiopia was associated with an 8.2 percentage point greater decrease in open defecation (22 pp). The full sample included kebeles in two dissimilar regions to study how effectiveness differed between settings. In Oromia, open defecation decreased by 26.2 percentage points during teacher-facilitated CLTS and 49.1 percentage points during conventional CLTS. In the SNNP region, there were no significant changes in open defecation associated with either intervention. The difference in outcomes is larger between regions than between interventions, indicating that context may be the greater determinant of effectiveness, which is not surprising given the variation in sanitation outcomes between settings in other studies.49−51
The only published impact evaluation of CLTS, from Mali, reports a 23 percentage point reduction in open defecation.19 Evaluations of India’s Total Sanitation Campaign report a 10 to 29 percentage point increased ownership of latrines with signs of use.21,23,24 These four studies were for a 21 to 30 month time frame. We found an overall 15.3 percentage point reduction in open defecation over a 12 month time frame during CLTS in Ethiopia, which is comparable to these figures. The majority of households stopping open defecation switched to private latrine use, which did not appear to be influenced by economic status (as indicated by household roofing material).
Our study reveals the challenges that teachers face in leading the promotion of community-wide sanitation behavior change. Teachers did not engage kebele leaders as quickly as did health workers, who drew on their prior relationship with kebele leaders. Interviews indicated that kebele leaders carried the most authority and influence during the CLTS interventions. Another study reported that health workers were more effective when influential leaders were trained and supported their messages.52 ODF certification dates (Table 3), while not a precise measure of open defecation levels, show that teachers CLTS may have had continuing impact beyond follow-up surveys. Given that trained local actors continued living and working in project kebeles once the project had ended, it is plausible that sanitation activity and behavior change would have continued after the follow-up survey. Plan was able to train teachers as facilitators because the school catchment area aligned with the level of CLTS facilitation: the kebele. We hypothesize that training teachers as facilitators would be less effective in countries where the school catchment area does not align with the level of CLTS facilitation.
We analyzed latrine materials, maintenance, cleanliness, and handwashing material availability alongside sanitation practices, which revealed the importance of careful consideration of target outcomes and data validation. Self-reported and visually confirmed latrine ownership were similar (0.2% difference). However, 24.8% of visually inspected latrines had unstable and unsafe flooring. Self-reported latrine ownership was a good proxy for latrine ownership in this setting; however, both were poor proxies for access to a latrine with stable and safe flooring, and their use in evaluations could lead to inaccurate results and conclusions.
The primary purpose of CLTS is eliminating open defecation. Others have found that this may mean cheap, nondurable latrines are built and handwashing is not fully addressed.20,53 We found the same pattern. Open defecation decreased by 15.3 percentage points through increased latrine sharing and unstable latrines being upgraded or replaced. Ownership of “improved” latrines with more durable flooring materials, the standard used in international monitoring,31,48 did not change significantly. Handwashing materials at latrines increased minimally (4.5 percentage points). Households may have prioritized maintenance and care for facilities over investments in hardware, possibly due to a lack of market availability of construction materials and latrine components.
Decreases in open defecation and increases in stable latrine ownership were highest in the Oromia region, where baseline open defecation was highest. This suggests that CLTS may be most appropriate where there are high levels of open defecation. Further improvements in sanitation and hygiene may require addressing supply and financing issues, which, when addressed together, can increase ownership of hygienic latrines.45
This study has four potential limitations: nonrandom assignment of kebeles, a small number of study sites, effect estimates limited to a comparison of interventions, and a study duration limited to 1 year. Uncertainty regarding internal validity cannot be completely dispelled with nonrandom assignment of the six study kebeles. Comparing multiple regression models suggested that prematching kebeles was successful at minimizing bias. Use of a difference-in-difference estimator and the inclusion of covariates in regressions further decrease the chance of bias in effect estimates. The effect estimates for teacher-facilitated CLTS compared to conventional CLTS are robust, as they vary little across outcomes and regression models. Because no true control group was included, this study compares the effectiveness of two interventions but does not estimate the effectiveness of CLTS. Changes in outcomes that occurred beyond the 1-year follow-up survey are not captured in this paper.
Teachers may be more valuable to WaSH interventions by supporting health workers and local leaders once a project is initiated rather than leading the effort. This could be an attractive option in areas where health workers are overburdened, as is the case in Ethiopia. CLTS was not an appropriate intervention where open defecation was lowest. CLTS was associated with increased ownership of stable, well-maintained latrines and handwashing stations; however, there was no increase in more durable improved latrines. Advancing to more durable and sustainable latrines may require CLTS in combination or series with programs that target supply chains and financing. An operational research methodology enabled an assessment of the implementation process, multiple outcomes, and variation of outcomes by setting.
Acknowledgments
The findings in this article are a result of a subagreement to the University of North Carolina at Chapel Hill from Plan International USA, which was a recipient of a grant from the Bill & Melinda Gates Foundation (OPP1028953). Additional funding from a National Institute of Environmental Health Sciences Training Grant (T32ES007018) supported the primary author’s time. Neither funder had any role in study design, execution, or article preparation. The authors thank the study participants; Plan International USA for grant management; Plan International Ethiopia for implementation, supporting data collection, and interpreting findings; Atnafe Beyene for contributing to study design; the Ethiopian ministries of Health and Education for their support and participation; Dawit Belew Public Health Consulting for administering surveys; Kate Shields for supporting data cleaning and model preparation; and Chris Wiesen at the Odum Institute at UNC for supporting analysis.
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acs.est.6b01021.
Tables S1-S12 and Figures S1-S2. (PDF)
The authors declare the following competing financial interest(s): Abiyot Geremew, Messele Yetie, and Fisseha Atalie are involved in the ongoing implementation of community-led total sanitation and hygiene in Ethiopia.
Supplementary Material
References
- WHO/UNICEF. Progress on Sanitation and Drinking Water: 2015 Update and MDG Assessment; WHO: Geneva, Switzerland, 2015.
- Rukmini S.Survey secrets: how the type of question asked affects survey findings. Hindu., 20151–2.
- Coffey D.; Spears D.. How can a large sample survey monitor open defecation in rural India for the Swatch Bharat Abhiyan?; RICE working paper; 2014. [Google Scholar]
- Prüss-Ustün A.; Bartram J.; Clasen T. F.; Colford J. M.; Cumming O.; Curtis V. A.; Bonjour S.; Dangour A. D.; De France J.; Fewtrell L.; et al. Burden of disease from inadequate water, sanitation and hygiene in low- and middle-income settings: a retrospective analysis of data from 145 countries. Trop. Med. Int. Health 2014, 19 (8), 894–905. 10.1111/tmi.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dangour A. D.; Watson L.; Cumming O.; Boisson S.; Che Y.; Velleman Y.; Cavill S.; Allen E.; Uauy R. Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children (review). Cochrane Libr. 2013, 8, 99. 10.1002/14651858.CD009382.pub2. [DOI] [PubMed] [Google Scholar]
- Lin A.; Arnold B. F.; Afreen S.; Goto R.; Huda T. M. N.; Haque R.; Raqib R.; Unicomb L.; Ahmed T.; Colford J. M.; et al. Household environmental conditions are associated with enteropathy and impaired growth in rural Bangladesh. Am. J. Trop. Med. Hyg. 2013, 89 (1), 130–137. 10.4269/ajtmh.12-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rah J. H.; Cronin A. A.; Badgaiyan B.; Aguayo V. M.; Coates S.; Ahmed S. Household sanitation and personal hygiene practices are associated with child stunting in rural India: a cross-sectional analysis of surveys. BMJ. Open 2015, 5, e005180. 10.1136/bmjopen-2014-005180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears D.; Ghosh A.; Cumming O.. Open defecation and childhood stunting in India: an ecological analysis of new data from 112 districts. PLoS One 2013, 8 ( (9), ) DOI: 10.1371/journal.pone.0073784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears D.How Much International Variation in Child Height Can Sanitation Explain?; Policy Research Working Paper 6351; The World Bank: Washington, DC, 2013.
- Jenkins M. W.; Curtis V. A. Achieving the “good life”: why some people want latrines in rural Benin. Soc. Sci. Med. 2005, 61, 2446–2459. 10.1016/j.socscimed.2005.04.036. [DOI] [PubMed] [Google Scholar]
- Jenkins M. W.; Scott B. Behavioral indicators of household decision-making and demand for sanitation and potential gains from social marketing in Ghana. Soc. Sci. Med. 2007, 64 (12), 2427–2442. 10.1016/j.socscimed.2007.03.010. [DOI] [PubMed] [Google Scholar]
- Mahon T.; Fernandes M. Menstrual hygiene in South Asia: a neglected issue for WASH (water, sanitation and hygiene) programmes. Gend. Dev. 2010, 18 (1), 99–113. 10.1080/13552071003600083. [DOI] [Google Scholar]
- Jasper C.; Le T.-T.; Bartram J. Water and sanitation in schools: a systematic review of the health and educational outcomes. Int. J. Environ. Res. Public Health 2012, 9 (8), 2772–2787. 10.3390/ijerph9082772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton G.; Haller L.; Bartram J.. Economic and Health Effects of Increasing Coverage of Low-Cost Household Drinking-Water Supply and Sanitation Interventions to Countries off-Track to Meet MDG target 10; World Health Organization: Geneva, Switzerland, 2007.
- Kar K.; Chambers R.. Handbook on Community-Led Total Sanitation; Plan UK and Institute of Development Studies: Brighton, England, 2008; Vol. 44. [Google Scholar]
- IDS. The CLTS approach. http://www.communityledtotalsanitation.org/page/clts-approach (accessed Feb 1, 2015).
- Federal Democratic Republic of Ethiopia. The WaSH Implementation Framework; Federal Democratic Republic of Ethiopia: Addis Ababa, Ethiopia, 2011; 138 pp.
- Venkataramanan V.Testing CLTS Approaches for Scalability: Systematic Literature Review; Plan International USA Inc.: Washington, D.C., 2012; https://waterinstitute.unc.edu/files/2015/03/CLTS-Systematic-Literature-Review-Final-Report-Appendix-1-4.pdf.
- Pickering A. J.; Djebbari H.; Lopez C.; Coulibaly M.; Alzua M. L. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. Lancet Glob. Heal. 2015, 3, e701–e711. 10.1016/S2214-109X(15)00144-8. [DOI] [PubMed] [Google Scholar]
- Whaley L.; Webster J. The effectiveness and sustainability of two demand-driven sanitation and hygiene approaches in Zimbabwe. J. Water, Sanit. Hyg. Dev. 2011, 1 (1), 20–36. 10.2166/washdev.2011.015. [DOI] [Google Scholar]
- Clasen T. F.; Boisson S.; Routray P.; Torondel B.; Bell M.; Cumming O.; Ensink J.; Freeman M. C.; Jenkins M. W.; Odagiri M.; et al. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: a cluster-randomised trial. Lancet Glob. Heal. 2014, 2 (14), e645–e653. 10.1016/S2214-109X(14)70307-9. [DOI] [PubMed] [Google Scholar]
- Dickinson K. L.; Patil S. R.; Pattanayak S. K.; Poulos C.; Yang J.-C. Nature’s call: impacts of sanitation choices in Orissa, India. Econ. Dev. Cult. Change 2015, 64 (1), 1–29. 10.1086/682958. [DOI] [Google Scholar]
- Pattanayak S. K.; Yang J.-C.; Dickinson K. L.; Poulos C.; Patil S. R.; Mallick R. K.; Blitstein J. L.; Praharaj P. Shame or subsidy revisited: social mobilization for sanitation in Orissa, India. Bull. World Health Organ. 2009, 87 (8), 580–587. 10.2471/BLT.08.057422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil S. R.; Arnold B. F.; Salvatore A. L.; Briceno B.; Ganguly S.; Colford J. M.; Gertler P. J. The effect of India’s Total Sanitation Campaign on defecation behaviors and child health in rural Madhya Pradesh: a cluster randomized controlled trial. PLoS Med. 2014, 11 (8), 1–17. 10.1371/journal.pmed.1001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears D.Effects of rural sanitation on infant mortality and human capital: evidence from India’s Total Sanitation Campaign; Research Program in Development Studies Working Paper;Princeton University: Princeton, NJ, 2012.
- Schmidt W.-P. The elusive effect of water and sanitation on the global burden of disease. Trop. Med. Int. Health 2014, 19 (5), 522–527. 10.1111/tmi.12286. [DOI] [PubMed] [Google Scholar]
- Glasgow R. E.; Klesges L. M.; Dzewaltowski D. A.; Bull S. S.; Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice?. Ann. Behav. Med. 2004, 27 (1), 3–12. 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- Madon T.; Hofman K. J.; Kupfer L.; Glass R. I. Implementation science. Science 2007, 318, 1728–1729. 10.1126/science.1150009. [DOI] [PubMed] [Google Scholar]
- Besley T.; Ghatak M. Reforming public service delivery. J. Afr. Econ. 2007, 16 (1), 127–156. 10.1093/jae/ejm026. [DOI] [Google Scholar]
- Hunter D. J. Relationship between evidence and policy: a case of evidence-based policy or policy-based evidence?. Public Health 2009, 123, 583–586. 10.1016/j.puhe.2009.07.011. [DOI] [PubMed] [Google Scholar]
- WHO/UNICEF. Progress on Drinking Water and Sanitatation: 2014 Update; WHO: Geneva, Switzerland, 2014.
- Federal Ministry of Health. Health Extension Program in Ethiopia: Profile; Addis Ababa, Ethiopia, 2007; 24 p.
- Chambers R.School-Led Total Sanitation: Reflections on the Potential of the Shebedino Pilot Pioneered by Plan Ethiopia and the Local Administration; Community-Led Total Sanitation: Brighton, England, 2011.
- Blanton E.; Ombeki S.; Oluoch G. O.; Mwaki A.; Wannemuehler K.; Quick R. Evaluation of the role of school children in the promotion of point-of-use water treatment and handwashing in schools and households-Nyanza Province, Western Kenya, 2007. Am. J. Trop. Med. Hyg. 2010, 82 (4), 664–671. 10.4269/ajtmh.2010.09-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen A.; Ma H.; Ou J.; Billhimer W.; Long T.; Mintz E.; Hoekstra R. M.; Luby S. P. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am. J. Trop. Med. Hyg. 2007, 76 (6), 1166–1173. [PubMed] [Google Scholar]
- Freudenthal S.; Ahlberg B. M.; Mtweve S.; Nyindo P.; Poggensee G.; Krantz I. School-based prevention of schistosomiasis: initiating a participatory action research project in northern Tanzania. Acta Trop. 2006, 100, 79–87. 10.1016/j.actatropica.2006.09.013. [DOI] [PubMed] [Google Scholar]
- Magnussen P.; Ndawi B.; Sheshe A. K.; Byskov J.; Mbwana K.; Christensen N. O. The impact of a school health programme on the prevalence and morbidity of urinary schistosomiasis in Mwera Division, Pangani District, Tanzania. Trans. R. Soc. Trop. Med. Hyg. 2001, 95, 58–64. 10.1016/S0035-9203(01)90333-5. [DOI] [PubMed] [Google Scholar]
- Ethiopian Ministry of Health. Implementation Guideline for CLTSH Programming; Ethiopian Ministry of Health: Addis Ababa, Ethiopia, 2012, 35 p.
- Ethiopian Ministry of Health. CLTSH verification and certification protocol; Ethiopian Ministry of Health: Addis Ababa, Ethiopia, 2012.
- Plan International Ethiopia. Teacher-Facilitated Community-Led Total Sanitation: Implementation Narrative; Plan International Ethiopia: Addis Ababa, Ethiopia, 2015.
- Plan International Ethiopia. Trainers’ Guide on Community-Led Total Sanitation and Hygiene (CLTSH) Approaches; Plan International Ethiopia: Addis Ababa, Ethiopia, 2012; 72 pp.
- Crocker J.; Rowe R.. Community-Led Total Sanitation in Ethiopia: Findings from a Situational Assessment; Plan International Ethiopia: Addis Ababa, Ethiopia, 2015; http://waterinstitute.unc.edu/files/2015/03/situational-assessment-ethiopia-2015-02.pdf.
- Pattanayak S. K.; Poulos C.; Yang J.-C.; Patil S. R.; Wendland K. J. Of taps and toilets: quasi-experimental protocol for evaluating community-demand-driven projects. J. Water Health 2009, 7 (3), 434–451. 10.2166/wh.2009.059. [DOI] [PubMed] [Google Scholar]
- Pattanayak S. K.; Pfaff A. Behavior, environment, and health in developing countries: evaluation and valuation. Annu. Rev. Resour. Econ. 2009, 1, 183–217. 10.1146/annurev.resource.050708.144053. [DOI] [Google Scholar]
- Guiteras R.; Levinsohn J.; Mobarak A. M. Encouraging sanitation investment in the developing world: a cluster-randomized trial. Science 2015, 348 (6237), 903–906. 10.1126/science.aaa0491. [DOI] [PubMed] [Google Scholar]
- Hernandez O.; Tobias S.. Access and behavioral outcome indicators for water, sanitation, and hygiene. USAID Hygiene Improvement Project: Washington, D.C., 2010; 81 p.
- Grosh M.; Glewwe P.. Designing Household Survey Questionnaires for Developing Countries: Lessons from 15 Years of the Living Standards Measurement Study; The World Bank: Washington, DC, 2000. [Google Scholar]
- Bartram J.; Brocklehurst C.; Fisher M. B.; Luyendijk R.; Hossain R.; Wardlaw T.; Gordon B. Global monitoring of water supply and sanitation: history, methods and future challenges. Int. J. Environ. Res. Public Health 2014, 11, 8137–8165. 10.3390/ijerph110808137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton G.; Haller L.; Bartram J. Global cost-benefit analysis of water supply and sanitation interventions. J. Water Health 2007, 5 (4), 481–502. 10.2166/wh.2007.009. [DOI] [PubMed] [Google Scholar]
- Clasen T. F.; Bostoen K.; Schmidt W.-P.; Boisson S.; Fung I. C. H.; Jenkins M. W.; Scott B.; Sugden S.; Cairncross S. Interventions to improve disposal of human excreta for preventing diarrhoea (review). Cochrane Libr. 2010, 6, 32. 10.1002/14651858.CD007180.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waddington H.; Snilstveit B.; White H.; Fewtrell L.. Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhoea in Developing Countries; 3ie: New Delhi, India, 2009.
- Lee W.; Stoeckel J.; Jintaganont P.; Romanarak T.; Kullavanijaya S. The impact of a community based health education program on the incidence of diarrheal disease in southern Thailand. Southeast Asian J. Trop. Med. Public Heal. 1991, 22 (4), 548–556. [PubMed] [Google Scholar]
- Tyndale-Biscoe P.; Bond M.; Kidd R.. Plan International ODF Sustainability Study; Community-Led Total Sanitation: Brighton, England, 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.