Abstract
Background and Objectives
Substance use disorders among youth remain a serious public health problem. Although research has overwhelmingly supported the use of evidenced-based interventions, one of the primary limitations of the current evidence base is that for the vast majority of treatments, the developers of the treatments are also the ones conducting research on them, raising the possibility of allegiance bias.
Methods
The present study was an independently conducted randomized controlled trial (n =126) comparing an evidenced-based treatment for adolescent substance use, Adolescent-Community Reinforcement Approach (A-CRA), and assertive continuing care (ACC), to services as usual (SAU) provided by a juvenile probation department. Latent growth curve modeling was used to compare the treatments on change in substance use assessed by the Global Appraisal of Individual Needs (GAIN) at baseline and 3, 6, and 12 months following treatment entry.
Results
All youth evidenced a substantial reduction in substance use frequency and substance-related problems following treatment; however, youth treated with A-CRA/ACC evidenced a substantially greater decrease in substance-related problems.
Conclusions and Scientific Significance
Results are consistent with studies conducted by A-CRA/ACC model developers supporting the effectiveness of the clinical approach and, because the outcomes resulted from an independent replication, are encouraging for the transportation potential of A-CRA/ACC.
BACKGROUND AND OBJECTIVES
After a period of decline throughout the 1980s and early 1990s, recent years have seen a resurgence in drug use among America’s youth.1 In recent years, modifications have occurred in the services landscape resulting in many adolescents with substance use disorders receiving treatment in the juvenile justice system.2 Fortunately, research suggests that treatments originally developed to reach youth in traditional substance abuse treatment settings are also effective when implemented in the juvenile justice system.3,4
In spite of research documenting the progress that developing and evaluating empirically supported treatments (ESTs) has had on the field of substance use treatment, the evidence-based practice movement has also been the topic of considerable debate with both sides citing important and relevant concerns including the influence of allegiance bias, the influence of researchers’ therapeutic allegiance on the results of treatment outcome studies. Indeed, in Chambless and Hollon’s landmark paper5 establishing definitions for ESTs that persist to the current day, these authors emphasize the importance of: (1) the need for independent replications and (2) testing treatments in typical treatment settings. Both of these features are included in the current study. Empirically, recent data suggest that the developers of treatments investigated in randomized controlled trials (RCTs) tend to report larger pre- to post-treatment effect sizes for the experimental treatment, compared to those reported by researchers with low or no allegiance to the same treatment.6 Because treatments that have been rigorously investigated are typically the candidates for wide-scale dissemination, independent replication supporting the effectiveness of empirically supported treatments is necessary to provide some generalizability in treatment effects and thereby extend the field’s progress in broaching the research-practice divide.
The current study reports the results of an independently conducted RCT of the Adolescent-Community Reinforcement Approach followed by assertive continuing care as compared to services as usual for adolescents under the community supervision of a juvenile probation agency. The site for this study, along with 10 other sites located throughout the United States, received funding from SAMHSA/CSAT (TI-06-007) to implement A-CRA/ACC. The site at which the current study was conducted is the only site that implemented an RCT design. The effectiveness of A-CRA for adolescent substance use problems has been supported in randomized clinical trials and a large-scale implementation study with demographically diverse youth treated in various settings.7,8 ACC has shown promise in two randomized controlled trials of adolescents discharged from residential treatment,9,10 the findings from which have been more impressive than when it has been used as a standalone intervention (ie, not being preceded by A-CRA) following outpatient treatment.11 Based on previous studies indicating that SAU comparisons can show decreases with justice-involved youth,12–14 we hypothesized that both treatment and SAU comparison groups would show decreases in the frequency of substance use and substance-related problems, but that decreases would be significantly greater for youth treated with A-CRA/ACC relative to those who received SAU.15,16
METHODS
Participants
One hundred twenty-six youth between the ages of 12 and 17 (M =15.2, SD =1.07) living in a rural/suburban area of southeast Texas participated in this study. Eligibility criteria for the study consisted of: (1) being between the ages of 12 and 17 years of age; (2) indicating a moderate to severe alcohol or drug use problem on the GAIN-Short Screener17 (GAIN-SS; see below); and (3) a willingness to participate in 3 months of treatment along with follow-up assessments. Potential participants were excluded if they demonstrated symptoms of severe psychopathology such as intellectual disabilities, acute suicidality, or psychotic symptoms, or had a history of violent offenses (per JPD regulations). A power analysis conducted via simulation algorithms included in the software Mplus indicated that the study was adequately powered to detect a medium effect size (d =.5) with a projected sample of 120.
The participants were largely male (74%) and White, Non-Hispanic (79%), with smaller proportions identifying as Hispanic (14%), Black/African American (6%), and Asian (1%), consistent with the demographic characteristics of the area. All youth were under community supervision of the local juvenile probation department (JPD)—typically consisting of regular meetings with a JPO (weekly for most youth) and drug testing via urine specimens—through the duration of the study. Referrals from the JPD are generally received from law enforcement officers, school officials, justice and municipal courts, and other probation departments. Please see Table 1 for more detail on participants’ clinical characteristics.
TABLE 1.
Sample characteristics
| Variable | A-CRA (n =63) | SAU (n =63) | p |
|---|---|---|---|
| Gender | .403 | ||
| Male | 50 (79) | 46 (73) | |
| Female | 13 (21) | 17 (27) | |
| Ethnicity | .455 | ||
| Caucasian/White | 47 (75) | 49 (78) | |
| African American | 3 (5) | 4 (6) | |
| Hispanic | 9 (14) | 9 (14) | |
| Other | 4 (6) | 1 (2) | |
| Family type | .960 | ||
| Both parents | 19 (30) | 21 (33) | |
| Single parent | 33 (52) | 33 (52) | |
| Other | 11 (18) | 9 (15) | |
| AOD abuse/dependencea | 55 (87) | 56 (89) | .783 |
| Comorbiditya | |||
| GAD | 9 (14) | 9 (14) | 1.00 |
| Depressive disorder | 27 (43) | 27 (43) | 1.00 |
| Conduct disorder | 32 (52) | 36 (57) | .535 |
| ADHD | 29 (46) | 27 (43) | .720 |
ACRA, adolescent community reinforcement approach; ADHD, attention deficit hyperactivity disorder; AOD, alcohol and/or other drug; GAD, generalized anxiety disorder; M, mean; n, number of participants; SAU, services as usual; SD, standard deviation.
Diagnoses are approximated from GAIN items and should not be considered clinically definitive.
Procedure
The current study was approved and monitored by two Institutional Review Boards (IRB): the Protection of Human Subjects Committee at Sam Houston State University and the Phoenix House IRB. Recruitment for participants began in February 2008 and continued through June 2010. Participants were screened for eligibility by the JPD using the GAIN-SS. Adolescents identified as having a moderate or severe alcohol or drug use problem by the GAIN-SS or who were known to be using drugs by youths’ juvenile probation officers (JPOs) were invited to participate in the study by an outreach specialist.
Prior to randomization or beginning treatment, adolescents completed an intake assessment conducted by assessors trained and certified in administering study measures (see below). Assessments were conducted in locations convenient for the participants, typically their homes. The assessments were administered verbally by trained doctoral students who logged responses into a laptop computer or using paper and pencil. Follow-up assessments were conducted at 3, 6, and 12 months following intake, and participants were compensated $20 for completing each of these assessments. Assessments using the measures described below typically lasted approximately 2 hours for the baseline and 1 hour for the follow-ups.
Following completion of the intake assessment, a project coordinator randomized participants to receive A-CRA/ACC or SAU using the Urn Randomization software18 to ensure equivalence on the following variables: age, gender, race, number of previous arrests, and severity of drug use as measured by the GAIN-SS. Participants and their caregiver(s) were alerted to the treatment to which they were assigned following randomization. All participants randomized were included in the intent-to-treat (ITT) analyses.
Treatment Conditions
A-CRA/ACC
A-CRA was developed for adolescents as an adaptation of the Community Reinforcement Approach (CRA), an intervention developed for the treatment of alcohol abuse in adults.19 In 1997, work began to adapt CRA and expand its use to adolescent substance users. This culminated in the manualization of the newly adapted treatment20 for the Cannabis Youth Treatment study.7 While the general structure of CRA was maintained, various components were added or modified to make the treatment developmentally appropriate and increase its effectiveness in adolescent populations. The treatment is designed for weekly sessions delivered over 3–4 months and is flexible in terms of the settings in which it is delivered.
ACC is a home-based continuing care approach that works in conjunction with A-CRA. In the present study, ACC services were delivered over a 12–14-week period beyond the initial episode of A-CRA. ACC case managers are trained in the A-CRA approach and combine the techniques described above with assertive case management (eg, providing transportation to high school equivalency degree classes).
SAU
Adolescents randomized to SAU typically received one of the following services: (1) drug education class (21% [n =13]); (2) alternative education program administered by the juvenile probation program (10% [n =6]); (3) individual counseling provided by counselors at the juvenile probation department or in the community (41% [n =26]); (4) diversion (11% [n =7]); and (5) family intervention (8% [n =5]). All SAU options included regular contact with a JPO and varying contact with mental health professionals. Of these options, the individual counseling provided the most consistent contact, with weekly sessions being the norm. Drug education consisted of developmentally appropriate prevention programming provided by Master’s level clinicians. Formal services outside of JPO contact were not required in the diversion condition. Theoretically, the youth could have been assigned to more intensive programs as well, including a twice-weekly intensive substance use program and a drug court, but these options were not used in the current study. Subsequent analyses showed no differences in treatment outcomes between these programming options.
All adolescents were under community supervision provided by JPOs while receiving treatment, which lasted approximately 6 months. Both interventions had approximately the same planned duration and level of JPO involvement.
Treatment Fidelity
Given the variety of options available for the SAU condition, many of which were not standardized/manualized interventions, we have fidelity data only for therapists delivering the A-CRA/ACC condition. Five therapists and one case manager delivered the A-CRA/ACC condition. Clinical supervision was provided by two supervisors trained and certified in A-CRA/ACC, occurred on a weekly basis, and included audiotape review and feedback on a session rated for treatment fidelity.
Clinicians, both therapists and case manager, were certified under a standardized implementation model21 with funding provided as part of the SAMHSA/CSAT implementation effort. It included standardized training for clinicians and onsite supervisors, fidelity assessment and feedback, and ongoing coaching. Clinicians submitted audio-recordings of their sessions via a secure internet-based portal; these sessions were in turn rated for fidelity to the A-CRA/ACC model by trained raters. Treatment fidelity was primarily monitored by the first author and lead clinical supervisor with some support provided by the treatment developers through bi-monthly coaching calls provided to all sites as part of the implementation effort. Fidelity scores were based on a coding manual containing operational definitions for components subsumed in a total of 15 procedures, along with overall A-CRA/ACC philosophy and objectives and overall clinical skills.22 Previous studies describe the procedures involved in training raters and have established interrater reliability for the ratings.23 After therapists were certified in the approach, random fidelity reviews were conducted to assess ongoing adherence to the intervention.
The A-CRA/ACC Exposure Scale (AES)24 is a count indexing the number of unique A-CRA/ACC procedures a client received during their treatment episode and ranges from 0 to 15. On average, participants received a score of 9.8 on the AES (SD =2.3), as compared to an AES of 8.9 reported in Garner et al.24
Measures
Client characteristics, outcomes, and services received came from the Global Appraisal of Individual Needs (GAIN).25 Research indicates GAIN subscales have demonstrated good-to-excellent internal consistency (α =.74–.90) in girls and boys of diverse cultural backgrounds and in diverse settings.26 Compared to family/collateral data and urine testing, the GAIN has demonstrated moderate to excellent consistency (K =.70–.90).27
The GAIN’s Substance Problem Scale (SPS) measures severity of drug use problems. It has good internal consistency (α =.88) and test-retest reliability (r =.73),26 as well as strong convergent validity with other measures of substance abuse and dependence.28 The GAIN Substance Frequency Scale (SFS) consists of six items and measures the amount and frequency of alcohol and other drug use within the past 90 days. The SFS has demonstrated good internal consistency (α =.88).29
In addition to these self-report assessments, a program administrator provided the research team with a deidentified dataset containing the number of JPO contacts made with each youth. Because youth in both conditions were monitored by their JPOs for approximately 6 months following entry to the study, we included the number of contacts as a covariate in the outcome analyses reported below.
RESULTS
Baseline Characteristics
Between-treatment equivalence was tested using analyses of variance (for continuous variables) and chi-square tests (for categorical variables). Results of statistical tests for continuous measures are reported here, and those for categorical variables are included in Table 1. The two groups were similar in age (A-CRA: M =15.08, SD =1.11; SAU: M =15.30, SD =1.03; t [124] =1.17, ns) as well as having a similar number of lifetime arrests (A-CRA: M =1.79, SD =3.74; SAU: M =1.84, SD =1.39; t [124] =.95, ns). There were no significant differences (p <.05) between treatment groups at baseline on any variable.
Consent and Attrition Rates
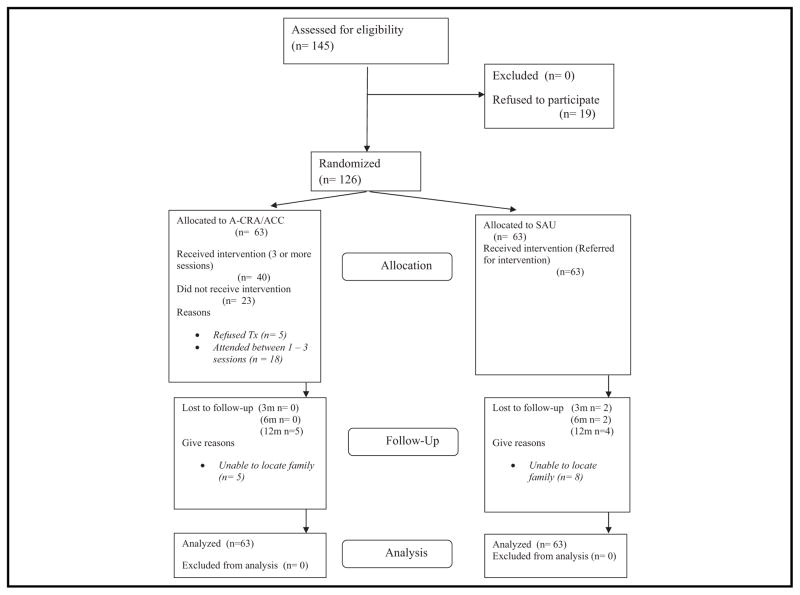
One hundred forty-five youth met the study’s eligibility criteria. Nineteen participants either declined to participate themselves or their parents did not provide their permission, resulting in a 87% consent rate. Assessment attrition rates after randomization (total at each assessment point) were: 3 months: 3%; 6 months: 6%; 12 months: 10%. There were no differences in assessment follow-up rates between the two treatments (ps are .310, .465, and .380 for 3-, 6-, and 12-month follow-ups, respectively). See Fig. 1 for details on the CONSORT flow chart.
FIGURE 1.
CONSORT flow diagram.
Data Analytic Approach
Latent growth curve (LGC) modeling using robust maximum likelihood estimation was used to analyze individual client change. Missing data were handled with full information maximum likelihood (FIML) estimation, under the assumption that the data were missing at random (MAR).30 To evaluate the MAR assumption we correlated background characteristics and baseline values of our outcome measures with a variable reflecting missingness in any of our outcome variables at any assessment point. These correlations were uniformly small (range r =.04–.14). Along with intervention condition, we included gender, age, ethnicity, and number of JPO contacts as covariates to the LGC models to test the impact of intervention type on initial status and change over time (ie, the intercept and slope growth parameters) above the influence of the covariates. Intervention effects were demonstrated by a statistically significant slope parameter, as tested by the pseudo-z test associated with treatment condition. LGC modeling was conducted using Mplus (Version 7.1).31 Both effect sizes (Cohen’s d) and significance tests associated with intervention effects are reported. Effect sizes were calculated using methods developed for growth curve modeling.32
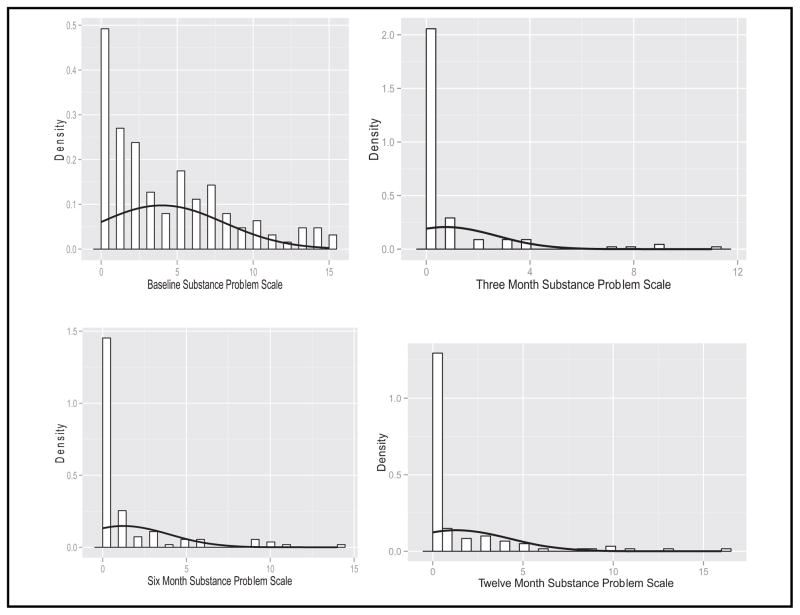
Examination of kernel density plots (see Fig. 2) revealed a high proportion of participants reporting no substance use at each assessment. Therefore, we used a two-part growth modeling approach33 to estimate separate but correlated continuous and categorical LGC models. Two-part growth modeling was specifically developed to address non-normality caused by a preponderance of zeros.34 As implemented in Mplus, two-part growth modeling applies a natural log transformation to the continuous outcomes. The modeling approach was successful in bringing skewness and kurtosis within acceptable levels (<2). Further, we used the robust maximum likelihood estimator for all analyses to minimize the impact of non-normality on the results.
FIGURE 2.
Kernel density plots for GAIN Substance Problem Scale at each assessment.
Treatment Outcomes
Please see Table 2 for descriptive statistics for substance use outcomes. As hypothesized, youth in both treatment and comparison groups showed significant reduction in substance use frequency and problems. The proportion of youth reporting no use (the categorical part of the frequency model) significantly increased (Mean Slope =−.58, standard error [SE] =.09, pseudo-z =−6.78, p <.001), and among those reporting continued use (the continuous part of the model), frequency significantly decreased over time (Mean Slope =−.39, SE =.07, pseudo-z =−5.72, p <.001). Similarly, results indicate an increasingly greater number of participants from both conditions reporting no problems (Mean Slope =−.64, SE =.11, pseudo-z =−6.05, p <.001) and significant decreases among those reporting problems (Mean Slope =−.13, SE =.05, pseudo-z =−2.42, p =.016).
TABLE 2.
Means and standard deviations for substance use outcome variables
| Outcome measure | Intake
|
3 months
|
6 months
|
12 months
|
Effect sizea |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Substance problem scale | .98 | ||||
| A-CRA/ACC | 4.51 (4.51) | .56 (1.52) | .90 (2.10) | 1.16 (2.34) | |
| SAU | 3.48 (3.56) | .97 (2.28) | 1.64 (3.19) | 1.53 (3.42) | |
| No substance problems | |||||
| A-CRA/ACC (n [%]) | 14 (22) | 50 (81) | 44 (73) | 38 (66) | |
| SAU (n [%]) | 17 (27) | 42 (70) | 36 (62) | 40 (73) | |
| Substance frequency scale | .39 | ||||
| A-CRA/ACC | .23 (.18) | .04 (.09) | .04 (.09) | .06 (.09) | |
| SAU | .18 (.16) | .04 (.09) | .05 (.09) | .07 (.15) | |
| No substance use | |||||
| A-CRA/ACC (n [%]) | 2 (3) | 40 (65) | 32 (53) | 24 (41) | |
| SAU (n [%]) | 4 (6) | 33 (55) | 30 (52) | 24 (44) | |
ACC, assertive community care; A-CRA, adolescent community reinforcement approach; M, mean; n, number of participants; SAU, services as usual; SD, standard deviation.
Effect size shown is Cohen’s d for treatment comparison for the continuous part of the two-part model.
Comparing the treatments, youth receiving A-CRA/ACC showed a significantly greater decrease in the continuous part of the substance use problems two-part model (Treatment Slope =−.26, SE =.10, pseudo-z =−2.64, p =.008, d =.98). These differences were not significant for the substance use frequency model (Treatment Slope =−.07, SE =.13, pseudo-z =−.53, ns, d =.39). Likewise, there were no differences in the categorical parts of the models for both outcomes (Frequency: Treatment Slope =−.01, SE =.32, pseudo-z =−.04, ns, d =.04; Problems: Treatment Slope =−.06, SE =.23, pseudo-z =−.23, ns, d =.19).
DISCUSSION AND CONCLUSIONS
The primary question addressed in the current study is the effectiveness of A-CRA/ACC as compared to existing services for substance using, justice-involved youth. Youth in both treatment and comparison groups significantly decreased the frequency of their substance use and problems associated with it—68% and 66% decreases, respectively—over the 12 months following their entry to the study. Therefore, it is clear that both treatment and comparison groups were effective, and the results are clinically meaningful. With respect to substance use frequency, participants on average decreased from using an average of 23% of the days in the previous 90 to 4% of the days for A-CRA/ACC and from 18% to 4% with SAU (see Table 2). Not only did they decrease the frequency of use, but a large enough proportion of adolescents reported abstaining from substance use over the previous 90 days at both 6- and 12-month follow-ups (65%/53% and 55%/52% for A-CRA/ACC and SAU, respectively) that it necessitated we used a modeling approach that accounted for the large number of zeros participants reported. Further, youth receiving A-CRA/ ACC decreased their problems associated with substance use significantly more than youth receiving services as usual, with the effect size indicating a large magnitude difference. The findings from this study are consistent with other studies demonstrating that A-CRA/ACC is an effective intervention for youth with substance use disorders7,10,35 and extends the positive findings resulting from ACC to outpatient treatment. The positive findings in the present study may have been facilitated by the continuation of A-CRA procedures carried through both the primary and continuing care outpatient phases.
The sample comprising the current study was comparable to previous A-CRA studies in terms of substance use, but unlike previous A-CRA/ACC studies, all participants in the current study were involved in the justice system. Treatment delivery was consistent with the A-CRA/ACC described in previous implementation studies,8,10 and the clinicians delivered the intervention with satisfactory fidelity. Effect sizes demonstrated in the current study were larger than those obtained in previous A-CRA/ACC studies assessing substance use frequency (typically small: f =.127; f =.0410; β =.1135), particularly the large effect size associated with participants who reported at least some substance problems over the follow-up period. Therefore, the overall aim of the project—to independently replicate results from previous A-CRA trials—was achieved. However, it should be mentioned that of the four treatment contrasts examined, only one showed significant between-treatment differences. Further, the abstinence rates found in the current study should be interpreted in line with the proverbial glass “ half full.” While the optimistic interpretation is that the roughly 50% abstinence rate at 12 months is consistent with a large literature of adolescent substance abuse treatment trials,36 one could also argue that 50% of youth returning to drug use (at least once) is insufficient. Perhaps abstinence rates achieved with adolescents could be strengthened by extending ACC further in time and drawing from recent work with adult continuing care interventions.37,38
In terms of the clinical relevance and policy implications of the study’s findings, it must be noted that A-CRA/ACC was implemented with substantial front-end work and costs that may constitute a barrier to implementation for some juvenile probation agencies. However, a broader perspective is necessary to evaluate this treatment’s dissemination potential. Most notably, A-CRA/ACC has been successfully disseminated—in 43 states and over 250 provider organizations, many of which serve a high proportion of justice-involved youth.35 While a less-intensive, presumably less costly (at least in terms of front end costs) option may be more attractive than a treatment such as A-CRA/ACC to programs looking to enhance their substance abuse treatment services, several points should be considered. First, A-CRA/ACC has proved to be cost-effective when compared to other research-supported treatments.7 Second, it should be noted that the significant treatment effect favoring A-CRA/ACC was realized with the Substance Problem Index, which assesses clinically significant problems including DSM IV substance abuse and dependence symptoms. A-CRA/ACC reduced these problems by 88% (compared to 72% with SAU) at 3 months and 74% (compared to 56% with SAU) at 12 months. Third, A-CRA is a very flexible approach consisting of a menu of 19 different procedures that clinicians are trained to individualize to the particular needs of each client and has demonstrated effectiveness over a wide range of substance use and co-occurring problem impairment.39 Many JPDs, similar to the one in the current study, offer a range of services with an attempt to match service intensity to adolescent impairment. Therefore, the fact that A-CRA/ACC performed better than a combination of five different SAU options suggests that services may actually be consolidated (with improved clinical outcomes and potential cost savings) by implementing A-CRA/ACC with justice-involved adolescents. An additional advantage of A-CRA/ACC relative to SAU is well-defined, standardized fidelity monitoring integrated within the clinical supervision process.
Limitations
The findings of the current study should be considered in light of several limitations. The major limitation related to the current findings is the lack of diversity. Youth participating in this study were 75% male and 80% Caucasian, and therefore, the extent of the generalizabililty of findings reported here to females or youth of other ethnicities is yet unknown. However, prior large-scale research has shown A-CRA to be effective across gender and ethnicity.8 Second, the intensity of the services provided to youth randomized to SAU varied as youth were assigned to several different options. Unfortunately, our sample size was not large enough to allow us to stratify by treatment intensity to provide a stronger test of our primary hypothesis, although post hoc treatment comparisons indicated there were no differences in treatment outcomes between the different SAU programming options. Of note, some of the more commonly used options (drug education, diversion) were less intense than the ACRA/ACC treatment, which precludes us from concluding with certainty that treatment type, rather than treatment intensity, was responsible for the superior outcomes realized by those receiving ACRA/ACC. Third, the outcomes we report here were also based on youth self-reports, and therefore could not be substantiated by the results of urine testing.
In conclusion, A-CRA/ACC was supported as an effective treatment for juvenile justice involved adolescents with substance use disorders. This treatment was delivered by bachelor and master level therapists hired from the community, and counseling sessions were conducted at the JPD and client homes over a period of time commensurate with standard practice. Therefore, it is representative of services that could conceivably be delivered in other communities with justice-involved youth, albeit with some initial investment in training and certifying clinical staff. Further, the study was an independent replication conducted in actual practice settings in accordance with Chambless’s and Hollon’s recommendations for establishing empirically supported therapies.5 In sum, the results suggest that A-CRA/ACC is a viable option for treating justice-involved youth and that this treatment should be more widely disseminated and adopted by juvenile justice agencies.
Acknowledgments
This research was supported by the Center for Substance Abuse Treatment Grant (Rockville, MD) TI-17817 (Craig Henderson, PI); support for GAIN follow-up assessments was provided by National Institute on Drug Abuse Grant R01 DA011323 (Michael Dennis, PI).
We are thankful for the partnerships with our collaborators at Montgomery County Juvenile Probation Department and the Phoenix House of Texas and for the families that participated in this study.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2010. Institute for Social Research, The University of Michigan; Ann Arbor: 2011. [Google Scholar]
- 2.Hawkins EH. A tale of two systems: Co-Occurring mental health and substance abuse disorders treatment for adolescents. Annu Rev Psychol. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- 3.Hogue AT, Henderson CE, Ozechowski TJ, et al. Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007–2013. J Clin Child Adolesc Psychol. 2014;43:695–720. doi: 10.1080/15374416.2014.915550. [DOI] [PubMed] [Google Scholar]
- 4.Boustani M, Henderson CE, Liddle HA. Family-based treatments for adolescent substance abuse: How scientific advances yield new developmental challenges. In: Brown SA, Zuckerds RA, editors. The Oxford Handbook of Adolescent Substance Abuse. New York: Oxford University Press; 2016. [Google Scholar]
- 5.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- 6.Leykin Y, DeRubeis RJ. Allegiance in psychotherapy outcome research: Separating association from bias. Clin Psychol. 2009;16:54–65. [Google Scholar]
- 7.Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Godley SH, Hedges K, Hunter B. Gender and racial differences in treatment process and outcome among participants in the adolescent community reinforcement approach. Psychol Addict Behav. 2011;25:143–154. doi: 10.1037/a0022179. [DOI] [PubMed] [Google Scholar]
- 9.Godley MD, Godley SH, Dennis ML, et al. A randomized trial of assertive continuing care and contingency management for adolescents with substance use disorders. J Consult Clin Psychol. 2014;82:40–51. doi: 10.1037/a0035264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godley MD, Godley SH, Dennis ML, et al. The effect of assertive continuing care on continuing care linkage, adherence, and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- 11.Godley SH, Garner BR, Passetti LL, et al. Adolescent outpatient treatment and continuing care: Main findings from a randomized controlled trial. Drug and Alcohol Depend. 2010;110:44–54. doi: 10.1016/j.drugalcdep.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dakof GA, Henderson CE, Rowe CL, et al. A randomized controlled trial of multidimensional family therapy in juvenile drug court. J Family Psychol. 2015;29:232–241. doi: 10.1037/fam0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henggeler SW, Melton GB, Brondino MJ, et al. Multisystemic therapy with violent and chronic juvenile offenders and their families: The role of treatment fidelity in successful dissemination. J Consult Clin Psychol. 1997;65:821–833. doi: 10.1037//0022-006x.65.5.821. [DOI] [PubMed] [Google Scholar]
- 14.Henggeler SW, Pickrel SG, Brondino MJ. Multisystemic treatment of substance-abusing and -dependent delinquents: Outcomes, treatment fidelity, and transportability. Ment Health Serv Res. 1999;1:171–184. doi: 10.1023/a:1022373813261. [DOI] [PubMed] [Google Scholar]
- 15.Chamberlain P, Reid J. Comparison of two community alternatives to incarceration for chronic juvenile offenders. J Consult Clin Psychol. 1998;6:624–633. doi: 10.1037//0022-006x.66.4.624. [DOI] [PubMed] [Google Scholar]
- 16.Curtis NM, Ronan KR, Borduin CM. Multisystemic treatment: A meta-analysis of outcome studies. J Family Psychol. 2004;18:411–419. doi: 10.1037/0893-3200.18.3.411. [DOI] [PubMed] [Google Scholar]
- 17.Dennis ML, Chan Y-F, Funk R. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing, and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15:80–91. doi: 10.1080/10550490601006055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stout RL, Wirtz PW, Carbonari JP, et al. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- 19.Hunt GM, Azrin NH. A community-reinforcement approach to alcoholism. Behav Res Therapy. 1973;11:91–104. doi: 10.1016/0005-7967(73)90072-7. [DOI] [PubMed] [Google Scholar]
- 20.Godley SH, Meyers RJ, Smith JE, et al. The Adolescent Community Reinforcement Approach (ACRA) for Adolescent Cannabis Users, Cannabis Youth Treatment Manual Series. Vol. 4. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. DHHS Publication No. (SMA) 01–3489. [Google Scholar]
- 21.Godley SH, Garner BR, Smith JE, et al. A large-scale dissemination and implementation model for evidence-based treatment and continuing care. Clin Psychol. 2011;18:67–83. doi: 10.1111/j.1468-2850.2011.01236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith JE, Lundy SL, Gianini L. Community Reinforcement Approach (CRA) and Adolescent Community Reinforcement Approach (A-CRA) Therapist Coding Manual. Normal, IL: Chestnut Health Systems; 2007. [Google Scholar]
- 23.Smith JE, Gianini LM, Garner BR, et al. A behaviorally-anchored rating system to monitor treatment integrity for community clinicians using the adolescent community reinforcement approach. J Child Adolesc Subst Abuse. 2014;23:185–199. doi: 10.1080/1067828X.2012.729258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garner BR, Godley SH, Funk RR, et al. Exposure to adolescent community reinforcement approach treatment procedures as a mediator of the relationship between adolescent substance abuse treatment retention and outcome. J Subst Abuse Treat. 2009;36:252–264. doi: 10.1016/j.jsat.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dennis ML, Titus JC, White M, et al. Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures. Bloomington, IL: Author; 2003. Retrieved from http://www.gaincc.org/gaini. [Google Scholar]
- 26.Lennox R, Dennis ML, Ives M, et al. The construct and predictive validity of different approaches to combining urine and self-reported drug use measures among older adolescents after substance abuse treatment. Am J Addit. 2006;15S:92–101. doi: 10.1080/10550490601006089. [DOI] [PubMed] [Google Scholar]
- 27.Dennis ML, Funk R, Godley S, et al. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99:120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- 28.Smith DC, Hall JA, Williams JK, et al. Comparative efficacy of family and group treatment for adolescent substance abuse. Am J Addict. 2006;15S:131–136. doi: 10.1080/10550490601006253. [DOI] [PubMed] [Google Scholar]
- 29.Titus JC, Dennis ML, White WL, et al. Gender differences in victimization severity and outcomes among adolescents treated for substance abuse. Child Maltreat. 2003;8:19–35. doi: 10.1177/1077559502239612. [DOI] [PubMed] [Google Scholar]
- 30.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2. New York: Wiley; 2002. [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2014. [Google Scholar]
- 32.Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown EC, Catalano RF, Fleming CB, et al. Adolescent substance use outcomes in the raising healthy children project: A two-part latent growth curve analysis. J Consult Clin Psychol. 2005;73:699–710. doi: 10.1037/0022-006X.73.4.699. [DOI] [PubMed] [Google Scholar]
- 34.Olsen MK, Schafer JL. A two-part random-effects model for semi-continuous longitudinal data. J Am Stat Assoc. 2001;96:730–745. [Google Scholar]
- 35.Hunter BD, Godley SH, Hesson-McInnis MS, et al. Longitudinal change mechanisms for substance use and illegal activity for adolescents in treatment. Psychol Addict Behav. 2014;28:507–515. doi: 10.1037/a0034199. [DOI] [PubMed] [Google Scholar]
- 36.Winters KC, Botzet AM, Fahnhorst T. Advances in adolescent substance abuse treatment. Curr Psychiatry Rep. 2011;13:416–421. doi: 10.1007/s11920-011-0214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McKay JR, Van Horn DH, Lynch KG, et al. An adaptive approach for identifying cocaine dependent patients who benefit from extended continuing care. J Consult Clin Psychol. 2013;81:1063. doi: 10.1037/a0034265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Godley SH, Hunter BD, Fernandez-Artamendi S, et al. A comparison of treatment outcomes for adolescent community reinforcement approach participants with and without co-occurring disorders. J Subst Abuse Treat. 2014;46:463–471. doi: 10.1016/j.jsat.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]