Abstract
Study Objectives:
Poor sleep is a risk factor for the development and recurrence of depression. Selective serotonin reuptake inhibitor (SSRI) use is consistently associated with good subjective sleep in clinically depressed patient populations. However, studies in the general population are lacking. Our objective was to investigate the association between SSRIs and subjective sleep in a middle-aged and elderly population in a daily practice setting.
Methods:
We included participants from the prospective Rotterdam Study cohort. Participants had up to two subjective sleep measurements assessed with Pittsburgh Sleep Quality Index ([PSQI], number of measurements = 14,770). SSRI use was based on pharmacy records. We assessed the association between SSRIs and PSQI score and its sub-components, with nonusers of any antidepressant as reference. Analyses were, among others, adjusted for presence of depressive symptoms and concurrent psycholeptic drug use.
Results:
We included 9,267 participants, average baseline age 66.3 y (standard deviation 10.6), and 57.6% women. SSRI use was significantly associated with a 0.78-point lower PSQI score (95% confidence interval [CI] −1.11; −0.44) which reflects better sleep, compared with non-use. The association was more prominent in continuous SSRI users (−0.71 points, 95% CI −1.18; −0.24). Of the sub-components, SSRIs were associated with 0.70-h longer sleep duration (95% CI 0.56; 0.85), higher sleep quality, higher sleep efficiency, and in contrast more daytime dysfunction.
Conclusions:
SSRI use was associated with better subjective sleep, after adjustment for depressive symptoms and concurrent psycholeptic drug use. This suggests that, in clinical practice in the middle-aged and elderly population, the sleep quality of some persons may benefit from, continued, SSRI use.
Citation:
Aarts N, Zuurbier LA, Noordam R, Hofman A, Tiemeier H, Stricker BH, Visser LE. Use of selective serotonin reuptake inhibitors and sleep quality: a population-based study. J Clin Sleep Med 2016;12(7):989–995.
Keywords: antidepressive agents, population surveillance, questionnaires, sleep
INTRODUCTION
Sleep and depression are highly associated. The most common disturbances in the sleep pattern of a depressed person are low sleep efficiency and little deep sleep.1–4 Poor sleep has been shown to be a risk factor for the development or recurrence of depression.2,5–8 However, antidepressant drugs can have positive and negative effects on sleep.9–13
Selective serotonin reuptake inhibitors (SSRIs) are considered as activating antidepressants and a risk factor for poor sleep according to most objective sleep measurements, although sedative properties and daytime somnolence have occasionally been reported for SSRIs.10,12–16 Studies in non-depressed individuals regarding the association between SSRIs and subjective sleep reported inconsistent results.9,11,12,17–21 Whereas, in clinically depressed patient populations, SSRI use is consistently associated with an improved subjective sleep.3,9,11,22 The favorable results in depressed populations might represent the improvement of mental health or relief of depressive symptoms.9,22 So far, most studies focused on subjective perception of sleep as a secondary outcome in clinical trials of antidepressants that are limited by small sample size, short follow-up, or concomitant benzodiazepine use.23 To our knowledge, to date, no population-based study investigated whether SSRIs are associated with better subjective sleep in the middle-aged and elderly population.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Use of SSRIs is consistently associated with good subjective sleep in clinically depressed patient populations. However, to our knowledge, no population-based study investigated whether SSRIs are associated with good subjective sleep in the middle-aged and elderly population in daily practice.
Study Impact: Our results suggest that sleep quality in the middle-aged and elderly population may benefit from continued SSRI use. This is important, as a patient's own perception is relevant in the course of treatment, relief of depressive symptoms and overall well-being.
Therefore, our objective was to investigate the association between SSRI use and different subjective sleep parameters in a population-based cohort study. Additionally, to evaluate the effect of sleep medication and depressive symptoms, we adjusted for concurrent psycholeptic drug use or presence of depressive symptoms and studied potential effect modification.
METHODS
Setting
The Rotterdam Study is a prospective population-based cohort study that investigates incidence of, and risk factors for, several age-related diseases. The study was initiated in 1990, and after extension over the years, comprises a total of 14,926 participants. All participants were 45 y or older at baseline. After baseline examination, follow-up examinations were conducted every 4 to 5 y. Extensive information on morbidity and mortality is available for participants on a day-to-day basis from general practitioner records. Detailed information on design, objectives and methods of the Rotterdam Study has been published elsewhere.24,25 The Rotterdam Study has been approved by the medical ethics committee according to the Wet Bevolkingsonderzoek: ERGO (Population Study Act Rotterdam Study), executed by the Ministry of Health, Welfare and Sports of the Netherlands. Written informed consent was signed by all study participants.
Study Population
We included participants from interview rounds from January 2002 through December 2008 and March 2009 through January 2014. These interview rounds included the Pittsburgh Sleep Quality Index (PSQI).26 A total of 9,897 and 6,874 participants, respectively, underwent home interview during these rounds. Measurements of participants with considerable cognitive impairment (Mini-Mental State Examination [MMSE] score below 24),27 measurements with less than 5 (out of 7) valid sleep components on the PSQI,26 or measurements from participants who used other antidepressants than SSRIs at the time of interview were excluded from the analyses.
Exposure Definition
Antidepressant drug use was assessed on the basis of pharmacy dispensing records. Electronic pharmacy records were available from January 1, 1991 onward. These include the date of dispensing, the total amount of drug units per prescription, the dispensed daily number of units, the product name of the drug and the Anatomical Therapeutic Chemical (ATC) code.28 The duration of a dispensing was calculated by dividing the total number of dispensed pills/capsules by the prescribed daily number. Treatment episodes were based on consecutive dispensings in which a treatment gap between antidepressant drug dispensings of up to 30 days was still considered as one continuous episode. Participants were considered current users if the interview date fell within an antidepressant drug treatment episode. SSRI users were defined based on the fourth level ATC-code = ‘N06AB’. The average dose was defined as the ratio between the prescribed daily dose and the defined daily dose (PDD/DDD ratio), as determined by the World Health Organization.28 Users of all other antidepressant drugs were excluded from analyses.
Assessment of Sleep Parameters
Based on the Dutch version of the PSQI we assessed subjective sleep parameters.26 The PSQI is a self-rated questionnaire that measures sleep parameters retrospectively over a 1-mo period. The questionnaire consists of seven separate components (sleep duration, sleep disturbances, sleep latency, daytime dysfunction, sleep efficiency, sleep quality, use of sleep medication) with scores ranging from 0 to 3. Based on these seven components a global PSQI score can be calculated, ranging from 0 to 21 in which a higher score corresponds to poorer sleep.26 For our research question, we excluded the component ‘use of sleep medication’ from the global PSQI score, as part of our exposure of interest is equal to the component sleep medication (i.e., benzodiazepines). In the current study, the PSQI score ranged from 0 to 18 points, with a higher score indicative of impaired sleep.
Covariables
We considered the following covariables as potential confounding factors: sex, age, educational level, employment status, body mass index (BMI), depressive symptoms, alcohol intake, and psycholeptic drug use. Except for educational level, all covariables were time-varying and defined at time of the PSQI measurements. Educational level was assessed by home interview at study entry. We categorized educational status in four groups as previously described for the Rotterdam Study and similar to the United Nations Educational, Scientific and Cultural Organization classification (e.g. basic = primary education, low = lower vocational, lower and intermediate general, medium = intermediate vocational, higher general, high = higher vocational and university).29,30 Current employment status (yes/no) was based on questionnaire data. BMI was defined as weight (in kilograms) divided by height (in meters squared), measured at the research center. At the interview rounds, depressive symptoms and alcohol intake were assessed. Depressive symptoms were assessed with a Dutch version of the Center for Epidemiological Studies Depression Scale (CES-D).31 A score of 16 and higher was considered as an indicator for clinically relevant depressive symptoms.32 Alcohol intake was assessed as the average consumption of glasses of alcohol in a week. This amount was converted into grams of alcohol on an average day. Psycholeptic drug use (ATC = ‘N05’) was defined as a dispensing of antipsychotics, anxiolytics, hypnotics, or sedatives within 90 days before an interview date and was based on the available pharmacy dispensing records.
Statistical Analyses
Baseline was defined as the first eligible PSQI measurement of a participant included in the study. Missing values were observed, this percentage was highest for BMI (12.0%) and MMSE score (8.3%). Missing values were handled by multiple imputation using five imputations.
We studied the association between SSRI use and repeated measurements of the global PSQI score and its subcomponents. We used repeated measurement techniques (Generalized Estimating Equations) for our analyses, to take into account within-person correlations between visits. We chose the independent working correlation matrix according to the lowest corrected quasi likelihood under independence model criterion.33,34 Only the global PSQI score and sleep duration were analyzed as continuous variables. Sleep onset latency, sleep disturbances, daytime dysfunction, sleep efficiency, and sleep quality were modeled as binary outcome. For the binary outcomes, the cutoff was based on their questionnaire score (0 to 1 [good sleep] versus 2 to 3 [poor sleep]).
Subsequently, we studied whether there was a dose-response relationship between the average prescribed number of DDDs and global PSQI score, and we assessed the association between individual SSRIs and the global PSQI score. Moreover, we studied effect modification by psycholeptic drug use or by presence of depressive symptoms on the association between SSRI use and the global PSQI score and its subcomponents. Interaction terms were added to the model and results were subsequently stratified by concurrent psycholeptic drug use or by presence of depressive symptoms.
To assess the longitudinal association between SSRI use and PSQI scores at the follow-up measurement round, we used linear and logistic regression models and adjusted for baseline PSQI scores. This enabled us to study the association between SSRI use and PSQI scores, while accounting for interperson differences in sleep at baseline. SSRI exposure was assessed at the baseline and follow-up measurement round and classified as: incident use at the follow-up measurement (incident use), current use at both measurements (continuation of use) or only SSRI exposure at the baseline measurement round (cessation of use). All analyses were compared to non-use of any antidepressant at both measurement rounds.
All statistical models were adjusted for age and sex (model 1), or in the full model additionally adjusted for educational level, employment status, BMI, CES-D score, alcohol intake, and psycholeptic drug use (model 2). Data were analyzed using IBM SPSS statistics (version 21.0, IBM Corp., Somers, NY, USA).
RESULTS
Baseline Characteristics
The total study population consisted of 9,267 participants, with a total of 14,770 PSQI measurements (Figure 1). At baseline, the study population comprised of 57.6% women and a mean age of 66.3 y (standard deviation = 10.6). Baseline characteristics are presented in Table 1.
Figure 1. Flow-chart of the study population.
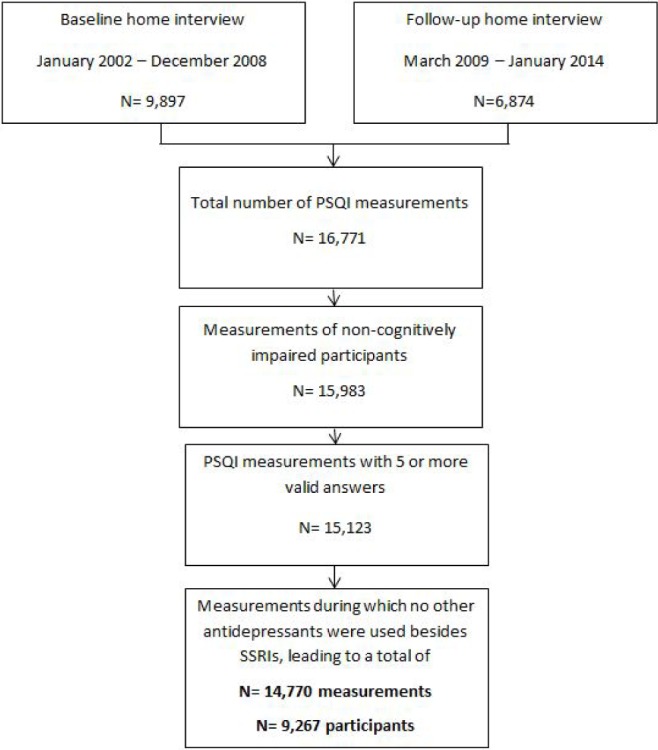
PSQI, Pittsburg Sleep Quality Index; SSRIs, Selective Serotonin Reuptake Inhibitors.
Table 1.
Baseline characteristics of the study population (n = 9,267).
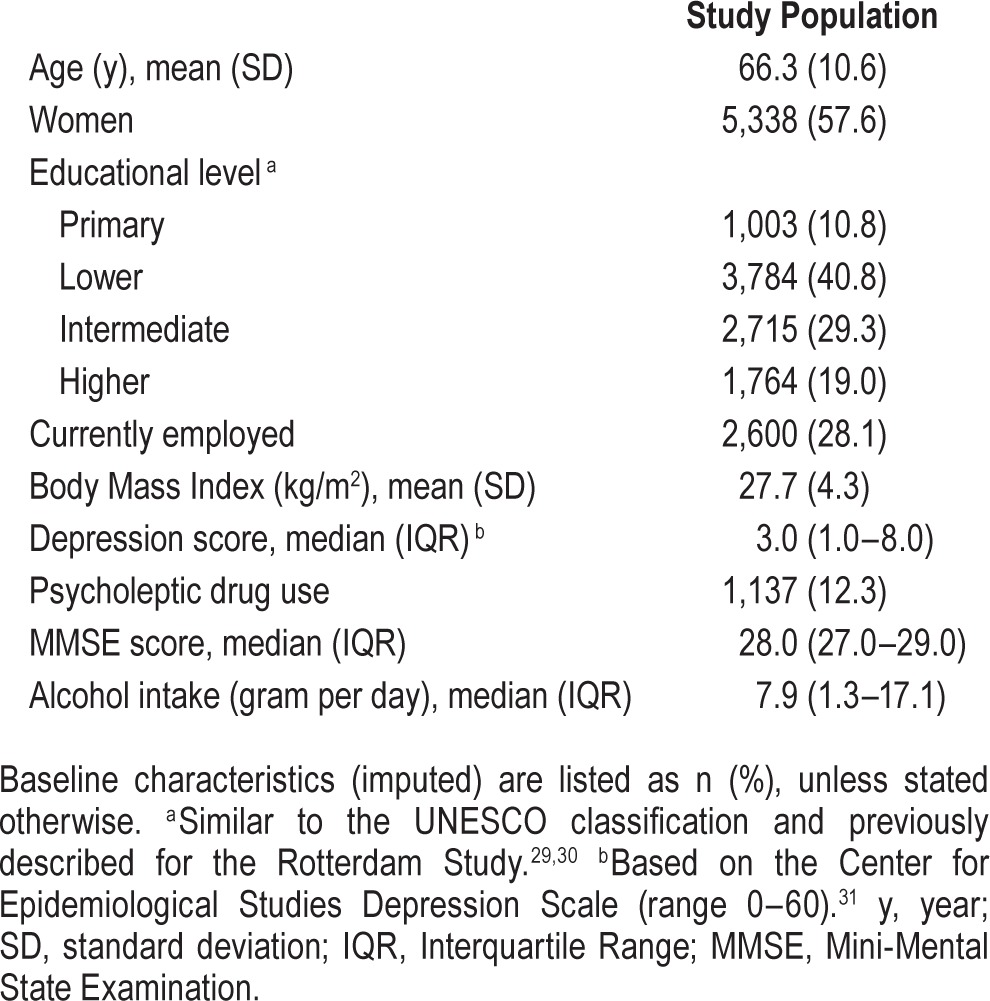
SSRIs and Global PSQI
In the age- and sex-adjusted model, SSRI use was not associated with the global PSQI score (B 0.26; 95% confidence interval [CI] −0.12; 0.63, Table 2). However, after full statistical adjustment, we observed that SSRI use was associated with a significant 0.78-point lower global PSQI score (95% CI −1.11; −0.44), equivalent to a 20.1% difference with non-use. Three PSQI subcomponents significantly contributed to the lower global PSQI score: longer sleep duration (B 0.70 h, 95% CI 0.56; 0.85), better sleep quality (odds ratio [OR] 0.52, 95% CI 0.37; 0.71), and higher sleep efficiency (OR 0.65, 95% CI 0.48; 0.88) in the fully adjusted model. In contrast, SSRI use was associated with more daytime dysfunction (OR 1.48, 95% CI 1.02; 2.16).
Table 2.
Association between selective serotonin reuptake inhibitor use and the global Pittsburg Sleep Quality Index score and its subcomponents.
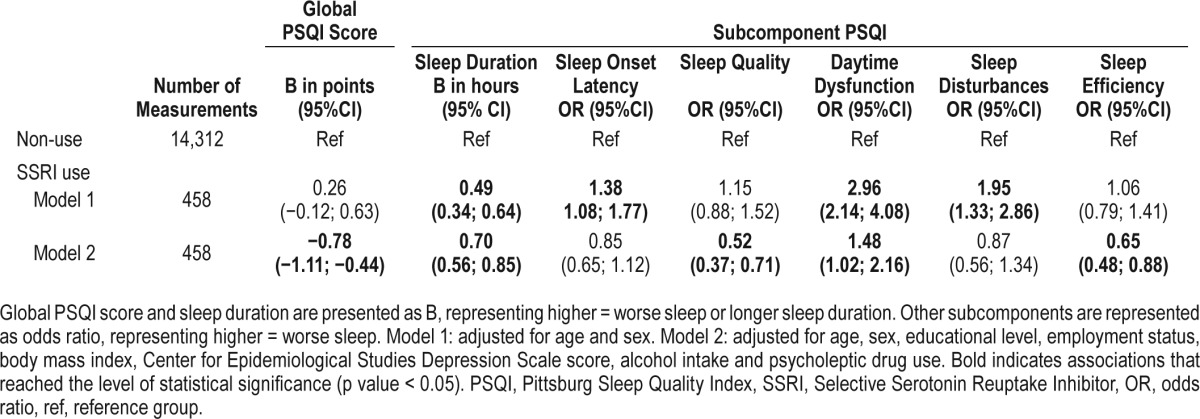
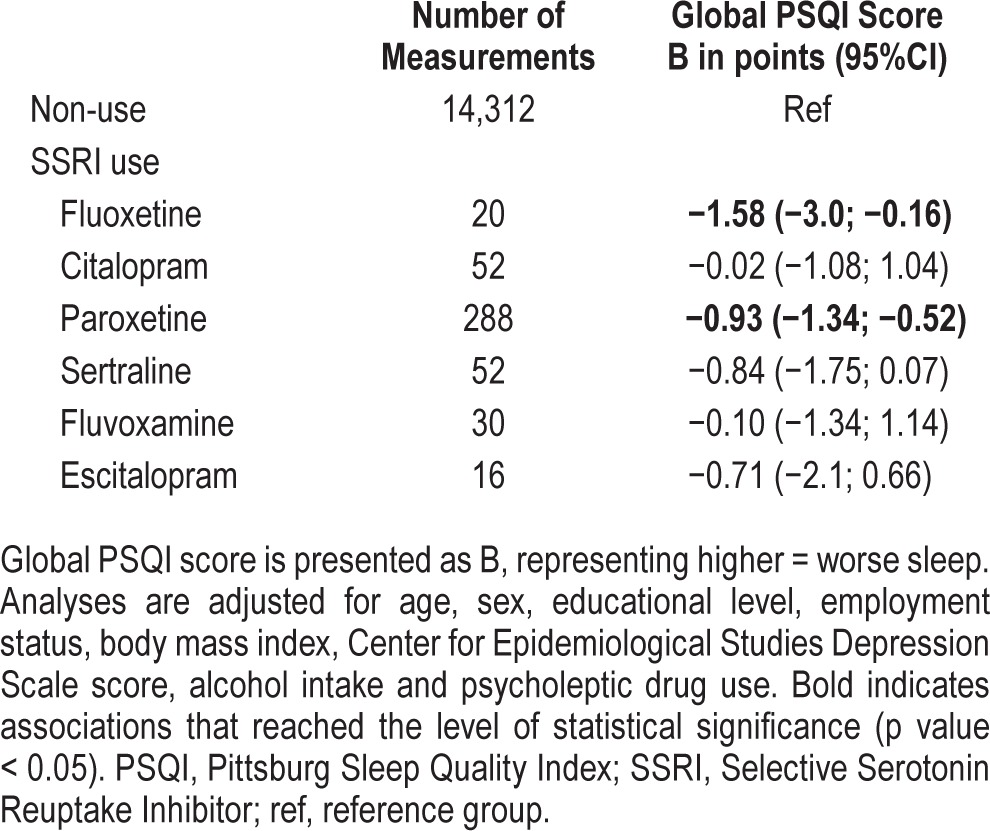
A dose-response relationship was observed between the average prescribed dose and the global PSQI score (p for trend < 0.001, Figure 2). Almost all individual SSRIs were associated with a lower global PSQI score, although not all statistically significant for each SSRI (Table 3). Paroxetine was prescribed in 63% of the measurements in SSRI users. Effect modification by psycholeptic drug use was observed for the association between SSRIs and global PSQI score (p for interaction = 0.048). When stratified by concurrent use of psycholeptic drugs, SSRI use was in both groups associated with a lower global PSQI score, but point estimates were stronger in the group of concurrent psycholeptic drug use (no psycholeptic use: B −0.57, 95% CI −0.94; −0.20, psycholeptic use: B −1.09, 95% CI −1.71; −0.47, respectively, Table S1 in the supplemental material). A longer sleep duration was also observed in both groups and point estimates were stronger in the group of concurrent psycholeptic drug users (p for interaction = 0.005). All other subcomponents were similarly associated with SSRI use when stratified by concurrent psycholeptic drug use. Furthermore, no effect modification by depression score was observed (p for interaction = 0.338), which suggest that the association between SSRIs and global PSQI score was not different in participants with or without clinically significant depressive symptoms.
Figure 2. Association of selective serotonin reuptake inhibitor dose with global Pittsburg Sleep Quality Index score.
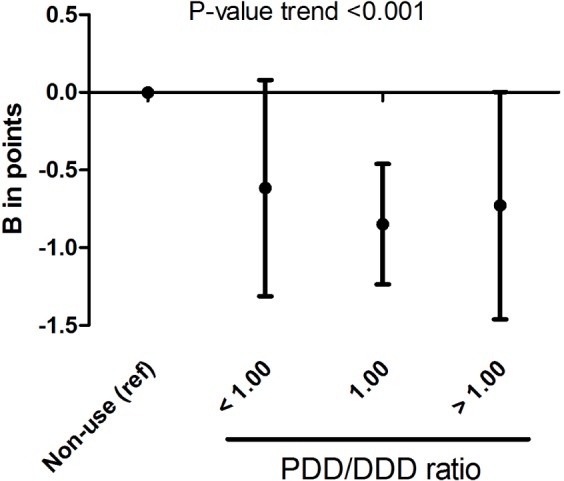
ref, reference group; PDD/DDD ratio, prescribed daily dose/defined daily dose.
Table 3.
Association between use of individual selective serotonin reuptake inhibitors and the global Pittsburg Sleep Quality Index score.
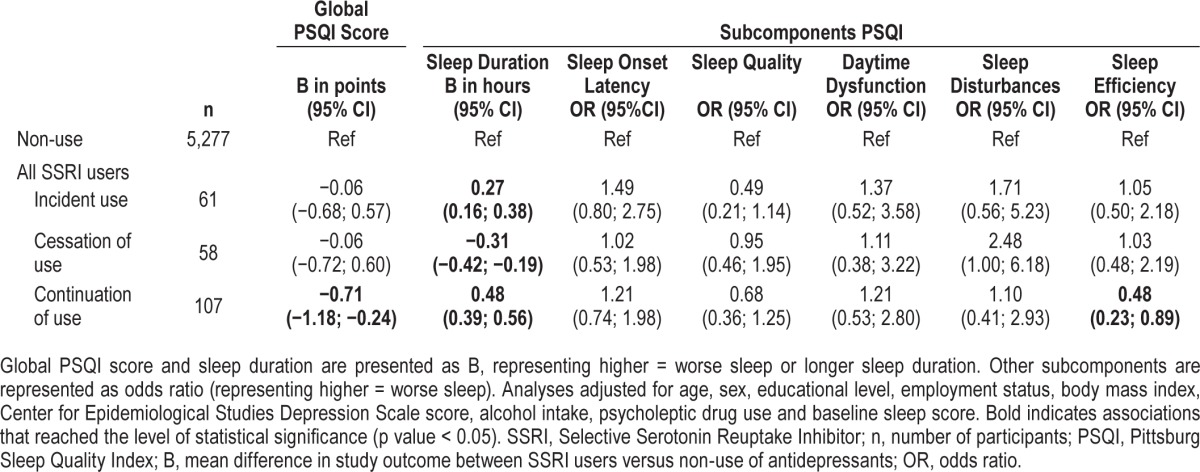
Longitudinal Analyses
Continuation of SSRI use was associated with 0.71-point lower PSQI score (95% CI −1.18; −0.24) and higher sleep efficiency (OR 0.48, 95%CI 0.23; 0.89) at the follow-up measurement round, when we adjusted for the baseline sleep scores and compared with non-users (Table 4). Also, continuation of SSRI use was associated with 0.48 h longer sleep duration (95% CI: 0.39; 0.56), and this was to a lesser extent also observed in incident SSRI users (B 0.27 h, 95% 0.16; 0.38), when compared with nonuse. However, cessation of SSRI use was associated with 0.31 h shorter sleep duration (95% CI −0.42; −0.19) and borderline significantly with more sleep disturbances (OR 2.48, 95% CI 1.00; 6.18).
Table 4.
Longitudinal association between selective serotonin reuptake inhibitor use and the global Pittsburg Sleep Quality Index score and its subcomponents.
DISCUSSION
The results of this study showed a beneficiary association of SSRI use with subjective sleep. However, use of SSRIs was also associated with a higher risk of daytime dysfunction. These associations were only observed when psycholeptic drug use and presence of depressive symptoms were carefully accounted for. Consistently, these associations were also observed in longitudinal analyses of continuous users.
In clinically depressed populations, SSRI use was repeatedly associated with improved subjective sleep.9,11,22 However, in these previous studies, the improved subjective sleep was possibly biased by the remitting depressive symptoms and more general improvement in mental health.9,22 Typically these studies focused on the change in sleep quality from start of antidepressant treatment until the end of treatment. However, results from studies in healthy participants are still inconsistent with respect to their effect of SSRIs on sleep quality.9,11,12,17–22 Our results suggest that SSRI use is associated with better subjective sleep, after we carefully accounted for presence of depressive symptoms, and ruled out possible effect modification by depressive symptoms. We observed a longer total sleep time, better sleep quality, and higher sleep efficiency. In contrast, we observed an association between SSRI use and a higher risk for daytime dysfunction. Daytime dysfunction assessed with the PSQI is based on trouble staying awake during driving, eating meals, engaging in social activity, and problems with keeping up enthusiasm to get things done. An increased daytime dysfunction might represent residual depressive symptoms that diminish enthusiasm in daily live and daily activities. This would only represent residual symptoms as we already adjusted for presence of depressive symptoms with the CES-D. However, an increased daytime function could also suggest that SSRIs have sedative properties. Therefore, we think our results support the previous literature, which reports sedative properties and beneficial sleep effects of SSRIs in healthy participants.18,20,21 These results were observed for almost all individual SSRIs, but associations were most prominent in fluoxetine and paroxetine users, of which the latter was most often prescribed of all SSRIs (at 63% of the measurements).
Our study, embedded in a population-based cohort, in the middle-aged and elderly population has some novel aspects compared with previous studies. First, SSRI and psycho-leptic drug use was allowed concurrently and associations were present in SSRI users while adjusting for psycholeptic drug use. Beneficial associations of SSRI use were present with or without psycholeptic drug use. Second, we could study the dose-response relationship between SSRI use and global PSQI score. A significant p for trend might suggest a more valid drug effect, although the association was mainly driven by a large group of SSRI users with an average dose of one DDD. Third, we were able to adjust for baseline PSQI scores and took SSRI use at two measurement rounds into consideration, which added a longitudinal component to our analyses. This enabled us to study the association between SSRIs and PSQI scores, irrespective of interperson differences in sleep at baseline. Moreover, we could study the effect of continuous use, incident use or cessation of SSRI treatment on subjective sleep. As our cross-sectional and longitudinal results of continuous users were in line with each other, this would suggest that our results on SSRIs and subjective sleep are robust. Especially as cessation of treatment seems to be associated with shorter sleep duration and more sleep disturbances. However, we would have expected a stronger beneficial association in incident SSRI users as well. This might suggest that continuous users represent a selected population of SSRI users on successful maintenance treatment, whereas other SSRI users might discontinue unsuccessful treatment. Thus, because of the association in continuous SSRI users and the fact that we used subjective sleep measures, an effect of improvement in mental health might still be present. Nevertheless, our results in the middle-aged and elderly population are important, as a patient's own perception is relevant in the course of treatment, relief of depressive symptoms and overall well-being.11,35
Limitations and Strengths
Strengths of our study are the large sample size, population-based character, and the prospectively gathered electronic pharmacy records that we used to determine antidepressant and psycholeptic drug exposure. Some limitations of our study should be mentioned. First, the PSQI questionnaire and its separate components have not been designed and validated to be used in pharmacoepidemiological studies. However, most previous studies used the Leeds Sleep Evaluation Questionnaire or the sleep factor scores of the Hamilton Rating Scale for Depression, which are also not designed for this specific research question. Still, the PSQI is considered to be a valid questionnaire with a good test-retest reliability.26 Second, confounding by indication might bias our results as depression itself is associated with sleep disorders. However, we observed a positive association between SSRI use and sleep quality and we were able to adjust for, and study effect modification by, depressive symptoms. Moreover, SSRIs have a relatively homogenous indication profile–they are mostly used for depression and anxiety36,37–and these indications have both been negatively associated with sleep quality. Third, the numbers were low in our consecutive analyses with continuous and incident SSRI users, and with numbers of individual SSRI users; therefore, interpretation should be done with caution. Fourth, ideally we would have been able to make a direct individual comparison with objective sleep measurements. Fifth, our results were based on a middle-aged and elderly population and results may not be generalizable for the complete general population. Sixth, drug exposure was based on dispensing records and not on actual intake. However, any misclassification of exposure would probably be random in this setting.
CONCLUSIONS
Within our population-based cohort study of middle-aged and elderly individuals, we observed an association between SSRI use and better subjective sleep. This association was found after carefully taking into account depressive symptoms and concurrent psycholeptic drug use, and was more prominent in continuous users. These results suggest that in the middle-aged and elderly population the sleep quality of some persons may benefit from continued SSRI use in daily practice.
DISCLOSURE STATEMENT
This was not an industry supported study. The Rotterdam Study is supported by the Erasmus MC and Erasmus University Rotterdam; the Netherlands Organization for Scientific Research (NWO); the Netherlands Organization for Health Research and Development (ZonMw); the Research Institute for Diseases in the Elderly (RIDE); the Netherlands Genomics Initiative (NGI); the Ministry of Education, Culture and Sciences; the Ministry of Health Welfare and Sports; the European Commission (DG XII); and the Municipality of Rotterdam. This study was funded by the ZonMw (Netherlands Organization for Health Research and Development) Priority Medicines Elderly program (113101002; non-commercial). The work of Henning Tiemeier is supported by a NWO-ZonMw VIDI grant (number: 017.106.370, Nederlandse Organisatie voor Wetenschappelijk Onderzoek - The Dutch Medical Research Agency). None of the funders had any role in design and conduct of this study; collection, management, analysis, and interpretation of the data; and review, or approval of the manuscript. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study is grateful to all inhabitants, general practitioners, and pharmacists from the Ommoord district for their contribution to the Rotterdam Study.
ABBREVIATIONS
- ATC
Anatomical Therapeutic Chemical
- BMI
body mass index
- CES-D
Center for Epidemiological Studies Depression scale
- CI
confidence interval
- MMSE
Mini-Mental State Examination
- OR
odds ratio
- PDD/DDD ratio
the ratio between the prescribed daily dose and the defined daily dose
- PSQI
Pittsburgh Sleep Quality Index
- SSRI
selective serotonin reuptake inhibitor
REFERENCES
- 1.Thase ME, Kupfer DJ, Fasiczka AJ, Buysse DJ, Simons AD, Frank E. Identifying an abnormal electroencephalographic sleep profile to characterize major depressive disorder. Biol Psychiatry. 1997;41:964–73. doi: 10.1016/S0006-3223(96)00259-4. [DOI] [PubMed] [Google Scholar]
- 2.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–69. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- 3.Argyropoulos SV, Wilson SJ. Sleep disturbances in depression and the effects of antidepressants. Int Rev Psychiatry. 2005;17:237–45. doi: 10.1080/09540260500104458. [DOI] [PubMed] [Google Scholar]
- 4.Thase ME. Depression and sleep: pathophysiology and treatment. Dialogues Clin Neurosci. 2006;8:217–26. doi: 10.31887/DCNS.2006.8.2/mthase. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 6.Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract. 2005;55:864–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Jaussent I, Bouyer J, Ancelin ML, et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep. 2011;34:1103–10. doi: 10.5665/SLEEP.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee E, Cho HJ, Olmstead R, Levin MJ, Oxman MN, Irwin MR. Persistent sleep disturbance: a risk factor for recurrent depression in community-dwelling older adults. Sleep. 2013;36:1685–91. doi: 10.5665/sleep.3128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oberndorfer S, Saletu-Zyhlarz G, Saletu B. Effects of selective serotonin reuptake inhibitors on objective and subjective sleep quality. Neuropsychobiology. 2000;42:69–81. doi: 10.1159/000026676. [DOI] [PubMed] [Google Scholar]
- 10.Winokur A, Gary KA, Rodner S, Rae-Red C, Fernando AT, Szuba MP. Depression, sleep physiology, and antidepressant drugs. Depress Anxiety. 2001;14:19–28. doi: 10.1002/da.1043. [DOI] [PubMed] [Google Scholar]
- 11.Wilson S, Argyropoulos S. Antidepressants and sleep: a qualitative review of the literature. Drugs. 2005;65:927–47. doi: 10.2165/00003495-200565070-00003. [DOI] [PubMed] [Google Scholar]
- 12.Mayers AG, Baldwin DS. Antidepressants and their effect on sleep. Hum Psychopharmacol. 2005;20:533–59. doi: 10.1002/hup.726. [DOI] [PubMed] [Google Scholar]
- 13.DeMartinis NA, Winokur A. Effects of psychiatric medications on sleep and sleep disorders. CNS Neurol Disord Drug Targets. 2007;6:17–29. doi: 10.2174/187152707779940835. [DOI] [PubMed] [Google Scholar]
- 14.Mendels J, Kiev A, Fabre LF. Double-blind comparison of citalopram and placebo in depressed outpatients with melancholia. Depress Anxiety. 1999;9:54–60. [PubMed] [Google Scholar]
- 15.Beasley CM, Jr, Sayler ME, Weiss AM, Potvin JH. Fluoxetine: activating and sedating effects at multiple fixed doses. J Clin Psychopharmacol. 1992;12:328–33. [PubMed] [Google Scholar]
- 16.Gursky JT, Krahn LE. The effects of antidepressants on sleep: a review. Harv Rev Psychiatry. 2000;8:298–306. [PubMed] [Google Scholar]
- 17.Saletu B, Frey R, Krupka M, Anderer P, Grunberger J, See WR. Sleep laboratory studies on the single-dose effects of serotonin reuptake inhibitors paroxetine and fluoxetine on human sleep and awakening qualities. Sleep. 1991;14:439–47. doi: 10.1093/sleep/14.5.439. [DOI] [PubMed] [Google Scholar]
- 18.Vasar V, Appelberg B, Rimon R, Selvaratnam J. The effect of fluoxetine on sleep: a longitudinal, double-blind polysomnographic study of healthy volunteers. Int Clin Psychopharmacol. 1994;9:203–6. doi: 10.1097/00004850-199409000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Ridout F, Meadows R, Johnsen S, Hindmarch I. A placebo controlled investigation into the effects of paroxetine and mirtazapine on measures related to car driving performance. Hum Psychopharmacol. 2003;18:261–9. doi: 10.1002/hup.494. [DOI] [PubMed] [Google Scholar]
- 20.Wilson SJ, Bailey JE, Alford C, Nutt DJ. Sleep and daytime sleepiness the next day following single night-time dose of fluvoxamine, dothiepin and placebo in normal volunteers. J Psychopharmacol. 2000;14:378–86. doi: 10.1177/026988110001400420. [DOI] [PubMed] [Google Scholar]
- 21.Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: a randomized controlled trial. Menopause. 2012;19:848–55. doi: 10.1097/gme.0b013e3182476099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zisapel N, Laudon M. Subjective assessment of the effects of CNS-active drugs on sleep by the Leeds sleep evaluation questionnaire: a review. Hum Psychopharmacol. 2003;18:1–20. doi: 10.1002/hup.455. [DOI] [PubMed] [Google Scholar]
- 23.Clark MS, Smith PO, Jamieson B. FPIN's clinical inquiries: antidepressants for the treatment of insomnia in patients with depression. Am Fam Physician. 2011;84:1–2. [PubMed] [Google Scholar]
- 24.Hofman A, Grobbee DE, De Jong PTVM, Van den Ouweland FA. Determinants of disease and disability in the elderly: The Rotterdam Elderly Study. Eur J Epidemiol. 1991;7:403–22. doi: 10.1007/BF00145007. [DOI] [PubMed] [Google Scholar]
- 25.Hofman A, Murad S, Duijn C, et al. The Rotterdam Study: 2014 objectives and design update. Eur J Epidemiol. 2013;28:889–926. doi: 10.1007/s10654-013-9866-z. [DOI] [PubMed] [Google Scholar]
- 26.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 27.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. ATC/DDD Index 2014. World Health Organization Collaborating Centre for Drug Statistics Methodology Oslo, Norway. [Accessed September 2013]. Available from: http://www.whocc.no/atc_ddd_index.
- 29.United Nations Educational, Scientific and Cultural Organization (UNESCO) International Standard Classification of Education (ISCED) 1976. Available from: http://unesdoc.unesco.org/images/0002/000209/020992eb.pdf.
- 30.van Rossum CTM. Socioeconomic Inequalities in Cardiovascular Disease in an Ageing Population [Thesis] Erasmus University Rotterdam. 1999 [Google Scholar]
- 31.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 32.Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychol Med. 1997;27:231–5. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- 33.Gardiner JC, Luo Z, Roman LA. Fixed effects, random effects and GEE: what are the differences? Stat Med. 2009;28:221–39. doi: 10.1002/sim.3478. [DOI] [PubMed] [Google Scholar]
- 34.Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21:467–74. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- 35.Murata Y, Kamishioiri Y, Tanaka K, et al. Severe sleepiness and excess sleep duration induced by paroxetine treatment is a beneficial pharmacological effect, not an adverse reaction. J Affect Disord. 2013;150:1209–12. doi: 10.1016/j.jad.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 36.Gardarsdottir H, Heerdink ER, van Dijk L, Egberts AC. Indications for antidepressant drug prescribing in general practice in the Netherlands. J Affect Disord. 2007;98:109–15. doi: 10.1016/j.jad.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Noordam R, Aarts N, Verhamme KM, Sturkenboom MC, Stricker BH, Visser LE. Prescription and indication trends of antidepressant drugs in the Netherlands between 1996 and 2012: a dynamic population-based study. Eur J Clin Pharmacol. 2015;71:369–75. doi: 10.1007/s00228-014-1803-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


